Abstract
Background
Abdominal donor site complications in bilateral pedicled transverse rectus abdominis muscle (TRAM) have been a concern when compared with bilateral deep inferior epigastric perforator (DIEP) flap breast reconstruction. This study aimed to assess the strength, endurance, and motor control in patients undergoing DIEP and TRAM flaps.
Methods
A prospective, cohort study was performed at a single institution including patients who underwent pedicled TRAM and DIEP flap reconstruction after mastectomy from August 2017 to August 2018. Patients underwent pre- and postoperative testing involving rectus abdominis, prone plank, side bridge, and trunk flexor tests. Descriptive analyses and multivariate linear regressions were performed.
Results
The final analysis included a total of 9 patients, 4 of whom underwent TRAM flap reconstruction while 5 underwent DIEP flap reconstruction. The tests were not statistically significant between the TRAM versus DIEP groups, including rectus abdominis mean time decrease (0.25 vs 0.60 sec, P = .51), prone plank time increase (1.38 vs 1.38 sec, P = .51), right side bridge time increase (7.54 sec vs 32.15 sec, P = 1.00), left side bridge time increase (2.14 vs 44.5 sec, P = .37), and trunk flexor time decrease (4.68 vs 1.68 sec, P = .44). Overall complications were similar between the 2 groups.
Conclusions
No significant difference in abdominal donor site morbidity was found when comparing the 2 groups. This article provides a point of conversation with patients when discussing available reconstruction options.
Keywords: DIEP, TRAM, Reconstruction, Abdominal, Function
Introduction
Breast reconstructive surgery has become a fundamental component of the overall treatment for patients diagnosed with breast cancer. Studies have demonstrated increased long-term patient satisfaction with autologous reconstruction when compared with implant-based reconstruction.1,6 With both transverse rectus abdominis muscle (TRAM) and deep inferior epigastric perforator (DIEP) flap procedures, abdominal wall tissues are transposed to the chest wall. The free TRAM flap was first described in 1979 by Holmstrom, followed by pedicled TRAM flap in 1982 by Hartrampf.7,8 The DIEP flap was subsequently described in 1994 by Allen in attempts to reconstruct like with like and potentially decrease hernia and abdominal muscle weakness rates.9
Since then, studies have been conducted to compare the benefits and complications of the 2 techniques; specifically, the abdominal donor site complications commonly attributed to the sacrifice of the rectus abdominis muscle in the TRAM flap. However, the method of evaluation of postoperative abdominal function after breast reconstruction has been inconsistent.
Previous studies have used sit-ups, hernia rates, bulge rates, and self-reported questionnaires to test outcomes, with conflicting outcomes.1,10,13,14 These, however, are deficient methods of measuring abdominal morbidity. The sit-up primarily tests one domain of muscle performance—strength. To better measure the impact on a patient's life, tests of strength, endurance, and motor control should be included in the examination. The rectus abdominis test, also known as a sit-up, has been shown to effectively assess the strength of rectus abdominis as well as all abdominal muscle sites.15 With multiple repetitions, the sit-up can also be used to test endurance.16 The prone plank, side bridge, and trunk flexor tests have been validated to assess core endurance, and they have become standard endurance tests established by McGill.17,21 Finally, the lower abdominal progression test is the current standard test of motor control due to its ability to recruit the core stabilizers.22,23
This study used quantifiable and reproducible measurements of abdominal muscle performance to compare pre- and postoperative abdominal function measurements in patients undergoing TRAM and DIEP flap surgeries. If major differences in the degree of loss of core muscle function were found between patients receiving TRAM and DIEP procedures, then this information could help guide the choice of which procedure is best for individual patients. Also, certain patients with particularly large losses of postsurgical abdominal muscle function could be identified for possible therapeutic interventions for strengthening.
We hypothesized that assessing a patient's core muscle performance via a composite fitness test is a valuable means to measure abdominal morbidity. The main objective of the study was to evaluate core muscle performance in DIEP and TRAM flap patients.
Patients and Methods
This is a prospective, cohort study designed to measure core abdominal muscle strength using simple physical tests. This tool will evaluate the potential loss of core abdominal muscle function in patients who have received abdominally based autologous breast reconstruction.
All female patients over the age of 18 years seeking bilateral DIEP and bilateral pedicled TRAM flap-based reconstruction between August 2017 and August 2018 from 2 of the surgical coinvestigators were considered for study enrollment. Additionally, the included patients were those willing to remain for a longer appointment during the pre- and postsurgical physical testing visits. Excluded from the study were patients who may have any comorbid conditions that would prevent them from carrying out the presurgical physical tests, as determined by the study physicians. The determination of flap choice of DIEP versus TRAM was mainly based on surgeon's technique preference for abdominal-based autologous reconstruction, though patient factors were also considered.
