Abstract
Background:
Fall occurrences and the associated risk of injury are debilitating and major health concerns in the older population. Several interventions have been investigated and implemented to address the needs of balance impairments and to reduce the increased risk of falls. This study aimed to compare the effectiveness of the Otago exercise program (OEP) and gaze stability exercises (GSE) on balance and the risk of falls in older adults residing at an old age home facility.
Methods:
Thirty elderly participants were equally and randomly divided into 2 groups: Group OEP received the OEP, and group GSE received GSE for 8 weeks (thrice a week). In addition, both groups also performed core muscle-strengthening exercises. The outcome measures were the Berg balance scale (BBS) and the Fall efficacy scale-International (FES-I).
Results:
The interventions resulted in significant improvements (P < .001) in both outcome measures in both groups. The mean pretest BBS scores of groups OEP and GSE increased from 40.4 and 39.2 to the mean post-test scores of 48 and 45.2, respectively. Similarly, the mean pretest FES-I scores of groups OEP and GSE also improved from 39.47 and 40.4 to the mean post-test scores of 32.73 and 36.07. The between-group comparison showed greater improvement (P < .05) in OEP group in both variables.
Conclusions:
OEP and GSE were found to be beneficial rehabilitation programs in improving balance and fear of falls in healthy older adults. However, the OEP was found to be a more effective intervention and may allow better balance and fall prevention improvements.
Trial Registration:
The study has been registered in clinicaltrials.gov (ID: NCT05781776; on 23/03/2023).
Keywords: balance, exercises, falls, older adults, rehabilitation
1. Introduction
Due to the advancement in medical and health sciences, modern civilization has witnessed a tremendous rise in life expectancy in the past 2 centuries. As a result, the older population is also advancing in volume with an increase in life span due to enhanced medical care and improved living standards.[1]
However, with progressive aging, older individuals are commonly subjected to the following complications, reduced muscle mass, strength, bone density, abnormal breathing, a long reaction time, cognitive ability deterioration, and a tendency to fall.[2] Additionally, the progressive loss of movement and balance instability associated with aging can further lead to disability among the older population.[3] Therefore, maintaining a good balance is an essential motor skill that involves integrating sensory input associated with the body’s orientation concerning the surrounding environment with the subsequent ability to respond suitably to maintain body movement control.[4]
Given that the vestibular system plays one of the primary roles in maintaining balance, this system is subjected to degradation as a sequel of aging, resulting in reduced visual VOR (vestibular-ocular reflex) gain. This reduction in VOR gain contributes to the retinal slip (motion of visuals of images on the surface of the retina). Thus, the individual experiences diminished visual acuity during head motion and loss of balance towards body rotation which affects his/her gait.[4,5] The intense training of VOR has been indicated to improve balance and reduce the risk of falls.[6,7]
Although the vestibular system primarily carries the systems that provide sensory information; however, somatosensory and visual systems also play their assigned roles in maintaining balance.[8,9] With aging, there is an impact on balance that has been associated with attritional changes in these sensory structures. Correspondingly, with the age-related changes, any deviations in the standing posture require quick and appropriate corrective strategies to maintain a stable standing balance.[3] In addition, the balance gets further challenged with the simultaneous performance of rapid movements.[10] These changes that yield balance impairments can be accredited to a decline in proprioception, reaction time, muscle strength and power, and impaired sensorimotor integration, which has been shown to increase the possibility of falls and subsequent injuries.[11] Moreover, the incorporation of drugs to cope with other pathological age-related conditions could exacerbate balance and locomotion among the elderly.[12]
