Abstract
Inhalers are a key aspect of managing airways disease. With effective use, they can reduce symptoms, reduce the frequency of exacerbations and thus reduce usage of healthcare services. Inhalers are associated with a significant carbon footprint, accounting for 3% of NHS' carbon emissions. We aimed to audit inhaler technique, patient preferences and inhaler prescribing and disposal to identify areas for improving the sustainability of respiratory care. An audit tool was created, and patient interviews conducted across eight different sites. Our data demonstrate that inhaler users, while self-reporting high levels of confidence in their inhaler technique, frequently make errors in inhaler technique. Additionally, the majority of patients considered the carbon footprint of their inhalers important and would consider changing to a lower carbon alternative. The majority of patients surveyed were not disposing of their inhalers correctly. This short audit has identified key areas for improvement in the quality and sustainability of respiratory care.
Questions.
-
-
To what extent does UK respiratory care meet best practice guidelines (specifically those relating to patient education, use and disposal)?
-
-
What issues relating to the patient education, use and disposal of inhalers are a priority to address? What barriers are there to improvements?
-
-
Can improvements add sustainable value to our healthcare systems as assessed by the triple bottom line?
Alt-text: Unlabelled box
Introduction
As health services strive to reduce their environmental impacts and the consequent negative health impacts of their activities, respiratory care represents a key domain where improvements can be made.1,2 Inhalers are the mainstay of the management of airway disease, both for symptom control and reduction of risk of exacerbation.3, 4 Inhalers have impacts across multiple environmental domains, with significant associated harms to human health locally and globally.5 Among other impacts, inhaler production depletes limited natural resources and contributes to climate change and air pollution, their use involves release of greenhouse gas emissions, and their disposal contributes to land, air and water pollution.6 While some of these environmental impacts have not been quantified, their contribution to climate change has been estimated. Inhalers account for around 3% of the English National Health Service (NHS)’s total greenhouse gas emissions.7 Appropriate inhaler prescribing, use and disposal are important both to maximise the efficacy of inhalers and the quality of respiratory care, and to improve the sustainability of respiratory care. It is important to note that the reduction of respiratory exacerbations that result in hospitalisations, improves patients’ experiences and reduces environmental harms from healthcare delivery.8
British Thoracic Society (BTS) guidance recommends switching to lower carbon inhalers where appropriate.9 It is important to identify patients who would benefit from lower carbon alternatives to their current inhaler. Inhalers selection requires appropriate choice of the active medication delivered, dose of medication and mechanism of delivery of medication into the airways. Commonly available devices are metered dose inhalers (MDIs), dry powder inhalers (DPIs) and soft mist inhalers (SMIs).3 MDIs use a propellant gas to deliver medication into the airways, DPIs rely on turbulent flow generated by the user and SMIs aerosolise the medication to be inhaled. All inhalers have environmental impacts.6 All inhalers, including propellant-free inhalers (DPIs and SMIs), have proven effects on fossil fuel depletion, terrestrial acidification and freshwater and marine eutrophication.6 MDIs have the biggest impact in terms of direct greenhouse gas emissions due to the high global warming potential (GWP) of the propellant used, which can be up to 3,350 times greater than CO2.5 As the NHS strives to reach Net Zero, inhalers represent a key domain where improvements can be made.1 Delivering good quality respiratory care itself contributes to a sustainable healthcare system, as better disease control results in reduced healthcare usage, thus reducing healthcare environmental impacts.8 Where good disease control is achieved by using lower carbon alternative inhalers, this entails even larger carbon savings.10
This project aimed to audit inhaler technique, patient preferences and practice / prescribing at secondary care sites to identify areas of improvement. To facilitate this, we developed and tested the usability of an inhaler audit tool.
Methods
Audit design
Auditable principles were identified based on NICE and BTS guidance.11,12 A series of questions were drafted to assess whether these standards had been met for a given patient (proforma in appendix). The proforma included one question about the patient's respiratory condition, but no further demographic data were collected. The audit proforma was piloted twice with six and then 20 inpatients. Each time feedback from healthcare professionals and patients was used to improve the proforma.
