Abstract
Background
Chronic low back pain (CLBP) is a common issue among the working-age population. Sleeping position may affect CLBP, with the prone position commonly suggested to be avoided. This study aims to examine the relationship between preferred and avoided sleeping positions and to explore the frequency of increased pain in various sleeping positions among patients with nonspecific CLBP and pain and disability levels.
Methods
This cross-sectional study included all adult patients referred for specialist consultation for CLBP at the outpatient clinic of the Central Hospital of Central Finland’s spine department. Pain intensity was measured using a visual analog scale (VAS), and disability was assessed with the Oswestry Disability Index (ODI). Patients completed a questionnaire detailing the main sleeping positions and positions avoided due to low back pain (LBP).
Results
The study enrolled 375 consecutive patients, with a mean age of 51 ± 17 years; 64% (n=240) were female. The mean VAS score was 63 ± 24, and the mean Oswestry Index was 38 ± 18%. The majority of patients (87%, n=327) reported sleeping in a side-lying position, followed by supine (47%, n=176) and prone (22%, n=82) positions. A negative correlation was found between age and the preference for sleeping in the prone position. No significant gender differences in sleep positions were observed (p=0.69). Sleep was disturbed in 77% of patients (n=289) due to LBP, and 87% (n=327) reported difficulties due to LBP when getting up. Overall, 92% of participants (n=345) experienced difficulties sleeping or getting up in the morning due to LBP. Many patients avoided certain positions due to pain: 42% (n=157) avoided the prone position, 35% (n=131) the back, 15% (n=56) the left side, and 13% (n=49) the right side. Although the prone position was most commonly linked with pain, especially among women, our findings suggest that any sleeping position could potentially exacerbate pain in individuals with CLBP.
Conclusions
This study highlights the variability in how sleeping positions affect pain in patients with nonspecific CLBP. While the prone position is most frequently associated with increased pain, individual preferences and responses vary significantly, and often sidelying and supine positions provoke pain. The diversity in sleeping positions that exacerbate pain highlights the need for tailored advice in the management of patients with CLBP.
Keywords: working-age population, epidemiologic studies, sleeping habits, oswestry index, disability, sleeping posture, sleeping ergonomics
Introduction
Chronic low back pain (CLBP) affects 10% to 23% of the working-age population, making it a prevalent health issue [1]. It leads to high treatment costs, increased sick leave, and significant individual suffering. More than half of those with CLBP report impaired sleep, often experiencing significantly worse sleep quality and efficiency than those without CLBP [2-5]. A one-point increase on a ten-point visual analog scale (VAS) correlates with a 10% higher likelihood of sleep disturbances [6]. Sleep’s duration and quality are crucial for physical and mental health [7]. In CLBP patients, poor sleep independently exacerbates medical costs and healthcare visits beyond the impacts of pain intensity and disability [8].
Significant associations exist between spinal pain and sleeping postures, including supine, prone, and partial side-lying positions [9]. Pain may arise from the lumbar spine’s tissues, such as the outer intervertebral discs, joint capsules, ligaments, fasciae, and muscles, due to prolonged low-load compression, shear, or torsion forces [10]. However, the relationship between sleeping positions and CLBP among patients seeking specialist care remains unexplored. This study aims to investigate the connection between nonspecific CLBP and pain related to certain sleeping positions. We examined how often different sleeping positions cause pain and their associations with low back pain (LBP), leg pain, and disability.
Materials and methods
We conducted a cross-sectional study at the outpatient clinic of the Central Hospital of Central Finland’s spine department. Adults with LBP, unresponsive to conservative treatment in primary or occupational healthcare, were referred for further evaluation at this tertiary-care spine clinic following the LBP guideline [11]. We considered all referred patients as potential study participants. The Central Hospital, serving a population of 270,000, hosts the region’s only tertiary-care spine clinic. The inclusion criteria were Finnish-speaking adults over the age of 18, with LBP persisting for over three months. We excluded patients with radicular pain or specific CLBP causes like ankylosing spondylitis, fibromyalgia, tumors, and vertebral fractures.
