I. Introduction
This year, about 569,490 Americans, greater than 1,500 people a day, are expected to die of cancer. Cancer has supplanted heart disease as the leading cause of death in the United States in men and women under the age of 85 years (American Cancer Society, Facts and Figures 2010). Cancer also has a major economic impact on the US economy, with 2010 estimates of cancer associated costs of $263.8 billion (American Cancer Society, Facts and Figures 2010). The four most common cancers (lung, colorectal, prostate, and breast cancer) account for more than half of all cancer incidences in the United States. Surgery, chemotherapy and radiotherapy are the most established therapies for patients with these malignancies (American Cancer Society, Facts and Figures 2010). Surgery continues to be the most effective therapy for cancer in the United States. It is several-fold more effective than chemotherapy and radiation in curing patients with cancer. Unfortunately, many people are not surgical candidates due to advanced stage disease or co-morbid conditions.
Over the last two decades, both mortality and observed cancer survival statistics have improved dramatically both in patients that do and do not undergo surgery. This likely reflects an improvement in cancer care in the United States. Since 1973, the Survival Epidemiology and End Results (SEER) Program sponsored by the National Cancer Institute has kept a publicly-accessible database that has cataloged the outcome of cancer patients (Surveillance, Epidemiology, and End Results Program. Bethesda, SEER Stat Database). These data include information regarding incidence and mortality, as well as the initial surgical and adjuvant therapy provided for the treatment of cancer. This improvement in survival and mortality in this database over the last 20 years is likely due to better screening and detection, biologically targeted systemic therapies, improved surveillance, improved surgical methods, improved patient selection, and more effective adjuvant therapies. Cancer surveillance has also improved dramatically with the improvement in preoperative imaging and minimally invasive and non-invasive staging techniques such as mammography, colonoscopy, endobronchial ultrasound and prostate-specific antigen testing.
The goal of this short discussion is to highlight some of the trends that have been observed in cancer and surgery over the last twenty years and the role that surgery continues to play in the oncologic community. We found that surgery still remains an effective therapy for solid tumors in the United States and dramatically improves survival rates for patients with solid tumors. The proportion of cancer patients undergoing surgery has declined over the last 20 years for all major cancer types. Additionally, we found that local and systemic recurrences continue to be the Achilles heel of Surgical Oncology: although surgery does improve survival, almost one-third of surgical patients will ultimately recur locally and/or systemically. This is an important reminder to surgeons that we must work diligently to improve cancer care for our patients preoperatively, intraoperatively and postoperatively in order to prevent these recurrences. Research and clinical trials should be focused on this major objective in the coming decades.
II. Cancer Survival Has Improved Over the Last Twenty Years
In the United States, surgical resection currently offers the best opportunity to cure solid tumor malignancies. On reviewing the SEER database data obtained from 2000–2004, we found a total of 777,136 out of 1,190,322 registered patients with solid organ cancers who underwent surgery. When examining post-operative five-year survivals for the four most commonly diagnosed cancers, Kaplan-Meier analysis demonstrates significant survival benefits for patients qualifying for surgery resection (Figure 1a). The most dramatic increase in observed survival was seen in lung cancer, with an increase in survival for surgical versus nonsurgical cohorts of 11 fold at 5 years (Figure 1b). Increases of 3.7 and 2.5 fold were seen in modern colorectal and breast cancer cohorts, respectively; while only a 1.2 fold increase was noted in contemporary prostate cancer cohorts (Figure 1b). A weighted average of patients who underwent surgery for these malignancies yielded a five year survival of 74.8% versus 42.1% in nonsurgical patients. It is important to interpret these survival benefits with the understanding that various factors including histology, stage, and comorbidities influence surgical candidacy, and likely confound long-term outcomes.