Recruitment
Participating sites in the UK were recruited via written invitation to healthcare professionals, this included information on benefits in terms of improving quality of care, learning opportunities for participating clinicians and requirements in terms of time and team members. This was disseminated via respiratory and sustainability networks including UK Respiratory SpR Network and Centre for Sustainable Healthcare Respiratory Network. A webinar was hosted to outline the project plan and timing, and to discuss queries with case study sites. A second webinar was held with all participating sites to enable all participating teams to input into the proforma design.
Participants
Patients were considered eligible for the study if they were i) an inpatient on an adult ward and ii) using inhaled therapies. Participating teams included patients on respiratory or acute medical wards. Patients deemed to be lacking mental capacity were not interviewed.
Audit dissemination and sites
Each site gained Caldicott approval. Teams were made up of a respiratory consultant, specialist nurse or registrar and a junior doctor or nurse. A senior supervisory team member (respiratory consultant) was mandatory. Participating sites included a mix of district general hospitals and teaching hospitals in both rural and urban settings. Participating sites were:
Addenbrookes Hospital (Cambridge University Hospitals NHS Foundation Trust), Oxford University Hospitals, Princess Royal Telford (Shrewsbury and Telford), Whipps Cross Hospital (Barts Health NHS Foundation Trust), Dumfries and Galloway Royal Infirmary (NHS Dumfries and Galloway), Kings College London Hospital (Kings College London NHS Foundation Trust), Chesterfield Royal Hospital (Chesterfield Royal Hospital NHS Foundation Trust) and Bristol Royal Infirmary (University Hospitals Bristol NHS Foundation Trust).
Data collection and analysis
The audit data were collected at each site by participating teams and then emailed securely via NHS email to be collated. Inhaler technique was scored against six steps for DPIs and five for MDIs, from these an inhaler technique score (corresponding to the rate of correct steps) was generated. Surveys were collated and analysed in Excel. Descriptive statistics were calculated. One site did not use the most recent version of the spreadsheet (taking into account edits during the webinar review), therefore they did not provide data for a number of the questions and for these questions data from only seven sites were included.
Results
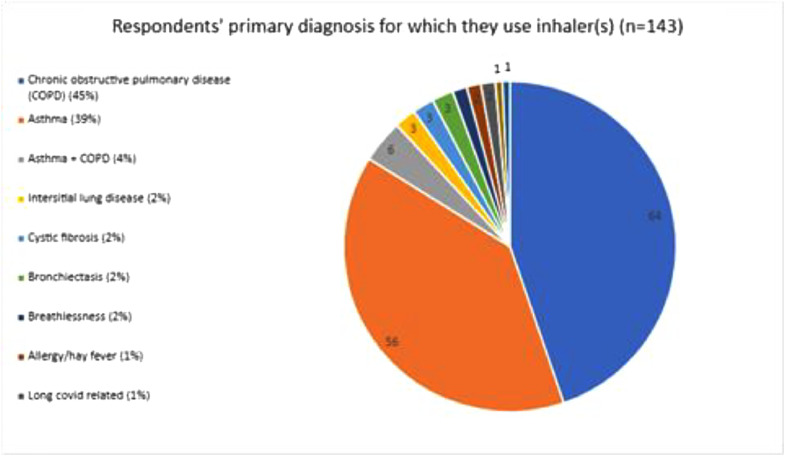
Description of respondents (Pie chart 1)
Pie Chart 1.
Respondents’ primary diagnosis for which they use inhaler(s) (n = 143). Chronic obstructive pulmonary disease (COPD) (45%). Asthma + COPD (4%). Interstitial lung disease (2%). Cystic fibrosis (2%). Bronchiectasis (2%). Allergy/ hay fever (2%). Long covid related (1%).
There were 143 respondents from eight centres, asthma (39%), COPD (45%), mixed (4%) and a remaining 12% with other diagnoses. Patients who used both DPIs and MDIs answered for each type of device they used, fewer respondents answered relating to DPIs (n = 68) compared with MDIs (n = 126).
Inhaler technique (Table 1, Table 2, Table 3)
Table 1.