The Research Ethics Committee of the Central Finland Health Care District approved the study (Approval Number 1E/2017). The procedure of the study was performed according to the relevant guidelines and regulations of the Declaration of Helsinki [12].
Study instrument
Patients completed a pre-visit questionnaire at home, detailing their medical history and main sleeping positions, including positions avoided due to LBP and factors worsening it. The questionnaire also gathered basic demographic information and back pain triggers and relievers. We assessed back and leg pain over the previous week using a VAS (scale 0-100) [13] and disability using the Oswestry Disability Index (ODI) [14]. The ODI measures daily life functionality across 10 areas, with scores ranging from 0 (the least disability) to 100 (the most severe disability). We used the validated Finnish ODI version [15].
Statistical analysis
We presented descriptive statistics as means ± standard deviation, counts (n), and percentages. We compared groups using the t-test, analysis of variance, and Pearson’s chi-squared test. We assessed variable normality with graphical methods and the Shapiro-Wilk W test. Data were analyzed using Stata 16.1 (StataCorp LP, College Station, TX, USA).
Results
We included 375 consecutive adult patients with unspecific CLBP in the study. The average age of the patients was 51 ± 17 years, with females comprising 64% of the study population (n=240; Table 1). Eighty-five participants (23%) were smokers. The mean ODI score was 38% ± 18%, and the mean score on the VAS for pain was 63 ± 24. More than half of the patients reported referred leg pain, with mean VAS scores of 52 ± 66 for the right leg and 52 ± 33 for the left leg. Seventy-seven percent (n=289) of the patients experienced sleep disturbances due to LBP at night, and 87% (n=327) reported difficulties while getting up. A total of 92% (n=349) had challenges sleeping or rising in the morning because of LBP. We observed no significant differences between genders.
Table 1. Demographic and clinical data of patients (N=375) with chronic low back pain.
Abbreviations: LBP: low back pain; SD: standard deviation; VAS: visual analog scale; ODI: Oswestry Disability Index. *Mean leg pain during last week in those who had leg pain.
| Patient Information | Female (n=240) | Male (n=135) | |
| Demographic data | Age (years), mean ± SD | 52 ±17 | 50 ± 16 |
| Height (cm), mean ± SD | 163 ± 7 | 179 ± 7 | |
| Weight (kg), mean ± SD | 74 ± 19 | 91 ± 20 | |
| Body mass index (kg/m2), mean ± SD | 28 ± 7 | 29 ± 6 | |
| Clinical data | Smoking, n (%) | 50 (21%) | 35 (26%) |
| ODI, mean ± SD | 39 ± 17 | 38 ± 19 | |
| LBP (VAS), mean ± SD | 64 ± 23 | 60 ± 25 | |
| LBP at night, n (%) | 194 (81%) | 95 (70%) | |
| LBP in the morning, n (%) | 212 (88%) | 115 (85%) | |
| LBP night or morning, n (%) | 225 (92%) | 124 (92%) | |
| Leg pain right, n (%) | 146 (61%) | 76 (56%) | |
| Leg pain right (VAS), mean ± SD* | 60 ± 25 | 56 ± 26 | |
| Leg pain left, n (%) | 140 (59%) | 67 (50%) | |
| Leg pain left (VAS), mean ± SD* | 58 ± 28 | 57 ± 26 | |
| Sleeping position | Side, n (%) | 209 (87%) | 118 (87%) |
| Supine, n (%) | 115 (48%) | 61 (45%) | |
| Prone, n (%) | 53 (22%) | 29 (21%) | |
Side-lying was the predominant sleep position, with 87% (n=327) of both men and women preferring it (p<0.001). Approximately 47% of participants slept on their backs (n=176), and only 22% (n=82) preferred the prone position, again with no significant gender difference (p=0.69). Forty-three percent of the patients (n=161) reported changing their sleep position throughout the night. Individuals who slept in a prone position were, on average, 10 years younger than those who preferred other positions (Table 2), indicating a significant association between age and sleep position (p<0.001). Eight percent of patients (n=30) had a body mass index (BMI) between 35 and 40 kg/m2, and 5% (n=198) had a BMI over 40 kg/m2, with no significant correlation between BMI and sleep position (p=0.70). Patients who slept in a side-lying position had significantly higher mean ODI scores than those in other positions (p<0.001). However, we found no significant association between sleep position and LBP during the night (p=0.84).
