Key Points
Question
In Black and Hispanic stroke survivors with uncontrolled hypertension, does home blood pressure telemonitoring (HBPTM) plus nurse case management (NCM) result in greater systolic blood pressure reduction than HBPTM alone?
Findings
In this randomized clinical trial that included 450 predominantly low-income Black and Hispanic stroke survivors with uncontrolled hypertension and significant comorbidity, those in the NCM plus HBPTM group had a relatively greater systolic blood pressure reduction than those in the HBPTM alone group at 12 months (−15.1 mm Hg and −5.8 mm Hg, respectively). There was no difference in the rate of recurrent stroke between both groups at 24 months (4.0% in the NCM plus HBPTM group and 4.0% in the HBPTM alone group).
Meaning
Findings support implementation of a NCM-enhanced HBPTM program for management of hypertension in low-income Black and Hispanic stroke survivors with uncontrolled hypertension.
Abstract
Importance
Black and Hispanic patients have high rates of recurrent stroke and uncontrolled hypertension in the US. The effectiveness of home blood pressure telemonitoring (HBPTM) and telephonic nurse case management (NCM) among low-income Black and Hispanic patients with stroke is unknown.
Objective
To determine whether NCM plus HBPTM results in greater systolic blood pressure (SBP) reduction at 12 months and lower rate of stroke recurrence at 24 months than HBPTM alone among Black and Hispanic stroke survivors with uncontrolled hypertension.
Design, Setting, and Participants
Practice-based, multicenter, randomized clinical trial in 8 stroke centers and ambulatory practices in New York City. Black and Hispanic study participants were enrolled between April 18, 2014, and December 19, 2017, with a final follow-up visit on December 31, 2019.
Interventions
Participants were randomly assigned to receive either HBPTM alone (12 home BP measurements/week for 12 months, with results transmitted to a clinician; n = 226) or NCM plus HBPTM (20 counseling calls over 12 months; n = 224).
Main Outcomes and Measures
Primary outcomes were change in SBP at 12 months and rate of recurrent stroke at 24 months. Final statistical analyses were completed March 14, 2024.
Results
Among 450 participants who were enrolled and randomized (mean [SD] age, 61.7 [11.0] years; 51% were Black [n = 231]; 44% were women [n = 200]; 31% had ≥3 comorbid conditions [n = 137]; 72% had household income <$25 000/y [n = 234/324]), 358 (80%) completed the trial. Those in the NCM plus HBPTM group had a significantly greater SBP reduction than those in the HBPTM alone group at 12 months (−15.1 mm Hg [95% CI, −17.2 to −13.0] vs −5.8 mm Hg [95% CI, −7.9 to −3.7], respectively; P < .001). The between-group difference in SBP reduction at 12 months, adjusted for primary care physician clustering, was −8.1 mm Hg (95% CI, −11.2 to −5.0; P < .001) at 12 months. The rate of recurrent stroke was similar between both groups at 24 months (4.0% in the NCM plus HBPTM group vs 4.0% in the HBPTM alone group, P > .99).
Conclusions and Relevance
Among predominantly low-income Black and Hispanic stroke survivors with uncontrolled hypertension, addition of NCM to HBPTM led to greater SBP reduction than HBPTM alone. Additional studies are needed to understand the long-term clinical outcomes, cost-effectiveness, and generalizability of NCM-enhanced telehealth programs among low-income Black and Hispanic stroke survivors with significant comorbidity.
Trial Registration
Clinical Trials.gov Identifier: NCT02011685
This clinical trial compares the effectiveness of nurse case management plus home blood pressure telemonitoring (HBPTM) vs HBPTM alone in achieving greater systolic blood pressure reduction at 12 months and lower rate of stroke recurrence at 24 months among Black and Hispanic stroke survivors with uncontrolled hypertension.
Introduction
Although significant reduction in stroke mortality has been achieved in the past decade,1 Black and Hispanic patients have worse outcomes and disproportionately higher rates of recurrent stroke than White patients.2 These disparities can be explained by high burden of secondary stroke risk factors in these populations,3,4 of which hypertension is the most important risk factor.5 For example, the impact of elevated systolic blood pressure (SBP) on stroke risk is 3 times greater for Black than for White populations.6 While BP control is imperative to decrease the risk of recurrent stroke,7 Black adults have poorer BP control than White adults.8 Reasons for the disparity in BP control are multifactorial and have been linked to a lack of treatment intensification, poor medication adherence, and access to care.9,10
Evidence-based approaches, such as self-measured BP monitoring, are associated with a reduction in BP and improved BP control.11 A 2018 Cochrane Review of secondary stroke prevention interventions showed that multilevel interventions that involved integrated multidisciplinary care, promotion of self-management behaviors, and regular patient monitoring were associated with the largest BP reductions.12 Two evidence-based interventions with these characteristics are home BP telemonitoring (HBPTM) with regular feedback to patients and their primary care physicians (PCPs)13 and telephonic nurse case management (NCM), which provides patient support to enhance self-management behaviors.14 Although the efficacy of HBPTM vs usual care has been demonstrated,15 its implementation and comparative effectiveness in low-income Black and Hispanic patients with high cardiovascular risk and significant comorbidity are unknown.
This clinical trial evaluated the comparative effectiveness of telephonic NCM plus HBPTM vs HBPTM alone on SBP reduction among Black and Hispanic stroke survivors with uncontrolled hypertension. It was hypothesized that patients randomized to the NCM plus HBPTM group would have a greater reduction in SBP than with HBPTM alone.
Methods
Trial Design and Oversight
This study was a practice-based, multicenter, 2-group, randomized clinical trial that was approved by the institutional review boards of NYU Grossman School of Medicine, the Biomedical Research Alliance of New York, and Columbia University Medical Center. All patients provided written informed consent, and trial data were monitored by an independent data and safety monitoring board. Details of the trial rationale, design, and methods have been described16 and are also available in the study protocol (Supplement 1). This study followed the Consolidated Standards of Reporting Trials guidelines (Figure 1).
Figure 1. Screening, Randomization, and Flow of Patients Through a Trial of Nurse Case Management and Home Blood Pressure Telemonitoring for Blood Pressure Control.
