In France mortality from ischaemic heart disease is about a quarter of that in Britain.1–7 The major risk factors are no more favourable in France, and this so called “French paradox” has not been satisfactorily explained. Table 1 shows the difference in mortality from heart disease between the countries, and table 2 shows the similar levels of animal fat consumption, serum total cholesterol and high density lipoprotein cholesterol concentrations, blood pressure, and (in men) smoking. The French paradox is usually attributed to the higher consumption of alcohol in France, notably of wine,2–5 and some have suggested a specific effect of red wine. In this article we assess quantitatively the extent to which this and other possible explanations can account for the low rate of heart disease in France. We then consider a novel “time lag” hypothesis, which, we believe, is the main explanation for the paradox.
Summary points
Mortality from ischaemic heart disease in France is about a quarter of that in Britain, but the major risk factors are similar
Undercertification of ischaemic heart disease in France could account for about 20% of the difference
The high consumption of alcohol in France, and of red wine in particular, explains little of the difference
We propose that the difference is due to the time lag between increases in consumption of animal fat and serum cholesterol concentrations and the resulting increase in mortality from heart disease—similar to the recognised time lag between smoking and lung cancer. Consumption of animal fat and serum cholesterol concentrations increased only recently in France but did so decades ago in Britain
Evidence supports this explanation: mortality from heart disease across countries, including France, correlates strongly with levels of animal fat consumption and serum cholesterol in the past (30 years ago) but only weakly to recent levels. Based on past levels, mortality data for France are not discrepant
Table 1.
Mortality (No of deaths/100 000) from ischaemic heart disease and poorly specified causes in people aged 55-64 in France and Britain in 19927 8
| Certified cause of death (ICD-9 code) | Men
|
Women
|
|||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| France |
Britain |
Difference |
Ratio |
France |
Britain |
Difference |
Ratio |
||||||||
| Ischaemic heart disease (410-4) | 128 | 487 | −359 | 1:4 | 27 | 153 | −126 | 1:6 | |||||||
| All poorly specified or unspecified causes: | 71 | 3 | 68 | 24:1 | 25 | 2 | 23 | 12:1 | |||||||
| Unspecified or unknown causes (799.9)* | 24 | 1 | 23 | 8 | 0.3 | 8 | |||||||||
| Poorly specified cardiac causes*: | 47 | 2 | 45 | 17 | 2 | 15 | |||||||||
| Ventricular or unspecified dysrhythmia (427.1, 427.4, 427.8, 427.9) | 6 | 1 | 2 | 1 | |||||||||||
| Cardiac arrest (427.5) | 9 | 0 | 3 | 0 | |||||||||||
| Heart failure (428) | 19 | 1 | 7 | 1 | |||||||||||
| Unspecified heart or cardiovascular disease (429.2, 429.9, 440.9) | 5 | 0 | 2 | 0 | |||||||||||
| Cardiogenic shock (785.5) | 3 | 0 | 1 | 0 | |||||||||||
| Sudden death (798.1) | 4 | 0 | 1 | 0 | |||||||||||
| Ischaemic heart disease plus poorly specified causes | 199 | 490 | −291 | 1:2.5 | 52 | 155 | −103 | 1:3 | |||||||
French data provided by Dr Françoise Hatton, INSERM.
Table 2.
Average values of risk factors for ischaemic heart disease in France and Britain, 1985-1990
| France | Britain | |
|---|---|---|
| National consumption data | ||
| No of cigarettes (per adult daily)9 | 6.4 | 6.5 |
| Animal fat (% of total energy intake)2 | 25.7 | 27.0 |
| Fruit and vegetables (% of total energy intake)2 | 5.0 | 4.3 |
| Survey data (age 50-70 years) | ||
| Percentage who smoked cigarettes9-13: | ||
| Men | 32 | 29 |
| Women | 9 | 30 |
| Mean serum total cholesterol concentration (mmol/l)12-19: | ||
| Men | 6.1 | 6.2 |
| Women | 6.5 | 6.7 |
| Mean high density lipoprotein cholesterol concentration (mmol/l)14-19: | ||
| Men | 1.3 | 1.3 |
| Women | 1.5 | 1.5 |
| Mean systolic blood pressure (mm Hg)12 13: | ||
| Men | 150 | 148 |
| Women | 149 | 148 |
This hypothesis arises from the observation that animal fat consumption and serum cholesterol concentration have been similar in France and Britain for a relatively short time—about 15 years. For decades up to 1970, France had lower animal fat consumption (about 21% of total energy consumption v 31% in Britain) and serum cholesterol (5.7 v 6.3 mmol/l), and only between 1970 and 1980 did French values increase to those in Britain.2,12–25 There must be a time lag between the increase in serum cholesterol concentration and the full effect of the resulting increase in coronary artery atheroma and risk of death from ischaemic heart disease. The observations that Western populations are exposed to high levels of dietary saturated fat and serum cholesterol from childhood, that atheroma progresses slowly throughout life, and that only about 1% of men die from ischaemic heart disease before the age of 509 suggest that decades of exposure must elapse. We propose that this is the main explanation for the low mortality from ischaemic heart disease in France. A similar time lag is recognised with smoking and lung cancer, in which it is the smoking habit of 30-40 years ago that is important in determining current risk,26 and a long incubation period for heart disease has been previously proposed.27
Previous explanations of the paradox
Undercertification of ischaemic heart disease
Not all deaths caused by ischaemic heart disease in France are classified as such; French doctors tend to certify some (such as those caused by heart failure and other late complications of myocardial infarction) as poorly specified causes.5,28 Table 1 shows that poor certification is important but can only partly explain the paradox. The excess attribution of deaths to poorly specified cardiac causes in France is equivalent to 12% of the difference in mortality from heart disease between France and Britain (45/359 in men and 15/126 in women), and to all poorly specified causes is equivalent to 19% (68/359 and 23/126).