Figure 1:
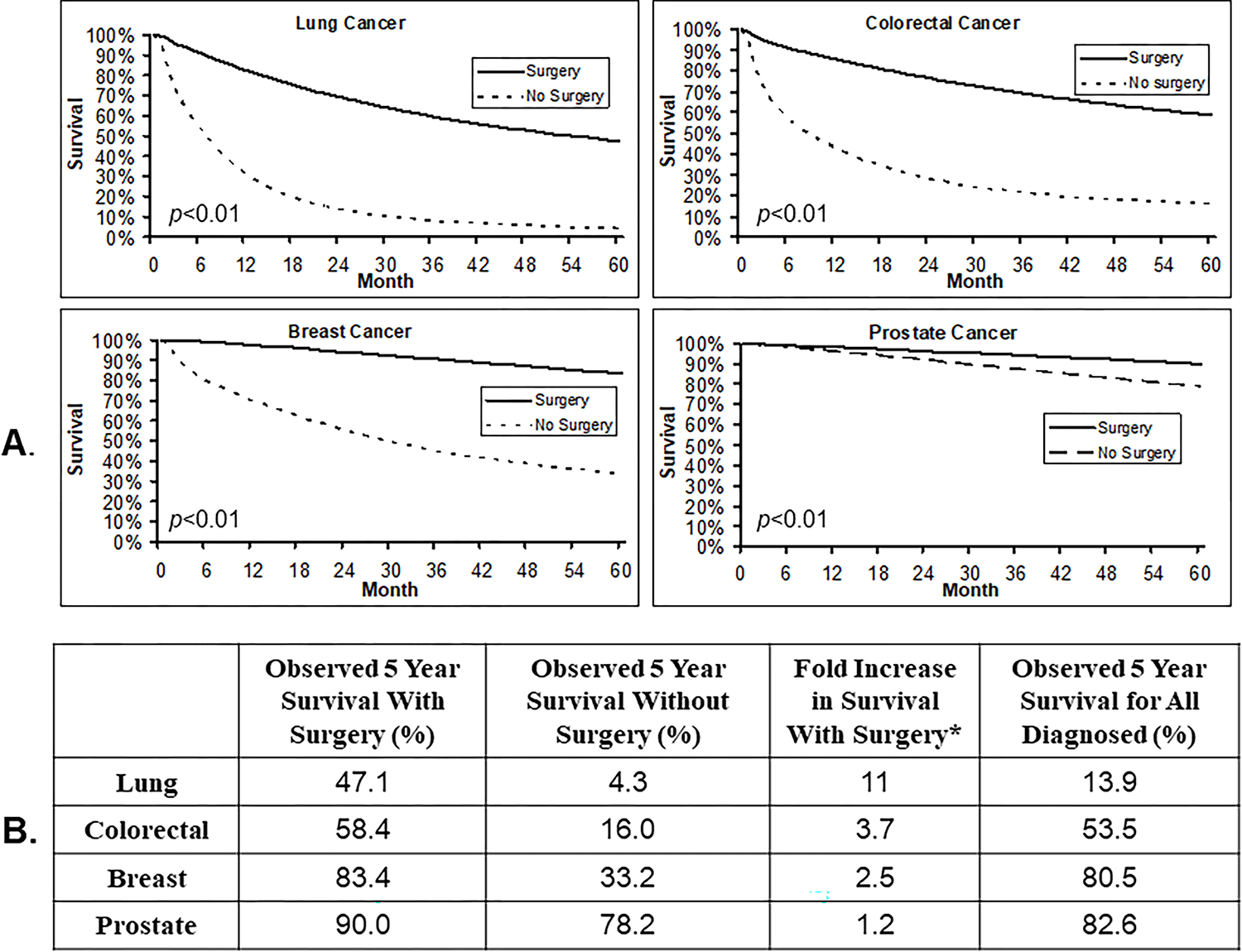
Representation of 5 year survival among patients diagnosed with Lung, Colorectal, Breast, and Prostate Cancers. Data were obtained from SEER database using SEER*Stat software (A) Kaplan-Meier analysis demonstrating survival benefits observed in patients undergoing surgery versus no surgery. (B) Tabulation of survival statistics for those diagnosed with Lung, Colorectal, Breast, and Prostate Cancers.
* values were calculated using the following equation: (observed 5 year survival with surgery)/(observed 5 year survival without surgery)
Clearly, the importance of surgery’s role in the oncology community is well established; however, the proportion of patients with cancer undergoing surgery for lung, breast, colorectal, and prostate cancers has decreased over the twenty years. Between 1983–1987, 71.6% of patients diagnosed with these tumors were treated surgically, versus 65.3% of those patients diagnosed between 2000–2004. The greatest decrease in proportion was 17% decrease observed in lung cancer, while breast cancer only slightly decreased by 1.1%. Prostate and colorectal cancers saw an overall decrease in the use of surgical intervention of 11.4% and 3.0%, respectively. This data almost certainly suggests improvements in non-surgical therapies (such as targeted biological therapies, chemotherapy and radiation therapy), along with an improvement in diagnostic imaging and testing that may reveal metastasis preoperatively thereby eliminating previously acceptable surgical candidates. Finally, changes in referral patterns and more aggressive medical and radiation oncology communities have had subtle effects in this finding.
