Acute urinary retention refers to the sudden inability to pass urine. It will often be unexpected, usually inconvenient, and always painful. If a man lives long enough his risk of having an episode of acute urinary retention is remarkably high. Over 1 in 10 men in their 70s will experience acute urinary retention within the next five years.1 The risk for men in their 80s is nearly 1 in 3.
Treatment depends largely on where the episode occurred. In some areas men have catheters inserted by their general practitioners (with immediate relief of pain), in others patients have to get to hospital first.2 Once a catheter is inserted treatment depends on local policy. Some men will be sent home with a catheter and collection bag, others will spend a night or two in hospital, and a few will find themselves consenting to prostatectomy the next day.3 Those sent home will have to wait to be readmitted for a trial without catheter or prostatectomy, or both (if the trial fails).
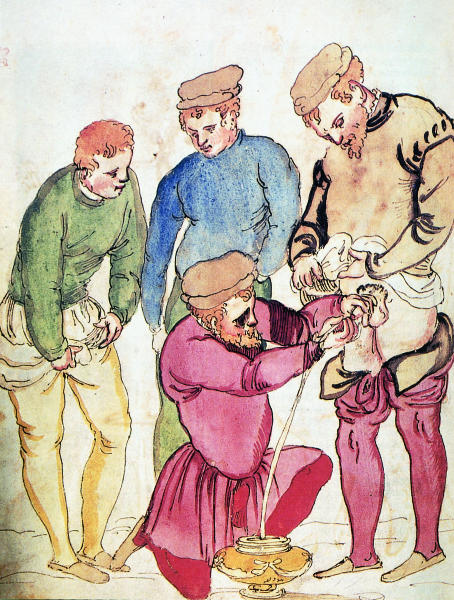
Our understanding of why men develop acute urinary retention has been limited. Until recently, the only way to deal with the condition was to drain the bladder with a catheter. Over the centuries only the materials, silicone rubber instead of silver and ivory, have changed (fig 1). However, recent developments offer hope of better treatment. Firstly, high quality experimental and community based studies have greatly improved our understanding of the epidemiology and pathogenesis of acute urinary retention. Secondly, recent reports suggest that acute urinary retention might be preventable in some men. Thirdly, development in catheter technology might substantially improve management and make hospital admission unnecessary.
Summary points
A man in his 70s has a 1 in 10 chance of experiencing acute urinary retention within 5 years
Men with urinary symptoms, big prostates, and poor urinary flows are at greater risk
Many episodes are precipitated by operations performed under general anaesthetic
Acute urinary retention results in a prostatectomy in about half of men
Finasteride can halve the risk of acute urinary retention over three years compared with placebo
New catheters are being developed that could allow outpatient treatment and reduce the need for prostatectomy
Figure 1.
Silver urethral catheters. Some of these catheters held a piece of caustic in the tip, which was believed to treat urethral obstructions
Methods
As no systematic reviews of acute urinary retention have been published we conducted a Medline search from 1966 to February 1998 using the words acute urinary retention or acute retention of urine. We identified 383 records, and these were reduced to 162 by limiting records to English language reports which contained abstracts on acute urinary retention in men. Most were case reports describing unusual causes of acute urinary retention. We tried to classify these into broad groups. The papers referred to represent what we consider to be the best examples. So as not to overlook recent work, we hand searched abstracts presented at four leading urological congresses in the past two years (American Urological Association, Societé International de Urologie, European Association of Urology, and British Association of Urological Surgeons).
Why does it happen?
We are still not sure what causes acute urinary retention. The many case reports give some indication of the broad range of clinical contexts in which acute urinary retention occurs (box). All the reports describe—either explicitly or implicitly—at least one of three processes. Firstly, there are conditions that require higher than normal pressures to start off the voiding cycle: any event or process which increases the resistance to the flow of urine. This can be either a simple mechanical obstruction such as a foreign body or a dynamic obstruction, which might result from an increase in smooth or striated muscle tone, or both. Secondly, acute urinary retention might result from an interruption of either the sensory innervation of the bladder wall or the motor supply of the bladder muscle. Thirdly, are the cases recognised anecdotally by most urologists in which the bladder has been allowed to overdistend.
