Abstract
Background
The Malaysian healthcare system is under strain due to an aging population, the rising prevalence of chronic diseases, and heavy workloads among physicians. As costs and requirements continue to rise, telemedicine is critical for bridging gaps in supply and demand. However, there are limited studies on telemedicine adoption among Malaysian physicians. Furthermore, the existing literature on telemedicine adoption does not contain a comprehensive framework that integrates the multidimensional social influence, and technological, clinical, and individual factors.
Objective
This research investigates the adoption of telemedicine among Malaysian physicians. It draws from the Technology Acceptance Model (TAM) and Kelman's Social Influence Theory.
Methods
A survey was conducted among 230 participants in hospitals located in Kuala Lumpur and Selangor. The data were analyzed using Partial Least Squares Structural Equation Modeling (PLS-SEM).
Results
The study identified crucial factors influencing telemedicine adoption, including informational influences, rewards, perceived ease of use, and usefulness. Meanwhile, the Importance-performance Map Analysis (IPMA) identified perceived ease of use as the most important factor for physicians, but the highest performance was patient’s records.
Conclusions
The proposed integrated model enhances the understanding of telemedicine adoption and highlights the differential effects of individual, technological, clinical, and multidimensional social influence factors from the physicians’ perspective. The findings can guide future studies and influence implementation strategies for telemedicine promotion in the Malaysian healthcare context. Hospitals should prioritize user-friendly technology and information provision, while telemedicine providers should enhance the accessibility of patient records to facilitate telemedicine adoption. Policymakers should consider supporting training programs that will boost physicians’ confidence in effectively utilizing telemedicine.
Keywords: Telemedicine , physicians, adoption, TAM, quantitative , social influence theory, Malaysia, behavior
Introduction
Healthcare is more than just about individual well-being; it is a fundamental pillar upon which the prosperity and stability of nations are built. 1 According to the World Health Organization, 2 global spending on healthcare has doubled in real terms over the past two decades, reaching USD 9 trillion and 10.8% of GDP in 2020 (an increase from 8.5% in 2000). Demographic shifts, which include aging populations and an increased prevalence of chronic diseases, place an ever-growing burden on healthcare systems. In this era of burgeoning healthcare needs and costs, telemedicine has garnered significant global attention. As a transformative paradigm in healthcare, telemedicine is not only a driver of expenses but also a solution for the widening the gap between healthcare supply and demand.
Telemedicine is the utilization of telecommunications technology and digital platforms for healthcare providers to remotely provide medical services, consultation, diagnosis, treatment, and health-related information to patients. This innovative approach transcends geographical boundaries by allowing patients to conveniently access healthcare services regardless of their physical location. 3 However, telemedicine adoption within the global healthcare community was relatively sluggish before the COVID-19 pandemic. This is primarily because it was considered an alternative rather than a mainstream method of healthcare delivery. 4 However, healthcare provision underwent significant changes in 2021, and telemedicine usage skyrocketed by a remarkable sixfold compared to 2019, particularly in larger healthcare settings such as community health centers and academic medical institutions. 5
In Malaysia, the use of telemedicine in the healthcare system is gaining increasing importance. Based on data from the Department of Statistics Malaysia, the country's aging population is expected to surpass 15% of the total population by 2030; this will cause an influx of older individuals and those with chronic diseases into the primary care system. This trend will significantly burden the healthcare system in Malaysia. 6 The Malaysian healthcare system has two tiers: a government-subsidized public sector and a fee-for-service private sector. The public sector offers comprehensive and affordable care through primary healthcare facilities linked to specialized hospitals, while the private sector caters to wealthier individuals who can afford higher fees. Even though Malaysia's mixed public-private healthcare system ensures tangible accessibility, its healthcare workforce does not adequately meet the rising healthcare demands of the country. 7
According to the Ministry of Health Malaysia, 8 there are currently 2.4 doctors per 1000 population in Malaysia. While this figure is higher than that of neighboring countries such as Thailand and Vietnam, it is lower than Singapore, Japan, and Australia. In primary care, the per capita density of physicians is 1.5 per 1000 population in urban areas and 1.1 per 1000 population in rural areas. 9 This disparity, coupled with a substantial increase in patient visits in the public sector, has led to overloaded clinics that cause congestion and exceed physician capacity.6,9 In summary, the aging population, the increased prevalence of chronic diseases, and the heavy physician workload have placed a growing burden on Malaysia's healthcare systems. Telemedicine is a crucial solution that could bridge the widening gap between healthcare supply and demand amidst escalating healthcare needs and costs. 10
Telemedicine has made significant strides in Malaysia, with the government launching its first telemedicine blueprint in 1997 as part of the Multimedia Super Corridor Project. 11 This initiative aimed to employ the use of telemedicine in the country's healthcare system. In 2019, Malaysia's Ministry of Health (MOH) launched a teleconsultation pilot using video consultation technologies at five public primary care clinics to enhance healthcare accessibility and alleviate congestion at these clinics. 12 In line with global trends, telemedicine use also increased during the COVID-19 pandemic. By the end of 2020, telemedicine services had expanded to cover 35 additional public primary care clinics, with many other clinics also proactively initiating teleconsultation in response to the crisis. 11 This growth was driven by the need to provide healthcare services while minimizing the risk of virus transmission and maximizing the potential to improve research, disease control, and clinical management. 13
In recent years, there has been a noticeable trend of increasing global studies examining telemedicine adoption. Many of these studies commonly utilize technology acceptance models, such as TAM or Unified Theory of Acceptance and Use of Technology (UTAUT), to evaluate telemedicine adoption. 14–21 Nevertheless, studies have criticized solely relying on the TAM and UTAUT models to explain technology adoption.22,23 For instance, researchers argue that the functional and utilitarian benefits proposed in TAM, such as perceived ease of use, do not sufficiently explain consumer technology acceptance. 24 In addition, recent studies like those by Cobelli et al. 14 and Vidal-Silva et al. 15 heavily emphasize compliance aspects of subjective norms within the UTAUT framework, but they overlook the critical process of identification and internalization aspects in social influence. 25 Thus, there is a call to expand the focus beyond mere compliance-based social influence, as this tends to diminish in impact over time with increased individual experience.
Despite the recent surge in telemedicine adoption studies, there remains a dearth of literature concerning telemedicine adoption from the physician's perspective, especially in developing Southeast Asian countries like Malaysia. Accordingly, Pereira et al. (2023) emphasized the need for future research to investigate telemedicine adoption from the perspective of physicians. While telemedicine can minimize contact with sick patients and reduce the transmission of microbes, 26 its increased and evolving use has raised challenges and limitations that can strain healthcare providers. Therefore, understanding the physician’s perspective on telemedicine adoption is crucial, as the acceptance of telemedicine by physicians is a major barrier preventing its effective implementation in the healthcare system.13,27–30
Therefore, the objective of this study is to investigate the adoption of telemedicine among doctors and physicians in Malaysia by employing a combined approach of the Technology Acceptance Model 31 and Kelman's Social Influence Theory. 32 This dual-theory approach integrates the elements of successful technology adoption from TAM with the multidimensional social and clinical factors that could influence telemedicine adoption among physicians. 22 By amalgamating these theories, the study aims to provide a comprehensive understanding of the factors that shape healthcare professionals’ and physicians’ perspectives on the proposed application of telemedicine. It also aims to offer a holistic view that acknowledges both technological feasibility and the human aspects of healthcare delivery. The study's findings will be essential in influencing telemedicine implementation in Malaysia, as it will aid the Ministry of Health's efforts in planning and driving increased adoption among physicians in Malaysian hospitals.
Literature review and theoretical background
It has become imperative for both scholars and practitioners to understand the factors influencing telemedicine adoption. To address this, researchers have proposed several theoretical models to elucidate the complexities of telemedicine acceptance. Commonly utilized models include UTAUT, UTAUT2, and TAM. For example, studies that have employed these models include those by Cobelli et al.,14,33 Klingberg et al., 34 Vidal-Silva et al., 15 Kabra and Songroya, 17 Schmitz et al., 35 Ong et al., 1 Arfi et al., 36 Rajak and Shaw, 37 and Yamin and Alyoubi. 38 Other commonly adopted models include the behavioral model, 39 the theory of planned behavior, 40 the Unified Model of e-Government Adoption (UMEGA), 41 the social cognitive theory, 21 and the value-based adoption model. 19 However, some studies20,42 have opted to use relevant variables from existing research without adhering to specific theories or models. Additionally, some studies have used combined models16,18,38,43 to predict telemedicine adoption, demonstrating the continued relevance and applicability of established theoretical frameworks in contemporary research. These approaches are aligned with Hubona and Geitz, 44 who observed that revising the existing models with external variables can influence the proportions of usage frequency and usage amount variances. The discussed papers above published from 2020 to 2024 are summarized in Table 1, which showcases the utilization of various popularly used adoption models.
Table 1.
