ABSTRACT
Background: Symptom accommodation by family members (FMs) of individuals with posttraumatic stress disorder (PTSD) includes FMs’ participation in patients’ avoidance/safety behaviours and constraining self-expression to minimise conflict, potentially maintaining patients’ symptoms. The Significant Others’ Responses to Trauma Scale (SORTS) is the only existing measure of accommodation in PTSD but has not been rigorously psychometrically tested.
Objective: We aimed to conduct further psychometric analyses to determine the factor structure and overall performance of the SORTS. Method: We conducted exploratory and confirmatory factor analyses using a sample of N = 715 FMs (85.7% female, 62.1% White, 86.7% romantic partners of individuals with elevated PTSD symptoms).
Results: After dropping cross-loading items, results indicated good fit for a higher-order model of accommodation with two factors: an anger-related accommodation factor encompassed items related largely to minimising conflict, and an anxiety-related accommodation factor encompassed items related primarily to changes to the FM’s activities. Accommodation was positively related to PTSD severity and negatively related to relationship satisfaction, although the factors showed somewhat distinct associations. Item Response Theory analyses indicated that the scale provided good information and robust coverage of different accommodation levels.
Conclusions: SORTS data should be analysed as both a single score as well as two factors to explore the factors’ potential differential performance across treatment and relationship outcomes.
KEYWORDS: PTSD, accommodation, anger, partner, couple
HIGHLIGHTS
We examined the Significant Others’ Responses to Trauma Scale (SORTS), a measure of symptom accommodation in PTSD, among a large sample of family members.
As measured by the SORTS, accommodation in PTSD could be broken down into two aspects: anger-related accommodation and anxiety-related accommodation.
Accommodation was positively related to PTSD severity and negatively related to relationship satisfaction.
Abstract
Antecedentes: La acomodación de los síntomas por miembros de la familia (MFs) de las personas con trastorno de estrés postraumático (TEPT) incluye a la participación de los MFs en las conductas de evitación/seguridad y la contención de las propias expresiones para minimizar el conflicto, lo que potencialmente promueve la continuidad de los síntomas del paciente. La escala para la respuesta de las personas significativas (SORTS por sus siglas en inglés) es la única escala desarrollada para medir la acomodación de los síntomas en el TEPT, pero no ha sido evaluada psicométricamente de forma rigurosa.
Objetivo: Conducir análisis psicométricos adicionales para determinar la estructura factorial y el desempeño general de la SORTS.
Métodos: Se realizó un análisis factorial exploratorio y confirmatorio a partir de una muestra de n = 715 MFs (85,7 % mujeres, 62,1 % de raza blanca, 86,7 % parejas románticas de personas con elevados síntomas del TEPT).
Resultados: Luego de retirar ítems con cargas cruzadas, los resultados indicaron un adecuado ajuste para un modelo de acomodación de orden alto con dos factores: un factor de acomodación asociado con la ira que incluía ítems ampliamente relacionados a la minimización de conflicto y un factor de acomodación asociado a la ansiedad que incluía ítems asociados principalmente en cambios en las actividades de los MFs. La acomodación estaba asociada de forma directa a la severidad de los síntomas del TEPT y de forma inversa a la satisfacción con la relación; no obstante, los factores mostraron algunas asociaciones distintas. Los análisis basados en la teoría de respuesta a ítems mostraron que la escala brindaba buena información y una cobertura robusta sobre los diferentes niveles de acomodación.
Conclusión: Los datos de la SORTS deben ser analizados tanto como un puntaje único como en dos puntajes para cada uno de sus factores de forma que se explore el desempeño potencial de cada factor durante el tratamiento y en los resultados en las relaciones interpersonales.
PALABRAS CLAVE: TEPT, acomodación, ira, pareja, pareja sentimental
Symptom accommodation by family members (FMs) or other loved ones1 of individuals with psychopathology includes FM participation in disorder-related avoidance and safety behaviours and constraining one’s self-expression to minimise conflict. Accommodation is associated with greater symptom severity among patients (e.g. Lebowitz et al., 2016; Merlo et al., 2009) and greater psychological distress among FMs (e.g. Amir et al., 2000; Calvocoressi et al., 1995; Thompson-Hollands et al., 2014) across multiple disorders, including posttraumatic stress disorder (PTSD; American Psychiatric Association, 2013). According to the Cognitive–Behavioral Interpersonal Theory of PTSD (Monson et al., 2010), accommodation can contribute to the maintenance of PTSD symptoms, relationship difficulties, and FM psychological distress by reinforcing identified patients’ (IPs’) avoidance and safety behaviours and reducing opportunities for mutually reinforcing shared activities, affective expression, and self-disclosure, including disclosure about the trauma. Indeed, research with romantic dyads has shown that partners’ accommodation of IPs’ PTSD symptoms is associated with higher levels of IP PTSD symptom severity and partner psychological distress over time, as well as with lower levels of IP and partner relationship satisfaction (Campbell et al., 2017; Fredman et al., 2014, 2016, 2022; Howard et al., 2023).
FM accommodation in PTSD may take many forms, mirroring the diversity of PTSD symptoms and presentations (Galatzer-Levy & Bryant, 2013; Reuman & Thompson-Hollands, 2020). FMs may overtly take over certain tasks (e.g. shopping in crowded stores), thereby allowing the IP to avoid trauma-related stimuli. The FM and IP may also engage in dyadic-level avoidance of situations that are challenging for the IP but would be enjoyable for the FM if not for the PTSD (e.g. going to the movies). Finally, the FM may engage in more subtle or internally focused avoidance, such as not mentioning the IP’s trauma or trauma reminders or bringing up certain topics of conversation with the IP that could elicit emotional arousal. This latter type of accommodation may extend to avoiding any type of behaviour or interaction that would provoke conflict with the IP. These accommodative behaviours are understandable in the sense that they can reduce the short-term distress of IPs and FMs (e.g. Fredman et al., 2023; Weber et al., 2019). However, the accommodation may prevent the IP from fully encountering trauma-related stimuli and learning to tolerate and manage distressing feelings.
Fredman et al. (2014) developed the Significant Others’ Responses to Trauma Scale (SORTS) to facilitate the measurement of accommodation by the significant others of individuals with PTSD. The SORTS items were developed based upon measures of accommodation and theoretically related constructs in obsessive compulsive disorder, substance abuse, and mood and anxiety disorders (e.g. Calvocoressi et al., 1995; Fredman et al., 2004, 2008; Rotunda et al., 2004). In consultation with subject matter experts in the National Center for PTSD, Fredman et al. (2014) generated items that could describe FM accommodative responses to the PTSD symptoms listed in the Diagnostic and Statistical Manual of Mental Disorders (4th ed., DSM-IV-TR; American Psychiatric Association, 2000); the items were then reviewed in focus groups of patients with PTSD and their romantic partners. These consultations were an effort to increase the content validity of the scale. However, no underlying factor structure was proposed at the time of item generation. The authors next tested the items in a convenience sample of 46 treatment-seeking dyads (all romantic couples, see Monson et al., 2012). This initial psychometric evaluation of the SORTS represented a unique opportunity to conduct a proof-of-concept study with a clinical sample to determine if accommodation could be validly and reliably assessed in the intimate relationship context of PTSD, given that it was uncommon to involve significant others in PTSD treatment at that time. The results supported the reliability of the SORTS vis-à-vis internal consistency and item-total correlations and construct validity vis- à-vis convergence with measures of patient and partner psychological distress and relationship adjustment; however, the sample size was not sufficient to conduct a more rigorous psychometric evaluation using factor analysis or item response theory.