Responses to the question ‘How confident are you with your inhaler technique for this inhaler?’ for dry powder and metered dose inhalers.
| Answer | Number of respondents for dry powder inhalers (DPI) (n = 68) | Number of respondents for metered dose inhaler (MDI) (n = 126) |
|---|---|---|
| Very confident | 36 (58%) | 72 (57%) |
| Confident | 28 (41%) | 38 (30%) |
| Somewhat confident | 2 (3%) | 10 (8%) |
| Not at all confident | 1 (1%) | 5 (4%) |
| Other | 1 (1%) | 1 (1%) |
Table 2.
Responses to the question ‘Has a healthcare professional demonstrated good inhaler technique for this inhaler to you before? If so, was that in the last one month, the last one year, or longer ago?’ for dry powder and metered dose inhalers.
| Answer | Number of responses for dry powder inhaler (DPI) (n = 68) | Number of responses for metered dose inhaler (MDI) (n = 126) |
|---|---|---|
| Yes <1 month ago | 11 (16%) | 20 (16%) |
| Yes 1m-12 m ago | 13 (19%) | 24 (19%) |
| Yes >1 year ago | 31 (46%) | 66 (52%) |
| No never | 12 (18%) | 15 (12%) |
| Unsure | 1 (1%) | 1 (1%) |
Table 3.
Inhaler technique scores attained by respondents when assessed by survey providing clinician, for dry powder and metered dose inhalers.
| Inhaler technique score (/6) | Number of respondents attaining score for dry powder inhalers (DPI) (n = 68) | Inhaler technique score (/5) | Number of respondents attaining score for metered dose inhaler (MDI) (n = 123) |
|---|---|---|---|
| 1 | 2 (3%) | 1 | 5 (4%) |
| 2 | 2 (3%) | 2 | 14 (11%) |
| 3 | 6 (9%) | 3 | 27 (22%) |
| 4 | 14 (21%) | 4 | 37 (30%) |
| 5 | 21 (31%) | 5 | 40 (33%) |
| 6 | 23 (34%) |
Score were assessed as per the instructions on the audit proforma (appendix). Patients received a point for each correctly attained step in inhaler usage to generate a score /6 for DPI and /5 for MDI.
Summary of steps:
DPI
1. Prepare the inhaler (as per inhaler, eg shake inhaler, remove mouth piece).
2. Empty lungs.
3. Positioning (sat up straight, chin inclined up).
4. Mouth seal.
5. Fast, deep inhalation.
6. Hold breath for 30 s.
MDI
1. Prepare inhaler e.g. remove mouthpiece, attach spacer.
2. Empty lungs.
3. Positioning (sat up straight, chin inclined up).
4. Mouth seal.
Appropriate inhalation – slow and gentle if no spacer or five tidal breaths if using spacer, plus appropriate spacing between doses if multiple doses.
For DPI use, only 34% demonstrated perfect technique (6/6 steps performed correctly). For MDI use, only 33% demonstrated perfect technique (5/5 steps performed correctly). For MDI users prescribed two puffs at the same time (35% of users), 93% demonstrated incorrect technique taking this dose regimen. 100% demonstrated perfect technique when prescribed two puffs separated by 30 s in-between doses (this includes re-mixing the drug and propellant by shaking). We are unable to report on inspiratory effort used due to insufficient data received. Patients had high levels of reported confidence in their own technique. 94% of DPI users were confident or very confident, compared with 87% of MDI users.
In both DPI and MDI users, 66% could not recall having inhaler technique demonstrated by a healthcare professional in the last 12 months.
Inhaler prescribing and disposal (Tables 4,5)
Table 4.
Responses to the question ‘Do you know when this inhaler needs replacing?’ for dry powder and metered dose inhalers. This refers to the patient's opinion.
| Answer | Number of responses for dry powder inhaler (DPI) (n = 68) | Number of responses for metered dose inhaler (MDI) (n = 125) |
|---|---|---|
| Yes | 59 (87%) | 75 (60%) |
| No | 9 (13%) | 50 (40%) |
Table 5.
