Abstract
Laboratory strains of Sindbis virus must bind to the negatively charged glycosaminoglycan heparan sulfate in order to efficiently infect cultured cells. During infection of mice, however, we have frequently observed the development of large-plaque viral mutants with a reduced ability to bind to heparan sulfate. Sequencing of these mutants revealed changes of positively charged amino acids in putative heparin-binding domains of the E2 glycoprotein. Recombinant viruses were constructed with these changes as single amino acid substitutions in a strain Toto 1101 background. All exhibited decreased binding to heparan sulfate and had larger plaques than Toto 1101. When injected subcutaneously into neonatal mice, large-plaque viruses produced higher-titer viremia and often caused higher mortality. Because circulating heparin-binding proteins are known to be rapidly sequestered by tissue heparan sulfate, we measured the kinetics of viral clearance following intravenous injection. Much of the parental small-plaque Toto 1101 strain of Sindbis virus was cleared from the circulation by the liver within minutes, in contrast to recombinant large-plaque viruses, which had longer circulating half-lives. These findings indicate that a decreased ability to bind to heparan sulfate allows more efficient viral production in vivo, which may in turn lead to increased mortality. Because Sindbis virus is only one of a growing number of viruses from many families which have been shown to bind to heparan sulfate, these results may be generally applicable to the pathogenesis of such viruses.
The alphaviruses are RNA viruses which are carried by hematophagous insects, such as mosquitoes, and can infect a wide variety of mammalian and avian hosts. In vertebrates, they can replicate extremely rapidly and cause high-titer viremia, which allows transmission of the virus to new mosquitoes. Sindbis virus (SV) is a particularly well-studied alphavirus which causes a mild rash and arthritis in humans but can cause fatal encephalomyelitis in mice.
The cell surface receptors which allow alphaviruses such as SV to infect such a broad variety of species have not yet been conclusively determined, but it has recently been shown that SV can attach to heparan sulfate (HS), a negatively charged glycosaminoglycan expressed on many types of cells (4, 23, 32). Sulfated glycosaminoglycans on the cell surface and in the extracellular matrix normally bind a wide variety of growth factors, chemokines, enzymes, and matrix components (30, 45) but are also important in the attachment of a number of bacteria, protozoa, and viruses (42). Proteins typically bind electrostatically to HS by use of stretches of positively charged amino acids such as Lys and Arg, and attachment of SV to HS is presumably mediated in the same fashion. Although the use of cell surface HS greatly increases the efficiency of SV attachment, it is not absolutely required for infection, and a distantly related Alphavirus, Ross River virus, does not bind HS at all (4). It has been proposed that the ability of SV to bind HS could be an adaptation which arose in laboratory strains during repeated passaging in tissue culture and that wild-type strains of SV might not bind well to HS (32). Nevertheless, SV joins a growing number of viruses which have been shown to bind HS, including many herpesviruses, human immunodeficiency virus type 1 (HIV-1), dengue virus, adeno-associated virus type 2, respiratory syncytial virus, foot-and-mouth disease virus (FMDV), human papillomavirus type 11, and vaccinia virus (6, 16, 18, 26, 33, 38, 46, 54). A study of the relevance of HS to the pathogenesis of SV may therefore lead to parallel insights into the in vivo behavior of other HS-binding viruses.
The alphavirus virion structure is relatively simple, with an outer lipid layer which is derived from the host cell membrane and which contains 240 copies of the viral E1 and E2 glycoproteins (44). The E2 glycoprotein is synthesized as a larger precursor which is cleaved into E2 and another short protein, E3, which remains associated with the virion for some alphaviruses, although not for SV. Inside the virion is an icosahedral capsid which surrounds the 11.7-kb positive-sense RNA genome. During infection, the E2 glycoprotein is largely responsible for binding to cells. After the virus is endocytosed, an acid-induced rearrangement of the glycoproteins exposes a hydrophobic domain of E1, allowing fusion of the viral and cellular membranes and penetration of the capsid into the cytoplasm.
Pharmacokinetic studies have shown that when HS-binding proteins are injected intravenously, they are rapidly cleared from the circulation through binding to tissue HS (27, 28). There is reason to suspect that HS-binding viruses may behave in the same manner. A number of studies have shown that alphavirus strains have different clearance rates after intravenous injection, with small-plaque (SP) variants typically having shorter half-lives than large-plaque (LP) variants (20, 22, 40), but the reason for these findings has been unknown. We have proposed that binding to HS controls both the plaque size and the circulating half-life and that SP variants are cleared more quickly from the circulation because they bind better to HS (4). This characteristic may contribute to lower levels of viremia during infection with SP variants and consequent lower mortality rates. The present study was undertaken to explore this hypothesis, with the additional aim of defining the regions of the SV glycoproteins which are involved in binding to HS.
MATERIALS AND METHODS
Viruses and cells.
BHK-21 cells were grown in Dulbecco's modified Eagle medium containing 10% heat-inactivated fetal calf serum and 50 μg of gentamicin per ml. CHO-K1 and glycosaminoglycan-deficient pgsA-745 cells (10) were grown in Ham's F-12 medium with the same supplements. SV strains Toto 1101 (41) and AR339 were grown and passaged on BHK cells. Plaque assays were performed as previously described (4) with BHK cells under 0.6% Bacto Agar (Difco, Detroit, Mich.) or agarose (Gibco BRL, Gaithersburg, Md.).
Site-directed mutagenesis of Toto 1101 was performed with a 1.2-kb StuI/BssHII fragment by use of the GeneEditor mutagenesis system (Promega, Madison, Wis.). After being cloned into pToto1101, the entire 1.2-kb region was verified by sequencing. Plasmids were linearized with XhoI, and capped RNA was transcribed with an Invitroscript CAP kit (Invitrogen, Carlsbad, Calif.). RNA was electroporated into 5 × 106 pgsA-745 cells, and virus was allowed to grow for 2 days in Ham's F-12 medium containing 10% heat-inactivated fetal calf serum. Titers of stocks were determined by a plaque assay with BHK cells under agar. For measuring plaque size, plates were overlaid with either agar or agarose, and after 2 days, the diameters of at least 15 plaques were measured to the nearest 0.5 mm.
[35S]Met-Cys-labeled viral stocks were grown on BHK cells as described previously (4) following infection with unpassaged pgsA-745-derived stocks at a multiplicity of infection of 0.5 to 1. Unlabeled high-titer viral stocks for intravenous clearance studies were grown in a similar manner. Both labeled and unlabeled stocks were purified as described previously (4) by pelleting with polyethylene glycol, banding on a potassium tartrate gradient, and pelleting through a 15% sucrose cushion.
Binding of radiolabeled virus to CHO and pgsA-745 cell monolayers at 4°C was determined as previously described (4) in phosphate-buffered saline (PBS) (pH 7.2) with 0.5 mM MgCl2, 0.5 mM CaCl2, and 0.5% bovine serum albumin.