The SORTS remains the only measure of accommodation in PTSD. It is now widely used in dyadically focused PTSD research and treatment (e.g. Allen et al., 2021; Campbell et al., 2017; Fredman et al., 2021; Pukay-Martin et al., 2022) and was part of the standardised assessment battery used for the US Department of Veterans Affairs’ national dissemination of cognitive–behavioural conjoint therapy for PTSD (Monson & Fredman, 2012). More recently, the SORTS has been used to examine interpersonal predictors of treatment response to individual psychotherapy for PTSD. For example, Howard et al. (2023) demonstrated that, among veterans participating in trauma-focused individual psychotherapy, higher levels of support person accommodation predicted greater PTSD symptom severity approximately 4 months later through reduced homework compliance. However, no dedicated psychometric work beyond the initial validation paper has been conducted. Given the theoretical importance of accommodation as a potential maintaining factor in PTSD but also a modifiable treatment target in couple/conjoint therapies for PTSD (Fredman et al., 2021; Monson et al., 2010; Monson & Fredman, 2012; Pukay-Martin et al., 2015, 2022), a deeper evaluation of the psychometric performance of the SORTS is critically needed. Specifically, it is necessary to conclusively determine: (1) whether accommodation as measured by the SORTS is a unidimensional or multidimensional construct (e.g. frequency of accommodation versus distress about accommodation; or, different types of accommodative behaviours, such as accommodation in response to IP’s anger-related PTSD symptoms versus anxiety-related PTSD symptoms); (2) how well existing SORTS items function as indicators of the underlying construct(s); and (3) whether the existing SORTS items adequately capture a range of accommodation levels.
With regard to the factor structure of the SORTS, most researchers have used a single summed score to quantify overall accommodation (e.g. Fredman et al., 2016; Pukay-Martin et al., 2022; Thompson-Hollands et al., 2021), although some have analysed the frequency subscale and the distress subscale separately (e.g. Fredman et al., 2021; Renshaw et al., 2020). However, neither approach has been empirically validated, and it is possible that a third factor structure is the best fit to the data. Once the factor structure is determined, an assessment of how well each item functions will provide an indicator of the underlying factor(s).
Both the summed total score method of scoring the SORTS and the frequency/distress subscale summed score approach rely on the assumption that all items accurately distinguish between people with higher and lower levels of accommodation. Yet, it may be the case that certain items are more accurate than others. Additionally, different ratings within items (e.g. selecting Never versus Several times a week) or differences between items themselves may correspond to different portions of the underlying accommodation construct. For example, ‘tiptoeing’ around the person with PTSD on a weekly basis could indicate a greater level of accommodation than daily avoidance of trauma reminders, although the latter is rated more highly per the SORTS scoring rubric. Item Response Theory (IRT; Reise et al., 2005) allows for the examination of the probability of a certain response on a measure relative to an individual’s true level of an underlying psychological construct (θ). Item discrimination (a) refers to the extent to which a particular item can differentiate between individuals of different levels of the underlying construct, and item difficulty (b) refers to the level of the underlying construct necessary to endorse the item. The use of IRT to test the performance of the individual SORTS items and response options within items will permit the evaluation of the extent to which certain items better distinguish between respondents who are high versus low in accommodation, as well as the degree to which items/responses adequately cover the continuum of accommodation levels and/or are redundant. Ultimately, both the factor analysis and IRT may identify areas in which SORTS items should be revised or removed or new items generated.
We hypothesised that the SORTS would have a multifactorial structure, although we considered the exact nature of that structure to be exploratory. We further hypothesised that the SORTS factor(s) would demonstrate a medium correlation with IPs’ and FMs’ ratings of the IPs’ PTSD symptom severity across all clusters (e.g. Allen et al., 2021; Campbell et al., 2017), a large correlation with FMs’ relationship satisfaction, and a medium correlation with IPs’ relationship satisfaction (e.g. Fredman et al., 2014, 2022). We considered the IRT analyses to be exploratory, as no such analyses have ever been conducted on the SORTS. Establishing the factor structure of the SORTS, along with demonstrating the relationship of the factor(s) with relevant constructs and the performance of individual items, will enhance the usefulness of the SORTS measure and allow for more nuanced investigation of accommodation as a construct.
1. Method
1.1. Participants
We gathered SORTS data from multiple research investigations and clinical programmes specialising in PTSD. The senior author (SJF) reached out to clinics and research programmes that were known to have administered the SORTS and requested that these programmes share data for the purpose of further scale validation/analysis. All programmes that were approached agreed to provide their data. We requested as many of the following variables as were available from a given setting, although not all settings had collected all variables: FM’s age, gender, race, ethnicity, educational level, relationship to IP, PTSD status, and veteran/military status; IP’s age, gender, race, ethnicity, educational level, PTSD status, PTSD symptom severity, and veteran/military status.
Upon receiving the datasets, we removed 22 participants who had completed the SORTS as part of a ‘dual PTSD dyad’ because of concerns that accommodation by FMs who had a diagnosis of PTSD might be conflated with avoidance driven by the FM’s own symptoms.2 This resulted in a final sample size of N = 715. The overwhelming majority of SORTS respondents in the sample were female romantic partners of a male service member or veteran. Demographic information about the SORTS respondent sample is shown in Table 1.
Table 1.
Demographics of SORTS respondents.
| EFA sample (n = 272) n (%) |
CFA sample (n = 443) n (%) |
Total sample (n = 715) n (%) |
|
|---|---|---|---|
| Mean age (SD) | 30.49 (5.51) | 37.23 (12.20) | 34.10 (10.24) |
| IP is a service member/veteran | |||
| Yes | 272 (100%) | 283 (63.9%) | 555 (77.6%) |
| No | 0 (0%) | 51 (11.5%) | 51 (7.1%) |
| Unknown | 0 (0%) | 109 (24.6%) | 109 (15.2%) |
| FM is a woman | |||
| Yes | 272 (100%) | 341 (77.0%) | 613 (85.7%) |
| No | 0 (0%) | 88 (19.9%) | 88 (12.3%) |
| Unknown | 0 (0%) | 14 (3.2%) | 14 (2.0%) |
| FM is IP’s romantic partner | |||
| Yes | 272 (100%) | 348 (78.6%) | 620 (86.7%) |
| No | 0 (0%) | 90 (20.3%) | 90 (12.6%) |
| Unknown | 0 (0%) | 5 (1.1%) | 4 (0.6%) |
| FM racea | |||
| White | 236 (86.8%) | 208 (47.0%) | 444 (62.1%) |
| Black/African American/African | 14 (5.1%) | 39 (8.8%) | 53 (7.4%) |
| American Indian/Alaskan Native/Indigenous Canadian | 4 (1.5%) | 6 (1.4%) | 10 (1.4%) |
| Asian/Asian American/South Asian/Native Hawaiian/Pacific Islander | 7 (2.6%) | 28 (6.3%) | 35 (4.9%) |
| Biracial/Other | 14 (5.1%) | 31 (7.0%) | 45 (6.3%) |
| Unknown | 0 (0%) | 131 (29.6%) | 131 (18.3%) |
| FM ethnicity | |||
| Hispanic | 27 (9.9%) | 25 (5.6%) | 52 (7.3%) |
| Non-Hispanic | 245 (90.1%) | 132 (29.8%) | 377 (52.7%) |
| Unknown | 0 (0%) | 286 (64.6%) | 286 (40.0%) |
| SORTS collected as research | 272 (100%) | 314 (70.9%) | 586 (82.0%) |
| SORTS collected in routine clinical care | 0 (0.0%) | 129 (29.1%) | 129 (18.0%) |
Note. SORTS = Significant Others’ Responses to Trauma Scale. EFA = exploratory factor analysis; CFA = confirmatory factor analysis; IP = identified patient; FM = family member.
