Abstract
Background
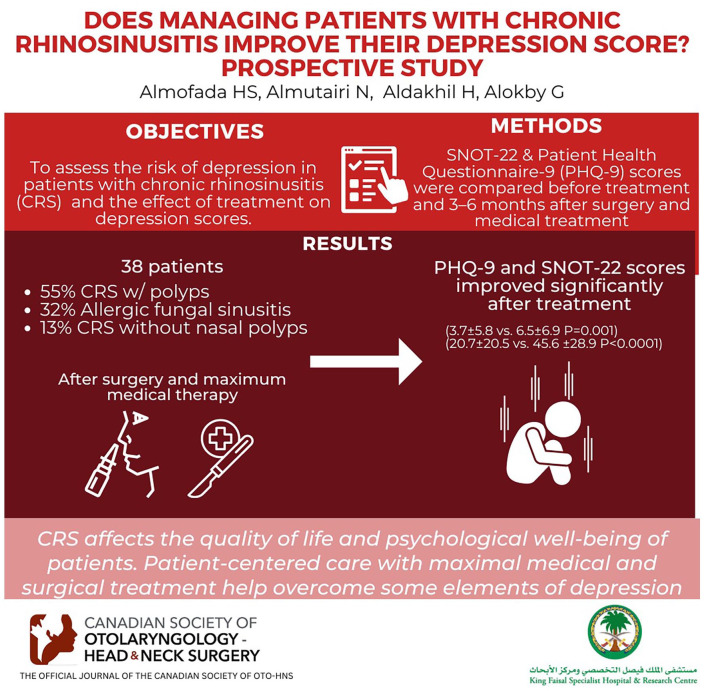
To assess the risk of depression in patients with chronic rhinosinusitis (CRS) in a tertiary care center and the effect of treatment on depression scores.
Methods
This prospective cohort study was conducted at King Faisal Specialist Hospital and Research Center, Riyadh, Saudi Arabia, between November 2021 and June 2022 and included adult patients (≥14 years) with CRS. The validated Arabic or English Sinonasal Outcome Test (SNOT-22) and Patient Health Questionnaire-9 (PHQ-9) were used before treatment and 3 to 6 months after surgery and maximal medical treatment. PHQ-9 scores were compared at baseline and follow-up visits. The relationship between changes in SNOT-22 and PHQ-9 scores were assessed using Spearman’s correlation and simple linear regression.
Results
Overall, 38 participants with a mean ± SD age of 32.7 ± 12 years were enrolled. CRS with nasal polyps (55.26%) was the most frequently seen condition, followed by allergic fungal CRS (31.58%) and CRS without nasal polyps (13.16%). Six patients (15.7%) had PHQ-9 scores ≥10, indicating they had major depressive disorder. PHQ-9 and SNOT-22 scores improved significantly after treatment (3.7 ± 5.8 vs 6.5 ± 6.9 pretreatment, P = .001; 20.7 ± 20.5 vs 45.6 ± 28.9 pretreatment, P < .0001, respectively). Mean ± SD change in PHQ-9 and SNOT-22 scores was −2.7 ± 7 and −24.9 ± 29.8, respectively. SNOT-22 and PHQ-9 scores were positively correlated (r = .522, P < .001). PHQ-9 score change was significantly associated with SNOT-22 score change (β = .178, 95% confidence interval 0.12-0.23, P < .0001).
Conclusion
CRS affects the quality of life and psychological well-being of patients. Patient-centered care with maximal medical and surgical treatment help overcome its deleterious consequences.
Keywords: chronic rhinosinusitis, depression, Sinonasal Outcome Test, Patient Health Questionnaire-9
Graphical abstract.