Smoking
The prevalence of smoking in men is similar in France (32%) and Britain (29%), but in women it is lower in France (9% v 30%) (table 2). These patterns have persisted for over 30 years9 and are reflected in mortality from lung cancer (similar in French and British men but lower in French than British women7). The low prevalence of smoking in French women is consistent with the fact that the ratio of mortality from ischaemic heart disease in French to British women (1:3) is lower than the equivalent ratio in men (1:2.5) (table 1). Given that the risk of ischaemic heart disease in 55-64 year old smokers is twice that of non-smokers,29 the risk in French women ((2×9%)+(1×91%)) divided by that in British women ((2×30%)+(1×70%)) is 84%, and 84% of 1:3 (the ratio of mortality in French women to that in British women) is 1:2.5, the same as the ratio in men. The sex difference is explained, but not the residual mortality ratio of 1:2.5 in both sexes.
Alcohol
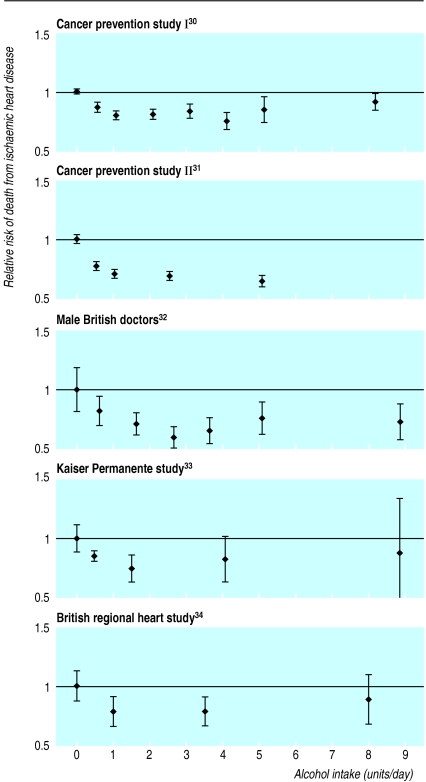
Figure 1 shows the relative risk of mortality from ischaemic heart disease according to alcohol consumption in the American Cancer Society’s cancer prevention study I (the largest cohort study in the world, with 18 771 deaths from ischaemic heart disease),30 cancer prevention study II (10 252 deaths from ischaemic heart disease),31 and in the three next largest cohort studies (recording 1061 deaths,32 940 deaths,33 and 611 events34). The studies show a consistent reduction in risk of about 20% in people who drink about one unit of alcohol a day than in people who drink none but, taken together, indicate that drinking more than about one unit a day confers little or no further protection. The data are consistent with a dose-response relation. The pattern is the same in men and women.31,33 This non-linear dose-response relation probably reflects a summation of opposing effects of alcohol: the protective effects (mainly the increase in serum concentration of high density lipoprotein cholesterol but also the favourable changes in haemostatic factors) are countered by the higher blood pressure, which increases risk.
Figure 1.
Relative risk (95% confidence interval) of death from ischaemic heart disease according to alcohol consumption (non-drinkers=1.0; one unit equivalent to a standard drink) in the five largest cohort studies.30–34 (Confidence intervals of relative risk estimates calculated from those of the corresponding absolute mortalities)
If all French men and no British men drank at least one unit of alcohol a day, other factors being equal, the difference in ischaemic heart disease would be about 20%. If half of British men drank at least one unit of alcohol daily the difference would be 10%, and if three quarters of British men did so it would be 5%. The last value approximates the current prevalence,10,12 but the difference in mortality from heart disease from differences in alcohol consumption will be even smaller than 5% because not all French men drink alcohol and because occasional alcohol consumption (<1 unit a day, more common in Britain) confers some protection. The greater alcohol consumption in France than Britain (18.4 v 5.7 litres of ethanol per adult in 1965, 13.1 v 8.5 in 19882) reflects a higher average consumption per drinker rather than a higher prevalence of drinkers and so does not further reduce the incidence of ischaemic heart disease.