Table 2. Demographic and clinical data of chronic low back pain patients (N=375) according to sleeping position.
LBP: low back pain; SD: standard deviation; VAS: visual analog scale.
| Patient data | Sleeping position | P-value | |||
| Side (n=213) | Supine (n=114) | Prone (n=48) | |||
| Demographic data | Female, n (%) | 130 (61%) | 83 (73%) | 27 (56%) | 0.69 |
| Male, n (%) | 83 (39%) | 31 (27%) | 21 (44%) | ||
| Age in years, mean ± SD | 54 ± 17 | 50 ± 16 | 42 ± 15 | <0.001 | |
| BMI (kg/m2), mean ± SD | 28.4 ± 5.9 | 27.2 ± 6.0 | 28.8 ± 9.0 | 0.70 | |
| Clinical data | LBP (VAS), mean ± SD | 63 ± 24 | 62 ± 24 | 60 ± 24 | 0.36 |
| Leg pain (VAS), mean ± SD | 61 ± 28 | 52 ± 28 | 50 ± 30 | 0.007 | |
| Oswestry, mean ± SD | 41 ± 17 | 36 ± 17 | 33 ± 18 | <0.001 | |
| Aggravates LBP | Standing, n (%) | 151 (71%) | 74 (65%) | 24 (50%) | 0.007 |
| Walking, n (%) | 124 (58%) | 61 (54%) | 22 (46%) | 0.11 | |
| Sitting, n (%) | 142 (67%) | 72 (63%) | 36 (75%) | 0.54 | |
| Working, n (%) | 114 (54%) | 67 (59%) | 30 (63%) | 0.19 | |
| Leisure, n (%) | 49 (23%) | 24 (21%) | 12 (25%) | 0.94 | |
| Lying, n (%) | 49 (23%) | 17 (15%) | 12 (25%) | 0.63 | |
| LBP occurs | Sleeping, n (%) | 164 (77%) | 87 (76%) | 38 (79%) | 0.84 |
| Getting up, n (%) | 187 (88%) | 99 (87%) | 41 (85%) | 0.64 | |
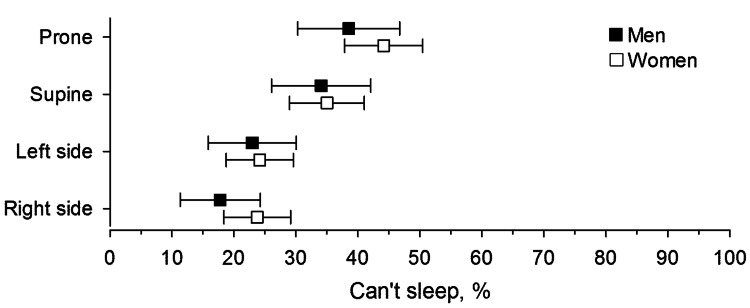
Seventy-six percent of the patients (n=285) reported avoiding one or more sleeping positions that worsened their LBP to the extent that they could not sleep in those positions (Figure 1). Both women and men were more likely to avoid sleeping in the prone and supine positions compared to the side-lying position (p<0.001). Forty-four percent of women (n=106), compared to 39% of men (n=53), were unable to sleep in the prone position, a difference that was statistically significant (p=0.04).
Figure 1. Sleeping position where patients with chronic low back pain were unable to sleep.
Error bars indicate 95% confidence interval.
The supine position was avoided due to LBP by 34% of men (n=46) and 35% of women (n=84). Sixteen percent of women (n=38) and 13% of men (n=18) avoided lying on their left side due to LBP, while 16% of women (n=38) and 8% of men (n=11) avoided the right side. Only 8% of women (n=19) and 10% (n=14) of men reported avoiding both side-lying positions due to LBP. Fifty-six percent of the patients (n=210) reported that LBP was exacerbated at work, with no significant gender difference. Lying down relieved back pain for 59% of both men (n=80) and women (n=142).