Heparin-Sepharose chromatography.
Prepacked 1-ml heparin-Sepharose HiTrap columns (Amersham Pharmacia Biotech, Piscataway, N.J.) were equilibrated with 10 ml of 50 mM NaCl–5 mM phosphate (pH 7.5)–0.5% bovine serum albumin. This step was followed by the addition of 1 ml of the same buffer containing 100,000 cpm of 35S-labeled virus at a rate of 1 ml/min and collection of 1-ml fractions. After 10 ml of the same 50 mM NaCl buffer was added, the virus was eluted with a 40-ml linear gradient from 50 to 500 mM NaCl. Any remaining virus was removed with 10 ml of 0.5% sodium dodecyl sulfate. Fractions were counted by liquid scintillation spectroscopy, and the NaCl concentration of the peak fraction was determined with a conductivity meter.
ELISA.
Half-area 96-well plates were coated with polyethylene glycol-precipitated virus at 0.6 μg per well. Monoclonal antibodies (MAb) reactive against the SV E2 glycoprotein were added to duplicate wells as 1:1,000 dilutions of ascitic fluid. Two MAb directed against the E2c epitope, R6 (37) and G5 (51), along with 202, an antibody reactive with the E2ab epitope (36), and 3E1, a negative control MAb against herpes simplex virus, were used. The enzyme-linked immunosorbent assay (ELISA) was developed with a rabbit anti-mouse antibody conjugated to horseradish peroxidase, and samples were reacted with o-phenylenediamine for 30 min at room temperature. Optical densities at 450 nm of <0.1 were considered negative, and values of >0.3 were considered positive.
Mice.
Alpha/beta interferon (IFN-α/β) receptor-deficient (A129) mice were obtained from B&K Universal (Hull, United Kingdom) and bred in a specific-pathogen-free facility at Johns Hopkins University. Antibody-deficient (μMT) mice were obtained from Jackson Laboratories (Bar Harbor, Maine). Viral virulence was determined with 2-day-old litters of CD-1 mice obtained from Charles River Laboratories (Wilmington, Mass.). Mice were injected subcutaneously with 1,000 PFU of unpassaged pgsA-745-grown virus in 30 μl of Hank's balanced salt solution and were monitored daily for 15 days. At least four litters of mice (total of at least 38 mice) were used per virus.
For intravenous clearance studies, 5- to 7-week-old male ICR mice (Taconic, Germantown, N.Y.) weighing 30 to 40 g were anesthetized intraperitoneally with tribromoethanol (Avertin; 0.5 mg per g of body weight) and kept anesthetized until the end of the experiment. Mice were injected intravenously via the tail vein with about 107 PFU of gradient-purified virus in 100 μl of PBS. Blood was collected from the retro-orbital plexus at 2, 5, 10, 20, 30, and 45 min postinjection by use of a 20-μl capillary tube. Blood was allowed to clot at room temperature, and the amount of virus in the serum was determined by a plaque assay with BHK cells. The clearance curves were fitted to the equation V = Ae−t/α + Be−t/β, where V is the viral concentration in PFU per milliliter and t is the time postinjection. Weighted (1/V) nonlinear regression was performed with SigmaPlot (SPSS, Chicago, Ill.). The viral concentrations were normalized by dividing them by V0, the concentration of virus at 0 min postinjection, which was calculated according to the above equation.
Alternatively, ICR mice were injected intravenously with approximately 150,000 cpm of 35S-labeled purified virus in 100 μl of PBS. At 30 min postinjection, mice were exsanguinated by perfusion with PBS. Various organs were collected and dissolved in 5 M NaOH for 4 to 5 h at 70°C. Following the addition of Liquiscint (National Diagnostics, Atlanta, Ga.) and neutralization with glacial acetic acid, counts were determined by liquid scintillation spectroscopy.
RESULTS
Derivation of LP viruses.
Agar contains a sulfated polysaccharide which interferes with the efficient attachment of certain viruses to cells (49, 50). Agarose is a purified form of agar which does not contain sulfated polysaccharides. We have hypothesized that viruses which bind strongly to HS are impaired by the sulfated polysaccharide in agar and therefore have a smaller plaque size under agar than they do under agarose (4). In contrast, the finding that the plaque size of a virus under agar is large and essentially equal to the plaque size under agarose may be evidence that a virus binds less well to glycosaminoglycans. We noticed that within a few days after infection of mice with SP strains of SV, such as Toto 1101 and AR339, serum frequently had a mixture of SP and LP viruses when assayed on BHK monolayers under agar. The LP mutants presumably enjoy a selective advantage during infection (see below). For these experiments, it was helpful to use models with long-lasting and high-titer serum viremia, such as mice deficient in antibody or the type I interferon receptor, although infection of normal neonatal mice also resulted in LP mutants. Even so, LP viruses were not found in every animal, and the percentage of LP viruses in the serum of any given mouse was variable, ranging from a small percentage to 80%.
LP viruses from individual mice were isolated, plaque purified, and expanded on BHK cells. RNA was isolated from infected cells and amplified by reverse transcription-PCR for complete sequencing of the E2, 6K, and E1 genes and partial sequencing of the E3 gene, including the furin protease cleavage site at the E3-E2 junction. 6K is a short hydrophobic protein that is present in the virion lipid membrane in small amounts and is not expected to interact with cellular receptors. Every LP isolate had at least one amino acid change in the E2 ectodomain (Table 1), while no coding changes in the E1, 6K, or E3 regions were found. In some cases, a second LP isolate from the same animal was sequenced; these pairs of isolates always had identical mutations.
TABLE 1.
Sequencing of LP isolates from infected mice
| Virus | Coding change(s) in E2a | Parental virus | Mouse serum sourceb |
|---|---|---|---|
| 11D2 | R157H | Toto 1101 | Adult IFN-α/β receptor knockout |
| 11E2 | D5V, K76E | Toto 1101 | Adult IFN-α/β receptor knockout |
| 11G1 | K159E, T161Kc | Toto 1101 | Adult IFN-α/β receptor knockout |
| 105 | K76N, T308S | AR339 | Adult μMT (antibody deficient) |
| 106 | K230M | AR339 | Adult μMT (antibody deficient) |
| 4A1 | N62D | Toto 1101 | Neonatal CD-1 |
All LP mutants had at least one amino acid change in E2 but none in E1 or 6K.
Mice were infected subcutaneously, except for μMT mice, which were infected intracerebrally.
Sequencing of the parental Toto 1101 virus, which had been passaged several times in BHK cells, showed that the parental population contained some viruses with the T161K mutation.