Background
Chronic rhinosinusitis (CRS) considerably affects the quality of life and psychological well-being of patients owing to its discomforting symptoms and negative effect on mood, sleep, and cognitive ability, thereby imposing a substantial financial burden.1,2 Many studies have found a relationship between CRS and depression, with a much higher incidence of depression in patients with CRS than in the general population and at a level that is similar to that seen in patients with other debilitating chronic diseases such as heart and kidney diseases and various cancers.1-5 In the general population, the life-time risk of being diagnosed with anxiety, depression, and dysthymia is 16.6%, 6.7%, and 3.6%, respectively.4,5 However, patients with CRS have a prevalence of approximately 15% for anxiety, 30% for depression, and 26% for dysthymia.2,6,7
Various scoring systems have been used to assess the disruption caused by CRS on patients’ lives. To this end, the 22-item Sinonasal Outcome Test (SNOT-22) and Rhinosinusitis Symptoms Disability Index are the most commonly used tools.1,3,7-12 Furthermore, the Hospital Anxiety and Depression Score, 2-item Patient Health Questionnaire, 9-item Patient Health Questionnaire (PHQ-9), and Beck Depression Inventory are the most commonly used screening tools for patients’ psychological well-being.2,3,7,9-13
Bhattacharyya et al reported that depression and anxiety had no effect on the symptoms reported by patients with CRS and should not guide or affect the diagnostic strategy of CRS. 7 Notably, in multiple studies using different scoring systems, most patients with CRS reported relief in their sinonasal symptoms with decreased symptom and psychological instrument scores following surgical/medical management.2,3,7-10,13,14 Nevertheless, other studies found no significant difference in sinonasal and depression scores postsurgical treatment.2,11
The Arabic translation of the PHQ has been found to be valid in detecting depression and other mental health disorders. 15 The Arabic translation of the SNOT-22 has been validated and found to be reliable with good internal consistency.16,17 In this study, we aimed to compare the scores before and after elective surgical intervention followed by maximal medical treatment. To our knowledge, this is the first study to compare the SNOT-22 and PHQ-9 scores in an Arabic population and one of the few studies worldwide to assess these scores pre- and postsurgery using a validated tool.
Methods
Study Design and Population
Approval was obtained from the research and ethics committee at King Faisal Specialist Hospital and Research Center (approval number: 2211154). This study was performed in accordance with the ethical standards of the institutional and/or national research committee and the guidelines of the 1964 Helsinki Declaration and its later amendments or comparable ethical standards, and informed consent was obtained from all study participants.
This prospective cohort study commenced in November 2021 and continued until the end of July 2022. Patients were allocated at the first clinic visit. Adult patients (>14 years) who fulfilled the diagnostic criteria for CRS according to the European Position Paper on Rhinosinusitis and nasal polyps 18 and received medical and surgical treatment were included. Patients who had a history of psychiatric illness, did not speak Arabic, had incomplete data, were illiterate, or did not agree to participate were excluded.
Data were collected at 2 time points (baseline and clinical follow-up visit after treatment). Each patient completed the validated Arabic version of SNOT-22 and PHQ-9 before treatment and 3 to 6 months posttreatment; the questionnaires were provided to the patients and filled during the clinic visits. Data on demographics, comorbidities (such as asthma, diabetes, hypertension), and CRS phenotypes were also retrieved. Patients with discontinued follow-up were contacted for missing data.
Outcomes
The primary objective was to compare the SNOT-22 and PHQ-9 scores before and after CRS patients received appropriate surgical intervention and medical treatment. The secondary objective was to study the relationship between depression severity and the SNOT-22 score.
Sample Size
The sample size was calculated using Stata version 17.0, based on a pilot study of our population (N = 11), which compared the PHQ-9 score before and after treatment and showed a mean of −5 and standard deviation of 8.3. With a significance criterion of α = .05 and power = 0.90, the minimum sample size needed was 33 participants for the paired t test. An additional 10% was added to the sample owing to the expected nonresponse rate; thus, the final sample size was 38.