Summary of literature reports on telemedicine adoption from 2020–2024.
| Item | Author | Year | Country | Theory/Model | Subject | Technology studied/ Platform | Findings (Factors influencing the adoption) |
Limitation |
|---|---|---|---|---|---|---|---|---|
| 1. | Cobelli et al. 14 | 2024 | Italy | UTAUT, self-determination theory, and social identity theory. | Pharmacists | E-health | Performance expectancy, effort expectation and social influence. | - Self-selection bias. - Cultural differences. |
| 2. | Vidal-Silva et al. 15 | 2024 | Chili | UTAUT2 | Not specific | Telemedicine | Performance expectancy, social influence, and price value | - Data was collected from individual who have internet access (Not patient/users/physician) |
| 3. | Lu et al. 18 | 2024 | China | TAM & Health Belief Model | General population | Telemedicine | Perceived usefulness, trust, social influence, economic benefits, and perceived severity. |
- The samples are from a certain region, and psychological, cultural, and economic differences between regions may lead to different results. |
| 4. | Cobelli et al. 33 | 2023 | Itali | Market-orientation paradigm & UTAUT New predictor: Market orientation |
Pharmacists | Telemedicine | Performance expectancy, effort expectancy and facilitating conditions. |
− Data collected from specific type of pharmacists and Italian pharmacists only. - Data collection during peak of COVID-19 pandemic. |
| 5. | Upadhyay et al.
41
|
2023 | India | Unified model of e-government adoption (UMEGA) New predictor: perceived severity, self-efficacy, and political trust |
Consumer | E-government telemedicine service | Attitude, political trust and facilitating conditions. | - Online data collection only. |
| 6. | Pereira et al. 16 | 2023 | Portugal | Diffusion of innovation theory, UTAUT, health belief model, and concerns for information privacy framework | Young people in two institutes of higher education | Video consultations | Attitude, performance expectancy, and COVID-19. | - Selected samples (young people) are not representative enough. |
| 7. | Kim & Han 39 | 2023 | Korea | Behavioral model | Older adults | Telemedicine & healthcare devices | Usefulness, information, cost saving, subjective health, and income. | - Functional and emotional values are neglected. |
| 8. | Kabra & Songroya 17 | 2023 | India | UTAUT Additional variables: Personal innovativeness |
Medical practitioners | Telemedicine | Effort expectancy, facilitating conditions, performance expectancy, social influence, and personal innovativeness | - Further research from doctors’ perspective is required. |
| 9. | Xiong & Zuo 19 | 2023 | China | Value-based adoption model | Frontline health care professionals |
Mobile platform of medical and senior care (MPMSC) | Outcome expectations, perceived mobility, perceived effort, and privacy concerns predict perceived value. Perceive value and legal concern affect intention to adopt. |
- Did not study factors in-depth. - This study investigated at the individual level only. Organizational level related factors are neglected. |
| 10. | Yuen et al. 43 | 2023 | Singapore | Health Belief Model, Perceived Value Theory, and the Self-Determination Theory |
Residents in Singapore who has used telehealth services |
Telehealth | Perceived threat, cues to action, and perceived relatedness directly affect perceived value, while self-efficacy, perceived relatedness, and perceived autonomy have a direct impact on emotion. Perceived value of telehealth services has a direct and indirect positive influence on intention to adopt telehealth services through emotions. | - The study conducted in Singapore only which commonly viewed as a tech-savvy population. - This study is inclined toward users’ psychological aspects, external factors are neglected. |
| 11. | Schmitz et al. 35 | 2022 | Spain | UTAUT2 New predictor: perceived security and perceived product advantage |
Patient | Telemedicine | Performance expectancy, hedonic motivation, perceived security, and perceived product advantage. |
- Partial of the constructs from UTAUT are tested. |
| 12. | Ma et al. 20 | 2022 | China | None | Health care professionals | Telemedicine | Short service duration, convenience of the operating system, cost subsidy incentive and the promotion of professional titles. |
- The scope of research needs to be further expanded. - Geographical bias |
| 13. | Ong et al. 1 | 2022 | Philippines | UTAUT2 |
Not specific | Telemedicine | Performance expectancy, effort expectancy, hedonic motivation, social influence, and resistance to use | - Data was collected from individual who have internet access (Not patient/users/physician) - Actual behavior not measured. |
| 14. | Alexandra et al. 46 | 2021 | Indonesia | TAM Predictors categorized into user dimension and the technology dimension |
Individuals familiar with or having prior experience using a hospital's teleconsultation application. | Telemedicine | Contamination avoidance, safety, reliability, professionalism, PEoU, PUse, and information quality |
- Most of the respondents have age between 17 to 25 years old and live in the Greater Jakarta area which limit the result of this study. |
| 15. | Cobelli et al. 40 | 2021 | Italy | Theory of planned behavior | Pharmacist | Telemedicine | Attitude and perceived behavioral control |
- Convenient sampling was used. |
| 16. | Rajak & Shaw 37 | 2021 | India | TAM Additional variables: social influence, technology anxiety, trust, perceived risk, perceived physical condition, resistance to change |
Individuals were chosen based on their use of Android/smartphone devices and access to internet services on their phones. | mHealth (mobile health) | Social influence, perceived risk, resistance to change, physical conditions, and attitude. | - Respondents were new users of technology. |
| 17. | Arfi et al. 36 | 2021 | France | UTAUT Additional variables: Perceived trust and perceived risk |
Patient | E-health | Effort expectancy, social influence, facilitating conditions, and perceived trust (indirect- with perceived risk as mediator). | - This research was conducted among the French population only, and its size limits the generalization of the findings. - Data collection during pandemic. |
| 18. | Ahmed et al. 42 | 2021 | Ethiopia | None | Health professionals |
Telemedicine | Attitude, patient-physician relationship, and ease of use. | - No theoretical supports. |
| 19. | Wu et al. 21 | 2021 | China | Social cognitive theory | Patient | Telemedicine | Self-efficacy and trust | - Focuses on a region with high levels of telemedicine development only. - Most of the sample comprised middle-aged and old people, while fewer younger people were studied. - Did not consider other external variables |
| 20. | Kamal et al. 22 | 2020 | Pakistan | TAM Additional variable: social influence, facilitating conditions, trust, privacy, perceived risk, technological anxiety and resistance towards technology |
Patient | Telemedicine | PEoU, technological anxiety, social influence, PEoUf, trust, facilitating conditions, perceived risk, and resistance to technology. |
- Participant were mainly patients. |
| 21. | Yamin & Alyoubi 38 | 2020 | Saudi | UTAUT, task technology fit model New predictor: Awareness and self-efficacy |
Individual familiar with telemedicine applications, computers and mobile devices. |
Telemedicine- wireless sensor network applications | Performance expectancy, social influence, effort expectancy, facilitating condition, task technology fit, awareness, and self-efficacy |
- Results based on single country i.e., Saudi Arabia thus, results may differ when comparing with other countries. - Used online and non-random convenience sampling approach. |
| 22. | Klingberg et al. 34 | 2020 | Tanzania | TAM; Additional variables: compatibility, image, voluntariness, self-efficacy, anxiety, social influence and facilitating conditions |
Health providers | mHealth | Attitude. Compatibility and perceived ease of use affect PUse. Image, social influence, anxiety, perceived ease of use, and PUse affect attitude |
- Study setting was limited to Dar Es Salaam, Tanzania, health workers’ perceptions may differ from those working in rural area. - Small sample size. |
It is worth noting that most telemedicine studies have been conducted using samples from China,15,18–21 with limited representation from Southeast Asian and developing countries, including Malaysia. In this study, we adopted the TAM 31 and Kelman's Social Influence Theory. 32 The following sections provide a detailed discussion of these two theories and their importance in filling the existing gaps.
Technology acceptance model (TAM)
Technology acceptance is described as an individual's psychological condition regarding his or her voluntary or intention to use a specific technology. Users’ willingness to use technology is a critical component for the adoption of a new technology. Hence, researchers have introduced several models over the past decades to explore the characteristics of technology adoption among users.
Among the available theories, TAM and UTAUT are the most widely used models to predict individuals’ technology acceptance behaviors in the health context. 45 Based on a systematic literature review by Garavand et al., 27 most existing research on physicians’ acceptance of telemedicine builds on TAM. TAM utilizes Perceived Usefulness (PUse) and Perceived Ease of Use (PEoU) to assess how technological aspects affect a user's intention to use technology. 31 For instance, Lu et al., 18 Kamal et al., 22 and Alexandra et al. 46 adopted TAM to explain physicians’ intentions to use telemedicine. TAM has been widely adopted because it is easily applied in different research settings. In addition, TAM has been recognized as the most powerful and frequently used model in predicting the use and acceptance of numerous technologies.
