Abstract
Background:
Dental sealants are effective in the prevention of dental caries in children at elevated risk levels and are a Healthy People 2030 objective. Electronic health record (EHR)-based clinical decision support systems (CDSS) have demonstrated the ability to improve patient care provided. A dental quality measure (DQM) related to dental sealant placement for children at elevated risk of caries was targeted for improvement using a CDSS.
Methods:
A validated DQM was adapted to assess an individual patient’s need for dental sealant placement. A CDSS was implemented to advise the care team if a child was at elevated caries risk and had sealant-eligible first or second molars. Data on dental sealant placement at examination visits over a 5-year period were analysed, including 32 months prior to CDSS implementation and 28 months post-implementation.
Results:
Between January 1, 2018, and December 31, 2022, 59,047 examination visits for children at elevated caries risk with sealant-eligible teeth were assessed. With the implementation of CDSS and training to support the clinical care team in September 2020, the appropriate placement of dental sealants at examination visits increased from 27% to 60% (p < 0.00001).
Conclusion:
Integration of CDSS into an EHR as part of a quality improvement program was effective in increasing the delivery of sealants in eligible first and second molars of children aged 5–15 considered at high caries risk.
Practical Implications:
EHR-based CDSS can be implemented that improve standardization and the provision of timely and appropriate patient care in dental practices.
Keywords: Preventive care, Evidence-based dentistry, Decision Support Systems, Dental Caries, Sealants, Quality Improvement, High caries risk
INTRODUCTION
Dental sealants are effective in the prevention of dental caries in adolescents with elevated caries risk during the formative years of adult dentition. When sealants are placed appropriately on the first and second molars of children with elevated risk of caries, including molars with deep pits and fissures, they have been proven to reduce the development of caries on these teeth.1 Sealants placed on children at low risk of caries do not provide similar benefits and have no measurable impact on the prevention of caries.2
Given that sealants are an evidence-based treatment in preventing and arresting pit and fissure occlusal caries in molars, increasing the proportion of children and adolescents who have dental sealants on one or more molars is a Healthy People 2030 objective with a 42.5% target.3 However, even with this focus from the US Department of Health and Human Services, only 37% of children and adolescents aged 3 to 19 had received dental sealants during reporting years of 2013–2016, regardless of caries risk status.3
Willamette Dental Group (WDG) is a privately held, accountable care, risk-bearing entity that provides oral health care for more than 450,000 members at 50 practices across Oregon, Washington, and Idaho. Delivery of high-quality evidence-based and preventative care has been a core practice and expectation of WDG dental providers for decades. Historically, adherence to guidelines for placement of dental sealants at WDG has been measured through annual metrics supplemented by a manual chart audit process with follow up training and mentorship as needed.
Dental quality measures (DQMs) provide a valuable tool to assess and analyze the performance of a practice, population, or individual care provider. The Dental Quality Alliance (DQA) has taken leadership in development and promotion of DQMs. The DQA has published measures that rely primarily on claims-based data to report results related to utilization and quality of dental services for adults and children enrolled in public and private insurance programs.4 When assessed across an enterprise, DQMs reveal trends, inconsistencies, and disparities in care that can be acted upon as part of a quality improvement process. While DQMs can provide accurate results upon the end of the measurement period, they are commonly unable to accurately assess results during the measurement period. This limits the ability of DQMs to deliver real time evidence to aid in the regular cycle of a quality improvement program and improve timely delivery of appropriate care.
With the implementation of DQMs for dental sealants, the sealant placement rate at WDG, while meeting national benchmarks, was assessed as both generally lower than expectations and inconsistent across the organization, with variation of rates between offices.5 Inconsistent results across offices or longitudinally over time present opportunities for quality improvement in attempts to reduce this variation.6 The appropriate placement of sealants was identified as an opportunity for an organizational quality improvement effort.
A key challenge to increasing the appropriate placement of dental sealants was identified for patients who were planned for sealants but did not return for the procedure. Placing dental sealants is a relatively quick procedure and can often be delivered as a same-day service during a routine recall visit. This is time saving and cost-effective for the patient and office, preventing the need for an extra visit, and hence could increase the placement rate of sealants.