Some studies/clinics permitted participants to select more than one racial identity, so totals may exceed 100%
1.2. Measures
1.2.1. Accommodation
Participants completed the SORTS as part of their baseline visit for the study/clinic, or, in the case of one contributing study, at the 1-month post-baseline visit (see Allen et al., 2021). The SORTS includes 14 items reflecting accommodative behaviours by family members. Respondents are asked to rate (separately) the frequency with which they engaged in the behaviour over the past month on a scale from 0 (Never) to 4 (Daily or almost every day) and how much they were bothered by engaging in the behaviour on a scale from 0 (Not at all) to 4 (Extremely). As noted above, the 28 responses are commonly summed into a total score, although some investigators calculate totals of the frequency and distress subscales separately.
One contributing study had slightly modified the SORTS instructions and response options. Specifically, (Allen et al., 2021) asked respondents to rate their accommodation over the past 6 months, rather than the standard 1 month, to align with the interval between assessments in that study. Notably, prior studies using the SORTS have found extremely high stability in scores (Fredman et al., 2014, 2016). Allen et al. (2021) also provided a not applicable option for each item; such responses were coded as zeros. Additionally, because the individual frequency/distress items on the SORTS are paired (i.e. the respondent first rates how often they have engaged in a particular form of accommodation and next rates how distressed they are by engaging in that form of accommodation), we rescored as zeros any distress items where the corresponding frequency item had been rated a zero.
1.2.2. PTSD symptom severity
Some contributing samples had included administrations of the PTSD Checklist for DSM-IV (military version, PCL-M; Weathers et al., 1993). The PCL-M is a widely-used measure of military-related PTSD symptoms, consisting of 17 items corresponding to the symptoms of PTSD in DSM-IV; the measure has strong psychometric properties (Wilkins et al., 2011) and scores on the PCL-M are highly correlated with scores on the PTSD Checklist for DSM-5 (PCL-5; Weathers et al., 2013) (e.g. Moshier et al., 2019). We obtained item-level PCL-M responses from 228 IPs. Additionally, a smaller number of contributing samples had asked FMs to rate their perception of the IP’s symptom severity; we obtained item-level data of this collateral-rated PCL-M from 149 FM participants. We analysed the PCL-M according to its symptom clusters, using the four-factor emotional numbing model (King et al., 1998).
1.2.3. Relationship satisfaction
Some contributing samples had included administration of the Couple Satisfaction Index (CSI; Funk & Rogge, 2007). The CSI consists of 32 items assessing romantic relationship satisfaction. The CSI is a unidimensional scale and has been shown in IRT analyses to outperform other common measures of relationship satisfaction (Funk & Rogge, 2007). We obtained CSI total scores from 185 FMs and 185 IPs (each rating their own relationship satisfaction).
1.3. Data analysis
We conducted all analyses using Mplus version 7 (Muthén & Muthén, 2012). Missing data were minimal, with only 1.24% of SORTS item-level responses missing. To conduct the exploratory factor analysis (EFA) and confirmatory factor analysis (CFA) tests on completely independent samples, we ran the EFA within a single large study sample (n = 272, from (Allen et al., 2021)). We used oblique (geomin) rotation to allow for potential correlation among factors. We conducted the EFAs using two possible scoring methods for the SORTS; first, summing the paired frequency and distress scores for each of the 14 items reflecting accommodation, such that there were 14 items whose possible scores ranged from 0 to 8. We treated these items as continuous and examined EFA solutions of up to four factors3 using eigenvalues, parallel analysis, fit statistics, and patterns of factor loading. For these models, we used the robust maximum likelihood estimator (MLR). We also conducted separate EFAs on both the 14 frequency items and the 14 distress items. These items were treated as ordinal due to their possible score range of 0–4 (Flora & Curran, 2004; Wirth & Edwards, 2007); accordingly, we used the weighted least squares means and variances adjusted (WLSMV) estimator in these models. Again, we examined EFA solutions of up to four factors using eigenvalues, fit statistics, and patterns of factor loading.
Following EFA, we pooled the remaining samples into the CFA sample (n = 443). Using a pooled sample for the CFA allowed for the examination of the novel measurement model in an independent group of respondents with more heterogeneity compared to the single-study sample for the EFA. We evaluated model fit using χ2, Bentler comparative fit index (CFI), Tucker-Lewis index (TLI), root mean square error of approximation (RMSEA), and standardised root mean square residual (RMSR). We considered fit statistics collectively for each model and used established criteria to determine close fit: χ2 p values > .05, CFI and TLI ≥ 0.95, and lower limit of the RMSEA 90% confidence interval and RMSR < .05 (Bentler, 1990; Brown, 2015; Browne & Cudeck, 1992; Hu & Bentler, 1999). We compared the fit of several alternative CFAs. Given that some investigators have used totals of the frequency and distress subscales in their analyses, we conducted a CFA in which all frequency items loaded onto a single latent Frequency factor and all distress items loaded onto a single latent Distress factor. Because the frequency and distress items were not summed in this model, we again treated items as ordinal and used the WLSMV estimator. For all subsequent CFA models, which were derived from the EFA findings, we combined the paired frequency and distress items, treating these summed items as continuous and using the robust maximum likelihood (MLR) estimator.
Additionally, we examined construct validity in the CFA sample by testing correlations between the SORTS factors that were identified through EFA and both the PCL-M symptom clusters and the CSI total score. We used procedures developed by Meng et al. (1992) to examine contrasts between theoretically more – versus less-related symptom clusters for each factor.
Finally, we used IRT to examine the discrimination and difficulty of individual SORTS items. For the IRT analyses, we considered the frequency and distress items separately and used the WLSMV estimator. We obtained item discrimination and item difficulty scores for each item. Item discrimination (a) indicates the degree to which an item accurately differentiates between participants of varying accommodation levels at that item’s point of median probability of endorsement. Item difficulty (b) identifies the level of accommodation (in standard deviation units) above which respondents become more likely to endorse an item than not (e.g. the point at which 50% of respondents endorse a symptom). The higher the estimated item difficulty, the greater the level of accommodation that is needed for probable item endorsement. In addition to these two scores, we obtained item information curves (IIC) and item characteristic curves (ICC) for each item. IICs graphically depict measurement precision across the continuum of the respondent’s level of accommodation. The value at the apex of the IIC corresponds to the item difficulty. ICCs are a visual depiction of the relationship between the level of accommodation and the probability of item endorsement for that item. Steeper slopes indicate an item has greater discrimination.
1.4. Transparency and openness
Data used in the present study were aggregated across multiple studies/clinical programmes; as a result of differences in the individual Data Use Agreements that govern this aggregation, the data are not available to outside investigators. Syntax used in all analyses are available by emailing the corresponding author. We report all data exclusions, all manipulations, and all measures in the study. Supplementary Table S1 displays the data available across the contributing datasets. The study design and analytic plan were not publicly preregistered.
2. Results
2.1. Factor structure
As noted above, we conducted two types of EFA: (1) with the paired frequency and distress items summed together, yielding 14 items ranging in score from 0 to 8, and (2) considering the frequency and distress items in separate EFAs, each with 14 items ranging in score from 0 to 4. In all cases, eigenvalues were above 1.0 for solutions with one or two factors, indicating a maximum of two factors should be extracted. Parallel analysis within the summed frequency/distress model likewise indicated that a maximum of two factors should be extracted (parallel analysis is not possible when using categorical or ordinal items). Model fit statistics were adequate for a two-factor model, whereas a one-factor model provided poor fit to the data (see Supplementary Table S2). Examination of the patterns of factor loadings revealed essentially identical item loadings onto the two latent factors of the summed frequency/distress model and the individual models of only frequency items and only distress items (see Supplementary Table S3). Items 2 (avoidance of physical closeness), 8 (managing relationships with others), and 10 (avoidance of discussion of the trauma) had salient cross-loadings on both factors in all three models; items 2 and 10 were almost equally weighted across the two factors in all analyses, although the patterns of primary versus cross-loadings shifted slightly across models. See Table 2 for the factor loadings from the summed frequency/distress model. We considered Factor 1 to represent ‘anger-related accommodation’ (encompassed by items related to managing conflict or explosivity) and Factor 2 to represent ‘anxiety-related accommodation' (encompassed by items related to avoidance or changing routine). Correlation of the two factors was high across all three models (rs = .68 – .70, see Supplementary Table S4).
