Abstract
Empirical evidence demonstrates that publicly funded adult health insurance through the Affordable Care Act (ACA) has had positive effects on low-income adults. We examine whether the ACA’s Medicaid expansions influenced child development and family functioning in low-income households. We use a difference-in-differences framework exploiting cross-state policy variation and focusing on children in low-income families from a nationally representative, longitudinal sample followed from kindergarten to fifth grade. The ACA Medicaid expansions improved children’s reading test scores by approximately 2 percent (0.04 SD). Potential mechanisms for these effects within families are more time spent reading at home, less parental help with homework, and eating dinner together. We find no effects on children’s math test scores or socioemotional skills.
Keywords: academic achievement, socioemotional skills, low-income, health insurance, Affordable Care Act, Medicaid
JEL codes: J13, I13, I18
1. INTRODUCTION
One of the largest expansions to the social safety net in recent years was increased public funding for adult health insurance coverage with the passage of the Patient Protection and Affordable Care Act (ACA) in 2010. As part of the law, federal funds were provided to states to expand Medicaid coverage to nonelderly, non-disabled adults with incomes below 138% of the federal poverty line (FPL). As a result, uninsured rates among parents dropped from 18% in 2013 to 11% in 2017 (Haley et al., 2019).
The effect of the Medicaid expansions on adults has been studied extensively, with evidence that the expansions improved adults’ economic stability, housing and food security, and physical and mental health (see Glied et al., 2020, Mazurenko et al., 2018, and Soni et al., 2020 for reviews). Although coverage was not expanded for children, theoretical and empirical evidence suggests that health insurance coverage for parents may have positive benefits for children’s academic and socioemotional development through multiple indirect mechanisms, including reductions in parenting stress and more consistent family routines (Burak, 2019; Gassman-Pines & Hill, 2013; Morrissey, 2012). Further, increased awareness of children’s eligibility for health insurance coverage and access to health care for children may exert more direct influences on children’s well-being (Cohodes et al., 2016; De La Mata, 2012; Qureshi & Gangopadhyaya, 2021).
In this study, we address two related questions. First, did the ACA’s Medicaid expansions to low-income adults, including parents, affect children’s academic achievement and socioemotional skill development? Second, did any impacts on child development occur through changes in family functioning? To answer these questions, we use longitudinal data on a representative sample of children from the 2010–2011 Early Childhood Longitudinal Study-Kindergarten Cohort (ECLS-K:2011). We study a subsample of households in which adults likely became eligible for Medicaid based upon pre-Medicaid expansion household income. We then compare children in states that expanded Medicaid to states that did not expand Medicaid using a difference-in-differences (DD) research design. With longitudinal data, we are able to adjust for within-household factors, isolating the effects of Medicaid expansion. We focus on broad domains of children’s academic achievement and socioemotional skill development, covering reading and math achievement, ability to relate with adults and peers (social skills), and mental health symptoms (externalizing and internalizing behaviors). To identify potential mechanisms by which adult eligibility for health insurance from the expansions may have influenced child development, we also examine family functioning, with measures of parenting behaviors and routines. The results provide the first piece of evidence on the extent to which expansions in publicly funded health insurance for adults may extend to children’s development during middle childhood.
We find the ACA Medicaid expansions improved children’s reading test scores by approximately 2% within two years of expansion. We find no significant effects for children’s math test scores or socioemotional skills. Potential mechanisms for these effects are increases in the amount of time children spend reading at home, by about 14%, and frequency of eating dinner as a family, by about 2.5%. We also found reductions in how frequently parents helped their children with homework every week (about 8%). Results are robust to a variety of sensitivity analyses. For example, among a sample of children from high-income households, we find no significant effects on academic achievement. We also examine a more precise subset of households in states that expanded – those between each state’s pre-ACA parental eligibility income thresholds and 138% FPL – and the impacts are larger.
We make several contributions to the literature. First, we examine the causal impact of public health insurance for low-income adults on children’s academic and socioemotional development. By studying changes in children’s academic achievement and socioemotional skill development between states that expanded Medicaid through the ACA and those that did not in a nationally representative sample, we are able to identify plausibly causal effects through the quasi-experimental nature of the expansion implementation. Second, by exploiting longitudinal data on children and their families, we can adjust for time-invariant child- and family-level factors that may predict outcomes. Third, we limit the analytic sample to children in households most likely to be affected by the public health insurance expansions based on pre-ACA household income. Finally, we explore several potential mechanisms by examining parenting behaviors and routines. In sum, this study adds to a growing literature examining the role of policies beyond traditional education policies that show potential to improve children’s educational and developmental outcomes.
2. BACKGROUND
2.1. Impacts of the ACA Medicaid Expansions on Adults
Robust empirical evidence has documented the positive impacts of the ACA Medicaid expansions on adults across two domains of well-being that may indirectly benefit children. First, the ACA Medicaid expansions improved adults’ health. For example, the expansion increased adults’ health insurance coverage, access to healthcare, and preventive healthcare (Courtemanche et al., 2017; Johnston et al., 2018; Kaestner et al. 2017; McMorrow et al., 2017; Miller & Wherry, 2017; Simon et al., 2017; Sommers et al., 2015; Soni et al., 2020; Wehby et al., 2018; Wherry & Miller, 2016). Although the effects on self-assessed health and health behaviors are mixed (Cotti et al., 2019; Courtemanche et al., 2018a, 2018b, 2019; McMorrow et al., 2017; Simon et al., 2017; Sommers et al., 2015), mortality has declined, driven by fewer disease-related and other health conditions amenable to gaining health insurance such as diabetes (Borgschulte & Vogler, 2020; Goldin et al., 2019; Miller et al., 2019; Sommers et al., 2012). The expansions were also linked with improvements in behavioral health and health care utilization, documented through increased use of substance abuse treatments (Grooms & Ortega, 2019; Maclean & Saloner, 2019; Meinhofer & Witman, 2018), and reductions in both violent and property crime (He & Barkowski, 2020; Vogler, 2020). Though most of the literature focuses on adults without dependent children, gaining access to health insurance among parents has also been found to reduce parents’ psychological distress (McMorrow et al., 2017).
Second, a growing literature has demonstrated substantial effects of the ACA Medicaid expansions on the economic well-being of low-income adults (Glied et al., 2020). For example, the expansions reduced out-of-pocket medical expenses (Abramowitz, 2020), medical bills (Miller et al., 2018), and debt (Brevoort et al., 2017). The expansions were also found to improve child support payments (Bullinger, 2020), suggesting that even for “childless adults” (i.e., those without dependent children, but who may be responsible for paying child support) gaining health insurance may have affected children. Finally, the ACA Medicaid expansions improved housing and food security (Allen et al, 2019; Himmelstein, 2019; Zewde et al. 2019). These improvements in financial well-being have been documented among low-income parents, in particular (Wisk et al., 2020; McMorrow et al., 2017). Taken together, these studies show that low-income households, including those with children, have benefited economically from the Medicaid expansions.
2.2. Mechanisms Linking Parental Health and Financial Well-being to Children’s Development
Theoretical models posit that improvements to parents’ health and economic well-being may indirectly influence children through reduced parenting stress, increased parenting time, and more consistent family routines (Becker, 1993; Bradley & Corwyn, 2004; Conger et al., 1997; Fiese & Schwartz, 2008; Yeung et al., 2002). For example, a higher family income improves families’ ability to buffer stressful or unexpected situations, create routines, spend time with children, and navigate family relationships (Bradley & Corwyn, 2004; Corak, 2013; Fiese & Schwartz, 2008; Yeung et al., 2002). Parents’ physical and psychological health also have indirect benefits for children’s development in that the choices parents make regarding their childrearing is in part determined by their own health (Case & Paxson, 2002). If parents are more stressed, anxious, or depressed they may be more likely to exhibit less sensitive, warm, or consistent parenting practices, thereby adversely impacting children’s development (Conger et al., 1997). Indeed, there is a strong evidence base linking social policies, including the Earned Income Tax Credit, food assistance, public health insurance, and childcare subsidies, to child development through family functioning and income (Burak, 2019; Gassman-Pines & Hill, 2013).
In addition to these indirect pathways, there is evidence that Medicaid expansions for adults spillover onto children’s health insurance coverage through increased awareness of children’s eligibility for Medicaid coverage. For example, Medicaid expansions for adults during the 1990s and early 2000s substantially increased Medicaid enrollment among children (Hamersma et al., 2019). More recently, in addition to parents gaining coverage through the ACA Medicaid expansions, health insurance coverage of low-income children increased (Hudson & Moriya, 2017) and children’s uninsurance rates dropped (Ugwi et al., 2019). These “welcome mat” effects are the result of spillovers from parents who became newly eligible for Medicaid under the ACA and then enroll their children in Medicaid coverage as well.
On this note, Medicaid coverage for children has both short- and long-term benefits for those children. In the short-term, children benefit through increased preventative health care (De La Mata, 2012), including vaccines (Joyce & Racine, 2005), as well as access to mental and behavioral health care. As one example with distinct implications for academic performance, children without health insurance coverage are less likely to be diagnosed with attention-deficit/hyperactivity disorder (ADHD) and receive proper ADHD treatment, suggesting unmet treatment needs (Morgan, et al., 2013). Relative to children with private health insurance, children with Medicaid are more likely to be diagnosed with ADHD potentially suggesting that Medicaid coverage may facilitate medical care and lead to ADHD diagnosis and treatment (Morrill, 2018).
