RESUME
RESUME
Introduction: L’anesthésie rachidienne continue pour la chirurgie de la fracture de la hanche chez le sujet âgé préserve plus l’hémody-namique per opératoire comparativement à l’anesthésie générale et à la rachianesthésie en injection unique. Mais, le risque de survenue d’une hypotension n’est jamais nul. Objectif : Montrer que la bupivacaïne hypobare dans la rachianesthésie continue préserve mieux l’hémodynamique comparativement à la bupivacaïne isobare. Méthodes : Il s’agissait d’une étude prospective randomisée contrôlée en simple aveugle. Cent dix patients âgés de plus de 65 ans ont été randomisés pour recevoir de la bupivacaïne hypobare ou de la bupivacaïne isobare. Des doses répétées de 2,5 mg de bupivacaïne ont été injectées pour un bloc sensitif à T12. L’hypotension et l’hypotension sévère ont été définies comme une diminution de plus de 20% et de 30% de la pression artérielle systolique de base. L’analyse statistique a utilisé les tests Chi2 et Student pour comparer le nombre et le pourcentage ou la moyenne et la médiane. P<0,05 était significatif. Résultats : Moins de patients ont présenté une hypotension et une hypotension sévère dans le groupe hypobare que dans le groupe isobare (respectivement 53 % contre 73 % ; p<0,05 et 22% contre 53 % ; p< 0,01). La consommation d’éphédrine était significativement plus faible dans le groupe bupivacaine hypobare (1.9 vs 5.6 mg; p<0,01). Conclusion: La bupivacaïne hypobare est associée à une meilleure stabilité hémodynamique dans la rachianesthésie titrée pour la chirurgie de la fracture de la hanche du sujet âgé
ABSTRACT
INTRODUCTION: Continuous spinal anesthesia for surgical repair of hip fracture in elderly patients has been shown to preserve hemodynamics better than general and single shoot spinal anesthesia. However, hypotension still occurs, even with continuous spinal anesthesia. AIM: This study aimed to demonstrate that hypobaric bupivacaine is more effective in preserving hemodynamics than isobaric bupivacaine when patients are operated in lateral position. METHODS: It was a prospective randomized controlled single-blind study conducted in an orthopaedic institute during two years (2017–2018). One hundred and ten patients aged more than 65 years, scheduled for hip fracture repair, were randomized to receive either hypobaric or isobaric bupivacaine. Repeated doses of 2.5 mg bupivacaine were injected until sensory blockade reached T12. Hypotension and severe hypotension were defined as a decrease of more than 20% and 30% from the baseline systolic arterial blood pressure and were treated with ephedrine. Statistical analysis used Chi2 and Student tests to compare either number and percentage or mean and median. P<0.05 was significant. RESULTS: Less patients experienced hypotension and severe hypotension in hypobaric group than in isobaric group (respectively 53% vs. 73%; p<0.05 and 22% vs. 53%; p< 0.01). Ephedrine consumption was significantly lower in hypobaric group (1.9 mg vs. 5.6 mg; p<0.01). CONCLUSION: Hypobaric bupivacaine may be used rather than isobaric bupivacaine for further preserving hemodynamics in continuous spinal anesthesia for hip fracture surgery in elderly.
INTRODUCTION
Surgery for hip fracture in elderly patients is associated with high rates of morbidity (1, 2).
Anesthesia type is hypothesized to be related to mortality among these patients.
However, recent studies found no difference in mortality with all techniques (3,5).
Nevertheless, anesthesia is still hypothesized to have an effect on mortality
In a re-analysed prospective 11,085 records of hip fracture in elderly, incidence of spinal-induced hypotension can be as high as 73% and the risk of death increased significantly as blood pressure fell (6).
Continuous spinal anesthesia (CSA) showed a better hemodynamic stability when compared to general anesthesia (7) and to single shoot spinal anesthesia (8,9).
But, hypotension is still observed (8,10).
Spinal block on lateral position with either hypo or hyperbaric local anaesthetic solutions achieved better hemodynamic stability (11 ).
Hemodynamic profile during CSA in lateral position has not been studied.