However, several studies have raised doubts about using solely TAM to identify technology acceptance.22,23 Researchers have argued that functional and utilitarian benefits, such as perceived ease of use, do not adequately explain consumer technology acceptance. 24 Hence, the original TAM has been used with additional variables or integrated with other models or theories to better reflect the users’ technology adoption. For instance, several researchers have extended the original TAM with additional constructs such as perceived incentives, self-efficacy, accessibility of patients and medical records, 47 user profile, subjective norms, and physician security and confidentiality, 48 image, self-efficacy, voluntariness, compatibility, and anxiety, 34 and others. Besides, certain studies also integrated TAM with other theories, such as the Theory of Planned Behavior 49 and the Capabilities Approach. 23 A recent study by Lu et al. 18 also integrated TAM with the Health Belief Model to investigate telemedicine adoption. Therefore, these revised or integrated frameworks can provide more thorough evidence of the adoption of technologies among physicians.
In developing countries like Malaysia, telemedicine is perceived as an effective and innovative alternative approach to healthcare services. In the telemedicine adoption context, TAM does not account for the potential impact of multidimensional social and clinical factors that can potentially influence physicians’ telemedicine adoption. 22 Hence, this study enhances TAM by integrating it with Kelman's Social Influence Theory to reflect the effects of the multidimensional social influence and technological factors that potentially influence physicians’ telemedicine adoption. In addition, we added self-efficacy as the individual factors and clinical factors and included accessibility of medical records and accessibility of patients to investigate the acceptance of telemedicine among physicians in detail.
Kelman's Social Influence Theory
Social influence plays a critical role in determining a person's attitudes, beliefs, and actions. 32 Kelman's Social Influence Theory suggests three conceptually distinct approaches that influence a person's acceptance of an induced behavior. According to Kelman, social influences can be categorized into three different perspectives that influence a person's behavior, namely compliance, identification, and internalization. 32 Compliance refers to an act of willingly adopting the induced behavior to attain rewards (or approval) while simultaneously avoiding penalties (or disapproval). The satisfaction derived from compliance is closely tied to the social effect of yielding the influence. Identification takes place when individuals engage in the suggested behavior to establish or maintain a mutually beneficial relationship with another person or a group. In this case, satisfaction arises from “the act of conforming itself” as it strengthens the desired relationship. Internalization occurs when individuals willingly accept, influence, and believe that the suggested behavior aligns with their values and conveys the thoughts and behaviors of others. They embrace the induced behavior because they recognize its consistency with their values, and this alignment with their values provides satisfaction.
Nevertheless, popular technology acceptance models, such as UTAUT, are focused on the compliance aspect of social influences. Most existing studies on telemedicine adoption, such as Cobelli et al. 14 and Vidal-Silva et al., 15 have also focused on the compliance aspect of social influence in their studies. This argument has been underscored by Wang et al., 25 who stated that the existing technology acceptance models like TPB, TAM2, and UTAUT often rely heavily on subjective norms. These norms primarily emphasized operationalizing the compliance aspect of social influence. The process of identification and internalization aspects of social influence as proposed by Kelman 32 are ignored in the existing technological acceptance models. 50 Previous studies have highlighted the importance of investigating different social influence processes in technology adoption because the benefits of identification and internalization are likely to last longer, whereas compliance-based social influence effects may diminish with experience. 25 In line with this notion, Venkatesh and Morris 51 also indicated that the diminishing impact of compliance-based social influence might be due to the users’ tendency to internalize others’ judgments and emphasize their own opinions. Hence, the single aspect of social influence (e.g., compliance) as proposed in well-known technology acceptance models may not accurately predict the users’ technology adoption and behavior; several researchers have therefore made efforts to integrate the three perspectives of social influence processes.25,50
The existing literature on telemedicine studies mostly builds on well-known technology acceptance models like TAM or UTAUT, which focus on a single aspect of social influences. Even though Malhotra and Galletta 50 and Wang et al. 25 have made progress by adopting Kelman's Social Influence Theory to conceptualize the other social influence factors in the organizational setting, no consistent significance was revealed in these studies. Furthermore, while a recent study by Lu et al. 52 investigated the multidimensional social influence on health-related technology adoption in China, this domain remains understudied in the context of telemedicine adoption, particularly in developing Southeast Asian countries such as Malaysia. As a result, this study proposes a more inclusive conceptualization of social influence to predict physician telemedicine adoption by developing hypotheses that integrate TAM with Kelman's Social Influence Theory. This provides a comprehensive overview of how technological factors and multidimensional social influence affect physicians’ intention to use telemedicine in the Malaysian context. The following sections provide the hypothesis based on the constructs proposed.
Hypothesis development
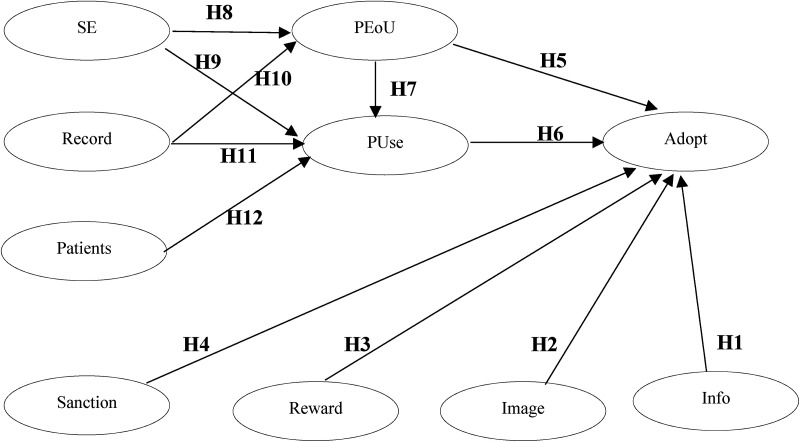
Building on the TAM and Kelman's Social Influence Theory, a research model was proposed to investigate physicians’ intentions to use telemedicine (Figure 1). As proposed in Kelman's social influence theory, this study first assessed identification (image), internalization (informational influences), and compliance (rewards and sanctions) to reflect the multidimensional social influence that potentially influences telemedicine adoption. Then, the hypothesis for PEoU and PUse from the TAM is proposed. Following that, the hypothesis and discussions for individual factors (self-efficacy) and clinical factors (accessibility of patients and medical records) are presented as the antecedents of PEoU and PUse of telemedicine. Table 2 provides an overview of the definitions for each construct.
Figure 1.
Research model.
Table 2.
Definition of constructs.
| Constructs | Definitions |
|---|---|
| Reward | The positive outcomes that an employee expects to receive when engaging in the desired behavior, such as bonuses, recognition from supervisors, and salary increases. 69 |
| Sanction | The withdrawal of positive consequences or application of negative consequences from supervisor such as coercion, punishment, or disapproval. 69 |
| Image | The extent to which the use of an innovation is perceived to increase a person's image or status in his or her social system. 61 |
| Informational influences (Info) | The influence to accept information obtained from other people as evidence of reality. 54 |
| Self-efficacy (SE) | An individual's own perception of being able to perform an action or a task according to certain scenarios. 79 |
| Perceived usefulness (PUse) | The degree a physician perceives that telemedicine adoption will enhance the procedures and results of health treatment. 47 |
| Perceived ease of use (PEoU) | The degree a physician's perception of the ease of using telemedicine services. 47 |
| Accessibility of Patients (Patients) | The degree that physicians perceive that using telemedicine can enhance communication with underserved patients who reside far from medical institutions or hospitals. 47 |
| Accessibility of medical records (Record) | The extent to which physicians perceive that telemedicine usage will enhance patient health and offer accurate and current patient information.47,75 |
| Telemedicine adoption (Adopt) | The degree of a physician's behavioral intention to use telemedicine service. 47 |
Internalization
Internalization occurs when the process of deciding or adopting a behavior depends on how closely one's values align with those of other members of the group. They may view the induced behavior as beneficial in resolving a problem or congruent with their needs. 32 In other words, an individual will likely be involved in the desired behavior if the influential agent's values are aligned with their value systems, and they perceive the respective behaviors to be intrinsically rewarding. Venkatesh and Davis 53 also confirmed that if a subordinate recommends that a given technology is useful, an individual will undergo internalization by believing that technology is useful. As a result, the person chooses to accept the external influence. Informational influence was therefore used to reflect that a person undergoes the process of internalizing external information.25,52
Informational influence (Info)
According to Deutsch and Gerard, 54 the influence to accept information obtained from other people as evidence of reality is known as informational influence. In the healthcare context, physicians regularly interact with colleagues and can observe colleagues’ behaviors. 55 With that, internalization is probably stimulated when physicians try to identify with their colleagues. 56 To properly interpret the situation's reality and behavior, people could be influenced to adopt technology. 57 In line with this discussion, Lu et al. 52 found informational influence to positively impact the physician's acceptance of healthcare technology during the pre-adoption stage but not the post-adoption stage; extrinsic benefits (e.g., rewards and image enhancement) more effectively compensate for the difficulties and efforts the physician faces in the post-adoption stage. Likewise, Bagozzi and Dholakia 58 claimed that people will have the intention of joining a social organization if they become aware that they and other members share similar values. However, Cheung and Lee 59 failed to justify the influence of the shared similar values and goals of the online social networking intention. In contrast, Tong et al. 56 revealed that informational influence indirectly affects the physician's use of information systems in healthcare. Therefore, this study proposes that physicians may become aware of the value of telemedicine through interactions and sharing similar values with subordinates and peers. Consequently, these informational influences will cause physicians to use telemedicine. The hypothesis is proposed as follows:
H1: Informational influence (Info) exerts a positive influence on telemedicine adoption (Adopt).