Instruments/Questionnaire
22-Item Sinonasal Outcome Test
SNOT-22 is an updated modification of the SNOT questionnaire, and it has been validated to assess disease severity and quality of life of patients with sinonasal diseases.16-18 It analyzes rhinological symptoms, ear and facial symptoms, sleep quality, and psychological well-being. It comprises 22 self-reported questions, where each question is given a score ranging from 0 to 5, with higher scores indicating more pronounced severity. It has been translated and validated in multiple languages including Arabic. 16 The Arabic version has been validated and cross-validated in 2 studies.16,17
Patient Health Questionnaire-9
PHQ-9 is a well-known tool for screening psychological disorders, particularly depression.5,11,13,19 It has 9 questions, scored 0 to 3 based on symptoms in the prior 2 weeks. A score of ≥10 has a sensitivity and specificity of 88%; however, the clinical diagnosis is more complex and demanding.5,11,13,19 Furthermore, sorting patients based on PHQ-9 results into mild, moderate, moderately severe, and severe groups based on scores of 5 to 9, 10 to 14, 15 to 19, and 20 to 27, respectively, has been found to be acceptable.3,20 The minimal clinical important difference (MCID) is 5 points. 19 The Arabic translation was validated by AlHadi et al. 15
Statistical Analysis
Descriptive statistics are presented as means and standard deviations or frequencies and percentages. Owing to skewed distribution, a Wilcoxon signed-rank nonparametric test was used to compare PHQ-9 and SNOT-22 scores between the baseline and follow-up visits. The relationship between changes in SNOT-22 and PHQ-9 scores was assessed using Spearman’s correlation and simple linear regression. Statistical significance was set at P < .05. All statistical analyses were performed using Stata version 17.0 (StataCorp LLC).
Results
A total of 38 participants were enrolled in this study with a mean age of 32.7 ± 12 years. There were 20 men (52.6%) and 18 women (47.4%). Most patients had CRS with nasal polyps (CRSwNP) (55.26%, n = 21), followed by allergic fungal CRS (31.58%, n = 12) and CRS without nasal polyps (CRSsNP) (13.16%, n = 5). Twenty patients had comorbidities—hypertension (n = 2), diabetes (n = 4), asthma (n = 12), cystic fibrosis (n = 3), obesity (n = 1), and others (n = 10). The treatment protocol comprised primary/revision surgery with maximal medical treatment (MMT). Surgeries were scheduled after the first encounter in clinic (within 1-2 months) along with patient consent for a complete functional endoscopic sinus surgery (bilateral maxillectomy, ethmoidectomy anterior/posterior, sphenoidotomy, and frontal sinus surgery if needed). Cystic fibrosis patients received more aggressive surgeries (medical maxillectomy and extended sinusotomy). Furthermore, MMT was started before surgery and consisted of oral steroid course pre- and postoperatively, postoperation nasal douching with budesonide irrigation, course of antibiotic postoperatively, and/or short-term intranasal decongestant. Six patients scored ≥10 (15.7%) on PHQ-9, indicating provisional diagnosis of major depressive disorder (Table 1). These patients were counseled in the clinic about the result and offered a psychiatric evaluation.
Table 1.
Clinical and Demographic Characteristics of Study Participants.
| Characteristics | (N = 38), mean ± SD or n (%) |
|---|---|
| Age (years) | 32.7 ± 12 |
| Sex, male | 20 (52.63) |
| Diagnosis | |
| °CRSsNP | 5 (13.16) |
| °CRSwNP | 21 (55.26) |
| °CRSwNP (AF) | 12 (31.58) |
| Treatment | |
| °Medical | 13 (24.21) |
| °Surgical | 25 (65.79) |
| °Comorbidity | 20 (52.63) |
Abbreviations: CRSsNP, chronic rhinosinusitis without nasal polyps; CRSwNP, chronic rhinosinusitis with nasal polyps; CRSwNP (AF), allergic fungal chronic rhinosinusitis.
Patient scores revealed a significant improvement in the median PHQ-9 scores after treatment (2 vs 4.5 pretreatment, P = .001) and SNOT-22 scores (13 vs 38 pretreatment, P < .001). Further subanalysis conducted on patients at risk of depression, the intervention demonstrated clinical significance achieving the MCID, and the P-value remained statistically significant (Table 2).
Table 2.
Comparison of Outcome Measures Before and After Treatment of Chronic Rhinosinusitis.
| N | Baseline, median [Q1 to Q3] | After treatment, median [Q1 to Q3] | Median change [Q1 to Q3] | P-value | |
|---|---|---|---|---|---|
| PHQ-9 | 38 | 4.5 [0 to 11] | 2 [0 to 4] | −1 [−5 to 0] | .001 |
| SNOT-22 | 38 | 38 [25 to 69] | 13 [6 to 29] | −21 [−40 to −2] | <.001 |
| PHQ-9 a | 19 | 11 [7 to 14] | 4 [3 to 6] | −5 [−8 to −1] | <.001 |
Abbreviations: PHQ-9, Patient Health Questionnaire-9; SNOT-22, Sinonasal Outcome Test.