Preliminary characterization of LP isolates indicated a reduced ability to bind heparin (data not shown). To examine the effect of specific E2 mutations in the absence of other potential changes in unsequenced regions of the viral genome, individual codon changes were introduced into plasmid pToto1101 in order to transcribe infectious SV RNA (41). When more than one mutation was found in an individual virus, the change involving the loss of a positively charged amino acid was chosen (Table 2), as such residues might participate directly in binding to sulfates on HS. Mutation of the Lys at residue 76 of E2 was found in two separate isolates, one with a change to Asn and one with a change to Glu (Table 1). Because a change of Lys 76 to Thr has previously been reported to occur during selection for budding in cultured cells under low-ionic-strength conditions (34), we also constructed a virus containing Thr at this position.
TABLE 2.
Recombinant viruses
| Virus | Plaque diam (mm) with:
|
Heparin-Sepharose elution (mM NaCl) | ELISA reactivityb of E2 MAb:
|
|||
|---|---|---|---|---|---|---|
| Agar | Agarose | R6 | G5 | 202 | ||
| Toto 1101 | 1.3 ± 0.4a | 3.3 ± 0.7 | 323 | + | + | + |
| R157H | 2.5 ± 0.7 | 2.8 ± 0.6 | 289 | + | + | + |
| N62D | 2.0 ± 0.7 | 2.2 ± 0.6 | 276 | − | + | + |
| K159E | 2.8 ± 0.8 | 2.6 ± 0.7 | 261 | − | + | + |
| K230M | 2.4 ± 0.8 | 2.6 ± 0.7 | 202 | + | + | + |
| K76N | 2.3 ± 0.9 | 2.5 ± 0.7 | 142 | + | + | + |
| K76T | 2.3 ± 0.8 | 2.6 ± 0.8 | 97 | + | + | + |
| K76E | 3.1 ± 0.8 | 2.5 ± 0.8 | 66 | + | + | + |
The plaque size (mean ± standard deviation) of Toto 1101 under agar was significantly smaller (P, <0.05) than those of all other viruses under agar and was also significantly smaller than that of Toto 1101 under agarose (Kruskal-Wallis analysis of variance ranks followed by Dunn's multiple-comparison test).
+, reactivity; −, no reactivity.
Transfection and passaging of non-HS-binding SV variants on BHK cells can result in the rapid selection of HS-binding mutant viruses, which are at a selective advantage in tissue cultures because they bind much better to BHK cells (32). To minimize such selection pressure, we transfected viral RNA into pgsA-745 cells (which do not synthesize HS) and produced high-titer stocks by infecting BHK cells with the unpassaged virus at a relatively high multiplicity of infection (see Materials and Methods).
All seven of the recombinant viruses produced plaques under agar which were significantly larger than plaques made by the parental strain Toto 1101 (Table 2), indicating that the LP phenotypes of the original viral isolates were due solely to mutations in the E2 glycoprotein.
Viral binding to heparin, HS, and MAb.
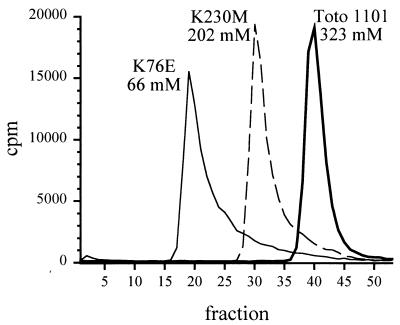
Radiolabeled, purified preparations of Toto 1101 and the seven recombinant viruses were examined by heparin-Sepharose chromatography. Heparin is a more highly sulfated glycosaminoglycan than HS, but the carbohydrate structure is otherwise similar. Mutated viruses were eluted from heparin-Sepharose columns at a range of NaCl concentrations, but all were eluted earlier than Toto 1101, indicating weaker binding to heparin (Fig. 1 and Table 2). All three viruses with substitutions for Lys 76 bound poorly to heparin. However, the virus containing the polar amino acid Asn at position 76 had the best binding of the three—heparin-binding sites sometimes contain Asn or Gln residues which interact with heparin through hydrogen bonds (15). Virus with Thr 76 bound more poorly to heparin than virus with Asn 76, and the negatively charged Glu 76 mutant bound most poorly of all. This result may indicate that the residue at position 76 interacts directly with sulfates on heparin and that the overall charge of the E2 glycoprotein at this position is important in determining the strength of the interaction.
FIG. 1.
Viral binding to heparin. Radiolabeled SV was applied to heparin-Sepharose and eluted with a 50 to 500 mM NaCl gradient. Elution at a higher NaCl concentration indicates stronger binding to heparin. Eluted virus is intact and fully infectious. (Five other viruses are not shown; see Table 2 for results.)
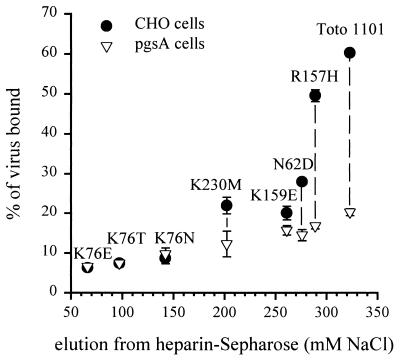
When viral binding to monolayers of CHO cells was examined, the percentage of virus bound by the monolayers correlated well (r2, 0.76) with the ability of the virus to bind to heparin (Fig. 2). CHO cells express HS and chondroitin sulfate, but the CHO-derived pgsA-745 cell line expresses neither of these glycosaminoglycans (10). When binding to pgsA-745 cells was examined, viruses such as Toto 1101 and R157H, which bound strongly to CHO cells, bound much less well to pgsA-745 cells. In contrast, viruses K76E, K76T, and K76N bound equally well to CHO and pgsA-745 cells, indicating that they were essentially unable to bind to cellular HS. Surprisingly, however, there was a correlation (r2, 0.96) between heparin binding and binding to pgsA-745 cells (Fig. 2). In other words, even in the complete absence of cellular HS, viruses such as Toto 1101 and R157H were two- to threefold better at binding to pgsA-745 cells than K76E, K76T, and K76N were. This result may indicate that disrupting the ability of the virus to bind to heparin and HS also decreases the ability to bind to other, nonglycosaminoglycan receptors.
FIG. 2.
Viral binding to cultured cells. Radiolabeled SV was allowed to bind to CHO or glycosaminoglycan-deficient pgsA-745 cells at 4°C for 2 h. The mean binding ± standard deviation for three replicates is shown. The data along the x axis are taken from Table 2.
Two of the mutations found in our LP viruses, N62D and K159E, have been previously described by Pence et al. during selection for antibody escape mutants which fail to bind MAb R6, a neutralizing antibody against the E2c epitope (39). Because we established that these two amino acid changes also decrease binding to heparin, we examined whether a lack of reactivity to MAb R6 was a general feature of viruses with impaired binding to heparin. Of the seven mutants, however, only N62D and K159E failed to bind to MAb R6 (Table 2), indicating that this was not the case. All eight viruses bound equal amounts of MAb G5 (another antibody against the E2c epitope) and MAb 202, an antibody against the E2ab epitope.
Behavior in mice.