There is also a growing literature providing evidence of long-term impacts on children, extending to children’s educational and economic outcomes in adulthood. For example, Medicaid access during childhood has had long-run improvements on schooling (Cohodes et al., 2016), mortality (Goodman-Bacon, 2018), health (Boudreaux et al., 2016), and wages (Brown et al., 2015), all measured in adulthood. The benefits have even extended to these children’s offspring in the form of healthier birth outcomes (East et al., 2019). Given this research on the long-term effects, there are also likely short-run effects on children’s development that are understudied.
In sum, there are multiple direct and indirect pathways through which adult health insurance may influence children’s academic achievement and socioemotional functioning. Drawing upon the robust literature finding positive impacts on adults, combined with theoretical and empirical evidence on the mechanisms through which social policy may influence children (Burak, 2019; Gassman-Pines & Hill, 2013), parental insurance eligibility may affect children through child receipt of health insurance as well as changes in family functioning.
3.0. METHODS
3.1. Data
Data come from the 2010–2011 Early Childhood Longitudinal Study-Kindergarten Cohort (ECLS-K:2011). Sponsored by the National Center for Educational Statistics (NCES), the ECLS-K:2011 is a nationally representative sample of children who attended kindergarten in the United States during the 2010–2011 academic year. From 90 groups of counties, 950 public and private schools were selected for inclusion in the ECLS-K sample. From these schools, approximately 18,170 kindergarten students were enrolled in the study. Data were collected on children, their families, and their teachers in the fall and spring of kindergarten (2010–2011), first grade (2011–2012), second grade (2012–2013), and then annually each spring through fifth grade (2016) for a total of 9 waves of data collection. However, in waves 3 (fall 2011) and 5 (fall 2012), only a subset of children (about one-third of the full sample, also referred to as the fall subsample) were interviewed. We do not include data from those waves to ensure consistency across our longitudinal sample. In all, we use data primarily from 7 waves that follow the full sample of children. Children were approximately 5.5 years old at the first data collection.
3.2. Sample
The analytic sample is comprised of children from low-income families who were eligible for the direct child assessments, had complete data on household income and the outcomes variables, and did not move across state lines during the study period (see Figure S1 for details on the sample construction). Briefly, in the spring of 2013, which was one year prior to the ACA Medicaid expansions, parents reported their household income level and household size from the prior year. We limit the sample to children in households with incomes below 138% of the FPL1 before the ACA to obtain a sample of those likely to have become newly eligible for Medicaid through the ACA expansions. We drop a small number of children (n = 30) that move across states to ensure that exposure to state-level health insurance expansions was captured accurately in the longitudinal models. We also make sample exclusions to account for missing values on key variables (household income, state identifiers), and use sampling weights to account for the complex survey design, non-response, and attrition over the waves, resulting in an analytic sample of about 2,500 children across models. Thus, the results are generalizable to children in low-income households who attended kindergarten in the U.S. in fall 2010.
3.3. Measures
3.3.1. Children’s academic achievement.
Children’s academic achievement was assessed at each wave using standardized assessments of children’s reading and math achievement. Based on the 2009 NAEP Reading Framework, the reading assessment was an untimed item response theory (IRT)-scaled assessment with strong psychometric properties (αavg. = .95) capturing children’s basic reading skills, such as letter recognition, as well as more advanced skills in vocabulary knowledge and reading comprehension (Tourangeau et al., 2018). Children’s math achievement was a measure of conceptual knowledge, procedural knowledge, and problem solving, capturing children’s understanding of numerical properties and operations, measurement, spatial and geometry skills, data and statistical analysis, and algebraic knowledge. The assessment was based on the 1996 NAEP Mathematics Frameworks and, similar to the reading assessment was an untimed, IRT-scaled assessment with excellent psychometric properties (αavg. = .93; Tourangeau et al., 2018).
3.3.2. Children’s socioemotional skills.
Children’s socioemotional skills were assessed at each wave using teacher reports on questionnaire items adapted from the Social Skills Rating System (SSRS), a commonly used and validated set of measures assessing children’s externalizing problems, internalizing problems, and social skills (Gresham & Elliott, 1990). Teachers responded to each item on a 4-point Likert scale (0 = never to 3 = very often). Within each construct, items were averaged to create a composite. Higher values indicated greater social skills (αavg = .85), externalizing problems (αavg = .80), and internalizing problems (αavg = .75).
3.3.3. Family functioning.
We use three measures to assess aspects of family functioning that have been shown in prior research to be related to children’s development within low-income families (Becker et al., 1993; Bradley & Corwyn, 2004; Conger et al., 1997; Duncan et al., 2019; Elliott & Bachman, 2018; Hill & Tyson, 2009; Longo et al., 2017; Sénéchal & LeFevre, 2002; Votruba-Drzal, 2006). At each wave, parents reported the number of minutes per week their child spent reading outside of school, number of days per week they eat dinner with their child, ranging from 0 to 7, and the number of times per week parents helped them with their homework (1 = Never; 2 = Less than once a week; 3 = 1–2 times a week; 4 = 3–4 times a week; 5 = 5 or more times a week).2 We converted the categorical homework help variable to a continuous scale by imputing the mid-point of the provided category for each wave (0 = Never; 0.5 = Less than once a week; 1.5 = 1–2 times a week; 3.5 = 3–4 times a week; and 5 = 5 or more times a week). For ease of interpretation, we created a binary measure to capture eating dinner together (1= 4 or more days a week; 0 = Fewer than 4 days a week).3
3.3.4. Child and family characteristics.
When relevant, we consider individual-level and family-level covariates; specifically, indicators for children’s sex and race/ethnicity, children’s age in months, age in years of the oldest parent, and indicators for a high school degree among at least one parent. Because we primarily rely on models that included child fixed effects, however, we omit all time-invariant characteristics from the final model specifications. Descriptive statistics of selected time-invariant child and family characteristics in our analytic sample are shown in Table 1 to contextualize the nature of the sample.
Table 1.
Descriptive Statistics of Children in Low-Income Households (< 138% FPL)
| All States | Non-Expansion States | Expansion States | |||
|---|---|---|---|---|---|
|
| |||||
| N a | Mean | SD | Mean | Mean | |
| Academic Outcomes | |||||
| Reading scores | 26,300 | 94.782 | 31.251 | 93.755 | 95.765 |
| Math scores | 26,280 | 75.618 | 32.209 | 74.224 | 76.953 |
|
Socioemotional Outcomes | |||||
| Externalizing problems | 23,680 | 1.711 | 0.648 | 1.709 | 1.713 |
| Internalizing problems | 23,440 | 1.593 | 0.548 | 1.577 | 1.609 |
| Social skills | 23,110 | 3.018 | 0.665 | 3.030 | 3.005 |
|
Family Functioning | |||||
| # of minutes reading outside school | 16,320 | 23.274 | 16.680 | 23.093 | 23.449 |
| # times/week parent helps with homework | 13,180 | 2.929 | 1.599 | 2.940 | 2.919 |
| # of days/week parent eats dinner with child | 16,510 | 5.765 | 1.818 | 5.744 | 5.787 |
|
Family and Child Characteristics | |||||
| Male | 26,900 | 0.514 | 0.499 | 0.522 | 0.506 |
| Black | 26,900 | 0.159 | 0.366 | 0.226 | 0.096 |
| Hispanic | 26,900 | 0.466 | 0.498 | 0.430 | 0.500 |
| White | 26,900 | 0.252 | 0.434 | 0.265 | 0.239 |
| Child age (in months) | 26,900 | 96.723 | 22.506 | 96.514 | 96.922 |
| Parent age (in years) | 26,900 | 32.067 | 7.752 | 31.696 | 32.474 |
| Parent has high school diploma or more | 26,900 | 0.328 | 0.469 | 0.331 | 0.323 |
|
Time-varying State Characteristics | |||||
| Unemployment rate | 26,900 | 7.331 | 2.163 | 6.849 | 7.789 |
| EITC rate | 26,900 | 0.073 | 0.154 | 0.020 | 0.123 |
| TANF/SNAP max. benefits for family of 3 ($) | 26,900 | 942.504 | 183.460 | 809.002 | 1069.16 |
| Minimum wage | 26,900 | 7.615 | 0.792 | 7.208 | 8.002 |
Notes: Means and SDs are unweighted. The difference between expansion and non-expansion states is statistically significant at p < .05 for all variables except externalizing problems, reading time outside school, and eating dinner together.
Sample sizes (in child-years) are rounded to the nearest 10 as per dataset guidelines.
3.3.5. State characteristics.
Finally, we include time-varying characteristics of states that may differentially affect our key outcome measures in households across states, and may also be correlated with state decisions to expand Medicaid. For example, there are differences in the post-2010 economic recovery across states that may be correlated with both Medicaid expansion and child development. We include the following characteristics: state unemployment rates, state Earned Income Tax Credit (EITC) rates, state minimum wages, and the maximum Temporary Assistance for Needy Family (TANF) and Supplemental Nutrition Assistance Program (SNAP) combined benefits for a family of three at the state-year level.
3.4. Analytical Approach
The ACA originally required all states to expand Medicaid. However, in 2012, the Supreme Court allowed states to opt out of this requirement. By the end of 2015, 31 states plus Washington, D.C. had expanded Medicaid, with most states expanding in 2014. Due to ECLS-K:2011’s clustered sampling framework, there were no children sampled from 10 states. Twenty-five expansion states and 16 non-expansion states remain. Table S1 shows details of states’ expansion decisions and our coding schematic.
