Abstract
Purpose of review
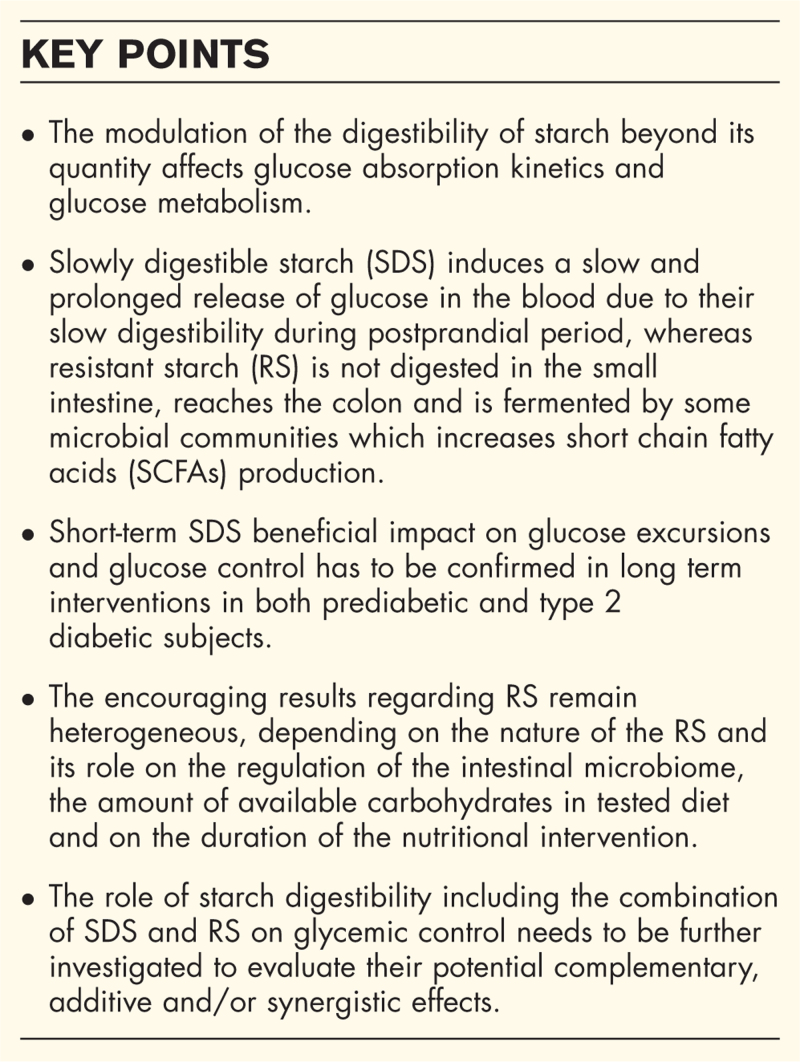
This review will summarize recent studies assessing the effect of slowly digestible starch (SDS) and resistant starch (RS) on glucose metabolism in healthy, prediabetic or type 2 diabetic adults.
Recent findings
Currently, a particular interest in starch and its digestibility has arisen, with data showing a positive effect of SDS and RS on the glucose homeostasis of healthy, at-risk, prediabetic and type 2 diabetic patients but research is ongoing.
Summary
Carbohydrates (CHO) and especially starch play a major role in the prevention and management of metabolic diseases such as type 2 diabetes (T2D). This largely depends on the quality and the digestibility (rate and extent) of the ingested starchy products, beyond their quantity. SDS have been poorly studied but display a beneficial effect on reducing glucose excursions in healthy and insulin-resistant subjects and a relevant potential to improve glucose control in type 2 diabetic individuals. As for RS, the results appear to be encouraging but remain heterogeneous, depending the nature of the RS and its role on microbiota modulation. Further studies are needed to confirm the present results and investigate the potential complementary beneficial effects of SDS and RS on long-term glucose homeostasis to prevent cardiometabolic diseases.
