An occupational disease may be defined simply as one that is caused, or made worse, by exposure at work. While epidemiological studies of populations can determine whether disease is attributable to a particular type or level of exposure, for an individual patient this is less clear. Judgments about the patterns of exposure likely to be causal may be made in medicolegal cases or claims for compensation but these decisions have little value in determining the true extent of disease caused by work, not least because of the absence of reliable exposure data. Information about the incidence and distribution of such diseases is thus far from complete. This review describes recent advances in the understanding of the patterns and causes of occupational disease.
Summary points
An understanding of the causes of occupational disease requires both good epidemiology and detailed knowledge of the nature of exposure and the susceptibility of those exposed
Concern about the effects of workplace exposures on male reproductive capacity remains great despite the paucity of evidence for hypotheses about male mediated effects on the fetus
Good evaluative studies of preventive programmes are needed but are in short supply
Future advances in prevention of chronic non-malignant disease may come in part through better understanding of the role of psychosocial factors in the workplace
Despite our best efforts, occupational disease persists and may contribute significantly to disability in elderly people long past retirement
Methods
This article is based on published information on occupational disease from general and specialist medical journals and from epidemiological, psychological, and ergonomic journals, and from my own ongoing research. A review was carried out of all articles published since January 1997 in four influential occupational health journals: Occupational and Environmental Medicine, American Journal of Industrial Medicine, Scandinavian Journal of Work and Environment and Health, and Annals of Occupational Hygiene.
Distribution of disease
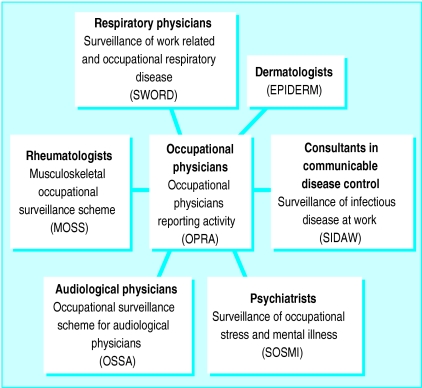
Some years ago the then Director of Medical Services of the UK Health and Safety Executive addressed the need to have information on the burden of occupational disease in order to set rational priorities for prevention.1 Of the methods advocated the most promising was the voluntary reporting of new cases of occupational disease by specialist physicians. At that time two occupational disease surveillance schemes were in place, one for respiratory disease (SWORD; Surveillance of Work Related and Occupational Respiratory Disease) and one for dermatoses (EPIDERM).2,3 In April 1998 these two schemes were brought together with five other surveillance schemes for occupational physicians, rheumatologists, consultants in communicable disease, audiological physicians, and psychiatrists to form the Occupational Disease Intelligence Network (ODIN) (fig 1). Some 2000 consultant physicians participate in these schemes providing an estimated total in excess of 20 000 new cases of occupational disease per year.
Figure 1.
Occupational disease surveillance schemes in Occupational Disease Intelligence Network
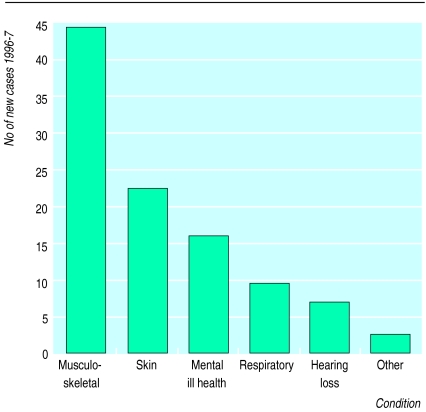
Figure 2 shows the distribution of diseases reported by occupational physicians in the first 2 years of their specialist surveillance scheme (OPRA; Occupational Physicians Reporting Activity). Of an estimated 21 686 cases, nearly one half were musculoskeletal disorders, a proportion similar to that self reported by workers.4 Each specialist physician participating in the Occupational Disease Intelligence Network receives a monthly or quarterly summary of incident cases including the distribution by occupation, industry, and suspected cause.
Figure 2.