We use the variation in the ACA Medicaid expansions to identify the effect of adult Medicaid eligibility on children’s academic achievement and socioemotional skills, and families’ functioning. We estimate a series of difference-in-differences models, in which we compared the developmental trajectory of each child and family outcome before the Medicaid expansion (fall 2010 through spring 2013, when children entered kindergarten through the spring of second grade) and after the expansion in January 2014 (spring 2014 through spring 2016, when children were in third through fifth grades) between the expansion and non-expansion states. Specifically, we estimate the following baseline model:
| (1) |
Where Y is the child or family outcome. Expansionst is a binary variable equal to 1 if child i lives in state s that expanded Medicaid during time t, and zero otherwise. The parameter of interest is , which represents the effect of the ACA Medicaid expansion. Although some states expanded before 2014, early expanders are treated as if they expanded in 2014 since there is evidence of a welcome mat effect in 2014 (Courtemanche et al., 2016; Frean et al., 2017) and some of these states only partially expanded early (Sommers et al., 2013). Models include child and wave fixed effects, and the time-varying state-level covariates described earlier. The inclusion of child fixed effects captured all time-invariant factors related to a child’s development, such as constant family characteristics and unobservable features. Because the analytic sample only included children who did not move across states during the study period, state fixed effects (δs) and all time-invariant child- and family-characteristics (Xi) were subsumed by the child fixed effects, (αi), in these models. All statistical analyses were weighted to adjust for sampling procedures, nonresponse, differential attrition, and standard errors were clustered at the state level (Bertrand et al., 2004).
4. RESULTS
4.1. Descriptive Statistics
Table 1 presents descriptive statistics of the analytic sample including the number of observations, means, and standard deviations for the key variables. Summary statistics are pooled across all waves for the roughly 2,500 children included in the analytic sample. The last two columns compare the mean between states that expanded Medicaid versus those that did not. Children from low-income households in states that expanded Medicaid, on average, had higher math and reading scores, fewer internalizing problems, and greater social skills in comparison to children in states that did not expand Medicaid. Differences in levels across these groups of states before the ACA expansions were implemented are not a problem for the difference-in-differences approach we employ, as this approach relies on changes in trends across these two groups to isolate the effects of the policy.
The main identification assumption is that, absent the ACA Medicaid expansions for low-income adults, outcomes for children and families in both the expansion and non-expansion states would have continued on the same trends despite differing average levels. Figure 1 visually presents trends in our outcomes of interest by state expansion status both before and after the ACA expansion in 2014. As expected, we observed common trends in the growth trajectories for all children and families in our analytic sample. We also formally tested if there were statistically significant differences in linear trends between the growth trajectories of children from low-income households residing in expansion and non-expansion states during the pre-expansion time-period for our primary outcomes of interest. We use a regression-adjusted model interacting a linear wave-term with the state expansion status for pre-expansion years and find that they hold with the exception of children’s math scores and eating dinner together, lending credibility to our identification strategy (see Appendix Table S2).
Figure 1. Raw Trends in Variables of Interest.
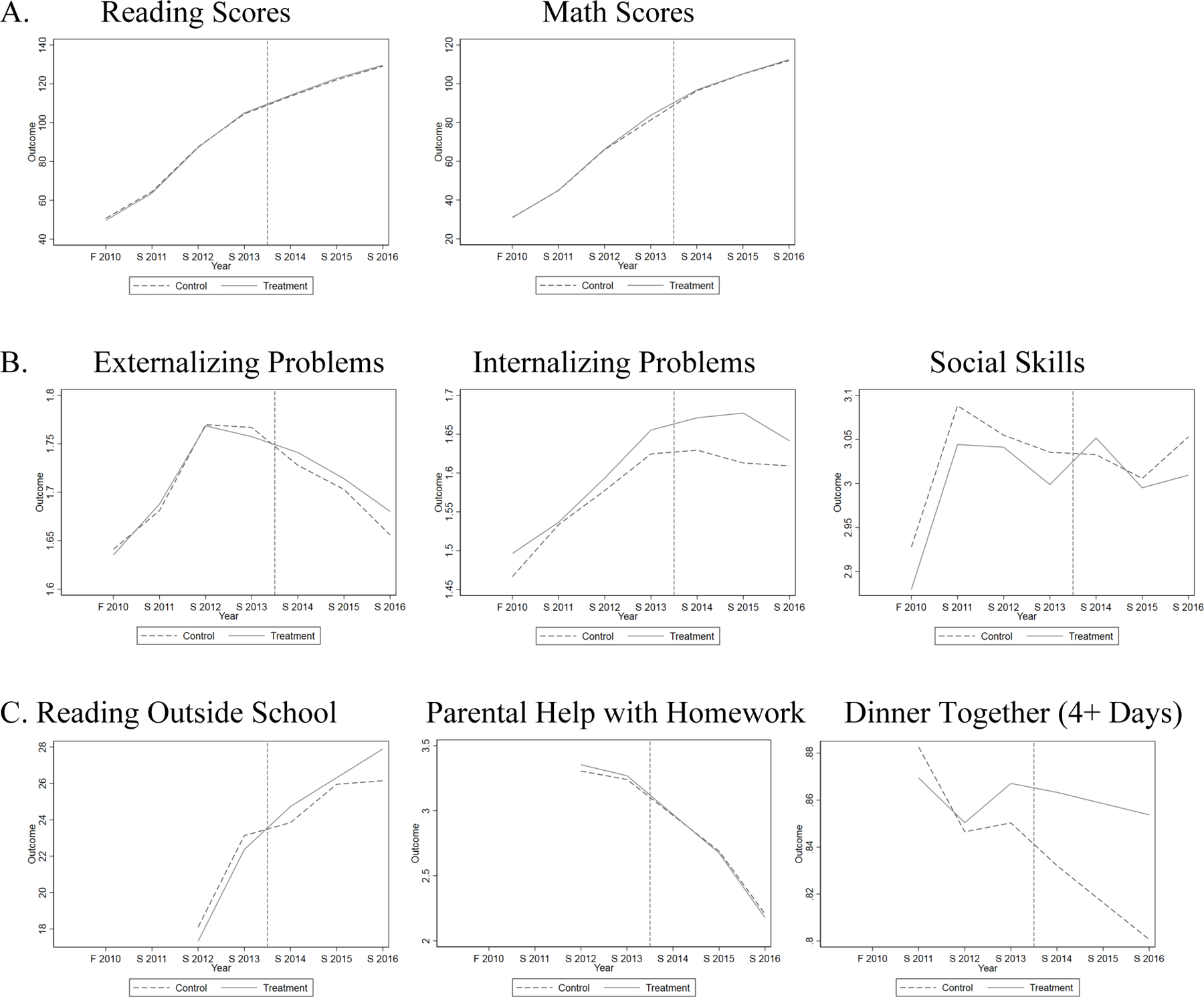
Notes: Data from ECLS:K 2011. Expansion states are the treatment states, and non-expansion states are the control states. The x-axis (Year) represents the survey wave, F=fall and S=spring. The vertical line represents January 2014, when the ACA Medicaid expansions were largely implemented. Sample is limited to children in households with incomes below 138% FPL.
4.2. Impact of the ACA Medicaid Expansions on Children and Families
The primary goal of this study is to examine whether public health insurance eligibility among low-income adults influenced child academic achievement and socioemotional skills and family functioning. The main results are presented in Table 2 with each column of each panel corresponding to a different OLS regression. We report the coefficients of interest, the standard errors, means of the dependent variables, number of observations (child-year and child-level), and the R-squared (within-child). The coefficients in columns 1, 3, and 5 provide the baseline results across the main outcomes of interest, without adding state-level time varying characteristics. The DD estimate is positive and statistically significant for reading scores implying improvements in reading scores among children as a result of the ACA Medicaid expansions for low-income adults. The DD estimate is positive, but not statistically significant at conventional levels, for math scores.
Table 2.
