This cohort study of data from the UK Biobank examines associations between cumulative lifetime cannabis use and all-cause, cardiovascular disease, and cancer mortality.
Key Points
Question
Is there an association between cannabis use and all-cause, cardiovascular disease (CVD), and cancer mortality?
Findings
In this cohort study of 121 895 participants, in the fully adjusted model among females, the risk for CVD mortality was significantly higher among heavy cannabis users compared with never users; there was no association among males. No association was observed among females or males for all-cause and cancer mortality.
Meaning
The findings suggest that heavy cannabis use is associated with CVD mortality among females.
Abstract
Importance
The association between mortality and cannabis use remains unclear.
Objective
To examine sex-stratified associations of cumulative lifetime cannabis use with all-cause, cardiovascular disease (CVD), and cancer mortality in the UK Biobank population.
Design, Setting, and Participants
This cohort study used data from volunteers in the UK Biobank population. Participant monitoring for mortality in the UK Biobank study commenced from the point of their inclusion between 2006 and 2010 and continued until December 19, 2020. Data regarding the causes of death were sourced from the National Health Service Information Centre. Data were analyzed from inception of study inclusion to December 2020.
Exposure
Cannabis use status was assessed by questionnaire and categorized as heavy, moderate, low, and never.
Main Outcomes and Measures
The main outcomes were all-cause, CVD, and cancer mortality. Sex-stratified associations of cumulative lifetime cannabis use with mortality were estimated using Cox proportional hazards regression with adjustment for demographic and clinical variables.
Results
Among 121 895 participants (54.51% females with mean [SD] age of 55.15 [7.64] years; 45.49% males with mean [SD] age of 56.46 [7.79] years) during an overall median of 11.80 years (IQR, 10.53-13.22 years) of follow-up, 2375 total deaths occurred, including 1411 deaths from CVD and 440 from cancer. In males, after full adjustment, the hazard ratios (HRs) were 1.28 (95% CI, 0.90-1.81) for all-cause mortality, 0.98 (95% CI, 0.43-2.25) for CVD mortality, and 1.09 (95% CI, 0.71-1.67) for cancer mortality among heavy cannabis users compared with never users. In females, after full adjustment, the HRs were 1.49 (95% CI, 0.92-2.40) for all-cause mortality, 2.67 (95% CI, 1.19-4.32) for CVD mortality, and 1.61 (95% CI, 0.91-2.83) for cancer mortality among heavy cannabis users compared with never users. In female current tobacco users, after full adjustment, heavy cannabis use was associated with all-cause mortality (HR, 2.25; 95% CI, 1.12-4.53), CVD mortality (HR, 2.56; 95% CI, 1.43-15.36), and cancer mortality (HR, 3.52; 95% CI, 1.50-8.33) and among never tobacco users was associated with CVD mortality (HR, 2.98; 95% CI, 1.67-6.61). In male current tobacco users, heavy cannabis use was associated with cancer mortality (HR, 2.44; 95% CI, 1.14-5.23).
Conclusions and Relevance
In this study, a positive association between CVD mortality and heavy lifetime cannabis use was observed among females. Longitudinal studies are needed in general populations to investigate the potential effects of cannabis on mortality.
Introduction
Cannabis is the most commonly consumed illegal drug globally. Considering the growing movement toward legalizing cannabis across various regions, it has become increasingly critical to comprehend the health consequences of its habitual use. Recent research has indicated a potential increase in cardiovascular (CV) risks associated with cannabis consumption.1,2,3,4,5 However, these studies have been constrained by their focus on specific population segments, which may affect the perceived association of cannabis with CV health.6,7 Additionally, there has been a scarcity of research exploring how cannabis use might affect females and males differently.8,9 Alongside these concerns, the use of cannabis for medical purposes is rapidly expanding,10 yet our understanding of its safety and effectiveness for different medical conditions remains limited.11
While the use of cannabis continues to gain popularity, its broader effects on public health within the general population is not yet fully understood. It was acknowledged in 1 study12 that using cannabis is associated with a heightened risk of being involved in motor vehicle accidents. Additionally, emerging research suggests a possible association between cannabis use and the onset of acute myocardial infarction as well as an elevated risk of ischemic stroke.13 Yet, when it comes to understanding how cannabis use might relate to overall mortality and specific causes of death, the research landscape is limited and presents conflicting findings.
To date, only a couple of studies (of Swedish men aged 18-19 years14 and US patients aged 40 to 49 years15) have suggested that heavy use of marijuana may be associated with an increased risk of death from all causes,14,15 and only 1 study suggested an association with CV mortality.16 On the other hand, several other studies have not found any association between marijuana use and mortality from all causes or specifically from CV diseases (CVDs).7,17,18,19 It is important to note, however, that those studies’ conclusions are potentially limited by factors such as varying methods of measuring marijuana exposure, a limited age range of participants (15-50 years for most of the studies), small sample sizes, or short follow-up durations.7,14,15,17,18,19 Furthermore, to my knowledge, only 1 study thus far has explored the association between marijuana use and cancer mortality, but it did not find an association.16
In 2018, the 12-month prevalence of cannabis use was estimated at 3.9% worldwide; 15.4% of European Union inhabitants aged 15 to 35 years used cannabis in the previous year, and 0.6% of the European population met criteria for cannabis use disorder, resulting in 158 million disability-adjusted life-years.20 Thus, a necessity to understand the association between cannabis use and mortality risk has become more pressing. There is a crucial need to assess the risks of all-cause mortality and its specific underlying causes in association with cannabis use among general populations. The purpose of this study was to examine sex-stratified associations of cumulative lifetime cannabis use with all-cause, CVD, and cancer mortality in the UK Biobank population.
Methods
UK Biobank Population
This cohort study used data from the UK Biobank. The UK Biobank is a forward-looking cohort initiative aimed at investigating, preventing, diagnosing, and treating chronic diseases—notably CVD—in adults. The extensive study encompassed 502 478 individuals from across 22 cities in the UK, all registered with the UK National Health Service. Participants were aged between 40 and 69 years when they joined the UK Biobank between 2006 and 2010 and were thoroughly phenotyped and genotyped. This process involved responses to detailed questionnaires, participation in computer-assisted interviews, and undergoing various physical and functional assessments. Additionally, the collection of biological samples, including blood, urine, and saliva, was integral to the study.21 All participants in the UK Biobank study provided their informed consent electronically. The UK Biobank obtained ethical approval from the North West Multi-center Research Ethics Committee, which extends its jurisdiction across the entire UK. The current study adhered to the principles outlined in the Declaration of Helsinki22 and received approval from the North West–Haydock Research Ethics Committee. This study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline.