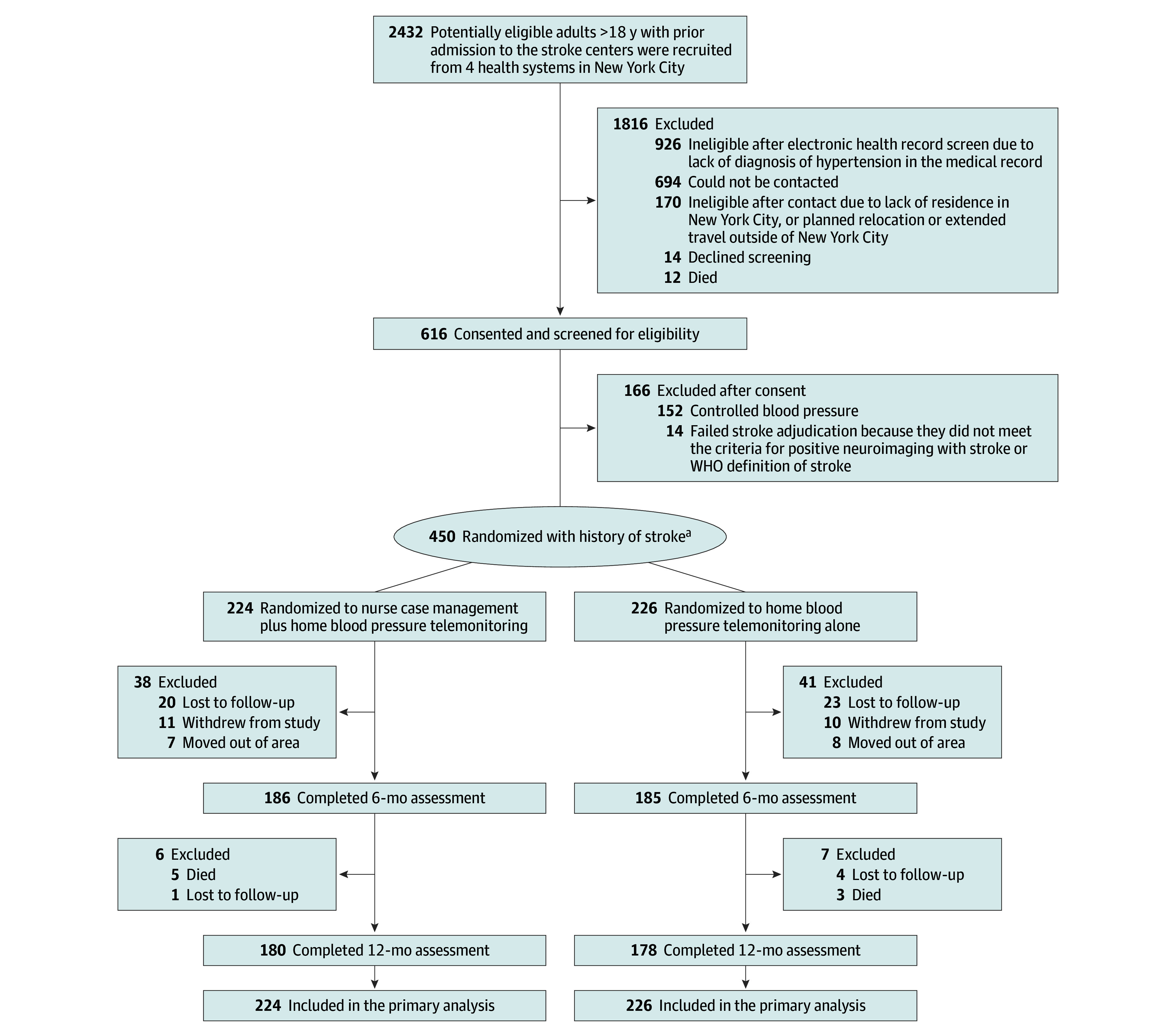
WHO indicates World Health Organization.
aRandomization occurred after completion of a baseline interview and was conducted using a SAS macro performed by the data coordinating center. Randomization was performed for individual patients within primary care physicians.
Trial Sites and Patient Population
The trial was conducted in 8 stroke centers and ambulatory care practices across 4 health systems (5 New York City Health and Hospital Corporation [HHC] hospitals and 3 academic medical centers [NYU Langone Health, SUNY Downstate Medical Center, and Columbia University Medical Center]). Patients were eligible if they were 18 years or older; self-identified as Black or Hispanic; fluent in English or Spanish; 1 month or more post discharge for stroke with moderate or less disability (modified Rankin Scale score ≤3); and had uncontrolled hypertension (SBP ≥130 mm Hg based on the mean of 3 readings taken at 1 screening visit). This study focused on Black and Hispanic patients because they have a higher rate of stroke burden and effectiveness of HBPTM combined with NCM has not been evaluated in this population. Patients with cognitive impairment, speech impairment, psychiatric comorbidity, end-stage kidney disease, or dialysis were excluded.16
Recruitment and Randomization
A multistep process using a combination of electronic health record review, patient self-report, and external stroke adjudication was used to identify potentially eligible patients, who were consented and randomly assigned in a 1:1 ratio to NCM plus HBPTM or HBPTM alone. Randomization occurred after completion of a baseline interview and was conducted using a SAS macro (SAS Institute) performed by the data coordinating center. Because rolling enrollment was required, an algorithm developed in SAS using random numbers and cut scores was used to ensure balance of the number of patients within PCPs. A random number from 0 to 1 was used to determine the assignment group. The standard cut score for the 2 groups was set at 0.5 for the first number of participants from the same PCP (eg, 6). Those who received a random number between 0 and 0.5 were assigned to the HBPTM group; those with a random number greater than 0.5 were assigned to the NCM plus HBPTM group. The balance between the groups within each group was carefully weighted after the total number of participants from a group reached a number greater than n. Randomization was performed for individual patients within PCPs by the data coordinating center. Given the nature of the intervention, the investigators, participants, and research assistants collecting evaluation data were not blinded; however, the PCPs in control of treatment in both of the treatment groups were blinded. Trained research assistants who knew the study hypothesis completed the in-office BP measurements. Participants were enrolled between April 18, 2014, and December 19, 2017, with a final follow-up visit on December 31, 2019.
Trial Interventions
Full details of the interventions are published elsewhere.16 Briefly, patients in both groups received automated home BP monitors (UA-767 Plus, A&D) with telemonitoring capability for wireless transmission of data to a secure server. Patients were instructed to take 12 BP readings per week (twice in the morning and evening, 3 days a week) for 12 months. The readings were transmitted to a web-based portal, and monthly reports were sent to patients and their PCPs. The monitors were preprogrammed with alert values (systolic BP <90 or >180 mm Hg, and diastolic BP <55 or >110 mm Hg), which activated an email and short message service (SMS) message to the research physician prompting a telephone call to the patient.
In addition, patients in the HBPTM alone group received printed National Institutes of Health material on stroke and management of hypertension, while those in the NCM plus HBPTM group received 20 telephone counseling calls from trained nurse case managers who were part of HHC’s telehealth program that provides personalized education and disease management for patients with chronic diseases. The telephone calls occurred weekly in months 0 to 2, biweekly in months 3 and 4, and monthly for months 5 to 12. During the calls, the nurse discussed information about BP, stroke symptoms, and lifestyle changes (eg, physical activity, weight loss, dietary changes, medication adherence) that could lower BP. The nurse also provided reinforcement of the HBPTM protocol and addressed the patient’s progress and challenges. Recommendations were made to PCPs by nurse case managers. Medication changes were left to the discretion of the PCPs.
Trial Measurements
In-office BP was measured at baseline, 6 months, and 12 months by research staff using a validated automated device (WatchBP Office, Microlife). Self-report measures included demographics; socioeconomic status; history of alcohol, nicotine, and drug use; health care utilization; Charlson Comorbidity Index score17; executive function18; depressive symptoms19; modified Rankin Scale score20; functional status21; health-related quality of life22; diet23; and physical activity.24
Trial Outcomes
The primary outcomes were (1) within-patient change in SBP from baseline to 12 months, defined as the mean of 3 BP readings taken by a trained research assistant using a validated automated BP monitor (WatchBP) and (2) rate of recurrent stroke at 24 months. The secondary outcomes were 12- and 24-month cost-effectiveness, which were collected as outlined in the study protocol (Supplement 1).