We aimed in this study to demonstrate that hypobaric bupivacaine unilateral CSA is more effective in preserving hemodynamics compared to isobaric bupivacaine
METHODES
Type of study:
It was a prospective, randomized, controlled, single-blinded study performed between 2017 and 2019.
All patients or relatives given informed written consent.
The study was approved by the local ethics committee (number: CE-IMKO 2015/104).
Study was registered in Pan African Clinical Trials Registry: PACTR201606001657480.
Patients:
Patients aged more than 65 years, scheduled for surgical repair of hip fracture were eligible to the study.
Patients with any contraindication to spinal anaesthesia (SA) or peripheral nerve blocks including hemostasis impairment, local infection, and allergic reaction to local anesthetics were not included.
Patients with cognitive disorders and no verbal contact were also excluded.
Study procedures
: No sedative premedication was received before arriving in the operating room.
Patients had standard monitoring with electrocardiogram, pulse oximetry and non invasive arterial blood pressure.
An intravenous infusion of 10 ml.kg-1 of saline was initiated and patients received nasal oxygen (2 l.min-1).
Ultrasound guided (Sonosite; Fujifilm, Japan) femoral nerve block was performed using a 21-G needle (Vygon; Ecouen, France) with twenty ml of 1.5% lidocaine
After 10 min, patients were placed in the lateral position with the fractured side up.
Spinal puncture was performed with a 19-gauge Tuohy needle (Arrow, USA) at the L4-L5 or L3-L4 interspace using a midline approach. Three cm of a 22-gauge catheter was introduced through the needle, directed to the fractured side.
Patients were then randomized (computer table with sealed envelope)to two groups:
Group HB received 0.25% hypobaric bupivacaine, prepared diluting each 1 ml of 0.5% isobaric bupivacaine with 1 ml of sterile water
Group IB received 0.5% isobaric bupivacaine
In view of the 0.2 ml capacity of the catheter and the little volume of the anaesthetic solution to be injected, a 1-ml syringe was used to perform injections.
The catheter was filled with 0.2 ml of the anaesthetic solution
An initial dose of 2.5 mg bupivacaine with 2.5 µg sufentanil was injected through the catheter with an injection rate of 1 ml per 30 sec.
After 10 min, sensory blockade was estimated, and 2.5 mg of bupivacaine was added if sensory blockade was < T12 in the fractured side
Additional 1 mg bupivacaine was injected until sensory blockade reached T12 in the operated side.
Intraoperatively additional 1 mg bupivacaine was added according to patient analgesic demand.
In case of failure of lumbar puncture or insufficient block after a total dose of 7.5 mg bupivacaine, general anesthesia (GA) was performed and the patient was excluded from the statistical analysis.
Spinal catheters were removed after the surgery.
Anaesthesiologists who did CSA and injected the first bolus of bupivacaine were not implicated in patient assessment
Collected data:
Arterial blood pressure and heart rate were recorded before the CSA (baseline), and every 5 min all over the procedure.
The baseline was determined from the average of 3 consecutive readings taken before the administration of fluid.
Hypotension was defined as a decrease of more than 20% from the baseline systolic blood pressure (SBP)
Severe hypotension was defined as a decrease in SBP more than 30% of baseline value.
Hypotension was treated with IV boluses ofephedrine 6 mg repeated every 5 min
Bradycardia was defined by heart rate < 50 bpm and was treated by ephedrine 6 mg
The anaesthesiologist in charge of the patient was free to manage fluid therapy.
Sensory blockade was assessed by a pinprick test and motor block was assessed using Bromage scale.
Total consumption of bupivacaine, total vasopressor administered, and the amounts of fluid infused were recorded.
Day one after surgery, blood urea, creatinine, hemoglobin and troponin were meseared
An electrocardiogram was performed
Urinary retention, post-operative nausea and vomiting, headache and neurologic complications were assessed.
Our primary outcome was the incidence of hypotension (percentage of patients who experienced at least one episode of hypotension) and severe hypotension among the 2 groups
Secondary outcomes were : ΔSBP=(SBP at T0 – Minimal SBP)/ SBP T0 (T0: measure before CSA), total bupivacaine consumption, vasopressor use, fluid infusion and cardiovascular complications (electrocardiogram modification or elevated troponin).