Identification
Based on the psychological attachment theory, identification is another social influence approach that affects a person's behavior. Kelman 32 defines identification as an individual's development of induced behavior to generate a positive image with other people or groups. A person attempts to act like others who have reference power through identification. An individual's perception of the potential effects of using technology is therefore likely to be affected by the convincing information provided by significant others. 60
Image
According to Moore and Benbasat, 61 image refers to the extent to which the use of an innovation is perceived to increase a person's image or status in his or her social system. Venkatesh and Davis 53 confirmed that images significantly affect user acceptance of technology. In addition, in an organizational setting, Malhotra and Galletta 50 revealed that identification positively impacts employees’ system usage behavior. In the context of the healthcare field, Kummer et al. 62 revealed the importance of image as a predictor of technology acceptance among healthcare personnel. However, Jeng and Tzeng 63 found that images had an insignificant influence on the intention to use healthcare-related systems among medical professionals. The rationale behind this might be that medical professionals are usually well-trained experts in their field; hence, they are less likely to be affected by social influences like the image factor. 63 Due to the inconsistent findings on the effects of images, more research is required. Chong et al. 64 also highlighted that the influence of image in the healthcare context is a relatively understudied domain. Hence, we propose that image positively influences physicians’ intentions to use telemedicine. Physicians who are inexperienced and new to telemedicine will more likely rely on more accessible cues to assess their use decision, like the anticipated image gain associated with technology use. With that, the hypothesis is posited as follows:
H2: Image (Image) exerts a positive influence on telemedicine adoption (Adopt).
Compliance (reward and sanction)
Compliance is “when a person accepts the induced behavior as he or she wishes to obtain favorable responses from another person or group.” People tend to conform to compliance to get approval or rewards and to avoid punishments or sanctions. Following the concept proposed by Kelman, 32 this study assesses compliance based on the expectations imposed on one by influential people in the context of rewards or sanctions. Previous studies have shown that compliance reflected through reward and sanction has a significant influence on changing an individual's behavior.65,66 In the existing literature, Podsakoff et al. 67 and Sims 68 discovered that rewards have a greater influence on the employee's performance than sanctions, while Liang et al. 65 found that sanctions have a greater effect.
Reward
Reward is when superiors apply positive consequences to subordinates. Reward refers to the positive outcomes that an employee expects to receive when engaging in the desired behavior, such as bonuses, recognition from supervisors, and salary increases. 69 Rewards are important because they serve as an external reinforcement for induced behavior. 70 Due to the absence of a new technology's actual usage experience, people often feel unsure of the new technology's performance. Hence, people will make decisions mostly based on the information obtained from supervisor advocacy and training. 66 Karahanna et al. 71 revealed that the adoption ambiguity can be reduced and the technology is legitimized if the employee receives rewards from the supervisor or hospital administration. Previous research has shown that if employees are rewarded or receive approval, they can successfully develop technology acceptance.65,72 For instance, Malik et al. 70 showed that rewards would enhance the employee's performance in the creativity field. Also, Bulgurcu et al. 72 found that rewards influence the employee's intention to comply with the security policy.
In the healthcare context, Tong et al. 56 discovered that rewards from hospital management can enhance the direct use of an electronic medical record (EMR) system. When the physician expects to obtain rewards from the supervisors, they will perform the expected behavior.66,73 In China, Lu et al. 52 also confirmed that the reward from hospital management or supervisors positively influences physicians’ intention to use healthcare-related information technology in hospitals. According to Kelman, 32 an individual is more likely to participate in a particular adoption behavior when they believe the agent will provide positive consequences (i.e., rewards). Based on the existing literature and discussion, this study proposes that rewards can positively influence the physician's intention to use telemedicine in hospitals. A hypothesis is posited as follows:
H3: Reward (Reward) exerts a positive influence on telemedicine adoption (Adopt).
Sanction
Another important element of compliance is sanction, which refers to the withdrawal of positive consequences or application of negative consequences from a supervisor such as coercion, punishment, or disapproval. 69 The impact of sanctions is significant as the employees typically wish to prevent unfavorable consequences, for instance, their supervisor's coercion or disapproval of any sort. 74 The concept of sanctions has been widely adopted in an organizational setting. Previous research on the organizational context revealed that sanctions and punishment can control the behavior of the employee and increase the firm's performance effectively. 67
During the pre-adoption stage, a physician would lack knowledge of using a new telemedicine system. Hence, the management can legitimize the behavior by imposing sanctions to lower the physician's uncertainties about new technology. 71 When physicians want to prevent sanctions and avoid disapproval from their supervisors, they will comply with the desired behaviors.65,66,73 In the context of healthcare studies, Tong et al. 56 revealed that coercion from hospital management can increase the physician's direct use of the electronic medical record (EMR) system to avoid negative consequences. In addition, Lu et al. 52 also confirmed that sanction would positively influence the physician EMR system acceptance. Hence, this study proposes that physicians would be inclined to use telemedicine if there are sanctions imposed. The hypothesis is posit as follows:
H4: Sanction (Sanction) exerts a positive influence on telemedicine adoption (Adopt).
Perceived Usefulness (PUse) and Perceived Ease of Use (PEoU)
Following a systematic literature review conducted by Garavand et al., 27 the TAM was the most frequently adopted theory to explain physicians’ telemedicine acceptance. Specifically, PEoU and PUse from TAM are the two major predictors that influence telemedicine acceptance among physicians.27,45 PUse refers to the degree a physician perceives that telemedicine adoption will enhance the procedures and results of health treatment. 47 Whereas, PEoU is defined as a physician's perception of the ease of using telemedicine services. 47 Physicians deemed telemedicine useful if it improved patient care and delivery, reduced response time for medical services, improved documentation, enabled accuracy, and affordable health monitoring.47,75 In other words, physicians are inclined to use telemedicine if they perceive it as useful.
Previous studies have affirmed the importance of PEoU and PUse in the context of telemedicine. In Indonesia, Alexandra et al. 46 demonstrated that these factors, namely PEoU and PUse, have a positive impact on an individual's intention to use telemedicine services. In addition, Kamal et al. 22 illustrated that within developing nations, PEoU and PUse play vital roles as predictors of telemedicine adoption. From the perspective of physicians, existing studies confirmed the impact of PEoU and PUse on physicians’ intention to use telemedicine services.27,45,47,76 Based on the literature, this study proposes that:
H5: Perceived ease of use (PEoU) exerts a positive influence on telemedicine adoption (Adopt).
H6: Perceived usefulness (PUse) exerts a positive influence on telemedicine adoption (Adopt).
Moreover, prior research has demonstrated that PEoU directly affects the perceived usefulness of telemedicine among physicians.34,47,77,78 Similarly, this study proposes that physicians will perceive telemedicine to be useful if it is easy to use.
H7: Perceived ease of use (PEoU) exerts a positive influence on perceived usefulness (PUse).
Antecedents of PEoU and PUse
Self-efficacy (SE)
According to Bandura, 79 self-efficacy refers to an individual's perception of being able to perform an action or a task according to certain scenarios. In this study, self-efficacy is defined as a physician's confidence in their ability to use telemedicine devices.47,77,80 Self-efficacy is one of the main factors that influence physicians’ acceptance of telemedicine technology. 27 Zobair et al. 81 confirmed that self-efficacy affects a person's expectations of telemedicine adoption. Many studies have confirmed the significant influence of self-efficacy in the telemedicine context.82,83 Moreover, self-efficacy also affects intention through PEoU and PUse. 84 For example, Rho et al. 47 discovered that physicians’ self-efficacy significantly influences their perception of the ease of use and usefulness of telemedicine services. Hence, this study proposes that greater self-efficacy among physicians will positively influence the PEoU and PUse of telemedicine. The hypotheses is proposed as follows:
H8: Self-efficacy (SE) exerts a positive influence on perceived ease of use (PEoU).
H9: Self-efficacy (SE) exerts a positive influence on perceived usefulness (PUse).