Keywords: diabetes, glycemic control, glycemic profile, starch digestibility
INTRODUCTION
It is estimated that as of 2021, approximately 537 million adults presented with diabetes of which 90% were with type 2 diabetes (T2D) [1]. Dietary carbohydrates (CHO) are the main determinant of meal-related blood glucose excursions and thus play a major role in the management and prevention of T2D [2]. A specific attention must be paid on starch digestibility, as sugars need to be limited [3]. The concept of low glycemic index (GI) based of the lower glycemic response of foods supports the crucial impact of the type of CHO consumed for glucose homeostasis [4]. Starches, which is the main source of daily energy, is mainly provided by tubers such as potatoes, cereals (corn, wheat, rice), legumes (lentils, cheakpeas) and some fruits (plantain banana, mango) [5,6].
Starch is a glucose polymer with two main components: amylose which has a linear structure consisting in d-glucose residues linked by alpha 1,4-glycosidic bonds and amylopectin which has a ramified structure that consists of linear sections with alpha 1,4-glycosidic bonds ramified with alpha 1,6-glycosidic bonds [7]. Starch is digested in the small intestine for available starch fraction and reaches the colon for the nondigestible part, that is, resistant starch (RS). Different factors affect starch digestibility. For instance, the botanical origin of starch determines the amylose/amylopectin ratio. The ratio between these two molecules impacts the rate and extent of starch digestibility, with amylose being digested more slowly than amylopectin. Due to molecular structure of starch including complexation with other molecules (e.g. proteins, lipids) in the food matrix, its digestibility is modified [8]. Also, cooking conditions and in particular water content, temperature and pressure applied may influence its digestibility: shorter and lower temperature and lower water content leads to higher SDS content [9]. Several in vitro methodologies evaluated starch digestibility. One, which has been recognized by some Regulatory Authorities (as the European Food Safety Agency), defined starch digestibility in three fractions: rapidly digestible starch (RDS) digested in 20 min, slowly digestible starch (SDS) digested between 20 and 120 min and RS, which is not digested and behave like a fiber and fermented in the colon [10]. RS can be classified in five categories (from RS1 to RS5) which are detailed in Table 1[9,11]. The originality of this review lies in bringing together the impact of SDS and RS on glucose metabolism to determine the value of combining them. So, the purpose of this review is to highlight the current state of research regarding the impact of SDS and RS on glucose metabolism in healthy, at risk, prediabetic or T2D diabetic adults.
Table 1.
| Type | Description | Food sources |
| RS1 | Physically inaccessible starch thanks to an encapsulated structure which prevents contact between amylase and starch within the digestive system | Whole or partly milled grains Seeds Legumes |
| RS2 | Native starch granules (raw) with a special crystalline structure and high-starch density | Raw potato Green banana High-amylose maize |
| RS3 | Retrograded starch obtained after cooking starch which induced gelatinization process then cooling which induced retrogradation process | Cooked and cooled potatoes, bread, pasta, rice Food products with repeated moist heat treatment |
| RS4 | Chemically modified starch or with the introduction of new functional groups | Foods in which modified starches have been used (e.g.: certain breads and cakes) |
| RS5 | Amylose-lipid complex that cannot be penetrated by water or amylase | Native starch granules Processed starch: amylose in bonded to lipid molecules, though either cooking or processing. |
Box 1.
no caption available
EFFECTS OF SLOWLY DIGESTIBLE STARCH AND RESISTANT STARCH ON GLYCEMIC PROFILE OF HEALTHY ADULTS
By using stable isotopes to measure the appearance and disappearance of glucose in plasma, it has been demonstrated that SDS induced a slow and prolonged release of glucose in plasma, resulting in a reduced postprandial glycemic response and consequently a low extended GI [12,13▪]. An acute study was performed on 20 healthy subjects who were given a single portion of starchy products with varying levels of SDS. These products were matched for the amount of available CHO by adapting products serving size to reach 50 g of available CHO for each. Products with the highest SDS content between 23.9 and 27.5 g/100 g induced the lowest glycemic responses, with the lowest incremental area under the curve (iAUC) 0–120 min of glucose and glycemic peak, associated with the lowest iAUC of insulin concentration [14]. A meta-analysis based on five studies using different SDS contents and matrices (SDS microspheres, pasta, breads, potatoes, biscuits, porridge) and culinary processes (boiling and cooling, rotary molding) over a single intake showed some discrepancies. The acute consumption of SDS had a positive effect on glycemic profile with a significant reduction of postprandial glycemia in 2 studies without effect in the others. Moreover a positive association between glycemia, insulinemia, incretins and glucagon in one hand and SDS intake in the other hand has been found [13▪]. More widely, another meta-analysis confirmed that the slow release of exogenous glucose is associated to the lower glycemic and insulin responses [15]. From this review, 10 out of the 12 studies included in the meta-analysis evaluated the effect of SDS on glycemic profile. There is a consensus that limitation of postprandial glycemic and insulin responses has a beneficial effect on the prevention of T2D [16]. Recently, no studies have been performed on the long-term impact of SDS on glucose homeostasis in healthy subjects.