A specific effect of wine
There is a strong association across countries between higher consumption of wine (but not beer or spirits) and lower mortality from ischaemic heart disease.2–5 This ecological association encouraged the view that the protective effect of alcohol was specific to wine. Wine consumption in France is high,2 and it was natural to invoke this as an explanation for the paradox. But epidemiological evidence shows that the protective effect of wine is no greater than that of beer or spirits.35–37 All alcoholic drinks produce the changes in serum high density lipoprotein cholesterol concentration and haemostatic factors that reduce risk,37–42 and randomised crossover studies have shown that ethanol produces them.41,42
A specific protective effect of red wine has been proposed on the basis that, in relation to its alcohol content, red wine contains more phenolic compounds (with antioxidant activity) than other drinks,43–45 although blood concentrations do not increase in proportion to dose.43 It also increases the proportion of polyunsaturated fatty acids in platelet phospholipids.46 But the evidence does not support an important role for either of these factors in the causation of ischaemic heart disease.45–47 One of the five large cohort studies cited above included people who drank only red wine or only white wine, and there was no difference in their risk of heart disease.36
Garlic and onions
The suggestion that consumption of garlic and onions could account for the low mortality from heart disease in France is based on ecological associations,1,48,49 and direct supportive evidence is lacking. Trials that suggested that garlic reduced serum cholesterol concentration had methodological flaws,50 and well designed trials have shown no effect.50,51
The time lag hypothesis
Evidence for the hypothesis
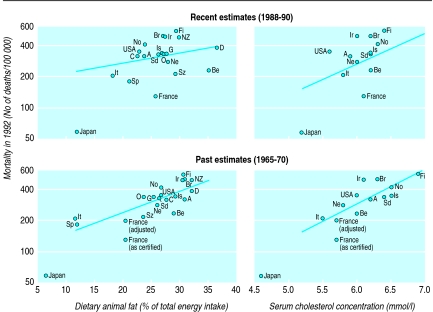
If there is a delay between an increase in serum cholesterol concentration and the resulting increase in mortality from ischaemic heart disease, current death rates from heart disease would relate to past levels of dietary fat and serum cholesterol better than to present day levels. Figure 2 shows current (1992) mortality from heart disease in men in 20 countries plotted against their recent (1988) and their past (1965) consumption of animal fat.2 Mortality from ischaemic heart disease was strongly associated with past animal fat consumption, accounting for 54% of the variance in mortality from heart disease between countries (r2=0.54, P<0.001), but this was not so for recent consumption (r2=0.07, P=0.28). The difference between past and recent consumption was highly significant (F116=21.8, P=0.003). Entering the data on past and recent consumption together in regression analysis did not predict mortality from heart disease better than did the past data alone. With the earlier data, the position of France is less discrepant from that of other countries, and after adjustment for the French undercertification of ischaemic heart disease it fits the overall trend well.
Figure 2.
Mortality from ischaemic heart disease in men aged 55-64 years in 1992 related to recent and past estimates of animal fat consumption and average serum cholesterol concentrations in 20 countries. Japan was omitted as an outlier in determining the regression lines. The position of France is shown with and without allowing for undercertification of ischaemic heart disease (see table 1). Table 3 shows data used in the graphs and the code for each country
Figure 2 also shows current (1992) mortality from ischaemic heart disease in men plotted against estimates of recent (about 1990) and past (about 1970) national average serum cholesterol concentrations in 13 countries (table 3 shows the sources of the estimates). As with animal fat consumption, mortality was strongly associated with past values (r2=0.55, P=0.006) but not with recent values (r2=0.08, P=0.36), use of both past values and recent values did not enhance prediction of heart disease mortality compared with using past data alone, and the difference between past and recent values was highly significant (F19=15.1, P=0.004). After adjustment for French undercertification of ischaemic heart disease, the position of France is not discrepant.
Table 3.
Mortality (No of deaths/100 000) from ischaemic heart disease in men aged 55-64 in 20 countries, with past and recent values of animal fat consumption, serum cholesterol concentration, and alcohol consumption
| Country | Mortality from ischaemic heart disease 19927 | Animal fat consumption (% of total energy intake)†
|
Mean serum cholesterol concentration (mmol/l) in men aged 50-70*
|
Alcohol consumption, 1988 (litres ethanol/ person)2 | |||
|---|---|---|---|---|---|---|---|
| 1965 | 1988 | 1970 | 1990 | ||||
| Japan22 52-54 |
58 |
6.6 | 11.9 | 4.6 | 5.2 | 6.0 | |
| France13-17 20 21 | 128 | 20.5 | 25.7 | 5.7 | 6.1 | 13.1 | |
| Spain (Sp) | 179 | 12.0 | 21.1 | 12.2 | |||
| Italy (It)17 22 55 56 | 204 | 11.7 | 18.2 | 5.5 | 5.8 | 10.2 | |
| Switzerland (Sz) | 211 | 23.6 | 29.1 | 11.1 | |||
| Belgium (Be)17 22 | 228‡ | 28.9 | 35.0 | 6.0 | 6.2 | 9.5 | |
| Netherlands (Ne)17 22 57 | 275 | 26.0 | 27.8 | 5.8 | 6.0 | 8.1 | |
| Canada (C) | 311 | 27.6 | 22.5 | 9.1 | |||
| Australia (A)22 58 | 311 | 30.8 | 23.7 | 6.2 | 5.9 | 9.2 | |
| West Germany (G) | 322 | 25.4 | 27.5 | 10.7 | |||
| Austria (O) | 328 | 23.7 | 27.1 | 11.3 | |||
| Sweden (Sd)22 59 60 | 329 | 26.5 | 26.2 | 6.4 | 6.2 | 5.6 | |
| Iceland (Is)22 | 333 | 29.3 | 26.8 | 6.5 | 6.2 | 3.5 | |
| United States (USA)22 | 345 | 26.7 | 22.8 | 5.9 | 5.6 | 7.2 | |
| Denmark (D) | 377 | 32.0 | 36.4 | 9.5 | |||
| Norway (No)17 22 61 62 | 405 | 26.7 | 23.8 | 6.5 | 6.3 | 4.4 | |
| New Zealand (NZ) | 476 | 32.1 | 29.7 | 9.6 | |||
| Ireland (Ir)22 63 | 482 | 30.4 | 27.3 | 6.1 | 5.9 | 7.1 | |
| Britain (Br)12 18 19 22 | 489 | 30.8 | 27.0 | 6.3 | 6.2 | 8.5 | |
| Finland (Fi)22 64-66 | 547 | 30.5 | 29.2 | 6.9 | 6.3 | 6.9 | |
Reference numbers after countries refer to sources of estimates of serum cholesterol concentration.