New cases of diseases (n=21 686) reported by occupational physicians to Occupational Physicians Reporting Activity during 1996-7
Causes
In promoting the practice of occupational health a simple message may be the most effective—lead, radiation, and asbestos are bad for people, silicosis kills, and occupational disease can be eliminated by better work practices. Scientific advance, however, comes only from questioning such a simplistic approach. The hazard of exposure to a substance may depend on the form the substance takes, the circumstances of the exposure, or the worker’s susceptibility. Thus silica, classified by the International Agency for Research on Cancer as a human carcinogen may be carcinogenic only in certain industrial processes perhaps because of external factors affecting its biological activity or distribution of its polymorphs.5 Asbestos undoubtedly causes mesothelioma but the likelihood of this depends on the fibre type. Chrysotile is less likely to cause this cancer than crocidolite or amosite and then perhaps only when contaminated with tremolite.6 The carcinogenicity of man made mineral fibres developed as substitutes for asbestos seem to depend on their durability in the lung.7 In contrast, ultrafine particles seem to be much more harmful to the lung than an equivalent mass of fine particles of the same material8 with the substantial component of ultrafine particles in environmental9 and occupational10 air pollution thought to be responsible for increases in cardiovascular mortality. These advances in knowledge have been achieved by refining information on the nature of the exposure once the class of hazardous substance has been identified in epidemiological studies.
Another area in which closer study of exposure has forwarded knowledge is occupational asthma, where discussion has been not simply about the nature of the substance that can produce asthma by immunological or other mechanisms but also the type and concentration of exposure. It seems, for example, that a single high exposure to a respiratory irritant may induce reactive airways disease that is clinically similar to asthma11 and that, for certain chemicals of low molecular weight, dermal exposure may be sufficient to sensitise the respiratory tract.12 Extensive work by the group at the National Heart and Lung Institute in London has shown a clear exposure-response relation for the development of specific IgE and asthma caused by the inhalation at work of both inhaled proteins, such as rat urine protein,13 and low molecular weight chemicals, such as acid anhydrides.14 The maximum risk of disease is highest in the first 2 years of exposure and is further increased in people who smoke cigarettes.
The National Heart and Lung Institute group and other groups have also investigated differences in susceptibility to occupational hazards on the basis of a person’s genotype. Sensitisation to several chemical causes of asthma is related to specific HLA genotype. Sensitisation to the acid anhydride tremellitic anhydride15 and to the complex platinum salt ammonium hexachloroplatinate16 is increased in those with HLA DR3. Bignon et al showed that asthma caused by isocyanates was more likely to occur in people with a particular combination of HLA DQB1 alleles.17 Balboni et al suggested this increased susceptibility was due to the presence of aspartic acid in position 57 of the HLA DQB1 molecule (HLA DQB Asp 57).18 Similarly, the risk of developing chronic beryllium disease is greatly increased in those with HLA DPB1 Glu 69.19
In occupational health, the identification of a substance as hazardous always carries a cost. This cost may be very significant particularly if no safe level of exposure can be achieved and no effective substitute found. In 1990 it was postulated that paternal exposure to radiation at work was responsible for the excess of childhood leukaemias at Seascale in west Cumbria.20 The implications of this hypothesis, both scientifically and for the nuclear industry, were considerable, and publication of the hypothesis led to further epidemiological and experimental work. This work was reviewed recently by the Committee on Medical Aspects of Radiation in the Environment, which concluded that “paternal preconception irradiation cannot account for the Seascale childhood leukaemia excess.”21 A review of recent advances in occupational health in 1990 would no doubt have included Gardner et al’s paper as a landmark investigation, which it was, but the more recent rejection of the hypothesis can be seen as an advance of equal importance.