Impact of the ACA Medicaid Expansion on Child Development and Family Functioning Among Children from Low-Income Households (< 138% FPL)
| A. Academic Outcomes | Reading Scores | Math Scores | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| (1) | (2) | (3) | (4) | |||
| Expansion | 1.167* | 1.151~ | 0.527 | 0.111 | ||
| (0.523) | (0.582) | (1.093) | (1.090) | |||
| Mean of DV | 50.84 | 50.84 | 31.38 | 31.38 | ||
| Time Varying State Covariates | No | Yes | No | Yes | ||
| Observations (Child-year) | 17,070 | 17,070 | 17,060 | 17,060 | ||
| Observations (Child) | 2,520 | 2,520 | 2,520 | 2,520 | ||
| R-squared | 0.929 | 0.929 | 0.937 | 0.937 | ||
| B. Socioemotional Outcomes | Externalizing Problems | Internalizing Problems | Social Skills | |||
|
| ||||||
| (1) | (2) | (3) | (4) | (5) | (6) | |
|
| ||||||
| Expansion | 0.018 | 0.007 | 0.028 | 0.023 | 0.033 | 0.028 |
| (0.025) | (0.028) | (0.020) | (0.024) | (0.033) | (0.035) | |
| Mean of DV | 1.65 | 1.65 | 1.50 | 1.50 | 2.90 | 2.90 |
| Time Varying State Covariates | No | Yes | No | Yes | No | Yes |
| Observations (Child-year) | 15,440 | 15,440 | 15,290 | 15,290 | 15,080 | 15,080 |
| Observations (Child) | 2,500 | 2,500 | 2,500 | 2,500 | 2,500 | 2,500 |
| R-squared | 0.012 | 0.012 | 0.016 | 0.016 | 0.011 | 0.011 |
| C. Family Functioning | Reading Outside School | Parental Help with Homework | Dinner Together (4 days or more in a week) | |||
|
| ||||||
| (1) | (2) | (3) | (4) | (5) | (6) | |
|
| ||||||
| Expansion | 2.436** | 2.405** | −0.217* | −0.267* | 0.047*** | 0.048** |
| (0.708) | (0.826) | (0.087) | (0.108) | (0.011) | (0.014) | |
| Mean of DV | 17.92 | 17.92 | 3.347 | 3.347 | 0.887 | 0.887 |
| Time Varying State Covariates | No | Yes | No | Yes | No | Yes |
| Observations (Child-year) | 11,580 | 11,580 | 9,300 | 9,300 | 11,390 | 11,390 |
| Observations (Child) | 2,520 | 2,520 | 2,520 | 2,520 | 2,530 | 2,530 |
| R-squared | 0.065 | 0.066 | 0.151 | 0.152 | 0.007 | 0.007 |
Notes: Each column of each panel corresponds to a different OLS regression model. Each model includes wave and child fixed effects and sampling weights. Expansion represents β1 from equation (1), and measures the average effect of the Medicaid expansions after it took place. Mean of each dependent variable (DV) provides the within-child average of the DV after controlling for just wave fixed effects. Heteroscedasticity-robust standard errors, in parentheses, are clustered at the state level. Sample sizes are rounded to the nearest 10 as per dataset guidelines.
p < 0.10
p < 0.05
p < 0.01
p < 0.001.
As shown in columns 2, 4, and 6, these results are also robust to the inclusion of state-level time-varying controls. We provide the mean within-child (across waves) for each outcome of interest in the second row to contextualize the relative effect sizes. Perhaps not surprisingly, the magnitude of the effect sizes is small but meaningful. Specifically, reading scores increased by about 1.151 scaled points (p = 0.055). Relative to the mean of 50.84, this increase represents an improvement of about 2.3%. In terms of standardized effect sizes that is more common in the education literature, this translates to 0.04 standard deviations (SDs).
Panel B depicts the DD estimates for children’s socioemotional outcomes. Though the estimates are all positive, we observe no significant effects of the ACA Medicaid expansions on social skills or externalizing and internalizing problems among children from low-income households, regardless of the inclusion of state covariates.
Panel C presents results for various measures of family functioning, which we hypothesize are potential mechanisms through which parental health insurance eligibility may influence children’s development. We note that these measures are important independent of their potential relation with child development, and are therefore their own contribution to the literature. Overall, these results show significant improvements in family functioning and routines as a result of the ACA Medicaid expansions. Specifically, columns 2 and 6 show that children in low-income households read about 2.41 more minutes per week outside of school (~13.4%)4 and were 4.8 percentage points more likely to eat dinner with their families on 4 or more days per week (~5%). On the other hand, in column 4 we also observe small, but statistically significant, decreases in how frequently parents helped their children with homework every week (~8%), a point we return to in the discussion.
We next conduct three sets of subsample analyses to examine heterogeneity in treatment effects by race/ethnicity, high/low income within the sample of low-income households, and parental marital status (e.g., not married vs. married) for our primary academic outcomes of interest (see Appendix Table S3). We find that the effect on children’s reading scores is primarily driven by Black children and children from households with incomes below the median income (approximately $17,500 prior to expansion in 2014) in our analytic sample. We also observe an improvement in math scores among Black children. These results suggest that the benefits of health insurance expansions on children’s academic achievement might be reaching more vulnerable subgroups of children, even among those from low-income families. However, we interpret these results with caution due to small sample sizes (results on other outcome variables show similar heterogenous effects, although imprecise, and are available from the authors on request).
5. PLACEBO CHECK
First, the ACA Medicaid expansions affect adult health insurance access among low-income households in states that expanded their programs. Therefore, our main results are limited to low-income households that should be eligible for Medicaid based on their reported household income and family size. We would not expect Medicaid expansions to affect high-income households in the states that expanded versus those that did not. Therefore, in Table 3, we present analogous DD estimates from equation (1) among children residing in households with annual household income greater than $50,000 (roughly equivalent to 400% FPL) in Spring 2013. As seen in Table 3, we did not observe any statistically significant effects for any outcomes with the exception of parents helping with homework in this high-income sub-sample. Further, many of the estimates are negative. This placebo check gives us additional confidence in our results on reading scores, reading outside of school, and eating dinner together.
Table 3.
Impact of the ACA Medicaid Expansion on Child Development and Family Functioning Among Children from High-Income Households (> $50,000 Annual Household Income)
| A. Academic Outcomes | Reading Scores | Math Scores | |
|---|---|---|---|
|
| |||
| (1) | (2) | ||
| Expansion | 0.410 | 0.026 | |
| (0.519) | (0.662) | ||
| Mean of DV | 73.21 | 54.92 | |
| Observations (Child-year) | 27,190 | 27,190 | |
| Observations (Child) | 5,760 | 5,760 | |
| R-squared | 0.908 | 0.934 | |
| B. Socioemotional Outcomes | Externalizing Problems | Internalizing Problems | Social Skills |
|
| |||
| (1) | (2) | (3) | |
|
| |||
| Expansion | −0.000 | −0.001 | −0.005 |
| (0.016) | (0.012) | (0.019) | |
| Mean of DV | 1.541 | 1.445 | 3.250 |
| Observations (Child-year) | 25,390 | 25,340 | 25,220 |
| Observations (Child) | 5,600 | 5,600 | 5,610 |
| R-squared | 0.016 | 0.008 | 0.001 |
| C. Family Functioning | ReaReading Outside School | PaParental Help with Homework | Dinner Together (4 days or more in a week) |
|
| |||
| (1) | (2) | (3) | |
|
| |||
| Expansion | −0.235 | −0.188* | −0.013 |
| (0.577) | (0.086) | (0.016) | |
| Mean of DV | 17.93 | 3.180 | 0.887 |
| Observations (Child-year) | 22,730 | 18,190 | 22,250 |
| Observations (Child) | 5,590 | 5,590 | 5,690 |
| R-squared | 0.111 | 0.176 | 0.013 |
Notes: Each column of each panel corresponds to a different OLS regression model. Each model includes wave and child fixed effects, state-level covariates, and sampling weights. Expansion represents β1 from equation (1), estimated for sub-sample of higher-income (> $50,000 annual household income) households only, and measures the average effect of the Medicaid expansions after it took place. Mean of each dependent variable (DV) provides the within-child average of the DV after controlling for just wave fixed effects. Heteroscedasticity-robust standard errors, in parentheses, are clustered at the state level. Sample sizes are rounded to the nearest 10 as per dataset guidelines.
p < 0.10
p < 0.05
p < 0.01
p < 0.001.
6. PARENTAL ELIGIBILITY PRE-ACA
In our main models, we define treatment status to include states that expanded Medicaid to low-income adults through the ACA. Prior to the ACA, however, states had different income thresholds for low-income parents, meaning that the generosity of the ACA Medicaid expansions varied across states. For example, in Arizona, parents whose household income was less than 106% of the FPL were eligible for Medicaid in 2011. In Oregon, only parents whose household income was less than 40% of the FPL were eligible for Medicaid in 2011. Both states expanded their Medicaid programs through the ACA, and all adults whose household income was less than 138% of the FPL became newly-eligible in 2014. The expansion likely affected a larger proportion of families in Oregon than in Arizona, however. Alternatively, some states had income eligibility thresholds for parents above 138% FPL, and actually lowered their thresholds to meet the 138% level (e.g., Illinois).
To more precisely capture these nuances in parental eligibility, in this robustness check, we redefine treatment status. Specifically, we estimate the following model using the sample of children from low-income households (<138% FPL) but only include those children whose parents would have been newly eligible. In other words, we drop children whose parents were likely eligible for Medicaid based on pre-ACA income thresholds, even in expansion states:
| (2) |
Where equals 1 if child lives in a household with a household income between state s’s pre-ACA parental income eligibility threshold and 138% FPL (calculated using parental income eligibility in 2011; this variable is not time-varying).5 The control group consists of children in low-income households (<138% FPL) that reside in states that did not expand Medicaid through the ACA. All other elements remain the same as in equation 1. Essentially, this analysis aims to isolate treatment effects on child and family outcomes on children whose parents were most likely to be newly eligible under ACA, and on whom we would expect the effects to be tighter. We also show the raw trends in the various outcomes for these different groups across the waves separately (see Figure S2).
In Table 4, we present estimates from equation (2). We find larger and more precisely estimated effects on our primary academic outcomes of interest. For example, in this analysis, we find an improvement in reading scores of about 3% compared to approximately 2% in the main model, increases in time spent reading of 16% compared to 13.4%, and increases in the likelihood of eating dinner together 4 days or more per week by 6% compared to 5%. Effects on parental help with homework are directionally similar but imprecise. This robustness check gives us further confidence in our results on reading scores and family functioning. In other words, children whose parents were most likely to have gained eligibility for Medicaid under the ACA seem to show the largest effects on reading scores. However, as described earlier, because “welcome mat” effects have been documented for children in households that were eligible for Medicaid before the ACA, we believe that the estimates from the baseline DD specification provides a better estimate of magnitude of the intent-to-treat effects on child development and family functioning.
