Abstract
Background
The implementation of maternity waiting home (MWH) has been used as a strategy to improve maternal health outcomes in low-resource settings such as Ethiopia. However, MWH utilization is low in Ethiopia, and women's access to MWH depends largely on male partners' decisions. This study explored male-partners perspectives of MWHs including their experiences of paternal support in rural Ethiopia.
Study design
An exploratory qualitative study with a phenomenological methodological orientation was performed.
Methods
This study was conducted in Ana-Lemo and Gibe districts of Hadiya Zone, in rural Southern Ethiopia. The study participants were male partners. A purposive sampling technique was used to recruit 47 participants. Data were collected from May 10–25, 2023. Four focus group discussions, 15 in-depth interviews, and observations were conducted. The interviews were audio-recorded, transcribed and the thematic content analysis was performed using ATLAS.ti 7.1.4 software.
Results
This study showed that male-partners participated in spousal communication and provided practical support such as sharing household chores and financial support; however, they did not accompany their spouses to health facilities. Long distances, lack of transportation, poor referral services, and perceived poor quality of care were barriers to maternal health services. Furthermore, male-partners demonstrated poor awareness and unfavorable attitudes of MWHs.
Conclusions
Male-partners participated in spousal communication, shared household chores and provided financial support to their spouses; however, they did not accompany them to health facilities. They had poor awareness and unfavorable attitudes of MWHs. Creating awareness among male partners may improve their attitude towards MWHs and other maternal health services in rural Ethiopia.
Keywords: Qualitative research, Maternity waiting home, Male partners, Paternal support, Maternal health, Ethiopia
What this study adds
-
⁃
This study found that male partners participated in spousal communication, shared household chores and provided financial support. However, they did not accompany their spouses to healthcare facilities during pregnancy.
-
⁃
Male partners demonstrated poor awareness and unfavorable attitudes toward maternity waiting homes.
Implications for practice
-
⁃
Creating awareness through health education among male partners may improve their attitudes toward maternity waiting homes as well as the practices of paternal support.
1. Introduction
The World Health Organization (WHO) recommends the implementation of maternity waiting homes (MWH) as a strategy to improve the maternal and newborn health outcomes in low-resource settings [1]. Maternity waiting home is a shelter located near a qualified health facility where a pregnant woman can stay and be transferred to delivery wards shortly before childbirth, or earlier should complications arise [2]. Ethiopia has implemented MWHs for several decades; however, its utilization is low in the country [3,4].
Some of the important barriers of women's access to MWHs were household chores and the fact that their use of MWHs depends largely on male-partners’ decisions [5,6]. Given the patriarchal dominance, final decisions regarding MWH use in Ethiopia is mainly made by male-partners [7]. In some instances, male-partners prevented women from using MWHs [8]. Studies showed that involving male-partners can contribute to improvements in health behaviors and the use of maternal health services [9]. However, in a study from Ethiopia, only half of the male-partners were involved in MWHs [10], implying significant proportion of male-partners did not involve in MWHs. Some of the important roles of male partners in MWHs included decision-making and securing funds for transport, food, cleaning materials, and clothes for the mother and the newborn to use during and after labor [7].
In a study from rural Zambia, male partners perceived several potential benefits of MWHs, including improved access to health facility delivery services and treatment in case of labor complications [7]. However, studies that explore male partners' perspectives of MWHs are deficient in Ethiopia. Therefore, this study explored male partners’ perspectives of MWHs, including their experiences of paternal support in rural Ethiopia. In this study, male partner refers to the husband of a woman living together at the time of this study.
2. Methods
2.1. Study setting and period
The study was conducted in Gibe and Ana-Lemo districts of Hadiya Zone in rural Southern Ethiopia, from 10th – 25th of May 2023. The two districts were purposefully selected based on the availability of functional MWHs. There were 10 health centers with functional MWHs in these two districts. Based on the information we obtained from the Zonal health department, the total estimated population of the two districts was 295,000 in 2023. Moreover, there was one primary hospital and 42 health posts in the two districts. The livelihood of the population mainly depends on agriculture.
2.2. Study design
An exploratory qualitative study with a phenomenological methodological orientation was performed.