Table 2.
Standardised exploratory factor analysis loadings of a two-factor SORTS model with continuous scores.
| Managing explosivity/conflict | Avoidance and changing routine | |
|---|---|---|
| (Factor 1) | (Factor 2) | |
| 1. Avoid [Name] because of his/her irritable or angry mood? | 0.823 | 0.014 |
| 2. Avoid being physically close with [Name] because of his/her discomfort? | 0.285* | 0.345 |
| 3. Cancel or rearrange plans or social activities because [Name] did not want to do them? | 0.106 | 0.685 |
| 4. Avoid doing things, going places, or seeing people with [Name] that make him/her anxious or uncomfortable? | −0.042 | 0.803 |
| 5. ‘Bite your tongue’ or hold back from trying to discuss any relationship issues with [Name]? | 0.899 | −0.051 |
| 6. Take over a task or chore for [Name] that he/she is uncomfortable doing because of his/her traumatic event? | 0.047 | 0.457 |
| 7. Help [Name] with a task because he/she was having trouble concentrating? | 0.136 | 0.505 |
| 8. Make excuses to others for [Name]’s behaviour or try to manage his/her relationships with other people? | 0.665 | 0.175* |
| 9. ‘Tiptoe’ around [Name] so as not to anger him/her? | 0.908 | −0.008 |
| 10. Avoid discussing events related to [Name]’s traumatic event(s) in front of him/her to avoid his/her becoming upset? | 0.321* | 0.374 |
| 11. Not share your own feelings or concerns with [Name] due to concerns that he/she would become upset? | 0.788 | 0.033 |
| 12. Change your routine due to [Name]’s difficulties? | −0.001 | 0.806 |
| 13. How much have you modified your leisure activities due to [Name]’s difficulties? | −0.001 | 0.813 |
| 14. Give up control to [Name] because of his/her desire to be in charge? | 0.642 | −0.001 |
Note. * = significant cross-loading. SORTS = Significant Others’ Responses to Trauma Scale.
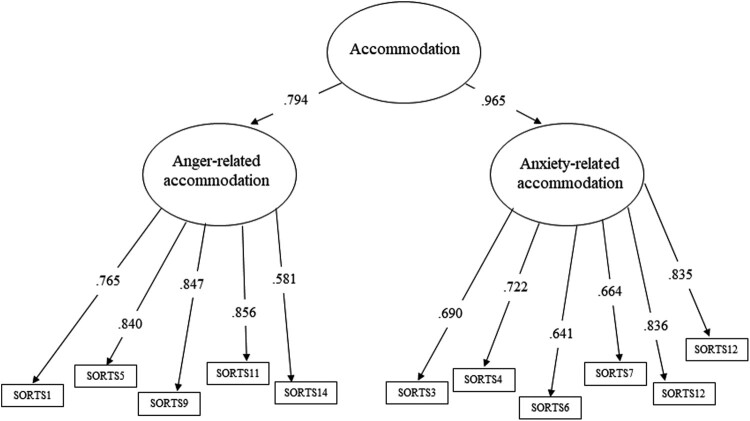
Next, we proceeded to CFA analysis, comparing several models. The two-factor model representing Frequency and Distress as latent factors provided poor fit to the data (see Table 3). We next conducted a CFA that aligned with the summed EFA model, allowing items to load only on their primary factor (items 1, 5, 8, 9, 11, and 14 loading onto Factor 1 and items 2, 3, 4, 6, 7, 10, 12, and 13 loading onto Factor 2). Collective review of this model’s fit indices compared to those of the Frequency and Distress model showed substantially improved fit; however, we could not directly compare the models, as they are not nested. Next, we conducted a CFA in which we discarded the cross-loading items, using only the remaining 11 items. This model demonstrated good fit. Further, the Satorra-Bentler scaled chi-square test indicated that removing the three poorly-performing items significantly improved model fit (χ2 (33) = 115.00, p < .001). Correlations among Factor 1 (anger-related accommodation) and Factor 2 (anxiety-related accommodation) were high (rs = .77 – .83) across both models. Finally, we tested a higher-order model in which both factors from the final 11-item model were allowed to load onto a single higher-order factor of accommodation; this model also provided good fit to the data. As the higher-order model is most parsimonious, it is recommended as the optimal model (see Figure 1). See Table 3 for fit statistics for all CFA models.
Table 3.
Fit statistics for CFA models.
| Chi-sq | CFI | TLI | RMSEA 90% CI | RMSR | |
|---|---|---|---|---|---|
| Frequency and Distress model | 4278.208 (p < .001) |
.835 | .821 | 0.155–0.164 | N/A |
| 14 items | 251.960 (p < .001) |
.926 | .912 | 0.063–0.082 | 0.052 |
| 11 items | 136.617 (p < .001) |
.949 | .935 | 0.057–0.083 | 0.040 |
| Higher-order model with 11 items | 136.617 (p < .001) |
.949 | .935 | 0.057–0.083 | 0.040 |
Note. CFI = Bentler comparative fit index; TLI = Tucker-Lewis index; RMSEA 90% CI = root mean square error of approximation 90% confidence interval; RMSR = standardised root mean square residual.
Figure 1.
Higher-order measurement model of the significant others’ Responses to Trauma Scale with items identified through exploratory factor analysis.
2.2. Discriminant and criterion validity
Correlations among the SORTS factors and the PCL (IP- and FM-rated) and the CSI are presented in Table 4. Both SORTS factors were moderately correlated with the IP-rated PCL symptom clusters (rs = .40 – .52, all ps < .001). Planned contrasts following the procedure outlined by Meng et al. (1992) were used to compare the correlation of SORTS Factor 1 (anger-related accommodation) with both IP-rated hyperarousal and IP-rated avoidance and to compare SORTS factor 2 (anxiety-related accommodation) with both IP-rated hyperarousal and IP-rated avoidance. These specific clusters were selected because we anticipated that hyperarousal symptoms (which include anger/aggression) would be primarily associated with FMs’ accommodation of anger whereas avoidance symptoms would be primarily associated with FMs’ accommodation of anxiety. Results indicated that IP-rated hyperarousal was more strongly associated with Factor 1 than IP-rated avoidance (Z = 2.63) but that the associations of these IP-rated clusters with Factor 2 were not significantly different (Z = 0.82).
Table 4.
Correlations among SORTS Factors, PTSD symptoms rated by IP and FM, and relationship satisfaction.