Discussion
Over 90% of the CLBP patients reported experiencing significant discomfort in bed at night and/or while getting up. Three-quarters identified certain sleeping positions as exacerbating their LBP. Prior research suggests that the prone position offers the least support for the lower back and is not recommended for individuals with CLBP [16]. Our findings support this perspective, highlighting the prone position as the most avoided posture for sleeping. Although body weight is more evenly distributed in the supine and prone positions, these positions may increase lumbar lordosis, subsequently loading the lumbar facet joints [17]. Moreover, the prone position is associated with significant issues such as buckling of the ligamentum flavum, increased spondylolisthesis, and facet joint subluxation leading to foraminal stenosis, as observed in magnetic resonance imaging in patients with low back pain with or without radiculopathy [18].
The side-lying posture is the most commonly adopted sleeping position, with over 60% of European adults preferring it for most of the night [19,20]. Similarly, our study found side-lying to be the preferred sleeping posture, possibly because other positions often aggravate LBP. However, the side-lying position was linked to a higher Oswestry Disability Index and more referred leg pain. This posture exerts considerable pressure on the hip area, potentially irritating the lower back [21].
Sleeping position showed no correlation with BMI or LBP, and gender did not significantly influence sleeping posture choice. However, we observed that older age groups were less likely to sleep in the prone position, aligning with previous research findings. LBP’s multifactorial nature includes potential contributions from environmental factors, hereditary factors, psychosocial aspects, degenerative disorders, or trauma, varying by individual [22]. Moreover, alcohol, drugs, smoking, and medicine abuse may influence both sleep and pain experiences. Sleep posture, as a factor, warrants further consideration. Notably, not all patients experienced pain while lying down; discomfort arose more commonly when getting out of bed, possibly due to deeper sleep, a higher pain tolerance, less severe pain, or biomechanical factors related to movement during sleep. Cary et al. [20] discovered that patients with LBP spent significantly more time in postures that provoked their symptoms compared to asymptomatic controls. Although the sample sizes were small, the significance of advising on sleeping position in preventing and treating LBP is supported by randomized controlled studies [23,24]. In those studies, a significant majority of participants reported that certain sleeping positions adversely affected their LBP, necessitating the avoidance of these sleeping positions. Interestingly, this contrasts with this study’s findings, which state that over half of the patients felt relief from CLBP when lying down. This suggests that a lower axial load on the spine while lying down and finding a comfortable position can alleviate CLBP. However, sleep positions may change uncontrollably multiple times throughout the night, and thus, pain-provoking sleeping positions may exist [20].
The strength of this study lies in its large sample size, which represents patients with moderate to severe CLBP seeking specialist consultation. Employing the VAS and ODI to assess pain intensity and disability provides data about the severity of symptoms in the patient population. The results offer a broad perspective on CLBP and sleeping positions among a clinic-attending population seeking help for their symptoms. The study highlights both variations in sleeping positions and their avoidance due to pain, offering a nuanced understanding of how CLBP affects this part of daily living.
The study had some limitations. The study relied on patient-reported sleep positions, capturing only the positions at sleep onset and upon awakenings, thus not fully accounting for changes throughout the night. Adults change their sleeping position up to four times per hour in their twenties, decreasing to twice per hour after age 65 [25]. Including objective measurements to track sleeping position changes throughout the night would have added valuable insights. The cross-sectional design of this study limits our ability to establish causality between sleeping positions and CLBP severity.
Conclusions
This study explored the preferred sleeping position and the frequency of increased pain in various sleeping positions among patients with nonspecific CLBP. It examined the relationship between sleeping positions, pain, and disability levels. The side-lying posture was the most preferred sleeping position. Our findings indicate that specific sleeping positions aggravate LBP in a majority of CLBP patients. While prone and supine positions are most likely to provoke LBP, side-lying positions also cause discomfort for many. The variation in pain-inducing sleeping positions among individuals underscores the importance of personalized guidance in managing CLBP.