Concurrently, balance plays a major role in constituting a high risk of falls and a subsequent reduction in balance confidence.[13] The impact of these psychological changes, the fear of falls and low balance confidence results in lesser autonomy, activity limitations, and community participation restrictions, thereby fostering functional decline and dependence.[14] For individuals aged over 65, falls events are common and are considered a major health concern that causes morbidity, mortality, reduced functioning, and hospitalizations. The risk is multifold to 50% beyond 80 years.[15] By virtue of the injuries associated with falls (such as fractures), they are considered a component of the “geriatric giants” among the older population.[16]
Naturally, older adults adopt a wider gait coupled with reduced walking speed, step length, and muscle strength in the lower extremities. In addition, environmental factors such as poorly illuminated rooms, uneven and textured surfaces, and moving walkways also predispose these individuals to a further risk of falls.[17] Although, the cause of falls is multifactorial, older individuals with postural instability and associated fear of falls are subjected to a greater probability of fall risk.[18]
Therefore, fall prevention amongst the elderly is paramount to prevent short- and long-term impairments in older people as the aftermath of a fall can heavily impact their and their families’ quality of life.[19] To that end, several exercise programs, such as balance training, strengthening programs, and endurance training, have been investigated and adapted by clinicians to evaluate their usefulness in promoting physical fitness and reducing fall risk.[20]
The Otago Exercise Program (OEP) is a multimodal exercises program which was developed by Professor John Campbell at the University of Otago in Dunedin, New Zealand, encompassing all the components necessary to yield improvements in the balance, strength, and functional capacity of the elderly population.[21,22] Additionally, it has also been effective in reducing fall risks among older adults by improving muscle strength performance of the lower extremities and cognitive function.[2,23] The OEP comprises twelve balance exercises and 5 strengthening exercises and has been considered a feasible approach to be utilized as a home-based rehabilitation.[2]
Literature affirms that vestibular rehabilitation is a well-established method to improve balance-related impairments.[24] To counter the impact of exaggerated retinal slip resulting from VOR degradation due to natural aging, gaze stabilization exercises (GSE) were established to minimize retinal slippage[5] GSE aims to foster vestibular adaptation to promote the recovery of vestibular response through the reciprocal interaction between the visual and vestibular systems during head movements.[25] These exercises operate on vestibular adaptation and substitution mechanisms to reduce symptoms by eliciting continuous exposure to sensory inputs.[26] They have gained popularity in improving balance and fear of falls to promote vestibular rehabilitation amongst older individuals.[27]
Earlier studies have investigated both individual and combined effects of the two effective interventions to improve balance and reduce fall risk, however, no study has drawn a comparison between the two.[28–32] Therefore, the present study aimed to compare the effects of GSE vs. the OEP on balance and fear of falls in community-dwelling elderly individuals. The present study hypothesized that there is a significant difference between the effects of OEP and GSE.
2. Methods
2.1. Participants, inclusion, and exclusion criteria
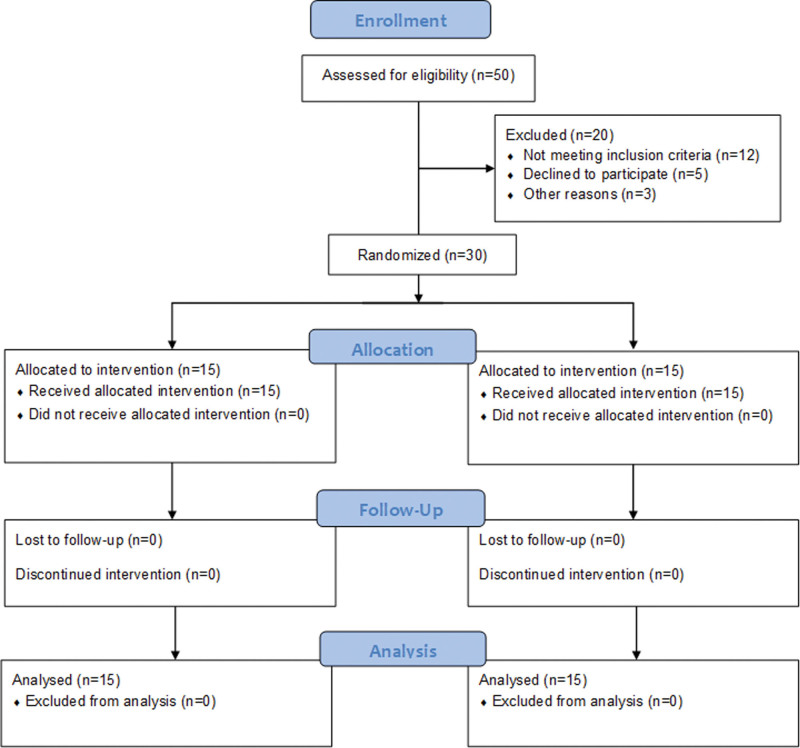
A minimum group size of 30 participants is regarded as necessary for experimental research to draw a valid generalization.[33] Therefore, thirty elderly participants with a risk of fall (both males and females) between the ages 65 to 70 years from Vayojana old age home, Cheruvanchery, were recruited for the study. All the participants were independently ambulating and performing activities of daily living at the time of inclusion into the study. The other inclusion criteria for participation in the study were as follows: Berg Balance Scale (BBS) score between 35 and 45, Dynamic Gait Index score between 11 and 19, and mini-mental status exam scores > 22. Participants with severe vision or hearing impairment, neurological disorders including epilepsy, Alzheimer’s disease, vertigo, Parkinson disease, and stroke, muscular disorders which limit functional activity (OA, RA, etc.), medications that affect balance, severe cardiovascular conditions, recent lower limb injury or surgery, obesity were excluded from the study. Table 1 shows the demographic characteristics of participants, and Figure 1 shows the number of assessed, recruited, randomized, and analyzed participants.