Statistical analysis:
To determine the number of patients by group, we used the study of Minville et al. (8) who compared hypotension after spinal anesthesia performed with 7.5 mg of isobaric bupivacaine versus CSA performed with initial dose of 2.5 mg of the same solution.
hey found, in the CSA group, that 31% of the patients experienced at least one episode of hypotension.
We hypothesized that the use of hypobaric bupivacaine will reduce this occurrence to 10%
The sample size for a superiority trial yielded a sample size of 55 patients for each group, with a study power of 80% and a significance level of 0.05.
Statistical analyses were performed using the SPSS® software(version 17, SPSS Inc, IBM, USA).
Quantitative data were expressed in mean (SD) or median [interquartile] depending on their distribution (Kolmogorov-Smirnov test for normality).
Categorical data were expressed as n (%)
Qualitative data were analyzed by χ2 test and quantitative data by Student t-test if the distribution was normal or Mann-Whitney U-test if the distribution was not normal
P< 0.05 was considered statistically significant.
RESULTS
Four hundred and twelve patients were eligible to inclusion during the study period (Figure 1: Flowchart).
One hundred and fourteen patients were randomized.
Three patients were excluded because of failure to perform CSA.
Finally, 55 patients were analyzed in group HB and 56 patients in group IB
The two groups were similar in respect to demographic and surgical data (Table 1).
The mean time to operate on patients was 4.9 ± 1.5 days in group HB and 4.4 ± 1.3 days in group IB.
Significantly less patients experienced hypotension in group HB (53% vs 73%, p=0.028).
Significantly less patients experienced severe hypotension in group HB (22% vs 53%, p=0.007).
Hypobaric group patients needed significantly less ephedrine (1.9 mg vs 5.6 mg, p=0.022).
There was no significant difference in fluid therapy and total bupivacaine.
In the first post-operative 24 hours, 3 patients in each group presented a cardio-vascular complication (electrocardiogram modification, elevated troponin).
All blood tests were unchanged in both groups. Blood transfusion needs were not different
Urine retention and post operative nausea and vomiting were not different.
No patient complained about either headache or neurologic deficit.
Figure 1. Flow char .
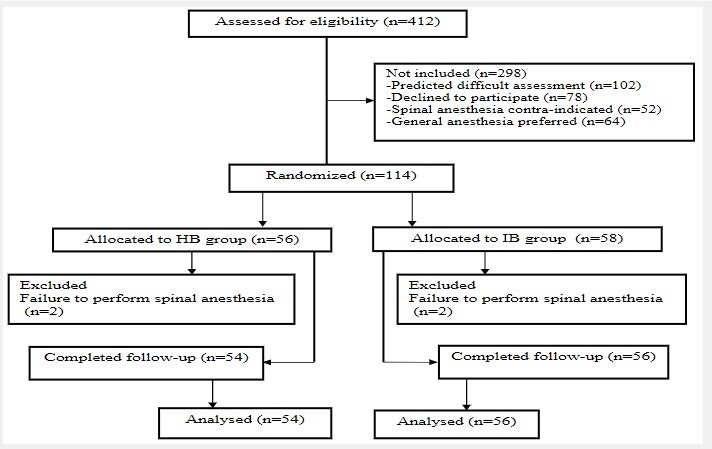
Table 1 : Demographic and surgical data .
|
HB group (n=54) |
IB group (n=56) |
P |
|
|---|---|---|---|
|
Sex (M/F) |
23/31 |
21/35 |
0.21 |
|
Age (years) |
76 ± 7 |
78 ± 6 |
0.30 |
|
Height (cm) |
164 ± 6 |
163 ± 8 |
0.82 |
|
Weight (kg) |
71 ± 10 |
67 ± 12 |
0.54 |
|
BMI (kg/m2) |
26 ± 3 |
25 ± 3 |
0.65 |
|
ASA class (I/II/III) |
13/31/10 |
13/34/9 |
|
|
Co-morbidities |
|
||
|
Type of surgery |
|
||
|
Time to surgery (days) |
4.9 ± 1.6 |
4.4 ± 2.0 |
0.55 |
|
Surgical duration (min) |
68 ± 19 |
69 ± 25 |
0.86 |
Table 2 : Main intraoperative data .