Post hoc outcomes included, first, BP control at 6 and 12 months (because national hypertension treatment guidelines changed during the study period, BP control was defined in 2 ways: at study inception using the 2014 Eighth Joint National Committee guidelines as BP <140/90 mm Hg25 and later by the 2017 American College of Cardiology/American Heart Association guidelines as BP <130/80 mm Hg26). Second, treatment intensification—defined as any of the following changes in antihypertensive medications: increased dose of at least 1 medication, change in the class of medication, addition of another class of medication, or initiation of a fixed-dose combination pill27—was also performed. Two variables were computed: the first measured treatment intensification from baseline to 6 months and from 6 to 12 months and the second carried intensification at 6 months forward to 12 months. Third, 2 measures of adherence were evaluated: (1) adherence with the NCM intervention (defined 3 ways: 100% adherence [completed all 20 calls], 75% adherence [completion of ≥15 calls], and 50% adherence [completion of ≥10 calls]) and (2) adherence with HBPTM (defined 2 ways using numbers of weeks of data available: strict adherence [>75% of available weeks having ≥12 readings with ≥3 readings per week] and moderate adherence [>75% of available weeks with ≥6 readings with ≥2 readings per week]). Fourth, post hoc outcomes of mortality as well as other vascular events, including heart attack and heart failure, were collected and examined.
Sample Size Calculation
Power for the primary outcome of within-patient change in SBP from baseline to 12 months28,29 was calculated as follows. Based on estimates from studies of telemedicine in Black and Hispanic patients, it was estimated that the baseline and longitudinal standard deviations of SBP at baseline would be between 18 and 22 mm Hg.30 The observed mean differences were from 3 to 8 mm Hg for SBP. We posited that the enhanced telemedicine intervention would result in an effect size ranging from a 6- to 8-point difference in SBP and powered the study for the primary outcome of continuous SBP at 80% with α level of .05 for a 2-tailed test to detect (depending on varying assumptions) a 6- to 8-mm Hg greater reduction in SBP in the NCM plus HBPTM group than the HBPTM alone group at 12 months. The power calculation incorporated clustering with an estimated cluster size of 5 patients per PCP, intracluster correlation (ICC) of 0.03, and variance inflation factor of 1 + (clustersize − 1) × ICC = 1.12. The observed cluster size for this study was 1.61 and the estimate for the ICC was 0.0004. The sample size was based on recruitment of 450 patients, of whom 350 were expected to complete the 12-month follow-up.31,32 Power for the primary outcome of rate of stroke at 24 months was examined using the sample size formula for the log-rank test. Assuming a variance inflation factor of 112%, α = .05, and a sample size of around 225 per group provided 80% power to detect a 10% group difference in reduction in the rate of stroke at 24 months.33,34
Statistical Analysis
Analysis of longitudinal data was performed on an intent-to-treat basis and adjusted for clustering of patients within PCP using SAS PROC Mixed. The statistical tests were based on trajectories (slopes) estimated from observed data points over 3 waves of data (baseline, 6 months, and 12 months). Significance tests were 2-tailed, with the α level prespecified as .05 for each primary outcome without adjustment for multiplicity. The outcomes in the models were treated as continuous variables and did not require prior transformation, based on graphical inspection of the distribution of the outcomes and of the residuals from the models. Adjusted means and standard errors of the outcomes at baseline and follow-up were estimated. The number of clusters was 279 PCPs with a mean cluster size of 1.6 per PCP (minimum = 1; maximum = 38; median = 1). Using the maximum likelihood method, the ICC for SBP was 0.0004. The best covariance structure was selected based on examination of the Akaike information criterion35 and the Schwarz bayesian information criterion.36 A compound symmetry covariance structure was observed to be superior and was thus used in all analyses.
In sensitivity analysis, a repeated-measures mixed analysis of variance approach, adjusting for clustering within PCP, was used to examine the within-group and between-group effects. Prior to analyses, baseline values of all potential confounder/predictor variables were examined to determine whether any covariates required modeling due to imbalance among groups. Examination of baseline differences on key variables between completers and those lost to follow-up showed that modeling missing data was not required. The full information maximum-likelihood approach was used to estimate treatment effects.
Longitudinal BP and stroke analyses of patients were performed according to their randomization groups and adjusted for clustering patients within PCP using SAS Proc Mixed and Glimmix, assuming a compound symmetry covariance structure. For the 24-month recurrent stroke analyses, Kaplan-Meier curves were constructed and compared between groups with the log-rank statistic. Overall and longitudinal treatment intensification were examined. BP control and treatment intensification were post hoc analyses performed as exploratory or hypothesis generating. All analyses were performed using SAS version 9.4 software (SAS Institute).
Results
Trial Participants
Of 2432 potentially eligible patients, a total of 450 patients were enrolled and randomized. There were 445 participants enrolled prior to the 2017 American College of Cardiology/American Heart Association guidelines and 5 enrolled after the guidelines (Figure 1). The groups were balanced across baseline characteristics (Table 1). BP data for all 3 waves (baseline, 6-month, and 12-month time points) were available for 354 participants (78.7%), and at least 2 waves were available for 379 (84.2%). The retention rate was 79.6% for both groups (Figure 1).
Table 1. Baseline Characteristics of a Trial of Nurse Case Management and Home Blood Pressure Telemonitoring for Blood Pressure Control.
| Variable | No. (%) | |
|---|---|---|
| Home blood pressure telemonitoring plus nurse case management (n = 224) | Home blood pressure telemonitoring alone (n = 226) | |
| Demographics | ||
| Age, mean (SD), y | 62.3 (11.5) | 61.1 (10.5) |
| Sex | ||
| Male | 119 (53.1) | 131 (58.0) |
| Female | 105 (46.9) | 95 (42.0) |
| Race and ethnicitya | ||
| Black, non-Hispanic | 125 (55.8) | 106 (46.9) |
| Hispanic | 99 (44.2) | 120 (53.1) |
| Married/domestic partnership | 95 (42.4) | 94 (41.8) |
| Less than a high school education (did not graduate high school) | 91 (43.1) | 118 (54.6) |
| Employed (part-time/full-time/self-employed) | 36 (16.1) | 44 (20.0) |
| Annual household income <$25 000b | 115 (71.9) | 119 (72.6) |
| Medical history | ||
| Stroke type, ischemic | 170 (75.9) | 174 (77.0) |
| Time from stroke to study screening, median (IQR), mo | 3.3 (1.7-9.4) | 3.3 (1.9-9.9) |
| Modified Rankin Scale score (0-6; higher score indicates greater disability), mean (SD) | 1.7 (1.0) | 1.7 (1.1) |
| Charlson Comorbidity Indexc | ||
| No comorbidity | 54 (24.3) | 35 (15.6) |
| 1-2 Comorbid conditions | 108 (48.6) | 112 (50.0) |
| ≥3 Comorbid conditions | 60 (27.0) | 77 (34.3) |
| Obese (BMI ≥30) | 101 (46.5) | 97 (45.1) |
| History of diabetes | 104 (46.4) | 112 (49.6) |
| Currently smokes | 38 (17.4) | 25 (11.5) |
| Currently drinks alcohol | 62 (28.7) | 67 (30.5) |
| Laboratory findings | ||
| Blood pressure, mean (SD), mm Hg | ||
| Systolic | 150.0 (15.2) | 148.0 (14.4) |
| Diastolic | 87.7 (12.3) | 87.9 (12.7) |
Abbreviation: BMI, body mass index (calculated as weight in kilograms divided by height in meters squared).