2.3. Sampling technique and sample size
Two districts (Gibe and Ana-Lemo) were selected based on the availability of MWHs. Five health facilities (Megacho, Omochora, Fonko, Achamo, and Bandelecho health centers) which had functional MWHs were selected. Then the participants were recruited using purposive sampling technique from the catchments of the selected health centers. Health centers heads and health extension workers (from remote health posts) assisted in the recruitment of the participants.
As a result, a total of 47 participants were recruited. The participants were allocated to the focus groups and in-depth interviews purposively based on their residence and feasibility of gathering for the focus groups. Four focus group discussions (FGD) with an average number of 8 participants and 15 in-depth interviews (IDI) were performed. The questions for FGDs focused on exploring participants views on MWHs whereas questions for IDI addressed both views on MWHs and experiences of paternal support. Thus, IDIs were primarily used to explore participants’ personal experiences of paternal support, including views on MWHs, whereas FGDs were used to explore perspectives on MWHs. The sample size was determined based on the concept of theoretical saturation [11]. The data saturation was considered when new ideas were no longer obtained from the interviews.
2.4. Study participants
The study participants were male-partners of women who gave birth in the last 12 months and were living together at the time of the study.
2.5. Inclusion criteria
Male-partners of women who had given birth in the last 12 months prior to the study lived at least ≥2 h of walking distance from the nearest health facility, had limited access to transportation, and were willing to participate in the study. All the recruited participants participated in the study.
2.6. Data collection procedures
Data were collected through IDIs, FGDs and observations. Informed consent was obtained from each participant. The interview guides were prepared by the research team members (S1 Appendix & S2 Appendix). The in-depth interviews took 20–45 min whereas the FGDs lasted 30–55 min, and all were audio-recorded.
2.7. Research team composition and their relationship with study participants
The research team was composed of three investigators: two from Jimma University, Ethiopia; and one from Torrens University Australia, Adelaide, Australia. Two assistants who participated in data collection were public health experts. Neither the investigators nor the research assistants had a prior relationship with the participants.
2.8. Data analysis
The FGD and IDI audio-records were transcribed, and thematic content analysis was performed. Data analysis process comprises three steps. First, the primary author developed a priori codebook based on the study objectives and interview guides. Second, this codebook was further refined by the other two investigators, and the coding process was completed by using ATLAS.ti 7.1.4. Third, the codes were categorized into a priori developed themes based on the similarity in participants’ opinions. Newly emerging themes were assessed to see their compatibility with the priori established themes.
We used the Consolidated Criteria for Reporting Qualitative Research (COREQ) checklist [12] to guide reporting of this study. To illustrate the themes, narrative texts were used in combination with quotes from participants.
2.9. Patient and public involvement
It was not possible to involve patients or the public in the design, conduct, reporting, or dissemination plans of our research. The study results will be shared with the participants and the public once published. We thank all the participants.
3. Results
3.1. Characteristics of the participants
The study showed that above half of the participants were in the age group 30–39 years. Likewise, more than half of the participants had no formal education, and nearly three-fourths were farmers (Table 1).
Table 1.
Characteristics of the participants in rural Ethiopia, 2023.
| Characteristics | Category | Number of participants |
|---|---|---|
| Age | 20–29 | 9 |
| 30–39 | 26 | |
| 40–49 | 10 | |
| ≥50 | 2 | |
| Educational status | No formal education | 25 |
| Primary (Grade 1–8) | 12 | |
| Secondary (Grade 9–12) | 6 | |
| Tertiary (> Grade 12) | 4 | |
| Occupation | Farmer | 35 |
| Government employee | 8 | |
| Others* | 4 | |
| Number of children | 0–2 | 11 |
| 3–4 | 24 | |
| ≥5 | 12 |
Others*: Community volunteers or local militia.
3.2. Availability of infrastructures and basic facilities at MWHs
All of the MWHs were found in the compound of the health facilities, and seven of them were independent houses whereas three were rooms originally built as part of the health facility but dedicated for MWH services. The MWHs without pipe water sources transported drinking water from municipality water sources. We observed registration books at eight of the MWHs (Table 2).
Table 2.