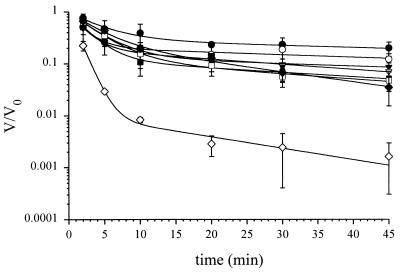
Heparin-binding proteins tend to have very short half-lives in the circulation, being rapidly sequestered by tissue HS, particularly in the liver, which has the most highly sulfated HS of any organ (2, 35, 53, 55). It has been reported in several studies that plaque variants of alphaviruses are cleared at variable rates from the circulation after an intravenous injection, with LP variants typically having longer half-lives (19, 20, 40). Because it is now apparent that one of the factors contributing to increased plaque size is a decreased ability to bind to sulfated polysaccharides, we reexamined the elimination of virus from the circulation. Purified viral preparations were injected intravenously as a bolus, and blood was collected at intervals for 45 min. The parental virus, Toto 1101, was cleared from the circulation much faster than any of the seven viruses having reduced heparin affinity (Fig. 3). All viruses were eliminated with biphasic kinetics (see Discussion). The clearance of infectious virus shown here represents actual physical removal of the virus from the circulation and is not due merely to inactivation of infectivity. Previous studies have shown that alphaviruses, regardless of plaque size, are not inactivated by serum or whole blood (22, 40), and clearance of radiolabeled alphaviruses from the circulation has been shown to follow kinetics identical to the clearance of PFU (20, 21).
FIG. 3.
Kinetics of viral clearance. Mice were injected intravenously with a 100-μl bolus of purified virus. Serum was collected, and titers were determined by a plaque assay with BHK cells at various times postinjection; V/V0 indicates the fraction of virus remaining. Each point represents the mean ± standard deviation for three mice. Curves were fitted by nonlinear regression as described in Materials and Methods. Symbols: ●, K76T; ○, K230M; ▾, N62D; ▿, K159E; ■, K76E; □, K76N; ⧫, R157H; ◊, Toto 1101.
In order to determine the organ distribution of virus following clearance from the circulation, various radiolabeled viruses were injected intravenously, and selected organs were collected after perfusion of the mice 30 min later. For Toto 1101, about half of the injected counts were found in the liver, with a much smaller amount being associated with the spleen (Table 3). When K159E and K76E were injected, the liver contained significantly smaller amounts than had been found with Toto 1101 (P, <0.05, as determined by an analysis of variance followed by a Tukey test). K159E and K76E were also found in the spleen, although the amounts were highly variable, with no significant differences compared to the amount of Toto 1101. For all three viruses, little radioactivity could be found in the kidneys, lungs, or brain. Not all of the injected counts were recovered—for K159E and K76E, 7 to 9% of the virus was still in the circulation at this time (Fig. 3), and the remaining virus was presumed to be distributed widely throughout the body. Another Alphavirus, Venezuelan equine encephalitis virus (VEE virus), shows a similar organ distribution after intravenous injection (20).
TABLE 3.
Organ distribution of radiolabeled virus 30 min after intravenous injection
| Organ | Mean % of total counts injected ± SD (n = 3) for:
|
||
|---|---|---|---|
| Toto 1101 | K159E | K76E | |
| Liver | 53.0 ± 4.7 | 21.8 ± 0.9 | 12.0 ± 2.8 |
| Spleen | 4.1 ± 0.8 | 12.6 ± 7.9 | 10.8 ± 8.6 |
| Kidneys | 0.53 ± 0.02 | 0.89 ± 0.13 | 0.70 ± 0.08 |
| Lungs | 0.24 ± 0.05 | 0.47 ± 0.19 | 0.50 ± 0.24 |
| Brain | 0.05 ± 0.03 | 0.09 ± 0.01 | 0.08 ± 0.01 |
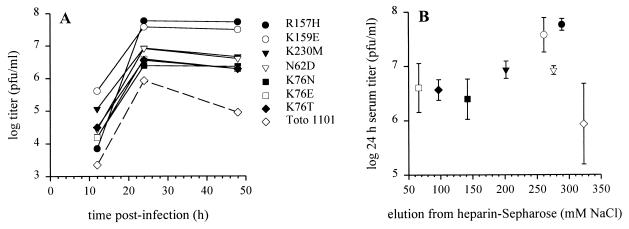
Toto 1101 and each of the seven recombinant viruses were injected subcutaneously into 2-day-old mice, and serum titers were assayed over the following 2 days (Fig. 4A). In every case, mice infected with an LP mutant had significantly higher titers than mice infected with Toto 1101. However, when the peak serum titer was plotted against the strength of association with heparin, no obvious relationship between these two factors was apparent (Fig. 4B). Thus, while reducing the ability of the viruses to bind to HS always led to higher viremia, the mutations may have had other effects on the ability of the viruses to replicate. It should be pointed out that plaque assays are an imperfect measure of the amount of a virus when the viruses being compared do not bind equally well to HS. Viruses such as Toto 1101 and R157H bind much better to BHK cells and will have a lower particle/PFU ratio than viruses such as K76E.
FIG. 4.
Serum titers. (A) CD-1 pups (2 days old) were infected subcutaneously with 1,000 PFU of virus, and serum titers were assessed at various times by a plaque assay (mean for three mice at each time point; error bars are not shown). All LP viruses retained their LP phenotype. A two-way analysis of variance showed a significant (P, <0.0001) effect of viral strain on titer, and titers of Toto 1101 were lower than those of all seven mutant viruses when compared by Scheffe's test (P, <0.05). (B) Plotting of peak titer (mean ± standard deviation) versus elution from heparin-Sepharose failed to indicate a simple correlation between virus replication in vivo and the strength of binding to heparin.
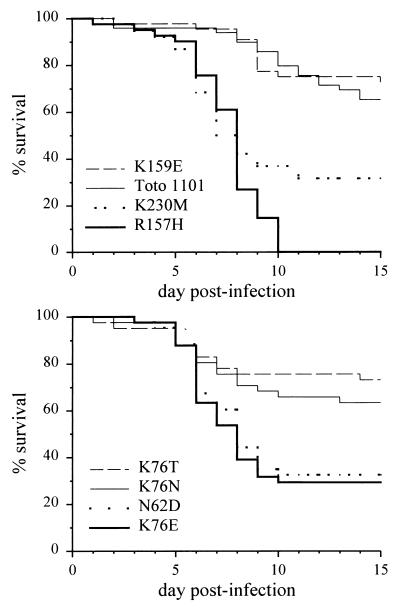
Four of the seven mutants (N62D, K76E, R157H, and K230M) produced significantly greater mortality than Toto 1101 when injected subcutaneously into 2-day-old mice (Fig. 5). The three remaining mutants (K76T, K76N, and K159E) had survival curves that were approximately similar to that of Toto 1101. Thus, even though all seven mutants produced significantly higher viremia than Toto 1101, only four caused significantly increased mortality.