The data gathered in the UK Biobank encompass a wide range of factors. These include socioeconomic variables, behavioral and lifestyle information, a comprehensive mental health assessment, clinical diagnoses, and treatments. Furthermore, the cohort has been a rich source of genetic information, with imaging and physiological biomarkers obtained from blood and urine samples. The protocol that guided this extensive collection and analysis of data are thoroughly documented in the scientific literature.23
Ascertainment of Mortality
Participant monitoring for mortality in the UK Biobank study commenced from the point of their inclusion. Follow-up was systematically concluded on December 19, 2020, for all participants. Data regarding the causes of death were sourced from the National Health Service Information Centre. For those interested in the specifics of how these data were linked and processed, comprehensive details are accessible online.24
Causes of CVD mortality were defined with main cause of death corresponding to International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10) codes I00 to I78, G951, H341, H342, O10, S066, Z951, and Z955.25 Causes of cancer mortality were defined with main cause of death corresponding to ICD-10 codes C00 to C96, D00 to D48, and Z85.25
Cannabis Use
Cannabis use was determined through a self-reported questionnaire. Participants were queried about their total lifetime use of cannabis with the question, “Have you ever used cannabis (marijuana, grass, hash, ganja, blow, draw, skunk, weed, spliff, dope), even if it was a long time ago?” Based on their responses, those who answered “no” were categorized as control individuals, while those who answered “yes” were classified as cannabis users. Furthermore, I divided these users into 3 distinct groups, reflecting the frequency of their reported use per the questionnaire categories. These categories included low users of cannabis, defined as those who reported lifetime use 1 to 2 times or 3 to 10 times, and continued users, subdivided into moderate users (11-100 times) and heavy users (>100 times).26 Heavy cannabis use could also be defined, as in the literature, as daily or near daily use for at least a few months.27
Covariates
Systolic and diastolic blood pressure were measured twice at the assessment center during the inclusion consultation using an automated blood pressure device (OMRON 705IT electronic blood pressure monitor [OMRON Healthcare Europe]). Alternatively, measurements were taken manually with a sphygmomanometer and stethoscope in cases in which the blood pressure device failed or the largest cuff did not fit the individual’s arm.28
Hypertension was defined as having a systolic blood pressure of at least 140 mm Hg and/or a diastolic blood pressure of at least 90 mm Hg. This definition aligns with the guidelines set by the European Society of Cardiology and includes cases managed with antihypertensive drugs or diagnosed by a clinician.
Diabetes status was determined by either the use of antidiabetic medication, a diagnosis of diabetes, or a fasting glucose concentration of 126.13 mg/dL or greater (to convert to mmol/L, multiply by 0.0555).29 Dyslipidemia was identified if an individual had a fasting plasma total cholesterol level of 255.21 mg/dL or greater, low-density lipoprotein cholesterol level of 158.30 mg/dL or greater (to convert to mmol/L, multiply by 0.0259), or triglyceride level greater than 150.44 mg/dL (to convert to mmol/L, multiply by 0.0113) or if they were taking statin medication. Medication use was assessed through the question, “Do you regularly take any of the following medications?” Cardiovascular diseases were defined by myocardial infarction, angina, and stroke as diagnosed by a clinician and reported in questionnaires.
Body mass index (BMI) was calculated as weight in kilograms divided by height in meters squared and was categorized as high (>30), moderate (25-30), or low (<25). Detailed information on biological parameters can be found in the UK Biobank protocol.30
Educational level was classified into 3 categories: high (college or university degree), intermediate (A/AS levels or equivalent, O levels/General Certificate of Secondary Education or equivalent, or other professional qualifications [eg, nursing, teaching]), and low (none of the aforementioned). Income level was categorized as high (>£52 000 [US$65 312] per year), moderate (£18 000-£51 999 [US$22 608-$65 311] per year), and low (<£18 000 [US$22 608] per year).
Tobacco smoking and alcohol use were self-reported. For alcohol use status, participants had to report their alcohol use as “current,” “past,” or “never.” In the UK Biobank, the number of years of smoking is calculated by subtracting the age of starting smoking from the age smoking was stopped (or age at inclusion for current tobacco users) using the following equation: pack-years = number of cigarettes per day/(20 × [age stopped smoking − age started smoking]). Antidepressant use was reported by Davis et al31 and was included as a confounding factor due to its association with CV risk32 and the association between cannabis use and depression.33
Statistical Analysis
Characteristics of the study population were described as means with SDs for continuous variables. Categorical variables were described as numbers and proportions. Comparisons between groups were performed using t tests for continuous variables; analysis of variance was performed to assess differences between groups. Pearson χ2 test was performed for categorical variables. Statistical analyses were stratified by sex due to cannabis consumption differences between females and males.34,35
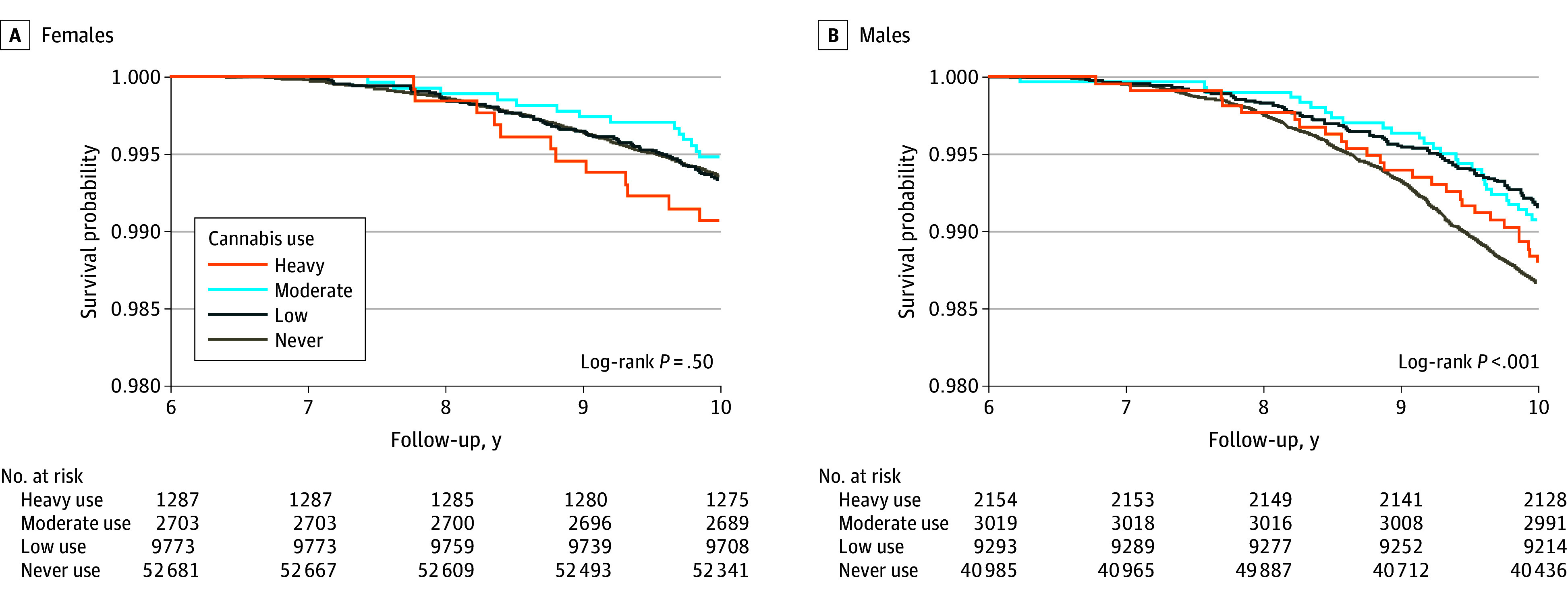
Cox proportional hazards regression models were used to estimate the hazard ratios (HRs) and 95% CIs for the associations between cannabis use and risk of all-cause mortality and cause-specific hazard models for the risk of cause-specific mortality (CV and cancer). Kaplan-Meier analyses censored at 10 years’ follow-up were performed and compared by log-rank test. Follow-up time for each participant was calculated as the difference between the examination date in the UK Biobank and the last known date alive (December 19, 2020) or censored from the linked mortality-life data.