Table 1.
Participants’ demographic characteristics, baseline values of dependent variables, and P values for the Shapiro–Wilk test of normality.
| Characteristics | Group OEP mean ± SD |
P value | Group GSE mean ± SD |
P value |
|---|---|---|---|---|
| Gender (n) | Male: 11; Female: 19 | Male: 13; Female: 17 | ||
| Age (yr) | 67.6 ± 1.81 | 67.47 ± 1.73 | ||
| Height (cm) | 169.33 ± 2.32 | 169.33 ± 2.31 | ||
| Weight (kg) | 67.16 ± 1.39 | 67.66 ± 1.38 | ||
| BMI (kg/m2) | 23.6 ± 0.47 | 23.12 ± 0.54 | ||
| MMSE score (n) | 25.26 ± 2.25 | 24.86 ± 1.96 | ||
| BBS baseline | 40.4 ± 3.14 | .437 | 39.2 ± 3.83 | .372 |
| FES-I baseline | 39.47 ± 3.96 | .741 | 40.4 ± 3.33 | .832 |
BBS = Berg balance scale, BMI = body mass index, FES-I = fall efficacy scale-international, GSE = Gaze stability exercises, OEP = Otago exercise program, SD = standard deviation.
Figure 1.
Consolidated Standards of Reporting Trials (CONSORT) flowchart showing the number of participants assessed for eligibility, randomized, and analyzed during the study.
2.1.1. Ethics approval, consent to participate, study period and clinicaltrial registration
Before the study, the purpose and procedure were explained to the participants, and their written informed consent was obtained. All methods were performed in accordance with the relevant guidelines and regulations. The study received approval from the Institutional Ethical Committee of the Co-operative Institute of Health Sciences (Approval No. MSECO4/2019; Date October 31, 2020), Thalassery, and was conducted in accordance with the declaration of Helsinki. Participants were recruited and followed up from November 2020 to February 2021. The study has been registered in clinicaltrials.gov (ID: NCT05781776; on March 23, 2023). This study adhered to CONSORT guidelines.
2.1.2. Procedure
This clinical trial followed a two-arm pretest-posttest design. All participants were assigned randomly into two intervention groups, group OEP (n = 15) and group GSE (n = 15). An independent researcher not associated with this study performed the process of randomization and allocation of participants. IBM SPSS software version 26 and the lottery method were used for randomization. The outcome assessor was blinded to the allocation. Group OEP was given the OEP and core muscle strengthening exercise, and group GSE was given the GSE and core muscle strengthening exercise. The exercises were performed 3 times per week for 8 weeks. Two assessment tools were utilized to measure the participants’ balance and fear of falling: The BBS and the Fall efficacy scale-international (FES-I), administered before the first intervention and post-study. The study was conducted at the physical therapy laboratory of the Co-operative Institute of Health Sciences, Thalasseri.