FIG. 5.
Survival curves. Litters of 2-day-old CD-1 pups were infected subcutaneously with 1,000 PFU of virus, and survival was monitored for 15 days. R157H, K230M, N62D, and K76E produced significantly greater mortality than Toto 1101. Survival curves were compared pairwise against Toto 1101 by use of the log rank test with a threshold for significance (P) of <0.0071; the Bonferonni correction for multiple comparisons was used.
DISCUSSION
In this study, we derived a panel of viruses with different abilities to bind HS, both to define the HS-interacting regions of the SV glycoproteins and to find out how the ability to bind HS influences infection in vivo. Because the plaque size of SV is affected by interaction with sulfated polysaccharides in agar, we were able to easily screen for viruses with a reduced ability to bind HS. Low-HS-binding LP mutants arose spontaneously during infection in mice and had alterations scattered through a wide region of the E2 glycoprotein. Viruses with these changes in E2 were cleared more slowly from the blood, caused higher viremia, and often induced greater mortality.
Binding of E2 to HS.
In the absence of detailed structural information about the alphavirus E2 glycoprotein, it is difficult to demonstrate that any particular amino acid is part of a binding site for HS or even that the amino acid is exposed on the surface of the virion. The mutations described here could, for example, alter the tertiary structure of E2 and obscure an HS-binding site located elsewhere on E2 or E1. Nevertheless, four of the five mutated positions (K76, R157, K159, and K230) encode Lys or Arg. Because interactions between HS and proteins are primarily electrostatic and involve negatively charged sulfates binding to positively charged amino acids, these four residues have the potential to interact directly with HS. The remaining mutation in this study, N62D, did not involve the loss of a positively charged amino acid, but the gain of a negatively charged Asp might interfere with binding to HS by electrostatic repulsion.
It is likely that the Lys at position 76 directly participates in binding to HS, since replacing Lys 76 with negatively charged Glu resulted in poorer binding to heparin than was seen for viruses with either Asn or Thr at this position (Table 2). This result suggests that the charge of the amino acid at position 76 may be an important determinant of the strength of the interaction between E2 and heparin. An analogous mutation in VEE virus, changing the wild-type Glu 76 to Lys, results in an SP virus which replicates to lower titers in vivo and causes less mortality (7, 13).
Klimstra et al. have shown that mutations at additional E2 residues can alter the binding of SV to HS (32). Many strains of SV have a Lys at position 70 of E2, and changing this residue to Glu leads to a decreased ability to bind to HS. Also, substitution of an Arg for the Ser at position 114 results in an increase in binding to HS (32). The involvement of positively charged residues again suggests that these may contribute directly to binding of HS rather than indirectly by altering the tertiary structure of E2. In addition, although E3 is normally shed from the virion, the positively charged furin protease cleavage site at the C terminus of E3 can mediate binding to HS in cleavage-defective mutants when E3 remains attached to E2 (31).
It may appear odd that mutations over such a wide stretch of E2, spanning residues 62 to 230, can affect binding to HS, especially given that many HS-binding proteins have very short HS-binding sites containing clusters of Lys and Arg residues (15). However, HS-binding sites can also be formed when positively charged residues are brought into proximity in the tertiary or quaternary structure of a protein. Indeed, it has recently been shown that the HS-binding site on the surface of FMDV virions lies at the intersection of three different capsid proteins (11). Furthermore, the finding of a widely distributed HS-binding site on E2 is compatible with the fact that the E2c epitope is conformational and covers a large stretch of E2. Binding of MAb R6 to this epitope is affected by mutations in residues 62, 96, 114, and 159, which are distant from each other in the primary protein sequence but are likely to be located near each other in the three-dimensional folded structure of E2 (37, 39).
Viral behavior in vivo.
Although numerous viruses bind to HS and it is easy to show that this activity increases the efficiency of viral attachment to cultured cells, almost no studies have examined how binding to HS influences infection in vivo. Sa-Carvalho et al. have shown that variants of FMDV which bind well to HS are attenuated in cattle, showing a decreased ability to spread from the site of inoculation (43). We (4) and others (32) have proposed that the ability of SV to bind HS may cause attenuation in vivo in a similar manner.
Fortunately, a great deal is known about how HS-binding proteins behave in vivo. Pharmacokinetic studies on HS-binding proteins, such as bactericidal/permeability-increasing protein, extracellular-superoxide dismutase, and hepatocyte growth factor/scatter factor, have demonstrated rapid biphasic clearance from the circulation after intravenous injection (1, 14, 28). The biphasic decay can be modeled as the sum of two exponential equations (12). The early, rapid phase of clearance is strongly influenced by binding to HS; clearance during this phase can be decreased by coinjecting heparin (27, 52), digesting tissue HS with intravenous heparinase (25), or mutating basic residues so that the protein is no longer able to bind HS (14, 28). Because the liver contains large amounts of highly sulfated HS (35), a large percentage of the protein removed from the circulation can be found in this organ (2, 25, 27, 53, 55).
A number of investigations into the clearance of alphaviruses from the circulation were performed 20 to 30 years ago; these included studies on SV (40), western equine encephalitis virus (19), and VEE virus (20–22). All showed that SP variants were typically cleared faster after an intravenous injection than LP variants. One of these studies demonstrated the accumulation of VEE virus in the liver, with virions deposited in sinusoids and the spaces of Disse, as well as within vacuoles of Kupffer cells (20). Given what is now known about the clearance of HS-binding proteins from the circulation and given that plaque size can be a marker for the ability to bind HS, it seems likely that the differences in clearance rates in these studies were due to differences in viral binding to HS.
The seven mutant viruses in the present study all produced larger plaques under agar than the parental virus Toto 1101 and showed less binding to heparin and cellular HS. All of these mutants also were cleared more slowly from the circulation and caused higher viremia than Toto 1101. These findings together with what is known about the behavior of HS-binding proteins in vivo provide strong evidence that the ability to bind HS has a negative impact on SV production in vivo. It is interesting to note that, even though the viruses showed a broad range of ability to bind heparin and cellular HS, the plaque size and clearance from the circulation both showed threshold behavior—Toto 1101 had SPs and was cleared quickly from the circulation, but all of the LPs were approximately the same size, and all of the LP viruses were cleared at about the same relatively slow rate.
In addition to accelerated clearance, another mechanism which might prevent HS-binding viruses from achieving high viremia is interaction with HS in the extracellular matrix near the site of viral production. When extracellular-superoxide dismutase is injected subcutaneously or intramuscularly, it diffuses away from the injection site far more slowly than truncated variants of the enzyme which do not bind HS (29). The equilibrium amount of virus in the blood is a function of both the rate of release of new virus into the circulation and the rate of clearance, and both of these may be decreased if the virus can bind HS.
