Abstract
Mature cystic teratomas (MCTs) arise from totipotent cells. While the ovaries are the most common sites, extragonadal teratomas are very rare. This case report describes the clinical details of a 20-year-old woman who was found to have a large pelvi-abdominal mass on clinical and imaging studies and elevated levels of CA-125. Because of the uncertainties of the origin of the mass, a multidisciplinary team suggested exploratory laparotomy with a mesenteric cyst as a differential diagnosis. Laparotomy showed both ovaries to be normal and revealed a large omental MCT, which was excised. Histopathology confirmed the diagnosis.
Keywords: Ovarian cyst, Teratoma, Omental teratoma, Mesenteric cyst
Highlights
-
•
Extragonadal teratomas are very rare and their diagnosis is challenging.
-
•
Mesenteric cysts; rare and may have clinical and imaging similarities with extragonadal teratoma.
-
•
Multidisciplinary management is advised in cases where the diagnosis in not clear.
1. Introduction
Mature cystic teratomas (MCTs) are benign tumors that develop from totipotent germ cells; they may contain various tissue components such as hair, bone, teeth, fat, and neural tissue [1]. They account for 10–20% of all ovarian tumors and are the most common ovarian germ cell tumors among women of reproductive age, mainly in those under the age of 20 years. While mostly benign, malignant transformation may occur in 0.1–0.2% of cases [2]. The typical site of MCTs is in the midline of the body, but they may be located in the mediastinum, nasal sinuses, and pineal gland. Very rarely, they may occur at sites away from the midline, such as the abdominal wall, the retroperitoneal space, and cecum [3]. The vast majority of MCTs arise from the ovaries, and extragonadal MCTs are very rare, representing only 1–5% of all germ cell tumors [4]. Furthermore, mesenteric cysts are very rare benign intra-abdominal tumors, with an incidence of 1/250,000 among patients admitted to hospital, that have nonspecific clinical presentations and vary in size from a few millimetres to many centimetres [5].
2. Case Presentation
A 20-year-old nulligravid, healthy woman presented to the obstetrics and gynaecology out-patient clinic with intermittent right lower abdominal pain that had lasted four months. Her menarche was at the age of 13 years, and her menstrual cycles were regular. She was not using contraception because she was trying to conceive. The pain had progressed over the month prior to presentation and was associated with anorexia, nausea, constipation, urinary urgency, and dyspareunia.
Physical examination showed a body mass index of 22 kg/m2 and an 18-week size, non-tender, mobile pelvi-abdominal mass. Pelvic examination revealed a normal-sized, anteverted, mobile uterus and a large pelvi-abdominal mass which was found to be separated from the uterus.
A trans-vaginal pelvic ultrasound scan confirmed the presence of a right lower abdominal 15 cm × 15 cm, well-defined cystic mass with solid components and calcification. The ovaries were not clearly visualized.
Based on the finding of a complex mass, the origin of which was not determined, abdominal and pelvic magnetic resonance imaging (MRI) with intravenous contrast was requested, and the results showed normal liver, spleen, and a well-defined septated right lower abdominal mass measuring about 8 cm × 11 cm × 13 cm. Post-contrast images showed regular peripheral and no internal enhancement. The uterus appeared unremarkable, with normal endometrium. Both ovaries were visualized and reported as normal, and there was no evidence of ascites or enlarged pelvic or paraaortic lymph nodes (Fig. 1).
Fig. 1.

Post-contrast magnetic resonance image of the mass.
Hematological and biochemical investigations were requested, including full blood count, kidney and liver function test, and urine analysis and culture, and they were all within normal range. The tumor markers that were requested included alpha fetoprotein (AFP), B-human chorionic gonadotrophins (B-HCG), lactate dehydrogenase (LDH), and carbohydrate antigen-125 (CA-125). The results were all within normal range except for the CA-125 level, which was 183 u/ml (normal range < 35u/ml).