Several papers studied both short- and long-term intake effects of RS in healthy individuals. It has been well accepted and confirmed recently that the replacement of available CHO by RS led to the reduction of postprandial glycemic and insulin responses [17,18] whereas there was no effect on glycemic response when tested- and control products contained the same amount of available CHO [17–20]. A reduction in glycemic responses has been shown with acute consumption of amylose-rich products, the amount of which correlates with the amount of RS [21,22]. Also, two studies on acute of 17.9–29.7 g RS4 consumption have also shown a reduction in postprandial glycemic and insulinemic responses [23,24], regardless of the dose of RS4 [24]. For all these last studies the amount of CHO between tested- and control product was matched [21–24]. More widely, a review summarized the acute effect of dietary fibers in healthy individuals including 41 studies: 6 ones investigated the single intake of RS in addition of available CHO. Five of them showed that RS could improve glycemia by lowering glucose iAUC 0–120 min and from these five, three of them revealed a lower peak of glucose after the consumption of RS in healthy individuals [25▪▪]. Indeed, RS may be an effective way to reduce postprandial glycemic response in short term. However, even if insulin response was regularly associated to this decrease in glycemic response, the associated mechanisms were not elucidated and require more research.
Few long-term intake studies in healthy subjects have been found in the recent literature on native RS2. From 4 to 12 weeks, based on five studies concerning healthy individuals in a review on all populations, data showed mixed results with an improvement only in insulin sensitivity measured by a euglycemic-hyperinsulinemic clamp after intervention in three studies and no impact on glycemic profile for two studies. All amounts of available CHO were equal between test and control products [17]. The same results have been found in another study, with an improvement in postprandial glycemia and insulinemia after one week of intervention in healthy subjects, but no matching for available CHO content. The better glycemic profile observed was associated with changes in microbiota composition, with in particular an increase in bacterial butyrate-producers [26,27].
Overall, starch digestibility modulation appears to have a positive effect on the glycemic profile of healthy individuals. In short or long term interventions, the variability in the amount of CHO between test and control products leads to discrepancies.
EFFECTS OF SLOWLY DIGESTIBLE STARCH AND RESISTANT STARCH ON GLYCEMIC PROFILE OF AT RISK OR PREDIABETIC ADULTS
Dietary advices are very important for at-risk or prediabetic populations, in order to avoid or at least delay T2D onset and the need of medications [25▪▪].
In 2017, the effects of 17.9 g of SDS for 100 g of biscuit introducing in breakfast of individuals at risk during three weeks were investigated. Data showed a reduction in fasting blood glucose levels and postprandial blood glucose and insulin responses, with matched amounts of CHO between the low-SDS and high-SDS products. Despite the positive effects of SDS on glycemic profile and the low-grade inflammatory parameters, also reported, did not change [28]. To our knowledge, the longer-term impact of SDS on glucose homeostasis in at risk or prediabetic subjects has not been studied.