With the objective to increase the rate of appropriate sealant placement and ultimately lower the incidence of dental caries in their pediatric (ages 5 to 15) population, an electronic health record (EHR)-delivered clinical decision support system (CDSS) was implemented. We evaluated the impact of this CDSS to assist the WDG clinical care team to provide same-day sealants when appropriately indicated for children at an elevated risk for caries. A CDSS seeks to provide actionable information at the point of care to make it easier to provide the right care.7 We know from multiple randomized controlled trials that well-implemented CDSSs, employing suitable patient data, derived from rich EHR repositories, can produce large and important improvements in care processes.8 Notably, CDSSs are thought to mitigate medication errors, improve patient safety through reminder alerts, increase adherence to clinical guidelines, reducing test duplication, and can provide support for diagnostic coding and ordering of tests.9
METHODS
A team of oral health care professionals and informatics analysts adapted the logic from an earlier developed DQM for dental sealant placement,5 to a per visit measure to assess an individual patient’s need for sealants at each visit. The DQM for sealant placement provided logic to assess if patients with sealable teeth received a sealant during the annual reporting period.10 To provide the clinical care team with decision support at the time of visit, this logic was adapted to automatically assess a patient’s appropriateness for sealant placement at each exam visit. The CDSS identified patients meeting the criteria of age, between 5 and 15 years, and elevated caries risk assessment (CRA), moderate, high, or extreme, and further evaluated each case for any sealant-eligible teeth. IRB approval was obtained to conduct this study and STROBE guidelines were followed.
Sealant-eligible teeth were determined from the EHR data as any fully erupted first or second permanent molars that had not previously been sealed, treated, planned for treatment, or diagnosed with caries. Past and planned treatment included any restoration, except for class V buccal or facial surface restorations, endodontic procedure, including pulpotomy, pulpectomy or root canal therapy, extraction or fixed prosthodontic procedure that was either previously completed or was planned for the tooth. Diagnosis of caries was assessed based on the documentation of active caries on the tooth except for buccal and facial surface caries only. Active caries and planned and completed restorations on the buccal and facial surface were excluded as their presence alone, in absence of any occlusal caries or procedure, should not preclude the placement of dental sealants on a tooth.
At examination visits, children meeting the criteria for age and elevated CRA with at least one sealant-eligible tooth activated the CDSS to remind the clinical care team of the indication for placement of dental sealants. The CDSS is implemented as a passive checklist of process and disease-prevention tasks for the care team to review and complete at each visit. The checklist is automatically updated from EHR data as tasks are completed for the visit. The CDSS includes process measures to enforce completion of CRA, “base” charting including dentition, existing restorations and findings, and planned procedures recorded with a dental diagnosis. Overall, the WDG providers routinely complete over 98% of these process measures.11 The process measures are supplemented with a Quality Improvement Score (QIS) comprised of several measures for appropriateness of care including prevention metrics for completion of sealants and fluoride.
For each visit, the CDSS (Figure 1) presents the clinical care team with a set of tasks appropriate for the type of visit, examination, operative, hygiene or emergency, and patient factors considering age, dentition, risk factors and history. Feedback clearly highlights any outstanding or overdue tasks and includes evidence to support the suggested care. The format is educational for the care team, supporting their delivery of care meeting evidence-based standards adopted by the organization while also aiding with communication with the patient. Additionally, a clinical dashboard is available to monitor performance and trends and identify opportunities for improvement for each office/provider (Figure 2).
Figure 1:
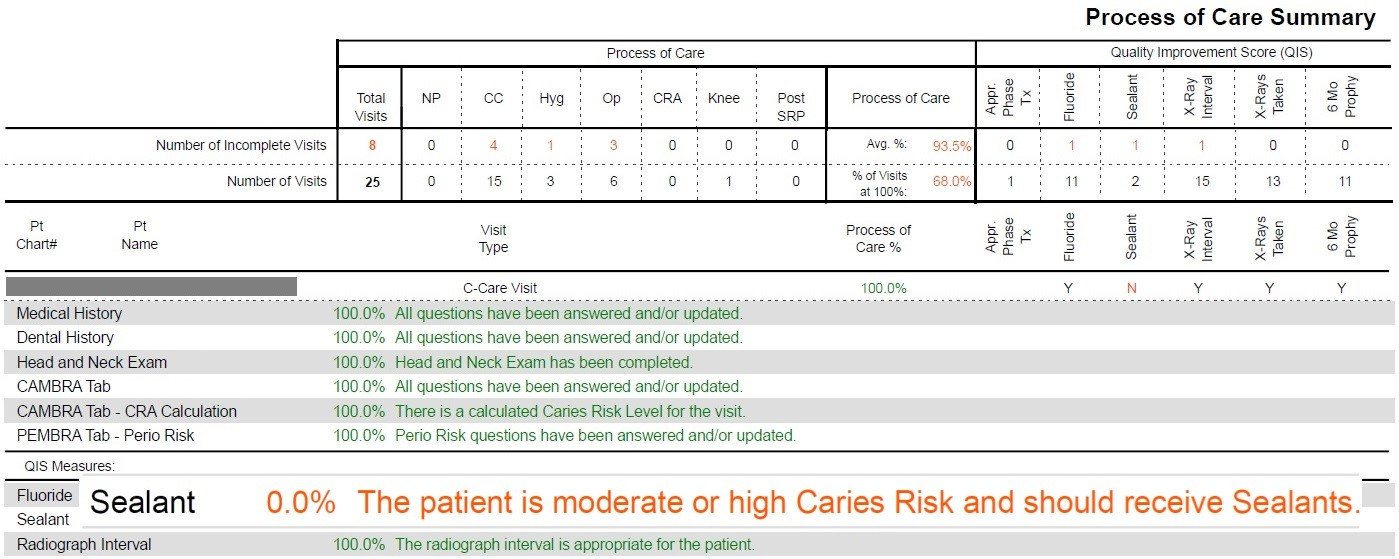
CDSS: Process of Care summary, highlighting the Sealant measure.