Derived from data from food balance sheets of United Nations Food and Agricultural Organisation.2 Although data were available, Israel was not included as data on fat consumption in 1965 may not apply to present population because of more recent immigration. ‡1989 mortality.
The regression line of past serum cholesterol concentration on ischaemic heart disease (fig 2) indicates that a decrease in serum cholesterol of 0.6 mmol/l is associated with a 37% lower mortality from ischaemic heart disease (95% confidence interval 18% to 52%), virtually identical to the estimate from the seven countries study.67 Serum cholesterol concentration in 1970 was 0.6 mmol/l lower in France than in Britain (5.7 v 6.3 mmol/l, table 3), and this explains most of its lower mortality from heart disease. It may seem surprising that the associations of heart disease with recent animal fat and cholesterol were so weak: they became significant when Japan (an outlier) was included in the analysis, but the relation with past values remained substantially stronger (for animal fat, F117=22.7, P<0.001; for serum cholesterol, F110=18.9, P=0.001). The associations were unaffected by including data on tobacco consumption9 and fruit and vegetable consumption2 as potential confounders.
Dietary confounding and the failure of the wine hypothesis
Wine consumption is associated with lower mortality from ischaemic heart disease across countries, as discussed above. Including wine with recent animal fat consumption in a multivariate analysis resulted in more of the variance in heart disease being explained, and this observation was interpreted as indicating a protective effect of wine.3,4 But in a multivariate analysis in which past animal fat consumption is used instead of recent consumption, wine consumption (past or recent) is no longer associated with mortality from heart disease and does not add to the variance explained. The association between wine and low ischaemic heart disease arose because wine consumption is associated across countries with the change in animal fat consumption from 1965 to 1988 (r2=0.46, P=0.001). Countries with high wine consumption are those in which saturated fat consumption used to be low but increased in recent years (France, Italy, Spain, and Switzerland, for example). The low mortality from ischaemic heart disease reflects the earlier low levels of saturated fat consumption, for which wine is simply an indirect marker—a confounding factor.
Duration of the time lag
The data in figure 2 indicate that the time lag between an increase in fat consumption and its maximal effect on heart disease risk is at least 25 years. It could be longer, but the analysis cannot be repeated with data from before 1965-70 as these are scanty and may be unreliable. The time lag could be as long as 35 years because this was the interval between the peak in the production of food of animal origin in Britain (which increased by two thirds between 1880 and 1936 but did not materially increase thereafter24,25) and the peak in mortality from ischaemic heart disease (which attained a plateau in 1971).
This slow increase in mortality from ischaemic heart disease after an increase in serum cholesterol concentration contrasts with the much more rapid decrease in mortality from ischaemic heart disease after a reduction in serum cholesterol. The randomised controlled trials of reducing serum cholesterol concentration show that the maximal reduction in mortality from heart disease is largely attained after about two years.67 Slow inception and rapid reversal are not inconsistent, and one should not be used to suggest that the other is incorrect. The relative risk of smoking related diseases also increases slowly after starting smoking but falls soon after stopping smoking.26
Possible contrary observations
Data on mortality from heart disease in France now cover a period of about 15 years since the increase in animal fat consumption. Some increase in heart disease in France relative to Britain might now be expected, but none is seen.7 No inference can be drawn, however, because, since 1980, mortality from heart disease has decreased by about half in all economically developed countries,7 largely due to the introduction of effective preventive treatments, and this effect is likely to dominate the effect of trends in risk factors. The treatments seem to have been used more extensively in France than in Britain: in 1993, 34% of survivors of infarcts in France took cholesterol lowering drugs compared with 4% of survivors in Britain, 63% took aspirin compared with 38%, 20% took anticoagulants compared with 5%, and 48% took β blockers compared with 20%.12,68 Also, a study suggests that serum cholesterol concentrations in France, having peaked in about 1980, may have subsequently decreased (by 0.4 mmol/l).69 The persistently low mortality from heart disease in France is therefore not surprising and does not refute the time lag hypothesis. Indeed, France is not unique in this; in Japan fat consumption and serum cholesterol concentration increased over the same period (fig 2), but heart disease has not.
The time lag hypothesis may help to explain the difference in heart disease between Britain and France but not the north-south difference across Britain, since dietary patterns in one part of the country relative to another have not materially changed over the past 40 years.22,25 This difference is likely to be due to the persistent differences between north and south in smoking and diet.70 In France the data are insufficient to determine whether the time lag hypothesis may partly explain its regional variations in heart disease. Britain is colder than France (by 2°C on average), but even if temperature were a causal factor it could explain little of the difference in heart disease either across each country or between the countries. The 20% excess winter mortality from heart disease in Britain (largely explained by higher concentration of clotting factors attributable to winter respiratory infections71) relates to an average temperature difference of 6°C,70 so the 2°C temperature difference would account for a difference in heart disease of only about 7%. This, and the small effect of its below average alcohol consumption, may help to explain why Britain has slightly higher than expected heart disease mortality in figure 2.