The authors have declared that no competing interests exist.
Author Contributions
Concept and design: Jari Ylinen
Acquisition, analysis, or interpretation of data: Jari Ylinen, Arja Häkkinen, Hannu Kautiainen, Juhani Multanen
Drafting of the manuscript: Jari Ylinen
Critical review of the manuscript for important intellectual content: Jari Ylinen, Arja Häkkinen, Hannu Kautiainen, Juhani Multanen
Human Ethics
Consent was obtained or waived by all participants in this study. Research Ethics Committee of the Central Finland Health Care District issued approval 1E/2017. The committee's position was that approval was not needed, because this was an interview study without treatment intervention
Animal Ethics
Animal subjects: All authors have confirmed that this study did not involve animal subjects or tissue.
References
- 1.The Global Spine Care Initiative: a summary of the global burden of low back and neck pain studies. Hurwitz EL, Randhawa K, Yu H, Côté P, Haldeman S. Eur Spine J. 2018;27:796–801. doi: 10.1007/s00586-017-5432-9. [DOI] [PubMed] [Google Scholar]
- 2.Associates of insomnia in people with chronic spinal pain: a systematic review and meta-analysis. Bilterys T, Siffain C, De Maeyer I, et al. J Clin Med. 2021;10:3175. doi: 10.3390/jcm10143175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Investigation of sleep disturbance in chronic low back pain: an age- and gender-matched case-control study over a 7-night period. van de Water AT, Eadie J, Hurley DA. Man Ther. 2011;16:550–556. doi: 10.1016/j.math.2011.05.004. [DOI] [PubMed] [Google Scholar]
- 4.The association between sleep and chronic spinal pain: a systematic review from the last decade. Van Looveren E, Bilterys T, Munneke W, et al. J Clin Med. 2021;10:3836. doi: 10.3390/jcm10173836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Objective and subjective assessment of sleep in chronic low back pain patients compared with healthy age and gender matched controls: a pilot study. O'Donoghue GM, Fox N, Heneghan C, Hurley DA. BMC Musculoskelet Disord. 2009;10:122. doi: 10.1186/1471-2474-10-122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rethinking the sleep-health link. Matricciani L, Bin YS, Lallukka T, et al. Sleep Health. 2018;4:339–348. doi: 10.1016/j.sleh.2018.05.004. [DOI] [PubMed] [Google Scholar]
- 7.Quality of sleep in patients with chronic low back pain: a case-control study. Marty M, Rozenberg S, Duplan B, Thomas P, Duquesnoy B, Allaert F. Eur Spine J. 2008;17:839–844. doi: 10.1007/s00586-008-0660-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Does disordered sleep moderate the relationship between pain, disability and downstream health care utilization in patients with low back pain? A longitudinal cohort from the US Military Health System. Rhon DI, O'Hagan E, Mysliwiec V, Lentz TA. Spine (Phila Pa 1976) 2019;44:1481–1491. doi: 10.1097/BRS.0000000000003114. [DOI] [PubMed] [Google Scholar]
- 9.Identifying relationships between sleep posture and non-specific spinal symptoms in adults: a scoping review. Cary D, Briffa K, McKenna L. BMJ Open. 2019;9:0. doi: 10.1136/bmjopen-2018-027633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Comprehensive anatomical and immunohistochemical review of the innervation of the human spine and joints with application to an improved understanding of back pain. Youssef P, Loukas M, Chapman JR, Oskouian RJ, Tubbs RS. Childs Nerv Syst. 2016;32:243–251. doi: 10.1007/s00381-015-2880-6. [DOI] [PubMed] [Google Scholar]