Figure 2:
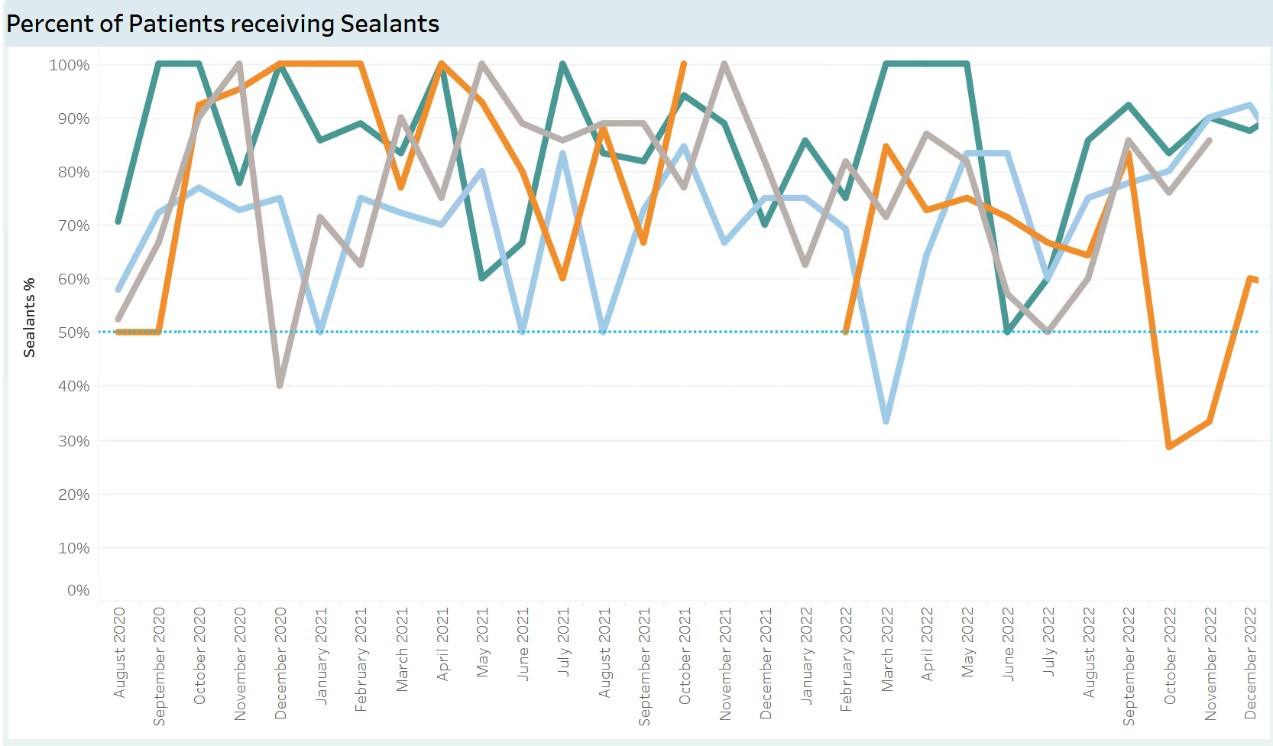
Dashboard to monitor sealant placement performance and trend for individual doctors at an office. Colored lines on the chart each represent a provider.
Rather than employing pop-up messages that have been commonly used for CDSS interventions and have shown to contribute to provider fatigue,12 the system is passive allowing the care team to work through each visit, reviewing and completing tasks as needed. A percentage completion indicator, showing visit progress as a number between 0 to 100% is displayed in the EHR’s task bar. As tasks are completed, the progress indicator increases, and the care team’s goal is to achieve the 100% completion for each visit before the patient leaves. A summarized view of daily patients seen, with analysis to the patient level, allows the office to manage their cases effectively.
Data on pediatric examination visits over a 5-year period, January 1, 2018, to December 31, 2022, were queried directly from the EHR database. The CDSS for sealant placement was implemented in September 2020, providing 32 months of pre-implementation data and 28 months post-implementation data to compare. The rates of sealant placement, as a percentage of sealant-eligible examination visits for children with elevated CRA, were calculated pre- and post-implementation of CDSS, and rate comparisons were completed by office with a paired-samples t-test. Appropriate dental sealant placement in eligible patients’ rates by month were calculated and included in a p control chart (Figure 3) with upper and lower control limits (±2 standard deviations). Patients were excluded from the analysis if CRA was low or not documented or if no sealant-eligible teeth were present at the examination visit.