Examples of case reports describing unusual presentations of acute urinary retention
Cases which suggest a mechanical obstruction to bladder emptying
Severe urethral inflammation after exposure to a nonoxynol-9 based vaginal contraceptive pessary during unprotected intercourse4
Chronic lymphocytic leukaemia infiltrating the prostate5
Staphylococcal prostatic abscess6
Case which suggests bladder overdistension
Tumour arising from within a giant bladder diverticulum which presented as an abdominal mass7
Cases which suggest increased sphincter tone
Neurofibromatosis in the bladder neck and prostate causing increased tone in external sphincter8
After anorectal surgery; thought to be due to increased sphincter tone9
Cases which suggest interference with sensory or motor innervation to the bladder
Diabetic cystopathy10
Transverse myelitis attributed to Lyme disease11
2 days after herpes zoster lesions in the sacral dermatomes (S2-S4) resulting in reversible bladder dysfunction12
After intense anal intercourse13
Overdistension is probably the cause of one of the most common forms of acute urinary retention: that following surgery under general anaesthesia.1,14 In these circumstances the bladder, unless catheterised, fills to a high volume. In the postoperative period opiates or opioids, which are often given as part of a general anaesthetic, decrease the sensation of bladder fullness. Loss of sensation might be further complicated by anticholinergic drugs (reducing the capacity of the bladder to work) and the high α adrenergic tone after surgery (increasing urinary sphincter tone). When bladder and sphincter pressures are measured in men with acute urinary retention the findings are variable.15 Men who on urodynamic testing were unable to contract their bladder required catheters for longer than men whose bladder motor function was preserved. Retention was invariably associated with abnormally high urethral pressures and bladder volumes. Both returned to normal during catheterisation.
Experimental studies have shown both reversible and irreversible changes when acute urinary retention is induced in animals. Changes in non-adrenergic, non-cholinergic neurotransmitters have been noted in rats.16 Depletion of vasoactive polypeptide, neuropeptide Y, and substance P in the bladder wall of rats occurred within three hours of forced diuresis against an obstructed urethra. The depletion was transient, with values returning to normal after the distension was relieved. However, studies in guinea pigs have shown that if acute urinary retention is not relieved cell death in the ganglia within the bladder wall is evident within 24 hours and established by 48 hours.17
Who is at risk?
Almost all patients with acute urinary retention will be men aged over 60, and most will have some identifiable predisposing factor. Acute urinary retention occurring in anyone else should be carefully evaluated. Infants may have appendicitis,18 children may have a lymphoma,19 and young adults may have demyelination or spinal cord compression.20 All women require a pelvic examination, careful neurological assessment, and ultrasonography of the pelvis as minimum investigation.
Estimates of 10 year cumulative incidence range from 4% to 73%.21 Most are based on single practice series with very different populations, so these figures are little help in estimating the risk in specific groups of men. A recent community study from Minnesota provides a more precise estimate. Acute urinary retention in men less than 60 years old was rare. However, in the older age groups the risk increased with age. Men aged 70-79 years had a 1 in 10 chance of developing acute urinary retention in the subsequent five years. If they reported urinary symptoms, the risk was greater. Three other factors increased the risk of acute urinary retention: a large prostate (relative risk 2.0, 95% confidence interval 1.0 to 9.0); low peak urine flow rate (3.9, 2.3 to 6.6); and abnormally high concentration of serum prostate specific antigen. In the placebo arm of a large pharmaceutical study of men with enlarged prostates and lower urinary tract symptoms, prostate specific antigen was the strongest predictor of both acute urinary retention and the need for prostatic surgery.22
For men in the United Kingdom the Minnesota estimates are almost certainly conservative as men in the United States have prostatectomy earlier than those in the United Kingdom.23,24 Prostatectomy (and presumably other interventions) lowers the risk of acute urinary retention by about a factor of 10 (relative risk 0.1, 95% confidence interval 0.01 to 0.09) in men with moderate lower urinary tract symptoms compared with men who have no treatment.25,26
How is it treated?