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. SORTS Factor 1 (anger) | 1 | |||||||||||
| 2. SORTS Factor 2 (avoid) | .672** | 1 | ||||||||||
| 3. PCL reexperiencing | .427** | .414** | 1 | |||||||||
| 4. PCL avoidance | .403** | .411** | .718** | 1 | ||||||||
| 5. PCL numbing | .475** | .467** | .693** | .648** | 1 | |||||||
| 6. PCL hyperarousal | .524** | .449** | .750** | .659** | .725** | 1 | ||||||
| 7. FM-rated PCL reexperiencing | .304** | .398** | .383** | .364** | .334** | .301** | 1 | |||||
| 8. FM-rated PCL avoidance | .274** | .387** | .367** | .388** | .335** | .321** | .571** | 1 | ||||
| 9. FM-rated PCL numbing | .295** | .268** | .199* | .241** | .260** | .234** | .374** | .447** | 1 | |||
| 10. FM-rated PCL hyperarousal | .501** | .465** | .371** | .419** | .398** | .411** | .672** | .576** | .439** | 1 | ||
| 11. FM CSI | −.573** | −.415** | .081 | .236 | −.024 | .204 | .177 | .402 | .282 | .459 | 1 | |
| 12. IP CSI | −.442** | −.270** | .028 | .097 | −.211 | −.094 | −.078 | −.201 | −.415 | −.183 | .581** | 1 |
Note. SORTS = Significant Others’ Responses to Trauma Scale. IP = identified patient. FM = family member. PCL = PTSD Checklist-Military Version. CSI = Couple Satisfaction Index. Ns for SORTS correlation with PCL and FM-rated PCL were 228 and 149, respectively. N for SORTS correlation with CSI was 185. Ns for CSI correlation with PCL and FM-rated PCL were 17 and 17, respectively.
Regarding the FM-rated PCL symptom clusters, again, the correlations with the SORTS factors were generally moderate, although there was a broader range than with the IP-rated PCL (rs = .27 – .50, all ps < .001, see Table 4). Planned contrasts were again used to compare the correlation of SORTS Factor 1 (anger-related accommodation) with both FM-rated hyperarousal and FM-rated avoidance and also SORTS Factor 2 (anxiety-related accommodation) with both FM-rated hyperarousal and FM-rated avoidance. Results indicated that FM-rated hyperarousal was more strongly associated with Factor 1 than FM-rated avoidance (Z = 3.44) but that the associations of these FM-rated clusters with Factor 2 were not significantly different (Z = 1.19).
Finally, regarding relationship satisfaction, both SORTS factors were negatively correlated with both FM- and IP-rated satisfaction (rs = −.27 to −.57, all ps < .001), though the correlations with FM-rated satisfaction were stronger than for IP-rated satisfaction (Z = 2.41 for Factor 1 and Z = 2.31 for Factor 2). Correlations of relationship satisfaction with SORTS Factor 1 (anger-related accommodation) were also stronger than with SORTS Factor 2 (anxiety-related accommodation) across both IPs (Z = 3.07) and FMs (Z = 2.44).
2.3. IRT results
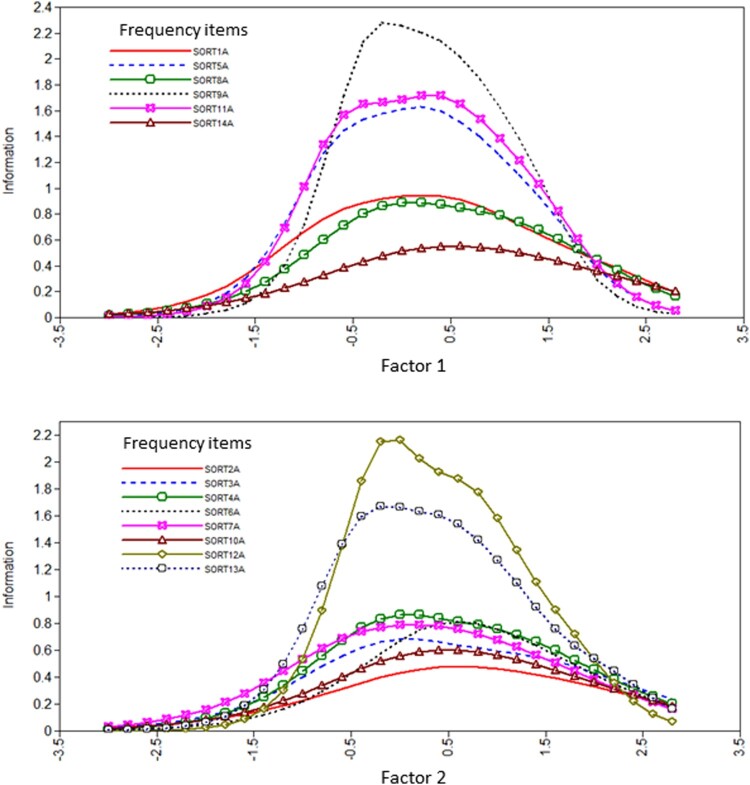
We report estimated discrimination and difficulty parameters in Supplementary Table S5 and present ICCs in Supplementary Figures S1 and S2 and frequency IICs in Figure 2. With regard to interpretation, both the IIC and ICC figures contain an x-axis which is a standardised symptom score with a mean of zero and an SD of 1. In the IIC, the y-axis depicts the information provided by the item at a given level of the latent trait, whereas in the ICC the y-axis depicts the probability of item endorsement.
Figure 2.
Item information curves (IICs) for individual frequency items from the Significant other’s Responses to Trauma Scale (SORTS) loading onto Factor 1 (anger-related accommodation) and factor (anxiety-related accommodation).
As shown in Figure 2, among the Factor 1 (anger-related accommodation) frequency items, item 9A provided the most information, followed by items 5A and 11A. As indicated by the overlapping curves in the IIC, items tended to provide the most information at approximately the same level. The relatively flat curve of item 14A indicates that this item provides substantially less information about level of accommodation relative to the other items. Among the Factor 1 frequency items, items 1A (ɑ = 1.964), 8A (ɑ = 1.898) and 14A (ɑ = 1.402) provided relatively poorer discrimination, whereas items 5A (ɑ = 2.773), 9A (ɑ = 3.376), and 11A (ɑ = 2.938) distinguished well among individuals low and high in this factor. Finally, as shown in the ICC curves in Supplementary Figure S1, items 8A and 14A tended to have less differentiation in the probabilities of endorsement across the highest response options; this contrasts with the other items in the group (e.g. 9A), where the patterns of responding are more distinct across the response options. Factor 1 distress items showed a similar pattern of results as the corresponding frequency items (see Supplementary Table S5 and Supplementary Figure S1).
Among the Factor 2 (anxiety-related accommodation) frequency items, items 12A and 13A provided notably more information than the remaining items, whereas item 2A provided the least. Again, the IIC curves were substantially overlapping at the same level of accommodation (see Figure 2). Several items evidenced poor discrimination (2A ɑ = 1.307, 3A ɑ = 1.652, 4A ɑ = 1.871, 6A ɑ = 1.726, 7A ɑ = 1.734, and 10A ɑ = 1.483), whereas items 12A (ɑ = 3.210) and 13A (ɑ = 2.783) distinguished well among individuals low and high in this factor. Per the ICC curves in Supplementary Figure S2, items 2A, 6A, and 10A all had relatively little differentiation in the probabilities of endorsement across the most severe response options. Factor 2 distress items showed a similar pattern of results as the corresponding frequency items (see Supplementary Table S5 and Supplementary Figure S2).
A visual representation of all response levels for all items is shown in Supplementary Figure S3. Distribution of item difficulty values provided coverage from below average to >4.0 standard deviations above average across both factors. However, there were instances of redundancy, particularly within Factor 2 (anxiety-related accommodation).
3. Discussion
Using a large sample of FM respondents (overwhelmingly the female romantic partners of male service members and veterans), we completed an analysis of the factor structure, criterion validity, and item-level performance of the SORTS. We determined that a higher-order model of accommodation, with two factors reflecting underlying anger-related and anxiety-related accommodation constructs, provided the best fit to the data.