Responses to the question ‘How do you most frequently dispose of your inhalers?’ for all respondents.
| Answer | Number responses (n = 122) |
|---|---|
| Return to pharmacy | 16 (13%) |
| Household waste bin | 71 (58%) |
| Recycling bin | 27 (22%) |
| Recycling bin + return to pharmacy | 1 (1%) |
| Other | 7 (6%) |
When asked whether they knew when to replace the inhaler, 87% of DPI users responded ‘Yes’, whereas 60% of MDI users responded ‘Yes’. The majority of DPI and MDI users requested their inhalers when required (54% and 65% respectively) rather than receiving them automatically (37% and 33% respectively).
When asked how patients most frequently dispose of their inhalers, the majority responded ‘Household waste bin’ (58%), with only 13% returning inhalers to the pharmacy. Most patients were unaware that inhalers could not be recycled in the local council recycling bin (78%).
Patient preferences (Table 6)
Table 6.
Responses to the question ‘How important to you is:’ for each of the following factors, for all respondents.
| Answer | ‘Being able to use your inhaler correctly and easily’ (n=143) | ‘Being able to tell how many doses are left in your inhaler’ (n=142) | ‘Having to clean your spacer frequently’ (n=122) | ‘Being able to carry your inhaler (and your spacer, if applicable) around with you easily‘ (n=122) | ‘That your inhaler has a low carbon footprint’ (n=122) |
|---|---|---|---|---|---|
| Very important | 111 (78%) | 77 (54%) | 24 (37%*) | 63 (53%*) | 45 (37%) |
| Important | 26 (18%) | 41 (29%) | 14 (22%*) | 38 (32%*) | 34 (28%) |
| Somewhat important | 5 (%) | 14 (10%) | 9 (14%*) | 8 (7%*) | 15 (12%) |
| Not important | 1 (1%) | 11 (8%) | 18 (28%*) | 11 (9%*) | 28 (23%) |
| Other | 0 (0%) | 0 (0%) | NA | NA | NA |
| Not applicable | NA | NA | 57 (47%) | 2 (2%) | 0 (0%) |
Values indicate number of responses for each question.
NA = not applicable.
%s calculated for respondent group who answered that the question was applicable to them.
96% of patients answered that being able to use the inhaler correctly and easily was either ‘Important’ or ‘Very Important’ to them. 83% of patients answered that being able to tell how many doses remain in the inhaler was either ‘Important’ or ‘Very Important’ to them. 85% of patients answered that portability of the inhaler was either ‘Important’ or ‘Very Important’ to them. 65% of patients answered that inhalers having a low carbon footprint was either ‘Important’ or ‘Very Important’ to them.
When asked whether patients would consider switching to a different inhaler, 92% said they would do so for improved ease of use, 68% for increased portability, 69% for a lower carbon footprint, 51% for no requirement for a spacer and 28% said they would not change their current inhaler.
Discussion
Our study has demonstrated high-levels of poor inhaler technique but willingness of patients to consider changes for effectiveness, ease of use or environmental reasons and opportunities to improve inhaler use in the UK.
Inhaler technique
The percentage of patients making at least one error in inhaler technique in our study was 66% for DPIs and 67% for MDIs. Similar levels of inhaler errors have been demonstrated in other studies.2,13 Exact comparison of levels of poor technique is difficult as studies use different definitions of error, however reported rates are up to 90%.14 Poor technique has been linked to worse disease control and increase use of healthcare services (eg for exacerbations of asthma or COPD).14 Increased use of services, and of inhalers themselves, increases the carbon footprint of respiratory care.
Despite this high rate of error, patients’ confidence in their own inhaler technique is generally high. This overestimation of inhaler technique has been reported on widely.13, 15, 16, 17 This is significant as time pressures have been stated by clinicians as a barrier to assessing inhaler technique and asking patients confidence may be used as a proxy for a full assessment.16,18 Our study adds to the evidence that confidence is unlikely to be an appropriate surrogate marker for patient demonstration of technique at inhaler reviews.
Our study revealed that a minority (34%) of patients reported receiving a demonstration of inhaler technique in the past year. Concerningly, 18% and 12% for DPI and MDI users respectively, reported never receiving a demonstration. NICE (National Institute for Health and Care Excellence) guidelines emphasise ‘regular’ assessment of inhaler technique to ensure patients can use their inhalers.11 There is evidence that regular assessments and corrections of inhaler techniques improve disease control.19,20
The low levels of correct technique that we have seen in this study suggest that there is unmet need to educate patients about correct inhaler technique. We have identified poor technique as an area that can improve both the effectiveness and sustainability of respiratory care. We therefore recommend a focus on inhaler technique during inhaler reviews, and ensuring patients are using current inhalers correctly, prior to escalating care in other (more resource and carbon intensive) ways.