Acute urinary retention is treated by catheterisation. This is usually done in accident and emergency departments and followed by hospital admission. In some places, catheterisation is done by general practitioners or community nurses and is followed by an outpatient referral to a urologist.2 The catheter is usually placed urethrally, although some favour the suprapubic approach, particularly if the catheter is going to be in place for some time.27
Once a man is catheterised a decision is made whether to undertake a trial without catheter. Again the proportion of men having a trial without catheter depends largely on local practice. Some urologists regard acute urinary retention and previous lower urinary tract symptoms as an absolute indication for prostatectomy.23 Others tend to allow most men a trial of voiding.
Predicting who will successfully void is not easy. Half of men who initially void successfully will experience recurrent acute urinary retention within a week, and 68% will experience a second episode within a year. Recurrence is 90% for men with an initial peak urinary flow rate less than 5 ml/s.28 Factors that make failure more likely include age greater than 75 years and drained volume of urine greater than 1 litre. Though a measurement is not readily available, the inability of the bladder to mount a strong detrusor contraction (>3.4 kPa) strongly predicts failure.29
Some subgroups will have lower failure rates. Community based studies1 have shown that if acute urinary retention occurred after general anaesthesia, most men subsequently void successfully.
Men who fail their trial without catheter and who are fit enough for an operation will usually elect to have a prostatectomy. In the United Kingdom just under half of men will be sent home with their catheter and drainage device to await their operation.3 Of these, half have their operation within a month, and most (88%) within three months. Though inconvenient, interval prostatectomy is associated with marginally better outcome. Men were more likely to void successfully after their prostatectomy if they had had a period of catheterisation, and they were also less likely to require a second procedure because of bleeding. Symptomatic outcome was unaffected by catheterisation.3 This observation is important because prostatectomy performed for acute urinary retention rather than for urinary symptoms alone is more risky. A large observational cohort study found that, compared with men having prostatectomy to relieve lower urinary tract symptoms, men who had prostatectomy after acute urinary retention were at increased risk of intraoperative complications (relative risk 1.8, 95% confidence interval 1.3 to 2.5), transfusion (2.5, 1.8 to 3.3), postoperative complications (1.6, 1.2 to 2.0), and hospital death (3.3, 1.2 to 9.3).3 Many though not all of these differences can be explained by noting that men having prostatectomy for acute urinary retention are older, less fit, and tend to have bigger prostates than men who have a prostatectomy for other reasons.
Men having their prostatectomy because of acute urinary retention have slightly worse outcome in terms of reduced symptoms and improvements in quality of life.3 The chances of successful prostatectomy also fall if there is evidence of bladder muscle failure: high volumes of retained urine (>1.5 l), inability to generate high bladder pressures (>2.7 kPa), or absence of unstable bladder contractions.29
Any advances likely?
Acute urinary retention can be prevented. Men randomised to finasteride, a drug which reduces the size of the prostate by inhibiting the formation of dihydrotestosterone from testosterone, had a 57% (95% confidence interval 40 to 69) lower risk of acute urinary retention over four years compared with men receiving placebo.30 Because acute urinary retention was a relatively infrequent event in this group, the reduction in absolute risk was 7% (placebo) to 3% (finasteride). Interestingly, men taking finasteride who had no obvious cause for their acute urinary retention were less likely to require prostatectomy than men receiving placebo (33% v 72%).
Because acute urinary retention is relatively infrequent and not life threatening, few would argue that we should embark on a widespread prevention programme. To prevent a single episode of acute urinary retention or prostatectomy 15 men with pre-existing urinary symptoms would have to be treated for four years. Selective use in men with known risk factors (moderate to severe urinary symptoms, large prostates, and poor urinary flow rates) is probably warranted. There may be a future role for secondary prevention. However, finasteride has not yet been shown to prevent recurrences in men who successfully void after a first episode of acute urinary retention.
Two strategies could help improve the chances of successful withdrawal of the catheter after acute urinary retention. The first relates to the amount of time the bladder needs to be drained for complete recovery. Djavan et al found that increasing the period of bladder drainage improved the chances of voiding when the catheter was removed.31 Successful voiding was achieved by 44% of men randomised to immediate removal, 51% randomised to removal after two days, and 62% randomised to removal after seven days. Longer drainage was particularly important for men who had retained high volumes of urine. They concluded that men with retention volumes greater than 1.3 l should be encouraged to have longer periods of drainage.