The emergence of an anxiety-related factor is unsurprising and aligns with the conceptualisation of accommodation in anxiety and fear-based disorders as facilitating anxious avoidance (e.g. Calvocoressi et al., 1995; Thompson-Hollands et al., 2014). However, the presence of a anger-related factor is notable and perhaps more specific to PTSD compared to other disorders. Irritable behaviour and persistent negative mood (including anger) are symptoms of PTSD (American Psychiatric Association, 2013), and anger is a more prominent feature of PTSD compared to other disorders (Olatunji et al., 2010). Anger is a very challenging PTSD symptom from an interpersonal standpoint. Social information processing models outline how trauma cues operate within a social environment, resulting in a heightened risk for negative emotional and behavioural responses when IPs have information processing biases (Monson et al., 2010; Taft et al., 2017). Aggressive behaviour may be a strategy to assert control over trauma cues and the resulting anxious or fear-based reaction (Olatunji et al., 2010). FMs of patients with PTSD often have a deep sense of being on edge around their loved one. Reuman and Thompson-Hollands (2020) noted that the centrality of anger in PTSD has potentially significant implications for accommodation in PTSD relative to other disorders. However, it is notable that the two factors that were identified in EFA were strongly correlated in the CFA model, indicating that there may be many features of the IP, FM, and relationship that relate to both.
Results from the discriminant and criterion validity analyses largely conformed to our hypotheses. Relationship satisfaction was negatively associated with SORTS scores, more strongly for FMs than for IPs and more strongly for anger-related accommodation compared to anxiety-related accommodation. The association between accommodation and decreased relationship satisfaction has been demonstrated in both community and military samples (e.g. Fredman et al., 2014, 2022). Despite accommodation being linked in some cases to a desire to be helpful to the IP and/or a desire to maintain the relationship (Renshaw et al., 2020), ultimately these behaviours (in combination with PTSD itself) appear to wear away at enjoyment and connection. PTSD symptoms were positively associated with accommodation, as has been shown in prior studies (Allen et al., 2021; Campbell et al., 2017). We found that anger-related accommodation was more highly associated with hyperarousal than with avoidance (as rated by IPs and FMs), likely because the hyperarousal cluster includes symptoms of irritability. Anxiety-related accommodation showed a somewhat unexpected pattern with PTSD symptom clusters: it did not correlate more highly with avoidance symptoms than with hyperarousal symptoms (again as rated by both IPs and FMs). Interestingly, across all the FM-rated symptom clusters, hyperarousal showed the highest absolute correlation with both anger-related and anxiety-related accommodation. It may be that FMs who perceive the IP to be especially irritable and ‘on edge’ as a result of PTSD are attempting to preemptively avert both angry and anxious responses.
Regarding the IRT analyses, the SORTS scores provided reasonable coverage from below to slightly above average for each factor and substantial coverage for respondents with high levels of accommodation. There was redundancy, especially in scores >2.0 SD, but some of this overlap in difficulty was driven by the three cross-loading items that are recommended for removal (see below).
3.1. Recommendations for SORTS administration and scoring
Several SORTS items performed somewhat less well in the factor analysis, with substantial cross-loadings and, in some cases, weaker loadings overall. We recommend that these items (2, 8, and 10) no longer be included in SORTS administration and scoring.
Regarding scoring, the results of our higher-order factor analysis support the use of a total score in routine clinical practice. However, in research settings we encourage analysis of the factors in addition to the total score, as the factors showed somewhat distinct performances across the criterion /discriminant validity analyses; these differences (and others that may yet emerge) may ultimately provide important nuance to our understanding of accommodation. Future research on the performance of these factors may also help to inform their use in routine clinical practice.
3.2. Constraints on generality
The EFA sample was not especially diverse in terms of race/ethnicity, although the CFA sample had more variability and the model continued to fit the data well. Many of the aggregated samples were from research studies, which may differ from clinical samples in meaningful ways. Some of the aggregated studies were specifically limited to romantic couples and/or limited to military/veteran men partnered with civilian women (and even if participants in a given study were not required to fit this pattern, these dyads were highly over-represented in our overall participant pool); therefore, we cannot determine whether our study findings generalise to the broader population. Finally, we had hoped to conduct tests of measurement invariance but were underpowered across many potential variables of interest (e.g. veteran versus civilian IP; male versus female FM; male versus female IP; romantic versus non-romantic dyads; White versus non-White FMs). We strongly encourage further exploration of the SORTS’ psychometric properties in diverse samples.
3.3. Limitations
In addition to the constraints on generality described above, the study had other limitations. Although our sample was quite large and adequately powered to test the models and scale parameters of interest, it was amassed via requests to individual clinics/research programmes by the study authors rather than via an a priori data collection approach or an open call to settings that, unbeknownst to us, may be routinely administering the SORTS. This may have resulted in biases in the data that influenced our findings. Furthermore, many samples did not assess and/or report information regarding FMs’ own PTSD symptoms (see Supplementary Table S1). FMs who are themselves experiencing significant PTSD symptoms may display different patterns of accommodation compared to FMs without notable PTSD symptoms, but we were unable to probe this in the current data set.
3.4. Conclusions
The SORTS demonstrated good fit in a higher-order model of accommodation with two factors. The identified factors were anger-related accommodation, encompassing items related to minimising conflict and FM constraints on their self-expression, and anxiety-related accommodation, encompassing items related to taking on additional responsibilities or changes to the FM’s recreational or social activities. Accommodation was positively related to PTSD severity (as rated by both IPs and FMs) and negatively related to relationship satisfaction, with anger-related accommodation being particularly associated with reduced satisfaction, and FMs showing a stronger relationship between any accommodation and reduced satisfaction compared to IPs. IRT analyses indicated that the SORTS items generally performed well and covered a broad range of accommodation levels. Our results add to the understanding of the construct of accommodation in PTSD and increase confidence in the SORTS’ psychometric properties, although we also identified some items that could be revised in future versions to potentially increase the scale’s psychometric performance. Although our results support analysing the scale using a total score for clinical purposes at this time, future researchers are encouraged to also analyse the SORTS according to the two factors identified here, as they may ultimately demonstrate distinct patterns of association with other clinical features and treatment outcomes.
Supplementary Material
Acknowledgments
We thank the STRONG STAR Consortium and the Consortium to Alleviate PTSD for contributing a portion of the data used in these analyses. The views expressed herein are solely those of the authors and do not reflect an endorsement by or the official policy or position of Brooke Army Medical Center, Carl R. Darnall Army Medical Center, the US Army Medical Department, the Defense Health Agency, the US Army Office of the Surgeon General, the Department of the Army, the Department of the Air Force, the Department of Defense, the Department of Veterans Affairs, nor any agencies of the US Government.
Funding Statement
A portion of the funding for this work was made possible by the US Department of Veterans Affairs (Clinical Sciences Research and Development Service award # IK2 CX001589 to Johanna Thompson-Hollands). A portion of the funding for this work was made possible by the US Department of Defense through the US Army Medical Research and Materiel Command, Congressionally Directed Medical Research Programs, Psychological Health and Traumatic Brain Injury Research Program awards W81XWH-08-02-109 (Alan L. Peterson), W81XWH-08-02-0114 (Brett T. Litz), and W81XWH-08-02-0115 (Candice M. Monson). Additional research support was provided by Consortium to Alleviate PTSD (CAP) award numbers W81XWH-13-2-0065 from the US Department of Defense, Defense Health Program, Psychological Health and Traumatic Brain Injury Research Program (PH/TBI RP), and I01CX001136-01 from the US Department of Veterans Affairs, Office of Research & Development, Clinical Science Research & Development Service. Further funding was provided by the National Institute of Mental Health (R34 MH076813 to Candice M. Monson and 1F31 MH098581 to Sarah B. Campbell), the Canadian Institutes of Health Research (106683 to Candice M. Monson), and the US Department of Defense through the US Army Medical Research and Materiel Command, Congressionally Directed Medical Research Programs (W81XWH-12-1-0090 to Elizabeth S. Allen).