Subgroup analysis on patients screening at-risk of depression (PHQ-9 ≥ 5).
A significant positive correlation was observed between the changes of SNOT-22 and PHQ-9 scores (r = .522, P < .001) using Spearman’s correlation (Figure 1).
Figure 1.
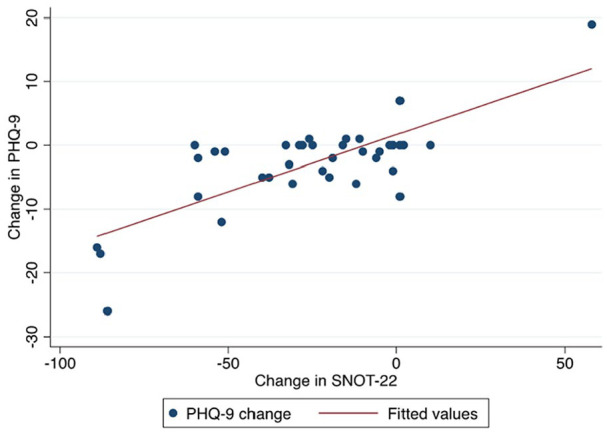
Change in SNOT-22 score versus change in PHQ-9 score of patients with chronic rhinosinusitis. PHQ-9, Patient Health Questionnaire-9; SNOT-22, Sinonasal Outcome Test.
Simple linear regression was used to test whether improvement in the SNOT-22 score predicted improvement in the PHQ-9 score. The model demonstrated an adjusted R 2 value of .568. The change in PHQ-9 score was significantly associated with the change in SNOT-22 score (β = .178, 95% confidence interval 0.12-0.23, P < .001; Figure 1).
Discussion
Numerous studies have found an association between CRS and mental well-being,1-3,7,21 with depression and anxiety being the most prevalent psychological diseases in patients with CRS.1-3,6,7,21 Interestingly, the prevalence of depression and anxiety in patients with CRS was comparable to that in patients with chronic diseases.1-3,7,21 Furthermore, studies have postulated that the risk of depression increases with prolonged CRS.2,21
Our results showed a significant correlation between SNOT-22 scores and PHQ-9 score severity confirming the association between them. These findings are comparable to findings studies by Vandelaar et al, 3 Litvack et al, 10 and Yoo et al. 22
Few studies have investigated CRS treatment outcomes in relation to depression risk, and most studies used validated self-reported questionnaires and reported significant positive results.2,8-10,14 This is similar to our study findings that showed a statistically significant decrease in PHQ-9 scores after treatment (P < .001). However, other studies failed to show any significance.2,11 This discrepancy may be related to the implementation of different measurable scores across published studies, which could have affected their results.
In reference to the CRS phenotype, Kim et al found that patients with CRSsNP are at a higher risk of such mental conditions than those with CRSwNP, though the latter is known to cause more severe symptoms. 21 However, a recent systemic review concluded that the results regarding the phenotype of CRS and depression are inconclusive. 2 Furthermore, studies failed to determine an association between comorbidity, age, race, allergic rhinitis, smoking, and depression in patients with CRS, whereas the relationships between female sex, asthma, and fibromyalgia are controversial. 2 Owing to the limited number of CRS patients with nasal polyps and unequal distribution between independent variables, statistical analysis of the data was not feasible.