Patient preferences
We found that the majority (65%) of patients surveyed think that the carbon footprint of their inhaler is important, a larger majority (69%) would consider switching to a lower carbon alternative if one was available. Other important factors for patients when making decisions regarding switching inhalers were ease of use, transportability and dose counters. Similar studies have showed similar levels of willingness to switch to lower carbon alternatives (60% of MDI users).21, 22, 23 D'Ancona et al found that a large proportion (65% of patients/carers surveyed) were unaware of the environmental impact of inhalers.23 These findings together highlight the importance of including information about the environmental impact of inhalers when discussing treatment options with patients as outlined in NICE's patient decision making aid.24 Despite this preference for lower carbon inhalers, previous studies have shown there is a larger proportion of MDI prescriptions in the UK, compared with other European countries.25 Additionally, there is large variation between local CCG guidance, with 26% offering no first line DPI for at least one stage of asthma management.26 This indicates that our practice and guidance do not accurately account for patient preference.
Inhaler disposal
Despite there currently being no nationwide inhaler recycling scheme, it remains important to return inhalers to the pharmacy to ensure they can be disposed of through clinical incineration, minimising landfill and the release of unused propellant gas into the atmosphere.27,28 Most patients do not dispose of their inhalers correctly – only 13% returned them to the pharmacy. Reported rates in the literature of returning inhalers to pharmacies ranged from 2–35%.29, 30, 31 In our audit 78% incorrectly thought they could be disposed of in local council recycling bins. Other studies show similar misconceptions surrounding inhaler disposal. Encouragingly in previous studies there appears to be high motivation for recycling – between 98.3–100% of patients said that they will dispose of inhalers appropriately in the future after being told how.29, 30, 31 Thus, if this knowledge gap was addressed it may result in significant behaviour change.
Prescribing
Approximately a third of patients audited receive their inhalers on repeat prescription automatically each month (37% of DPI users and 33% MDI users). For inhalers used with regular dosing this may be appropriate, however for inhalers used as relievers with unpredictable ‘PRN’ usage, this may represent over- or under-supply.32 To prevent oversupply of PRN medications, variable use prescription modalities could be used, where patients request new inhalers when it has run out. Furthermore, this gives greater potential for prescribers to monitor usage and notice when review may be required. Both MDIs and DPIs can be used with regular dosing, and thus it is hard to conclude whether this represents inappropriate prescribing.
Strengths and limitations
A strength of this study is that data were collected from multiple hospitals across the UK. We audited inhaled therapy across a range of diseases, with no exclusion of participants based on indication. The study took place in a ‘real world’ setting rather than during a trial or extended observational period. Therefore, the audit tool that we have created is likely to be usable and useful with inpatient populations using inhalers across the UK.
This study adds to the growing literature on patient perspectives regarding respiratory care. It also provides a proforma (in appendix) that can be used to better inform clinical decision making. The act of completing the audit also serves to raise awareness, review inhaler technique and start conversations with patients regarding the environmental impact of inhalers.
We did not collect demographic data. We could not adjust for or consider demographic factors which may affect inhaler technique and reasons for switching inhalers.2,13 It may be that the prevalence of these characteristics amongst our respondents contributed to the slight differences between our study and previous ones.
There is no consensus on how best to assess and report errors in inhaler technique. To assess errors, we used a self-assessment questionnaire followed by demonstrations by patients, this is common to other studies.2,13 There is the potential for interviewer bias and inter-observer variability as different interviewers were carrying out the assessments at different sites. We mitigated for this by training interviewers at an initial webinar, and ensuring each team had senior supervision. There is also the risk of social desirability bias, that patients reported what they felt the interviewer wanted to hear. Additionally, carrying out the interviews at times of acute admissions may not accurately reflect how patients view their inhalers most of the time, evidence shows that at times of crisis patients are more likely to consider changing their behaviour.33
The way in which errors in inhaler technique are reported is highly variable.2,13,34,35 We assessed patients against a set of errors identified as important in previous studies, however did not tailor this to specific devices, and as such may overestimate the number of ‘critical’ errors our patients were making.36 Additionally, inhaler technique was only assessed once so may not have reflected ongoing use.