Interestingly, on querying the SEER database using SEER*Stat (a statistical program that allows for specific searching of the SEER database), cancer survival of those qualifying for surgery was noted to have improved over the same time period. The most noteworthy improvements were in prostate cancer, which had an observed five-year survival of 59.7% for surgical patients during the 1983–1987 interval which improved to almost 90% during the 2000–2004 interval. Lung cancer patients undergoing surgery also improved their observed survival from 36.6% to 47.1%, a 28.7% increase. Breast and colorectal cancer saw improvements of 12.9% and 15%, respectively. These findings further support the essential role that surgery continues to play in the oncology field. Additionally, these findings give credence to the notion that tremendous strides have been made in screening/surveillance protocols, identification of optimal surgical candidates, and development of more potent systemic therapies which can be effectively utilized as surgical adjuvants.
III. Cancer Recurrence Remains the Biggest Challenge in Patients Undergoing Surgery
The SEER database does not track information regarding cancer recurrences following curative surgery. We, thus, performed a focused literature review of published recurrence data from large reports. In searching for literature the keywords “recurrence AND post-operative” were used. Only papers published over the last seven years were included in our search. We ultimately selected the largest series for each cancer. Although this may not be truly representative, it provides a framework for discussion. Our review found a common trend among these four cancers: patients diagnosed with post-operative recurrence, regardless of being local or systemic, experience poorer five year survival when compared to total surgical candidates. This is likely a result of these patients already having received adjuvant chemotherapy and/or radiation, or requiring second line or salvage therapy. In addition, these patients performance status often decline following surgery and adjuvant therapy, making it more likely to have a complication from second line or salvage therapy.
When examining long-term outcome following surgery for lung cancer, we consulted two recent, large-scaled studies which were conducted at major US academic center 1, 2. The largest report by Sugimura et al., a four year study following 1,073 patients treated surgically for non-small cell lung cancer at the Mayo Clinic in Rochester, documented that 41.5% of patients recurred postoperatively (Figure 2a). Of these, 43.8% recurred locally only and 56.2% distantly (Figure 2b) 1. The other study, which was completed by Kelsey and colleagues at Duke University, focused on early stage NSCLC and yielded similar recurrence rates of 36%2. The pattern of recurrence; however, was slightly different with 25% of recurrences occurring locally only and 75% occurring distantly 2.
Figure 2:

Post-operative recurrence data for Lung, Colorectal, Breast and Prostate Cancers. Data were obtained from focused literature review. (A) Percentage of patients undergoing surgery that are susbsequently diagnosed with cancer recurrence within 5 years of initial surgical resection. (B) Postoperative recurrences by location: local versus systemic.
For these patients with post-operative lung cancer recurrences, the survival was dismal. According to Sugimura’s report, the overall two- and five-year survivals for this recurrent cohort were found to be 17% and 12%, respectively (Table 1) 1. This indicates that post-operative recurrences in lung cancer frequently occur early, leading to poor outcome. Of note, the author commented that additional treatment was not an option in about a third of patients due to rapid disease progression 1.
Table 1:
Five year post-operative survival following surgery
| Five Year Survival Following Surgery (%)* | Five Year Survival Following Surgery with Recurrence (%)** | |
|---|---|---|
| Lung | 47% | 12%; ref 1 |
| Colorectal | 58% | 26%; ref 4 |
| Breast | 83% | 26%; ref 7 |
| Prostate | 90% | 93%; ref 9 |
Includes both survivorship of those with and without recurrences. Data obtained from SEER database
Includes only survival data of those with post-operative cancer recurrences.
Estimations based on literature review.
To analyze postoperative recurrences in colorectal cancer, we first reviewed a recent study completed by Tsikitis and colleagues which reported on 791 patients involved in the National Cancer Institute’s Clinical Outcomes of Surgical Therapy Trial 3. The overall recurrence rate was found to be 18.5% (Figure 2a) 3. From the data presented in the Tsikitis paper we estimate that approximately 14% of these recurrences occurred locoregionally (at the site of resection or at a local lymph node), whereas approximately 86% of recurrences occurred distantly (Figure 2b) 3. A report by Guyot and colleagus, which describes the follow-up following more than 3,600 post-operative colorectal patients, supports the Tsikitis report: the overall recurrence rate was approximately 29%, with 31% occurring locally with 69% occurring distantly (Figure 2a& 2b) 4. According Guyot’s report, recurrences for colorectal cancer is also associated with decreases in post-operative survival 4. The overall 5-year survival rate was 21.6%for those presenting systemic recurrences and 31.6% for those with local recurrences 4. After appropriate weighting, the 5 year survival following recurrence for colorectal cancer was estimated to be 26.9% (Table 1).