First, sex-stratified Cox proportional hazards regression models were adjusted for age. Second, the fully sex-stratified Cox proportional hazards regression models were adjusted for age, educational level, income, smoking history (pack-years), alcohol status, hypertension, diabetes, dyslipidemia, BMI, previous CVDs, and antidepressant medication use. Never users of cannabis were considered as the reference group in the analyses. Statistical analyses were performed from inception of study inclusion to December 2020 using SAS software, version 9.4 (SAS Institute Inc). Two-sided P <.05 was considered statistically significant.
Results
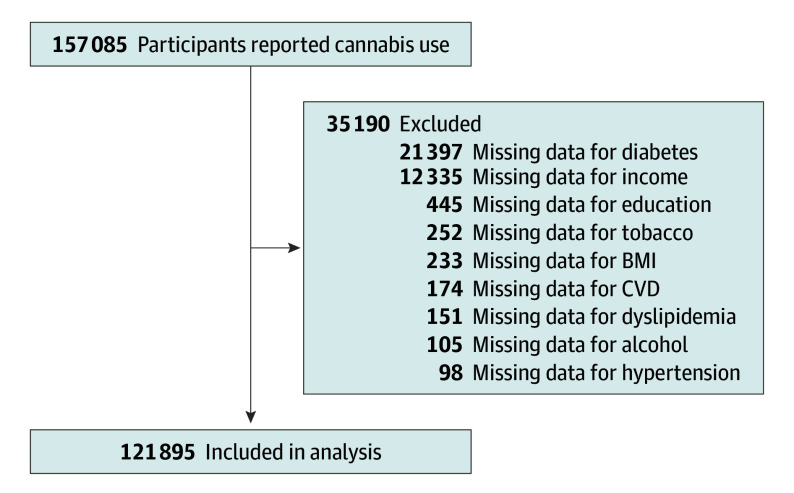
A total of 157 085 volunteers in the UK Biobank study who responded to the questions of cannabis use were included. Of them, 35 190 were excluded for missing data. Therefore, the study analyzed 121 895 volunteers (Figure 1): 66 444 females (54.51%) with mean (SD) age of 55.15 (7.64) years and 55 451 males (45.49%) with mean (SD) age of 56.46 (7.79) years. A total of 2154 males (3.88%) were heavy cannabis users compared with 1287 females (1.94%). Heavy cannabis users were more likely to be younger, report tobacco use, and show lower levels of alcohol use, hypertension, dyslipidemia, obesity, diabetes, high education, and high income (Table 1).
Figure 1. Flowchart of Study Participants.
BMI indicates body mass index; CVD, cardiovascular disease.
Table 1. Characteristics of the Study Population According to Sex and Cannabis Use Status, 2006-2010.
| Characteristic | Participants (N = 121 895)a | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Female (n = 66 444) | Male (n = 55 451) | |||||||||
| Heavy users (n = 1287) | Moderate users (n = 2703) | Low users (n = 9773) | Never users (n = 52 681) | P value | Heavy users (n = 2154) | Moderate users (n = 3019) | Low users (n = 9293) | Never users (n = 40 985) | P value | |
| Age, mean (SD), y | 50.52 (6.76) | 51.28 (6.83) | 52.51 (7.22) | 55.95 (7.56) | <.001 | 50.92 (6.99) | 52.00 (7.06) | 53.92 (7.47) | 57.66 (7.56) | <.001 |
| Follow-up, mean (SD), y | 11.73 (0.89) | 11.79 (0.89) | 11.78 (0.88) | 11.82 (0.87) | <.001 | 11.76 (0.90) | 11.75 (0.89) | 11.80 (0.89) | 11.80 (0.90) | .001 |
| Age at death, mean (SD), y | 84.62 (3.05) | 84.76 (2.37) | 84.80 (1.92) | 84.79 (1.90) | .04 | 84.62 (2.86) | 84.70 (2.46) | 84.74 (2.07) | 84.65 (2.25) | .003 |
| CVD | 13 (1.01) | 31 (1.15) | 107 (1.09) | 1027 (1.95) | <.001 | 67 (3.11) | 108 (3.58) | 397 (4.27) | 2591 (6.32) | <.001 |
| Hypertension | 240 (18.65) | 560 (20.72) | 2444 (25.01) | 18 039 (34.24) | <.001 | 874 (40.58) | 1317 (43.62) | 4546 (48.92) | 23 545 (57.45) | <.001 |
| Diabetes | 37 (2.87) | 100 (3.70) | 317 (3.24) | 2196 (4.17) | <.001 | 107 (4.97) | 136 (4.50) | 537 (5.78) | 2856 (6.97) | <.001 |
| Dyslipidemia | 502 (39.01) | 951 (35.18) | 3816 (39.05) | 24 874 (47.22) | <.001 | 1268 (58.87) | 1756 (58.16) | 5642 (60.71) | 25 961 (63.34) | <.001 |
| Alcohol use | ||||||||||
| Current | 1230 (95.57) | 2619 (96.89) | 9449 (96.68) | 49 052 (93.11) | <.001 | 2012 (93.41) | 2918 (96.65) | 9054 (97.43) | 39 046 (95.27) | <.001 |
| Past | 47 (3.65) | 67 (2.48) | 257 (2.63) | 1455 (2.76) | 133 (6.17) | 96 (3.18) | 214 (2.30) | 992 (2.42) | ||
| Never | 10 (0.78) | 17 (0.63) | 67 (0.69) | 2174 (4.13) | 9 (0.42) | 5 (0.17) | 25 (0.27) | 947 (2.31) | ||
| Educational levelb | ||||||||||
| High | 811 (63.01) | 1860 (68.81) | 6016 (61.56) | 21 787 (41.36) | <.001 | 1231 (57.15) | 1911 (63.30) | 5516 (59.36) | 18 304 (44.66) | <.001 |
| Moderate | 418 (32.48) | 769 (28.45) | 3370 (34.48) | 25 123 (47.69) | 779 (36.17) | 931 (30.84) | 3150 (33.90) | 17 904 (43.68) | ||
| Low | 58 (4.51) | 74 (2.74) | 387 (3.96) | 5771 (10.95) | 144 (6.69) | 177 (5.86) | 627 (6.75) | 4777 (11.66) | ||
| Incomec | ||||||||||
| High | 425 (33.02) | 1119 (41.40) | 4029 (41.23) | 15 154 (28.77) | <.001 | 886 (41.13) | 1569 (51.97) | 4432 (47.69) | 13 751 (33.55) | <.001 |
| Moderate | 625 (48.56) | 1288 (47.65) | 4655 (47.63) | 28 746 (54.57) | 973 (45.17) | 1182 (39.15) | 4074 (43.84) | 22 203 (54.17) | ||
| Low | 237 (18.41) | 296 (10.95) | 1089 (11.14) | 8781 (16.67) | 295 (13.70) | 268 (8.88) | 787 (8.47) | 5031 (12.28) | ||
| Tobacco smoking | ||||||||||
| Current | 454 (35.28) | 436 (16.13) | 1094 (11.19) | 2229 (4.23) | <.001 | 754 (35.00) | 480 (15.90) | 1174 (12.63) | 2360 (5.76) | <.001 |
| Past | 755 (58.66) | 1798 (66.52) | 4994 (51.10) | 14 283 (27.11) | 1197 (55.57) | 1757 (58.20) | 4448 (47.86) | 14 031 (34.23) | ||
| Never | 78 (6.06) | 469 (17.35) | 3685 (37.71) | 36 169 (68.66) | 203 (9.42) | 782 (25.90) | 3671 (39.50) | 24 594 (60.01) | ||
| Smoking history, mean (SD), pack-years | 16 (13) | 12 (13) | 9 (13) | 4 (10) | <.001 | 18 (16) | 13 (16) | 11 (16) | 7 (14) | <.001 |
| BMId | ||||||||||