In spite of the fact that all seven mutant viruses produced significantly higher viremia than Toto 1101 after subcutaneous injection in suckling mice, only four caused significantly greater mortality, suggesting that high viremia may be only one of the factors necessary for high virulence. It should be noted that the K159E mutation, which did not increase virulence in our study, did cause increased virulence in another viral clone (39), so the background strain of the virus modulates the effects of these mutations as well.
Laboratory strains of SV have typically undergone multiple passages in tissue cultures. Klimstra et al. demonstrated that passaging of a low-HS-binding strain can quickly select for mutants with increased affinity for HS and proposed that wild-type strains of SV may not bind well to HS (32). Viruses which bind strongly to HS not only may have decreased virulence but also may have trouble achieving high enough viremia to allow transmission to mosquitoes. However, the R157H and N62D mutants in our study retained some ability to bind to HS on cultured cells and yet still caused high viremia and high mortality. Further study of unpassaged wild-type isolates will be required to determine how well natural strains of SV bind HS.
Relevance to other viruses.
The general conclusion that strong binding to a ubiquitous carbohydrate such as HS causes attenuation in vivo may apply only to viruses which cause plasma viremia and to instances in which viral spread through the circulation contributes to dissemination within the infected host. High viremia is also an important factor in transmission from host to host for insect-borne arboviruses, such as SV and dengue. In contrast, for viruses such as herpes simplex virus type 1, infection is spread primarily from cell to cell and strong binding to HS is not necessarily deleterious.
FMDV is a picornavirus that infects cattle. It causes viremia, and there is evidence that spread through the bloodstream is important in the dissemination of the virus within the animal (48). Wild-type isolates of FMDV do not bind to HS, but upon tissue culture passaging, SP variants with the ability to bind to HS arise (18, 43). HS-binding variants attach better to cultured cells but are attenuated in mice and cattle (24, 43), apparently because of a reduced ability to spread from the site of inoculation. After injection of cattle with very high doses of an attenuated HS-binding variant, disease and systemic dissemination of the virus can be seen but are due to the development of non-HS-binding LP revertants (43). Thus, the virus is under strong selective pressure to not bind HS during infection in vivo. A study of the clearance of virulent FMDV from the circulation has been done (47); we would predict that avirulent, HS-binding variants would be cleared considerably faster.
HIV-1 uses CD4 as a receptor and various chemokine receptors as coreceptors. During the early stages of infection, viruses typically use CCR5 as a coreceptor and infect monocytes. At the point of progression to AIDS, there is typically a switch, and T-cell-tropic viruses which use CXCR4 or both CXCR4 and CCR5 arise. Interestingly, only variants that use CXCR4 or both CXCR4 and CCR5 can bind well to HS, and this activity correlates with an increase in the positive charge in the V3 loop (3, 52). Studies on simian immunodeficiency virus and HIV-1 have found very rapid clearance of virus from the circulation following intravenous injection of virus into monkeys (17, 56). In order to obtain a complete understanding of the dynamics of viral behavior, it will be necessary to study whether clearance from the circulation is changed by the ability of some strains to bind HS.
Finally, viruses that bind to other ubiquitously present carbohydrates can also show attenuation in vivo if they bind too avidly. Murine polyomavirus binds to sialic acid but does not encode a neuraminidase like influenza virus. Polyomavirus SP variants bind better to cultured cells than LP variants because they attach more avidly to branched sialic-acid-containing oligosaccharides (5); the difference in plaque size is due to binding of sialylated oligosaccharides in the overlay, analogous to the effect of agar sulfated polysaccharides on SV. When virus is injected intraperitoneally, SP viruses cause more tumors in the peritoneum than in the kidney, while the distribution of tumors is reversed for LP viruses (8). This pattern is due to the fact that LP variants can cause widely disseminated infection, whereas SP variants cannot (9). Thus, there are multiple ways by which receptor binding influences the pathogenesis of viral infections in vivo.
ACKNOWLEDGMENTS
This work was supported by a postdoctoral fellowship from the National Multiple Sclerosis Society (to A.P.B.) and grant R01-NS18596 from the National Institutes of Health (to D.E.G.).
We thank Gwendolyn Binder and Karl Zheng for several of the viruses in this study.
REFERENCES
- 1.Abrahamson S L, Wu H-M, Williams R E, Der K, Ottah N, Little R, Gazzano-Santoro H, Theofan G, Bauer R, Leigh S, Orme A, Horwitz A H, Carroll S F, Dedrick R L. Biochemical characterization of recombinant fusions of lipopolysaccharide binding protein and bactericidal/permeability-increasing protein. J Biol Chem. 1997;272:2149–2155. doi: 10.1074/jbc.272.4.2149. [DOI] [PubMed] [Google Scholar]
- 2.Bauer R J, Der K, Ottah-Ihejeto N, Barrientos J, Kung A H C. The role of liver and kidney on the pharmacokinetics of a recombinant amino terminal fragment of bactericidal/permeability-increasing protein in rats. Pharm Res. 1997;14:224–229. doi: 10.1023/a:1012013113759. [DOI] [PubMed] [Google Scholar]
- 3.Bhattacharyya D, Brooks B R, Callahan L. Positioning of positively charged residues in the V3 loop correlates with HIV type 1 syncytium-inducing phenotype. AIDS Res Hum Retrovir. 1996;12:83–90. doi: 10.1089/aid.1996.12.83. [DOI] [PubMed] [Google Scholar]
- 4.Byrnes A P, Griffin D E. Binding of Sindbis virus to cell surface heparan sulfate. J Virol. 1998;72:7349–7356. doi: 10.1128/jvi.72.9.7349-7356.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cahan L D, Singh R, Paulson J C. Sialyloligosaccharide receptors of binding variants of polyoma virus. Virology. 1983;130:281–289. doi: 10.1016/0042-6822(83)90083-1. [DOI] [PubMed] [Google Scholar]