Table 4.
Impact of the ACA Parental Income Eligibility Expansion on Child Development and Family Functioning Among Children from Low-Income Households (<138% FPL)
| A. Academic Outcomes | Reading Scores | Math Scores | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| (1) | (2) | (3) | (4) | |||
| Expansion | 1.637* | 1.528* | −0.120 | −0.124 | ||
| (0.786) | (0.720) | (1.118) | (1.076) | |||
| Mean of DV | 51.47 | 51.47 | 32.07 | 32.07 | ||
| Time Varying State Covariates | No | Yes | No | Yes | ||
| Observations (Child-year) | 8,200 | 8,200 | 8,220 | 8,220 | ||
| Observations (Child) | 1,220 | 1,220 | 1,220 | 1,220 | ||
| R-squared | 0.929 | 0.929 | 0.937 | 0.937 | ||
| B. Socioemotional Outcomes | Externalizing Problems | Internalizing Problems | Social Skills | |||
|
| ||||||
| (1) | (2) | (3) | (4) | (5) | (6) | |
|
| ||||||
| Expansion | 0.027 | 0.022 | −0.004 | 0.003 | 0.018 | 0.002 |
| (0.031) | (0.031) | (0.034) | (0.033) | (0.044) | (0.044) | |
| Mean of DV | 1.62 | 1.62 | 1.51 | 1.51 | 2.91 | 2.91 |
| Time Varying State Covariates | No | Yes | No | Yes | No | Yes |
| Observations (Child-year) | 7,640 | 7,640 | 7,570 | 7,570 | 7,460 | 7,460 |
| Observations (Child) | 1,210 | 1,210 | 1,210 | 1,210 | 1,210 | 1,210 |
| R-squared | 0.019 | 0.019 | 0.008 | 0.008 | 0.014 | 0.015 |
| C. Family Functioning | Reading Outside School | Parental Help with Homework | Dinner Together (4 or more days in a week) | |||
|
| ||||||
| (1) | (2) | (3) | (4) | (5) | (6) | |
|
| ||||||
| Expansion | 1.948~ | 2.898* | −0.145 | −0.163 | 0.061** | 0.059* |
| (1.109) | (1.154) | (0.129) | (0.164) | (0.019) | (0.026) | |
| Mean of DV | 17.73 | 17.73 | 3.250 | 3.250 | 0.889 | 0.889 |
| Time Varying State Covariates | No | Yes | No | Yes | No | Yes |
| Observations (Child-year) | 5,630 | 5,630 | 4,520 | 4,520 | 5,510 | 5,510 |
| Observations (Child) | 1,210 | 1,210 | 1,213 | 1,213 | 1,220 | 1,220 |
| R-squared | 0.065 | 0.066 | 0.156 | 0.158 | 0.009 | 0.010 |
Notes: Each column of each panel corresponds to a different OLS regression model. Each model includes wave and child fixed effects and sampling weights. Expansion represents β from equation (2), and measures the average effect of the Medicaid expansions after it took place. Mean of each dependent variable (DV) provides the within-child average of the DV after controlling for just wave fixed effects. Heteroscedasticity-robust standard errors, in parentheses, are clustered at the state level. Sample sizes are rounded to the nearest 10 as per dataset guidelines.
p < 0.10
p < 0.05
p < 0.01
p < 0.001.
7. SENSITIVITY CHECKS
To assess the robustness of our results, we perform a variety of sensitivity checks. These include (1) excluding states that expanded their Medicaid programs earlier or later than 2014; (2) adjusting for whether states adopted Common Core Standards (a broad-based curricular reform adopted by certain states between 2011 and 2015, [CCS]); (3) excluding sampling weights; and (4) adjusting for multiple hypothesis testing using a sharpened q-value estimate; and (5) adjusting for a small number of clusters using a wild bootstrap clustered p-value.6
In our main models, we include both states that expanded Medicaid early (i.e., before January 2014) and those that expanded late (i.e., after January 2014). Including early states may bias positive estimates downwards since people in these states had earlier access to public health insurance coverage through the ACA. In contrast, including late expansion states may bias positive estimates upwards since access to public health insurance occurred later. We therefore tested whether our main results are sensitive to the exclusion of either group of states (Appendix Table S1 lists the early and late expansion states). Tables S5 and S6, panel A reports these results, where the first column for each variable consists of estimates that exclude early expansion states and the second column offers estimates that exclude late expansion states. As predicted, excluding early expansion states tends to enhance the estimates, while excluding late expansion states tends to mute effects. Overall, however, excluding either group of states does not substantively change the main results.
Second, the assumptions of a difference-in-differences model would be violated if children from low-income families experienced other policies or macro-level changes to their environment between 2010 and 2016 that might be correlated with states’ decisions to expand Medicaid under the ACA and affect their outcomes. Given a potential overlap between states expanding Medicaid under the ACA and states adopting CCS, we include a variable that accounts for the adoption of CCS at the state-year level. Appendix Figure S3 shows a map of states that adopted CCS and the timing of adoption.7 Tables S5 and S6, panel B shows the results are similar to the main results offering additional evidence that the observed effects are from Medicaid expansions rather than other policy changes.
Finally, we test the sensitivity of the results to several analytical considerations. First, the results are robust to omitting sampling weights, as shown in panel C of Tables S5 and S6. In Table S7 we present adjusted p-values for multiple hypothesis testing and wild clustered bootstrap p-values from 1,000 replications. Despite less precision, these results are substantively similar to our main results.
8. DISCUSSION
In this paper, we examine the short-term effect of expanding public funding for adult health insurance coverage on children’s development and families’ functioning. We focus on children growing up in low-income families to isolate a sample of children whose parents would have been most likely to become eligible for health insurance coverage through the ACA’s Medicaid expansions. Prior research has found that these health insurance expansions improved adults’ physical and psychological health and economic outcomes (Glied et al., 2020; Mazurenko et al., 2018; Soni et al., 2020) and that these positive benefits occurred among the subpopulation of low-income adults with dependent children (McMorrow et al. 2017; Wisk et al., 2020). Although the ACA Medicaid expansions did not alter eligibility for health insurance coverage for children, theory and empirical evidence imply that improvements in parents’ well-being and income promote children’s development (Becker et al., 1993; Bradley & Corwyn, 2004; Burak, 2019; Conger et al., 1997; Corak, et al., 2013; Gassman-Pines & Hill, 2013; Yeung et al., 2002). In addition, there is evidence suggesting that increased parental awareness of publicly funded health insurance coverage can directly influence children through increased enrollment of children in health insurance plans and subsequent healthcare access (Cohodes et al., 2016; De La Mata, 2012).
One important contribution of the present study is the use of a nationally representative sample of children in low-income households with direct observations of children’s math and reading achievement and parents’ reports of families’ functioning. This allows us to investigate both impacts on children’s development and family-level mechanisms through which these impacts may occur. Additionally, our use of child-level, longitudinal data paired with a difference-in-differences framework that exploits cross-state policy variation enable us to uncover quasi-experimental effects of adult Medicaid eligibility on child development and family functioning, net of time-invariant child-specific factors, a novel feature of this study.
We find that expansions of adult eligibility for publicly funded health insurance positively influence low-income children’s reading scores. Specifically, the ACA Medicaid expansions improve children’s reading scores by about 2.3% (or a standardized effect size of roughly 0.04 SDs). We find no evidence that the expansions influence children’s math or socioemotional skills, as assessed in the domains of social skills, externalizing problems, and internalizing problems. Among the measures of family functioning, we find that the Medicaid expansions increase parental reports of time spent reading by children outside of school and eating dinner together. Results also suggest that the Medicaid expansions decrease the frequency with which parents help their children with homework. Taken together, results suggest that the improvements in children’s reading scores may have been due to improvements in families’ functioning. It is also likely that the increases in reading scores are a result of a combination of these mechanisms, in addition to other unobserved mechanisms. For example, we are unable to empirically test whether children are more likely to obtain medical diagnosis and treatment for various developmental or learning disorders, such as ADHD, which may aid in improving children’s functioning. Below, we contextualize these results in more detail.
8.1. Adult Health Insurance Expansions and Children’s Development
The improvements in reading scores are modest, but meaningful (about 2.3% or roughly 0.04 SDs on reading scores). The small effect size is not surprising given that children were in late elementary school when these skills were assessed following the expansion. To put this observed effect size in context, the median effect size on standardized reading scores from educational interventions evaluated rigorously using randomized control trials for students in grades 3–5 ranges between 0.09 and 0.11 SDs (Kraft, 2020). We would expect health policy spillovers on educational outcomes to be smaller in magnitude. When compared to limited past literature on the educational effects of similar health policy interventions, again, we find that our results are smaller in magnitude, but consistent with hypotheses. For example, Levine and Schanzenbach (2009) note that a 50-percentage point increase in public health insurance eligibility at birth improved children’s reading test scores (pooled 4th and 8th grade test scores) by 0.09 SDs. We would expect the estimates in this study to be smaller as we are evaluating parents’ health insurance eligibility expansion (which increased by roughly 34 percentage points on average in expansion states [see Mcmorrow et al., 2017])8 spillovers on children, rather than children’s own insurance access. Further, children in our study were in third grade when most insurance expansions that we evaluate occurred; health insurance eligibility at birth is likely to have larger effects.