Figure 3:
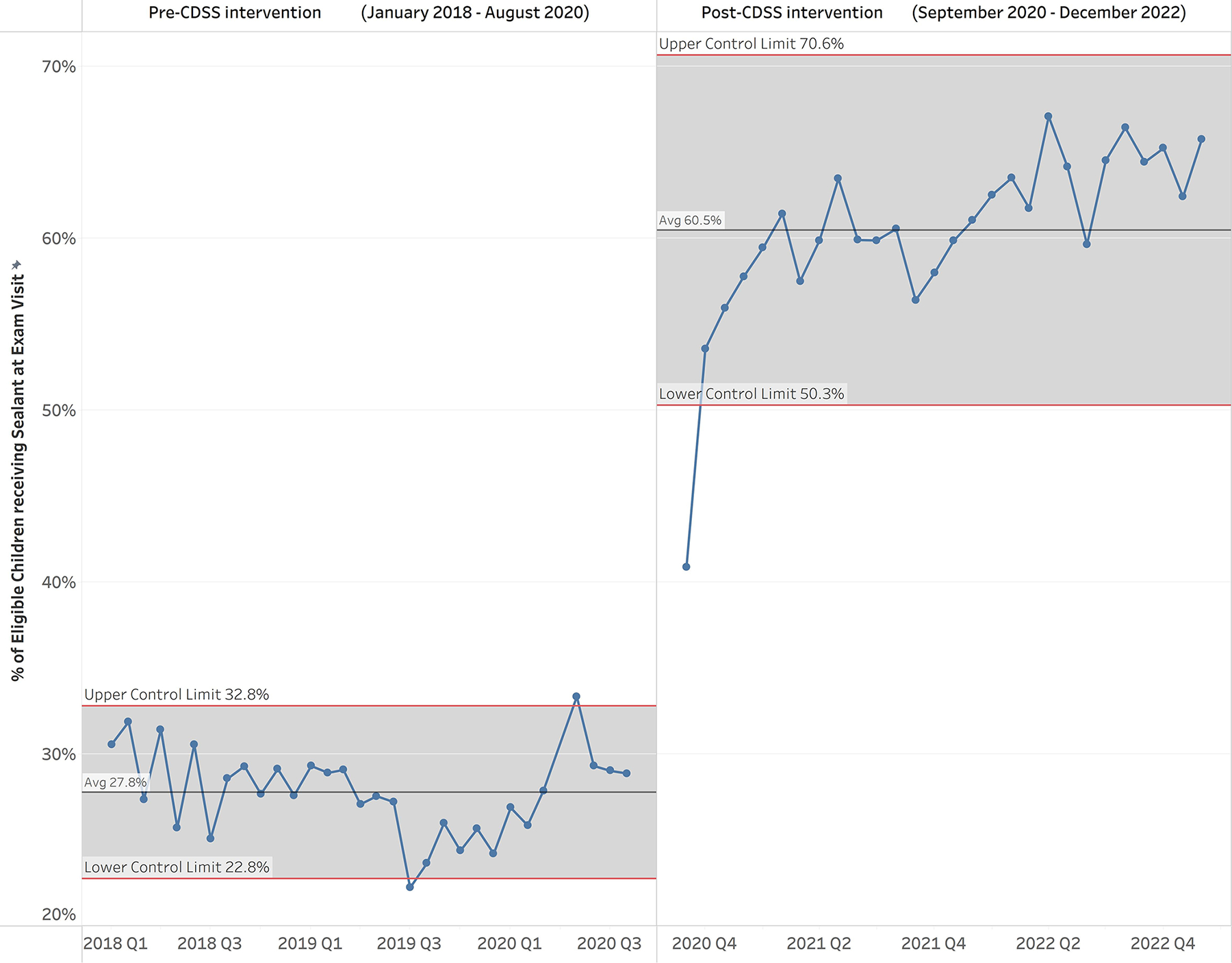
P control chart of percentage of eligible children receiving dental sealants at examination visits by month. Pre- and Post-CDSS intervention periods are separated.
RESULTS
Placement of sealants at comprehensive and periodic examination visits on children aged 5–15, with elevated caries risk, with first or second molars eligible for sealant(s), were measured pre- and post-implementation of the CDSS tool across a large network of nearly 50 clinics across Oregon, Washington, and Idaho. Over the 5-year period between January 1, 2018 and December 31, 2022, 59,047 examination visits (33,640 pre-implementation and 25,407 post-implementation) with children at elevated caries risk and sealant-eligible teeth were assessed.