|
HB group (n=54) |
IB group (n=56) |
P |
|
|
Unilateral blockade |
20 (37%) |
2 (3%) |
0.006 |
|
Hypotension |
29 (53%) |
41 (73%) |
0.0028 |
|
Severe hypotension |
12 (22%) |
30 (53%) |
0.007 |
|
Ephedrine (mg) |
1.9 ± 4.0 |
5.6 ± 8.0 |
0.022 |
|
Minimal SBP (mmHg) |
109 ± 18 |
103 ± 22 |
0.610 |
|
ΔSBP |
22 ± 11 |
27 ± 13 |
0.743 |
|
Total bupivacaine (mg) |
4.6 ± 1.8 |
4.8 ± 1.8 |
0.650 |
|
Fluids (ml) |
1247 ± 464 |
1282 ± 327 |
0.801 |
|
Cardiac complications |
3 (5%) |
3 (5%) |
0.900 |
DISCUSSION
In This study, we demonstrated that hypobaric bupivacaine caused fewer episodes of severe hypotension and less ephedrine consumption when compared to isobaric bupivacaine for continuous spinal anesthesia in lateral position.
Hemodynamic stability could be an important issue in elderly patients with hip fracture, as recent data suggests that the occurrence of hypotension may be correlated with mortality and cardiovascular complications in this population (6 ).
Hypotension is more common, and also more hazardous, in elderly patients.
In old patients, the rate of peripheral vascular resistance after spinal anesthesia may be reduced up to 25%, and the amount of cardiac output may drop to 10% (12).
In a pilot study performed in elderly population who suffer from heart diseases, haemodynamic changes using invasive monitoring demonstrated moderate reduction in systemic vascular resistance index and mean arterial pressure with a minimal cardiac index changing in SA group compared to GA group ( 13 ).
CSA allows titration of small amounts of local anesthetic to achieve the appropriate level and provide adequate duration of anesthesia with only minimal hemodynamic changes (14,15).
It showed a better hemodynamic stability when compared either to GA ( 7 ) or to single shoot SA ( 8 , 9 , 16 )
It was safely used in selected patients with co morbidities (17 ,18).However, hypotension is still observed in CSA ( 8 , 10 ) with an incidence up to 31%.
In our study, hypotension in isobaric group occurred in 73% and severe hypotension in 53%.
Unilateral spinal block with either hypo or hyperbaric local anaesthetic solutions in patients on lateral position was associated with a better hemodynamic stability ( 11 )
Unilateral spinal anesthesia allows use of lower dose local anesthetic (19,22) minimizing the incidence of hypotension/ severe hypotension but with a high proportion of patients who needed rescue IV anesthetics (19)
Unilateral spinal anesthesia with hypobaric solution allows slower installation of the sympathetic block as compared with a hyperbaric solution ( 23 )
Unilateral distribution of local anesthetic contributes to the reduction of sympathetic block ( 11 , 15 , 24 )
Limitation of local anesthetic doses and one-siding sympathetic block are the two mechanisms that largely explain the hemodynamic stability.
However, in more recent study, Lilot et al (25) demonstrated that the lowest effective dose of hypobaric ropivacaine providing 95% success in SA for elderly was 9 mg.
such dose was associated with 47% to 83% incidence of severe hypotension
Similarly, high incidence of hypotension was reported in our hypobaric group in 53% of patients but severe hypotension happened in only 22% of patient.
Lower rate of severe hypotension in our hypobaric group was basically due to low local anaesthetic dose we used; 4.8 mg.
Exclusive unilateral extension of blockade reported in 37% of patients of HB group could also be another explanation.
But such rate was consistent with other data ( 25 , 26 )
Nevertheless, patients in our study experienced a higher rate of hypotension than in other studies concerning CSA ( 8 , 10 , 27 )
Several hypotheses could be suggested
First of all, the prolonged time to operate on our patients.