In light of the results of the investigations, in particular the MRI and the elevated CA-125 level in the presence of normal ovaries on a pelvic MRI scan, surgical consultation was sought to help identify a possible non-gynecological origin of the mass, and the provisional surgical diagnosis was a mesenteric cyst.
Following discussion with the woman, an exploratory laparotomy was planned. Intraoperative findings showed a normal uterus, both tubes, and ovaries (Fig. 2). Additionally, a 16 cm × 11 cm × 6 cm cystic mass was identified which was torted against feeding vessels arising from the omentum (Fig. 3). The outer surface of the mass was smooth except for a 6 cm × 6 cm irregular area that contained skin and hair (Fig. 4). Exploration of the abdomen by the surgeon showed normal small and large intestine. Additionally, there were no palpable pelvic or paraaortic lymph nodes. The mass was excised and a peritoneal wash for cytology was collected. The woman had an uneventful postoperative course.
Fig. 2.
Laparotomy finding: normal uterus, ovaries, and both tubes.
Fig. 3.
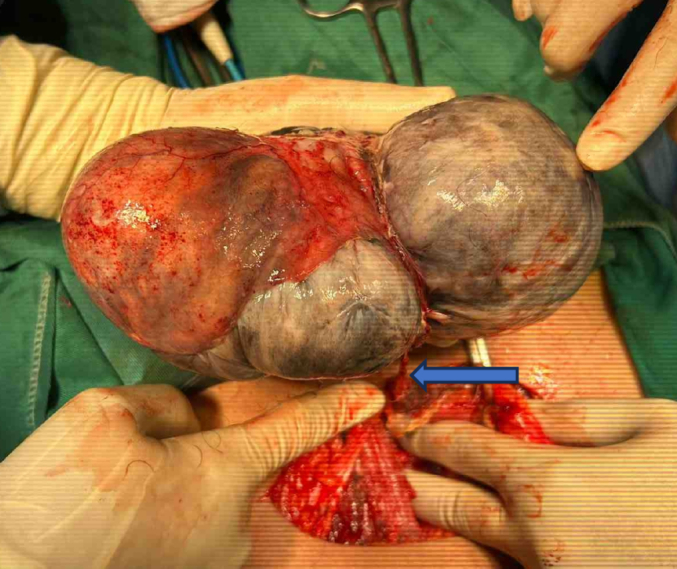
Laparotomy finding: large cystic mass with feeding vessels arising from the omentum (the arrow).
Fig. 4.

The surface of the mass showing skin and hair.
The results of the histopathological studies revealed a mature cystic teratoma with skin, skin appendages, muscle fibers, fibro-fatty tissue, hair, and ovarian tissue components. Staining with WT1 and inhibin immunostains confirmed the presence of ovarian tissue. Peritoneal fluid cytology was negative for malignant cells.
The woman was followed up in the gynaecology out-patient clinic at two and six weeks, when she was seen to have had an uneventful recovery.
3. Discussion
Mature cystic teratomas arise from totipotent cells, and the ovaries are the most common sites. Extragonadal sites are very rare [6]. While the pathophysiological mechanisms behind their development at extragonadal sites are poorly understood, three have been suggested. The first is that MCTs originate from germ cells that migrate to other sites during embryonic life [7], the second is autoamputation of ovarian teratoma and implantation into extragonadal sites, and the third is teratomas arising in a supernumerary ovary [8]. In our case, the development of an omental MCT could be explained by autoamputation because ovarian tissue components were identified in the mass. This is supported by another report where the microscopic ovarian tissue was present in 22 cases of omental MCTs [9]. We acknowledge that it is not clear how to distinguish autoamputation from the other mechanisms.
The challenge in this case is the finding of a pelvi-abdominal mass in the presence of normal-looking pelvic organs on imaging studies and an elevated CA-125 level. The surgical opinion suggested a mesenteric mass, which is a very rare surgical condition and can occur anywhere in the mesentery of the gastrointestinal tract. Additionally, mesenteric masses may range from being single or multiple, from a few millimetres to many centimetres, from unilocular to multilocular, and may contain a solid component, hence the similarities with MCTs on imaging studies [10]. Therefore, a multidisciplinary approach will improve patient management.