The endpoints assessed in the study were abdominal core strength as evaluated by the rectus abdominus test; endurance as evaluated by the prone plank, side bridge, and trunk flexor tests; and finally the lower abdominal progression test, which was used to evaluate abdominal core motor control. Tests were conducted in clinic prior to surgery for the baseline test and follow-up was conducted on postoperative visits. The study methods and design were approved by the Institutional Review Boards.
In the rectus abdominis test, the patients started in a supine position with their legs extended (Figure 1A). The patient performed trunk flexion with their arms crossed in front of them. A 5/5 was given when they were able to come up to sitting from supine with their arms behind their head. If they could sit up completely, they were scored 4/5. If they were only able to clear their shoulder blades, they were scored 3/5. If they could not lift their trunk, the arm position was modified to decrease difficulty for a grade of 2/5. If they could not raise their trunk at all, they received a grade of 1 (palpable muscle contraction) or 0 (no palpable muscle contraction). The resultant grade (0 to 5) was assigned for the test level at which the subject was last able to successfully compete the testing motion.
Figure 1.
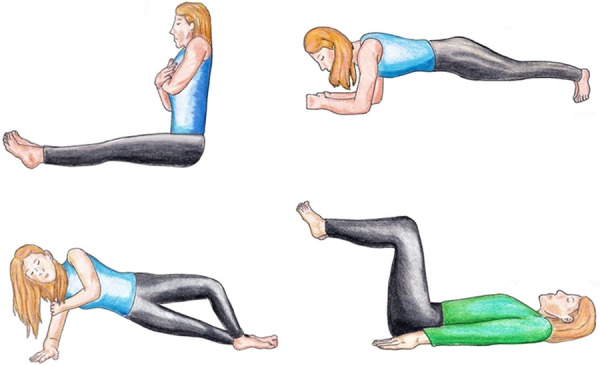
(A, top left) Rectus abdominis tests, (B, top right) prone plank, (C, bottom left) side bridge, and (D, bottom right) lower abdominal progression test.
For the prone plank test, the patient was positioned in prone and propped on their forearms (Figure 1B). The forearms were spaced shoulder-width apart. The feet were maintained close together, though not touching. The patient then raised their pelvis off the floor so that only the forearms and toes were in contact with the floor. The patient held this position, with shoulders, hips, and ankles in a straight line, until fatigue or pain prevented preservation of the position. Time was recorded in seconds.
In the side bridge tests, the patient laid on a mat on their side with legs extended (Figure 1C). The top foot was placed on the ground in front of the lower foot. Using 1 forearm for support, the patient then rose off the ground and maintained a straight line with their full body. The other arm was folded across the chest with the hand gripping the contralateral shoulder. This position was maintained until fatigue or pain prevented preservation of the position. The patient then repeated the test on the contralateral side. Time was recorded in seconds.
For the trunk flexor test, the patient sat on a test bench with the upper body inclined 60 degrees against a support with the hips and knees flexed 90 degrees. The patient was asked to maintain their position while the support is removed. The test was timed until the patient was no longer able to maintain the position. Finally, in the lower abdominal muscle progression test, the patient started in a position of supine hook—lying with the knees bent to 90 degrees (Figure 1D). During each test position, the patient contracted their abdominal muscles by pulling the navel toward the spine. The patient then performed the lower extremity movement as indicated for each of the levels of the test, alternating each leg, then both legs until they were unable to maintain a stable pelvis. The resultant modified grade of (0-5) was assigned for the test position at which the subject was last able to maintain a stable pelvic position as determined by the evaluator. Successful completion of each level and subsequent grading was determined by monitoring movement of the anterior superior iliac spine as a measure of pelvic stability. Finally, the revision procedures and complications were compared.
Descriptive analyses were utilized for demographic characteristics, the abdominal test scores, and complications. Two-sample t test, Fisher exact test, and Mann-Whitney U test were also performed to evaluate patient characteristics and study results. Logistic regression was utilized to determine the odds ratio of complications, controlling for age, body mass index (BMI; both preoperatively and postoperatively), and time for testing. The difference was determined to be significant if P ≤ .05.
Results
A total of 14 patients undergoing autologous breast reconstruction via TRAM or DIEP agreed to participate in the study. Two of the participants underwent baseline testing but ultimately underwent latissimus dorsi flap with expander reconstruction. They did not undergo follow-up testing and their data were excluded from the analysis. Additionally, 3 of the patients were excluded as they only underwent unilateral reconstruction. The final analysis included a total of 9 patients. A total of 4 patients underwent TRAM flap reconstruction and 5 underwent DIEP flap reconstruction.
There were no significant differences in the baseline demographics between the patients undergoing TRAM and DIEP flap reconstruction (Table 1). The mean age in DIEP flap group was 51 ± 4 years and 58 ± 7 years in TRAM flap group. The mean preoperative BMI was 32.10 ± 4.55 kg/m2 in DIEP flap group and 31.22 ± 2.57 kg/m2 in TRAM flap group. There was no significant difference in the test scores between DIEP and TRAM reconstruction (Table 2).