The mean time of 4 days before surgery could participate to increase intra operative hypovolemia in such sick elderly patients.
Unfortunately, logistic problems in operating theatre were the main reason.
This higher rate of hypotension may also account for our management of fluid resuscitation, since we did not use a systematic fluid loading after bupivacaine administering.
Dose of local anesthetic we used did not participate to such different results as it was either equivalent to dose used in some studies ( 8 , 15 ) or lower than others ( 10 , 27 ).
The incidence of hypotension remained high even in hypobaric group
Large volume we used for hypobaric group 1.8 ± 0.7 ml, could participate to a high sympathetic blockade.
In hypobaric group, more bolus were need as loading dose to get sensory blockade > T10 and an adequate motor block for surgery
That is why, we did not report any IV anaesthetic rescue in our study as reported for unilateral spinal anesthesia ( 26 ).
Even though, unilateral blockade was significantly more frequent in hypobaric group, it had participate to reduce incidence of hypotension compared to isobaric group but not enough to minimise such complication compared to unilateral spinal anesthesia.
Finally, the incidence of intra operative arterial hypotension varies depending on the definition used.
That well, the incidence of intraoperative arterial hypotension varies from 5% to 99% ( 25 )
We had chosen a 20% and 30% decrease of the initial systolic blood pressure.
This was the definition used in the study we referred to in the power analysis and sample size calculation ( 17 , 8 )
We didn’t report any technical failure in this study
The success rate of CSA is also high in literature ( 28 ).
But, a failure rate of 25% was reported recently ( 10 )
No cases of postdural puncture headache were recorded in our study.
We didn’t report any neurologic complication.
In a serie of 1,212 patients, no case of Cauda Equina syndrome or other major neurologic complications were reported ( 29 )
One important limitation of our study was the absence of blinding of care provider and data collector, due to different volumes of the anesthetic solutions.
One solution could have been to use 0.25% isobaric bupivacaine in the group IB
We did not opt for this solution because we aimed to compare our routine standard of care (CSA with 0.5% isobaric bupivacaine) with this proposed unilateral CSA with 0.25% hypobaric bupivacaine.
To conclude, this study showed that continuous spinal anesthesia with hypobaric bupivacaine may be used rather than isobaric bupivacaine for further preserving hemodynamics essentially for elderly patients with cardiovascular disorders.
Continuous spinal anaesthesia is a suitable technique for traumatic hip fracture surgical repair in elderly patients.
Other study may be necessary to confirm this conclusion in order to generalize its practice essentially in hip fractures for ASA physical-statut III elderly patients
References
- Kilci O, Un C, Sacan O, Gamli M, Baskan S, Baydar M. Postoperative Mortality after Hip Fracture Surgery: A 3 Years Follow Up. PLoS ONE. 2016;11:e0162097. doi: 10.1371/journal.pone.0162097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flikweert ER, Wendt KW, Diercks RL, Izaks GJ, Landsheer D, Stevens M. Complications after hip fracture surgery: are they preventable? Eur J Trauma Emerg Surg. 2018;44:573–580. doi: 10.1007/s00068-017-0826-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patorno E, Neuman MD, Schneeweiss S, Mogun H, Bateman TB. Comparative safety of anesthetic type for hip fracture surgery in adults: retrospective cohort study. BMJ. 2014;348:g4022. doi: 10.1136/bmj.g4022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neuman MD, Rosenbaum RP, Ludwig MJ, Zubizarreta RJ, Silber HJ. Anesthesia technique, mortality, and length of stay after hip fracture surgery. JAMA. 2014;311:2508–2517. doi: 10.1001/jama.2014.6499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guay J, Parker MJ, Gajendragadkar PR, Kopp S. Anaesthesia for hip fracture surgery in adults (Review) Cochrane Database Syst Rev. 2016 Feb 22;2(2):CD000521. doi: 10.1002/14651858.CD000521.