Some people will be more likely than others to participate in an audit (selection bias), although it is unknown whether these people are more or less likely to have good inhaler technique or consider switching inhalers. Patients may have been more likely to state that they would consider switching inhalers because it is known that people will consider behaviour changes at significant life events (such as a hospital admission).33
Conclusions
We have demonstrated that a simple audit proforma can be used as a tool to explore inhaler technique and patient preferences for inhalers. We audited inhaler practice at eight sites with 143 participants across the UK and have provided a baseline data set for future use. We demonstrated that despite high levels of confidence in inhaler technique, patients make regular errors and only a minority report having had recent demonstrations. The majority think that the environmental impact of inhalers is an important consideration when choosing inhalers. We also demonstrated important knowledge gaps surrounding inhaler disposal. These are important findings as the NHS aims to reach net zero, reducing the carbon footprint of healthcare while ensuring high quality care. Healthcare professionals, where appropriate to do so, should endeavour to support patients to safely switch to low-carbon inhalers and provide education on inhaler disposal and recycling. This methodology was useful for understanding patient preferences. We recommend that future projects also collect data regarding type of device, this is because different devices have different ‘critical errors’ and prescribing best practice. With patient preference aligning with sustainable choices switching to lower carbon inhalers is ‘low hanging fruit’ in the efforts to reduce the environmental impact of respiratory care. Future research should explore why despite patient preferences for low carbon inhalers, most patients historically receive MDIs.25
CRediT authorship contribution statement
Evie Rothwell: Writing – original draft, Writing – review & editing. Joseph McElvaney: Conceptualization, Investigation, Methodology, Project administration, Writing – review & editing, Data curation, Formal analysis. Alice Fitzpatrick: Conceptualization, Investigation, Methodology, Project administration, Writing – review & editing. Maria van Hove: Conceptualization, Investigation, Methodology, Project administration, Writing – review & editing. Anya Gopfert: Conceptualization, Investigation, Methodology, Project administration, Writing – review & editing. Lewis Standing: Conceptualization, Investigation, Methodology, Project administration, Writing – review & editing. Sarah Catherine Walpole: Conceptualization, Investigation, Methodology, Project administration, Writing – review & editing.
Declaration of competing interest
Sarah Walpole sits as a trustee of Healthcare Infection Society and is an Associate of the Centre for Sustainable Healthcare (both unpaid positions).
No other conflicts of interest.
Acknowledgments
Acknowledgements
We would like to thank participating sites for their support and input.
Footnotes
This article reflects the opinions of the author(s) and should not be taken to represent the policy of the Royal College of Physicians unless specifically stated.
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.fhj.2024.100141.
Appendix. Supplementary materials
References
- 1.Tennison I, Roschnik S, Ashby B, et al. Health care's response to climate change: a carbon footprint assessment of the NHS in England. Lancet Planetary Health. 2021;5(2):e84–e92. doi: 10.1016/S2542-5196(20)30271-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Melani AS, Bonavia M, Cilenti V, et al. Inhaler mishandling remains common in real life and is associated with reduced disease control. Respir Med. 2011;105(6):930–938. doi: 10.1016/j.rmed.2011.01.005. [DOI] [PubMed] [Google Scholar]
- 3.Scichilone N. Asthma control: the right inhaler for the right patient. Adv Ther. 2015;32(4):285–292. doi: 10.1007/s12325-015-0201-9. Epub 20150407PubMed PMID: 25845769; PMCID:PMC4415938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sanchis J, Corrigan C, Levy ML, Viejo JL. Inhaler devices – from theory to practice. Respir Med. 2013;107(4):495–502. doi: 10.1016/j.rmed.2012.12.007. [DOI] [PubMed] [Google Scholar]
- 5.Wilkinson A, Woodcock A. The environmental impact of inhalers for asthma: A green challenge and a golden opportunity. Br J Clin Pharmacol. 2022;88(7):3016–3022. doi: 10.1111/bcp.15135. [DOI] [PubMed] [Google Scholar]
- 6.Jeswani HK, Azapagic A. Life cycle environmental impacts of inhalers. J Clean Prod. 2019:237. doi: 10.1016/j.jclepro.2019.117733. [DOI] [Google Scholar]
- 7.NHS England. Delivering a ‘Net Zero’ national health service. 2022.