| High | 179 (13.91) | 407 (15.06) | 1625 (16.63) | 10 412 (19.76) | <.001 | 350 (16.25) | 549 (18.18) | 1891 (20.35) | 8950 (21.84) | <.001 |
| Moderate | 428 (33.26) | 789 (29.19) | 3245 (33.20) | 18 779 (35.65) | 990 (45.96) | 1429 (47.33) | 4561 (49.08) | 20 430 (49.85) | ||
| Low | 680 (52.84) | 1507 (55.75) | 4903 (50.17) | 23 490 (44.59) | 814 (37.79) | 1041 (34.48) | 2841 (30.57) | 11 605 (28.32) | ||
| Antidepressant use | 112 (8.70) | 200 (7.40) | 762 (7.80) | 3895 (7.39) | .20 | 121 (5.62) | 112 (3.71) | 343 (3.69) | 1481 (3.61) | <.001 |
Abbreviations: BMI, body mass index (calculated as weight in kilograms divided by height in meters squared); CVD, cardiovascular disease.
Data are presented as number (percentage) of participants unless otherwise indicated.
High educational level, college or university degree; moderate, A/AS levels or equivalent, O levels/General Certificate of Secondary Education or equivalent, or other professional qualifications; and low, none of these.
High income, greater than £52 000 (US$65 312) per year; moderate, £18 000 to £51 999 (US$22 608-$65 311) per year; and low, less than £18 000 (US$22 608) per year.
High BMI, greater than 30; moderate, 25 to 30; and low, less than 25.
The median follow-up overall was 11.80 years (IQR, 10.53-13.22 years); among females, median follow-up was 11.81 years (IQR, 10.54-13.24 years), and among males, it was 11.80 years (IQR, 10.53-13.21 years). During this time, 2375 total deaths occurred, including 1411 deaths from CVD and 440 from cancer. A total of 964 deaths among females (1.45%) and 1401 deaths among males (2.53%) were from all causes, including 125 (0.19%) and 315 (0.57%) deaths from CVD, respectively, and 658 (0.99%) and 753 (1.36%) deaths from cancer, respectively. Figure 2 presents the evolution of death according to cannabis status in both sexes.
Figure 2. Kaplan-Meier Curves for All-Cause Mortality in Females and Males According to Cannabis Use.
In males, after adjustment for age, the HRs among participants who were heavy cannabis users compared with never users were 1.50 (95% CI, 1.09-2.05) for all-cause mortality, 1.36 (95% CI, 0.70-2.69) for CVD mortality, and 1.18 (95% CI, 0.73-1.89) for cancer mortality (Table 2). In the fully adjusted model for males, the HRs among participants who were heavy cannabis users were 1.28 (95% CI, 0.90-1.81) for all-cause mortality, 0.98 (95% CI, 0.43-2.25) for CVD mortality, and 1.09 (95% CI, 0.71-1.67) for cancer mortality.
Table 2. Sex-Stratified Cox Proportional Hazards Regression Models for All-Cause, CVD, and Cancer Mortality.
| Model, variable | Hazard ratio (95% CI) | ||
|---|---|---|---|
| All-cause mortality | CVD mortality | Cancer mortality | |
| Females | |||
| Age-adjusted model | |||
| Cannabis use | |||
| Heavy | 1.88 (1.21-2.91) | 2.47 (1.13-5.38) | 1.99 (1.21-3.29) |
| Moderate | 1.20 (0.84-1.73) | 2.32 (0.79-6.05) | 1.10 (0.70-1.72) |
| Low | 1.17 (0.96-1.41) | 1.07 (0.60-1.92) | 1.22 (0.97-1.53) |
| Never | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Fully adjusted modela | |||
| Cannabis use | |||
| Heavy | 1.49 (0.92-2.40) | 2.67 (1.19-4.32) | 1.61 (0.91-2.83) |
| Moderate | 1.07 (0.72-1.60) | 2.24 (0.68-3.32) | 0.92 (0.55-1.56) |
| Low | 1.07 (0.87-1.33) | 0.94 (0.48-1.84) | 1.20 (0.93-1.55) |
| Never | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Males | |||
| Age-adjusted model | |||
| Cannabis use | |||
| Heavy | 1.50 (1.09-2.05) | 1.36 (0.70-2.69) | 1.18 (0.73-1.89) |
| Moderate | 1.11 (0.83-1.48) | 0.77 (0.38-1.58) | 1.29 (0.89-1.86) |
| Low | 0.95 (0.80-1.12) | 0.76 (0.52-1.11) | 1.03 (0.83-1.29) |
| Never | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Fully adjusted modela | |||
| Cannabis use | |||
| Heavy | 1.28 (0.90-1.81) | 0.98 (0.43-2.25) | 1.09 (0.71-1.67) |
| Moderate | 0.97 (0.70-1.36) | 0.80 (0.37-1.72) | 1.01 (0.60-1.71) |
| Low | 0.88 (0.72-1.07) | 0.75 (0.49-1.14) | 0.95 (0.74-1.21) |
| Never | 1 [Reference] | 1 [Reference] | 1 [Reference] |
Abbreviation: CVD, cardiovascular disease.
Adjusted for age, educational level, income, smoking history (pack-years), alcohol status, hypertension, diabetes, dyslipidemia, body mass index, previous CVDs, and antidepressant medication.
In females, after adjustment for age, the HRs among participants who were heavy cannabis users compared with never users were 1.88 (95% CI, 1.21-2.91) for all-cause mortality, 2.47 (95% CI, 1.13-5.38) for CVD mortality, and 1.99 (95% CI, 1.21-3.29) for cancer mortality (Table 2). In the fully adjusted model for females, the HRs among participants who were heavy cannabis users were 1.49 (95% CI, 0.92-2.40) for all-cause mortality, 2.67 (95% CI, 1.19-4.32) for CVD mortality, and 1.61 (95% CI, 0.91-2.83) for cancer mortality. Results for all covariates are shown in eTables 1 and 2 in Supplement 1.