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White SM, Moppett IK, Griffiths R, Johansen A, Wakeman R, Boulton C. Secondary analysis of outcomes after 11,085 hip fracture operations from the prospective UK anaesthesia sprint audit of practice (ASAP-2) Anaesthesia. 2016;71:506–514. doi: 10.1111/anae.13415. [DOI] [PubMed] [Google Scholar]
- Biboulet P, Jourdan A, Van Haevre V, Morau D, Bernard N, Bringuier S. Hemodynamic profile of target-controlled spinal anesthesia compared with 2 target-controlled general anesthesia techniques in elderly patients with cardiac comorbidities. Reg Anesth Pain Med. 2012;37:433–440. doi: 10.1097/AAP.0b013e318252e901. [DOI] [PubMed] [Google Scholar]
- Minville V, Fourcade O, Grousset D, Chassery C, Nguyen L, Asehnoune K. Spinal anesthesia using single injection small-dose bupivacaine versus continuous catheter injection techniques for surgical repair of hip fracture in elderly patients. Anest Analg. 2006;102:1559–1563. doi: 10.1213/01.ane.0000218421.18723.cf. [DOI] [PubMed] [Google Scholar]
- Baydilek Y, Yurtlu BS, Hanci V, Ayoğlu H, Okyay DR, Kayhan EG. The comparison of levobupivacaine in continuous or single dose spinal anesthesia for transurethral resection of prostate surgery. Braz J Anesthesiol. 2014;64:89–97. doi: 10.1016/j.bjane.2013.03.007. [DOI] [PubMed] [Google Scholar]
- Leyla TK, Sivrikaya GU, Eksioglu B, Hanci A, Dobrucali H. Comparison of unilateral spinal and continuous spinal anesthesia for hip surgery in elderly patients. Saudi J Anaesth. 2013;7:404–409. doi: 10.4103/1658-354X.121054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Imbelloni LE. The State of the Art of Unilateral Spinal Block. Rev Bras Anestesiol. 2007;57:589–591. doi: 10.1590/s0034-70942007000600001. [DOI] [PubMed] [Google Scholar]
- Rooke GA, Freund RP, Jacobson FA. Hemodynamic response and change in organ blood volume during spinal anesthesia in elderly men with cardiac disease. Anesth Analg. 1997;85:99–105. doi: 10.1097/00000539-199707000-00018. [DOI] [PubMed] [Google Scholar]
- Messina A, Frassanito L, Colombo D, Vergari A, Draisci G, Della Corte F, et al. Hemodynamic changes associated with spinal and general anesthesia for hip fracture surgery in severe ASA III elderly population: a pilot trial. Minerva Anestesiol. 2013;79:1021–2914. [PubMed] [Google Scholar]
- Sandby-Thomas M, Sullivan G, Hall JE. A national survey into the peri-operative anaesthetic management of patients presenting for surgical correction of a fractured neck of femur. Anaesthesia. 2008;63:250–258. doi: 10.1111/j.1365-2044.2007.05328.x. [DOI] [PubMed] [Google Scholar]
- Klimscha W, Weinstabl C, Ilias W, Mayer N, Kashanipour A, Schneider B, et al. Continuous spinal anesthesia with a microcatheter and low-dose bupivacaine decreases the hemodynamic effects of centroneuraxis blocks in elderly patients. Anesth Analg. 1993;77:275–280. doi: 10.1213/00000539-199377020-00011. [DOI] [PubMed] [Google Scholar]
- Maurer K, Bonvini JM, Ekatodramis G, Serena S, Borgeat A. Continuous spinal anesthesia/analgesia vs. single-shot spinal anesthesia with patient-controlled analgesia for elective hip arthroplasty. Acta Anaesthesiol Scand. 2003;47:878–883. doi: 10.1034/j.1399-6576.2003.00173.x. [DOI] [PubMed] [Google Scholar]