Accessibility of medical records (Record)
The accessibility of medical records refers to the extent to which physicians perceive that telemedicine usage will enhance patient health and offer accurate and current patient information.47,75 Physicians have stated that improved accessibility of patient’s medical records has led to quicker treatment delivery, shorter wait times for medical services, and more accurate medical assessments at lower costs.75,85 In addition, easy access to patient records has fostered improved documentation of patient’s medical issues, allowing for the provision of accurate and timely patient records. 75 Access to medical records is critical for physicians’ daily practices because it can lead to better clinical outcomes and healthcare performance.75,85 For instance, Sandberg et al. 75 revealed that physicians perceive telemedicine services as useful when they can access the patient's medical records conveniently by using telemedicine. Furthermore, Rho et al. 47 revealed that the accessibility of medical records significantly influences the physician's PUse of telemedicine but not the PEoU. With that, this study proposes that telemedicine will generate a positive perception of ease of use and usefulness among physicians when they have greater accessibility to medical records. Hence, the hypotheses are proposed:
H10: Accessibility of medical records (Record) exerts a positive influence on perceived ease of use (PEoU).
H11: Accessibility of medical records (Record) exerts a positive influence on perceived usefulness (PUse).
Accessibility of patients (Patients)
Accessibility of patients refers to the degree to which physicians perceive that using telemedicine can enhance communication with underserved patients who reside far from medical institutions or hospitals. 47 Telemedicine services hold great promise for improving access to care for a wide range of medical conditions, particularly for patients who live far from medical facilities or in rural areas. During the COVID-19 pandemic, Bhatia 86 found that people living in rural areas have a high intention to use telemedicine services. According to medical research, telemedicine is a potential tool for increasing patient accessibility to healthcare facilities. 22 The use of telemedicine allows physicians to provide medical consultation and care for patients who are separated from physicians by geographic distances. 87 Telemedicine services play an important role and improve patient care effectiveness, especially when physicians have a heavy workload to warrant contacting patients. Furthermore, Rho et al. 47 revealed that in Korea, the PUse was significantly influenced by the accessibility of patients. Therefore, this study follows the previous findings and proposes the following hypothesis:
H12: Accessibility of patients (Patients) exerts a positive influence on perceived usefulness (PUse).
Material and methods
Questionnaire design
This study gathered data using a cross-sectional survey with a structured questionnaire. The questionnaire has two sections. The first section collects demographic information from respondents. The second section contains items related to the constructs in the research model, as illustrated in Figure 1. The measurement items tapping the theoretical constructs were developed based on an extensive literature review. They were adapted from Compeau and Higgines, 88 Lu et al., 52 Martinez et al., 89 Moore and Benbasat, 61 O’Reilly and Chatman, 90 Rho et al., 47 Sandberg et al., 75 Whitten et al., 85 Vandenberg et al., 91 and Ventakash and Davis, 53 thus satisfying content validity. The sources of the items in the survey questionnaire are displayed in Table 3. All the items in part B were constructed as “strongly disagree” to “strongly agree” statements on a five-point Likert scale. Before collecting data, we had two physicians review the questionnaires to ensure the language and item comprehension were appropriate.
Table 3.
Operationalization of constructs.
| Constructs | Sources |
|---|---|
| Reward | O’Reilly and Chatman 90 |
| Sanction | Lu et al. 52 |
| Image | Moore and Benbasat 61 |
| Informational influences (Info) | Vandenberg et. al. 91 |
| Self-efficacy (SE) | Compeau and Higgines 88 |
| Perceived usefulness (PUse), Perceived ease of use (PEoU) | Venkatesh and Davis 53 |
| Telemedicine adoption (Adopt) | Lu et al. 52 |
| Patients | Rho et al. 47 , Martinez et al. 89 |
| Record | Rho et al. 47 , Whitten et al. 85 , Sandberg et al. 75 |
Research sample and survey administration
There are varying opinions in the literature regarding the determination of an appropriate sample size for different types of statistical analyses. In this study, a priori sample size calculation was based on G-power. Thus, a minimum participant size of 109 would be required with a 0.15 effect size, 0.05 alpha level, and 0.8 power.
The survey was conducted from February 2022 to August 2022. The sample comprises physicians with various specializations from both private and public hospitals in Wilayah Persekutuan Kuala Lumpur and Selangor, Malaysia. Specifically, we included respondents from the medical department and the primary care department due to their frequent reliance on telemedicine for managing chronic conditions and providing routine check-ups remotely. We excluded respondents from the surgical department and other departments as their telemedicine utilization is comparatively lower. By focusing on the medical and primary care departments, we aim to gather insights relevant to the effective implementation of telemedicine services in Malaysian hospital settings.
We created an online invitation containing a link to a questionnaire on Google Forms; the invitation was distributed through email and WhatsApp. We included a cover letter outlining the research objective within the survey. At the survey's outset, we identified the target audience to ensure respondents were our target audience. We described telemedicine to help respondents understand the technology used in the hospital. Written informed consent was sought from all respondents, who retained the right to withdraw at any time. Participation in this study was entirely voluntary and no compensation was offered. A total of 251 responses were collected. To handle non-responses effectively, we implemented rigorous data cleaning procedures before conducting data analysis. Some survey responses were excluded due to missing data or refusal to provide written consent, leaving a valid sample of 230 responses for further analysis. Given the physicians’ busy schedules, the number of responses obtained was deemed satisfactory.
Statistical analysis and results
Data analysis was performed using SPSS software for descriptive analysis. For the measurement and structural models, this study used Partial Least Squares Structural Equation Modeling (PLS-SEM) because it does not rely on the assumption of normality. Additionally, it is better suited for studies involving formative constructs as suggested by Chin. 92 Considering that survey data often does not follow a normal distribution and this study incorporates multiple formative constructs, PLS-SEM was utilized through SmartPLS version 3.2.8 for the data analysis.
Respondent demographics
The demographic information of the respondents is presented in Table 4. As shown, 73.5% of the respondents were female. The distribution of the respondents was 53.9% Malay, 33% Chinese, and 12.1% Indian. The respondents’ ages ranged from 20 years to over 50 years; the highest frequency was observed in the age group of 30–39 years (52.2%). The respondents were from the medical department (86.1%) and the primary care department (13.9%). The career longevity of respondents was as follows: less than 1 year (2.7%), 1–5 years (5.5%), 6–10 years (24.5%), and more than 10 years (67.3%). The respondents were employed by university hospitals (69.1%), tertiary government hospitals (17.8%), district government hospitals (3.9%), and private practices (9.1%).
Table 4.
Respondents’ information (n = 230).
| Characteristics | Frequency | Distributions (%) |
|---|---|---|
| Gender | ||
| Female | 169 | 73.5 |
| Male | 61 | 26.5 |
| Ethnicity | ||
| Malay | 124 | 53.9 |
| Chinese | 76 | 33.0 |
| Indian | 28 | 12.1 |
| Age | ||
| 20–29 years-old | 49 | 21.3 |
| 30–39 years-old | 120 | 52.2 |
| 40–49 years-old | 50 | 21.7 |
| 50 years-old and above | 11 | 4.8 |
| Department | ||
| Medical | 198 | 86.1 |
| Primary care | 32 | 13.9 |
| Career | ||
| Less than 1 year | 3 | 2.7 |
| 1–5 years | 6 | 5.5 |
| 6–10 years | 27 | 24.5 |
| more than 10 years | 74 | 67.3 |
| Hospital institution | ||
| University hospital | 159 | 69.1 |
| Tertiary general hospital | 41 | 17.8 |
| District General hospital | 9 | 3.9 |
| Hospital/private practice | 21 | 9.1 |
Common method bias
To address the issue of common method bias, this study conducted the marker variable test, a well-established approach for evaluating common methods bias (CMB). 93 In the questionnaire, we included an unmeasured marker variable, 94 which was conceptually unrelated to the other constructs. The results are presented in Table 5. They demonstrate that the R² changes were below 10% even with the inclusion of the marker variable, indicating the absence of significant CMB in this study.
Table 5.
Common method variance.
| R2 (Before adding in marker variable) | R2 (After adding in marker variables) | |
|---|---|---|
| Adopt | 0.469 | 0.475 |
| PEoU | 0.510 | 0.576 |
| PUse | 0.604 | 0.607 |
Evaluating the measurement model
Before proceeding with hypothesis analysis, it's crucial to assess the reliability and validity of the measurement items. This study examined the measurement model to evaluate the instrument's validity and reliability, following Hair et al. 95 guidelines. Since the model in this study comprises both formative constructs and reflective measurement items, the assessment criteria differ slightly. Subsequently, a structural model was employed to test the developed hypotheses.
Formative measurement model
This study involved four formative constructs (image, information, rewards, and sanction), which were validated following the guidelines proposed by Petter et al. 96 and Cenfetelli and Bassellier. 97 To assess the measurement model for these constructs, we examined weights, t-values, and variance inflation factors (VIF). First, we addressed the multicollinearity issue among the formative indicators using VIF. All VIF values below 5 indicated no significant multicollinearity, 98 as seen in Table 6.
Table 6.