Short-term consumption of RS has shown inconclusive effects on at metabolic risk subjects. Indeed, any effect of a single intake of 20 g of Native Banana Starch (NBS) rich in RS on postprandial glycemic or insulinemic responses in comparison to high-amylose maize starch containing the same amount of RS or digestible maize starch has been observed. In this study, all the supplements were matched for their amount of available CHO [29]. In another study in this population, an acute intake of RS3 formed by retrogradation has reduced the iAUC 0–120 min of insulin and GIP but not of glucose. However, a significant reduction at 15 and 30 min in glucose, insulin and GIP concentrations was observed [30]. A recent review with only one out of five studies in overweight subjects has shown an improvement in postprandial glycemic and insulinemic responses after the consumption of a scone rich in RS4 but control and test products did not contain the same amount of available CHO [25▪▪]. Recently, a meta-analysis of 31 studies including 5 acute studies in prediabetic adults, examined the effect of all types of RS on glycemic profile. Only RS1 and RS2 lowered postprandial glycemia, while RS2 affected insulin, highlighting different metabolic effects between RS types [31▪▪].
Recent data are available on the long-term RS consumption impact on glucose homeostasis of individuals at metabolic risk. Based on seven studies reviewed on this population, a reduction in fasting insulin and insulin resistance in this population with RS2 in a dose-dependent manner has been shown [17]. However, three meta-analyses on patients with overweight, obesity or metabolic syndrome highlighted discrepancies: the first one, including 10 studies in overweight or obese patients, showed an improvement in glycemic control with a lowering effect on fasting glucose, insulin and HbA1c [32] as the second which observed the same beneficial results after analyzing 10 studies [33] but the amount of available carbohydrates was not always the same between control and test products. The last one, based on 12 studies, showed limited evidence with no effect of RS2 on the glycemic profile and control of these patients [34]. Recently, studies have shown that RS4 reduced fasting glycemia and HbA1c in prediabetic subjects [35] and significantly lowered level in fasting plasma insulin and HOMA-IR (Homeostasis Model Assessment of Insulin Resistance) indicating a better insulin sensitivity following the ingestion of RS, even if HbA1c and fasting blood glucose did not change [36]. As in healthy subjects, RS stimulates the production of SCFAs by the microbiota, modulating the production of incretins, with beneficial effects on insulin production and sensitivity, and glucose disposal in tissues [31▪▪].
To conclude, the positive effects of SDS on CHO metabolism in this population are based on very few studies and need confirmation. Regarding RS, the results are rather heterogeneous, depending on the duration of the nutritional intervention, the type, the dose of RS used and the amount of CHO between the groups.
EFFECTS OF SLOWLY DIGESTIBLE STARCH AND RESISTANT STARCH ON GLYCEMIC PROFILE OF TYPE 2 DIABETIC PATIENTS
In diabetic population, maintaining glycemic control is essential to prevent cardiovascular complications [37].
The first study suggesting a role of SDS in glucose homeostasis in T2D patients was published in 1995. They reported that raw cornstarch rich in SDS used as an evening snack led to reduce nocturnal and morning hypoglycemia without causing hyperglycemia [12]. Since then, only one study was performed on SDS in T2D population. After 1 week-intake of a published 60 g of SDS-diet per day, several parameters of glycemic variability (GV) decreased compared to a low-SDS diet: Standard deviation (SD) was lowered by 17% and mean amplitude of glucose excursions (MAGE) was lowered by 23%; less time was spent in high glycemic target and lower postprandial glycemic excursions have been observed. As some of these parameters have repeatedly been correlated with HbA1c, these results are predictive of a longer-term HbA1c reduction with the diet [38–40]. However, the amount of available CHO between the low and high-SDS diets was not similar and it was a relatively short-term pilot study.
The results of short-term RS intake on glycemic control in T2D patients are highly heterogeneous. A study has shown no effect of NBS supplementation provided 40 g of RS during 4 days either on glycemic control or GV [41]. In contrast the same team comparing NBS with the same amount of RS and control after 4 days of consumption on glycemic responses have shown a reduction in fasting glycemia, peak glycemia and postprandial insulinemic responses after an oral meal tolerance test [42▪]. A review including 8 studies on T2D patients, confirmed this result and subgroup analyzes showed that this effect was greater in T2D patients compared with the prediabetic population [31▪▪].