Compliance with the evidence-based guidelines for appropriate sealant placement showed significant improvement across the entire organization following the CDSS implementation in September 2020. Overall, appropriate sealant placement at recall visits increased from an average below 30% (95% CI [22.8, 32.8]) prior to implementation of the CDSS to over 55% in the month following the CDSS implementation and maintaining consistently over 60% (95% CI [50.3, 70.6]) (Figure 3).
Based on this increased rate of appropriate sealant placement at examination visits, over the 28 months post-implementation, over 7,500 children at elevated risk of caries received sealants at their examination visit who may not have without the CDSS implementation.
A comparison of sealant placement by office for pre- and post-implementation of CDSS showed significant improvement in each of the offices that saw patients across the entire 5-year period (Figure 4). The mean pre-CDSS for sealant placement is 26.74%, while the mean post-CDSS is 58.74%. These data were subjected to the t test for paired samples, with the results showing a statistically significant improvement with a mean 32 percentage points (t = 14.14; n = 46; p < 0.00001) and Cohen’s d effect size of 2.08.
Figure 4:
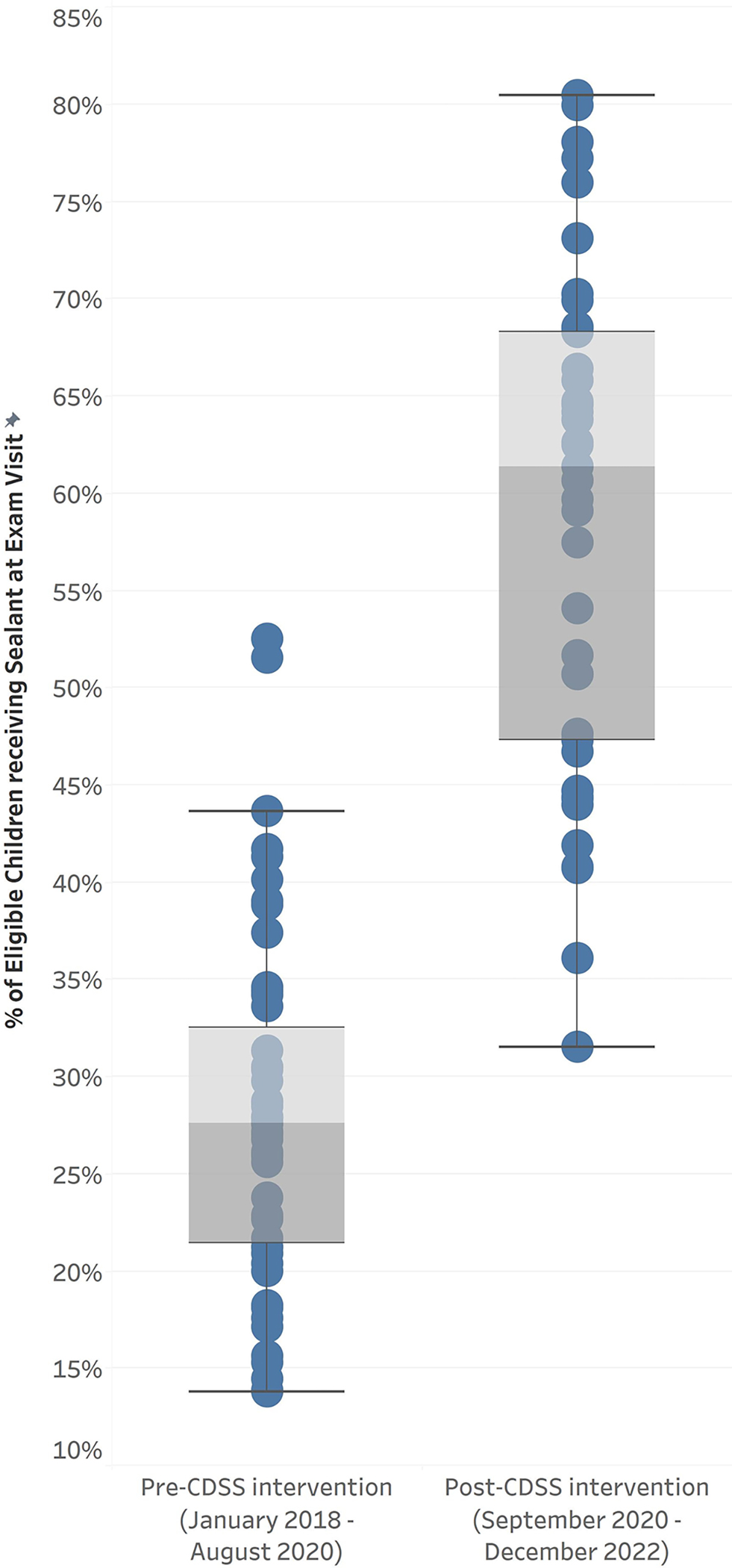
Variation of office performance on sealant placement measure, comparing Pre- and Post-CDSS implementation.