Evidence on the links between safety net programs and children’s academic achievement generally finds the most consistent effects around the transition into school and the early elementary years with less consistent, though limited, findings in the late elementary and adolescent years (Duncan et al., 2019). A similar pattern is found when examining changes in family income and children’s academic skill development. Increases in families’ incomes during early childhood have robust links with children’s academic achievement, but the findings show small or no associations during middle childhood (Duncan et al., 1998; Votruba-Drzal, 2006). Given the small associations documented to date, the slight improvements in reading scores among elementary-aged children in low-income families is promising evidence about the implications of public funding for adult health insurance. It is possible that future research on samples of younger children may yield larger effects.
We do not detect any statistically significant impacts of the Medicaid expansions on children’s math or socioemotional skills. While we had hypothesized that public expansions in adult health insurance would have similar implications across child outcomes, there are several potential explanations for these differential results. In relation to math scores, given that children’s development was only measured three times after the Medicaid expansions went into effect, it is plausible that any impacts had not yet emerged. For example, the cognitive processes underlying late elementary math achievement, including skills in mental rotation, algebraic knowledge, and calculation accuracy, may have not yet been influenced by changes in family functioning to the point where they generated substantially larger scores on the math achievement tests. In fact, emerging evidence points to the role of language and reading skills in the promotion of subsequent math skill performance (Bailey et al., 2020), suggesting that the impacts on reading scores may translate into benefits to math scores later, a question that should be explored in future research examining the longer-term impacts of the Medicaid expansions. Sustained exposure to health insurance and improved healthcare access over longer time periods may also result in larger and emergent effects on long-term child outcomes.
Additionally, while there is robust evidence of the importance of the home environment on math achievement prior to and at school entry at older ages (Elliott & Bachman, 2018), the quality of school math instruction has been found to be the most consistent predictor of math gains relative to children’s home environments among older children (Bachman et al., 2015; Jacob, 2005). Therefore, changes in family functioning may have less of an impact for elementary-aged children than it might have for younger children’s developing math abilities (Duncan et al., 1998; Votruba-Drzal, 2006). In contrast, children’s reading abilities continue to be associated with qualities of the home environment through elementary school (Jacob, 2005; Sénéchal & LeFevre, 2002). Indeed, earlier work examining the effect of children’s health insurance coverage through expansions in Medicaid and the State Children’s Health Insurance Program (SCHIP) found improvements in reading scores, but no effects for math scores (Levine & Schanzenbach, 2009).
We also hypothesized that the ACA Medicaid expansions would have positive implications for children’s socioemotional development. These hypotheses were based upon theoretical models about the role of family stress and economic resources on children’s socioemotional functioning (Conger et al., 1997), as well as empirical evidence finding children’s parent-reported internalizing and externalizing behaviors were positively associated with changes in family economic resources during middle childhood (Votruba-Drzal, 2006). We find no differences in teacher-reported socioemotional skills between children from expansion versus non-expansion states. It is possible that any changes in children’s socioemotional functioning were not captured by these measures or by teacher reports (versus parent or self-report). Nonetheless, we measured socioemotional functioning across three domains (social skills, externalizing problems, and internalizing problems). Findings provide preliminary evidence that the ACA Medicaid expansions had little impact on children’s socioemotional skills, results which should be replicated by future research examining different age groups and longer-term trajectories of socioemotional functioning.
8.2. Adult Health Insurance Expansions and Family Functioning
We also sought to understand potential mechanisms through which the expansions may have influenced children’s development. We draw upon theoretical models pointing to family functioning as explaining the links between social programs and children’s development (Becker, 1993; Conger et al., 1997; Gassman-Pines & Hill, 2013; Yeung et al., 2002). We find that the Medicaid expansions increased time spent reading by children outside of school and families’ dinner routines with children, an important predictor of child well-being (Fiese & Schwartz, 2008). Conversely, the Medicaid expansions decreased time spent helping children with homework, a seemingly counterintuitive finding which is supported in the literature. Specifically, parental help with homework by early adolescence has been negatively linked with children’s achievement, in part because less parental support is a signal of children’s growing abilities to independently complete their academic work outside of school without adult assistance (Hill & Tyson, 2009).
The findings on family functioning provide important evidence to suggest that parental eligibility for health insurance improved children’s home environments through children spending more time reading at home and eating dinner together as a family as well as needing less parental support with homework. While it is beyond the scope of this study to identify exactly how expansions in health insurance for adults may have translated to these forms of family functioning, it is possible to draw upon theoretical models of family stress (Conger et al., 1997; Yeung et al., 2002) to speculate that perhaps the documented benefits of the expansions for adults’ physical health (Simon et al., 2017; Soni et al., 2020; Gopalan et al. 2021), behavioral health (Maclean et al., 2019; Maclean & Saloner, 2019), and psychological health (McMorrow et al. 2017) had positive implications for parents’ behaviors in supporting their children.
Combined with the findings on children’s reading scores, and existing empirical work linking the home learning environment with children’s reading gains during elementary school (Sénéchal & LeFevre, 2002), these results suggest a potential pathway from parental health insurance to family functioning to reading skill development. Because of the concurrent measurement of family functioning and achievement at every wave in this data, we are only able to speculate about these observed mechanisms. Nevertheless, we find that the sign and magnitude of effects across the outcomes points in the same direction: public health insurance expansions to low-income households seem to have modest, but significant effects on children’s academic achievement, potentially flowing through improvements in family functioning.
8.3. Limitations
Although we are the first that we know of to examine the effects of the ACA Medicaid expansions on children’s development (including academic achievement), this study is not without limitations. First, there are only three post-expansion waves in our dataset, therefore, our results should be interpreted as short-term. Longer-term effects, such as those noted above, require further analysis than this data allows. Second, the magnitudes of our findings, while significant, are modest. In addition to the short-run nature of this study, this may be due to the focus on children in middle childhood versus early childhood. Future research is needed to understand the impact of the expansions on younger children, as well as on adolescents. Third, in determining potential mechanisms, we are limited in both frequency and consistency of questions asked in the survey across waves. It would have been ideal, for example, to have consistent measures of parental and child health insurance coverage, parent health care utilization, and more comprehensive measures of parental psychological and physical health, family stress, and family functioning. Unfortunately, these measures were not available in these data or were not measured consistently pre- and post-expansion. There is a critical need for more work that directly measures the mechanisms through which social policy, and publicly funded health insurance, in particular, impacts child development and achievement.
9. CONCLUSIONS AND IMPLICATIONS
The results of this study have several noteworthy policy implications. Although previous work has studied the effect of children’s health insurance coverage on children’s development, less is known about the indirect effects of parental health insurance coverage on children. Using representative data and quasi-experimental methods, we demonstrate that adult public health insurance eligibility improves children’s reading scores. Results also show that the expansions increased time children spent reading outside of school and the frequency of eating dinner together as a family, while reducing time spent by parents helping children with their homework. Taken together, these findings provide important evidence in light of ongoing policy debates regarding changes to the ACA, as well as the precarious nature of the job market and current economy, underscoring the uncertainty of employer-sponsored health care. Understanding the spillover effects of this policy is also important for appropriately documenting the costs and benefits of expanding Medicaid for the states that have not yet expanded their programs and for continuing the investments in the states that have implemented expansions. Finally, there are well-established income-based gaps in children’s development (Duncan et al., 2019). Connecting public programs to educational outcomes is crucial to reduce these gaps.
Supplementary Material
Acknowledgments
We are grateful for funding from the Spencer Foundation. We also acknowledge the restricted-use data access and a seed grant provided by the Population Research Institute at Penn State University, which is supported by an infrastructure grant by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (P2CHD041025), to Gopalan. We also acknowledge support from the UConn Office of the Vice President for Research to Lombardi. We thank Drew Bailey, Chloe East, Nathaniel Hendren, Michelle Marcus, and participants at the conferences of the Southern Economic Association, the Association of Education Finance and Policy, and the Association of Public Policy and Management for helpful comments and feedback on earlier drafts of the manuscript. All remaining errors are our own.
Footnotes
We declare no conflicts of interest.
Household income is reported as 18 separate categories in the ECLS-K:2011 (increments of $5,000 up to $75,001). Therefore, we manually construct an estimated household income as a percent of FPL for each child in the survey. To do so, we use reported household income and household size during Wave 5 (spring 2013, reporting on calendar year 2012 income), the midpoints of each income category, and 2012 poverty guidelines.
Measures of family functioning described below in 3.3.3 are not consistently asked across the 7 waves we use for this study in ECLS-K. For example, “reading minutes” is not collected in waves 1 and 2; “parental help with homework” is not collected in waves 1, 2, and 5. Because these are measured consistently in at least two pre- and two post-expansion waves, we include them in our analysis.
Results on the continuous measure are similar and available from the authors on request.
About 5% of the analytical sample reported 0 reading minutes per week outside school. So we also examined the effects on the extensive margin (whether the Medicaid expansions increased the number of children who read outside school at all) and intensive margin (whether the Medicaid expansion increased the minutes among those who already read outside school) separately. We find that the positive significant effect is driven almost entirely by intensive margin (DID coefficient of 2.40, p = 0.006) rather than the extensive margin (DID coefficient of 0.013, p = 0.242), which is unsurprising given the low number of children reporting 0 minutes of reading outside school.
Appendix Table S4 shows each expansion state’s parental income eligibility threshold in 2011.