Race and ethnicity information was self-reported by the participant during the eligibility screen. Answers other than Black or Hispanic were exclusion criteria.
Annual household income was dichotomized at $25 000 using the Federal Poverty Level for a family of 4 from the year 2018. Due to missing data, the number of patients with this information was 324.
The Charslon Comorbidity Index assigns weights to specific medical conditions, with a higher score indicating greater comorbidity severity. Presented is the categorization by quartiles.
Primary Outcomes
Systolic Blood Pressure Reduction
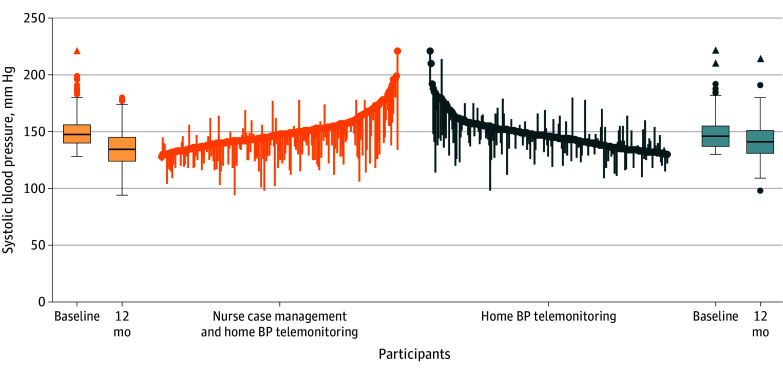
Both groups experienced a significant decline in model-based SBP from baseline to 12 months (P < .001), with the NCM plus HBPTM group experiencing a significantly greater decline than the HBPTM alone group (P < .001, treatment group by visit interaction term; Table 2; Figure 2; eFigure 1 in Supplement 2). At 12 months, SBP reduction was 15.1 mm Hg in the NCM plus HBPTM group (148.3 mm Hg to 133.2 mm Hg) vs 5.8 mm Hg in the HBPTM alone group (147.1 mm Hg to 141.3 mm Hg; Table 2). The between-group difference in SBP reduction was −8.1 mm Hg (95% CI, −11.2 to −5.0) at 12 months (P < .001; Table 2). Sensitivity analyses with 2 methods for modeling missing data and a different analytic model showed similar results, and model-based means were close in value to the observed means (eTables 4 and 7 and eFigure 2 in Supplement 2). In post hoc analyses, the 6-month between-group difference in SBP reduction was −3.4 mm Hg (95% CI, −5.8 to −1.1; P = .002).
Table 2. Longitudinal Descriptive Statistics by Treatment Group and Model Results for Systolic Blood Pressure (SBP).
| Outcome | Home blood pressure telemonitoring plus nurse case management (n = 224) | Home blood pressure telemonitoring (n = 226) | Absolute difference in difference (95% CI) | P value | ||||
|---|---|---|---|---|---|---|---|---|
| Baseline | Final | Difference (95% CI) | Baseline | Final | Difference (95% CI) | |||
| Primary outcomes | ||||||||
| SBP at 12 mo (95% CI), mm Hga | 148.3 (146.3 to 150.3) [n = 224] | 133.2 (131.0 to 135.4) [n = 180] | −15.1 (−17.2 to −13.0) | 147.1 (145.1 to 149.1) [n = 226] | 141.3 (139.1 to 143.5) [n = 178] | −5.8 (−7.9 to −3.7) | −8.1 (−11.2 to −5.0) | <.001 |
| Recurrent stroke at 24 mo, No. (%)b | 0 | 9 (4.0) | 0 | 9 (4.0) | >.99 | |||
| Post hoc outcome | ||||||||
| SBP at 6 mo (post hoc) | 148.3 (146.3 to 150.3) [n = 224] | 140.7 (139.1 to 143.4) [n = 186] | −7.6 (−9.4 to −5.8) | 147.1 (145.1 to 149.1) [n = 226] | 144.2 (142.5 to 145.9) [n = 185] | −2.9 (−4.7 to −1.1) | −3.4 (−5.8 to −1.1) | .002 |
Sample size and model-adjusted means and 95% CIs are reported for the SBP outcome. A repeated-measures linear mixed model, adjusting for clustering within primary care physician and assuming a compound symmetry covariance structure, was used for the SBP analysis.
Sample size and percentages are reported for the recurrent stroke at 24 months outcome. Fisher exact P value reported for comparison of recurrent stroke at 24 months between treatment groups.
Figure 2. Changes in Systolic Blood Pressure (BP) Between Baseline and 12-Month Follow-Up by Treatment Group.
The parallel line plot contains 1 vertical line for each participant with the circle representing baseline values and the line indicating increase or decrease in blood pressure. The boxes indicate median (crossbar) and first and third quartiles (box ends) with whiskers representing the furthest point 1.5 IQR distance from first and third quartiles. Lower whiskers represent minimum value if within the 1.5 IQR distance from the first quartile. Dots indicate values greater than 1.5 IQR distance from the first and third quartiles. Triangles indicate values greater than 3 IQR distance from the first and third quartiles.
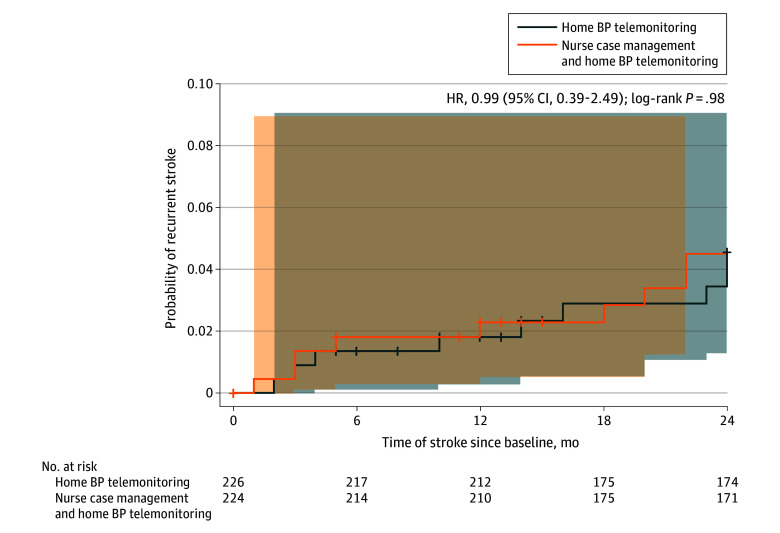
Recurrent Stroke
The frequency of recurrent strokes is shown in eTable 1 in Supplement 2. There were few differences between stroke and nonstroke groups, given the small number of recurrent strokes (eTable 1 in Supplement 2). Overall, 18 individuals experienced a recurrent stroke over 24 months (9 in the NCM plus HBPTM group and 9 in the HBPTM alone group, P > .99; eTable 2 in Supplement 2). Overall, two-thirds of the recurrent strokes were ischemic. The Kaplan-Meier survival curve is shown in Figure 3. Other vascular events measures were examined in post hoc analyses and are shown in eTable 3 in Supplement 2.
Figure 3. Survival Probability of the Primary Efficacy Outcome of Recurrent Stroke, Stratified by Treatment Group.