Table 1.
Baseline Characteristics
| Variable | Overall | DIEP | TRAM | P value |
|---|---|---|---|---|
| Age | 54 ± 7 | 51 ± 4 | 58 ± 7 | .08 |
| BMI (preop) | 31.71 ± 3.61 | 32.10 ± 4.55 | 31.22 ± 2.57 | .74 |
| BMI (postop) | 30.88 ± 4.20 | 30.79 ± 5.39 | 31.00 ± 2.88 | .95 |
| Testing postop (days) | 268.67 ± 200.85 | 270.60 ± 258.50 | 266.25 ± 135.91 | .98 |
Table 2.
Testing Comparing DIEP and TRAM
| Variable | Overall | DIEP | TRAM | P value |
|---|---|---|---|---|
| Baseline tests | ||||
| Rectus abdominis | 1.00 | |||
| 1 | 0 (0.00) | 0 (0.00) | 0 (0.00) | |
| 2 | 0 (0.00) | 0 (0.00) | 0 (0.00) | |
| 3 | 6 (66.67) | 3 (60.00) | 3 (75.00) | |
| 4 | 2 (22.22) | 1 (20.00) | 1 (25.00) | |
| 5 | 1 (11.11) | 1 (20.00) | 0 (0.00) | |
| Prone plank, s | 15.45 ± 930 | 13.00 ± 9.25 | 18.52 ± 9.71 | .41 |
| Right side bridge, s median [IQR] | 5.80 [9.13] | 9.13 [2.00] | 2.7 [5.6] | .06 |
| Left side bridge, s median [IQR] | 7.00 [10.60] | 8.00 [10.00] | 3.23 [8.53] | .14 |
| Trunk flexor, s | 18.00 ± 7.50 | 18.56 ± 9.06 | 17.31 ± 6.29 | .82 |
| Lower abdominal progression | – | |||
| 1 | ||||
| 2 | 0 (0.00) | 0 (0.00) | 0 (0.00) | |
| 3 | 0 (0.00) | 0 (0.00) | 0 (0.00) | |
| 4 | 0 (0.00) | 0 (0.00) | 0 (0.00) | |
| 5 | 0 (0.00) | 0(0.00) | 0 (0.00) | |
| 8 (100.00) | 4 (100.00) | 4 (100.00) | ||
| Postoperative tests | ||||
| Rectus abdominis | – | |||
| 1 | 0 (0.00) | 0 (0.00) | 0 (0.00) | |
| 2 | 0 (0.00) | 0 (0.00) | 0 (0.00) | |
| 3 | 9 (100.00) | 5 (100.00) | 4 (100.00) | |
| 4 | 0 (0.00) | 0 (0.00) | 0 (0.00) | |
| 5 | 0 (0.00) | 0 (0.00) | 0 (0.00) | |
| Prone plank, s | 16.83 ± 10.81 | 14.38 ± 12.07 | 19.90 ± 9.73 | .48 |
| Right side bridge, s | 11.42 ± 7.17 | 12.28 ± 8.19 | 10.34 ± 6.70 | .71 |
| Left side bridge, s | 9.30 ± 8.27 | 11.63 ± 10.30 | 6.40 ± 4.56 | .38 |
| Trunk flexor, s | 16.85 ± 10.67 | 20.23 ± 10.80 | 12.63 ± 10.26 | .32 |
| Lower abdominal progression | – | |||
| 1 | ||||
| 2 | 0 (0.00) | 0 (0.00) | 0 (0.00) | |
| 3 | 0 (0.00) | 0 (0.00) | 0 (0.00) | |
| 4 | 0 (0.00) | 0 (0.00) | 0 (0.00) | |
| 5 | 0 (0.00) | 0 (0.00) | 0 (0.00) | |
| 9 (100.00) | 5 (100.00) | 4 (100.00) | ||
| Complications | 1 (11.11) | 1 (20) | 0 (0.00) | 1.00 |
IQR, interquartile range
There was also no significant difference in complications with 20% of patients in DIEP flap group with donor site wounds requiring surgery and 0% in TRAM flap group (P = 1.00) (Table 2). Relative to TRAM flaps, DIEP flaps were not associated with higher odds of having more complications, holding all other variables constant (adjusted P = .97) (Table 3). Tables 4 and 5 list the preoperative and postoperative scores in the various tests in each DIEP and TRAM group.
Table 3.
Logistic Regression
| Variable | Unadjusted parameter estimate (SE) | Unadjusted P value | Adjusted parameter estimate (SE) | Adjusted P value |
|---|---|---|---|---|
| Complications | 23.70 (208.00) | .91 | 11.22 (273.40) | .97 |
SE – standard error
Table 4.