Availability of infrastructures and basic facilities at MWHs in rural Ethiopia, 2023.
| Variables | Response category | Frequency |
|---|---|---|
| Type of house | Traditional huts | 2 |
| Corrugated iron | 8 | |
| Number of classes | 2 | 6 |
| ≥3 | 4 | |
| Number of beds | 4 | 7 |
| ≥5 | 3 | |
| Cooking area | Yes | 10 |
| No | 0 | |
| Latrine | Yes | 10 |
| No | 0 | |
| Pipe water | Yes | 7 |
| No | 3 | |
| Bathroom | Yes | 10 |
| No | 0 | |
| Electricity | Yes | 10 |
| No | 0 | |
| Television | Yes | 10 |
| No | 0 | |
| Registration book | Yes | 8 |
| No | 2 |
4. Perspectives on MWHs and paternal support
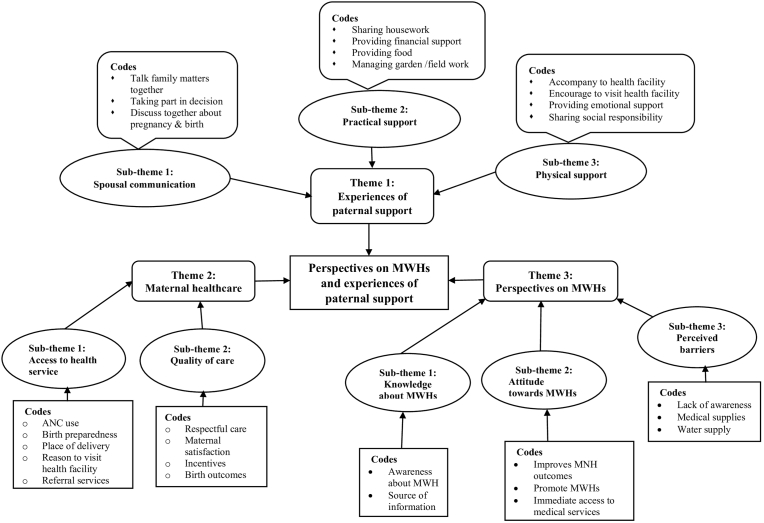
The data were coded and codes were grouped into three themes and eight sub-themes. The themes were experiences of paternal support, maternal healthcare, and perspectives on MWHs (Fig. 1).
Fig. 1.
Codes & themes flowchart.
4.1. Theme 1: experiences of paternal support
4.1.1. Spousal communication
Most participants said they talked with their spouses and made decisions regarding family matters including pregnancy and delivery issues. However, some did not exercise open communication on health matters. They mentioned lack of awareness about maternal health as a reason of poor communication.
“We usually talk and make decisions together. We openly talk about any issue, including health matters. For example, in her last pregnancy, we decided the place of delivery together.” (30–39 years old participant, IDI)
4.1.2. Practical support
Participants supported their spouses by sharing housework; however, some did not involve in any housework activity due to high burden of field works such as gardening and agriculture. In some situations, supporting one's wife was considered foolish due to the patriarchal nature of the family system and gender roles.
“I take care of my children, fetch water, wash clothes, and split firewood. Even I washed her feet although this is considered foolish in some instances.” (40–49 years old participant, IDI)
The participants did not allow their spouses to perform heavy tasks such as ploughing and splitting firewood during pregnancy.
“I provide food for her [my wife] and my children. In the last pregnancy, I prohibited her from ploughing and splitting firewood until one year after delivery.” (20–29 years old participant, IDI)
In addition, participants provided locally available foods to their spouses and cover maternal health service-related costs such as transportation and medication expenditures.
“I am responsible for my family's livelihood including food, transportation, and medications.” (30–39 years participant, IDI)
4.1.3. Physical support
Participants did not provide physical support to their spouses by accompanying them to health facilities during antenatal visits and childbirth. However, they made their spouses to feel relaxed and good and provided support by sharing their social responsibilities, such as participating in 'Iddirs' [Iddir - a local association where people gather and support each other[13].]
“I did not accompany my wife when she visited a health facility for antenatal care or delivery. But I covered her social responsibilities such as ‘Iddirs’.” (30–39 years old participant, IDI)
Participants mentioned that they could not stay with their expectant spouses at home during pregnancy due to various reasons such as work conditions. Family members such as woman's mother or sister stayed with the woman during pregnancy.