Public health implications
The time lag hypothesis, we believe, explains an interesting epidemiological paradox. But it is important to recognise that mortality from all causes in French men is similar to that in British men, despite their lower mortality from ischaemic heart disease (see table 4). The excess mortality from alcohol related causes is so large that it abolishes the survival advantage from the low mortality from heart disease, highlighting the public health problem from alcohol in French men. French women, in contrast, have done well: their mortality from all causes is a third lower than that in British women (table 4), a consequence of their moderate alcohol consumption, their diet, and their relatively low rate of smoking. Our paper has highlighted two important public health problems, the high mortality from heart disease in Britain and the high mortality from alcohol related causes in French men. Both are preventable.
Table 4.
Mortality (No of deaths/100 000) from alcohol related and other causes in people aged 55-64 in France and Britain, 19927 8
| Cause of death (ICD-9 code) | Men
|
Women
|
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| France† | Britain | Ratio | France† | Britain | Ratio | ||||||
| Alcohol related causes: | 348 | 105 | 3:1 | 82 | 40 | 2:1 | |||||
| Alcohol related cancers71: | |||||||||||
| Mouth and pharynx (140-149) | 56 | 11 | 5 | 4 | |||||||
| Oesophagus (150) | 44 | 28 | 4 | 9 | |||||||
| Liver (155.0) | 26 | 5 | 3 | 1 | |||||||
| Larynx (161) | 31 | 6 | 1 | 1 | |||||||
| Alcoholic dependence and alcoholic psychoses (291, 301)† | 20 | 1 | 4 | 0 | |||||||
| Cirrhosis of liver (571) | 72 | 19 | 27 | 11 | |||||||
| Motor vehicle accidents (E810-9) | 17 | 9 | 8 | 4 | |||||||
| Non-transport accidents (E880-E929) | 43 | 12 | 13 | 5 | |||||||
| Suicide (E950-9) | 39 | 14 | 17 | 5 | |||||||
| Ischaemic heart disease and poorly specified causes (from table 1) | 199 | 490 | 1:2.5 | 52 | 155 | 1:3 | |||||
| Lung cancer (162) | 184 | 161 | 1:1 | 18 | 74 | 1:4 | |||||
| All other causes | 631 | 618 | 1:1 | 365 | 543 | 1:1.5 | |||||
| All causes | 1362 | 1374 | 1:1 | 517 | 812 | 1:1.5 | |||||
French data provided by Dr Françoise Hatton, INSERM.
Acknowledgments
We thank Sir Christopher Paine who asked a question that prompted this work, Joan Morris for statistical assistance, Dr Françoise Hatton (INSERM) for providing unpublished data on French mortality, and Rory Collins and Leo Kinlen for their comments.
Footnotes
Funding: None.
Competing interest: None declared.
References
- 1.Tunstall-Pedoe H. Autres pays, autres moeurs: theories on why the French have less heart disease than the British. BMJ. 1988;297:1559–1560. doi: 10.1136/bmj.297.6663.1559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Criqui MH, Ringel BL. Does diet or alcohol explain the French paradox? Lancet. 1994;344:1719–1723. doi: 10.1016/s0140-6736(94)92883-5. [DOI] [PubMed] [Google Scholar]
- 3.Renaud S, De Lorgeril M. Wine, alcohol, platelets, and the French paradox for coronary heart disease. Lancet. 1992;339:1523–1526. doi: 10.1016/0140-6736(92)91277-f. [DOI] [PubMed] [Google Scholar]
- 4.Hegsted DM, Ausman LM. Diet, alcohol and coronary heart disease in men. J Nutr. 1988;118:1184–1189. doi: 10.1093/jn/118.10.1184. [DOI] [PubMed] [Google Scholar]
- 5.St Leger AS, Cochrane AL, Moore F. Factors associated with cardiac mortality in developed countries with particular reference to the consumption of wine. Lancet. 1979;i:1017–1020. doi: 10.1016/s0140-6736(79)92765-x. [DOI] [PubMed] [Google Scholar]
- 6.Artaud-Wild SM, Connor SL, Sexton G, Conner WE. Differences in coronary mortality can be explained by differences in cholesterol and saturated fat intakes in 40 countries but not in France and Finland. Circulation. 1993;88:2771–2779. doi: 10.1161/01.cir.88.6.2771. [DOI] [PubMed] [Google Scholar]
- 7.World Health Organisation. World health statistics annuals, 1985-95. Geneva: WHO; 1986-96. [Google Scholar]
- 8.Office of Population Censuses and Surveys. 1992 mortality statistics: cause. London: HMSO; 1993. [Google Scholar]
- 9.Nicolaides-Bouman A, Wald N, Forey B, Lee P. International smoking statistics. London, Oxford: Wolfson Institute of Preventive Medicine, Oxford University Press; 1993. [Google Scholar]
- 10.Office of Population Censuses and Surveys. Social survey division. Living in Britain: results from the 1994 general household survey. London: HMSO; 1996. [Google Scholar]
- 11.Wald N, Nicolaides-Bouman A. UK smoking statistics. London, Oxford: Wolfson Institute of Preventive Medicine, Oxford University Press; 1991. [Google Scholar]