Comparison of Pre- vs Postoperative for DIEP Reconstruction
| Variable | Preoperative | Postoperative | P value |
|---|---|---|---|
| Rectus abdominis | .44 | ||
| 1 | 0(0.00) | 0(0.00) | |
| 2 | 0(0.00) | 0(0.00) | |
| 3 | 3(60.00) | 5(100.00) | |
| 4 | 1(20.00) | 0(0.00) | |
| 5 | 1(20.00) | 0(0.00) | |
| Prone plank, s | 13.00 ± 9.25 | 14.38 ± 12. 07 | .84 |
| Right side bridge, s median [IQR] | 9.13 [2.00] | 13.28 [1.58] | .23 |
| Left side bridge, s median [IQR] | 8.00 [10.00] | 8.15 [14.60] | .53 |
| Trunk flexor, s | 18.56 ± 9.06 | 20.23 ± 10.80 | .80 |
| Lower abdominal progression | – | ||
| 1 | |||
| 2 | 0(0.00) | 0(0.00) | |
| 3 | 0(0.00) | 0(0.00) | |
| 4 | 0(0.00) | 0(0.00) | |
| 5 | 0(0.00) | 0(0.00) | |
| 4(100.00) | 5(100.00) |
Table 5.
Comparison Pre- vs Postoperative for TRAM Reconstruction
| Variable | Preoperative | Postoperative | P value |
|---|---|---|---|
| Rectus abdominis | 1.00 | ||
| 1 | 0(0.00) | 0(0.00) | |
| 2 | 0(0.00) | 0(0.00) | |
| 3 | 3(75.00) | 4(100.00) | |
| 4 | 1(25.00) | 0(0.00) | |
| 5 | 0(0.00) | 0(0.00) | |
| Prone plank, s | 18.52 ± 9.71 | 19.90 ± 9.73 | .85 |
| Right side bridge, s median [IQR] | 2.70 [5.60] | 9.14 [11.11] | .14 |
| Left side bridge, s median [IQR] | 3.23 [8.53] | 7.41 [5.70] | .24 |
| Trunk flexor, s | 17.31 ± 6.29 | 12.63 ± 1030 | .47 |
| Lower abdominal progression | – | ||
| 1 | 0(0.00) | 0(0.00) | |
| 2 | 0(0.00) | 0(0.00) | |
| 3 | 0(0.00) | 0(0.00) | |
| 4 | 0(0.00) | 0(0.00) | |
| 5 | 4(100.00) | 4(100.00) |
DIEP flap rectus abdominis mean time decreased 0.60 seconds (P = .51), the prone plank test mean time increased by 1.38 seconds post-procedure (P = 1.00), side bridge test on right side decreased 32.15 seconds (P = .32), side bridge test on left side decreased 44.57 seconds (P = .37), trunk flexor test increased by 1.67 seconds (P = .44), and there was no change in the lower abdominal progression test (all patients scored a 5 before and after surgery) (Table 6).
Table 6.
Comparison of Pre- and Postoperative Differences in Tests Between DIEP and TRAM
| Variable | DIEP | TRAM | P value |
|---|---|---|---|
| Difference in rectus abdominis | -0.60 ± 0.89 | -0.25 ± 0.50 | .51 |
| Difference in prone plank, s | 1.38 ± 13.61 | 1.38 ± 16.55 | 1.00 |
| Difference in right side bridge, s | -32.15 ± 78.21 | 7.54 ± 6.95 | .32 |
| Difference in left side bridge, s | -44.57 ± 103.16 | 2.14 ± 4.45 | .37 |
| Difference in trunk flexor, s | 1.67 ± 12.80 | -4.68 ± 9.74 | .44 |
| Difference in lower abdominal progression | 0.00 ± 0.00 | 0.00 ± 0.00 | – |
Difference = postoperative – preoperative score
With TRAM flap, the rectus abdominis mean time decreased 0.25 seconds from baseline (P = .51), prone plank mean increased by 1.38 seconds (P = 1.00), side bridge test on right side increased 7.54 seconds (P = .32), side bridge test on left side increased 2.14 seconds (P = .37), and finally, in the trunk flexor test, there was a decrease of 4.68 seconds (P = .44) (Table 6). Similarly, there was no difference in the before and after testing of the lower abdominal progression test as all patients scored a 5, before and after surgery.
Discussion
While the DIEP flap was described and is now becoming increasingly popular in breast reconstruction to reduce the rectus abdominis harvest, it has been questioned whether the anatomical deficit would create functional deficits. In our study, we attempted to evaluate not only the strength but endurance and motor control to assess how the other core stabilizers can compensate for the rectus abdominis loss. We did not find a significant deficit in either TRAM or DIEP flap groups, even with full incorporation of the muscle in the TRAM flap group.