After Gardner et al’s hypothesis, several studies of male mediated effects on the fetus were undertaken, some of which have now been published.22,23 Suggestions about declining sperm counts have prompted reviews and research funding on the effects of chemicals on male fertility.24,25 Despite considerable efforts, no effects have been found to match the impact of earlier work on azoospermia in men exposed to dibromochloropropane.26
Prevention
The aim of occupational health is to prevent disease, and advances can be measured not simply by knowledge of disease causation but also by the extent to which interventions are shown to be effective in reducing incidence or severity. With diseases of long latency it will inevitably be many years before decreased exposures today can result in less disease,27 but the intervention—for example, the substitution of non-allergenic gloves for those made of latex—may at times follow so obviously from the identification of a hazard that reduced incidence is evident from routine voluntary surveillance.28 In general, however, systematic evaluation of preventive measures in occupational health is seriously lacking, although methods have long been available.29 A recent attempt to assess, by systematic review, evidence from intervention studies on the prevention of back pain incidence judged the quality of the studies to be so poor that the reviewers were able to conclude only that exercise might help in the prevention of back pain but that training did not.30
Future advances
Detailed epidemiological studies being carried out to define, diagnose, and measure musculoskeletal disease and to characterise exposure should result in a clearer understanding of the relation between exposure and disease and of factors predicting its onset.31–36 Reduction in the incidence of such cases will require systematic investigation not only of physical job demands but also of those psychosocial factors in the workplace that may mediate disability and themselves be susceptible to intervention.37 The role of such psychological factors, specifically low job control, has been shown in new episodes of heart disease.38 If well designed intervention studies can show that reduction in disease results from increasing workers’ control over their jobs this will be a major advance in occupational health.
The elimination of occupational disease, however laudable an aim, remains unattainable; there are too many areas in which rapid progress seems unlikely. There is, for example, little advance in determining safe levels of exposure to respiratory sensitisers or of improving working conditions sufficiently to prevent asthma. The incidence of occupational dermatoses, barely mentioned in recent occupational health journals, continues largely unchecked. In diseases of long latency, biological markers of past exposure or future disease remain elusive, seriously limiting the capacity to show that protective measures proposed today will be effective. Recent work has begun to show the effects in elderly people of repeated exposures to hazards during their working life, but this is an area in which few studies have been reported.39 Large numbers of elderly people, mentally or physically disabled by work, would represent a very considerable cost to society, but the recognition and prevention of such late onset chronic disease does not seem to be at the top of any agenda.
Footnotes
Competing interests: None declared.
References
- 1.Carter JT. There’s a lot of it about. Br J Ind Med. 1991;48:289–291. doi: 10.1136/oem.48.5.289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Meredith SK, Taylor VM, McDonald JC. Occupational respiratory diseases in the United Kingdom 1989: a report to the British Thoracic Society and the Society of Occupational Medicine by the SWORD project group. Br J Ind Med. 1991;48:292–298. doi: 10.1136/oem.48.5.292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cherry NM, Beck M, Owen-Smith V. Proceedings of the 9th International Symposium on Epidemiology in Occupational Health. Cincinnati, OH: US Department of Health and Human Services; 1994. Surveillance of occupational skin diseases in the United Kingdom—the OCC-DERM project. [Google Scholar]