Recurrent stroke included stroke of ischemic and hemorrhagic nature. The mean (SD) follow-up period for both groups was 10.9 (5.3) months for the nurse case management plus home blood pressure (BP) telemonitoring group and 11.2 (6.1) months for the home blood pressure monitoring alone group. The shaded areas represent 95% Hall-Wellner confidence bands.
Post Hoc Outcomes
Blood Pressure Control
BP control improved over time, whether defined as BP less than 130/80 mm Hg (P < .001) or BP less than 140/90 mm Hg (P = .002), with the NCM plus HBPTM group achieving greater BP control than the HBPTM alone group (eTable 8 and eFigures 3 and 4 in Supplement 2). Using BP less than 130/80 mm Hg, the proportion of patients with BP control increased from 2.7% at baseline to 36.9% at 12 months in the NCM plus HBPTM group vs 2.0% at baseline to 16.9% at 12 months in the HBPTM alone group (P = .05). Using BP less than 140/90 mm Hg, the proportion of patients with BP control increased from 24.0% at baseline to 62.3% at 12 months in the NCM plus HBPTM group vs 27.8% at baseline to 41.3% at 12 months in the HBPTM alone group (P < .001). Sensitivity analyses with 2 methods for modeling missing data and a different analytic model showed similar results, and model-based proportions were close in value to the observed proportions (eTables 5 and 6 in Supplement 2).
Vascular Events and Deaths
Post hoc analyses of comorbidity and mortality were performed. Patients in the NCM plus HBPTM group had fewer comorbid conditions at 12 months compared with the HBPTM alone group (P = .007; eTable 3 in Supplement 2). Eight deaths occurred during the trial (3 in the HBPTM alone group and 5 in the NCM plus HBPTM group). The causes of these deaths included strokes (n = 4), myocardial infarction (n = 3), and 1 case where the cause was unknown. Because only 8 deaths occurred during the trial, between-group analysis were not performed.
Treatment Intensification
From baseline to 6 months, 41.4% of the NCM plus HBPTM group had treatment intensification vs 26.2% of the HBPTM alone group (P = .009). From 6 to 12 months, 25.8% of the NCM plus HBPTM group had treatment intensification vs 21.7% of the HBPTM alone group (P = .45; eTable 9 in Supplement 2). When treatment intensification at 6 months was carried forward to 12 months, the rate was higher in the NCM plus HBPTM group vs the HBPTM alone group (53.9% vs 40.0%, respectively, P = .03; eTable 9 in Supplement 2). The between-group difference in treatment intensification was significant in both the visit-to-visit analysis (P = .02) and the carry-forward analysis (P = .01). There was no significant difference between treatment groups over time for the visit-to-visit analysis.
Nurse Case Manager Call Adherence
There were 15 nurse case managers active in the trial and patients could have had multiple nurse case managers. Only patients in the intervention group (NCM plus HBPTM group) received calls from the nurse case managers, and individual nurse case managers were not linked to specific patients. Participants completed a mean (SD) of 5.5 (2.7) of 8 weekly calls (68.4%), 2.5 (1.6) of 4 biweekly calls (62.8%), and 4.5 (3.0) of 8 monthly calls (55.9%). Of 20 maximum calls, participants completed a mean (SD) of 12.5 (6.5) calls (62.3%). Only 6.3% of participants completed all 20 calls, 51.8% completed 15 calls or more (75% adherence), and 74.1% completed 10 calls or more (50% adherence) (eTable 10 in Supplement 2). None of the patient characteristics examined were significantly associated with 50% or 75% call adherence (eTable 11 in Supplement 2).
HBPTM Adherence
The NCM plus HBPTM group provided significantly more weeks of BP readings than the HBPTM alone group (mean, 46.3 vs 35.6; P < .001). The NCM plus HBPTM group also achieved strict adherence on significantly more weeks than the HBPTM alone group (mean, 9.7 vs 6.7; P = .04) and a greater percentage of weeks with strict adherence than the HBPTM alone group (19.4% vs 15.4%, P = .16). Only 7.9% of the NCM plus HBPTM group achieved strict adherence vs 4.7% of the HBPTM alone group (P = .22) (eTable 12 in Supplement 2). When adjusted for clustering within PCP, the NCM plus HBPTM group achieved strict adherence at a significantly higher rate than the HBPTM alone group (P = .01; eTable 13 in Supplement 2). A similar pattern was observed for moderate adherence (eTables 12 and 13 in Supplement 2).
Costs
Regarding costs, the per-participant rate including BP telemonitoring equipment was $938.77 for the HBPTM alone group and $1594.03 for the NCM plus HBPTM group. The per-participant cost for the NCM plus HBPTM group included services by a bilingual nurse employed by HHC. Equipment costs included rental fees for the BP device and modem, equipment installation, monthly service fee for the secure web-based portal access, insurance coverage, and deductible expense for loss of 90 devices.
Discussion
In this practice-based, multicenter, randomized clinical trial among low-income Black and Hispanic patients with stroke and uncontrolled hypertension, a NCM-enhanced telehealth program that combines use of HBPTM with telephonic NCM led to an 8.1–mm Hg greater SBP reduction and higher BP control rate than HBPTM alone at 12 months. There was no difference in the rate of recurrent stroke between both groups, likely due to the small number of recurrent strokes observed over a 24-month period (n = 18).
To our knowledge, this is the first large study to evaluate the comparative effectiveness of HBPTM with or without NCM for management of hypertension in Black and Hispanic patients with stroke across several hospital systems. It should be noted there are 4 relevant studies that evaluated hypertension control in patients with stroke. First was a UK study that evaluated the efficacy of self-monitoring of home BP plus medication self-titration vs usual care among 552 patients with high cardiovascular risk, including stroke, in 59 primary care practices. The intervention group had significantly greater SBP reduction (approximately 9 mm Hg) than the usual care group.37 Unlike the current study, this study did not evaluate the role of HBPTM. Second was the Telehealth After Stroke Care study, a small pilot study that compared the effect of a multicomponent intervention (HBPTM, NCM, and telehealth video visits with a nurse practitioner, pharmacist, and physician) vs usual care among 50 patients (83% Black or Hispanic) with stroke. Patients in the intervention group had a greater SBP reduction (mean [SD], 18.4 [22] mm Hg) than usual care.38 Unlike the current study, duration was only 3 months, and the intervention was complex with a small sample size. The third study, which was a negative trial, Discharge Educational Strategies for Reduction of Vascular Events (DESERVE), evaluated the efficacy of a culturally tailored skills-based educational intervention delivered by a community health coordinator, vs standard discharge care, on SBP reduction among 552 patients (66% Black or Hispanic) with stroke or transient ischemic attack.39 Fourth, the Secondary Stroke Prevention by Uniting Community and Chronic Care Model Teams Early to End Disparities (SUCCEED) clinical trial, which was also a negative trial, evaluated the effect of a multifaceted team intervention vs usual care on SBP reduction among 487 patients (90% Black or Hispanic) with stroke or transient ischemic attack in safety-net settings.40 Intervention components included at least 3 clinic visits with nurse practitioners, 3 community health worker home visits, and chronic disease self-management program workshops along with patient education. Although the patient population in the SUCCEED and DESERVE studies included Black and Hispanic patients, both programs were complex, did not evaluate HBPTM, and had low patient engagement.