On the contrary, Dulin et al demonstrated significantly decreased abdominal strength after bilateral pedicled TRAM surgery, and although there was shown to be a decrease in trunk flexion, which is one of the components we studied, they found that the only activity which was significantly negatively influenced was getting out of bed.24 This brings up an important point of the function of rectus abdominis being trunk flexion and the potentially limited effect this has on day-to-day activities in most patients. The effect of stabilization on the core and spine should also be considered given the importance of stability in daily function and injury prevention, and its effect on low back pain. Hodges et al consistently showed the importance of recruitment of transversus abdominus first, followed by the multifidus, obliques, and rectus abdominus.25,26 Given that multiple muscle recruitment is important in stabilization, it would bring up the question of whether abdominal exercise prior to surgery can prevent donor site complications. One study explored this but found that at 1 year, there was no difference in patients undergoing DIEP flap reconstruction who performed exercise prior to surgery compared with control subjects.27 This finding is limited in that the study did not explore the effect in patients undergoing TRAM flap reconstruction.
In line with the effect on patient's daily life, studies using questionnaires evaluating patients' perspective of loss of physical abdominal function were assessed. Two such studies demonstrated that there was no patient-perceived effect on physical abdominal function in patients undergoing muscle-sparing TRAM flap surgeries when compared with DIEP flap surgeries.12,28 However, this finding was not consistent, as another study showed that patients reported a decrease in abdominal physical well-being in pedicled TRAM flap patients when compared with DIEP flaps. However, this was not seen with DIEP versus muscle-sparing TRAM flap surgery. The same study also showed increased partial flap loss, fat necrosis, and hernia/bulge in pedicled TRAM flaps.29
All TRAM flaps in our study were reconstructed using onlay synthetic mesh. The use of mesh for reconstruction TRAM donor sites has been shown to be effective in reducing hernia and bulge rates. Furthermore, it has shown to be cost-effective when compared with primary closure given its clinical effectiveness.30,32
Another important consideration is the potential utility of muscle-sparing TRAM. Bassiouny et al compared free muscle-sparing TRAM with pedicled TRAM, finding increased hospital stay and blood loss in the muscle-sparing TRAM groups but similar operative time and abdominal morbidity when compared with pedicled TRAM. Abdominal muscle strength was initially decreased in the pedicled TRAM group, but it resolved in 3 months.33 Serletti et al found similar complications, outcomes, fitness, and abdominal strength in free TRAM flap group compared with pedicled TRAM group, with the only difference being increased cost of the free TRAM.34
The potential of muscle denervation during perforator dissection in DIEP flap harvest has also raised concerns. Occasionally, a small portion of the muscle also needs to be harvested when the perforator runs transversely. Previous studies have shown decreased abdominal muscle function with dissection of DIEP flap, with 1 prospective study demonstrating a functional decrease in 17.1% of patients with high BMI and hypertension, increasing the odds of decreased function.35 Two of the patients undergoing DIEP flap reconstruction in our study did require a small portion of muscle to be incorporated in the flap, but there was no significant difference in abdominal function in the DIEP flap groups despite the muscle harvest and 2 cases of deeper dissection.
It has been theorized that medial perforator harvest in DIEP flaps could potentially preserve the innervation since only the segmental intercostal nerves would potentially be dissected around the lateral branch perforators during harvest.36,37 Garvey et al explored this and found that there was no difference in abdominal morbidity as it relates to bulge or hernia formation when medial versus lateral row perforators were harvested, nor the number of perforators. Furthermore, there was no difference in abdominal wall morbidity when comparing muscle-sparing TRAM and DIEP flaps. The only significant factor in developing abdominal wall morbidity complications in that study was that of previous abdominal surgery.15 Contrary to that study, 2 other studies found harvesting medial perforators reduced the chance of abdominal bulge/hernia.38,39 Abdominal function as it relates to strength/endurance/motor control was not evaluated in these studies.
Lastly, although statistically insignificant, it is notable that there was an improved performance with bilateral bridge tests in TRAM groups and in prone plank and trunk flexor tests in DIEP groups when compared with baseline. Although the reason is unclear, it could possibly be attributed to familiarity with exercises during follow-up testing.
Limitations
A limitation of this study is that it is underpowered with a small sample size. This is a pilot study that will require a sample size of 100 for a power at 80% and alpha at 0.05. Secondly, although we attempted to objectively grade and time the exercises, the person administering the test could act as a confounder. The person analyzing also was not blinded, which could skew the way the tests were administered or timed. Similarly, the error in testing could potentially act as a confounding factor, as evidenced by high scoring in the lower abdominal progression test. Furthermore, the fact that the patients were familiar with the exercises during the postoperative analysis could explain why there was no significant reduction in function, as well as why there was a small, although insignificant, increase in abdominal function in some patients. As this study compared DIEP with pedicled TRAM performed by 2 different surgeons, future studies could look at comparing free TRAM with DIEP flaps performed by 1 surgeon to minimize potential confounders.