Measurement model.
| Constructs | Items | Scale | Loadings | Composite Reliability | Average Variance Extracted (AVE) |
|---|---|---|---|---|---|
| PEoU | PEoU1 | Reflective | 0.886 | 0.921 | 0.795 |
| PEoU2 | 0.901 | ||||
| PEoU3 | 0.888 | ||||
| PUse | PUse1 | Reflective | 0.874 | 0.903 | 0.699 |
| PUse2 | 0.826 | ||||
| PUse3 | 0.834 | ||||
| PUse4 | 0.809 | ||||
| Patients | Patients1 | Reflective | 0.959 | 0.958 | 0.919 |
| Patients2 | 0.958 | ||||
| Record | Record1 | Reflective | 0.929 | 0.956 | 0.88 |
| Record2 | 0.943 | ||||
| Record3 | 0.942 | ||||
| SE | SE1 | Reflective | 0.795 | 0.896 | 0.683 |
| SE2 | 0.787 | ||||
| SE3 | 0.865 | ||||
| SE4 | 0.855 | ||||
| Adopt | Adopt1 | Reflective | 0.914 | 0.954 | 0.874 |
| Adopt2 | 0.945 | ||||
| Adopt3 | 0.945 | ||||
| Weights | t-value | VIF | |||
| Info | Info1 | Formative | 0.142 | 0.643 | 2.406 |
| Info2 | 0.887 | 4.957 | 2.406 | ||
| Image | Image1 | Formative | 1.362 | 1.822 | 4.718 |
| Image2 | −0.430 | 0.489 | 4.718 | ||
| Reward | Reward1 | Formative | 0.651 | 0.908 | 3.468 |
| Reward2 | 0.388 | 0.537 | 3.468 | ||
| Sanction | Sanction1 | Formative | 0.023 | 0.033 | 2.818 |
| Sanction2 | 0.981 | 1.516 | 2.818 |
Next, we evaluated the significance and relevance of item weights in formative measurement models as the second step in our assessment. 98 We employed a bootstrapping procedure and generated 5000 subsamples to determine if outer weights in formative measurement models significantly differed from zero. One formative construct (Image) displays both positive and negative indicator weights. It is worth noting that negative weights may impact individual indicator interpretation but not the structural effects within the model, as indicated by previous research. 97 Additionally, removing an indicator should be done with caution, considering conceptual overlap which guided our decision to proceed with the existing indicators.
Reflective measurement model
For the reflective constructs (ease of use, patients, records, self-efficacy, usefulness, and intention), we evaluated the convergent and discriminant validities. To gauge convergent validity, we assessed loadings, average variance extracted (AVE), and composite reliability (CR) to assess the reflective measurement model. Guided by established thresholds, loadings should be ≥0.708, the AVE should be ≥ 0.5 and the CR should be ≥ 0.7. As shown in Table 6, all item loadings exceeded 0.708, AVE values surpassed 0.5, and CR values were above 0.7. For discriminant validity, the HTMT criterion99,100 was used. The results presented in Table 7 demonstrated that all HTMT values were below 0.85, even for the stricter criterion. Consequently, we can confidently conclude that respondents recognized the distinctiveness of all constructs. In summary, these validity tests confirm that the reflective measurement items are both valid and reliable.
Table 7.
HTMT.85 criterion.
| 1 | 2 | 3 | 4 | 5 | 6 | |
|---|---|---|---|---|---|---|
| PEoU | ||||||
| PUse | 0.766 | |||||
| Patients | 0.47 | 0.562 | ||||
| Record | 0.673 | 0.782 | 0.512 | |||
| SE | 0.774 | 0.728 | 0.671 | 0.733 | ||
| Adopt | 0.603 | 0.712 | 0.507 | 0.641 | 0.684 |
Structural model
Based on Hair et al., 101 we used multivariate skewness and kurtosis to examine the normality of our data. The results indicated significant Mardia's multivariate skewness (β = 22.515, p < 0.01) and Mardia's multivariate kurtosis (β = 174.274, p < 0.01), revealing that our collected data was not multivariate normal. Therefore, we opted for SmartPLS, a non-parametric analysis software, for our data analysis.
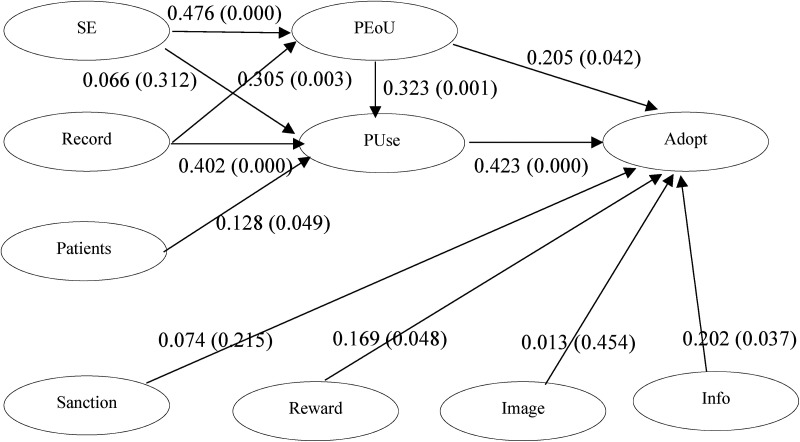
Once all variables in the measurement model met specific thresholds in the reliability and validity thresholds, we delved deeper into investigating the research hypotheses in the structural model. As suggested by Hair et al., 95 we used a 5000-sample bootstrapping procedure to evaluate path coefficients, standard errors, t-values, and p-values for the structural model. Additionally, we employed a combination of p-values, confidence intervals, and effect sizes to assess hypothesis significance. Table 8 and Figure 2 show the criteria used to evaluate the developed hypothesis.
Table 8.
Direct effects.
| Hypothesis | Relationship | Std. Beta | Std. Deviation | t-value | p-value | BCI LL | BCI UL | f2 |
|---|---|---|---|---|---|---|---|---|
| H1 | Info → Adopt | 0.202 | 0.113 | 1.784 | 0.037 | 0.022 | 0.396 | 0.039 |
| H2 | Image → Adopt | 0.013 | 0.113 | 0.116 | 0.454 | −0.185 | 0.178 | 0.000 |
| H3 | Reward → Adopt | 0.169 | 0.102 | 1.663 | 0.048 | 0.039 | 0.381 | 0.026 |
| H4 | Sanction → Adopt | 0.074 | 0.093 | 0.788 | 0.215 | −0.070 | 0.236 | 0.007 |
| H5 | PEoU → Adopt | 0.205 | 0.119 | 1.724 | 0.042 | 0.008 | 0.401 | 0.043 |
| H6 | PUse → Adopt | 0.423 | 0.125 | 3.392 | 0.000 | 0.229 | 0.639 | 0.139 |
| H7 | PEoU → PUse | 0.323 | 0.108 | 2.983 | 0.001 | 0.147 | 0.499 | 0.129 |
| H8 | SE → PEoU | 0.476 | 0.105 | 4.541 | 0.000 | 0.304 | 0.645 | 0.262 |
| H9 | SE → PUse | 0.066 | 0.136 | 0.49 | 0.312 | −0.144 | 0.296 | 0.004 |
| H10 | Record → PEoU | 0.305 | 0.113 | 2.707 | 0.003 | 0.121 | 0.485 | 0.108 |
| H11 | Record → PUse | 0.402 | 0.114 | 3.532 | 0.000 | 0.216 | 0.586 | 0.204 |
| H12 | Patients → PUse | 0.128 | 0.077 | 1.657 | 0.049 | −0.005 | 0.247 | 0.027 |
Note. We use 95% confidence interval with a bootstrapping of 5000
Figure 2.
Results of hypothesis testing.
Initially, we examined the effect of the six predictors on Adopt, resulting in an R2 of 0.469 (Q2 = 0.395), indicating that all six predictors collectively explained 46.9% of the variance in Adopt. Specifically, Info (β = 0.202, p = 0.037), Reward (β = 0.169, p = 0.048), PEoU (β = 0.205, p = 0.042), and PUse (β = 0.423, p < 0.01) exhibited positive relationships with Adopt, while Image (β = 0.013, p = 0.454) and Sanction (β = 0.074, p = 0.215) showed no relationship with Adopt. Thus, only hypotheses H1, H3, H5, and H6 were supported in this study, while H2 and H4 were not.
Next, we tested the effect of four predictors on PUse, resulting in an R2 of 0.604 (Q2= 0.589). This indicates that all four predictors collectively accounted for 60.4% of the variance in PUse. Notably, PEoU (β = 0.323, p < 0.01), Record (β = 0.402, p < 0.01), and Patients (β = 0.128, p = 0.049) displayed positive relationships with PUse, while SE (β = 0.066, p = 0.312) showed no significant relationship with it. Consequently, the hypotheses H7, H11, and H12 were supported in this study, but H9 was not.