The second strategy is pharmacological. Blockade of the α adrenergic receptors in the bladder neck and prostate may relax bladder smooth muscle sufficiently to give higher rates of successful voiding. A preliminary report of a randomised trial of α blockers and placebo for acute urinary retention suggested that men receiving α blockers were almost twice as likely to void successfully after catheter removal than men who received placebo.32 These are early, short term results, and the investigators are still recruiting. We will have to wait to confirm that these differences lead to a better long term outcome.
In future, traditional catheterisation might not be needed. Instrument makers are racing to come up with a device that will relieve acute urinary retention and allow the bladder and external (voluntary) sphincter to work normally. These devices work by stenting open the bladder neck and prostate, reducing the pressure required to start off micturition (fig 2). At present, such devices are slightly more difficult to place than a standard urethral catheter, but this may change. If these devices could be placed by a general practitioner or someone in accident and emergency, it would allow men to be discharged soon afterwards, continent and able to empty their bladder without difficulty. We have not arrived at this point yet, and will require much careful evaluation before we do. These prostatic catheters need to be removed at some point otherwise they will cause stone formation. At present this is done by pulling on a string that lies in the urethra. Biodegradable catheters are being considered but are at an earlier stage of development. The time which they take to dissolve would give drugs a chance to work. Hospital admission would be avoided and the need for prostatectomy almost certainly reduced.
Figure 2.
Modern prostatic catheters can keep the bladder neck and prostate open and, at the same time, allowing external (voluntary) sphincter to function
Clearly the role of prostatectomy as the best treatment for refractory acute urinary retention is being challenged. Interstitial treatments which deliver heat down a needle have been used with moderate success in men presenting in acute urinary retention.33 But prostatectomy in this situation has not yet been superseded. Nevertheless the advances in prevention and treatment give men approaching their 60th birthday reason to feel reassured.
Figure.
Catheter treatment from an Italian medical picture book by Henricus Kullmaurer and Albert Meher, 1510
Footnotes
Funding: None
Competing interests: ME has been involved in the development of a CD Rom intended for men with lower urinary tract problems. This project was funded by The Royal College of Surgeons of England, Department of Health, and Merck Sharp and Dohme. He has also received lecture fees from makers of α blockers and been involved in discussions with industry regarding the evaluation of prostatic catheters.
References
- 1.Jacobsen SJ, Jacobsen DJ, Girman CJ, Roberts RO, Rhodes T, Guess HA, et al. Natural history of prostatism: risk factors for acute urinary retention. J Urol. 1997;158:481–487. doi: 10.1016/s0022-5347(01)64508-7. [DOI] [PubMed] [Google Scholar]
- 2.Grose K, Brooman PJC, O’Reilly PH. Urological community nursing: a new concept in the delivery of urological care. Br J Urol. 1995;76:440–442. doi: 10.1111/j.1464-410x.1995.tb07741.x. [DOI] [PubMed] [Google Scholar]
- 3.Pickard R, Emberton M, Neal DE. The management of men with acute urinary retention. Br J Urol. 1998;81:712–720. doi: 10.1046/j.1464-410x.1998.00632.x. [DOI] [PubMed] [Google Scholar]