“I cannot stay with her at home. If I have to care for the cattle and work in the garden. Usually, stays at home with her mother or sister.” (30–39 years old participant, IDI)
4.2. Theme 2: maternal healthcare
4.2.1. Access to health services
Most of the participants witnessed that their spouses did not visit health facility for antenatal care (ANC). For some mothers, home delivery was the only preferred option as health facility is far from their living areas and access to transportation is limited. Some delivered on the road while being transported to health facilities.
“Only few women visit health facilities for ANC services due to fear of travelling long distances. Sometimes women delivered on the road while going to the health facilities for delivery. That is why women prefer home delivery.” (30–39 years old participant, FGD)
Long distances and lack of transportation were reasons for poor attendance at ANC and skilled birth.
“All of my children were delivered at home. Because we live far from the health facilities and there is no transportation.” (30–39 years old participant, FGD)
In addition, lack of timely referral services affect use of maternal health services. Lack of ambulance services and limited access to transportation aggravated this situation.
“I took her [my wife] to the health center which was 8 km far when labor starts but they referred her to a primary hospital. There was no ambulance for transportation. She delivered on the way before reaching the hospital.” (40–49 years old participant, IDI)
4.2.2. Quality of care
The perceived poor quality of care and health workers behavior affected women's decisions to use maternal health services. Health workers did not welcome women during ANC visits. The participants suggested that providing incentives to women at health facilities may encourage other women to visit health facilities.
“Sometimes health workers do not welcome them [pregnant women]. They are not good especially during labor and birth.”(30–39 years old participant, FGD)
4.3. Theme 3: perspectives on MWHs
4.3.1. Knowledge of MWHs
The participants’ demonstrated poor awareness of the MWHs. Participants who were informed about the existence of MWHs did not know what services were available at the MWHs.
“I was informed about maternity waiting home. It is a home where pregnant women stay until delivery. However, I do not know what services are available at MWHs.” (30–39 years old participant, IDI)
Healthcare professionals were sources of information. Some participants were informed about MWHs by the health workers at health facilities or health extension workers.
“I heard about waiting home when I came to the health center last year with my wife to get our child vaccinated. Nurses informed us. They showed us the home in the compound of a health facility.” (40–49 years old participant, IDI)
4.3.2. Attitude towards MWHs
Participants had unfavorable attitude towards MWHs. They thought that allowing their spouses to stay at MWH would be difficult for them due to housework burden and lack of someone to care for children left at home. They preferred their expectant to stay at home and go to health facility if need arise, rather than staying at MWH.
“I am not sure about the services provided at waiting home. But I think it will be difficult for a woman to stay away from home for weeks. Who will care for the kids and do the housework? Our women usually stay at home until delivery. We take them to health facilities only if they face a problem during labor.” (40–49 years old participant, FGD)
Furthermore, participants stated that women did not want to miss the ceremonies at home during childbirth. They would be surrounded with their families, relatives, and neighbor during labor and after birth while at home. However, they said educating the community about MWH in village and public gatherings (in marketplaces) may improve understanding and attitudes regarding MWH.
“Our women do not want to miss the cultural ceremonies at home during childbirth. They will be surrounded by families, neighbors and relatives. They will miss this if they stay at waiting home. In addition, we do not have proper knowledge about waiting home. I suggest health workers educate the women and community about waiting homes at market places.” (30–39 years old participant, FGD)
4.3.3. Perceived barriers to MWHs
Lack of awareness and problems with basic facilities, such as shortages of water and medical supplies, threaten women's use of MWHs. We observed that some of the MWHs did not have registration books.
“There is a shortage of water in this health center. The women at MWHs are facing the problem of water shortage to cook food and take baths. Sometimes there is a shortage of gloves and syringes.” (20–29 years old participant, FGD)
5. Discussion
Findings of this study showed that male-partners participated in spousal communication, sharing household chores, and financial support; however, they did not accompany their spouses to health facilities. In addition, male-partners had unfavorable attitude and poor awareness of MWHs.