- 8.Allen M. NHS England [Internet]: NHS England. 2023. [cited 2023]. Available from: https://www.england.nhs.uk/blog/delivering-high-quality-low-carbon-respiratory-care/.
- 9.British Thoracic Society. Position statement: the environment and lung health 2020. 2020.
- 10.Woodcock A, Janson C, Rees J, et al. Effects of switching from a metered dose inhaler to a dry powder inhaler on climate emissions and asthma control: post-hoc analysis. Thorax. 2022;77(12):1187–1192. doi: 10.1136/thoraxjnl-2021-218088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.National Institute for Health and Care Excellence (NICE). NICE guideline [NG80] Asthma: diagnosis, monitoring and chronic asthma management. 2017.
- 12.National Institute for Health and Care Excellence (NICE). NICE guideline [NG115] Chronic obstructive pulmonary disease in over 16s: diagnosis and management. 2018. [PubMed]
- 13.Chorão P, Pereira AM, Fonseca JA. Inhaler devices in asthma and COPD – An assessment of inhaler technique and patient preferences. Respir Med. 2014;108(7):968–975. doi: 10.1016/j.rmed.2014.04.019. [DOI] [PubMed] [Google Scholar]
- 14.Usmani OS, Lavorini F, Marshall J, et al. Critical inhaler errors in asthma and COPD: a systematic review of impact on health outcomes. Respir Res. 2018;19(1):10. doi: 10.1186/s12931-017-0710-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Press VG, Arora VM, Shah LM, et al. Teaching the use of respiratory inhalers to hospitalized patients with asthma or COPD: a randomized trial. J Gen Intern Med. 2012;27(10):1317–1325. doi: 10.1007/s11606-012-2090-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Litt HK, Press VG, Hull A, Siros M, Luna V, Volerman A. Association between inhaler technique and confidence among hospitalized children with asthma. Respir Med. 2020;174 doi: 10.1016/j.rmed.2020.106191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zajac P, Press V. Can inhaler confidence predict correct inhaler technique in patients? Chest. 2021;160(4, Supplement):A2346. doi: 10.1016/j.chest.2021.07.2036. [DOI] [Google Scholar]
- 18.Sleath B, Ayala GX, Gillette C, et al. Provider demonstration and assessment of child device technique during pediatric asthma visits. Pediatrics. 2011;127(4):642–648. doi: 10.1542/peds.2010-1206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gibson PG, Powell H, Wilson A, et al. Self-management education and regular practitioner review for adults with asthma. Cochrane Database Syst Rev. 2002;(3) doi: 10.1002/14651858.CD001117. PubMed PMID: CD001117. [DOI] [PubMed] [Google Scholar]
- 20.Takemura M, Kobayashi M, Kimura K, et al. Repeated instruction on inhalation technique improves adherence to the therapeutic regimen in asthma. J Asthma. 2010;47(2):202–208. doi: 10.3109/02770900903581692. [DOI] [PubMed] [Google Scholar]
- 21.Florman K, Wickham H, Hodge A, et al. S65 Global warming impact of inhalers: the patient perspective. Thorax. 2022;77(Suppl 1):A41. doi: 10.1136/thorax-2022-BTSabstracts.71. -A. [DOI] [Google Scholar]
- 22.Liew K, Wilkinson A. P280 How do we choose inhalers? patient and physician perspectives on environmental, financial and ease-of-use factors. Thorax. 2017;72(Suppl 3):A235–A2A7. doi: 10.1136/thoraxjnl-2017-210983.422. [DOI] [Google Scholar]
- 23.D'Ancona G, Cumella A, Renwick C, Walker S. The sustainability agenda and inhaled therapy: what do patients want? Eur Respiratory J. 2021;58(Suppl 65):PA3399. doi: 10.1183/13993003.congress-2021.PA3399. [DOI] [Google Scholar]
- 24.National Institute for Health and Care Excellence (NICE). NICE guidance [NG80] Asthma inhalers and climate change (patient decision aid). 2022.