- 11.Chapter 4. European guidelines for the management of chronic nonspecific low back pain. Airaksinen O, Brox JI, Cedraschi C, et al. Eur Spine J. 2006;15 Suppl 2:0–300. doi: 10.1007/s00586-006-1072-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.World Medical Association. 59th WMA General Assembly. Seoul: 59th WMA General Assembly; [ Apr; 2024 ]. 2008. Declaration of Helsinki: ethical principle for medical research involving human subjects. [Google Scholar]
- 13.Vertical or horizontal visual analogue scales. Scott J, Huskisson EC. Ann Rheum Dis. 1979;38:560. doi: 10.1136/ard.38.6.560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Roland-Morris disability questionnaire, Oswestry Disability Index, and Quebec back pain disability scale: which has superior measurement properties in older adults with low back pain? Jenks A, Hoekstra T, van Tulder M, Ostelo RW, Rubinstein SM, Chiarotto A. J Orthop Sports Phys Ther. 2022;52:457–469. doi: 10.2519/jospt.2022.10802. [DOI] [PubMed] [Google Scholar]
- 15.Reliability and validity study of the Finnish version 2.0 of the oswestry disability index. Pekkanen L, Kautiainen H, Ylinen J, Salo P, Häkkinen A. Spine (Phila Pa 1976) 2011;36:332–338. doi: 10.1097/BRS.0b013e3181cdd702. [DOI] [PubMed] [Google Scholar]
- 16.Self-reported versus recorded sleep position: an observational study. Gordon SJ, Grimmer KA, Trott P. Int J Allied Health Sci Pract. 2004;2:1. [Google Scholar]
- 17.The effect of patient position on psoas morphology and in lumbar lordosis. Amaral R, Daher MT, Pratali R, et al. World Neurosurg. 2021;153:0–40. doi: 10.1016/j.wneu.2021.06.067. [DOI] [PubMed] [Google Scholar]
- 18.Prone position MRI of the lumbar spine in patients with low back pain and/or radiculopathy refractory to treatment. Avellanal M, Ferreiro A, Riquelme I, Boezaart AP, Prats-Galino A, Reina MA. https://pubmed.ncbi.nlm.nih.gov/35901482/ Pain Physician. 2022;25:409–418. [PubMed] [Google Scholar]
- 19.Better backs by better beds? Bergholdt K, Fabricius RN, Bendix T. Spine (Phila Pa 1976) 2008;33:703–708. doi: 10.1097/BRS.0b013e3181695d3b. [DOI] [PubMed] [Google Scholar]
- 20.Examining relationships between sleep posture, waking spinal symptoms and quality of sleep: a cross sectional study. Cary D, Jacques A, Briffa K. PLoS One. 2021;16:0. doi: 10.1371/journal.pone.0260582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.The association between chronic low back pain and sleep: a systematic review. Kelly GA, Blake C, Power CK, O'keeffe D, Fullen BM. Clin J Pain. 2011;27:169–181. doi: 10.1097/AJP.0b013e3181f3bdd5. [DOI] [PubMed] [Google Scholar]
- 22.Lancet Low Back Pain Series Working Group. What low back pain is and why we need to pay attention? Hartvigsen J, Hancock MJ, Kongsted A, et al. Lancet. 2018;391:2356–2367. doi: 10.1016/S0140-6736(18)30480-X. [DOI] [PubMed] [Google Scholar]
- 23.Effects of sleeping position on back pain in physically active seniors: a controlled pilot study. Desouzart G, Matos R, Melo F, Filgueiras E. Work. 2015;53:235–240. doi: 10.3233/WOR-152243. [DOI] [PubMed] [Google Scholar]
- 24.Effectiveness of a back care pillow as an adjuvant physical therapy for chronic non-specific low back pain treatment: a randomized controlled trial. Prommanon B, Puntumetakul R, Puengsuwan P, Chatchawan U, Kamolrat T, Rittitod T, Yamauchi J. J Phys Ther Sci. 2015;27:2035–2038. doi: 10.1589/jpts.27.2035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sleep positions and position shifts in five age groups: an ontogenetic picture. De Koninck J, Lorrain D, Gagnon P. Sleep. 1992;15:143–149. doi: 10.1093/sleep/15.2.143. [DOI] [PubMed] [Google Scholar]