2.1.3. Training
2.1.3.1. Otago exercise program (OEP)
OEP consists of strengthening and balance exercises.[34,35] Strengthening of ankle plantar and dorsiflexors, knee extensors and flexors, and hip abductors are focused in this program. Ankle weight cuffs (1–3 kg) provide resistance for hip and knee exercises. The ankle plantar and dorsi flexors were strengthened by performing heel and toe raises. The progression was performed by increasing the duration and then weights.[34,35]
Stair walking, sit-to-stand, heel-to-toe walking backward, toe walking, heel walking, one-leg stands, tandem walking, tandem stance, sideways walking, turning around, walking backward, walking, and knee bends were used for balance exercises. Three levels were used for balance exercises: Level 1 was 2 hands holding on, Level 2 was one hand holding on, and Level 3 was no hands or support. The individuals repeated each exercise 10 times a day over 8 weeks.[34,35]
2.1.3.2. Gaze Stability exercises (GSE)
The exercise protocol in GSE included adaptation exercises and substitution exercises. In adaptation exercises, participants saw a stationary visual target while rotating their heads rapidly. In substitution exercises, with the intention of seeing clearly while performing the task, the subject moved their eyes and heads between targets. The target was moving the other way from the head movement.[31,36]
Adaptation exercises included: In sitting, vertical, and horizontal (stationary target) viewing exercises performed with a near target. Then performed with near and far (6–10 feet) targets. Then vertical and horizontal (stationary target) exercises were performed with near and far targets in standing position.[31,36]
Substitution exercises included: Eye-head movements between near targets (moving target) 4 feet away, horizontal/vertical, sitting. Eye-head movements between near targets (moving target) 4 feet away, horizontal/vertical, standing. The participants performed each of these exercises for 5 repetitions (approximately 30 minutes) 2 times a day (at least 4 hours rest in between) 3 times a week over 8 weeks.[31,36]
2.1.3.3. Core stability exercise
Core stability exercises included bridging, seated marching, straight leg raise, lower trunk rotation, seated oblique crunch, abdominal contraction, and curl-up, which were done in 5 repetitions (approximately 20 minutes), 3 times per week.[37]
2.1.3.4. Outcome measurement
For this study, 2 outcome measures were used to evaluate the impact of the given interventions on the participants: The BBS and the Fall Efficacy Scale-International (FES-I).
The BBS is a widely used functional assessment tool across the continuum of rehabilitation to evaluate functional balance and the risk of falls in elderly clients. This tool encompasses both static and dynamic balance components across 14 different activities (5 static and 9 dynamic) performed by the patient, graded on varying difficulty levels for different balance conditions. The BBS utilizes an ordinal grading on a 5-point scale (0–4) to rate the 14 task items, producing a global score of 56 with the lower score assigned to poor performance (score-0) and a greater score representing the accomplishment of the task independently (score-4).[38,39]
Fall efficacy Scale-International (FES-I) is a questionnaire to evaluate the fear of falls, primarily in community-dwelling older individuals. The FES-I form consists of 16 items related to various functional activities. The participant is asked to rate the level of each activity on a 4-point Likert scale. Through this evaluation, the participant indicates how concerned he was for fear of falling while performing the task regardless of its completion (total score being 64 where 1-not at all concerned and 4-greatly concerned). Therefore, a higher score implies a greater fear of falls.[40,41]
2.1.3.5. Data analysis
Data from thirty participants, fifteen participants in each group, were analyzed. Analysis of data was done by IBM SPSS version 28 (IBM, Armonk, New York, United States). The normality and homogeneity of the data were confirmed by the Shapiro–Wilk test (P > .05) and Levine’s test (P < .05), respectively. Parametric tests were used for with-in and between-group comparisons. A with-in-group comparison was performed using paired sample t test, and the between-group comparison was performed using the independent samples t test. A .05 level of significance was utilized for comparisons, and a significant difference was thought to have been indicated by a P ≤ .05. The confidence interval’s value was set at 95%.
3. Results
Table 1 presents baseline measurements of the dependent variables and the Shapiro–Wilk test of normality P values for both groups. Table 2 presents the BBS and FES-I with-in-group results in both groups.
Table 2.
With-in-group comparison results for groups OEP and GSE.
| Group | Performance tests | Baseline mean ± SD |
Post mean ± SD |
Mean difference | t | df | P value | Cohen d |
|---|---|---|---|---|---|---|---|---|
| OEP | BBS | 40.4 ± 3.14 | 48.0 ± 3.58 | 7.6 | 20.24 | 14 | <.001* | 5.22 |
| FES-I | 39.47 ± 3.96 | 32.73 ± 3.31 | −6.74 | −13.67 | 14 | <.001* | −3.53 | |
| GSE | BBS | 39.2 ± 3.83 | 45.27 ± 3.69 | 6.07 | 17.61 | 14 | <.001* | 4.54 |
| FES-I | 40.4 ± 3.33 | 36.07 ± 3.51 | −4.33 | −20.56 | 14 | <.001* | −5.30 |
BBS = Berg balance scale, df = degree of freedom, FES-I = fall efficacy scale-international, GSE = Gaze stability exercises, OEP = Otago exercise program, SD = standard deviation.