Chronic CRS is deemed to be a cause of depression and anxiety, as indicated recently. 2 The speculated mechanisms and associated factors can co-occur, such as lack of sleep, generalized fatigue, social burden, and cognitive impairment.1,2 Moreover, emerging evidence indicates that CRS has a negative impact on brain activity related to cognitive and response stimuli.2,22,23 To our knowledge, this prospective review is the first to use Arabic validated scores to compare sinonasal and depression symptoms and one of the few studies to compare the outcomes of the management based on validated self-reported scores. While the statistically significant improvement in PHQ-9 scores is noteworthy, it is crucial to exercise caution in interpreting the clinical significance of this finding, as it fell below the established MCID. We recognize that the minimal pre-intervention scores may have influenced the magnitude of change, potentially contributing to results that are statistically significant but possibly not clinically meaningful. Further studies are needed to address the effects of CRS treatment on patient well-being and the persistence of depression in patients with CRS. Although we calculated our sample size with a raised margin, our study had a smaller study population than other published studies. However, the prospective study design is the main strength of our study. In addition, the use of 2 different validated self-reported questionnaires for comparison was a clear advantage.
Conclusions
Our study confirmed a significant association between depression and CRS, as well as decrease in depression risk scores after CRS management. Therefore, it is highly important to consider depression when managing patients with CRS in otolaryngology practice to improve patient well-being and quality of life.
Footnotes
Author Contributions: H.S.A.: Literature review, data collection and manscritp writing. N.A.: Literature review and revising manscript. H. A.: Data collection and statastics analysis. G.A.: Supervisor.
Availability of Data and Materials: Information regarding the data supporting the results or analyses presented in the article can be reviewed and shared with the journal review committee if needed. However, the authors do not wish share it publicly owing to their confidential nature.
Ethics Approval and Consent to Participate: This study was performed in accordance with the ethical standards of the institutional and/or national research committee and the guidelines of the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. This study was approved by the research and ethics committee at King Faisal Specialist Hospital and Research Center (approval number: 2211154). Informed consent was obtained from all individual participants included in the study.
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Deconde AS, Soler ZM. Chronic rhinosinusitis: epidemiology and burden of disease. Am J Rhinol Allergy. 2016;30:134-139. doi: 10.2500/ajra.2016.30.4297 [DOI] [PubMed] [Google Scholar]
- 2. Schlosser RJ, Gage SE, Kohli P, Soler ZM. Burden of illness: a systematic review of depression in chronic rhinosinusitis. Am J Rhinol Allergy. 2016;30:250-256. doi: 10.2500/ajra.2016.30.4343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Vandelaar LJ, Jiang ZY, Saini A, Yao WC, Luong AU, Citardi MJ. PHQ-9 and SNOT-22: elucidating the prevalence of depression in chronic rhinosinusitis. Otolaryngol Head Neck Surg. 2020;162:142-147. doi: 10.1177/0194599819886852 [DOI] [PubMed] [Google Scholar]
- 4. Somers JM, Goldner EM, Waraich P, Hsu L. Prevalence and incidence studies of anxiety disorders: a systematic review of the literature. Can J Psychiatry. 2006;51:100-113. doi: 10.1177/070674370605100206 [DOI] [PubMed] [Google Scholar]
- 5. Waraich P, Goldner EM, Somers JM, Hsu L. Prevalence and incidence studies of mood disorders: a systematic review of the literature. Can J Psychiatry. 2004;49:124-138. doi: 10.1177/070674370404900208 [DOI] [PubMed] [Google Scholar]
- 6. Chen F, Liu L, Wang Y, Hu K, Ma B, Chi J. Prevalence of depression and anxiety in patients with chronic rhinosinusitis: a systematic review and meta-analysis. Otolaryngol Head Neck Surg. 2023;168:143-153. doi: 10.1177/01945998221082538 [DOI] [PubMed] [Google Scholar]