- 12.Office of Population Censuses and Surveys Social Survey Division. Health survey for England 1991-3. London: HMSO; 1993-5. [Google Scholar]
- 13.World Health Organisation. The WHO MONICA project: a worldwide monitoring system for cardiovascular diseases. World health statistics annual 1989. Geneva: WHO; 1990. [Google Scholar]
- 14.Schlienger JL, Simon C, Aby MA, Arveiler D, Schaffer P. Bilan lipidique dans une population adulte representative d’une region Francaise (Bas-Rhin) Pathol Biol. 1991;39:195–199. [PubMed] [Google Scholar]
- 15.Laurier D, Chau NP, Segond P PCV-Metra Group. Cholesterol and other cardiovascular risk factors in a working population in Ile-de-France (France): first results of the PCV-Metra study. Eur J Epidemiol. 1992;8:693–701. doi: 10.1007/BF00145386. [DOI] [PubMed] [Google Scholar]
- 16.Bonithon-Kopp C, Levenson J, Scarabin P, Guillanneuf M, Kirzin J, Malmejac A, et al. Longitudinal associations between plasma viscosity and cardiovascular risk factors in a middle-aged French population. Atherosclerosis. 1993;104:173–182. doi: 10.1016/0021-9150(93)90188-z. [DOI] [PubMed] [Google Scholar]
- 17.SENECA investigators. Nutritional status: serum lipids. Eur J Clin Nutr. 1991;45(suppl 3):53–61. [PubMed] [Google Scholar]
- 18.Office of Population Censuses and Surveys Social Survey Division. The dietary and nutritional survey of British adults. London: HMSO; 1990. [Google Scholar]
- 19.Mann JI, Lewis B, Shepherd J, Winder AF, Fenster S, Rose L, et al. Blood lipid concentrations and other cardiovascular risk factors: distribution, prevalence, and detection in Britain. BMJ. 1988;296:1702–1706. doi: 10.1136/bmj.296.6638.1702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cambien F, Ducimetiere P, Richard J. Total serum cholesterol and cancer mortality in a middle-aged male population. Am J Epidemiol. 1980;112:388–394. doi: 10.1093/oxfordjournals.aje.a113004. [DOI] [PubMed] [Google Scholar]
- 21.Malaspina JP, Bussière H, Le Calve G. The total cholesterol/HDL cholesterol ratio: a suitable atherogenesis index. Atherosclerosis. 1981;40:373–375. doi: 10.1016/0021-9150(81)90149-0. [DOI] [PubMed] [Google Scholar]
- 22.Law MR, Wald NJ. An ecological study of serum cholesterol and ischaemic heart disease between 1950 and 1990. Eur J Clin Nutr. 1994;48:305–325. [PubMed] [Google Scholar]
- 23.Jolliffe N, Archer M. Statistical associations between international coronary heart disease death rates and certain environmental factors. J Chronic Dis. 1959;9:636–652. doi: 10.1016/0021-9681(59)90114-6. [DOI] [PubMed] [Google Scholar]
- 24.Hollingsworth D. The application of the newer knowledge of nutrition. In: Drummond JC, Wilbraham A, editors. The Englishman’s food. London: Jonathan Cape; 1957. (Reissued by Pimlico, 1991.) [Google Scholar]
- 25.Ministry of Agriculture Fisheries and Food. Household food consumption and expenditure, 1954, 1960, 1970 and 1980. London: HMSO 1956, 1962, 1973, and 1982.
- 26.Doll R, Peto R. The causes of cancer: appendix E. J Natl Cancer Inst. 1981;66:1292–1305. [PubMed] [Google Scholar]
- 27.Rose G. Incubation period of coronary heart disease. BMJ. 1982;284:1600–1601. doi: 10.1136/bmj.284.6329.1600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.McMichael J. French wine and death certificates. Lancet. 1979;i:1186–1187. doi: 10.1016/s0140-6736(79)91862-2. [DOI] [PubMed] [Google Scholar]
- 29.Doll R, Peto R. Mortality in relation to smoking: 20 years’ observations on male British doctors. BMJ. 1976;ii:1525–1536. doi: 10.1136/bmj.2.6051.1525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Boffetta P, Garfinkel L. Alcohol drinking and mortality among men enrolled in an American Cancer Society prospective study. Epidemiology. 1990;1:342–348. doi: 10.1097/00001648-199009000-00003. [DOI] [PubMed] [Google Scholar]
- 31.Thun MJ, Peto R, Lopez AD, Monaco JH, Henley J, Heath CW, et al. Alcohol consumption and mortality among middle-aged and elderly US adults. N Engl J Med. 1997;24:1705–1714. doi: 10.1056/NEJM199712113372401. [DOI] [PubMed] [Google Scholar]
- 32.Doll R, Peto R, Hall E, Wheatley K, Gray R. Mortality in relation to consumption of alcohol: 13 years’ observations on male British doctors. BMJ. 1994;309:911–918. doi: 10.1136/bmj.309.6959.911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Klatsky AL, Armstrong MA, Friedman GD. Alcohol and mortality. Ann Intern Med. 1992;117:646–654. doi: 10.7326/0003-4819-117-8-646. [DOI] [PubMed] [Google Scholar]