- 6.Chen Y, Maguire T, Hileman R E, Fromm J R, Esko J D, Linhardt R J, Marks R M. Dengue virus infectivity depends on envelope protein binding to target cell heparan sulfate. Nat Med. 1997;3:866–871. doi: 10.1038/nm0897-866. [DOI] [PubMed] [Google Scholar]
- 7.Davis N L, Powell N, Greenwald G F, Willis L V, Johnson B J B, Smith J F, Johnston R E. Attenuating mutations in the E2 glycoprotein gene of Venezuelan equine encephalitis virus: construction of single and multiple mutants in a full-length cDNA clone. Virology. 1991;183:20–31. doi: 10.1016/0042-6822(91)90114-q. [DOI] [PubMed] [Google Scholar]
- 8.Diamond L. Cell transformation in vitro and tumor induction in vivo by large- and small-plaque polyoma virus. Virology. 1964;23:73–80. doi: 10.1016/s0042-6822(64)80009-x. [DOI] [PubMed] [Google Scholar]
- 9.Dubensky T W, Freund R, Dawe C J, Benjamin T L. Polyomavirus replication in mice: influences of VP1 type and route of inoculation. J Virol. 1991;65:342–349. doi: 10.1128/jvi.65.1.342-349.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Esko J D, Stewart T E, Taylor W H. Animal cell mutants defective in glycosaminoglycan biosynthesis. Proc Natl Acad Sci USA. 1985;82:3197–3201. doi: 10.1073/pnas.82.10.3197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fry E E, Lea S M, Jackson T, Newman J W I, Ellard F M, Blakemore W E, Abu-Ghazaleh R, Samuel A, King A M Q, Stuart D I. The structure and function of a foot-and-mouth disease virus-oligosaccharide receptor complex. EMBO J. 1999;18:543–554. doi: 10.1093/emboj/18.3.543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gibaldi M, Perrier D. Pharmacokinetics. New York, N.Y: Marcel Dekker, Inc.; 1975. pp. 45–96. [Google Scholar]
- 13.Grieder F B, Davis N L, Aronson J F, Charles P C, Sellon D C, Suzuki K, Johnston R E. Specific restrictions in the progression of Venezuelan equine encephalitis virus-induced disease resulting from single amino acid changes in the glycoproteins. Virology. 1995;206:994–1006. doi: 10.1006/viro.1995.1022. [DOI] [PubMed] [Google Scholar]
- 14.Hartmann G, Prospero T, Brinkmann V, Ozcelik Ö, Winter G, Hepple J, Batley S, Bladt F, Sachs M, Birchmeier C, Birchmeier W, Gherardi E. Engineered mutants of HGF/SF with reduced binding to heparan sulphate proteoglycans, decreased clearance and enhanced activity in vivo. Curr Biol. 1998;8:125–134. doi: 10.1016/s0960-9822(98)70059-4. [DOI] [PubMed] [Google Scholar]
- 15.Hileman R E, Fromm J R, Weiler J M, Linhardt R J. Glycosaminoglycan-protein interactions: definition of consensus sites in glycosaminoglycan binding proteins. Bioessays. 1998;20:156–167. doi: 10.1002/(SICI)1521-1878(199802)20:2<156::AID-BIES8>3.0.CO;2-R. [DOI] [PubMed] [Google Scholar]
- 16.Hsiao J-C, Chung C-S, Chang W. Cell surface proteoglycans are necessary for A27L protein-mediated cell fusion: identification of the N-terminal region of A27L protein as the glycosaminoglycan-binding domain. J Virol. 1998;72:8374–8379. doi: 10.1128/jvi.72.10.8374-8379.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Igarashi T, Brown C, Azadegan A, Haigwood N, Dimitrov D, Martin M A, Shibata R. Human immunodeficiency virus type 1 neutralizing antibodies accelerate clearance of cell-free virions from blood plasma. Nat Med. 1999;5:211–216. doi: 10.1038/5576. [DOI] [PubMed] [Google Scholar]
- 18.Jackson T, Ellard F M, Abu Ghazaleh R, Brookes S M, Blakemore W E, Corteyn A H, Stuart D I, Newman J W I, King A M Q. Efficient infection of cells in culture by type O foot-and-mouth disease virus requires binding to cell surface heparan sulfate. J Virol. 1996;70:5282–5287. doi: 10.1128/jvi.70.8.5282-5287.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jahrling P B. Virulence heterogeneity of a predominantly avirulent western equine encephalitis virus population. J Gen Virol. 1976;32:121–128. doi: 10.1099/0022-1317-32-1-121. [DOI] [PubMed] [Google Scholar]
- 20.Jahrling P B, Gorelkin L. Selective clearance of a benign clone of Venezuelan equine encephalitis virus from hamster plasma by hepatic reticuloendothelial cells. J Infect Dis. 1975;132:667–676. doi: 10.1093/infdis/132.6.667. [DOI] [PubMed] [Google Scholar]
- 21.Jahrling P B, Hilmas D E, Heard C D. Vascular clearance of Venezuelan equine encephalomyelitis viruses as a correlate to virulence for rhesus monkeys. Arch Virol. 1977;55:161–164. doi: 10.1007/BF01314490. [DOI] [PubMed] [Google Scholar]
- 22.Jahrling P B, Scherer W F. Growth curves and clearance rates of virulent and benign Venezuelan encephalitis viruses in hamsters. Infect Immun. 1973;8:456–462. doi: 10.1128/iai.8.3.456-462.1973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jan J-T, Byrnes A P, Griffin D E. Characterization of a Chinese hamster ovary cell line developed by retroviral insertional mutagenesis that is resistant to Sindbis virus infection. J Virol. 1999;73:4919–4924. doi: 10.1128/jvi.73.6.4919-4924.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jensen M J, Moore D M. Phenotypic and functional characterization of mouse attenuated and virulent variants of foot-and-mouth disease virus type O1 Campos. Virology. 1993;193:604–613. doi: 10.1006/viro.1993.1168. [DOI] [PubMed] [Google Scholar]
- 25.Ji Z-S, Sanan D A, Mahley R W. Intravenous heparinase inhibits remnant lipoprotein clearance from the plasma and uptake by the liver: in vivo role of heparan sulfate proteoglycans. J Lipid Res. 1995;36:583–592. [PubMed] [Google Scholar]
- 26.Joyce J G, Tung J S, Przysiecki C T, Cook J C, Lehman E D, Sands J A, Jansen K U, Keller P M. The L1 major capsid protein of human papillomavirus type 11 recombinant virus-like particles interacts with heparin and cell-surface glycosaminoglycans on human keratinocytes. J Biol Chem. 1999;274:5810–5822. doi: 10.1074/jbc.274.9.5810. [DOI] [PubMed] [Google Scholar]
- 27.Karlsson K, Marklund S L. Plasma clearance of human extracellular-superoxide dismutase C in rabbits. J Clin Investig. 1988;82:762–766. doi: 10.1172/JCI113676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Karlsson K, Sandström J, Edlund A, Edlund T, Marklund S L. Pharmacokinetics of extracellular-superoxide dismutase in the vascular system. Free Rad Biol Med. 1993;14:185–190. doi: 10.1016/0891-5849(93)90009-j. [DOI] [PubMed] [Google Scholar]
- 29.Karlsson K, Sandström J, Edlund A, Marklund S L. Turnover of extracellular-superoxide dismutase in tissues. Lab Investig. 1994;70:705–710. [PubMed] [Google Scholar]
- 30.Kjellén L, Lindahl U. Proteoglycans: structures and interactions. Annu Rev Biochem. 1991;60:443–475. doi: 10.1146/annurev.bi.60.070191.002303. [DOI] [PubMed] [Google Scholar]