The reasons for the findings of the current study likely include increased patient activation resulting from NCM and treatment intensification via increased titration of antihypertensive medications37,41 and reduced clinical inertia.42 Patients in the NCM plus HBPTM group were more adherent with the home BP monitoring protocol, demonstrating the positive impact of NCM support on self-management. Through feedback to the PCP, the telehealth program also resulted in a more responsive health care team as shown by greater treatment intensification in the NCM plus HBPTM group. Although the relative benefit of NCM plus HBPTM compared with HBPTM alone is clear, it should be noted that a significant proportion of patients in the NCM plus HBPTM group still had inadequate BP control by either standard (37.7% for 140/90 mm Hg and 63.1% for 130/80 mm Hg). Therefore, more still needs to be done in addition to the use of NCM in this patient population.
The rate of stroke recurrence in the current study was 4% at 24 months. This was much lower than the recurrent stroke rates reported for Black and Hispanic participants in other observational and interventional studies.43,44 A recent population-based study of 3816 stroke survivors in the Greater Cincinnati/Kentucky Stroke Study conducted by Robinson et al45 reported a stroke recurrence rate of 12.6% and 9% among Black vs White patients at 2 years, respectively. This was 2 to 3 times higher than that reported in the current study. In other longitudinal stroke prevention studies, Black and Hispanic patients were reported to have a yearly hemorrhagic stroke recurrence rate between 3.5% and 3.9%,2 and a population-based study of older medical beneficiaries reported the yearly rate of recurrent ischemic stroke of 9.4% across the US.46 Any comparison between the rates of recurrent stroke between the current study and other stroke prevention trials should be interpreted with caution due to the relatively small number of events in this study, methodological differences between the studies (population-based studies vs stroke prevention trials), and composition of the patient demographics.
The major strengths of this study included the pragmatic comparative effectiveness design, multicenter nature, utilization of an established telehealth program that uses telephonic NCM, and focus on low-income Black and Hispanic patients with significant comorbidity. The public health significance of this study in the era of the COVID-19 pandemic cannot be overstated, particularly given the disparate outcomes in Black and Hispanic patients.47 While the pandemic has laid bare structural inequities that underlie racial disparities in outcomes, comorbidities such as hypertension and stroke were implicated as attributable risk factors to explain some of the disparities in COVID-19–related deaths.48,49 In response to the pandemic, telehealth has not only assumed an expanded role in addressing structural inequities in care (via increased access to care for low-income Black and Hispanic patients), it has also mitigated the disruptions in care of patients at high risk for factors that cause cardiovascular disease such as hypertension. Findings from this study support use of remote patient monitoring and telephonic nurse management in low-income Black and Hispanic patients with stroke and significant comorbidity.
Limitations
This study had several limitations. First, the use of clinic measurements at baseline may have potentially excluded patients with blinded uncontrolled hypertension, a group at high risk for cardiovascular disease. Second, this was an unblinded study for investigators, participants, and research assistants collecting evaluation data. Additionally, it is possible that there may have been some unblinding of the PCPs who controlled medication treatment because the nurse case managers could send messages to the PCPs, effectively unblinding them. Third, although a stroke adjudication worksheet was used, a standardized instrument to screen for recurrent stroke events was not used; as such, this could have led to both general underdetection of stroke events and biased ascertainment of events favoring the active treatment group. Additional limitations included that this study was conducted in only 1 city and the large number of potentially eligible patients who did not participate, as shown in Figure 1, raising questions about generalizability.
Conclusions
Among Black and Hispanic patients with stroke and uncontrolled hypertension, the addition of NCM to HBPTM led to relatively greater SBP reduction than HBPTM alone. There was no difference in the rate of recurrent stroke between both groups, likely due to the small number of recurrent strokes observed over a 24-month period. Additional studies are needed to understand the long-term clinical outcomes, cost-effectiveness, and generalizability of NCM-enhanced telehealth programs and its dissemination as standard practice for management of hypertension in low-income Black and Hispanic stroke survivors with significant comorbidity.
Trial Protocol
eTable 1. Baseline Characteristics by Recurrent Stroke Since Baseline Status
eTable 2. Twenty-Four Month Recurrent Strokes (Adjudicated From Medical Records)
eTable 3. Twelve-Month Data for Self-Reported Heart Attack and Congestive Heart Failure by Treatment Group
eTable 4. Sensitivity Analysis Modeling Missingness for Systolic Blood Pressure
eTable 5. Sensitivity Analysis Modeling Missing Data for Achieved Blood Pressure Control at 130/80
eTable 6. Sensitivity Analysis Modeling Missing Data for Achieved Blood Pressure Control at 140/90
eTable 7. Sensitivity Analysis: Results of Repeated Measures ANOVA Mixed Models, Adjusting for Clustering Within PCP
eTable 8. Achievement of Blood Pressure Control
eTable 9. Treatment Intensification Over Time by Treatment Group
eTable 10. Observed Means (Standard Deviations) for Number of Nurse Case Management calls Completed and Proportion Adherent
eTable 11. Nurse Case Manager Call Adherence Outcome (Home BP Telemonitoring and Nurse Case Management Group Only) Modeled Using a Glimmix Model, Assuming a Logit Link, Adjusted for Clustering With PCP
eTable 12. Descriptive Statistics for Home Blood Pressure Telemonitoring Adherence Information
eTable 13. Home Blood Pressure Telemonitoring Adherence Outcome Using a Glimmix Model, Assuming a Logit Link Adjusted for Clustering within PCP
eFigure 1. Model Based Means for Systolic Blood Pressure by Treatment Group Over Time
eFigure 2. Model Based Means for SBP. Plot of Predicted Outcomes Based on ANOVA Mixed Models, Adjusting for Clustering within PCP
eFigure 3. Model-based Proportions for Achievement of Blood Pressure Less Than 130/80
eFigure 4. Model-based Proportions for Achievement of Blood Pressure Less Than 140/90
Data Sharing Statement
References