- 25.Lavorini F, Corrigan CJ, Barnes PJ, et al. Retail sales of inhalation devices in European countries: So much for a global policy. Respir Med. 2011;105(7):1099–1103. doi: 10.1016/j.rmed.2011.03.012. [DOI] [PubMed] [Google Scholar]
- 26.Twigg AJ, Wilkinson A, Smith JN. Local variation in low carbon footprint inhalers in pre-COVID pandemic primary care prescribing guidelines for adult asthma in England and its potential impact. Br J Clin Pharmacol. 2022;88(12):5083–5092. doi: 10.1111/bcp.15511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Murphy A, Howlett D, Gowson A, Lewis H. Understanding the feasibility and environmental effectiveness of a pilot postal inhaler recovery and recycling scheme. NPJ Prim Care Respir Med. 2023;33(1):5. doi: 10.1038/s41533-023-00327-w. Epub 20230121PubMed PMID: 36681666; PMCID:PMC9864496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Practise G. Inhalers [Webpage]. https://www.greenerpractice.co.uk/information-and-resources/information-for-patients/inhalers/: Greener Practise; 2024 [cited 2024 16/01/2024]. https://www.greenerpractice.co.uk/information-and-resources/information-for-patients/inhalers/; Webpage:[An article writen by the organisation Greener Practise with a view to educate the public regarding the sustainability issues surrounding inhalers.]. Available from: https://www.greenerpractice.co.uk/information-and-resources/information-for-patients/inhalers/.
- 29.Sivarajasingam V. BJGP Life [Internet]. BJGP Life: BJGP life. 2021. [cited 2023]. Available from: https://bjgplife.com/understanding-patients-knowledge-of-inhaler-recycling/.
- 30.De Vos R, Rupani H, Longstaff J, et al. Inhaler recycling prevalence in a secondary care clinic in England. Eur Respiratory J. 2020;56(suppl 64):1886. doi: 10.1183/13993003.congress-2020.1886. [DOI] [Google Scholar]
- 31.Baithun C, Rooke Z, Srinivas J. 718 ‘I know where you bin’: inhaler use and disposal practices within paediatrics at Milton Keynes University Hospital. Arch Dis Child. 2022;107(Suppl 2):A312–A3A3. doi: 10.1136/archdischild-2022-rcpch.504. [DOI] [Google Scholar]
- 32.De Simoni A, Hajmohammadi H, Pfeffer P, Cole J, Griffiths C, Hull SA. Reducing short-acting beta-agonist overprescribing in asthma: lessons from a quality-improvement prescribing project in East London. Br J General Practice. 2022;72(722):e619–ee26. doi: 10.3399/bjgp.2021.0725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ogden J, Hills L. Understanding sustained behavior change: the role of life crises and the process of reinvention. Health. 2008;12(4):419–437. doi: 10.1177/1363459308094417. PubMed PMID: 18818273. [DOI] [PubMed] [Google Scholar]
- 34.Lenney J, Innes JA, Crompton GK. Inappropriate inhaler use: assessment of use and patient preference of seven inhalation devices. EDICI. Respiratory Med. 2000;94(5):496–500. doi: 10.1053/rmed.1999.0767. PubMed PMID: 10868714. [DOI] [PubMed] [Google Scholar]
- 35.Khassawneh BY, Al-Ali MK, Alzoubi KH, et al. Handling of inhaler devices in actual pulmonary practice: metered-dose inhaler versus dry powder inhalers. Respir Care. 2008;53(3):324–328. https://pubmed.ncbi.nlm.nih.gov/18291048/ PubMed PMID:18291048. [PubMed] [Google Scholar]
- 36.Price DB, Román-Rodríguez M, McQueen RB, et al. Inhaler errors in the CRITIKAL study: type, frequency, and association with asthma outcomes. J Allergy Clin Immunol: Practice. 2017;5(4):1071–1081. doi: 10.1016/j.jaip.2017.01.004. e9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.