Wild cluster bootstrap p-values are only recommended if there are very few clusters, especially treatment clusters, in the analytical sample. With 25 expansion states (i.e., treatment clusters) and 16 non-expansion states in our sample (i.e., control clusters), cluster robust standard errors are valid for inference. Nevertheless, we also report wild cluster bootstrapped p-values created using “boottest” command in STATA from 1,000 replications which provides more conservative standard errors for inference in Table S7 (Cameron & Miller, 2008; 2015).
We use a measure of CCS “adoption” at the state-year level based on data from the National Conference of State Legislatures. More recent research, however, shows how implementation of these standards was uneven and lagged over multiple years both within and across states.
Because our data does not have measures on parents’ actual health insurance status, we are unable to examine the first-stage effect of the ACA expansions on the actual take-up of insurance among parents in our sample. The best comparable estimate of this first-stage effect is from McMorrow et al. (2017). They find that among low-income parents, Medicaid/CHIP insurance rates went up by roughly 11.8 percentage points in the first year (2015) after expansion among expansion states. A back-of-the-envelope calculation of the treatment on the treated (TOT) effect of 6 percentage points (translates to 13% relative change on a mean reading score of 50 points) is plausible. We use the above first-stage estimate of 0.118 and our DID reading score coefficient of 0.753 (unweighted DID estimate used here for valid comparisons) to calculate the TOT (0.753/0.118). This illustrates that the effect size estimate for reading is in line with what we might expect from past theoretical and empirical literature.
Contributor Information
Lindsey Rose Bullinger, School of Public Policy, Georgia Tech
Maithreyi Gopalan, Department of Education Policy Studies, Pennsylvania State University
Caitlin McPherran Lombardi, Department of Human Development and Family Sciences, University of Connecticut
REFERENCES
- Abramowitz J (2020). The effect of ACA state Medicaid expansions on medical out-of-pocket expenditures. Medical Care Research and Review, 77(1), 19–33. [DOI] [PubMed] [Google Scholar]
- Anderson ML (2008). Multiple inference and gender differences in the effects of early intervention: A reevaluation of the Abecedarian, Perry Preschool, and Early Training Projects. Journal of the American statistical Association, 103(484), 1481–1495. [Google Scholar]
- Allen HL, Eliason E, Zewde N, & Gross T (2019). Can Medicaid expansion prevent housing evictions? Health Affairs, 38(9), 1451–1457. [DOI] [PubMed] [Google Scholar]
- Bachman HJ, Votruba-Drzal E, El Nokali NE, & Castle Heatly M (2015). Opportunities for learning math in elementary school: Implications for SES disparities in procedural and conceptual math skills. American Educational Research Journal, 52(5), 894–923. [Google Scholar]
- Bailey DH, Oh Y, Farkas G, Morgan P, & Hillemeier M (2020). Reciprocal effects of reading and mathematics? Beyond the cross-lagged panel model. Developmental Psychology, 56(5), 912–921. [DOI] [PubMed] [Google Scholar]
- Becker GS (1993). Human capital: A theoretical and empirical analysis, with special reference to education (3rd ed.). University of Chicago Press. [Google Scholar]
- Benjamini Y, Krieger AM, & Yekutieli D (2006). Adaptive linear step-up procedures that control the false discovery rate. Biometrika, 93(3), 491–507. [Google Scholar]
- Bertrand M, Duflo E, & Mullainathan S (2004). How much should we trust differences-in-differences estimates? The Quarterly Journal of Economics, 119(1), 249–275. [Google Scholar]
- Borgschulte M, & Vogler J (2020). Did the ACA Medicaid expansion save lives? Journal of Health Economics, 72, 102333. [DOI] [PubMed] [Google Scholar]
- Boudreaux MH, Golberstein E, & McAlpine DD (2016). The long-term impacts of Medicaid exposure in early childhood: Evidence from the program’s origin. Journal of Health Economics, 45, 161–175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bradley RH, & Corwyn RF (2004). Family process investments that matter for child well-being. In Kalil A & DeLeire T (Eds.), Family investments in children: Resources and behaviors that promote success (pp. 1–32). Lawrence Erlbaum. [Google Scholar]
- Brevoort K, Grodzicki D, & Hackmann MB (2017). Medicaid and financial health (No. w24002). National Bureau of Economic Research. [Google Scholar]
- Brown DW, Kowalski AE, & Lurie IZ (2015). Medicaid as an investment in children: What is the long-term impact on tax receipts? (Working Paper No. 20835).
- Bullinger LR (2021). Child support and the Affordable Care Act Medicaid expansions. Journal of Policy Analysis and Management, 40(1), 42–77 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burak EW (2019). Parents’ and caregivers’ health insurance supports children’s healthy development. Society for Research in Child Development Child Evidence Briefs, 4, 1–2. [Google Scholar]
- Case A, & Paxson C (2002). Parental behavior and child health. Health Affairs, 21(2), 164–178. [DOI] [PubMed] [Google Scholar]
- Cameron AC, & Miller DL (2015). A practitioner’s guide to cluster-robust inference. Journal of Human Resources, 50(2), 317–372. 10.3368/jhr.50.2.317 [DOI] [Google Scholar]
- Cohodes SR, Grossman DS, Kleiner SA, & Lovenheim MF (2016). The effect of child health insurance access on schooling: Evidence from public insurance expansions. Journal of Human Resources, 51(3), 727–759. [Google Scholar]
- Conger RD, Conger KJ, & Elder GH (1997). Family economic hardship and adolescent adjustment: Mediating and moderating processes. In Duncan GJ & Brooks-Gunn J (Eds.), Consequences of growing up poor (pp. 288–310). Russell: Sage. [Google Scholar]
- Corak M (2013). Income inequality, equality of opportunity, and intergenerational mobility. Journal of Economic Perspectives, 27(3), 79–102. [Google Scholar]
- Cotti C, Nesson E, & Tefft N (2019). Impacts of the ACA Medicaid expansion on health behaviors: Evidence from household panel data. Health Economics, 28, 219–244. [DOI] [PubMed] [Google Scholar]
- Courtemanche C, Marton J, Ukert B, Yelowitz A, & Zapata D (2019). Effects of the Affordable Care Act on health behaviors after 3 years. Eastern Economic Journal, 45, 7–33. [Google Scholar]
- Courtemanche C, Marton J, Ukert B, Yelowitz A, & Zapata D (2018a). Early effects of the Affordable Care Act on health care access, risky health behaviors, and self-assessed health. Southern Economic Journal, 84, 660–691. [Google Scholar]
- Courtemanche C, Marton J, Ukert B, Yelowitz A, & Zapata D (2018b). Effects of the Affordable Care Act on health care access and self-assessed health after 3 years. INQUIRY: The Journal of Health Care Organization, Provision, and Financing, 55, 0046958018796361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Courtemanche C, Marton J, Ukert B, Yelowitz A, & Zapata D (2017). Early impacts of the Affordable Care Act on health insurance coverage in Medicaid expansion and non‐ expansion states. Journal of Policy Analysis and Management, 36(1), 178–210. [DOI] [PubMed] [Google Scholar]
- Courtemanche C, Marton J, & Yelowitz A (2016). Who gained insurance coverage in 2014, the first year of full ACA implementation? Health Economics, 25(6), 778–784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De La Mata D (2012). The effect of Medicaid eligibility on coverage, utilization, and children’s health. Health Economics, 21(9), 1061–1079. [DOI] [PubMed] [Google Scholar]
- Duncan G, Brooks-Gunn J, Yeung WJ, & Smith J (1998). How much does childhood poverty affect the life chances of children? American Sociological Review, 63, 406– 423. [Google Scholar]
- Duncan G, Magnuson K, Murnane R, & Votruba‐Drzal E (2019). Income inequality and the well‐being of American families. Family Relations, 68(3), 313–325. [Google Scholar]
- East CN, Miller S, Page M, & Wherry LR (2019). Multi-generational impacts of childhood access to the safety net: Early life exposure to Medicaid and the next generation’s health (Working Paper No. 23810). National Bureau of Economic Research. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eccles JS (1999). The development of children ages 6 to 14. Future of Children: When School Is Out, 9, 30– 44. [PubMed] [Google Scholar]
- Elliott L, & Bachman HJ (2018). How do parents foster young children’s math skills? Child Development Perspectives, 12(1), 16–21. [Google Scholar]
- Fiese BH, & Schwartz M (2008). Reclaiming the family table: Mealtimes and child health and well-being. Society for Research in Child Development Social Policy Report, 22(4). [Google Scholar]
- Frean M, Gruber J, & Sommers BD (2017). Premium subsidies, the mandate, and Medicaid expansion: Coverage effects of the Affordable Care Act. Journal of Health Economics, 53, 72–86. [DOI] [PubMed] [Google Scholar]
- Gassman‐Pines A, & Hill Z (2013). How social safety net programs affect family economic well‐being, family functioning, and children’s development. Child Development Perspectives, 7(3), 172–181. [Google Scholar]
- Glied SA, Collins SR, & Lin S (2020). Did the ACA lower Americans’ financial barriers to health care? A review of evidence to determine whether the Affordable Care Act was effective in lowering cost barriers to health insurance coverage and health care. Health Affairs, 39(3), 379–386. [DOI] [PubMed] [Google Scholar]