- 4.Saborio DV, Kennedy WA, Hole GP. Acute urinary retention secondary to urethral inflammation from a vaginal contraceptive suppository in a 17 year old boy. Urol Int. 1997;58:128–130. doi: 10.1159/000282968. [DOI] [PubMed] [Google Scholar]
- 5.Benekli M, Buyukasik Y, Haznedaroglu IC, Savas MC, Ozcebe OI. Chronic lymphocytic leukemia presenting as acute urinary retention due to leukemic infiltration of the prostate. Ann Hematol. 1996;73:143–144. doi: 10.1007/s002770050216. [DOI] [PubMed] [Google Scholar]
- 6.Savarirayan S, Shenykin Y, Gerard P, Wise GJ. Staphylococcus peri-prostatic abscess—an unusual cause of acute urinary retention. Urology. 1995;46:573–574. doi: 10.1016/s0090-4295(99)80277-5. [DOI] [PubMed] [Google Scholar]
- 7.Shah B, Rodriguez R, Krasnokutsky S. Tumour in a giant bladder diverticulum: a case report and review of the literature. Int Urol Nephrol. 1997;29:173–179. doi: 10.1007/BF02551338. [DOI] [PubMed] [Google Scholar]
- 8.Brown JA, Levy JB, Kramer SA. Genitourinary neurofibromatosis mimicking posterior urethral valves. Urology. 1997;49:960–962. doi: 10.1016/s0090-4295(97)00077-0. [DOI] [PubMed] [Google Scholar]
- 9.Barone JG, Cummings KB. Aetiology of acute urinary retention following benign ano-rectal surgery. Ann Surg. 1994;60:210–211. [PubMed] [Google Scholar]
- 10.Olapade-Olaopa EO, Morley RN, Carter CJ, Walmsley BH. Diabetic cystopathy presenting as primary acute urinary retention in a previously undiagnosed young male diabetic patient. J Diabetes Complications. 1997;11:350–351. doi: 10.1016/s1056-8727(96)00107-9. [DOI] [PubMed] [Google Scholar]
- 11.Olivares JP, Pallas F, Cecaldi M, Viton JM, Raoult D, Planche D, et al. Lyme disease presenting as isolated acute urinary retention caused by transverse myelitis: an electrophysiological and urodynamic study. Arch Phys Med Rehabil. 1995;76:1171–1172. doi: 10.1016/s0003-9993(95)80128-6. [DOI] [PubMed] [Google Scholar]
- 12.Cohen LM, Fowler JF, Owen LG, Callen JP. Urinary retention associated with herpes zoster infection. Int J Dermatol. 1993;32:24–26. doi: 10.1111/j.1365-4362.1993.tb00955.x. [DOI] [PubMed] [Google Scholar]
- 13.Godec CJ, Cass AS, Ruiz E. Another aspect of acute retention in young people. Ann Emerg Med. 1982;11:471–474. doi: 10.1016/s0196-0644(82)80064-4. [DOI] [PubMed] [Google Scholar]
- 14.Waterhouse N, Beaumont AR, Murray K, Staniforth P, Stone MH. Urinary retention after total hip replacement. A prospective study. J Bone Joint Surg Br. 1987;69:64–66. doi: 10.1302/0301-620X.69B1.2434510. [DOI] [PubMed] [Google Scholar]
- 15.Murray K, Massey A, Feneley RC. Acute urinary retention—a urodynamic assessment. Br J Urol. 1984;56:468–473. [PubMed] [Google Scholar]
- 16.Lasanen LT, Tammela TL, Liesi P, Waris T, Polak JM. The effect of acute distension on vasoactive intestinal peptide, neuropeptide Y and substance P immunoreactive nerves in the female rat urinary bladder. Urol Res. 1992;20:259–263. doi: 10.1007/BF00300255. [DOI] [PubMed] [Google Scholar]
- 17.Zhou Y, Ling EA. Effects of acute complete outlet obstruction on the NADPH-diaphorase reactivity in the intramurla ganglia of the guinea pig urinary bladder: light and electron microscopic studies. J Urol. 1997;158:916–923. doi: 10.1097/00005392-199709000-00072. [DOI] [PubMed] [Google Scholar]
- 18.Dever DP, Hulbert WC, Emmens RW, Rabinowitz R. Appendiceal abscess masquerading as acute urinary retention in children. Urology. 1985;25:289–292. doi: 10.1016/0090-4295(85)90331-0. [DOI] [PubMed] [Google Scholar]
- 19.Li CK, Yeung CK, Chow J, Shing M, Chik KW, Liu K, et al. Prostatic non-Hodgkin’s lymphoma causing acute urinary retention in childhood. Med Paediatr Oncol. 1995;25:420–422. doi: 10.1002/mpo.2950250510. [DOI] [PubMed] [Google Scholar]