DISCUSSION
Many barriers to appropriate placement of sealants and guideline implementation have been identified from private practice to large group practices. For providers, these include personal clinical experiences, concerns over liability, lack of understanding of standard of practice, being unaware of expectations, and knowledge and attitude regarding sealants.13,14 In general, parents’ attitude towards the use of caries preventive measures, including placement of sealants is significantly correlated to their gender, dental experience, level of education and size of the family.15Additionally, concerns regarding the materials used represent some common reasons for not proceeding with sealant placement.16,17 Changing dentists’ behavior around adoptions and implementation of clinical guidelines for the placement of sealants is not straight forward or obvious. Indeed, Carney concluded that publishing and emphasizing evidence-based guidelines, even from established and respected sources are not enough to guide change.18 Additionally, efforts in quality improvement through focusing on provider education alone have shown limited effectiveness and decreased compliance over time.19
Evidence-based guidelines and readily accessible educational materials are clearly not enough to assure that all children in need of dental sealants have sealants placed, although some progress has been made as an objective for Healthy People 2020 and 2030. DQMs while a good starting place to initiate and measure the success of quality improvement programs, cannot provide CDSS to directly assist clinical care teams in the timely delivery of appropriate care. However, DQMs can be easily adapted to provide care teams with CDSS to aide in quality of care provided on a per visit basis. Through the implementation of systems that deliver timely, accurate, and appropriate evidence-based information, CDSS provide significant advantages in practice. These include improved clinical efficiencies, a more engaged care team and patient, that are both supplied with the additional support of evidence and consistent standards of care. Ultimately, the result is an increased likelihood of favorable health outcomes.
CDSS that are both intelligent and easy to interpret can be effective in augmenting clinical decision making, hence improving the quality of care provided to the patient. CDSS can be classified as either active or passive depending on the level of interruption to the providers’ natural workflow.20 Passive CDSS typically have minimal impact to workflow and serve as a gentle reminder to consider a suggested intervention.19 Passive CDSS can be introduced with subtle changes in note templates or other areas and have been shown to improve compliance with preventive services and standards of care over time.19,21,22 Studies have shown that active CDSS pop-ups are a nuisance, leading to “alert fatigue” and diminished physician adherence over time.12 WDG has experienced with different methods of CDSS, including pop-up reminders, and have found these systems struggle with providing the right information to the right user at the right time. WDG’s passive CDSS that summarizes the visit progress and details of incomplete tasks, provides the care team with a simple yet effective interface to review as needed during the delivery of care.
A review of the current clinical workflow was completed to fully assess the problem of why sealants were not being placed. Several factors were identified, including patients not returning for planned care, other treatments taking precedence, and patients changing providers or insurance plans. This investigation led to updating workflows, guidelines, expectations and the CDSS with recommendations to complete the sealants on the same day whenever possible. Placing sealants while the patient is already in the chair for a routine examination visit would remove some of the identified barriers to support increased sealant placement. Doing so is also a benefit for the organization and patient alike in saving time and cost of return visits while ensuring appropriate prevention was delivered as soon as possible.
To address the opportunity for improvement and consistency across the offices, WDG implemented CDSS to advise the clinical care team. For children at elevated caries risk with sealant-eligible first or second molars, CDSS suggested that the child met the clinical guidelines for placement of dental sealants. Additionally, an easily accessible dashboard was made available to show daily and weekly progress for each office/provider, allowing for review and adjustment as part of the quality improvement cycle. The CDSS in conjunction with the dashboard had a positive effect on number of sealants placed as part of the examination visit, significantly increasing the overall placement of appropriate dental sealants. Despite not implementing this change with a control group, there were no other operational, clinical, financial, or environmental changes occurring during this period that would contribute to the increase in sealant placement at examination visits.
The logic behind the CDSS for appropriate sealant placement is complex, with well thought out parameters to consider patient appropriateness and visit needs as they relate to evidence-based standards of care. A significant challenge of measuring appropriate sealant placement is in the assessment of teeth eligible for sealants. This requires complete baseline charting and confirmation of the full eruption of the first and second molars. WDG completes full charting of all patients, yet there are still cases where documentation of eruption status is incomplete.
The measure is further complicated by the dependency on the CRA to determine that the patient would benefit from the sealant placement. Risk assessments are mostly clinician-dependent and are subject to incomplete and inaccurate data collection. Electronic data is vital to the ability to measure and provide accurate CDSS. WDG has implemented an effective CDSS for process management to ensure that each patient visit is thoroughly documented, including CRA and diagnoses for all patients and procedures. The completeness of the data allows for the assessment of appropriate care, such as the placement of sealants, and outcomes of care.