- Goldin J, Lurie IZ, & McCubbin J (2019). Health insurance and mortality: Experimental evidence from taxpayer outreach (Working Paper No. 26533). National Bureau of Economic Research. [Google Scholar]
- Goodman-Bacon A (2017). Public insurance and mortality: Evidence from Medicaid implementation. Journal of Political Economy, 126(1), 216–262. [Google Scholar]
- Gopalan M, Lombardi C, & Bullinger LR (2021). Effects of Parental Public Health Insurance Eligibility on Parent and Child Health Outcomes. SocArXiv. 10.31235/osf.io/vghk6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gresham FM, & Elliott SN (1990). Social skills rating system: Manual. American Guidance Service. [Google Scholar]
- Grooms J, & Ortega A (2019). Examining Medicaid expansion and the treatment of substance use disorders. AEA Papers and Proceedings, 109, 187–192. [Google Scholar]
- Haley J, Kenney GM, Wang R, Pan C, Lynch V, & Buettgens M (2019). Improvements in uninsurance and Medicaid/CHIP Participation among children and parents stalled in 2017. Urban Institute. [Google Scholar]
- Hamersma S, Kim M, & Timpe B (2019). The effect of parental Medicaid expansions on children’s health insurance coverage. Contemporary Economic Policy, 37(2), 297–311. [Google Scholar]
- He Q, & Barkowski S (2020). The effect of health insurance on crime: Evidence from the Affordable Care Act Medicaid expansion. Health Economics. [DOI] [PubMed]
- Hill NE, & Tyson DF (2009). Parental involvement in middle school: A meta-analytic assessment of the strategies that promote achievement. Developmental Psychology, 45(3), 740–763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Himmelstein G (2019). Effect of the Affordable Care Act’s Medicaid expansions on food security, 2010–2016. American Journal of Public Health, 109(9), 1243–1248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hudson JL, & Moriya AS (2017). Medicaid expansion for adults had measurable ‘welcome mat’ effects on their children. Health Affairs, 36(9), 1643–1651. [DOI] [PubMed] [Google Scholar]
- Jacob BA (2005). Accountability, incentives and behavior: The impact of high-stakes testing in the Chicago Public Schools. Journal of Public Economics, 89(5–6), 761–796. [Google Scholar]
- Johnston EM, Strahan AE, Joski P, Dunlop AL, & Adams EK (2018). Impacts of the Affordable Care Act’s Medicaid expansion on women of reproductive age: Differences by parental status and state policies. Women’s Health Issues, 28(2), 122–129. [DOI] [PubMed] [Google Scholar]
- Joyce T & Racine A (2005). CHIP shots: Association between the state children’s health insurance program and immunization rates. Pediatrics, 115(5), e526–e534. [DOI] [PubMed] [Google Scholar]
- Kaestner R, Garrett B, Chen J, Gangopadhyaya A, & Fleming C (2017). Effects of ACA Medicaid expansions on health insurance coverage and labor supply. Journal of Policy Analysis and Management, 36(3), 608–642. [DOI] [PubMed] [Google Scholar]
- Kowaleski-Jones L, & Duncan GJ (1999). The structure of achievement and behavior across middle childhood. Child Development, 70, 930– 943. [Google Scholar]
- Kraft MA (2020). Interpreting effect sizes of education interventions. Educational Researcher, 49(4), 241–253. [Google Scholar]
- Levine PB, & Schanzenbach D (2009). The impact of children’s public health insurance expansions on educational outcomes. In Forum for Health Economics & Policy (Vol. 12, No. 1). De Gruyter. [Google Scholar]
- Longo F, Lombardi CM & Dearing E (2017). Family investments in low-income children’s achievement and socioemotional functioning. Developmental Psychology, 53(12), 2273–2289. [DOI] [PubMed] [Google Scholar]
- Maclean JC, & Saloner B (2019). The effect of public insurance expansions on substance use disorder treatment: Evidence from the Affordable Care Act. Journal of Policy Analysis and Management, 38(2), 366–393. [PMC free article] [PubMed] [Google Scholar]
- Mazurenko O, Balio CP, Agarwal R, Carroll AE, & Menachemi N (2018). The effects of Medicaid expansion under the ACA: A systematic review. Health Affairs, 37(6), 944–950. [DOI] [PubMed] [Google Scholar]
- McMorrow S, Gates JA, Long SK, & Kenney GM (2017). Medicaid expansion increased coverage, improved affordability, and reduced psychological distress for low-income parents. Health Affairs, 36(5), 808–818. [DOI] [PubMed] [Google Scholar]
- Meinhofer A, & Witman AE (2018). The role of health insurance on treatment for opioid use disorders: Evidence from the Affordable Care Act Medicaid expansion. Journal of Health Economics, 60, 177–197. [DOI] [PubMed] [Google Scholar]
- Miller S, Johnson N, & Wherry LR (2021). Medicaid and Mortality: New Evidence From Linked Survey and Administrative Data*. The Quarterly Journal of Economics, 136(3), 1783–1829. [Google Scholar]
- Miller S, Hu L, Kaestner R, Mazumder B, & Wong A (2021). The ACA Medicaid Expansion in Michigan and Financial Health. Journal of Policy Analysis and Management, 40(2), 348–375. [Google Scholar]
- Miller S, & Wherry LR (2017). Health and access to care during the first 2 years of the ACA Medicaid expansions. New England Journal of Medicine, 376(10), 947–956. [DOI] [PubMed] [Google Scholar]
- Morgan PL, Staff J, Hillemeier MM, Farkas G, & Maczuga S (2013). Racial and ethnic disparities in ADHD diagnosis from kindergarten to eighth grade. Pediatrics, 132(1), 85–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morrill MS (2018). Special education financing and ADHD medications: A bitter pill to swallow. Journal of Policy Analysis and Management, 37(2), 384–402. [DOI] [PubMed] [Google Scholar]
- Morrissey TW (2012). Health reform and child health: Progress, cautions, and future directions. Child Development Perspectives, 6(2), 199–205. [Google Scholar]
- National Conference of State Legislatures (2014). Authority to formulate and approve state education standards. Retrieved from: https://www.ccrslegislation.info/ccr-state-policy-resources/adopting-agency/
- Qureshi JA, & Gangopadhyaya A (2021). Childhood Medicaid Eligibility and Human Capital. Economics of Education Review, 82, 102092. 10.1016/j.econedurev.2021.102092 [DOI] [Google Scholar]
- Sénéchal M, & LeFevre JA (2002). Parental involvement in the development of children’s reading skill: A five‐year longitudinal study. Child Development, 73(2), 445–460. [DOI] [PubMed] [Google Scholar]
- Simon K, Soni A, & Cawley J (2017). The impact of health insurance on preventive care and health behaviors: Evidence from the first two years of the ACA Medicaid expansions. Journal of Policy Analysis and Management, 36(2), 390–417. [DOI] [PubMed] [Google Scholar]
- Sommers BD, Arntson E, Kenney GM, & Epstein AM (2013). Lessons from early Medicaid expansions under health reform: Interviews with Medicaid officials. Medicare & Medicaid Research Review, 3(4). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sommers BD, Baicker K, & Epstein AM (2012). Mortality and access to care among adults after state Medicaid expansions. New England Journal of Medicine, 367(11), 1025–1034. [DOI] [PubMed] [Google Scholar]
- Sommers BD, Gunja MZ, Finegold K, & Musco T (2015). Changes in self-reported insurance coverage, access to care, and health under the Affordable Care Act. JAMA, 314(4), 366–374. [DOI] [PubMed] [Google Scholar]
- Soni A, Wherry LR, & Simon KI (2020). How have ACA insurance expansions affected health outcomes? Findings from the literature. Health Affairs, 39(3), 371–378. [DOI] [PubMed] [Google Scholar]
- Tourangeau K, Nord C, Lê T, Wallner-Allen K, Vaden-Kiernan N, Blaker L, & Najarian M (2018). Early Childhood Longitudinal Study, Kindergarten Class of 2010 –11 (ECLS-K:2011), User’s manual for the ECLS-K:2011. National Center for Education Statistics. [Google Scholar]
- Ugwi P, Lyu W, & Wehby GL (2019). The effects of the Patient Protection and Affordable Care Act on children’s health coverage. Medical Care, 57(2), 115–122. [DOI] [PubMed] [Google Scholar]
- Vogler J (2020). Access to healthcare and criminal behavior: Evidence from the ACA Medicaid expansions. Journal of Policy Analysis and Management, 39(4), 1166–1213. [Google Scholar]
- Votruba-Drzal E (2006). Economic disparities in middle childhood development: Does income matter? Developmental Psychology, 42, 1154– 1167. [DOI] [PubMed] [Google Scholar]
- Wehby GL, & Lyu W (2018). The impact of the ACA Medicaid expansions on health insurance coverage through 2015 and coverage disparities by age, race/ethnicity, and gender. Health Services Research, 53(2), 1248–1271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wherry LR, & Miller S (2016). Early coverage, access, utilization, and health effects associated with the Affordable Care Act Medicaid expansions: A quasi-experimental study. Annals of Internal Medicine, 164(12), 795–803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wisk LE, Peltz A, & Galbraith AA (2020). Changes in health care–related financial burden for U.S. families with children associated with the Affordable Care Act. JAMA Pediatrics, 174(11), 1032–1040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yeung WJ, Linver MR, & Brooks-Gunn J (2002). How money matters for young children’s development: Parental investment and family processes. Child Development, 73, 1861–1879. [DOI] [PubMed] [Google Scholar]
- Zewde N, Eliason E, Allen H, & Gross T (2019). The effects of the ACA Medicaid expansion on nationwide home evictions and eviction-court initiations: United States, 2000–2016. American Journal of Public Health, 109(10), 1379–1383. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