- 31.Klimstra W B, Heidner H W, Johnston R E. The furin protease cleavage recognition sequence of Sindbis virus PE2 can mediate virion attachment to cell surface heparan sulfate. J Virol. 1999;73:6299–6306. doi: 10.1128/jvi.73.8.6299-6306.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Klimstra W B, Ryman K D, Johnston R E. Adaptation of Sindbis virus to BHK cells selects for use of heparan sulfate as an attachment receptor. J Virol. 1998;72:7357–7366. doi: 10.1128/jvi.72.9.7357-7366.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Krusat T, Streckert H-J. Heparin-dependent attachment of respiratory syncytial virus (RSV) to host cells. Arch Virol. 1997;142:1247–1254. doi: 10.1007/s007050050156. [DOI] [PubMed] [Google Scholar]
- 34.Li M-L, Stollar V. A mutant of Sindbis virus which is released efficiently from cells maintained in low ionic strength medium. Virology. 1995;210:237–243. doi: 10.1006/viro.1995.1340. [DOI] [PubMed] [Google Scholar]
- 35.Lyon M, Deakin J A, Gallagher J T. Liver heparan sulfate structure: a novel molecular design. J Biol Chem. 1994;269:11208–11215. [PubMed] [Google Scholar]
- 36.Mendoza Q P, Stanley J, Griffin D E. Monoclonal antibodies to the E1 and E2 glycoproteins of Sindbis virus: definition of epitopes and efficiency of protection from fatal encephalitis. J Gen Virol. 1988;70:3015–3022. doi: 10.1099/0022-1317-69-12-3015. [DOI] [PubMed] [Google Scholar]
- 37.Olmsted R A, Meyer W J, Johnston R E. Characterization of Sindbis virus epitopes important for penetration in cell culture and pathogenesis in animals. Virology. 1986;148:245–254. doi: 10.1016/0042-6822(86)90322-3. [DOI] [PubMed] [Google Scholar]
- 38.Patel M, Yanagishita M, Roderiquez G, Bou-Habib D C, Oravecz T, Hascall B C, Norcross M A. Cell-surface heparan sulfate proteoglycan mediates HIV-1 infection of T-cell lines. AIDS Res Hum Retrovir. 1993;9:167–174. doi: 10.1089/aid.1993.9.167. [DOI] [PubMed] [Google Scholar]
- 39.Pence D F, Davis N L, Johnston R E. Antigenic and genetic characterization of Sindbis virus monoclonal antibody escape mutants which define a pathogenesis domain on glycoprotein E2. Virology. 1990;175:41–49. doi: 10.1016/0042-6822(90)90184-s. [DOI] [PubMed] [Google Scholar]
- 40.Postic B, Schleupner C J, Armstrong J A, Ho M. Two variants of Sindbis virus which differ in interferon induction and serum clearance. I. The phenomenon. J Infect Dis. 1969;120:339–347. doi: 10.1093/infdis/120.3.339. [DOI] [PubMed] [Google Scholar]
- 41.Rice C M, Levis R, Strauss J H, Huang H V. Production of infectious RNA transcripts from Sindbis virus cDNA clones: mapping of lethal mutations, rescue of a temperature-sensitive marker, and in vitro mutagenesis to generate defined mutants. J Virol. 1987;61:3809–3819. doi: 10.1128/jvi.61.12.3809-3819.1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Rostand K S, Esko J D. Microbial adherence to and invasion through proteoglycans. Infect Immun. 1997;65:1–8. doi: 10.1128/iai.65.1.1-8.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sa-Carvalho D, Rieder E, Baxt B, Rodarte R, Tanuri A, Mason P W. Tissue culture adaptation of foot-and-mouth disease virus selects viruses that bind to heparin and are attenuated in cattle. J Virol. 1997;71:5115–5123. doi: 10.1128/jvi.71.7.5115-5123.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Strauss J H, Strauss E G. The alphaviruses: gene expression, replication, and evolution. Microbiol Rev. 1994;58:491–562. doi: 10.1128/mr.58.3.491-562.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Stringer S E, Gallagher J T. Heparan sulphate. Int J Biochem Cell Biol. 1997;29:709–714. doi: 10.1016/s1357-2725(96)00170-7. [DOI] [PubMed] [Google Scholar]
- 46.Summerford C, Samulski R J. Membrane-associated heparan sulfate proteoglycan is a receptor for adeno-associated virus type 2 virions. J Virol. 1998;72:1438–1445. doi: 10.1128/jvi.72.2.1438-1445.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Sutmoller P, McVicar J W. Pathogenesis of foot-and-mouth disease: clearance of the virus from the circulation of cattle and goats during experimental viraemia. J Hyg. 1976;77:245–253. doi: 10.1017/s0022172400024670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Sutmoller P, McVicar J W. Pathogenesis of foot-and-mouth disease: the lung as an additional portal of entry of the virus. J Hyg. 1976;77:235–243. doi: 10.1017/s0022172400024669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Takemoto K K. Plaque mutants of animal viruses. Prog Med Virol. 1966;8:314–348. [PubMed] [Google Scholar]
- 50.Takemoto K K, Liebhaber H. Virus-polysaccharide interactions. I. An agar polysaccharide determining plaque morphology of EMC virus. Virology. 1961;14:456–462. doi: 10.1016/0042-6822(61)90338-5. [DOI] [PubMed] [Google Scholar]
- 51.Ubol S, Levine B, Lee S-H, Greenspan N S, Griffin D E. Roles of immunoglobulin valency and the heavy-chain constant domain in antibody-mediated downregulation of Sindbis virus replication in persistently infected neurons. J Virol. 1995;69:1990–1993. doi: 10.1128/jvi.69.3.1990-1993.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ugolini S, Mondor I, Sattentau Q J. HIV-1 attachment: another look. Trends Microbiol. 1999;7:144–149. doi: 10.1016/s0966-842x(99)01474-2. [DOI] [PubMed] [Google Scholar]
- 53.Wells M J, Blajchman M A. In vivo clearance of ternary complexes of vitronectin-thrombin-antithrombin is mediated by hepatic heparan sulfate proteoglycans. J Biol Chem. 1998;273:23440–23447. doi: 10.1074/jbc.273.36.23440. [DOI] [PubMed] [Google Scholar]
- 54.WuDunn D, Spear P G. Initial interaction of herpes simplex virus with cells is binding to heparan sulfate. J Virol. 1989;63:52–58. doi: 10.1128/jvi.63.1.52-58.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Yuge T, Furukawa A, Nakamura K, Nagashima Y, Shinozaki K, Nakamura T, Kimura R. Metabolism of the intravenously administered recombinant human basic fibroblast growth factor, trafermin, in liver and kidney: degradation implicated in its selective localization to the fenestrated type microvasculatures. Biol Pharm Bull. 1997;20:786–793. doi: 10.1248/bpb.20.786. [DOI] [PubMed] [Google Scholar]
- 56.Zhang L, Dailey P J, He T, Gettie A, Bonhoeffer S, Perelson A S, Ho D D. Rapid clearance of simian immunodeficiency virus particles from plasma of rhesus macaques. J Virol. 1999;73:855–860. doi: 10.1128/jvi.73.1.855-860.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]