Conclusions
This study found that there was not a significant difference between DIEP and TRAM flap reconstruction on abdominal donor site morbidity. Therefore, determining which type of reconstruction to offer to patients can be dependent on the surgeon's level of comfort with the type of technique and reconstruction as well as the discussion of the benefits and complications of each procedure with patients. Presenting the current data to patients regarding the abdominal morbidity and its effect on patients can aid in counseling and preoperative planning.
Acknowledgments
Ethics: The study methods and design were approved by the Institutional Review Boards.
Disclosures: The authors disclose no relevant financial or nonfinancial interests.
References
- 1.Nelson JA, Allen RJ Jr., Polanco T, et al. Long-term patient-reported outcomes following postmastectomy breast reconstruction: an 8-year examination of 3268 patients. Ann Surg. Sep 2019;270(3):473-483. doi:10.1097/sla.0000000000003467 10.1097/SLA.0000000000003467 [DOI] [PubMed] [Google Scholar]
- 2.Hu ES, Pusic AL, Waljee JF, et al. Patient-reported aesthetic satisfaction with breast reconstruction during the long-term survivorship period. Plast Reconstr Surg. Jul 2009;124(1):1-8. doi:10.1097/PRS.0b013e3181ab10b2 10.1097/PRS.0b013e3181ab10b2 [DOI] [PubMed] [Google Scholar]
- 3.Santosa KB, Qi J, Kim HM, Hamill JB, Wilkins EG, Pusic AL. Long-term patient-reported outcomes in postmastectomy breast reconstruction. JAMA Surg. Oct 1 2018;153(10):891-899. doi:10.1001/jamasurg.2018.1677 10.1001/jamasurg.2018.1677 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ménez T, Michot A, Tamburino S, Weigert R, Pinsolle V. Multicenter evaluation of quality of life and patient satisfaction after breast reconstruction, a long-term retrospective study. Ann Chir Plast Esthet. 2018;63(2):126-133. doi:10.1016/j.anplas.2017.07.022 [DOI] [PubMed] [Google Scholar]
- 5.Christensen BO, Overgaard J, Kettner LO, Damsgaard TE. Long-term evaluation of postmastectomy breast reconstruction. Acta Oncol. Oct 2011;50(7):1053-1061. doi:10.3109/0284186x.2011.584554 10.3109/0284186X.2011.584554 [DOI] [PubMed] [Google Scholar]
- 6.Craft RO, Colakoglu S, Curtis MS, et al. Patient satisfaction in unilateral and bilateral breast reconstruction [outcomes article]. Plast Reconstr Surg. Apr 2011;127(4):1417-1424. doi:10.1097/PRS.0b013e318208d12a 10.1097/PRS.0b013e318208d12a [DOI] [PubMed] [Google Scholar]
- 7.Holmstrom H. The free abdominoplasty flap and its use in breast reconstruction. An experimental study and clinical case report. Scand J Plast Reconstr Surg. 1979;13(3):423-427. doi:10.3109/02844317909013092 [DOI] [PubMed] [Google Scholar]
- 8.Hartrampf CR, Scheflan M, Black PW. Breast reconstruction with a transverse abdominal island flap. Plast Reconstr Surg. Feb 1982;69(2):216-225. doi:10.1097/00006534-198202000-00006 10.1097/00006534-198202000-00006 [DOI] [PubMed] [Google Scholar]
- 9.Allen RJ, Treece P. Deep inferior epigastric perforator flap for breast reconstruction. Ann Plast Surg. Jan 1994;32(1):32-38. doi:10.1097/00000637-199401000-00007 10.1097/00000637-199401000-00007 [DOI] [PubMed] [Google Scholar]
- 10.Chun YS, Sinha I, Turko A, Lipsitz S, Pribaz JJ. Outcomes and patient satisfaction following breast reconstruction with bilateral pedicled TRAM flaps in 105 consecutive patients. Plast Reconstr Surg. Jan 2010;125(1):1-9. doi:10.1097/PRS.0b013e3181c2a620 10.1097/PRS.0b013e3181c2a620 [DOI] [PubMed] [Google Scholar]
- 11.Wu LC, Bajaj A, Chang DW, Chevray PM. Comparison of donor-site morbidity of SIEA, DIEP, and muscle-sparing TRAM flaps for breast reconstruction. Plast Reconstr Surg. Sep 2008;122(3):702-709. doi:10.1097/PRS.0b013e3181823c15 10.1097/PRS.0b013e3181823c15 [DOI] [PubMed] [Google Scholar]