Significant.
Following training, the participants’ mean test scores for both tests in both groups improved significantly (P < .05). The mean pretest BBS scores of groups OEP and GSE increased from 40.4 and 39.2 to the mean post-test scores of 48 and 45.2, respectively. Similarly, the mean pretest FES-I scores of groups OEP and GSE also improved from 39.47 and 40.4 to the mean post-test scores of 32.73 and 36.07. The between-group comparisons revealed a significant improvement in BBS score (t (28) = 2.05; P = .04; Cohen d = 0.75) and FES-I score (t (28) = −2.67; P = .01; Cohen d = −0.97) in the group who performed the OEP along with core muscle strengthening exercise (group OEP). These results are presented in Table 3.
Table 3.
Between-group comparison results of post-intervention values of BBS and FES-I.
| t | df | Mean difference | P value | Cohen d | |
|---|---|---|---|---|---|
| BBS_Post | 2.05 | 28 | 2.73 | .04* | 0.75 |
| FES-I_Post | −2.67 | 28 | −3.33 | .01* | −0.97 |
BBS = Berg balance scale, df = degree of freedom, FES-I = fall efficacy scale-international.
Significant.
4. Discussion
Overall, the study results revealed that the participants in both groups improved on balance and fall efficacy scales; however, those who received OEP along with the core stability training showed higher improvements in balance and reduced fear of falls than those who received GSE with the core stability training regimen. Therefore, the study rejects the null hypothesis and accepts the alternative hypothesis. These results also align with another randomized controlled trial conducted by Abhijeet et al[16] who evaluated the impact of OEP compared with a conventional exercise program on balance in 20 older adults over 6 weeks. The study concluded that OEP was considerably more effective than the conventional rehabilitation protocol and had good adherence in the geriatric population.[4] Similarly, Beato et al[42] examined the efficacy of Otago-based home exercise protocol on reducing falls and the risk of falls in older community dwellers over 4 to 9 weeks. The study demonstrated that OEP effectively reduced the number of reported falls post-intervention. However, the study lacked a control group; therefore, the results cannot be generalized solely to the intervention used.[42]
Similarly, GSE is a commonly adopted rehabilitation strategy that capitalizes on the vestibular system’s innate recovery mechanism (plasticity) through adaptation exercises to minimize retinal slip during head movements.[43] It has been suggested that the magnitude of VOR gained through adaptation exercises is crucial to offset the impact of VOR degeneration following physiological aging.[4] Moreover, the empirical evidence also suggests that rigorous training of VOR along with other treatment protocols can effectively address balance recovery and fall prevention.[6,7] The results of our study are at par with other researchers’ findings which suggest that gaze stability exercises are effective among older adults in improving balance and reducing falls and fear of falls stemming from age-related vestibular deterioration.[4,27,44]
4.1. Clinical significance
The age-related decrements in the cognitive, visionary, somatosensory, vestibular, and musculoskeletal functions can significantly render balance and mobility deficits in the elderly, thereby increasing the risk of falls and promoting excessive dependence.[45,46] The OEP is considered an effective home-based program to improve psychological and individual well-being and community participation in homebound individuals or those who cannot afford regular clinical visits, particularly in rural areas. Data suggests that even short-term training through OEP has slight benefits in older adults with a history of falls, yet it can improve physical performance in those individuals. Therefore, clinicians must strive to promote adherence and persistence to accomplish long-term, substantial benefits, particularly in those who have experienced falls.
4.2. Limitations
There are a few limitations to this study. The study’s sample size was small, and fewer male participants were involved in the study. Additionally, the study duration was only 2 months, and the follow-up could not be established; thus, the long-term benefits of the interventions could not be evaluated. Further investigations are recommended to assess the longstanding efficiency of OEP through large-scale clinical trials focusing on individuals who have experienced falls in the past or those with apparent vestibular deficits.