In males who were current tobacco users, after adjustment for all covariates, heavy cannabis use was significantly associated with cancer mortality (HR, 2.44; 95% CI, 1.14-5.23). In females who currently used tobacco, after adjustment for all covariates, heavy cannabis use was significantly associated with all-cause mortality (HR, 2.25; 95% CI, 1.12-4.53), CVD mortality (HR, 2.56; 95% CI, 1.43-15.36), and cancer mortality (HR, 3.52; 95% CI, 1.50-8.33). Heavy cannabis use was associated with CVD mortality (HR, 2.98; 95% CI, 1.67-6.61) among females who had never used tobacco (Table 3).
Table 3. Fully Adjusted Sex-Stratified Cox Proportional Hazards Regression Models for All-Cause, CVD, and Cancer Mortality According to Tobacco Smoking Status.
| Variable | Hazard ratio (95% CI) | ||
|---|---|---|---|
| All-cause mortality | CVD mortality | Cancer mortality | |
| Females | |||
| Current tobacco use | |||
| Cannabis use | |||
| Heavy | 2.25 (1.12-4.53) | 2.56 (1.43-15.36) | 3.52 (1.50-8.33) |
| Moderate | 1.57 (0.68-3.63) | 2.31 (0.39-13.56) | 2.02 (1.04-3.92) |
| Low | 1.59 (0.96-2.66) | 0.62 (0.07-5.72) | 2.10 (0.69-4.39) |
| Never | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Past tobacco use | |||
| Cannabis use | |||
| Heavy | 0.87 (0.38-1.99) | NA | 1.03 (0.41-2.59) |
| Moderate | 0.87 (0.49-1.57) | 2.96 (0.92-9.53) | 0.66 (0.30-1.45) |
| Low | 1.09 (0.79-1.53) | 1.32 (0.51-3.43) | 1.27 (0.87-1.87) |
| Never | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Never tobacco use | |||
| Cannabis use | |||
| Heavy | 1.68 (0.23-11.97) | 2.98 (1.67-6.61) | NA |
| Moderate | 1.43 (0.64-3.22) | 2.39 (0.32-7.59) | 1.33 (0.49-3.59) |
| Low | 0.81 (0.56-1.21) | 0.87 (0.27-2.82) | 0.86 (0.54-1.34) |
| Never | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Males | |||
| Current tobacco use | |||
| Cannabis use | |||
| Heavy | 1.51 (0.83-2.73) | 1.11 (0.32-3.89) | 2.44 (1.14-5.23) |
| Moderate | 1.15 (0.64-2.05) | 0.90 (0.22-2.92) | 1.14 (0.46-2.82) |
| Low | 1.09 (0.71-1.68) | 0.53 (0.18-1.58) | 1.65 (0.94-2.91) |
| Never | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Past tobacco use | |||
| Cannabis use | |||
| Heavy | 1.25 (0.75-2.08) | 1.10 (0.33-3.63) | 1.15 (0.57-2.32) |
| Moderate | 0.78 (0.46-1.30) | 0.68 (0.21-2.20) | 0.83 (0.43-1.62) |
| Low | 0.95 (0.72-1.25) | 0.83 (0.46-1.52) | 0.99 (0.68-1.44) |
| Never | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Never tobacco use | |||
| Cannabis use | |||
| Heavy | 0.85 (0.21-3.43) | NA | NA |
| Moderate | 0.85 (0.40-1.80) | 0.56 (0.07-4.07) | 0.78 (0.29-2.12) |
| Low | 0.83 (0.43-1.91) | 0.71 (0.35-1.48) | 0.61 (0.28-1.99) |
| Never | 1 [Reference] | 1 [Reference] | 1 [Reference] |
Abbreviations: CVD, cardiovascular disease; NA, not applicable.
When excluding participants with hypertension, diabetes, obesity, current tobacco use, and previous CVD (55 517 participants [45.54%]), in females, heavy cannabis use was not associated with all-cause mortality (HR, 1.48; 95% CI, 0.64-3.39), cancer mortality (HR, 1.81; 95% CI, 0.73-4.50), or CVD mortality (HR, 1.81; 95% CI, 0.39-8.34). Similar results were observed among males (all-cause: HR, 1.15 [95% CI, 0.50-2.65]; cancer: HR, 0.92 [95% CI, 0.29-2.95]; CVD: HR, 1.35 [95% CI, 0.85-6.74]).
Moreover, in stratified analyses, we found that among females with overweight, heavy cannabis use was associated with all-cause mortality (HR, 2.23; 95% CI, 1.11-4.45) and cancer mortality (HR, 2.79; 95% CI, 1.32-5.88). Among males without hypertension, heavy cannabis use was associated with all-cause mortality (HR, 1.52; 95% CI, 1.01-2.32). Heavy cannabis use was associated with all-cause mortality (HR, 2.14; 95% CI, 1.29-3.54) and cancer mortality (HR, 2.43; 95% CI, 1.36-4.32) among females without hypertension. Among females without diabetes, heavy cannabis use was associated with CVD mortality (HR, 2.92; 95% CI, 1.21-7.05) (eTables 3-5 in Supplement 1).
When considering only the status of cannabis use among users compared with never users, no significant association with all-cause mortality (HR, 1.11; 95% CI, 0.91-1.34), CVD mortality (HR, 1.35; 95% CI, 0.80-2.27), or cancer mortality (HR, 1.18; 95% CI, 0.94-1.49) was shown among females. Similar results were observed among males (all-cause: HR, 1.06 [95% CI, 0.90-1.24]; CVD: HR, 1.27 [95% CI, 0.89-1.82]; cancer: HR, 1.02 [95% CI, 0.82-1.26]).
Discussion
The relationship between cannabis use and specific causes of mortality in the general population remains largely unexplored. Previous research has primarily focused on all-cause mortality among younger groups,14,15,16,17,18,19 with the majority of these studies,14,15,18,19 but not all,16,17 indicating a heightened risk of all-cause mortality associated with cannabis use. However, only a handful of studies have delved into the potential association between cannabis use and CVD mortality but found no association15,17,19; an exception is a study focused on 14 818 middle-aged (age 20-59 years) US adults with a median follow-up of 5.8 years that showed a significant association between ever use of cannabis and CVD mortality (HR, 2.29; 95% CI, 1.10-4.78).16 In contrast, another study tracking 1913 adults hospitalized for myocardial infarction over a median of 3.8 years reported a nondefinitive adjusted HR of 1.9 (95% CI, 0.6-6.3) for CVD mortality.15 This aligns with existing research indicating a greater risk of acute myocardial infarction and ischemic stroke associated with cannabis use.2,36 Other studies on this topic that primarily involved younger participants aged 18 to 30 years19 and 15 to 49 years17 did not find that higher mortality was associated with cannabis use.