In this study male-partners took part in spousal communication and provided financial support to their spouses; however, they did not accompany them to health facilities. The patriarchal nature of Ethiopian community [14] affects maternal healthcare utilization including MWHs. Likewise, in another study male partners involved in spousal communication and provided financial support to their spouses during pregnancy and childbirth [15,16]. This implies that interventions involving couples to improve maternal health services uptake including MWH may work in these settings, as families have a practice of couple communication, although the practice differs. Such interventions may also improve male partners’ participation in accompanying their spouses during antenatal visits and delivery to health facilities.
The participants also provided practical support to their spouses through sharing household chores. Likewise, a study from Zambia shows male-partners provided food, cleaning supplies, and clothing for the mothers and their newborns [7]. In contrast, other studies show that male-partners provided little or no support to their spouses [17,18]. Our study also revealed that, supporting one's wife is considered foolish. This can discourage paternal support and affect women's access to maternal health services including MWHs. Studies from Kenya and Nepal reveal that the feminization of maternal health issues and stigma discouraged male-partners involvement [15,19]. Therefore, the existence of social and cultural norms discourage paternal support and involvement in maternal health services including MWHs.
In this study, the ANC attendance was poor and women had the only option to prefer home delivery due to geographic barriers. Likewise, other studies show low attendance at ANC[20,21], women prefer traditional birth attendants or faith healers and do not use ANCif there is no illness during pregnancy [15,20], and home delivery was preferred because of lack of household and community support [22]. Long distances and lack of transportation, poor referral services, perceived poor quality of care and behavior of the healthcare staff were reasons for poor attendance at ANC and skilled birth. This is consistent with other studies that show the low quality of health services [23], poor attitude of health workers [24], and geographical distance and unavailability of transport services [15,20] are barriers to maternal health services. It is crucial to consider these factors while performing maternal health service interventions.
The participants had poor awareness of the MWHs. In line with this, another study shows that lack of awareness is one of the barriers that influences male-partners’ participation and women's access to MWHs [10]. In our study, health workers were source of information about MWH. In support of this, other studies stated health workers to be sources of information about MWH [8,25]. This indicates that health workers can be a potential source of information about maternal health services including MWH. In addition, in our study, participants had unfavorable attitude towards MWH. They perceived that it is difficult for women to stay at MWH due to housework and other family responsibilities at home. However, they suggested the promotion of MWHs at public gatherings to create community awareness and attitude towards MWH. In support, another study recommends mass-media campaigns to improve their awareness and attitudes of MWH [25]. This implies that educating the community about MWH may enable them to acquire the awareness of and favorable attitude towards MWH.
In some MWHs, shortages of medical supplies and water were challenges to service provisions. Similarly, other studies revealed that costs related to medical supplies during MWH stay and poor access to clean water are challenges to using MWHs [8,26]. Even though MWH services are free of charge, the lack of basic facilities, including clean water and medical supplies, might discourage women's access to MWHs.
5.1. Strengths and limitations of the study
We used multiple data collection methods, including IDI, FGD, and observations to improve the trustworthiness of the study. However, this study had a limitation. Because, the participants were male-partners whose spouses had given birth in that last 12 months. This might have caused a recall bias in data on experiences of paternal support.
6. Conclusion
This study showed that male-partners participated in spousal communication and provided practical support by sharing household chores and financial support. However, they did not provide physical support such as accompanying their spouses to health facilities. Long distances, lack of transportation, poor referral services, and poor quality of care were perceived barriers to maternal health services. Male-partners showed poor awareness and unfavorable attitude towards MWH. Creating awareness among male partners may improve their attitude towards MWHs and other maternal health services in rural Ethiopia.
Authors’ contributions
T.Y., H.G., and T.B. designed the study, organized the data collection, developed the codebook and analyzed the data. T.Y. prepared the draft manuscript. H.G., and T.B. critically reviewed and provided comments on the draft manuscript. All the authors have read and approved the final manuscript.
Ethics approval
Ethical approval letter was received from the IRB of Jimma University with reference number JUIRB-33/23. Consequently, a letter of permission was obtained from the Health Department of the Hadiya Zone, Southern Ethiopia. An informed consent was obtained from each participant prior to the start of data collection.
Consent for publication
Not applicable.
Availability of data and materials
All additional information is provided as supplementary information.
Funding
The authors did not receive any funding for the conduct or publication of this study.