- 7. Bhattacharyya N, Wasan A. Do anxiety and depression confound symptom reporting and diagnostic accuracy in chronic rhinosinusitis? Ann Otol Rhinol Laryngol. 2008;117:18-23. doi: 10.1177/000348940811700105 [DOI] [PubMed] [Google Scholar]
- 8. Levy JM, Mace JC, Deconde AS, Steele TO, Smith TL. Improvements in psychological dysfunction after endoscopic sinus surgery for patients with chronic rhinosinusitis. Int Forum Allergy Rhinol. 2016;6:906-913. doi: 10.1002/alr.21776 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Schlosser RJ, Hyer JM, Smith TL, et al. Depression-specific outcomes after treatment of chronic rhinosinusitis. JAMA Otolaryngol Head Neck Surg. 2016;142:370-376. doi: 10.1001/jamaoto.2015.3810 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Litvack JR, Mace J, Smith TL. Role of depression in outcomes of endoscopic sinus surgery. Otolaryngol Head Neck Surg. 2011;144:446-451. doi: 10.1177/0194599810391625 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Adams KN, Schuman TA, Ebert CS, You W, Tomoum MO, Senior BA. Self-reported anxiety and depression unchanged after endoscopic sinus surgery for chronic rhinosinusitis. Rhinology. 2018;56:234-240. doi: 10.4193/Rhin17.238 [DOI] [PubMed] [Google Scholar]
- 12. Ranford D, Tornari C, Takhar A, et al. Co-morbid anxiety and depression impacts on the correlation between symptom and radiological severity in patients with chronic rhinosinusitis. Rhinology. 2020;58:568-573. doi: 10.4193/Rhin20.075 [DOI] [PubMed] [Google Scholar]
- 13. Damm M, Quante G, Jungehuelsing M, Stennert E. Impact of functional endoscopic sinus surgery on symptoms and quality of life in chronic rhinosinusitis. Laryngoscope. 2002;112:310-315. doi: 10.1097/00005537-200202000-00020 [DOI] [PubMed] [Google Scholar]
- 14. Alt JA, Mace JC, Smith TL, Soler ZM. Endoscopic sinus surgery improves cognitive dysfunction in patients with chronic rhinosinusitis. Int Forum Allergy Rhinol. 2016;6:1264-1272. doi: 10.1002/alr.21820 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Alhadi AN, Alateeq DA, Al-Sharif E, et al. An Arabic translation, reliability, and validation of Patient Health Questionnaire in a Saudi sample. Ann Gen Psychiatry. 2017;16:32. doi: 10.1186/s12991-017-0155-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Alanazy F, AlDousary SA, Albosaily A, Aldriweesh T, Alsaleh S, Aldrees T. Psychometric Arabic Sino-nasal Outcome Test-22: validation and translation in chronic rhinosinusitis patients. Ann Saudi Med. 2018;38:22-27. doi: 10.5144/0256-4947.2018.22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Asiri M, Alokby G. Validation and cross-cultural adaptation of the Sinonasal Outcome Test (SNOT)-22 for the Arabian patient population. Cureus. 2019;11:e4447. doi: 10.7759/cureus.4447 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Fokkens WJ, Lund VJ, Hopkins C, et al. European position paper on rhinosinusitis and nasal polyps 2020. Rhinology. 2020;58:1-464. doi: 10.4193/Rhin20.401 [DOI] [PubMed] [Google Scholar]
- 19. Toma S, Hopkins C. Stratification of SNOT-22 scores into mild, moderate or severe and relationship with other subjective instruments. Rhinology. 2016;54:129-133. doi: 10.4193/Rhino15.072 [DOI] [PubMed] [Google Scholar]
- 20. Kroenke K, Spitzer RL, Williams JBW. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606-613. doi: 10.1046/j.1525-1497.2001.016009606.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Kim JY, Ko I, Kim MS, Yu MS, Cho BJ, Kim DK. Association of chronic rhinosinusitis with depression and anxiety in a nationwide insurance population. JAMA Otolaryngol Head Neck Surg. 2019;145:313-319. doi: 10.1001/jamaoto.2018.4103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Yoo F, Schlosser RJ, Storck KA, Ganjaei KG, Rowan NR, Soler ZM. Effects of endoscopic sinus surgery on objective and subjective measures of cognitive dysfunction in chronic rhinosinusitis. Int Forum Allergy Rhinol. 2019;9(10):1135-1143. [DOI] [PubMed] [Google Scholar]
- 23. Jafari A, De Lima Xavier L, Bernstein JD, Simonyan K, Bleier BS. Association of sinonasal inflammation with functional brain connectivity. JAMA Otolaryngol Head Neck Surg. 2021;147:534-543. doi: 10.1001/jamaoto.2021.0204 [DOI] [PMC free article] [PubMed] [Google Scholar]