Notes
Throughout the paper we use the term ‘family member’ (or FM) to encompass relatives/romantic partners and, in some cases, close friends.
Not all studies/clinics comprehensively assessed FMs for the presence of a current PTSD diagnosis, so it is possible that other ‘dual PTSD’ dyads remained in our final sample.
It is recommended that factors be identified by a minimum of three indicators in order to avoid underidentification (Brown, 2015), thus with 14 SORTS items we examined 1–4 factor solutions.
Disclosure statement
No potential conflict of interest were reported by the author(s).
Author contributions
Conceptualization: Johanna Thompson-Hollands, Steffany J. Fredman, Candice M. Monson, Daniel J. Lee; Data curation: Johanna Thompson-Hollands; Formal analysis: Johanna Thompson-Hollands, Daniel J. Lee; Funding acquisition: Johanna Thompson-Hollands, Steffany J. Fredman, Candice M. Monson, Elizabeth S. Allen, Sarah B. Campbell, Keith D. Renshaw, David S. Riggs, Stacey Young-McCaughan, Terence M. Keane, Alan L. Peterson; Investigation: Johanna Thompson-Hollands, Steffany J. Fredman, Candice M. Monson, Elizabeth S. Allen, Sarah B. Campbell, Nicole D. Pukay-Martin, Kathleen M. Chard, Joel Sprunger, Erica Birkley, Alan L. Peterson, Stacey Young-McCaughan, Katherine A. Dondanville; Methodology: Johanna Thompson-Hollands, Daniel J. Lee; Project administration: Johanna Thompson-Hollands; Supervision: Johanna Thompson-Hollands, Steffany J. Fredman; Visualization: Johanna Thompson-Hollands, Daniel J. Lee; Writing – original draft: Johanna Thompson-Hollands; Writing – review and editing: all authors.
Data availability statement
Data used in the present study were aggregated across multiple studies/clinical programmes; as a result of differences in the individual Data Use Agreements that govern this aggregation, the data are not available to outside investigators.
References
- Allen, E., Renshaw, K., Fredman, S. J., Le, Y., Rhoades, G., Markman, H., & Litz, B. (2021). Associations between service members’ posttraumatic stress disorder symptoms and partner accommodation over time. Journal of Traumatic Stress, 34(3), 596–606. 10.1002/jts.22645 [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association . (2000). Diagnostic and statistical manual of mental disorders (4th ed., text rev.). American Psychiatric Association. [Google Scholar]
- American Psychiatric Association . (2013). Diagnostic and statistical manual of mental disorders (5th ed.). 10.1176/appi.books.9780890425596 [DOI] [Google Scholar]
- Amir, N., Freshman, M., & Foa, E. B. (2000). Family distress and involvement in relatives of obsessive-compulsive disorder patients. Journal of Anxiety Disorders, 14(3), 209–217. 10.1016/S0887-6185(99)00032-8 [DOI] [PubMed] [Google Scholar]
- Bentler, P. M. (1990). Comparative fit indexes in structural models. Psychological Bulletin, 107(2), 238–246. 10.1037/0033-2909.107.2.238 [DOI] [PubMed] [Google Scholar]
- Brown, T. A. (2015). Confirmatory factor analysis for applied research (2nd ed.). The Guilford Press. [Google Scholar]
- Browne, M. W., & Cudeck, R. (1992). Alternative ways of assessing model fit. Sociological Methods & Research, 21(2), 230–258. 10.1177/0049124192021002005 [DOI] [Google Scholar]
- Calvocoressi, L., Lewis, B., Harris, M., Trufan, S. J., Goodman, W. K., McDougle, C. J., & Price, L. H. (1995). Family accommodation in obsessive-compulsive disorder. American Journal of Psychiatry, 152(3), 441–443. 10.1176/ajp.152.3.441 [DOI] [PubMed] [Google Scholar]
- Campbell, S. B., Renshaw, K. D., Kashdan, T. B., Curby, T. W., & Carter, S. P. (2017). A daily diary study of posttraumatic stress symptoms and romantic partner accommodation. Behavior Therapy, 48(2), 222–234. 10.1016/j.beth.2016.04.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flora, D. B., & Curran, P. J. (2004). An empirical evaluation of alternative methods of estimation for confirmatory factor analysis with ordinal data. Psychological Methods, 9(4), 466–491. 10.1037/1082-989X.9.4.466 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredman, S. J., Baucom, D. H., Miklowitz, D. J., & Stanton, S. E. (2008). Observed emotional involvement and overinvolvement in families of patients with bipolar disorder. Journal of Family Psychology, 22(1), 71–79. 10.1037/0893-3200.22.1.71 [DOI] [PubMed] [Google Scholar]
- Fredman, S. J., Chambless, D. L., & Steketee, G. (2004). Development and validation of an observational coding system for emotional overinvolvement. Journal of Family Psychology, 18(2), 339–347. 10.1037/0893-3200.18.2.339 [DOI] [PubMed] [Google Scholar]
- Fredman, S. J., Fischer, M. S., Baucom, D. H., Le, Y., Taverna, E. C., Chow, S.-M., Ram, N., & Marshall, A. D. (2023). PTSD symptom cluster severity predicts momentary emotion dynamics during couple conversations. Behavior Therapy, 54(2), 330–345. 10.1016/j.beth.2022.09.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredman, S. J., Le, Y., Macdonald, A., Monson, C. M., Rhoades, G. K., Dondanville, K. A., Blount, T. H., Hall-Clark, B. N., Fina, B. A., Mintz, J., Litz, B. T., Young-McCaughan, S., Jenkins, A. I. C., Yarvis, J. S., Keane, T. M., Peterson, A. L., & PTSD, for the C. to A . (2021). A closer examination of relational outcomes from a pilot study of abbreviated, intensive, multi-couple group cognitive-behavioral conjoint therapy for PTSD with military dyads. Family Process, 60(3), 712–726. 10.1111/famp.12654 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredman, S. J., Le, Y., Renshaw, K. D., & Allen, E. S. (2022). Longitudinal associations among service members’ PTSD symptoms, partner accommodation, and partner distress. Behavior Therapy, 53(6), 1161–1174. 10.1016/j.beth.2022.05.005 [DOI] [PubMed] [Google Scholar]
- Fredman, S. J., Pukay-Martin, N. D., Macdonald, A., Wagner, A. C., Vorstenbosch, V., & Monson, C. M. (2016). Partner accommodation moderates treatment outcomes for couple therapy for posttraumatic stress disorder. Journal of Consulting and Clinical Psychology, 84(1), 79–87. 10.1037/ccp0000061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredman, S. J., Vorstenbosch, V., Wagner, A. C., Macdonald, A., & Monson, C. M. (2014). Partner accommodation in posttraumatic stress disorder: Initial testing of the Significant Others’ Responses to Trauma Scale (SORTS). Journal of Anxiety Disorders, 28(4), 372–381. 10.1016/j.janxdis.2014.04.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Funk, J. L., & Rogge, R. D. (2007). Testing the ruler with item response theory: Increasing precision of measurement for relationship satisfaction with the Couples Satisfaction Index. Journal of Family Psychology, 21(4), 572–583. 10.1037/0893-3200.21.4.572 [DOI] [PubMed] [Google Scholar]
- Galatzer-Levy, I. R., & Bryant, R. A. (2013). 636,120 ways to have posttraumatic stress disorder. Perspectives on Psychological Science, 8(6), 651–662. 10.1177/1745691613504115 [DOI] [PubMed] [Google Scholar]