On longer-term intake, effects of RS are also unclear. A positive impact of RS on the glycemic profile and control of T2D patients, with a reduction in fasting glucose and HbA1c, after a high-RS low-protein diet, was observed [43]. A meta-analysis including three studies on T2D patients, has shown a decrease in fasting glucose and insulin [32] due to the same mechanism involved in prediabetic subjects. Another study showed that consumption of 40 g of RS2 for 12 weeks in T2D patients did not change the glycemic profile and control including fasting glucose and insulin, HbA1c and insulin sensitivity. However, they observed a tendency towards greater glucose uptake than control using arteriovenous sampling to assess muscle metabolism in vivo [17]. Same results were found in a review including 3 studies on this T2D population with no effect in glycemic profile after RS2 ingestion [33].
In conclusion, the effects of SDS on glycemic profile have to be confirmed in T2D population, particularly for the longer-term impact. With regard to RS, the results are contradictory, and it seems difficult to reach a conclusion on their effects on glycemic control in T2D patients also depending on the duration, the type, the dose of RS, and the amount of CHO used in the different studies. In addition, these results may be influenced by physical activity which is not always controlled, but also by the hypoglycemic treatments taken by patients, which should be taken into account.
CONCLUSION
As far as SDS are concerned, whether in very short or medium term-consumption, a positive impact of SDS on CHO homeostasis in healthy, at-risk, prediabetic or T2D populations has been shown. With regard to RS, although the results appear to be encouraging, they seem to be very much influenced by the nature of the RS and its role on microbiota modulation. Studies, mixing SDS and RS in the same diet, need to be addressed to evaluate the potential complementary beneficial effects of SDS and RS on long-term glucose homeostasis to prevent cardiometabolic diseases.
Acknowledgements
We would like to thank Dr Alexandra Meynier for her contribution on this review.
Financial support and sponsorship
None.
Conflicts of interest
S.V. is an employee of Mondelez International R&D.
REFERENCES AND RECOMMENDED READING
Papers of particular interest, published within the annual period of review, have been highlighted as:
▪ of special interest
▪▪ of outstanding interest
REFERENCES
- 1.Facts & figures. International Diabetes Federation. 2021. Available at: https://idf.org/about-diabetes/diabetes-facts-figures/ [Accessed January 16, 2024]. [Google Scholar]
- 2.Carbohydrate intake for adults and children: WHO guideline. World Health Organization; 2023. [PubMed] [Google Scholar]
- 3.Ley SH, Hamdy O, Mohan V, Hu BF. Prevention and management of type 2 diabetes: dietary components and nutritional strategies. Lancet 2014; 383:1999–2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jenkins DJA, Willett WC, Yusuf S, et al. Association of glycaemic index and glycaemic load with type 2 diabetes, cardiovascular disease, cancer, and all-cause mortality: a meta-analysis of mega cohorts of more than 100 000 participants. Lancet Diabetes Endocrinol 2024; 12:107–18. [DOI] [PubMed] [Google Scholar]
- 5.Holesh JE, Aslam S, Martin A. Physiology, carbohydrates. StatPearls, Treasure Island (FL): StatPearls Publishing; 2024. [PubMed] [Google Scholar]
- 6.Bello-Perez LA, Flores-Silva PC, Agama-Acevedo E, Tovar J. Starch digestibility: past, present, and future. J Sci Food Agric 2020; 100:5009–5016. [DOI] [PubMed] [Google Scholar]
- 7.Wang Z, Wang S, Xu Q, et al. Synthesis and functions of resistant starch. Adv Nutr 2023; 14:1131–1144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Robertson TM, Brown JE, Fielding BA, et al. Resistant starch production and glucose release from pre-prepared chilled food: the SPUD project. Nutr Bull 2021; 46:52–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Murillo S, Mallol A, Adot A, et al. Culinary strategies to manage glycemic response in people with type 2 diabetes: a narrative review. Front Nutr 2022; 9:1025993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Englyst HN, Kingman SM, Cummings JH. Classification and measurement of nutritionally important starch fractions. Eur J Clin Nutr 1992; 46: (Suppl 2): S33–S50. [PubMed] [Google Scholar]
- 11.Lockyer S, Nugent AP. Health effects of resistant starch. Nutr Bull 2017; 42:10–41. [Google Scholar]
- 12.Miao M, Jiang B, Cui SW, et al. Slowly digestible starch—a review. Crit Rev Food Sci Nutr 2015; 55:1642–1657. [DOI] [PubMed] [Google Scholar]
- 13▪.Wang Y, Zhou X, Xiang X, Miao M. Association of slowly digestible starch intake with reduction of postprandial glycemic response: an update meta-analysis. Foods 2022; 12:89. [DOI] [PMC free article] [PubMed] [Google Scholar]; The meta-analysis includes the most recent data and shows positive effects of SDS on postprandial responses in healthy individuals.
