Urologists have devised a formula that predicts the risk of a recurrence of prostate cancer after radical prostatectomy. The algorithm facilitates an accurate assessment of a patient’s life expectancy and the development of individualised treatment plans.
A team from the Johns Hopkins University Hospitals in Baltimore, Maryland, studied 1997 men who had radical prostatectomy for localised prostate cancer between 1982 and 1997. None of the patients received adjuvant hormone or radiation treatment. The men were followed for an average of 5.3 years, with more than 10000 patient years of data being compiled (JAMA 1999;281:1591-7).
The researchers studied the time it took for the concentration of prostate specific antigen to rise after surgery and whether metastatic disease developed during the study period. Prostate specific antigen is produced by the prostate gland, and the concentration of the antigen usually rises in cases of prostate cancer. After prostatectomy, concentrations of the antigen should be undetectable. A rise in serum concentrations of the antigen is therefore a biochemical marker of a recurrence. Of the patients studied, 315 had a rise in concentrations of the antigen, and 304 of these were followed. Only 103 (34%) of these patients developed metastatic disease. On average, it took eight years from the time when concentrations of the antigen were raised for metastases to appear. A total of 87%of the patients studied were free of metastases at 10 years and 82%at 15 years.
Factors which predicted metastatic disease included the histological grade of the tumour as measured by Gleason score, the time to initial rise in concentrations of the antigen, and the time that it took concentrations of the antigen to double. Patients at high risk of metastatic disease were those who had had high grade tumours, an antigen concentration that rose above 0 within two years of surgery, and a doubling time of 10 months or less. Men with high grade tumours (Gleason scores of 8 or above) had a 60%chance of cancer progression at five years from the time that antigen concentrations rose. In contrast, men with low grade tumours (Gleason scores of less than 8) had a 73%chance of remaining free of metastatic disease at five years, despite a rise in antigen concentrations.
These data allowed the researchers to construct a formula which predicts metastatic risk. Previously, there had been no way to stratify patients with prostate cancer by risk, and any rise in antigen concentrations was considered ominous. The new formula will allow doctors to better inform patients as to their life expectancy and treatment options.
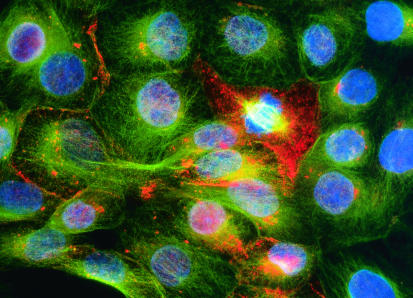
Figure.
NANCY KEDERSHA/SPL
Prostate cancer cells: risk of disease recurrence can now be predicted