Next, we assessed the effect of the two predictors on PEoU, leading to an R2 of 0.510 (Q2 = 0.501), explaining 51% of the variance in PEoU. Both SE (β = 0.476, p < 0.01) and Record (β = 0.305, p < 0.01) exhibited positive relationships with PEoU, supporting hypotheses H8 and H10.
Building upon the earlier hypothesis testing, the bias-corrected 95% confidence intervals for all hypotheses (except H2, H3, and H9) did not span zero, thus affirming their support. Conversely, H2, H4, and H9 were not supported, as their confidence intervals crossed 0.
To assess predictive relevance, we performed the PLSpredict analysis using a ten-fold procedure, following Shmueli et al. 102 PLSpredict generates case-level predictions at an item or construct level. According to Shmueli et al. (2019), there is strong predictive power if all item differences (PLS-LM) are lower than a threshold. In our case, all errors of the PLS model were lower than the LM model, indicating strong predictive power as shown in Table 9.
Table 9.
PLS-Predict.
| Constructs | Q²_predict |
|---|---|
| Adopt | 0.384 |
| Constructs | Items | PLS | LM | PLS-LM |
|---|---|---|---|---|
| Adopt1 | 0.749 | 0.849 | −0.100 | |
| Adopt | Adopt2 | 0.687 | 0.718 | −0.031 |
| Adopt3 | 0.680 | 0.737 | −0.057 |
Importance-performance map analysis
IPMA aims to assess the importance and performance of the predecessor constructs in explaining the target construct (Adopt). It identifies variables with high importance but relatively low performance, 103 indicating areas with potential for improvement and requiring special attention. In this study, we conducted an importance-performance map analysis (IPMA) as a post-hoc procedure in PLS, using performance impact as the outcome construct.
As per Aldholay et al., 104 in IPMA, the average latent variable scores of predecessor constructs represent their performance, whereas the total effects of predecessor constructs indicate their importance in shaping the target construct (Adopt). Performance scores were scaled from 1 to 100, with 1 indicating the lowest performance and 100 the highest (Hair et al., 2016). The results from Table 10 indicate the importance (total effects) and performance of predecessor constructs concerning the target construct (Adopt).
Table 10.
Importance-performance map analysis.
| Performances | Importance | |
|---|---|---|
| PEoU | 65.775 | 0.341 |
| PUse | 66.190 | 0.423 |
| Patients | 69.587 | 0.054 |
| Record | 68.119 | 0.274 |
| SE | 69.407 | 0.191 |
| Info | 64.751 | 0.202 |
| Image | 49.008 | 0.013 |
| Reward | 51.152 | 0.169 |
| Sanction | 32.460 | 0.074 |
The IMPA results revealed that the highest importance lies with PUse (0.423), followed by PEoU (0.341), and Info (0.202) as the result of their comparatively greater importance in comparison with that of other constructs within the proposed model. Therefore, to enhance telemedicine adoption, managerial efforts should prioritize focusing on telemedicine aspects related to PEoU, Puse, and Info.
Discussion
This study developed a research model based on the TAM and Kelman's Social Influence Theory to investigate physicians’ intention to use telemedicine. Kelman's Social Influence Theory was incorporated to account for various dimensions of social influence, including compliance (reward and sanction), identification (image), and internalization (informational influences). Additionally, we proposed a hypothesis for PEoU and PUse based on the TAM. Furthermore, this study introduced the individual factor of self-efficacy and clinical factors of patient and medical record accessibility as antecedents of TAM constructs. The results of our hypothesis testing are summarized in Table 11.
Table 11.
Summary of hypothesis testing.
| Hypothesis | Relationship | p-value | Decision |
|---|---|---|---|
| H1 | Info → Adopt | 0.037 | Supported |
| H2 | Image → Adopt | 0.454 | Not Supported |
| H3 | Reward → Adopt | 0.048 | Supported |
| H4 | Sanction → Adopt | 0.215 | Not Supported |
| H5 | PEoU → Adopt | 0.042 | Supported |
| H6 | PUse → Adopt | 0.000 | Supported |
| H7 | PEoU → PUse | 0.001 | Supported |
| H8 | SE → PEoU | 0.000 | Supported |
| H9 | SE → PUse | 0.312 | Not Supported |
| H10 | Record → PEoU | 0.003 | Supported |
| H11 | Record → PUse | 0.000 | Supported |
| H12 | Patients → PUse | 0.049 | Supported |
From the dimension of social influence, Reward and Info bolster physicians’ telemedicine adoption, while Image and Sanction have no effects. The findings align with earlier studies56,67,68 that found that rewards significantly influence adoption. This suggests that physicians are more likely to embrace telemedicine when they expect positive outcomes (rewards) from their supervisors. In addition, the positive influence of the informational influences is also in line with previous studies such as Lu et al., 52 who found that informational influence was positively related to the physician's acceptance of healthcare technology during the pre-adoption period. Hence, informational influence plays an important role in influencing telemedicine adoption as physicians may become aware of the value of telemedicine through interactions with their colleagues. Consequently, they will adopt telemedicine due to these informational influences. However, this study revealed that image and sanction do not influence telemedicine adoption among physicians. The insignificance of image in this study aligns with Jeng and Tzeng's 63 findings; however, it contradicts the findings of Malhotra and Galletta 50 as well as Kummer et al. 62 The insignificant influence of image may stem from the nature of physicians’ healthcare practice, as they often view themselves as healthcare professionals primarily responsible for providing patient care. Consequently, physicians may not associate telemedicine with image enhancement. 56 Conversely, this study also found an absence of influence from sanctions, which differs from the results of Tong et al. 56 and Lu et al. 52 One plausible explanation for this finding is that, within the context of compliance, physicians tend to focus more on achieving gains and rewards rather than avoiding loss or sanctions.
The study findings indicate that PEoU and PUse positively influence physicians’ adoption of telemedicine. Furthermore, this study also revealed that when they find telemedicine easy to use, it enhances their perception of its usefulness, aligning with prior literature.34,47,77,78 This suggests that physicians are more likely to embrace telemedicine in their healthcare services when it's user-friendly with significant benefits for diagnosis and healthcare management. Conversely, if the telemedicine application is perceived as complex, physicians may hesitate to use it due to the additional time and effort required to familiarize themselves with new technology. 46 As highlighted by Chau and Hu, 105 health professionals tend to adopt a pragmatic approach in their decisions regarding technology acceptance and prioritize the usefulness offered by the technology. Accordingly, this study showed that PUse plays a crucial role in telemedicine adoption among physicians. These results align with similar findings from previous telemedicine studies,27,45,76 but contradict studies such as Hoque et al. 106 The significant role of perceived ease of use and PUse in telemedicine adoption in Malaysia is consistent with the healthcare context of other countries such as Pakistan 22 and Indonesia. 46
Regarding the factors that influence TAM constructs, this study discovered that both proposed clinical factors of patient accessibility and medical record accessibility have a positive effect on PUse. These findings suggest that physicians view telemedicine as useful when it offers improved access to patients and their medical records, which is in line with the findings of Rho et al. 47 This could be because telemedicine excels at bridging the gap with underserved patients in remote areas, enhancing the physician's ability to provide efficient healthcare services. Additionally, easy access to patient records through telemedicine can enhance patient care and provide accurate and current information for physicians. Contrary to the findings of Rho et al. 47 in the Korean setting, this study revealed that a physician's self-efficacy does not impact their perception of telemedicine's usefulness. This discrepancy can be rationalized by acknowledging self-efficacy as an individual factor that varies among individuals. Moreover, a physician's belief in their capabilities does not directly influence their perception of telemedicine's usefulness. Instead, they appear to prioritize clinical factors such as patient and record accessibility when evaluating telemedicine's usefulness.
Lastly, medical record accessibility and self-efficacy positively influence physicians’ perception of telemedicine's ease of use. The significance of self-efficacy in the telemedicine context aligns with the majority of previous studies.82,83 However, the significant role of medical record accessibility in the current study contradicts Rho et al., 47 who did not find a significant relationship in their study. Since telemedicine is a relatively new and innovative technology, physicians who believe in their ability to use it will find it easy to use. Moreover, improved access to patient medical records allows physicians to access up-to-date patient information, leading to more accurate and effective healthcare treatment. This streamlined process can contribute to a smoother, more seamless telemedicine experience and ultimately enhance the perception of its ease of use among physicians.
Study limitations and future research
This study has certain limitations that should be considered when interpreting the findings. It's important to bear in mind the constraints associated with survey-based research, which relies on self-administered questionnaires and has a relatively low response rate. Firstly, the study's observational and cross-sectional design prevents us from establishing causal relationships between variables, given the heightened risk of endogeneity. Longitudinal studies are necessary to assess the impact of telemedicine adoption over time. Secondly, due to the limited participation rate, the results of our study may not fully indicate the factors influencing telemedicine adoption among all physicians. Thirdly, as with many questionnaire-based studies, self-reported information can introduce a social desirability bias that might impact the results. As respondents answered the survey with their organization as the frame of reference, findings may be limited to the surveyed organizations and lack universal applicability. Additionally, bias may have occurred due to the survey's sole reliance on respondents’ perceptions within their organizations. To address this, future studies should use a diverse sample and conduct comparative analyses across organizational contexts to enhance the generalizability of findings and identify contextual factors affecting outcomes.