- 4.Hodgson JT, Jones JR, Elliot RC, Osman J. Self reported work-related illness. HMSO: HSE Books; 1993. [Google Scholar]
- 5.International Agency for Research on Cancer. Monographs on the evaluation of the carcinogenic risk of chemicals to humans. Silica, some silicates, coal dust and para-aramid fibrils. Vol. 68. Lyons: International Agency for Research on Cancer; 1997. [PMC free article] [PubMed] [Google Scholar]
- 6.McDonald JC, McDonald AD. Chrysotile tremolite and carcinogenicity. Ann Occup Hyg. 1997;41:699–705. doi: 10.1016/S0003-4878(97)89350-7. [DOI] [PubMed] [Google Scholar]
- 7.Jones AD, Miller BG, Cullen RT, Searl A, Davis JMG, Buchanan D, et al. The colt fibre research programme: aspects of toxicological risk assessment. Ann Occup Hyg. 1997;41(suppl 1):244–250. [Google Scholar]
- 8.Donaldson K, Li XY, MacNee W. Ultrafine (nanometre) particle mediated lung injury. J Aerosol Sci. 1998;29:553–560. [Google Scholar]
- 9.Seaton A, MacNee W, Donaldson K, Godden D. Particulate air pollution and acute health effects. Lancet. 1995;345:176–178. doi: 10.1016/s0140-6736(95)90173-6. [DOI] [PubMed] [Google Scholar]
- 10.Sjögren B. Occupational exposure to dust: inflammation and ischaemic heart disease. Occup Environ Med. 1997;54:466–469. doi: 10.1136/oem.54.7.466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ross DJ, McDonald JC. Asthma following inhalation accidents reported to the SWORD project. Ann Occup Hyg. 1996;40:645–650. doi: 10.1016/s0003-4878(96)00022-1. [DOI] [PubMed] [Google Scholar]
- 12.Kimber I, Wilks MF. Chemical respiratory allergy. Toxicol Occup Health Issues. 1995;14:735–736. doi: 10.1177/096032719501400907. [DOI] [PubMed] [Google Scholar]
- 13.Cullinan P, Lowson D, Niewenhuijsen M, Gordon S, Tee RD, Venables KM, et al. Work related symptoms, sensitisation and estimated exposure in workers not previously exposed to laboratory rats. Occup Environ Med. 1994;51:589–592. doi: 10.1136/oem.51.9.589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Barker RD, van Tongeren MJA, Harris JM, Gardiner K, Venables KM, Newman Taylor AJ. Risk factors for sensitisation and respiratory symptoms among workers exposed to acid anhydrides: a cohort study. Occup Environ Med. 1998;55:684–691. doi: 10.1136/oem.55.10.684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Young RP, Barker RD, Pile KD, Cookson WOCM, Newman Taylor AJ. The association of HLA DR3 with specific IgE to inhaled acid anhydrides. Am J Respir Crit Care Med. 1995;151:219–221. doi: 10.1164/ajrccm.151.1.7812558. [DOI] [PubMed] [Google Scholar]
- 16.Lympany PA, Harris JM, Dowdeswell R, Cullinan P, du Bois RM, Newman Taylor AJ. Interaction of HLA phenotype and smoking with exposure in sensitisation to complex platinum salts. Am J Respir Crit Care Med. 1997;155:1335. doi: 10.1164/ajrccm.160.2.9807065. [DOI] [PubMed] [Google Scholar]
- 17.Bignon JS, Aron Y, Ju LY, Kopterschmitt MC, Garnier R, Mapp C, et al. HLA class II alleles in isocyanate-induced asthma. Am J Respir Crit Care Med. 1994;149:71–75. doi: 10.1164/ajrccm.149.1.8111601. [DOI] [PubMed] [Google Scholar]
- 18.Balboni A, Baricordi OR, Fabbri LM, Gandini E, Ciaccia A, Mapp CE. Association between toluene diisocyanate-induced asthma and DQB1 markers: a possible role for aspartic acid at position 57. Eur Respir J. 1996;9:207–210. doi: 10.1183/09031936.96.09020207. [DOI] [PubMed] [Google Scholar]
- 19.Richeldi L, Kreiss K, Mroz MM, Zhen B, Tartoni P, Saltini C. Interaction of genetic and exposure factors in the prevalence of berylliosis. Am J Ind Med. 1997;32:337–340. doi: 10.1002/(sici)1097-0274(199710)32:4<337::aid-ajim3>3.0.co;2-r. [DOI] [PubMed] [Google Scholar]
- 20.Gardner MJ, Hall AJ, Snee MP, Downes S, Powell CA, Terrell JD. Methods and basic data of case-control study of leukaemia and lymphoma among young people near Sellafield nuclear plant in west Cumbria. BMJ. 1990;300:429–434. doi: 10.1136/bmj.300.6722.429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Committee on medical aspects of radiation in the environment (COMARE) The incidence of cancer and leukaemia in young people in the vicinity of the Sellafield site, west Cumbria: further studies and an update of the situation since the publication of the report of the Black advisory group in 1984. 4th report. London: Department of Health; 1996. [Google Scholar]