4. Conclusion
Extragonadal MCTs are under-represented in the published literature. Preoperative diagnosis of an extragonadal teratoma may be challenging and a multidisciplinary approach is likely to improve treatment outcome.
Acknowledgments
Contributors
Fida Asali contributed to patient care, drafting the manuscript and undertaking the literature review.
Lubna Batayneh contributed to patient care, drafting the manuscript and undertaking the literature review.
Aseel Albtoush contributed to patient care, drafting the manuscript and undertaking the literature review.
Salim Abu Mahfouz contributed to drafting the manuscript, undertaking the literature review and revising the article critically for important intellectual content.
Ismaiel Abu Mahfouz supervised the work and manuscript preparation.
All authors approved the final submitted draft.
Funding
No specific grant from funding agencies in the public, commercial, or not-for-profit sectors supported the publication of this case report.
Patient consent
Written consent was obtained from the patient to use her details and the images included.
Provenance and peer review
This article was not commissioned and was peer reviewed.
Acknowledgments
Conflict of interest statement
The authors declare that they have no conflict of interest regarding the publication of this case report.
References
- 1.Sundar S., Umman P., Chisthi M. Mature ovarian teratoma presenting as small bowel obstruction. Indian J. Surg. 2013;75:411–413. doi: 10.1007/S12262-012-0502-Z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Khanna S., Srivastava V., Saroj S., Mishra S.P., Gupta S.K. An unusual presentation of ovarian teratoma: a case report. Case Rep. Emerg. Med. 2012;2012:1–2. doi: 10.1155/2012/845198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mishra T.S., Jena S.K., Kumari S., Purkait S., Ayyanar P., Nayak P. Cecal dermoid masquerading dermoid cyst of ovary: a case report and review of the literature. J. Med. Case Rep. 2021;15 doi: 10.1186/S13256-020-02570-Y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McKenney J.K., Heerema-Mckenney A., Rouse R.V. Extragonadal germ cell tumors: a review with emphasis on pathologic features, clinical prognostic variables, and differential diagnostic considerations. Adv. Anat. Pathol. 2007;14:69–92. doi: 10.1097/PAP.0B013E31803240E6. [DOI] [PubMed] [Google Scholar]
- 5.Bhattacharjee A., Kulkarni V., Lamture Y., Nagtode T., Ramteke H. A rare case of a mesenteric cyst. Cureus. 2022;14 doi: 10.7759/CUREUS.32015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Thway K., Polson A., Pope R., Thomas J.M., Fisher C. Extramammary Paget disease in a retrorectal dermoid cyst: report of a unique case. Am. J. Surg. Pathol. 2008;32:635–639. doi: 10.1097/PAS.0B013E318158427B. [DOI] [PubMed] [Google Scholar]
- 7.Hegde P. Extragonadal omental teratoma: a case report. J. Obstet. Gynaecol. Res. 2014;40:618–621. doi: 10.1111/JOG.12198. [DOI] [PubMed] [Google Scholar]
- 8.Rampinelli F., Donarini P., Visenzi C., Ficarelli S., Gambino A., Ciravolo G. The rare extragonadal omental teratoma: a case report. J. Minim. Invasive Gynecol. 2017;24:1046–1048. doi: 10.1016/J.JMIG.2017.05.022. [DOI] [PubMed] [Google Scholar]
- 9.Lee K.H., Song M.J., Jung I.C., Lee Y.S., Park E.K. Autoamputation of an ovarian mature cystic teratoma: a case report and a review of the literature. World J. Surg. Oncol. 2016;14 doi: 10.1186/S12957-016-0981-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pithawa A.K., Bansal A.S., Kochar S.P.S. Mesenteric cyst: a rare intra-abdominal tumour. Med. J. Armed Forces India. 2014;70:79–82. doi: 10.1016/J.MJAFI.2012.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]