Most EHRs have built-in facilities to support CDSS, however, their implementation has been limited by challenges in developing standards, associated costs and provider skepticism about it’s value and feasibility.23 While current EHR systems are limited in their ability to assess the accuracy of data collected, future systems involving artificial intelligence (AI) could help to alleviate the need for relying solely on manual chart review and data entry. These AI systems could interpret digital radiographs and intraoral scans to identify erupted and restored teeth to help with assessing and/or confirming sealant-eligible teeth. It is expected that EHRs will evolve to integrate these rapidly evolving AI technologies and make advancements that deliver better CDSS to providers that are easier to implement.24 However, the use of DQMs has been slow among independent dental providers, and adoption of CDSS for quality improvement efforts will be hindered by reimbursement models still focused on procedures instead of oral health outcomes.25
The next steps as part of the quality improvement cycle will be to solicit and interpret provider and patient feedback, monitor the success of the same-day sealant intervention, identify specific initiatives to address, and adjust training and ongoing refinement of the CDSS itself as necessary. One consideration is assessing ways to keep the benefits of the passive CDSS that providers do not find as a nuisance, but also making it more visible and accessible to interact to improve rates of appropriate care. With continued improvements in the delivery of preventive services, further assessment of patient health outcomes, e.g., lower caries risk and fewer new caries, will be evaluated to show the net effect of the increased delivery of appropriate sealants.
CONCLUSION
An effective CDSS around sealant placement can be integrated into a dental quality improvement program to successfully implement evidence-based guidelines that facilitate and improve the delivery of timely and appropriate patient care.
Acknowledgments:
This study received funding from U.S Department of Health and Human Services, National Institutes of Health, National Institute of Dental and Craniofacial Research, Grant number R01DE024166: Implementing Dental Quality Measures in Practice.
Footnotes
All authors declare no conflicts of interest.
Contributor Information
Joanna Mullins, VP of Strategic Business Operations, Willamette Dental Group, Hillsboro, OR, USA.
Ryan Brandon, Consultant, Willamette Dental Group and Skourtes Institute, Hillsboro, OR, USA.
Nicholas Skourtes, Vice President, Willamette Dental Group, Hillsboro, OR, USA.
Elsbeth Kalenderian, Dean and Professor, Marquette University School of Dentistry, Milwaukee, WI, USA.
Muhammad Walji, Director and Professor, Texas Center for Oral Healthcare Quality and Safety, Chair, Department of Clinical and Health Informatics, University of Texas Health Science Center at Houston, Houston, TX, USA.
REFERENCES
- 1.Wright JT, Tampi MP, Graham L, et al. Sealants for preventing and arresting pit-and-fissure occlusal caries in primary and permanent molars: A systematic review of randomized controlled trials-a report of the American Dental Association and the American Academy of Pediatric Dentistry. J Am Dent Assoc. Aug 2016;147(8):631–645.e18. doi: 10.1016/j.adaj.2016.06.003 [DOI] [PubMed] [Google Scholar]
- 2.Yansane A, Listl S, Dawda D, et al. Increasing value, reducing waste: tailoring the application of dental sealants according to individual caries risk. J Public Health Dent. Sep 2020;80 Suppl 2(Suppl 2):S8–S16. doi: 10.1111/jphd.12396 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Services USDoHaH. Oral Conditions. Healthy People 2030. Accessed September 10, 2023, 2023. https://health.gov/healthypeople/objectives-and-data/browse-objectives/oral-conditions [Google Scholar]
- 4.Association AD. Accessed 26 Dec 2023, https://www.ada.org/resources/research/dental-quality-alliance/dqa-dental-quality-measures
- 5.Kumar SV, Yansane A, Neumann A, et al. Measuring sealant placement in children at the dental practice level. J Am Dent Assoc. Oct 2020;151(10):745–754. doi: 10.1016/j.adaj.2020.06.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wheeler DJ. Understanding variation : the key to managing chaos. 2nd ed. SPC Press; 2000:x, 158 p. : ill. [Google Scholar]