- 22.Lin S, Hwang SA, Marshall EG, Marion D. Does paternal occupational lead exposure increase the risks of low birth weight or prematurity? Am J Epidemiol. 1998;148:173–181. doi: 10.1093/oxfordjournals.aje.a009621. [DOI] [PubMed] [Google Scholar]
- 23.Irgens A, Krüger K, Skorve AH, Irgens LM. Reproductive outcome in offspring of parents occupationally exposed to lead in Norway. Am J Epidemiol. 1998;34:431–437. doi: 10.1002/(sici)1097-0274(199811)34:5<431::aid-ajim3>3.0.co;2-t. [DOI] [PubMed] [Google Scholar]
- 24.Farrow S. Falling sperm quality: fact or fiction? BMJ. 1994;309:1–2. doi: 10.1136/bmj.309.6946.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tas S, Lauwerys R, Lison D. Occupational hazards for the male reproductive system. Crit Rev Toxicol. 1996;26:261–307. doi: 10.3109/10408449609012525. [DOI] [PubMed] [Google Scholar]
- 26.Whorton D, Krauss RM, Marshall S, Milby TH. Infertility in male pesticide workers. Lancet 1977:1259-61. [DOI] [PubMed]
- 27.Peto J, Hodgson J, Matthews FE, Jones JR. Continuing increases in mesothelioma mortality in Britain. Lancet. 1995;345:544–547. doi: 10.1016/s0140-6736(95)90462-x. [DOI] [PubMed] [Google Scholar]
- 28.Liss GM, Sussman GL, Deal K, Brown S, Cividino M, Siu S, et al. Latex allergy: epidemiological study of 1351 hospital workers. Occup Environ Med. 1997;54:335–342. doi: 10.1136/oem.54.5.335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cherry NM. Evaluation of preventive measures. In: McDonald JC, editor. The epidemiology of work related disease. London: BMJ Books; 1995. pp. 413–439. [Google Scholar]
- 30.Van Poppel MNM, Koes BW, Smid T, Bouter LM. A systematic review of controlled clinical trials on the prevention of back pain in industry. Occup Environ Med. 1997;54:841–847. doi: 10.1136/oem.54.12.841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Harrington JM, Carter JT, Birrell L, Gompertz D. Surveillance case definitions for work related upper limb pain syndromes. Occup Environ Med. 1998;55:1–8. doi: 10.1136/oem.55.4.264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Croft PR, Pope D, Zonca M, O’Neill T, Silman AJ. Measurement of shoulder related disability: results of a validation study. Ann Rheum Dis. 1994;53:525–528. doi: 10.1136/ard.53.8.525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Van der Beek AJ, Frings-Dresen MHW. Assessment of mechanical exposure in ergonomic epidemiology. Occup Environ Med. 1998;55:291–299. doi: 10.1136/oem.55.5.291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Griffin MJ. Measurement, evaluation, and assessment of occupational exposures to hand-transmitted vibration. Occup Environ Med. 1997;54:73–89. doi: 10.1136/oem.54.2.73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Punnett L. Ergonomic stressors and upper extremity disorders in vehicle manufacturing: cross sectional exposure-response trends. Occup Environ Med. 1998;55:414–420. doi: 10.1136/oem.55.6.414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Werner RA, Franzblau A, Albers JW, Buchele H, Armstrong TJ. Use of screening nerve conduction studies for predicting future carpal tunnel syndrome. Occup Environ Med. 1997;54:96–100. doi: 10.1136/oem.54.2.96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Krause N, Ragland DR, Greiner BA, Syme SL, Fisher JM. Psychological job factors associated with back and neck pain in public transit operators. Scand J Work Environ Health. 1997;23:179–186. doi: 10.5271/sjweh.196. [DOI] [PubMed] [Google Scholar]
- 38.Bosma H, Marmot MG, Hemingway H, Nicholson AC, Brunner E, Stansfield SA. Low job control and risk of coronary heart disease in Whitehall II (prospective cohort) study. BMJ. 1997;314:558–565. doi: 10.1136/bmj.314.7080.558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sobti A, Cooper C, Inskip H, Searle S, Coggon D. Occupational physical activity and long-term risk of musculoskeletal symptoms: a national survey of post office pensioners. Am J Ind Med. 1997;32:76–83. doi: 10.1002/(sici)1097-0274(199707)32:1<76::aid-ajim9>3.0.co;2-p. [DOI] [PubMed] [Google Scholar]