- 12.Bajaj AK, Chevray PM, Chang DW. Comparison of donor-site complications and functional outcomes in free muscle-sparing TRAM flap and free DIEP flap breast reconstruction. Plast Reconstr Surg. Mar 2006;117(3):737-746; discussion 747-750. doi:10.1097/01.prs.0000200062.97265.fb 10.1097/01.prs.0000200062.97265.fb [DOI] [PubMed] [Google Scholar]
- 13.Chang EI, Chang EI, Soto-Miranda MA, et al. Comprehensive analysis of donor-site morbidity in abdominally based free flap breast reconstruction. Plast Reconstr Surg. Dec 2013;132(6):1383-1391. doi:10.1097/PRS.0b013e3182a805a3 10.1097/PRS.0b013e3182a805a3 [DOI] [PubMed] [Google Scholar]
- 14.Ireton JE, Kluft JA, Ascherman JA. Unilateral and bilateral breast reconstruction with pedicled TRAM flaps: an outcomes analysis of 188 consecutive patients. Plast Reconstr Surg Glob Open. May 2013;1(2):1-7. doi:10.1097/GOX.0b013e3182944595 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Garvey PB, Salavati S, Feng L, Butler CE. Abdominal donor-site outcomes for medial versus lateral deep inferior epigastric artery branch perforator harvest. Plast Reconstr Surg. Jun 2011;127(6):2198-2205. doi:10.1097/PRS.0b013e3182131caf 10.1097/PRS.0b013e3182131caf [DOI] [PubMed] [Google Scholar]
- 16.Parfrey KC DD, Workman RC, Behm DG. The effects of different sit- and curl-up positions on activation of abdominal and hip flexor musculature. Appl Physiol Nutr Metab. 2008;33(5):888-895. 10.1139/H08-061 [DOI] [PubMed] [Google Scholar]
- 17.Atsushi I, Kaneoka K. The relationship between trunk endurance plank tests and athletic performance tests in adolescent soccer players. Int J Sports Phys Ther. 2016;11(5):718-724. [PMC free article] [PubMed] [Google Scholar]
- 18.Allen BA HJ, Burns RD, Williams SM. Effect of a core conditioning intervention on tests of trunk muscular endurance in school-aged children. J Strength Cond Res. 2014;28(7):2063-2070. 10.1519/JSC.0000000000000352 [DOI] [PubMed] [Google Scholar]
- 19.Swain R. Trunk muscle endurance and low back pain in female dance students. J Dance Med Sci. 2014;18(2):62-66. 10.12678/1089-313X.18.2.62 [DOI] [PubMed] [Google Scholar]
- 20.Lacote M, Miranda A, Bleton JP, Stevenin S. Clinical evaluation of muscle function. Churchill Livingstone; 1987:278-279. [Google Scholar]
- 21.McGill SM, Childs A, Liebenson C. Endurance times for low back stabilization exercises: clinical targets for testing and training from a normal database. Arch Phys Med Rehabil. Aug 1999;80(8):941-944. 10.1016/S0003-9993(99)90087-4 [DOI] [PubMed] [Google Scholar]
- 22.Dekart KQ. Test-re-test reliability of Sahrmann Lower Abdominal Core Stability Test for DII baseball athletes. ProQuest Dissertations Publishing. 2014. [Google Scholar]
- 23.Haladay DE, Denegar CR, Miller SJ, Challis J. Electromyographic and kinetic analysis of two abdominal muscle performance tests. Physiother Theory Pract. 2015;31(8):587-593. doi:10.3109/09593985.2015.1062945 10.3109/09593985.2015.1062945 [DOI] [PubMed] [Google Scholar]
- 24.Dulin WA, Avila RA, Verheyden CN, Grossman L. Evaluation of abdominal wall strength after TRAM flap surgery. Plas Reconstr Surg. May 2004;113(6):1662-1665; discussion 1666-1667. doi:10.1097/01.prs.0000117197.77201.14 10.1097/01.PRS.0000117197.77201.14 [DOI] [PubMed] [Google Scholar]
- 25.Hodges PW, Richardson CA. Inefficient muscular stabilization of the lumbar spine associated with low back pain. A motor control evaluation of transversus abdominis. Spine (Phila Pa 1976). Nov 15 1996;21(22):2640-2650. doi:10.1097/00007632-199611150-00014 10.1097/00007632-199611150-00014 [DOI] [PubMed] [Google Scholar]
- 26.Hodges PW, Richardson CA. Delayed postural contraction of transversus abdominis in low back pain associated with movement of the lower limb. J Spinal Disord. Feb 1998;11(1):46-56. 10.1097/00002517-199802000-00008 [DOI] [PubMed] [Google Scholar]
- 27.Futter CM, Weiler-Mithoff E, Hagen S, et al. Do pre-operative abdominal exercises prevent post-operative donor site complications for women undergoing DIEP flap breast reconstruction? A two-centre, prospective randomised controlled trial. Br J Plast Surg. Feb 2003;56(7):674-683. doi:10.1016/s0007-1226(03)00362-x 10.1016/S0007-1226(03)00362-X [DOI] [PubMed] [Google Scholar]