Literature review analyzing recurrences and long-term outcomes following breast cancer surgery revealed a similar trend. First, in a Canadian study conducted by Voduc et al. describes a cohort of 4,033 women who either received breast conserving surgery (BCS) or total mastectomy between 1986 and 1992 5. The combined recurrence rate was 18.5% (Figure 2a) 5. A second study conducted by Giordano and her colleagues at M.D. Anderson Cancer Center describes 834 women who developed breast cancer recurrences between 1974 and 2000 6. According to Giordano’s work, the dominant site of recurrence was local in 24.8% of patients while almost 75% of patients had a dominant site that was systemic (Figure 2b) 6. Finally, a study following 1,558 patients in England between 1989 and 2003 revealed a recurrence rate of 18.9%, supporting Voduc’s study (Figure 2a) 7. This study, completed by Imkampe and colleagues, breaks the site of recurrence into four groups: local, lymph node, bone and visceral. For the purposes of discussion and comparison we consider local and nodal recurrence to be local and bone and visceral recurrences to be distant 7. Using this methodology, 39% of recurrences occurred locally versus 61% distantly (Figure 2b) 7.
As in colon cancer, survival post-recurrence in breast cancer is highly dependent on the location of recurrence. The three year survival in recurrent breast cancer was shown to be 83% for patients who recurred locally 7. Regional and systemic recurrence dramatically decrease three year survivals to 33% for patients with nodal recurrence, 23% for patients who bone recurrence, and 13% for visceral recurrences including lung, liver, peritoneally or the nervous system 7. Combined, the estimated three year survival and five year survivals were estimated to be 37% and 26%, respectively (Table 1) 7.
The primary means of surveillance in prostate cancer, both pre-diagnosis and post-therapy has become the Prostate-Specific Antigen (PSA) test. Clinicians frequently refer to biochemical recurrence in prostate cancer patients, and much of the literature focuses on biochemical recurrence. In a recent long-term study published by Agarwal et al. of Case Western Reserve, of 4,342 men who underwent radical prostatectomy, 1003 or 23.1% recurred biochemically (Figure 2a) 8. In a second study by Freedland and colleagues at Johns Hopkins, almost 19% of those undergoing radical prostatectomy had evidence of biochemical recurrence (Figure 2b) 9.
In conclusion, although all surgeons hope to cures all their patients, local and systemic recurrences remain the main failure after surgery. Based on our literature search, as many as 20% to 40% of patients will recur following surgery. Overall, approximately 621,709 patients in the United States undergo surgery annually, and based on our study of the four most common cancers, we extrapolate that somewhere between 120,000 and 250,000 patients will suffer from a post-operative recurrence of their disease.
IV. Conclusion
Currently, in the United States, cancer patients are treated with either surgery, chemotherapy, or radiation, or a combination of these approaches. Surgery is the single most effective therapy for these cancers. For most cancers, survival for patients who undergo surgery increases anywhere from 2 to 10 fold compared to the same patients who are not surgical candidates. Although this may reflect the inherent benefits of cytoreduction, it is difficult to assess this as surgical candidacy is a product of various factors, thus, the ability to qualify for surgery immediately suggests earlier stage disease and a greater probability for a more favorable outcome.
Over the last 20 years, those patients qualifying for surgery has decreased. This is as a result of improved preoperative metastatic workup, alternative treatment strategies, and referral patterns in the United States. Despite this decrease in patients who qualify for surgery, the survival following the surgery has improved dramatically. Survival after surgery has improved for a variety of reasons. One explanation is due to improved preoperative staging. Advances in this area account for those patients who were previously thought to have early stage disease but are discovered to have advanced stage disease, ultimately do not undergo surgery. Secondly, improved screening regimen (colonoscopy, mammography, digital rectal exam, etc.) are better equipped to detect malignancies at early stages which sets the stage for better post-operative outcomes. Finally, adjuvant therapies have improved significantly in all cancer types, most notably in lung cancer and breast cancer.
The most important challenge to this surgical community is preventing recurrences. Recurrences tend to be the most common cause of failure in our community. Different cancers tend to favor either local versus systemic recurrence. This is largely related to disease biology and less likely to intraoperative issues.