- Fuzier R, Murat O, Gilbert ML, Magùes JP, Fourcade O. Continuous spinal anesthesia for femoral fracture in two patients with severe aortic stenosis. Ann Fr Anesth Reanim. 2006;25:528–531. doi: 10.1016/j.annfar.2006.01.007. [DOI] [PubMed] [Google Scholar]
- Lópeza MM, Guascha E, Schiraldia R, Maggia G, Alonsoa E, Gilsanza F. Continuous spinal anaesthesia with minimally invasive haemodynamic monitoring for surgical hip repair in two patients with severe aortic stenosis. Braz J Anesthesiol. 2016;66:82–519. doi: 10.1016/j.bjane.2013.03.010. [DOI] [PubMed] [Google Scholar]
- Errando CL, Soriano-Bru JL, Peiró CM, Úbeda J. Single shot spinal anaesthesia with hypobaric bupivacaine for hip fracture repair surgery in the elderly. Randomized, double blinded comparison of 3.75 mg vs. 7.5 mg C.L. Rev Esp Anestesiol Reanim. 2014;61:541–548. doi: 10.1016/j.redar.2014.07.001. [DOI] [PubMed] [Google Scholar]
- Kahloul M, Nakhli MS, Chouchene A, Chebbi N, Mhamdi S, Naija W. Comparison of two doses of hypobaric bupivacaine in unilateral spinal anesthesia for hip fracture surgery: 5 mg versus 7.5 mg. Pan Afr Med J. 2017;28:108. doi: 10.11604/pamj.2017.28.108.11421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meuret P, Bouvet L, Villet B, Hafez M, Allaouchiche B, Boselli E. Hypobaric Unilateral Spinal Anaesthesia versus General Anaesthesia in Elderly Patients Undergoing Hip Fracture Surgical Repair: A Prospective Randomised Open Trial. Turk J Anaesthesiol Reanim. 2018;46:121–130. doi: 10.5152/TJAR.2018.90699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Messina A, Frassanito L, Colombo D, Vergari A, Draisci G, Della Corte F, et al. Hemodynamic changes associated with spinal and general anesthesia for hip fracture surgery in severe elderly population: a pilot study. Minerva Anestesiol. 2013;79:1021–1029. [PubMed] [Google Scholar]
- Fettes PD, Hocking G, Peterson MK, Luck JF, Wildsmith JA. Comparison of plain and hyperbaric solutions of ropivacaine for spinal anaesthesia. Br J Anaesth. 2005;94:107–111. doi: 10.1093/bja/aei008. [DOI] [PubMed] [Google Scholar]
- Kaya M, Oğuz S, Aslan K, Kadioğullari N. A low-dose bupivacaine: a comparison of hyperbaric and hypobaric solutions for unilateral spinal anesthesia. Reg Anesth Pain Med. 2004;29:17–22. doi: 10.1016/j.rapm.2003.09.006. [DOI] [PubMed] [Google Scholar]
- Lilot M, Meuret P, Bouvet L, Caruso L, Dabouz R, Deléat-Besson R, et al. Hypobaric Spinal Anesthesia with Ropivacaine Plus Sufentanil for Traumatic Femoral Neck Surgery in the Elderly: A Dose-Response Study. Anesth Analg. 2013;117:259–264. doi: 10.1213/ANE.0b013e31828f29f8. [DOI] [PubMed] [Google Scholar]
- Meyer J, Enk D, Penner M. Unilateral spinal anesthesia using low-flow injection through a 29-gauge Quincke needle. Anesth Analg. 1996;82:1188–1191. doi: 10.1097/00000539-199606000-00015. [DOI] [PubMed] [Google Scholar]
- Imbelloni LE, Gouveia MA, Cordeiro JA. Continuous spinal anesthesia versus combined spinal epidural block for major orthopedic surgery: prospective randomized study. Sao Paulo Med J. 2009;127:7–11. doi: 10.1590/S1516-31802009000100003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Gessel E, Forster A, Gamulin Z. A prospective study of the feasibility of continuous spinal anesthesia in a university hospital. Anesth Analg. 1995;80:880–882. doi: 10.1097/00000539-199505000-00005. [DOI] [PubMed] [Google Scholar]
- Lux EA. Continuous spinal anesthesia for lower limb surgery: A retrospective analysis of 1212 cases. Local Reg Anesth. 2012;5:63–67. doi: 10.2147/LRA.S35535. [DOI] [PMC free article] [PubMed] [Google Scholar]