Informed consent
The purpose of the study is to understand your experience of paternal support and views on MWHs. The information you give us will benefit the women living in remote and rural areas who are suffering from problems of access to health facilities during pregnancy and childbirth. We will interview you for some minutes. Your voices will be recorded; however, your names will not be mentioned in the recording. Rather, codes will be assigned to the recording. We will remove all the voice recordings once we transcribed the data. The data generated from this study will be used for study purpose only. We warmly invite you to participate in this interview. You can withdraw after you we start the interview at any time, if you feel any discomfort.
Consent of the participant
I, the undersigned, have been informed and understood the purpose of the research. I have been told that the information I give will be used for the study purpose only, and my identity and the information I provide will be kept confidentially. Based on this information, I agree to participate in the study voluntarily.
Signature/finger print of the participant.
Declaration of competing interest
The authors declare that they have no competing interests.
Acknowledgements
Our sincere appreciation goes to Jimma University, Institute of Health, for granting the ethical approval for this study. Second, we thank the staff of the Hadiya Zone Health Department and all the study participants for their cooperation. Third, we thank Mizan Tepi University Teaching Hospital for giving us a vehicle (Land Cruiser Pickup) for this study, without which the data collection could have been difficult. Finally, we thank our driver, Mintesinot Shimelis Mekuria, for his great commitment and best driving skills throughout the rural areas, which was adventurous.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.puhip.2024.100513.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.World Health Organization . WHO; 2015. WHO Recommendations on Health Promotion Interventions for Maternal and Newborn Health 2015; p. 94.https://www.who.int/publications/i/item/9789241508742 [Internet] [PubMed] [Google Scholar]
- 2.World Health Organization . WHO; 1996. Maternity Waiting Homes: a Review of Experiences [Internet] p. 40.https://apps.who.int/iris/handle/10665/63432 [Google Scholar]
- 3.Gaym A., Pearson L., Soe K.W.W. Maternity waiting homes in Ethiopia: three decades experience. Ethiop. Med. J. 2012;50(3):209–219. [PubMed] [Google Scholar]
- 4.Kassa B.G., Ayele A.D., Belay H.G., et al. Utilisation of maternity waiting homes and its associated factors in Ethiopia: systematic reviews and meta-analysis. Clin Epidemiol Glob Heal. 2021;12:1–8. doi: 10.1016/j.cegh.2021.100891. [DOI] [Google Scholar]
- 5.Girma W., Tamiru D., Woldie M., et al. Exploring the experience and challenges of maternity waiting homes in Jimma, Southwest Ethiopia. Afr. J. Midwifery Women's Health. 2021;15(1):1–11. doi: 10.12968/ajmw.2020.0007. [DOI] [Google Scholar]
- 6.Sialubanje C., Massar K., van der Pijl M.S.G., et al. Improving access to skilled facility-based delivery services: women's beliefs on facilitators and barriers to the utilisation of maternity waiting homes in rural Zambia. Reprod. Health. 2015;12:61. doi: 10.1186/s12978-015-0051-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sialubanje C., Massar K., Kirch E.M., et al. Husbands' experiences and perceptions regarding the use of maternity waiting homes in rural Zambia. Int. J. Gynaecol. Obstet. 2016;133(1):108–111. doi: 10.1016/j.ijgo.2015.08.023. [DOI] [PubMed] [Google Scholar]
- 8.Kebede K.M., Mihrete K.M. Factors influencing women's access to the maternity waiting home in rural Southwest Ethiopia: a qualitative exploration. BMC Pregnancy Childbirth. 2020;20:296. doi: 10.1186/s12884-020-02988-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Doyle K., Kato-Wallace J. Male engagement in maternal, newborn, and child health: sexual reprodcutive health and rigths. MenCare: a global fatherhood campaign. 2013:39. https://men-care.org/wp-content/uploads/2016/12/Male-Engagement-in-MNCH-SRHR-Guide-Web.pdf [Internet] [Google Scholar]