- 34.Shaper AG, Wannamethee G, Walker M. Alcohol and coronary heart disease: a perspective from the British regional heart study. Int J Epidemiol. 1994;23:482–494. doi: 10.1093/ije/23.3.482. [DOI] [PubMed] [Google Scholar]
- 35.Rimm EB, Klatsky A, Grobbee D, Stampfer MJ. Review of moderate alcohol consumption and reduced risk of coronary heart disease: is the effect due to beer, wine, or spirits? BMJ. 1996;312:731–736. doi: 10.1136/bmj.312.7033.731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Klatsky AL, Armstrong MA, Friedman GD. Red wine, white wine, liquor, beer, and risk for coronary artery disease hospitalization. Am J Cardiol. 1997;80:416–420. doi: 10.1016/s0002-9149(97)00388-3. [DOI] [PubMed] [Google Scholar]
- 37.Marques-Vidal P, Ducimetière P, Evans A, Cambou J, Arveiler D. Alcohol consumption and myocardial infarction: a case-control study in France and Northern Ireland. Am J Epidemiol. 1996;143:1089–1093. doi: 10.1093/oxfordjournals.aje.a008683. [DOI] [PubMed] [Google Scholar]
- 38.Gaziano JM, Buring JE, Breslow JL, Goldhaber SZ, Rossner B, VanDenburgh M, et al. Moderate alcohol intake, increased levels of high-density lipoprotein and its subfractions, and decreased risk of myocardial infarction. N Engl J Med. 1993;329:1829–1834. doi: 10.1056/NEJM199312163292501. [DOI] [PubMed] [Google Scholar]
- 39.Suh I, Shaten J, Cutler A, Kuller L. Alcohol use and mortality from coronary heart disease: the role of high-density lipoprotein cholesterol. Ann Intern Med. 1992;116:881–887. doi: 10.7326/0003-4819-116-11-881. [DOI] [PubMed] [Google Scholar]
- 40.Hendriks HFJ, Veenstra J, Velthuis-te Wierik EJM, Schaafsma G, Kluft C. Effect of moderate dose of alcohol with evening meal on fibrinolytic factors. BMJ. 1994;308:1003–1006. doi: 10.1136/bmj.308.6935.1003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Forman MR, Beecher GR, Lanza E, Reichman ME, Graubard BI, Campbell WS, et al. Effect of alcohol consumption on plasma carotenoid concentrations in premenopausal women: a controlled dietary study. Am J Clin Nutr. 1995;62:131–135. doi: 10.1093/ajcn/62.1.131. [DOI] [PubMed] [Google Scholar]
- 42.Pellegrini N, Pareti FI, Stabile F, Brusamolino A, Simonetti P. Effects of moderate consumption of red wine on platelet aggregation and haemostatic variables in healthy volunteers. Eur J Clin Nutr. 1996;50:209–213. [PubMed] [Google Scholar]
- 43.Duthie GG, Pedersen MW, Gardner PT, Morrice PC, Jenkinson AM, McPhail DB, et al. The effect of whisky and wine consumption on total phenol content and antioxidant capacity of plasma from healthy volunteers. Eur J Clin Nutr. 1998;52:733–736. doi: 10.1038/sj.ejcn.1600635. [DOI] [PubMed] [Google Scholar]
- 44.Frankel EN, Kanner J, German JB, Parks E, Kinsella JE. Inhibition of oxidation of human low-density lipoprotein by phenolic substances in red wine. Lancet. 1993;341:454–457. doi: 10.1016/0140-6736(93)90206-v. [DOI] [PubMed] [Google Scholar]
- 45.Hertog MGL, Hollman PCH. Potential health effects of the dietary flavonol quercetin. Eur J Clin Nutr. 1996;50:63–71. [PubMed] [Google Scholar]
- 46.Pellegrini N, Simonetti P, Brusamolino A, Bottasso B, Pareti FI. Composition of platelet phospholipids after moderate consumption of red wine in healthy volunteers. Eur J Clin Nutr. 1996;50:535–541. [PubMed] [Google Scholar]
- 47.Muldoon MF, Kritchevsky SB. Flavonoids and heart disease. BMJ. 1996;312:458–459. doi: 10.1136/bmj.312.7029.458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Keys A. Wine, garlic, and CHD in seven countries. Lancet. 1980;i:145–146. doi: 10.1016/s0140-6736(80)90620-0. [DOI] [PubMed] [Google Scholar]
- 49.Buck C, Donner AP, Simpson H. Garlic, oil and ischaemic heart disease. Int J Epidemiol. 1982;11:294–295. [PubMed] [Google Scholar]
- 50.Neil HAW, Silagy CA, Lancaster T, Hodgeman J, Vos K, Moore JW, et al. Garlic powder in the treatment of moderate hyperlipidaemia: a controlled trial and meta-analysis. J R Coll Physicians Lond. 1996;30:329–333. [PMC free article] [PubMed] [Google Scholar]
- 51.Simons LA, Balasubramaniam S, von Konigsmark M, Parfitt A, Simons J, Peters W. On the effect of garlic on plasma lipids and lipoproteins in mild hypercholesterolaemia. Atherosclerosis. 1995;113:219–225. doi: 10.1016/0021-9150(94)05449-s. [DOI] [PubMed] [Google Scholar]
- 52.Okayama A, Ueshima H, Marmot MG, Elliott P, Yamakawa M, Kita Y. Different trends in serum cholesterol levels among rural and urban populations aged 40-59 in Japan from 1960-1990. J Clin Epidemiol. 1995;48:329–337. doi: 10.1016/0895-4356(94)00146-h. [DOI] [PubMed] [Google Scholar]
- 53.Kuzuya F, Shimokata H. Longitudinal changes in plasma cholesterol and triglyceride levels in Japanese male workers, 1977-1992. Ann N Y Acad Sci. 1995;748:510–513. doi: 10.1111/j.1749-6632.1994.tb17350.x. [DOI] [PubMed] [Google Scholar]