- 1.Lackland DT, Roccella EJ, Deutsch AF, et al. ; American Heart Association Stroke Council; Council on Cardiovascular and Stroke Nursing; Council on Quality of Care and Outcomes Research; Council on Functional Genomics and Translational Biology . Factors influencing the decline in stroke mortality: a statement from the American Heart Association/American Stroke Association. Stroke. 2014;45(1):315-353. doi: 10.1161/01.str.0000437068.30550.cf [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rodriguez-Torres A, Murphy M, Kourkoulis C, et al. Hypertension and intracerebral hemorrhage recurrence among White, Black, and Hispanic individuals. Neurology. 2018;91(1):e37-e44. doi: 10.1212/WNL.0000000000005729 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bravata DM, Wells CK, Gulanski B, et al. Racial disparities in stroke risk factors: the impact of socioeconomic status. Stroke. 2005;36(7):1507-1511. doi: 10.1161/01.STR.0000170991.63594.b6 [DOI] [PubMed] [Google Scholar]
- 4.McGruder HF, Malarcher AM, Antoine TL, Greenlund KJ, Croft JB. Racial and ethnic disparities in cardiovascular risk factors among stroke survivors: United States 1999 to 2001. Stroke. 2004;35(7):1557-1561. doi: 10.1161/01.STR.0000130427.84114.50 [DOI] [PubMed] [Google Scholar]
- 5.O’Donnell MJ, Chin SL, Rangarajan S, et al. ; INTERSTROKE investigators . Global and regional effects of potentially modifiable risk factors associated with acute stroke in 32 countries (INTERSTROKE): a case-control study. Lancet. 2016;388(10046):761-775. doi: 10.1016/S0140-6736(16)30506-2 [DOI] [PubMed] [Google Scholar]
- 6.Howard G, Lackland DT, Kleindorfer DO, et al. Racial differences in the impact of elevated systolic blood pressure on stroke risk. JAMA Intern Med. 2013;173(1):46-51. doi: 10.1001/2013.jamainternmed.857 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Benavente OR, Hart RG, McClure LA, Szychowski JM, Coffey CS, Pearce LA; SPS3 Investigators . Effects of clopidogrel added to aspirin in patients with recent lacunar stroke. N Engl J Med. 2012;367(9):817-825. doi: 10.1056/NEJMoa1204133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Akinyelure OP, Jaeger BC, Moore TL, et al. Racial differences in blood pressure control following stroke: the REGARDS Study. Stroke. 2021;52(12):3944-3952. doi: 10.1161/STROKEAHA.120.033108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Berlowitz DR, Ash AS, Hickey EC, et al. Inadequate management of blood pressure in a hypertensive population. N Engl J Med. 1998;339(27):1957-1963. doi: 10.1056/NEJM199812313392701 [DOI] [PubMed] [Google Scholar]
- 10.Burnier M, Egan BM. Adherence in hypertension. Circ Res. 2019;124(7):1124-1140. doi: 10.1161/CIRCRESAHA.118.313220 [DOI] [PubMed] [Google Scholar]
- 11.Shimbo D, Artinian NT, Basile JN, et al. ; American Heart Association and the American Medical Association . Self-measured blood pressure monitoring at home: a joint policy statement from the American Heart Association and American Medical Association. Circulation. 2020;142(4):e42-e63. doi: 10.1161/CIR.0000000000000803 [DOI] [PubMed] [Google Scholar]
- 12.Bridgwood B, Lager KE, Mistri AK, Khunti K, Wilson AD, Modi P. Interventions for improving modifiable risk factor control in the secondary prevention of stroke. Cochrane Database Syst Rev. 2018;5(5):CD009103. doi: 10.1161/STROKEAHA.118.022213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Agarwal R, Bills JE, Hecht TJ, Light RP. Role of home blood pressure monitoring in overcoming therapeutic inertia and improving hypertension control: a systematic review and meta-analysis. Hypertension. 2011;57(1):29-38. doi: 10.1161/HYPERTENSIONAHA.110.160911 [DOI] [PubMed] [Google Scholar]
- 14.Bosworth HB, Olsen MK, Gentry P, et al. Nurse administered telephone intervention for blood pressure control: a patient-tailored multifactorial intervention. Patient Educ Couns. 2005;57(1):5-14. doi: 10.1016/j.pec.2004.03.011 [DOI] [PubMed] [Google Scholar]
- 15.Duan Y, Xie Z, Dong F, et al. Effectiveness of home blood pressure telemonitoring: a systematic review and meta-analysis of randomised controlled studies. J Hum Hypertens. 2017;31(7):427-437. doi: 10.1038/jhh.2016.99 [DOI] [PubMed] [Google Scholar]
- 16.Spruill TM, Williams O, Teresi JA, et al. Comparative effectiveness of home blood pressure telemonitoring (HBPTM) plus nurse case management versus HBPTM alone among Black and Hispanic stroke survivors: study protocol for a randomized controlled trial. Trials. 2015;16:97-97. doi: 10.1186/s13063-015-0605-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373-383. doi: 10.1016/0021-9681(87)90171-8 [DOI] [PubMed] [Google Scholar]
- 18.Dubois B, Slachevsky A, Litvan I, Pillon B. The FAB: a Frontal Assessment Battery at bedside. Neurology. 2000;55(11):1621-1626. doi: 10.1212/WNL.55.11.1621 [DOI] [PubMed] [Google Scholar]
- 19.Pilkonis PA, Choi SW, Reise SP, Stover AM, Riley WT, Cella D; PROMIS Cooperative Group . Item banks for measuring emotional distress from the Patient-Reported Outcomes Measurement Information System (PROMIS): depression, anxiety, and anger. Assessment. 2011;18(3):263-283. doi: 10.1177/1073191111411667 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wilson JT, Hareendran A, Grant M, et al. Improving the assessment of outcomes in stroke: use of a structured interview to assign grades on the modified Rankin Scale. Stroke. 2002;33(9):2243-2246. doi: 10.1161/01.STR.0000027437.22450.BD [DOI] [PubMed] [Google Scholar]
- 21.Mahoney FI, Wood OH, Barthel DW. Rehabilitation of chronically ill patients: the influence of complications on the final goal. South Med J. 1958;51(5):605-609. doi: 10.1097/00007611-195805000-00011 [DOI] [PubMed] [Google Scholar]
- 22.EuroQol Group . EuroQol: a new facility for the measurement of health-related quality of life. Health Policy. 1990;16(3):199-208. doi: 10.1016/0168-8510(90)90421-9 [DOI] [PubMed] [Google Scholar]
- 23.Thompson FE, Midthune D, Subar AF, Kipnis V, Kahle LL, Schatzkin A. Development and evaluation of a short instrument to estimate usual dietary intake of percentage energy from fat. J Am Diet Assoc. 2007;107(5):760-767. doi: 10.1016/j.jada.2007.02.006 [DOI] [PubMed] [Google Scholar]
- 24.Craig CL, Marshall AL, Sjöström M, et al. International Physical Activity Questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003;35(8):1381-1395. doi: 10.1249/01.MSS.0000078924.61453.FB [DOI] [PubMed] [Google Scholar]
- 25.James PA, Oparil S, Carter BL, et al. 2014 Evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014;311(5):507-520. doi: 10.1001/jama.2013.284427 [DOI] [PubMed] [Google Scholar]
- 26.Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/pcna guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2018;71(19):e127-e248. doi: 10.1016/j.jacc.2017.11.006 [DOI] [PubMed] [Google Scholar]
- 27.Ogedegbe G, Tobin JN, Fernandez S, et al. Counseling African Americans to control hypertension: cluster-randomized clinical trial main effects. Circulation. 2014;129(20):2044-2051. doi: 10.1161/CIRCULATIONAHA.113.006650 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Diggle P, Liang KY, Zeger S. Analysis of Longitudinal Data. Oxford University Press; 1994. [Google Scholar]
- 29.Liu G, Liang KY. Sample size calculations for studies with correlated observations. Biometrics. 1997;53(3):937-947. doi: 10.2307/2533554 [DOI] [PubMed] [Google Scholar]