- 10.Asmare G., Nigatu D., Debela Y. Factors affecting male-partners’ involvement in maternity waiting home utilization in North Achefer district, Northwest Ethiopia: a cross-sectional study. PLoS One. 2020;17:1–19. doi: 10.1371/journal.pone.0263809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Saunders B., Sim J., Kingstone T., et al. Saturation in qualitative research: exploring its conceptualization and operationalization. Qual Quant. 2018;52(4):1893–1907. doi: 10.1007/s11135-017-0574-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tong A., Sainsbury P., Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int. J. Qual. Health Care. 2007;19(6):349–357. doi: 10.1093/intqhc/mzm042. [DOI] [PubMed] [Google Scholar]
- 13.Aredo D. The Iddir : an informal insurance arrangement in Ethiopia. Savings Dev. 2010;34(1):53–70. https://www.jstor.org/stable/41406511 [Google Scholar]
- 14.Dayanandan R. Gender issues in Ethiopia: sounds that reverberate in the highlands. J Int Issues. 2014;18(1):146–159. https://www.jstor.org/stable/48504958 [Google Scholar]
- 15.Bist B.S., Sherchan L.B., Basnet S., et al. Male involvement in reproductive, maternal and child health services: a qualitative study in Dhading district of Nepal. Soc Inq J Soc Sci Res. 2021;3(1):41–57. doi: 10.3126/sijssr.v3i1.46022. [DOI] [Google Scholar]
- 16.Nyamai P.K., Matheri J., Ngure K. Prevalence and correlates of male partner involvement in antenatal care services in Eastern Kenya: a cross-sectional study. Pan Afr Med J. 2022;41 doi: 10.11604/pamj.2022.41.167.31535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Maluka S.O., Peneza A.K. Perceptions on male involvement in pregnancy and childbirth in Masasi District, Tanzania: a qualitative study. Reprod. Health. 2018;15:68. doi: 10.1186/s12978-018-0512-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Aborigo R.A., Reidpath D.D., Oduro A.R., et al. Male involvement in maternal health: perspectives of opinion leaders. BMC Pregnancy Childbirth. 2018;18:3. doi: 10.1186/s12884-017-1641-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lusambili A.M., Muriuki P., Wisofschi S., et al. Male involvement in reproductive and maternal and new child health: an evaluative qualitative study on facilitators and barriers from rural Kenya. Front Public Heal. 2021;9:1–7. doi: 10.3389/fpubh.2021.644293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shibrea G., Zegeyeb B., Idriss-Wheelerc D., et al. Factors affecting the utilization of antenatal care services among women in Guinea: a population-based study. Fam. Pract. 2021;38(2):63–69. doi: 10.1093/fampra/cmaa053. [DOI] [PubMed] [Google Scholar]
- 21.Nxiweni P.Z., Oladimeji K.E., Nanjoh M., et al. Factors influencing the utilization of antenatal services among women of childbearing age in South Africa. Women. 2022;2(3):285–303. doi: 10.3390/women2030027. [DOI] [Google Scholar]
- 22.Teferi H.M., San Sebastian M., Baroudi M. Factors associated with home delivery preference among pregnant women in Ethiopia: a cross-sectional study. Glob. Health Action. 2022;15(1) doi: 10.1080/16549716.2022.2080934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hailu G.A., Weret Z.S., Adasho Z.A., et al. Quality of antenatal care and associated factors in public health centers in Addis Ababa, Ethiopia: a cross-sectional study. PLoS One. 2022;17:1–12. doi: 10.1371/journal.pone.0269710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sharma V., Leight J., Giroux N., et al. “That's a woman's problem”: a qualitative analysis to understand male involvement in maternal and newborn health in Jigawa State, Northern Nigeria. Reprod. Health. 2019;16:143. doi: 10.1186/s12978-019-0808-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gurara M.K., Geertruyden J.-P., Jacquemyn Y., Draulans V. Stakeholders perspectives on the implementation of maternity waiting homes in Rural Ethiopia : a qualitative study. Res Sq [Internet] 2021;1–25 doi: 10.21203/rs.3.rs-971096/v1. [DOI] [Google Scholar]
- 26.Gurara M.K., Jacquemyn Y., Ukke G.G., et al. Benefits, barriers and enablers of maternity waiting homes utilization in Ethiopia: an integrative review of national implementation experience to date. BMC Pregnancy Childbirth. 2022;22:675. doi: 10.1186/s12884-022-04954-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All additional information is provided as supplementary information.