- 7.Sperl-Hillen JM, Rossom RC, Kharbanda EO, et al. Priorities Wizard: Multisite Web-Based Primary Care Clinical Decision Support Improved Chronic Care Outcomes with High Use Rates and High Clinician Satisfaction Rates. EGEMS (Wash DC). Apr 3 2019;7(1):9. doi: 10.5334/egems.284 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.McDonald C, Abhyankar S. Clinical decision support and rich clinical repositories: a symbiotic relationship: comment on “Electronic health records and clinical decision support systems”. Arch Intern Med. May 23 2011;171(10):903–5. doi: 10.1001/archinternmed.2010.518 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sutton RT, Pincock D, Baumgart DC, Sadowski DC, Fedorak RN, Kroeker KI. An overview of clinical decision support systems: benefits, risks, and strategies for success. NPJ Digit Med. 2020;3:17. doi: 10.1038/s41746-020-0221-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kumar SV, Bangar S, Neumann A, et al. Assessing the validity of existing dental sealant quality measures. J Am Dent Assoc. Sep 2018;149(9):756–764.e1. doi: 10.1016/j.adaj.2018.05.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.White JM, Brandon RG, Mullins JM, Simmons KL, Kottek AM, Mertz EA. Tracking oral health in a standardized, evidence-based, prevention-focused dental care system. J Public Health Dent. Sep 2020;80 Suppl 2(Suppl 2):S35–S43. doi: 10.1111/jphd.12413 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ancker JS, Edwards A, Nosal S, et al. Effects of workload, work complexity, and repeated alerts on alert fatigue in a clinical decision support system. BMC Med Inform Decis Mak. Apr 10 2017;17(1):36. doi: 10.1186/s12911-017-0430-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.O’Donnell JA, Modesto A, Oakley M, Polk DE, Valappil B, Spallek H. Sealants and dental caries: insight into dentists’ behaviors regarding implementation of clinical practice recommendations. J Am Dent Assoc. Apr 2013;144(4):e24–30. doi: 10.14219/jada.archive.2013.0139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Polk DE, Weyant RJ, Shah NH, Fellows JL, Pihlstrom DJ, Frantsve-Hawley J. Barriers to sealant guideline implementation within a multi-site managed care dental practice. BMC Oral Health. Feb 02 2018;18(1):17. doi: 10.1186/s12903-018-0480-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Blumer S, Ratson T, Peretz B, Dagon N. Parents’ Attitude towards the Use of Fluorides and Fissure Sealants and its Effect on their Children’s Oral Health. J Clin Pediatr Dent. 2018;42(1):6–10. doi: 10.17796/1053-4628-42.1.2 [DOI] [PubMed] [Google Scholar]
- 16.Jo ED, Lee SB, Kang CM, Kim KM, Kwon JS. Release of Bisphenol A from Pit and Fissure Sealants According to Different pH Conditions. Polymers (Basel). Dec 23 2021;14(1)doi: 10.3390/polym14010037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Schafer TE, Lapp CA, Hanes CM, Lewis JB. What parents should know about estrogen-like compounds in dental materials. Pediatr Dent. Jan-Feb 2000;22(1):75–6. [PubMed] [Google Scholar]
- 18.Carney K Why We Change: Kirk vs Spock. Californal Dental Association Journal; 2018. p. 5–6. [Google Scholar]
- 19.Lukac PJ, Bell D, Sreedharan P, Gornbein JA, Lerner C. The Application of Dental Fluoride Varnish in Children: A Low Cost, High-Value Implementation Aided by Passive Clinical Decision Support. Appl Clin Inform. Mar 2023;14(2):245–253. doi: 10.1055/a-2011-8167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bell GC, Crews KR, Wilkinson MR, et al. Development and use of active clinical decision support for preemptive pharmacogenomics. J Am Med Inform Assoc. Feb 2014;21(e1):e93–9. doi: 10.1136/amiajnl-2013-001993 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Spiegel MC, Simpson AN, Philip A, et al. Development and implementation of a clinical decision support-based initiative to drive intravenous fluid prescribing. International journal of medical informatics. Dec 2021;156:104619. doi: 10.1016/j.ijmedinf.2021.104619 [DOI] [PubMed] [Google Scholar]
- 22.Dexter PR, Perkins SM, Maharry KS, Jones K, McDonald CJ. Inpatient computer-based standing orders vs physician reminders to increase influenza and pneumococcal vaccination rates: a randomized trial. JAMA. Nov 17 2004;292(19):2366–71. doi: 10.1001/jama.292.19.2366 [DOI] [PubMed] [Google Scholar]
- 23.Benoit B, Frédéric B, Jean-Charles D. Current state of dental informatics in the field of health information systems: a scoping review. BMC Oral Health. Apr 19 2022;22(1):131. doi: 10.1186/s12903-022-02163-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Khanagar SB, Al-Ehaideb A, Maganur PC, et al. Developments, application, and performance of artificial intelligence in dentistry - A systematic review. J Dent Sci. Jan 2021;16(1):508–522. doi: 10.1016/j.jds.2020.06.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fellows JL, Atchison KA, Chaffin J, Chávez EM, Tinanoff N. Oral Health in America: Implications for dental practice. J Am Dent Assoc. Jul 2022;153(7):601–609. doi: 10.1016/j.adaj.2022.04.002 [DOI] [PMC free article] [PubMed] [Google Scholar]