5. Conclusion
The OEP and GSE were found to be beneficial rehabilitation programs in improving balance and reducing the fear of falls in healthy older adults. However, OEP was found to be a more effective intervention than GSE in improving balance and preventing falls.
Acknowledgments
The authors extend their appreciation to the Deanship of Scientific Research, King Saud University for funding through Vice Deanship of Scientific Research Chairs; Rehabilitation Research Chair.
Author contributions
Conceptualization: Nimmi KP, Anjupriya D, Shibili Nuhmani, Masood Khan.
Data curation: Anjupriya D, Shibili Nuhmani.
Formal analysis: Nimmi KP.
Funding acquisition: Ahmad H. Alghadir.
Investigation: Anjupriya D.
Methodology: Nimmi KP, Masood Khan.
Project administration: Alvina Nawed, Ahmad H. Alghadir.
Resources: Alvina Nawed, Ahmad H. Alghadir.
Software: Ahmad H. Alghadir.
Supervision: Anjupriya D, Alvina Nawed, Shibili Nuhmani, Ahmad H. Alghadir.
Validation: Alvina Nawed, Shibili Nuhmani, Ahmad H. Alghadir.
Visualization: Alvina Nawed, Shibili Nuhmani, Masood Khan, Ahmad H. Alghadir.
Writing – original draft: Nimmi KP, Anjupriya D.
Writing – review & editing: Nimmi KP, Alvina Nawed, Shibili Nuhmani, Masood Khan, Ahmad H. Alghadir.
Abbreviations:
- BBS
- Berg balance scale
- FES-I
- fall efficacy scale-international
- GSE
- Gaze stability exercises
- OEP
- Otago exercise program
- VOR
- vestibulo-ocular reflex
This study was funded by King Saud University, Deanship of Scientific Research, Vice Deanship of Scientific Research Chairs; Rehabilitation Research Chair.
The authors have no conflicts of interest to disclose.
The datasets generated during and/or analyzed during the current study are not publicly available, but are available from the corresponding author on reasonable request.
How to cite this article: KP N, D A, Nawed A, Nuhmani S, Khan M, Alghadir AH. Comparison of effects of Otago exercise program vs gaze stability exercise on balance and fear of fall in older adults: A randomized trial. Medicine 2024;103:23(e38345).
Contributor Information
Nimmi KP, Email: nimmikpchandran@gmail.com.
Anjupriya D, Email: anjupriya4@gmail.com.
Alvina Nawed, Email: alvinanawed1818@gmail.com.
Shibili Nuhmani, Email: snuhmani@iau.edu.sa.
Ahmad H. Alghadir, Email: aalghadir@hotmail.com.
References
- [1].Oeppen J, Vaupel JW. Broken limits to life expectancy. Science. 2002;296:1029–31. [DOI] [PubMed] [Google Scholar]
- [2].Yang Y, Wang K, Liu H, et al. The impact of Otago exercise programme on the prevention of falls in older adult: a systematic review. Front Public Health. 2022;10:953593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Arzhane SSD, Hazrati M, Ashraf A. The effect of Otago exercise program training on balance and fear of falling in elderly individuals. 2019.