- 14.Cesbron-Lavau G, Goux A, Atkinson F, et al. Deep dive into the effects of food processing on limiting starch digestibility and lowering the glycemic response. Nutrients 2021; 13:381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Boers HM, Alssema M, Mela DJ, et al. The rate of glucose appearance is related to postprandial glucose and insulin responses in adults: a systematic review and meta-analysis of stable isotope studies. J Nutr 2019; 149:1896–1903. [DOI] [PubMed] [Google Scholar]
- 16.Livesey G, Taylor R, Livesey HF, et al. Dietary glycemic index and load and the risk of type 2 diabetes: a systematic review and updated meta-analyses of prospective cohort studies. Nutrients 2019; 11:E1280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Harris KF. An introductory review of resistant starch type 2 from high-amylose cereal grains and its effect on glucose and insulin homeostasis. Nutr Rev 2019; 77:748–764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Belobrajdic DP, Regina A, Klingner B, et al. High-amylose wheat lowers the postprandial glycemic response to bread in healthy adults: a randomized controlled crossover trial. J Nutr 2019; 149:1335–1345. [DOI] [PubMed] [Google Scholar]
- 19.Du Y, Wu Y, Xiao D, et al. Food prototype containing resistant starch type 4 on postprandial glycemic response in healthy adults. Food Funct 2020; 11:2231–2237. [DOI] [PubMed] [Google Scholar]
- 20.Steele TJ, Maningat CC, Seib PA, et al. Metabolic responses to native wheat starch (MidsolTM 50) versus resistant wheat starch type 4 (Fibersym® RW): standard versus marketplace testing protocols. Curr Dev Nutr 2021;5:nzab011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ang K, Bourgy C, Fenton H, et al. Noodles made from high amylose wheat flour attenuate postprandial glycaemia in healthy adults. Nutrients 2020; 12:E2171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Haini N, Jau-Shya L, Mohd Rosli RG, Mamat H. Effects of high-amylose maize starch on the glycemic index of Chinese steamed buns (CSB). Heliyon 2022; 8:e09375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gourineni V, Stewart ML, Wilcox ML, Maki KC. Nutritional bar with potato-based resistant starch attenuated post-prandial glucose and insulin response in healthy adults. Foods 2020; 9:E1679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Steele TJ, Steele CC, Maningat CC, et al. Glycemic and insulinemic responses of healthy humans to a nutrition bar with or without added Fibersym® RW, a cross-linked phosphorylated RS4-type resistant wheat starch. Int J Environ Res Public Health 2022; 19:13804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25▪▪.Tsitsou S, Athanasaki C, Dimitriadis G, Papakonstantinou E. Acute effects of dietary fiber in starchy foods on glycemic and insulinemic responses: a systematic review of randomized controlled crossover trials. Nutrients 2023; 15:2383. [DOI] [PMC free article] [PubMed] [Google Scholar]; In contrast to other studies in the literature, which have established the positive long-term effect of RS on glucose metabolism, this review examined the short-term effects of dietary fibers, including RS, and found that acute consumption of RS may improve glycemia in healthy individuals and insulinemia in overweight or obese adults.