The potential connection between cannabis use and CVD mortality is biologically credible. Research suggests that certain cannabinoids, like D9-tetrahydrocannabinol, that are key components of cannabis may contribute to inflammation, endothelial dysfunction, and atherosclerosis development.37 Another contributing factor could be the increased exposure to carbon monoxide through cannabis smoking, leading to higher levels of carboxyhemoglobin in the blood.38 This may impair the oxygen-carrying capacity in blood, reducing oxygen availability in tissues and cells, including myocardial cells, and potentially triggering angina, especially in individuals with preexisting coronary heart disease.15
Individuals who use cannabis are at an elevated risk of experiencing vessel ruptures, a condition exacerbated by the increased release of cerebral dopamine. This increase can stimulate cerebral blood flow, lead to vasospasms, and cause vasoconstriction.39 However, comprehensive data on the association of cannabis use with other CVDs is still lacking. There is some evidence suggesting an association between cannabis use and a heightened risk of heart failure40 and atherosclerosis, particularly among current tobacco users.41 Additionally, cannabis use has been associated with an increased risk of mortality following myocardial infarction.42,43,44
One study found a correlation between cannabis use and a higher risk of CVDs in individuals who do not use tobacco.45 Further research, even after adjusting for tobacco use, has indicated a causal relationship between cannabis use and an increased risk of small vessel strokes.46 Cannabis use may directly impact the CV system by raising blood pressure and heart rate, inducing vasoconstriction, and increasing carboxyhemoglobin levels, all of which elevate the risk of ischemia.36,42 Chronic cannabis use has been associated with higher levels of apolipoprotein C3 in the blood, a known risk factor for CVDs.36 Additionally, cannabis is often consumed alongside tobacco, alcohol, and other illicit drugs,43,47 a combination that can further amplify the risk of CV events and diseases.46
Sex differences for actions of cannabis use were observed in this study, which found a significant association between heavy cannabis use and CVD mortality among females overall and females who currently used tobacco but not among males. Earlier research highlighted variations by sex in both the frequency of cannabis use and the CV reactions associated with it.4,8 Insights from animal studies suggest that gonadal hormones might play a role in how cannabinoids affect metabolic balance and potentially influence the density of cannabinoid receptors in a sex-specific manner.48 The sensitivity of these cannabinoid receptors appears to be differentially affected by estrogen and testosterone, which could account for the observed sex disparities. Additionally, there is evidence indicating that over similar periods of cannabis use, females tend to consume fewer cannabis cigarettes than males.49 This leads to lower tetrahydrocannabinol concentrations in their bloodstream, possibly due to varying responses to the strength of the cannabis, which results in different use patterns between sexes.50
As this study observed for males and females overall, 1 previous study investigated the association between cannabis use and cancer mortality but did not find an association.16 The relationship between cannabis use and the incidence of cancer remains unclear. Current evidence, which is somewhat limited, suggests there might be an association between cannabis use and certain types of cancers, such as testicular51 and lung52 cancers, but is ambiguous for head, neck, and esophageal cancers.16 Future studies in humans are required to investigate the relationship between cannabis use and cancer mortality.
Strengths and Limitations
This study’s primary strength lies in the expansive sample size provided by the UK Biobank cohort. However, its cross-sectional design introduces limitations in establishing causality, leaving open the possibility of reverse causation. A notable concern is the low response rate of 5.5% in the UK Biobank study,53 which could introduce participant bias. Despite this, the robust sample size54 and high internal validity make it unlikely that these limitations significantly influenced the observed associations.55,56 The study’s focus on middle-aged participants from the UK also limits the generalizability of its findings to other age groups and ethnicities. Nonetheless, the use of standardized protocols in data collection by the UK Biobank enhances the external validity of the results, ensuring consistent data collection across various conditions and personnel.
The study, however, is not without limitations. Socioeconomic data, medical history, and comorbidities were primarily gathered through self-reported questionnaires or assessments during medical examinations at health centers. Additionally, the data collection period (2006-2010) may not accurately reflect current patterns and risks associated with cannabis use. Cannabis use was self-reported rather than verified through urine or blood tests, though the reliability of self-reported cannabis use is estimated to be congruent with drug tests in 89.8% of cases.57 In this study, there was no information on the frequency of cannabis use in the 30 days preceding the interview, making it challenging to differentiate between associations of short-term and long-term cannabis use with mortality. The study also lacked specific data on tetrahydrocannabinol levels, cannabidiol content, and the method of cannabis consumption (eg, vaping, oral). This absence of detailed information represents a significant limitation and points to the need for further research in these areas. No information during follow-up was collected for cannabis use; thus, some participants may have continued as long-term users or not. Consequently, it is possible that the impact of prolonged, regular cannabis use was not fully captured in these findings. Future research using more precise measurements of cannabis use over extended periods is necessary to validate these results. Additionally, as the precise dosage of cannabis was not consistently recorded across all study phases, the investigation was unable to determine whether there is a dose-response relationship between cannabis use and mortality. This aspect presents an important direction for exploration in upcoming studies.
Conclusions
This cohort study found a positive association between CVD mortality and heavy lifetime cannabis use among females. Longitudinal studies are needed in general populations to investigate potential causal effects of cannabis on mortality. Individuals using cannabis should be considered for appropriate CV risk–reduction strategies, especially among females.
eTable 1. Cox Proportional Hazards Regression Among Males for the Association With All-Cause Mortality
eTable 2. Cox Proportional Hazards Regression Among Females for the Association With All-Cause Mortality
eTable 3. Fully Adjusted Sex-Stratified Cox Proportional Hazards Regression Models for All-Cause, CVD, and Cancer Mortality According to BMI Level
eTable 4. Fully Adjusted Sex-Stratified Cox Proportional Hazards Regression Models for All-Cause, CVD, and Cancer Mortality According to Hypertension Status