Even in those patients that develop recurrences after surgery, five year survival following recurrence is still higher than those patients that did not initially qualify for surgery. Again, this may reflect the stage or histology of the disease at the initial presentation. This data suggests oncology surgeons have a clear opportunity for significant improvement in our field, specifically in preventing recurrences.
Surgeons have the opportunity to influence care in three areas for their patients: preoperatively, intraoperatively and postoperatively. Research and support of surgical investigations must focus on all aspects of patient care. Better staging and assessment preoperatively combined with neoadjuvant therapies for cancer subsets must continue to be evaluated in rigorous clinical trials. Intraoperative techniques to examine surgical margins, destroy residual disease and to detect metastatic lymph nodes have been revisited with imaging, rapid PCR testing, intraoperative photodynamic therapy and sentinel lymph node mapping. Immunotherapeutic approaches to alter perioperative immunosuppression to limit recurrences may have important prophylactic effects 10. Finally, postoperative therapies need to be explored and revisited with the medical and radiation oncology community. This provides ample evidence, and more importantly an opportunity, for surgeons to dedicate efforts in ongoing investigations in preventing postoperative recurrences. Advancements aimed at recurrence elimination would have a tremendous impact, and improve the lives of more than 100,000 individuals, each year, in the United States alone.
Synopsis:
Surgery remains the most effective treatment for solid-organ malignancies; however, more than half of cancer patients in the United States undergoing surgery develop recurrences within five years. These recurrences account for most postoperative deaths in Surgical Oncology, therefore, this is the most pressing challenge to our field. Our report describes recent recurrence trends from the SEER database, and we propose treatment strategies and potential solutions that should be considered as our field moves forward to minimize post-operative cancer recurrences.
Ackowledgements:
L.A.was supported from the Lavin Family Supporting Foundation. J.P. was supported by a Doris Duke Charitable Foundation Research Grant. S.S. was supported by the National Institutes of Health (K12CA076931) & American Cancer Society (#IRG-78-002-30).
References:
- 1.Sugimura H, Nichols FC, Yang P, et al. Survival after recurrent nonsmall-cell lung cancer after complete pulmonary resection. Ann Thorac Surg 2007; 83(2):409–17; discussioin 417–8. [DOI] [PubMed] [Google Scholar]
- 2.Kelsey CR, Marks LB, Hollis D, et al. Local recurrence after surgery for early stage lung cancer: an 11-year experience with 975 patients. Cancer 2009; 115(22):5218–27. [DOI] [PubMed] [Google Scholar]
- 3.Tsikitis VL, Malireddy K, Green EA, et al. Postoperative surveillance recommendations for early stage colon cancer based on results from the clinical outcomes of surgical therapy trial. J Clin Oncol 2009; 27(22):3671–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Guyot F, Faivre J, Manfredi S, et al. Time trends in the treatment and survival of recurrences from colorectal cancer. Ann Oncol 2005; 16(5):756–61. [DOI] [PubMed] [Google Scholar]
- 5.Voduc KD, Cheang MC, Tyldesley S, et al. Breast cancer subtypes and the risk of local and regional relapse. J Clin Oncol; 28(10):1684–91. [DOI] [PubMed] [Google Scholar]
- 6.Giordano SH, Buzdar AU, Smith TL, et al. Is breast cancer survival improving? Cancer 2004; 100(1):44–52. [DOI] [PubMed] [Google Scholar]
- 7.Imkampe A, Bendall S, Bates T. The significance of the site of recurrence to subsequent breast cancer survival. Eur J Surg Oncol 2007; 33(4):420–3. [DOI] [PubMed] [Google Scholar]
- 8.Agarwal PK, Sadetsky N, Konety BR, et al. Treatment failure after primary and salvage therapy for prostate cancer: likelihood, patterns of care, and outcomes. Cancer 2008; 112(2):307–14. [DOI] [PubMed] [Google Scholar]
- 9.Freedland SJ, Humphreys EB, Mangold LA, et al. Risk of prostate cancer-specific mortality following biochemical recurrence after radical prostatectomy. Jama 2005; 294(4):433–9. [DOI] [PubMed] [Google Scholar]
- 10.Shakhar G, Ben-Eliyahu S. Potential prophylactic measures against postoperative immunosuppression: could they reduce recurrence rates in oncological patients? Ann Surg Oncol 2003; 10(8):972–92. [DOI] [PubMed] [Google Scholar]