- 20.Tintinialli JE. Acute urinary retention as a presenting sign of spinal cord compression. Ann Emerg Med. 1986;15:1235–1237. doi: 10.1016/s0196-0644(86)80876-9. [DOI] [PubMed] [Google Scholar]
- 21.Meigs JB, Barry MJ. Natural history of benign prostatic hyperplasia. In: Kirby R, McConnell J, Fitzpatrick J, Roehrborn C, Boyle P, editors. Textbook of benign prostatic hyperplasia. Oxford: Isis Medical Media; 1996. pp. 125–135. [Google Scholar]
- 22.Lieber M, Fowler J, Castellanos R, Albertsen P, Coffield S, Hodge B, et al. PSA is the strongest predictor of BPH related outcomes: results of a 4-year placebo controlled trial. J Urol. 1998;159(suppl):107. [Google Scholar]
- 23.McConnell JD. Clinical practice guideline number 8. Rockville, MD: Agency for Health Care Policy and Research, US Department of Health and Human Services; 1994. Benign prostatic hyperplasia: diagnosis and treatment. (AHCPR publication 94-0582.) [PubMed] [Google Scholar]
- 24.Emberton M, Neal DE, Black N, Fordham M, Harrison M, McBrien MP, et al. The effect of prostatectomy on symptom reduction and quality of life. Br J Urol. 1995;77:233–247. doi: 10.1046/j.1464-410x.1996.88213.x. [DOI] [PubMed] [Google Scholar]
- 25.Wasson JH, Reda DJ, Bruskewitz RC, Elinson J, Keller AM, Henderson MG, et al. A comparison of transurethral surgery with watchful waiting for moderate symptoms of benign prostatic hyperplasia. N Engl J Med. 1995;332:75–79. doi: 10.1056/NEJM199501123320202. [DOI] [PubMed] [Google Scholar]
- 26.Flanigan RC, Reda DJ, Wasson JH, Anderson RJ, Abdellatif M, Bruskewitz RC, et al. 5-Year surgical outcome of surgical resection and watchful wait-ing for men with moderately symptomatic benign prostatic hyperplasia: a Department of Veterans Affairs cooperative study. J Urol. 1998;160:12–16. [PubMed] [Google Scholar]
- 27.Ichsan J, Hunt DR. Suprapubic catheters: a comparison of suprapubic versus urethral catheters in the treatment of acute urinary retention. Aust N Z J Surg. 1987;57:33–36. doi: 10.1111/j.1445-2197.1987.tb01236.x. [DOI] [PubMed] [Google Scholar]
- 28.Klarskov P, Andersen JT, Asmussen CF, Brenoe J, Jensen SK, Jensen IL, et al. Symptoms and signs predictive of the voiding patterns after acute urinary retention in men. Scand J Urol Nephrol. 1987;21:23–28. doi: 10.3109/00365598709180285. [DOI] [PubMed] [Google Scholar]
- 29.Djavan B, Madersbacher S, Klingler C, Marberger M. Urodynamic assessment of patients with acute urinary retention: is treatment failure after prostatectomy predictable. J Urol. 1997;158:1829–1833. doi: 10.1016/s0022-5347(01)64139-9. [DOI] [PubMed] [Google Scholar]
- 30.McConnell JD, Bruskewitz R, Walsh P, Andriole G, Lieber M, Holtgrewe HL, et al. The effect of finasteride on the risk of acute urinary retention and the need for surgical treatment among men with benign prostatic hyperplasia. N Engl J Med. 1998;338:557–563. doi: 10.1056/NEJM199802263380901. [DOI] [PubMed] [Google Scholar]
- 31.Djavan B, Shariat S, Omar M, Roehrborn CG, Marberger M. Does prolonged catheter drainage improve the chance of recovering voluntary voiding after acute retention of urine (AUR)? Eur Urol. 1998;33(suppl 1):110. [Google Scholar]
- 32.McNeill SA, Donat R, Pillai MK, Hargreave TB, Daruwalla P, Goodman CM, et al. Prospective multicentre randomised placebo double blind study of the effect of alfuzosin on the outcome of trial removal of catheter following acute urinary retention. J Urol. 1998;159(suppl):256. [Google Scholar]
- 33.Makar A, Thomas P, Fletcher M, Harrison N. Interstitial radiofrequency of the prostate in the management of acute urinary retention. Eur Urol. 1998;33(suppl):75. doi: 10.1046/j.1464-410x.1998.00624.x. [DOI] [PubMed] [Google Scholar]