- 26.Hughes RL, Horn WH, Finnegan P, et al. Resistant starch type 2 from wheat reduces postprandial glycemic response with concurrent alterations in gut microbiota composition. Nutrients 2021; 13:645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wen J-J, Li M-Z, Nie S-P. Dietary supplementation with resistant starch contributes to intestinal health. Curr Opin Clin Nutr Metab Care 2023; 26:334–340. [DOI] [PubMed] [Google Scholar]
- 28.Lambert-Porcheron S, Normand S, Blond E, et al. Modulation of starch digestibility in breakfast cereals consumed by subjects with metabolic risk: impact on markers of oxidative stress and inflammation during fasting and the postprandial period. Mol Nutr Food Res 2017; 61: [DOI] [PubMed] [Google Scholar]
- 29.García-Vázquez C, Ble-Castillo JL, Arias-Córdova Y, et al. Effects of resistant starch ingestion on postprandial lipemia and subjective appetite in overweight or obese subjects. Int J Environ Res Public Health 2019; 16:E3827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Patterson MA, Fong JN, Maiya M, et al. Chilled potatoes decrease postprandial glucose, insulin, and glucose-dependent insulinotropic peptide compared to boiled potatoes in females with elevated fasting glucose and insulin. Nutrients 2019; 11:2066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31▪▪.Pugh JE, Cai M, Altieri N, Frost G. A comparison of the effects of resistant starch types on glycemic response in individuals with type 2 diabetes or prediabetes: a systematic review and meta-analysis. Front Nutr 2023; 10:1118229. [DOI] [PMC free article] [PubMed] [Google Scholar]; The review looks at the short- and long-term effects of all types of RS, as well as the potential mechanisms involved in different populations.
- 32.Wang Y, Chen J, Song Y-H, et al. Effects of the resistant starch on glucose, insulin, insulin resistance, and lipid parameters in overweight or obese adults: a systematic review and meta-analysis. Nutr Diabetes 2019; 9:19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Halajzadeh J, Milajerdi A, Reiner Z, et al. Effects of resistant starch on glycemic control, serum lipoproteins and systemic inflammation in patients with metabolic syndrome and related disorders: a systematic review and meta-analysis of randomized controlled clinical trials. Crit Rev Food Sci Nutr 2020; 60:3172–3184. [DOI] [PubMed] [Google Scholar]
- 34.Snelson M, Jong J, Manolas D, et al. Metabolic effects of resistant starch type 2: a systematic literature review and meta-analysis of randomized controlled trials. Nutrients 2019; 11:E1833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Astina J, Saphyakhajorn W, Borompichaichartkul C, Sapwarobol S. Tapioca resistant maltodextrin as a carbohydrate source of oral nutrition supplement (ONS) on metabolic indicators: a clinical trial. Nutrients 2022; 14:916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Park J, Oh S-K, Doo M, et al. Effects of consuming heat-treated dodamssal brown rice containing resistant starch on glucose metabolism in humans. Nutrients 2023; 15:2248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Aroda VR, Eckel RH. Reconsidering the role of glycaemic control in cardiovascular disease risk in type 2 diabetes: a 21st century assessment. Diabetes Obes Metab 2022; 24:2297–2308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Breyton A-E, Lambert-Porcheron S, Laville M, et al. Relevance in clinical research to evaluate interventions in T2D, a literature review. Front Endocrinol (Lausanne) 2021; 12:666008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Goux A, Breyton A-E, Meynier A, et al. Design and validation of a diet rich in slowly digestible starch for type 2 diabetic patients for significant improvement in glycemic profile. Nutrients 2020; 12:E2404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Breyton A-E, Goux A, Lambert-Porcheron S, et al. Starch digestibility modulation significantly improves glycemic variability in type 2 diabetic subjects: a pilot study. Nutr Metab Cardiovasc Dis 2021; 31:237–246. [DOI] [PubMed] [Google Scholar]
- 41.Arias-Córdova Y, Ble-Castillo JL, García-Vázquez C, et al. Resistant starch consumption effects on glycemic control and glycemic variability in patients with type 2 diabetes: a randomized crossover study. Nutrients 2021; 13:4052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42▪.García-Vázquez C, Ble-Castillo JL, Arias-Córdova Y, et al. Effects of resistant starch on glycemic response, postprandial lipemia and appetite in subjects with type 2 diabetes. Eur J Nutr 2023; 62:2269–2278. [DOI] [PubMed] [Google Scholar]; The article shows a conclusive effect of starch on the glycemic profile of type 2 diabetes patients.
- 43.Meng Y, Bai H, Yu Q, et al. High-resistant starch, low-protein flour intervention on patients with early type 2 diabetic nephropathy: a randomized trial. J Ren Nutr 2019; 29:386–393. [DOI] [PubMed] [Google Scholar]