- 30.Shea S, Weinstock RS, Teresi JA, et al. ; IDEATel Consortium . A randomized trial comparing telemedicine case management with usual care in older, ethnically diverse, medically underserved patients with diabetes mellitus: 5 year results of the IDEATel study. J Am Med Inform Assoc. 2009;16(4):446-456. doi: 10.1197/jamia.M3157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chimowitz MI, Lynn MJ, Derdeyn CP, et al. ; SAMMPRIS Trial Investigators . Stenting versus aggressive medical therapy for intracranial arterial stenosis. N Engl J Med. 2011;365(11):993-1003. doi: 10.1056/NEJMoa1105335 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chimowitz MI, Lynn MJ, Howlett-Smith H, et al. ; Warfarin-Aspirin Symptomatic Intracranial Disease Trial Investigators . Comparison of warfarin and aspirin for symptomatic intracranial arterial stenosis. N Engl J Med. 2005;352(13):1305-1316. doi: 10.1056/NEJMoa043033 [DOI] [PubMed] [Google Scholar]
- 33.Hsieh FY, Lavori PW. Sample-size calculations for the Cox proportional hazards regression model with nonbinary covariates. Control Clin Trials. 2000;21(6):552-560. doi: 10.1016/S0197-2456(00)00104-5 [DOI] [PubMed] [Google Scholar]
- 34.Barthel FM, Babiker A, Royston P, Parmar MK. Evaluation of sample size and power for multi-arm survival trials allowing for non-uniform accrual, non-proportional hazards, loss to follow-up and cross-over. Stat Med. 2006;25(15):2521-2542. doi: 10.1002/sim.2517 [DOI] [PubMed] [Google Scholar]
- 35.Ripplinger J, Sullivan J. Does choice in model selection affect maximum likelihood analysis? Syst Biol. 2008;57(1):76-85. doi: 10.1080/10635150801898920 [DOI] [PubMed] [Google Scholar]
- 36.Schwarz G. Estimating the dimension of a model. Ann Stat. 1978;6(2):461-464. doi: 10.1214/aos/1176344136 [DOI] [Google Scholar]
- 37.McManus RJ, Mant J, Haque MS, et al. Effect of self-monitoring and medication self-titration on systolic blood pressure in hypertensive patients at high risk of cardiovascular disease: the TASMIN-SR randomized clinical trial. JAMA. 2014;312(8):799-808. doi: 10.1001/jama.2014.10057 [DOI] [PubMed] [Google Scholar]
- 38.Naqvi IA, Strobino K, Kuen Cheung Y, et al. Telehealth after stroke care pilot randomized trial of home blood pressure telemonitoring in an underserved setting. Stroke. 2022;53(12):3538-3547. doi: 10.1161/STROKEAHA.122.041020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Boden-Albala B, Goldmann E, Parikh NS, et al. Efficacy of a discharge educational strategy vs standard discharge care on reduction of vascular risk in patients with stroke and transient ischemic attack: the DESERVE randomized clinical trial. JAMA Neurol. 2019;76(1):20-27. doi: 10.1001/jamaneurol.2018.2926 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Towfighi A, Cheng EM, Ayala-Rivera M, et al. ; Secondary Stroke Prevention by Uniting Community and Chronic Care Model Teams Early to End Disparities (SUCCEED) Investigators . Effect of a coordinated community and chronic care model team intervention vs usual care on systolic blood pressure in patients with stroke or transient ischemic attack: the SUCCEED randomized clinical trial. JAMA Netw Open. 2021;4(2):e2036227. doi: 10.1001/jamanetworkopen.2020.36227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.McManus RJ, Mant J, Bray EP, et al. Telemonitoring and self-management in the control of hypertension (TASMINH2): a randomised controlled trial. Lancet. 2010;376(9736):163-172. doi: 10.1016/S0140-6736(10)60964-6 [DOI] [PubMed] [Google Scholar]
- 42.Crowley MJ, Smith VA, Olsen MK, et al. Treatment intensification in a hypertension telemanagement trial: clinical inertia or good clinical judgment? Hypertension. 2011;58(4):552-558. doi: 10.1161/HYPERTENSIONAHA.111.174367 [DOI] [PubMed] [Google Scholar]
- 43.Sacco RL, Diener HC, Yusuf S, et al. ; PRoFESS Study Group . Aspirin and extended-release dipyridamole versus clopidogrel for recurrent stroke. N Engl J Med. 2008;359(12):1238-1251. doi: 10.1056/NEJMoa0805002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Howard G, Kissela BM, Kleindorfer DO, et al. Differences in the role of Black race and stroke risk factors for first vs recurrent stroke. Neurology. 2016;86(7):637-642. doi: 10.1212/WNL.0000000000002376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Robinson DJ, Stanton R, Sucharew H, et al. Racial disparities in stroke recurrence: a population-based study. Neurology. 2022;99(22):e2464-e2473. doi: 10.1212/WNL.0000000000201225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Allen NB, Holford TR, Bracken MB, et al. Geographic variation in one-year recurrent ischemic stroke rates for elderly Medicare beneficiaries in the USA. Neuroepidemiology. 2010;34(2):123-129. doi: 10.1159/000274804 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Adhikari S, Pantaleo NP, Feldman JM, Ogedegbe O, Thorpe L, Troxel AB. Assessment of community-level disparities in coronavirus disease 2019 (COVID-19) infections and deaths in large US metropolitan areas. JAMA Netw Open. 2020;3(7):e2016938-e2016938. doi: 10.1001/jamanetworkopen.2020.16938 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Yancy CW. COVID-19 and African Americans. JAMA. 2020;323(19):1891-1892. doi: 10.1001/jama.2020.6548 [DOI] [PubMed] [Google Scholar]
- 49.Doumas M, Patoulias D, Katsimardou A, Stavropoulos K, Imprialos K, Karagiannis A. COVID-19 and increased mortality in African Americans: socioeconomic differences or does the renin angiotensin system also contribute? J Hum Hypertens. 2020;34(11):764-767. doi: 10.1038/s41371-020-0380-y [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Trial Protocol
eTable 1. Baseline Characteristics by Recurrent Stroke Since Baseline Status
eTable 2. Twenty-Four Month Recurrent Strokes (Adjudicated From Medical Records)
eTable 3. Twelve-Month Data for Self-Reported Heart Attack and Congestive Heart Failure by Treatment Group
eTable 4. Sensitivity Analysis Modeling Missingness for Systolic Blood Pressure
eTable 5. Sensitivity Analysis Modeling Missing Data for Achieved Blood Pressure Control at 130/80
eTable 6. Sensitivity Analysis Modeling Missing Data for Achieved Blood Pressure Control at 140/90
eTable 7. Sensitivity Analysis: Results of Repeated Measures ANOVA Mixed Models, Adjusting for Clustering Within PCP
eTable 8. Achievement of Blood Pressure Control
eTable 9. Treatment Intensification Over Time by Treatment Group
eTable 10. Observed Means (Standard Deviations) for Number of Nurse Case Management calls Completed and Proportion Adherent
eTable 11. Nurse Case Manager Call Adherence Outcome (Home BP Telemonitoring and Nurse Case Management Group Only) Modeled Using a Glimmix Model, Assuming a Logit Link, Adjusted for Clustering With PCP
eTable 12. Descriptive Statistics for Home Blood Pressure Telemonitoring Adherence Information
eTable 13. Home Blood Pressure Telemonitoring Adherence Outcome Using a Glimmix Model, Assuming a Logit Link Adjusted for Clustering within PCP
eFigure 1. Model Based Means for Systolic Blood Pressure by Treatment Group Over Time
eFigure 2. Model Based Means for SBP. Plot of Predicted Outcomes Based on ANOVA Mixed Models, Adjusting for Clustering within PCP
eFigure 3. Model-based Proportions for Achievement of Blood Pressure Less Than 130/80
eFigure 4. Model-based Proportions for Achievement of Blood Pressure Less Than 140/90
Data Sharing Statement