eTable 5. Fully Adjusted Sex-Stratified Cox Proportional Hazards Regression Models for All-Cause, CVD, and Cancer Mortality According to Diabetes Status
Data Sharing Statement
References
- 1.Thomas G, Kloner RA, Rezkalla S. Adverse cardiovascular, cerebrovascular, and peripheral vascular effects of marijuana inhalation: what cardiologists need to know. Am J Cardiol. 2014;113(1):187-190. doi: 10.1016/j.amjcard.2013.09.042 [DOI] [PubMed] [Google Scholar]
- 2.Mittleman MA, Lewis RA, Maclure M, Sherwood JB, Muller JE. Triggering myocardial infarction by marijuana. Circulation. 2001;103(23):2805-2809. doi: 10.1161/01.CIR.103.23.2805 [DOI] [PubMed] [Google Scholar]
- 3.Jouanjus E, Raymond V, Lapeyre-Mestre M, Wolff V. What is the current knowledge about the cardiovascular risk for users of cannabis-based products? a systematic review. Curr Atheroscler Rep. 2017;19(6):26. doi: 10.1007/s11883-017-0663-0 [DOI] [PubMed] [Google Scholar]
- 4.Vallée A. Association between cannabis use and ten-year estimated atherosclerotic cardiovascular disease risk in a middle-aged population survey. Eur J Intern Med. 2023;111:69-76. doi: 10.1016/j.ejim.2023.02.020 [DOI] [PubMed] [Google Scholar]
- 5.Vallée A. Association between lifetime cannabis use and arterial stiffness in a middle-aged general population. J Hypertens. 2023;41(4):658-669. doi: 10.1097/HJH.0000000000003389 [DOI] [PubMed] [Google Scholar]
- 6.Jouanjus E, Lapeyre-Mestre M, Micallef J; French Association of the Regional Abuse and Dependence Monitoring Centres (CEIP-A) Working Group on Cannabis Complications . Cannabis use: signal of increasing risk of serious cardiovascular disorders. J Am Heart Assoc. 2014;3(2):e000638. doi: 10.1161/JAHA.113.000638 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Reis JP, Auer R, Bancks MP, et al. Cumulative lifetime marijuana use and incident cardiovascular disease in middle age: the Coronary Artery Risk Development in Young Adults (CARDIA) Study. Am J Public Health. 2017;107(4):601-606. doi: 10.2105/AJPH.2017.303654 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Waterreus A, Di Prinzio P, Martin-Iverson MT, Morgan VA. Sex differences in the cardiometabolic health of cannabis users with a psychotic illness. Drug Alcohol Depend. 2019;194:447-452. doi: 10.1016/j.drugalcdep.2018.11.006 [DOI] [PubMed] [Google Scholar]
- 9.Wetherington CL. Sex-gender differences in drug abuse: a shift in the burden of proof? Exp Clin Psychopharmacol. 2007;15(5):411-417. doi: 10.1037/1064-1297.15.5.411 [DOI] [PubMed] [Google Scholar]
- 10.Park JY, Wu LT. Prevalence, reasons, perceived effects, and correlates of medical marijuana use: a review. Drug Alcohol Depend. 2017;177:1-13. doi: 10.1016/j.drugalcdep.2017.03.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Whiting PF, Wolff RF, Deshpande S, et al. Cannabinoids for medical use: a systematic review and meta-analysis. JAMA. 2015;313(24):2456-2473. doi: 10.1001/jama.2015.6358 [DOI] [PubMed] [Google Scholar]
- 12.Brubacher JR, Chan H, Erdelyi S, et al. Cannabis use as a risk factor for causing motor vehicle crashes: a prospective study. Addiction. 2019;114(9):1616-1626. doi: 10.1111/add.14663 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jeffers AM, Glantz S, Byers AL, Keyhani S. Association of cannabis use with cardiovascular outcomes among US adults. J Am Heart Assoc. 2024;13(5):e030178. doi: 10.1161/JAHA.123.030178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Manrique-Garcia E, Ponce de Leon A, Dalman C, Andréasson S, Allebeck P. Cannabis, psychosis, and mortality: a cohort study of 50,373 Swedish men. Am J Psychiatry. 2016;173(8):790-798. doi: 10.1176/appi.ajp.2016.14050637 [DOI] [PubMed] [Google Scholar]
- 15.Mukamal KJ, Maclure M, Muller JE, Mittleman MA. An exploratory prospective study of marijuana use and mortality following acute myocardial infarction. Am Heart J. 2008;155(3):465-470. doi: 10.1016/j.ahj.2007.10.049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sun Y, Liu B, Wallace RB, Bao W. Association of cannabis use with all-cause and cause-specific mortality among younger- and middle-aged US adults. Am J Prev Med. 2020;59(6):873-879. doi: 10.1016/j.amepre.2020.07.010 [DOI] [PubMed] [Google Scholar]
- 17.Sidney S, Beck JE, Tekawa IS, Quesenberry CP, Friedman GD. Marijuana use and mortality. Am J Public Health. 1997;87(4):585-590. doi: 10.2105/AJPH.87.4.585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Muhuri PK, Gfroerer JC. Mortality associated with illegal drug use among adults in the United States. Am J Drug Alcohol Abuse. 2011;37(3):155-164. doi: 10.3109/00952990.2011.553977 [DOI] [PubMed] [Google Scholar]
- 19.Andréasson S, Allebeck P. Cannabis and mortality among young men: a longitudinal study of Swedish conscripts. Scand J Soc Med. 1990;18(1):9-15. doi: 10.1177/140349489001800102 [DOI] [PubMed] [Google Scholar]
- 20.Manthey J, Freeman TP, Kilian C, López-Pelayo H, Rehm J. Public health monitoring of cannabis use in Europe: prevalence of use, cannabis potency, and treatment rates. Lancet Reg Health Eur. 2021;10:100227. doi: 10.1016/j.lanepe.2021.100227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sudlow C, Gallacher J, Allen N, et al. UK Biobank: an open access resource for identifying the causes of a wide range of complex diseases of middle and old age. PLoS Med. 2015;12(3):e1001779. doi: 10.1371/journal.pmed.1001779 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.World Medical Association . World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310(20):2191-2194. doi: 10.1001/jama.2013.281053 [DOI] [PubMed] [Google Scholar]
- 23.Bycroft C, Freeman C, Petkova D, et al. The UK Biobank resource with deep phenotyping and genomic data. Nature. 2018;562(7726):203-209. doi: 10.1038/s41586-018-0579-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Biobank UK. Mortality data: linkage to death registries. Version 3.0. Accessed January 31, 2024. https://biobank.ctsu.ox.ac.uk/crystal/refer.cgi?id=115559
- 25.Said MA, Eppinga RN, Lipsic E, Verweij N, van der Harst P. Relationship of arterial stiffness index and pulse pressure with cardiovascular disease and mortality. J Am Heart Assoc. 2018;7(2):e007621. doi: 10.1161/JAHA.117.007621 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Vallée A. Association between cannabis use and blood pressure levels according to comorbidities and socioeconomic status. Sci Rep. 2023;13(1):2069. doi: 10.1038/s41598-022-22841-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kroon E, Kuhns L, Hoch E, Cousijn J. Heavy cannabis use, dependence and the brain: a clinical perspective. Addiction. 2020;115(3):559-572. doi: 10.1111/add.14776 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Biobank UK. Arterial pulse-wave velocity. Accessed January 31, 2024. https://biobank.ndph.ox.ac.uk/ukb/ukb/docs/Pulsewave.pdf
- 29.Sarwar N, Gao P, Seshasai SR, et al. ; Emerging Risk Factors Collaboration . Diabetes mellitus, fasting blood glucose concentration, and risk of vascular disease: a collaborative meta-analysis of 102 prospective studies. Lancet. 2010;375(9733):2215-2222. doi: 10.1016/S0140-6736(10)60484-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.UK Biobank. Biomarker assay quality procedures: approaches used to minimise systematic and random errors (and the wider epidemiological implications). April 2, 2019. Accessed January 31, 2024. https://biobank.ctsu.ox.ac.uk/crystal/crystal/docs/biomarker_issues.pdf