- Howard, K. P., Spoont, M. R., Polusny, M. A., Eftekhari, A., Rosen, C. S., & Meis, L. A. (2023). The role of symptom accommodation in trauma-focused treatment engagement and response. Journal of Traumatic Stress. 36(3), 524–536. 10.1002/jts.22912 [DOI] [PubMed] [Google Scholar]
- Hu, L., & Bentler, P. M. (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal, 6(1), 1–55. 10.1080/10705519909540118 [DOI] [Google Scholar]
- King, D. W., Leskin, G. A., King, L. A., & Weathers, F. W. (1998). Confirmatory factor analysis of the Clinician-Administered PTSD Scale: Evidence for the dimensionality of posttraumatic stress disorder. Psychological Assessment, 10(2), 90–96. 10.1037/1040-3590.10.2.90 [DOI] [Google Scholar]
- Lebowitz, E. R., Panza, K. E., & Bloch, M. H. (2016). Family accommodation in obsessive-compulsive and anxiety disorders: A five-year update. Expert Review of Neurotherapeutics, 16(1), 45–53. 10.1586/14737175.2016.1126181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meng, X., Rosenthal, R., & Rubin, D. B. (1992). Comparing correlated correlation coefficients. Psychological Bulletin, 111(1), 172–175. 10.1037/0033-2909.111.1.172 [DOI] [Google Scholar]
- Merlo, L. J., Lehmkuhl, H. D., Geffken, G. R., & Storch, E. A. (2009). Decreased family accommodation associated with improved therapy outcome in pediatric obsessive–compulsive disorder. Journal of Consulting and Clinical Psychology, 77(2), 355–360. 10.1037/a0012652 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monson, C. M., & Fredman, S. J. (2012). Cognitive-behavioral conjoint therapy for PTSD: Harnessing the healing power of relationships. Guilford Press. [Google Scholar]
- Monson, C. M., Fredman, S. J., & Dekel, R. (2010). Posttraumatic stress disorder in an interpersonal context. In Beck J. G. (Ed.), Interpersonal processes in the anxiety disorders: Implications for understanding psychopathology and treatment (pp. 179–208). American Psychological Association. 10.1037/12084-007 [DOI] [Google Scholar]
- Monson, C. M., Fredman, S. J., Macdonald, A., Pukay-Martin, N. D., Resick, P. A., & Schnurr, P. P. (2012). Effect of cognitive-behavioral couple therapy for PTSD: A randomized controlled trial. JAMA, 308(7), 700–709. 10.1001/jama.2012.9307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moshier, S. J., Lee, D. J., Bovin, M. J., Gauthier, G., Zax, A., Rosen, R. C., Keane, T. M., & Marx, B. P. (2019). An empirical crosswalk for the PTSD checklist: Translating DSM-IV to DSM-5 using a veteran sample. Journal of Traumatic Stress, 32(5), 799–805. 10.1002/jts.22438 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén, L. K., & Muthén, B. O. (2012). MPlus (Version 7) [Computer software]. https://www.statmodel.com/.
- Olatunji, B. O., Ciesielski, B. G., & Tolin, D. F. (2010). Fear and loathing: A meta-analytic review of the specificity of anger in PTSD. Behavior Therapy, 41(1), 93–105. 10.1016/j.beth.2009.01.004 [DOI] [PubMed] [Google Scholar]
- Pukay-Martin, N. D., Fredman, S. J., Martin, C. E., Le, Y., Haney, A., Sullivan, C., Monson, C. M., & Chard, K. M. (2022). Effectiveness of cognitive behavioral conjoint therapy for posttraumatic stress disorder (PTSD) in a U.S. Veterans Affairs PTSD clinic. Journal of Traumatic Stress, 35(2), 644–658. 10.1002/jts.22781 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pukay-Martin, N. D., Torbit, L., Wanklyn, S. G., Shnaider, P., Lane, J. E., & Monson, C. M. (2015). An uncontrolled trial of a present-focused cognitive-behavioral conjoint therapy for posttraumatic stress disorder. Journal of Clinical Psychology, 71(4), 302–312. 10.1002/jclp.22166 [DOI] [PubMed] [Google Scholar]
- Reise, S. P., Ainsworth, A. T., & Haviland, M. G. (2005). Item response theory: Fundamentals, applications, and promise in psychological research. Current Directions in Psychological Science, 14(2), 95–101. 10.1111/j.0963-7214.2005.00342.x [DOI] [Google Scholar]
- Renshaw, K. D., Allen, E. S., Fredman, S. J., Giff, S. T., & Kern, C. (2020). Partners’ motivations for accommodating posttraumatic stress disorder symptoms in service members: The reasons for accommodation of PTSD scale. Journal of Anxiety Disorders, 71, 102199. 10.1016/j.janxdis.2020.102199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reuman, L., & Thompson-Hollands, J. (2020). Family accommodation in PTSD: Proposed considerations and distinctions from the established transdiagnostic literature. Clinical Psychology: Science and Practice, 30(4), 453–464. Advance online publication. 10.1111/cpsp.12375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rotunda, R. J., West, L., & O’Farrell, T. J. (2004). Enabling behavior in a clinical sample of alcohol-dependent clients and their partners. Journal of Substance Abuse Treatment, 26(4), 269–276. 10.1016/j.jsat.2004.01.007 [DOI] [PubMed] [Google Scholar]
- Taft, C. T., Creech, S. K., & Murphy, C. M. (2017). Anger and aggression in PTSD. Current Opinion in Psychology, 14, 67–71. 10.1016/j.copsyc.2016.11.008 [DOI] [PubMed] [Google Scholar]
- Thompson-Hollands, J., Kerns, C. E., Pincus, D. B., & Comer, J. S. (2014). Parental accommodation of child anxiety and related symptoms: Range, impact, and correlates. Journal of Anxiety Disorders, 28(8), 765–773. 10.1016/j.janxdis.2014.09.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson-Hollands, J., Lee, D. J., & Sloan, D. M. (2021). The use of a brief family intervention to reduce dropout among veterans in individual trauma-focused treatment: A randomized controlled trial. Journal of Traumatic Stress, 34(4), 829–839. 10.1002/jts.22680 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weathers, F. W., Litz, B., Herman, D. S., Huska, J., & Keane, T. M. (1993, October). The PTSD checklist: Reliability, validity, & diagnostic utility. Annual meeting of the International Society of Traumatic Stress Studies. [Google Scholar]
- Weathers, F. W., Litz, B. T., Keane, T. M., Palmieri, P. A., Marx, B. P., & Schnurr, P. P. (2013). The PTSD checklist for DSM-5 (PCL-5). www.ptsd.va.gov.
- Weber, D. M., Fischer, M. S., Baucom, D. H., Baucom, B. R. W., Kirby, J. S., Runfola, C. D., Matherne, C. E., & Bulik, C. M. (2019). The association between symptom accommodation and emotional coregulation in couples with binge eating disorder. Family Process, 58(4), 920–935. 10.1111/famp.12391 [DOI] [PubMed] [Google Scholar]
- Wilkins, K. C., Lang, A. J., & Norman, S. B. (2011). Synthesis of the psychometric properties of the PTSD checklist (PCL) military, civilian, and specific versions. Depression and Anxiety, 28(7), 596–606. 10.1002/da.20837 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wirth, R. J., & Edwards, M. C. (2007). Item factor analysis: Current approaches and future directions. Psychological Methods, 12(1), 58–79. 10.1037/1082-989X.12.1.58 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data used in the present study were aggregated across multiple studies/clinical programmes; as a result of differences in the individual Data Use Agreements that govern this aggregation, the data are not available to outside investigators.