- 54.Research Committee on Serum Lipid Level Survey 1990 in Japan. Current state of and recent trends in serum lipid levels in the general Japanese population. J Atherosclerosis Thromb. 1996;2:122–133. doi: 10.5551/jat1994.2.122. [DOI] [PubMed] [Google Scholar]
- 55.Pujia A, Gnasso A, Cortese C, Angotti E, Colonna A, Mattioli PL. Early extracoronary atherosclerosis and coronary heart disease risk factors in a sample of civil servants in southern Italy. Atherosclerosis. 1993;102:1–7. doi: 10.1016/0021-9150(93)90079-a. [DOI] [PubMed] [Google Scholar]
- 56.Vaccarino V, Borgatta A, Gallus G, Sirtori CR. Prevalence of coronary heart disease risk factors in northern-Italian male and female employees. Eur Heart J. 1995;16:761–769. doi: 10.1093/oxfordjournals.eurheartj.a060994. [DOI] [PubMed] [Google Scholar]
- 57.Verschuren WMM, Boerma GJM, Kromhout D. Total and HDL-cholesterol in the Netherlands: 1987-1992. Int J Epidemiol. 1994;23:948–956. doi: 10.1093/ije/23.5.948. [DOI] [PubMed] [Google Scholar]
- 58.Bennett SA, Magnus P. Trends in cardiovascular risk factors in Australia. Med J Aust. 1994;161:519–527. [PubMed] [Google Scholar]
- 59.Arnetz BB, Kallner A. Epidemiological assessment of hyperlipidaemia management in primary health care. Eur J Public Health. 1994;4:38–45. [Google Scholar]
- 60.Lindeberg S, Nilsson-Ehle P, Terént A, Vessby B, Scherstén B. Cardiovascular risk factors in a Melanesian population apparently free from stroke and ischaemic heart disease: the Kitava study. J Intern Med. 1994;236:331–340. doi: 10.1111/j.1365-2796.1994.tb00804.x. [DOI] [PubMed] [Google Scholar]
- 61.Fonnebo V. Coronary risk factors in Norwegian seventh-day adventists: a study of 247 seventh-day adventists and matched controls. Am J Epidemiol. 1992;135:504–508. doi: 10.1093/oxfordjournals.aje.a116317. [DOI] [PubMed] [Google Scholar]
- 62.Jacobsen BK, Stensvold I, Fylkesnes K, Kristiansen IS, Thelle DS. The Norland health study. Scand J Soc Med. 1992;20:184–187. doi: 10.1177/140349489202000309. [DOI] [PubMed] [Google Scholar]
- 63.Shelley E, Daly L, Collins C, Christie M, Conroy R, Gibney M, et al. Cardiovascular risk factor changes in the Kilkenny health project. Eur Heart J. 1995;16:752–760. doi: 10.1093/oxfordjournals.eurheartj.a060993. [DOI] [PubMed] [Google Scholar]
- 64.Strandberg TE, Salomaa VV, Vanhanen HT, Naukkarinen VA, Sarna SJ, Miettinen TA. Mortality in participants and non-participants of a multifactorial prevention study of cardiovascular diseases: a 28 year follow up of the Helsinki businessmen study. Br Heart J. 1995;74:449–454. doi: 10.1136/hrt.74.4.449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Vartiainen E, Puska P, Jousilahti P, Korhonen HJ, Tuomilehto J, Nissinen A. Twenty-year trends in coronary risk factors in North Karelia and in other areas of Finland. Int J Epidemiol. 1994;23:495–504. doi: 10.1093/ije/23.3.495. [DOI] [PubMed] [Google Scholar]
- 66.Pekkanen J, Uutela A, Valkonen T, Vartiainen E, Tuomilehto J, Puska P. Coronary risk factor levels: differences between educational groups in 1972-87 in eastern Finland. J Epidemiol Community Health. 1995;49:144–149. doi: 10.1136/jech.49.2.144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Law MR, Wald NJ, Thompson SG. By how much and how quickly does reduction in serum cholesterol concentration lower risk of ischaemic heart disease. BMJ. 1994;308:367–372. doi: 10.1136/bmj.308.6925.367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.De Lorgeril M, Salen P, Caillat-Vallet E, Hanauer M-T, Barthelemy JC, Mamelle N. Control of bias in dietary trial to prevent coronary recurrences: the Lyon diet heart study. Eur J Clin Nutr. 1997;51:116–122. doi: 10.1038/sj.ejcn.1600374. [DOI] [PubMed] [Google Scholar]
- 69.SENECA Investigators. Longitudinal changes in serum lipids of elderly Europeans. Eur J Clin Nutr. 1996;50:S25–S31. [PubMed] [Google Scholar]
- 70.Law MR, Morris JK. Why is mortality higher in poorer areas and in more northern areas of England and Wales? J Epidemiol Community Health. 1998;52:344–352. doi: 10.1136/jech.52.6.344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Woodhouse PR, Khaw KT, Plummer M, Foley A, Meade TW. Seasonal variations of plasma fibrinogen and factor VII activity in the elderly: winter infections and death from cardiovascular disease. Lancet. 1994;343:435–439. doi: 10.1016/s0140-6736(94)92689-1. [DOI] [PubMed] [Google Scholar]
- 72.Blot WJ. Alcohol and cancer. Cancer Res. 1992;52(suppl):2119–223S. [PubMed] [Google Scholar]