- [4].Bhardwaj V, Vats M. Effectiveness of gaze stability exercise on balance in healthy elderly population. Int J Physiother Res. 2014;2:642–7. [Google Scholar]
- [5].Herdman SJ. Role of vestibular adaptation in vestibular rehabilitation. Otolaryngol Head Neck Surg. 1998;119:49–54. [DOI] [PubMed] [Google Scholar]
- [6].Gardner MM, Buchner DM, Robertson MC, Campbell AJ. Practical implementation of an exercise-based falls prevention programme. Age Ageing. 2001;30:77–83. [DOI] [PubMed] [Google Scholar]
- [7].Simoceli L, Bittar RSM, Sznifer J. Adaptation exercises of vestibulo-ocular reflex on balance in the elderly. J Otolaryngol World. 2008;12:183–8. [Google Scholar]
- [8].Horak FB, Henry SM, Shumway-Cook A. Postural perturbations: new insights for treatment of balance disorders. Phys Ther. 1997;77:517–33. [DOI] [PubMed] [Google Scholar]
- [9].Woollacott MH. Systems contributing to balance disorders in older adults. J Gerontol A Biol Sci Med Sci. 2000;55:M424–8. [DOI] [PubMed] [Google Scholar]
- [10].Ganz DA, Bao Y, Shekelle PG, Rubenstein LZ. Will my patient fall? JAMA. 2007;297:77–86. [DOI] [PubMed] [Google Scholar]
- [11].Sturnieks DL, St George R, Lord SR. Balance disorders in the elderly. Neurophysiol Clin. 2008;38:467–78. [DOI] [PubMed] [Google Scholar]
- [12].Rose J, Gamble JG. Human Walking. Lippincott Williams & Wilkins; 2006. [Google Scholar]
- [13].Makino K, Makizako H, Doi T, et al. Fear of falling and gait parameters in older adults with and without fall history. Geriatr Gerontol Int. 2017;17:2455–9. [DOI] [PubMed] [Google Scholar]
- [14].Hartholt KA, van Beeck EF, Polinder S, et al. Societal consequences of falls in the older population: injuries, healthcare costs, and long-term reduced quality of life. J Trauma. 2011;71:748–53. [DOI] [PubMed] [Google Scholar]
- [15].Gardner MM, Robertson MC, Campbell AJ. Exercise in preventing falls and fall related injuries in older people: a review of randomised controlled trials. Br J Sports Med. 2000;34:7–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Manohare A, Hande D. Effect of 6 weeks Otago exercise program on balance in older adults. Int J Curr Adv Res. 2019;8:17784–8. [Google Scholar]
- [17].Appeadu MK, Bordoni B. Falls and fall prevention in the elderly. StatPearls. StatPearls Publishing; 2023. [PubMed] [Google Scholar]
- [18].Pua Y-H, Ong P-H, Clark RA, Matcher DB, Lim EC-W. Falls efficacy, postural balance, and risk for falls in older adults with falls-related emergency department visits: prospective cohort study. BMC Geriatr. 2017;17:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Dietscher C, Pelikan J, Bobek J, Nowak P, Organization WH. The Action Network on Measuring Population and Organizational Health Literacy (M-POHL): a network under the umbrella of the WHO European Health Information Initiative (EHII). Public Health Panorama. 2019;5:65–71. [Google Scholar]
- [20].Sherrington C, Tiedemann A, Fairhall N, Close JC, Lord SR. Exercise to prevent falls in older adults: an updated meta-analysis and best practice recommendations. NSW Public Health Bull. 2011;22:78–83. [DOI] [PubMed] [Google Scholar]
- [21].Kocic M, Stojanovic Z, Nikolic D, et al. The effectiveness of group Otago exercise program on physical function in nursing home residents older than 65 years: a randomized controlled trial. Arch Gerontol Geriatr. 2018;75:112–8. [DOI] [PubMed] [Google Scholar]
- [22].Chiu H-L, Yeh T-T, Lo Y-T, Liang P-J, Lee S-C. The effects of the Otago exercise programme on actual and perceived balance in older adults: a meta-analysis. PLoS One. 2021;16:e0255780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Shubert TE, Smith ML, Jiang L, Ory MG. Disseminating the Otago exercise program in the United States: perceived and actual physical performance improvements from participants. J Appl Gerontol. 2018;37:79–98. [DOI] [PubMed] [Google Scholar]
- [24].Felipe L, Hunnicutt S. Virtual reality as a vestibular rehabilitation tool for athletes after concussion: a literature review. Adv Rehabil. 2020;34:42–8. [Google Scholar]
- [25].Shelhamer M, Tiliket C, Roberts D, Kramer PD, Zee DS. Short-term vestibulo-ocular reflex adaptation in humans: II. Error signals. Exp Brain Res. 1994;100:328–36. [DOI] [PubMed] [Google Scholar]