- 28.Nahabedian MY, Tsangaris T, Momen B. Breast reconstruction with the DIEP flap or the muscle-sparing (MS-2) free TRAM flap: is there a difference? Plast Reconstr Surg. Feb 2005;115(2):436-444; discussion 445-446. doi:10.1097/01.prs.0000149404.57087.8e 10.1097/01.PRS.0000149404.57087.8E [DOI] [PubMed] [Google Scholar]
- 29.Macadam SA, Zhong T, Weichman K, et al. Quality of life and patient-reported outcomes in breast cancer survivors: a multicenter comparison of four abdominally based autologous reconstruction methods. Plast Reconstr Surg. Feb 2016;137(3):758-771. doi:10.1097/01.prs.0000479932.11170.8f 10.1097/01.prs.0000479932.11170.8f [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cyriac C, Sharma RK, Singh G. Assessment of the abdominal wall function after pedicled TRAM flap surgery for breast reconstruction: Use of modified mesh repair for the donor defect. Indian J Plast Surg. Feb 2010;43(2):166-172. doi:10.4103/0970-0358.73430 10.1055/s-0039-1699430 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Moscona RA, Ramon Y, Toledano H, Barzilay G. Use of synthetic mesh for the entire abdominal wall after TRAM flap transfer. Plast Reconstr Surg. Feb 1998;101(3):706-710; discussion 711-712. doi:10.1097/00006534-199803000-00018 10.1097/00006534-199803000-00018 [DOI] [PubMed] [Google Scholar]
- 32.Chatterjee A, Ramkumar DB, Dawli TB, Nigriny JF, Stotland MA, Ridgway EB. The use of mesh versus primary fascial closure of the abdominal donor site when using a transverse rectus abdominis myocutaneous flap for breast reconstruction: a cost-utility analysis. Plast Reconstr Surg. Feb 2015;135(3):682-689. doi:10.1097/prs.0000000000000957 10.1097/PRS.0000000000000957 [DOI] [PubMed] [Google Scholar]
- 33.Bassiouny MM, Maamoun SI, El-Shazly Sel D, Youssef OZ. TRAM flap for immediate post mastectomy reconstruction: comparison between pedicled and free transfer. J Egypt Natl Canc Inst. Feb 2005;17(4):231-238. [PubMed] [Google Scholar]
- 34.Serletti JM, Moran SL. Free versus the pedicled TRAM flap: a cost comparison and outcome analysis. Plast Reconstr Surg. Feb 1997;100(6):1418-1424; discussion 1425-1427. doi:10.1097/00006534-199711000-00006 10.1097/00006534-199711000-00006 [DOI] [PubMed] [Google Scholar]
- 35.Lee KT, Park JW, Mun GH. Impact of rectus muscle injury during perforator dissection on functional donor morbidity after deep inferior epigastric perforator flap breast reconstruction. Plast Reconstr Surg Glob Open. Feb 2019;7(10):e2484. doi:10.1097/gox.0000000000002484 10.1097/GOX.0000000000002484 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rozen WM, Ashton MW, Murray AC, Taylor GI. Avoiding denervation of rectus abdominis in DIEP flap harvest: the importance of medial row perforators. Plast Reconstr Surg. Feb 2008;122(3):710-716. doi:10.1097/PRS.0b013e318180ed8b 10.1097/PRS.0b013e318180ed8b [DOI] [PubMed] [Google Scholar]
- 37.Rozen WM, Tran TM, Barrington MJ, Ashton MW. Avoiding denervation of the rectus abdominis muscle in DIEP flap harvest III: a functional study of the nerves to the rectus using anesthetic blockade. Plast Reconstr Surg. Feb 2009;124(2):519-522. doi:10.1097/PRS.0b013e3181addbee 10.1097/PRS.0b013e3181addbee [DOI] [PubMed] [Google Scholar]
- 38.Butler DP, Plonczak AM, Reissis D, et al. Factors that predict deep inferior epigastric perforator flap donor site hernia and bulge. J Plast Surg Hand Surg. Feb 2018;52(6):338-342. doi:10.1080/2000656x.2018.1498790 10.1080/2000656X.2018.1498790 [DOI] [PubMed] [Google Scholar]
- 39.Hembd A, Teotia SS, Zhu H, Haddock NT. Optimizing perforator selection: a multivariable analysis of predictors for fat necrosis and abdominal morbidity in DIEP flap breast reconstruction. Plast Reconstr Surg. Feb 2018;142(3):583-592. doi:10.1097/prs.0000000000004631 10.1097/PRS.0000000000004631 [DOI] [PubMed] [Google Scholar]