- 31.Davis KAS, Cullen B, Adams M, et al. Indicators of mental disorders in UK Biobank—a comparison of approaches. Int J Methods Psychiatr Res. 2019;28(3):e1796. doi: 10.1002/mpr.1796 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jang HY, Kim JH, Song YK, et al. Antidepressant use and the risk of major adverse cardiovascular events in patients without known cardiovascular disease: a retrospective cohort study. Front Pharmacol. 2020;11:594474. doi: 10.3389/fphar.2020.594474 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lev-Ran S, Roerecke M, Le Foll B, George TP, McKenzie K, Rehm J. The association between cannabis use and depression: a systematic review and meta-analysis of longitudinal studies. Psychol Med. 2014;44(4):797-810. doi: 10.1017/S0033291713001438 [DOI] [PubMed] [Google Scholar]
- 34.Matheson J, Sproule B, Di Ciano P, et al. Sex differences in the acute effects of smoked cannabis: evidence from a human laboratory study of young adults. Psychopharmacology (Berl). 2020;237(2):305-316. doi: 10.1007/s00213-019-05369-y [DOI] [PubMed] [Google Scholar]
- 35.Vallée A. Sexual behaviors, cannabis, alcohol and monkeypox infection. Front Public Health. 2023;10:1054488. doi: 10.3389/fpubh.2022.1054488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rumalla K, Reddy AY, Mittal MK. Recreational marijuana use and acute ischemic stroke: a population-based analysis of hospitalized patients in the United States. J Neurol Sci. 2016;364:191-196. doi: 10.1016/j.jns.2016.01.066 [DOI] [PubMed] [Google Scholar]
- 37.Ravi D, Ghasemiesfe M, Korenstein D, Cascino T, Keyhani S. Associations between marijuana use and cardiovascular risk factors and outcomes: a systematic review. Ann Intern Med. 2018;168(3):187-194. doi: 10.7326/M17-1548 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Azorlosa JL, Greenwald MK, Stitzer ML. Marijuana smoking: effects of varying puff volume and breathhold duration. J Pharmacol Exp Ther. 1995;272(2):560-569. [PubMed] [Google Scholar]
- 39.Rumalla K, Reddy AY, Mittal MK. Association of recreational marijuana use with aneurysmal subarachnoid hemorrhage. J Stroke Cerebrovasc Dis. 2016;25(2):452-460. doi: 10.1016/j.jstrokecerebrovasdis.2015.10.019 [DOI] [PubMed] [Google Scholar]
- 40.Kalla A, Krishnamoorthy PM, Gopalakrishnan A, Figueredo VM. Cannabis use predicts risks of heart failure and cerebrovascular accidents: results from the National Inpatient Sample. J Cardiovasc Med (Hagerstown). 2018;19(9):480-484. doi: 10.2459/JCM.0000000000000681 [DOI] [PubMed] [Google Scholar]
- 41.Auer R, Sidney S, Goff D, et al. Lifetime marijuana use and subclinical atherosclerosis: the Coronary Artery Risk Development in Young Adults (CARDIA) Study. Addiction. 2018;113(5):845-856. doi: 10.1111/add.14110 [DOI] [PubMed] [Google Scholar]
- 42.Frost L, Mostofsky E, Rosenbloom JI, Mukamal KJ, Mittleman MA. Marijuana use and long-term mortality among survivors of acute myocardial infarction. Am Heart J. 2013;165(2):170-175. doi: 10.1016/j.ahj.2012.11.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.DeFilippis EM, Singh A, Divakaran S, et al. Cocaine and marijuana use among young adults with myocardial infarction. J Am Coll Cardiol. 2018;71(22):2540-2551. doi: 10.1016/j.jacc.2018.02.047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.DeFilippis EM, Bajaj NS, Singh A, et al. Marijuana use in patients with cardiovascular disease: JACC review topic of the week. J Am Coll Cardiol. 2020;75(3):320-332. doi: 10.1016/j.jacc.2019.11.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Winhusen T, Theobald J, Kaelber DC, Lewis D. The association between regular cannabis use, with and without tobacco co-use, and adverse cardiovascular outcomes: cannabis may have a greater impact in non-tobacco smokers. Am J Drug Alcohol Abuse. 2020;46(4):454-461. doi: 10.1080/00952990.2019.1676433 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Zhao J, Chen H, Zhuo C, Xia S. Cannabis use and the risk of cardiovascular diseases: a mendelian randomization study. Front Cardiovasc Med. 2021;8:676850. doi: 10.3389/fcvm.2021.676850 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Falkstedt D, Wolff V, Allebeck P, Hemmingsson T, Danielsson AK. Cannabis, tobacco, alcohol use, and the risk of early stroke: a population-based cohort study of 45 000 Swedish men. Stroke. 2017;48(2):265-270. doi: 10.1161/STROKEAHA.116.015565 [DOI] [PubMed] [Google Scholar]
- 48.Cooper ZD, Craft RM. Sex-dependent effects of cannabis and cannabinoids: a translational perspective. Neuropsychopharmacology. 2018;43(1):34-51. doi: 10.1038/npp.2017.140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Cuttler C, Mischley LK, Sexton M. Sex differences in cannabis use and effects: a cross-sectional survey of cannabis users. Cannabis Cannabinoid Res. 2016;1(1):166-175. doi: 10.1089/can.2016.0010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Fogel JS, Kelly TH, Westgate PM, Lile JA. Sex differences in the subjective effects of oral Δ9-THC in cannabis users. Pharmacol Biochem Behav. 2017;152:44-51. doi: 10.1016/j.pbb.2016.01.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ghasemiesfe M, Barrow B, Leonard S, Keyhani S, Korenstein D. Association between marijuana use and risk of cancer: a systematic review and meta-analysis. JAMA Netw Open. 2019;2(11):e1916318. doi: 10.1001/jamanetworkopen.2019.16318 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Callaghan RC, Allebeck P, Sidorchuk A. Marijuana use and risk of lung cancer: a 40-year cohort study. Cancer Causes Control. 2013;24(10):1811-1820. doi: 10.1007/s10552-013-0259-0 [DOI] [PubMed] [Google Scholar]
- 53.Batty GD, Gale CR, Kivimäki M, Deary IJ, Bell S. Comparison of risk factor associations in UK Biobank against representative, general population based studies with conventional response rates: prospective cohort study and individual participant meta-analysis. BMJ. 2020;368:m131. doi: 10.1136/bmj.m131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Keyes KM, Westreich D. UK Biobank, big data, and the consequences of non-representativeness. Lancet. 2019;393(10178):1297. doi: 10.1016/S0140-6736(18)33067-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Richiardi L, Pizzi C, Pearce N. Commentary: representativeness is usually not necessary and often should be avoided. Int J Epidemiol. 2013;42(4):1018-1022. doi: 10.1093/ije/dyt103 [DOI] [PubMed] [Google Scholar]
- 56.Rothman KJ, Gallacher JEJ, Hatch EE. Why representativeness should be avoided. Int J Epidemiol. 2013;42(4):1012-1014. doi: 10.1093/ije/dys223 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Harrison L. The validity of self-reported drug use in survey research: an overview and critique of research methods. NIDA Res Monogr. 1997;167:17-36. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. Cox Proportional Hazards Regression Among Males for the Association With All-Cause Mortality
eTable 2. Cox Proportional Hazards Regression Among Females for the Association With All-Cause Mortality
eTable 3. Fully Adjusted Sex-Stratified Cox Proportional Hazards Regression Models for All-Cause, CVD, and Cancer Mortality According to BMI Level
eTable 4. Fully Adjusted Sex-Stratified Cox Proportional Hazards Regression Models for All-Cause, CVD, and Cancer Mortality According to Hypertension Status
eTable 5. Fully Adjusted Sex-Stratified Cox Proportional Hazards Regression Models for All-Cause, CVD, and Cancer Mortality According to Diabetes Status
Data Sharing Statement