- [26].Fatima SN, Tanveer F, Shoukat F, Ahmad A, Siddique K. Effects of balance training with and without gaze stabilization exercises on clinical outcomes in elderly patients with chronic dizziness: a randomized controlled trial. J Bodyw Mov Ther. 2022;32:46–50. [DOI] [PubMed] [Google Scholar]
- [27].Porciuncula F, Johnson CC, Glickman LB. The effect of vestibular rehabilitation on adults with bilateral vestibular hypofunction: a systematic review. J Vestib Res. 2012;22:283–98. [DOI] [PubMed] [Google Scholar]
- [28].Martins AC, Santos C, Silva C, Baltazar D, Moreira J, Tavares N. Does modified Otago exercise program improves balance in older people? A systematic review. Prev Med Rep. 2018;11:231–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Patel NN, Pachpute S. The effects of Otago exercise programme for fall prevention in elderly people. Int J Physiother. 2015;2:633–9. [Google Scholar]
- [30].Khanna T, Singh S. Effect of gaze stability exercises on balance in elderly. J Dental Med Sci. 2014;13:41–8. [Google Scholar]
- [31].Correia A, Pimenta C, Alves M, Virella D. Better balance: a randomised controlled trial of oculomotor and gaze stability exercises to reduce risk of falling after stroke. Clin Rehabil. 2021;35:213–21. [DOI] [PubMed] [Google Scholar]
- [32].Vincent S, Joseph J. The combined effectiveness of gaze stability exercise and Otago exercise on balance and fall risk in elderly people. Int J Med Exerc Sci. 2017;03:390–401. [Google Scholar]
- [33].Kraemer HC, Blasey C. How Many Subjects? Statistical Power Analysis in Research. Sage Publications; 2015. [Google Scholar]
- [34].Kyrdalen IL, Moen K, Røysland AS, Helbostad JL. The Otago exercise program performed as group training versus home training in fall-prone older people: a randomized controlled trial. Physiother Res Int. 2014;19:108–16. [DOI] [PubMed] [Google Scholar]
- [35].Shubert TE, Smith ML, Goto L, Jiang L, Ory MG. Otago exercise program in the United States: comparison of 2 implementation models. Phys Ther. 2017;97:187–97. [DOI] [PubMed] [Google Scholar]
- [36].Hall CD, Heusel-Gillig L, Tusa RJ, Herdman SJ. Efficacy of gaze stability exercises in older adults with dizziness. J Neurol Phys Ther. 2010;34:64–9. [DOI] [PubMed] [Google Scholar]
- [37].Sadeghi H, Shojaedin SS, Alijanpour E, Abbasi A. The effects of core stability exercises on balance and walking in elderly fallers with mild cognitive impairment: a randomized control trial. J Res Rehabil Sci. 2020;16:110–7. [Google Scholar]
- [38].Miranda-Cantellops N, Tiu TK. Berg balance testing. 2021. [PubMed]
- [39].Pickenbrock HM, Diel A, Zapf A. A comparison between the Static Balance Test and the Berg Balance Scale: validity, reliability, and comparative resource use. Clin Rehabil. 2016;30:288–93. [DOI] [PubMed] [Google Scholar]
- [40].Dewan N, MacDermid JC. Fall efficacy scale-international (FES-I). J Physiother. 2014;60:60–60. [DOI] [PubMed] [Google Scholar]
- [41].Yardley L, Beyer N, Hauer K, Kempen G, Piot-Ziegler C, Todd C. Development and initial validation of the Falls Efficacy Scale-International (FES-I). Age Ageing. 2005;34:614–9. [DOI] [PubMed] [Google Scholar]
- [42].Beato M, Dawson N, Svien L, Wharton T. Examining the effects of an Otago-based home exercise program on falls and fall risks in an assisted living facility. J Geriatr Phys Ther. 2019;42:224–9. [DOI] [PubMed] [Google Scholar]
- [43].Herdman S. Exercise strategies for vestibular disorders. Ear Nose Throat J. 1989;68:961–4. [PubMed] [Google Scholar]
- [44].Mossman B, Mossman S, Purdie G, Schneider E. Age dependent normal horizontal VOR gain of head impulse test as measured with video-oculography. J Otolaryngol Head Neck Surg. 2015;44:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Shaffer SW, Harrison AL. Aging of the somatosensory system: a translational perspective. Phys Ther. 2007;87:193–207. [DOI] [PubMed] [Google Scholar]
- [46].Wolfson L, Whipple R, Derby C, et al. A dynamic posturography study of balance in healthy elderly. Neurology. 1992;42:2069. [DOI] [PubMed] [Google Scholar]