Theoretical and practical implications
Theoretical contributions
In Malaysia, telemedicine has great potential to fulfill the country's increasing demand for healthcare services. Furthermore, the use of telemedicine services can strengthen the traditional healthcare services that are currently in place. Nevertheless, telemedicine usage is not widely utilized in Malaysia. It is therefore important to investigate the factors that affect telemedicine adoption among physicians. Hence, this study makes a significant contribution to the limited research on telemedicine adoption in Malaysia by integrating the TAM and Kelman's Social Influence Theory to analyze physicians’ intentions to use telemedicine. The research model encompasses clinical factors (e.g., accessibility of medical records and patients), individual factors (e.g., self-efficacy), and multidimensional social influence factors (e.g., image and informational aspects).
The integration of TAM with Kelman's Social Influence Theory goes beyond the conventional focus on compliance-based social influences found in typical technology acceptance models like UTAUT. By incorporating Kelman's theory, which considers compliance, identification, and internalization aspects of social influence, this study comprehensively investigates telemedicine adoption among physicians. Specifically, the integration of theories is important as it expands the focus beyond mere compliance-based social influence, which tends to lose its impact over time as individuals gain experience. In contrast, the identification and internalization aspects of social influence as proposed in Kelman's Social Influence Theory, are more likely to have a lasting impact. Existing studies shown in Table 1, such as those by Cobelli et al. 14 and Vidal-Silva et al., 15 primarily emphasize compliance aspects of subjective norms. They overlook the critical processes of identification and internalization in social influence, as noted by Wang et al. 25 To fill these gaps, this study builds upon recent advancements by Malhotra and Galletta, 50 Wang et al., 25 and Lu et al. 52 to propose a more comprehensive framework for understanding telemedicine adoption among physicians, especially in developing countries like Malaysia. The research can shed more light on physicians’ perspectives on telemedicine and the factors considered by physicians when deciding whether to use telemedicine.
Next, this study also contributes to Kelman's Social Influence Theory by first applying this theory to understand the physician's telemedicine adoption in the context of Malaysia. In addition, this research also contributes to the existing literature by investigating the impact of social influences in multidimensional perspectives, which is theorized from Kelman's Social Influence Theory and able to explain the inconsistent effect of social influence in earlier studies. The findings highlight that not all dimensions of social influence equally influence a physician's adoption of telemedicine. This nuanced understanding can serve as a foundational framework to guide future research in this emerging field. By emphasizing the significance of considering multiple dimensions of social influence, researchers can more accurately capture and understand their impact on technology adoption. This comprehensive approach is essential for developing effective strategies and interventions to ensure the successful adoption and integration of technologies such as telemedicine into healthcare practices.
Practical implications
This study demonstrated that reward and informational influences can effectively encourage physicians to adopt telemedicine. However, the managerial level needs to be aware that emphasizing image and sanction does not effectively encourage telemedicine adoption. Thus, hospital management should acknowledge the importance of reward and informational influences and use these mechanisms to promote telemedicine use. For instance, management can reward physicians who use telemedicine effectively in healthcare services.
Policymakers may leverage this finding to design incentive structures and allocate funding within healthcare policies, including implementing reward systems or bonuses for physicians who demonstrate efficient utilization of telemedicine services. In addition, informational campaigns can be created to teach medical staff members about the features and advantages of telemedicine. This will promote an integrated and accepting culture in healthcare settings.
This study also revealed that the physicians’ perception of telemedicine's ease of use and usefulness positively influences their adoption, aligning with the original TAM framework. In addition, when telemedicine is easier to use, physicians find it more useful. This highlights the importance of technological factors, such as ease of use and usefulness, in the Malaysian healthcare context. Service providers should ensure that the features and functions of telemedicine are user-friendly and beneficial to increase physicians’ willingness to use it. Specifically, policymakers should prioritize investments that enhance the technological infrastructure supporting telemedicine services, given the critical importance of technological criteria such as usefulness and ease of use. This may involve allocating funding for projects aimed at developing user-friendly telemedicine platforms and ensuring widespread access to essential technology resources among physicians.
Furthermore, this study found that clinical factors, including accessibility of patients and medical records, positively influence physicians’ perceptions of telemedicine as a useful tool in healthcare. Therefore, telemedicine service providers should prioritize these clinical needs. For instance, they can enhance patient and medical record accessibility by establishing secure network systems that enable physicians to access patient information and records anywhere, anytime. With that, physicians can stay updated on patient health and reach underserved patients more effectively, ultimately improving the usefulness of telemedicine.
Next, the ease of accessing records and a physician's self-efficacy were shown to make telemedicine easier for physicians to use. Policymakers can engage in collaborative efforts with hospitals to establish training and support programs tailored to equip physicians with the essential skills and confidence required for the effective utilization of telemedicine services. Additionally, integrating telemedicine training into medical curricula prepares future physicians to use these tools confidently and effectively, meeting evolving healthcare needs. Moreover, policymakers can facilitate future collaboration between stakeholders to ensure seamless integration and exchange of patient records across different telemedicine platforms, thereby reducing barriers to access and improving ease of use for physicians.
In conclusion, the study's findings have significant practical implications for management, practitioners, and policymakers. Collaborative efforts among these stakeholders will optimize the adoption of telemedicine to enhance healthcare accessibility, efficiency, and quality in Malaysia. As a result, these developments could have a significant positive impact on healthcare systems as well as society as a whole. They would improve patient experiences, lower the cost of care, and boost resilience in the face of changing healthcare obstacles.
Conclusion
Promoting telemedicine acceptance among healthcare professionals presents a significant challenge, yet it is crucial for the successful implementation of telemedicine initiatives. This study significantly contributes to understanding telemedicine adoption among Malaysian physicians by integrating TAM and Kelman's Social Influence Theory. The findings enrich the existing literature by shedding light on how technological factors, clinical factors, and the various dimensions of social influence exert differential effects on physicians’ acceptance of telemedicine in Malaysia. This research lays a solid foundation for future studies and implementation strategies, and it fosters the seamless integration of telemedicine into healthcare practices.
Acknowledgments
We gratefully acknowledge the editors and anonymous reviewers for their constructive comments, which greatly improved our article.
Appendix 1. Constructs and items.
| Construct | Item | Source |
|---|---|---|
| Reward | • How hard I work on using the telemedicine services will be [is] directly linked to how much I am rewarded by the hospital management. | O’Reilly and Chatman 90 |
| • How hard I work on using the telemedicine services will be [is] directly linked to how much I am recognized by my supervisor. | ||
| Sanction | • To avoid punishment in my job by the hospital management, the telemedicine services usage will be [is] necessary. | Lu et al. 52 |
| • If I do not use the telemedicine services, my supervisor will disapprove me. | ||
| Image | • Using the telemedicine services will improve my image among my departmental peers. | Moore and Benbasat 61 |
| • Using the telemedicine services will improve my image among my hospital peers outside my department. | ||
| Informational influences (Info) | • Based on my observation of my departmental peers, what the telemedicine services usage stands for is important to me. | Vandenberg et al. 91 |
| • Based on my observation of my professional peers, what the telemedicine services usage stands for is important to me. | ||
| Self-efficacy (SE) | • I could complete a job or a task using telemedicine if I could call someone for help if I get stuck. | Compeau and Higgines 88 |
| • I could complete a job or a task using telemedicine if I had just the built-in help facility for assistance. | ||
| • I am confident in using the functions of telemedicine. | ||
| • I am confident in my understanding of the content of telemedicine. | ||
| Perceived usefulness (PUse) | • Using telemedicine will positively affect the treatment plan. | Venkatesh and Davis 53 |
| • Telemedicine is possible to provide more comprehensive care service. | ||
| • Telemedicine is efficient for diagnosing patients and scheduling. | ||
| • I can precisely monitor the patient's condition by using telemedicine. | ||
| Perceived ease of use (PEoU) | • It is easy to use the devices for telemedicine services. | Venkatesh and Davis 53 |
| • It is easy to learn how to use the new devices for telemedicine. | ||
| • It is easy to perform my job by using the telemedicine services. | ||
| Telemedicine adoption (Adopt) | • I have a positive intention to adopt the telemedicine service. | Lu et al. 52 |
| • I will gain accurate patient information and treatment histories if I use telemedicine service. | ||
| • I will provide telemedicine services and share the information through this service. | ||
| Patients | • I am able to be in contact with patients who seldom come to the clinic through telemedicine services. | Rho et al. 47 , Martinez et al. 89 |
| • I am able to be in contact with patients who cannot be easily delivered to the clinic through telemedicine services. | ||
| Record | • I can gather correct information about the patient by using telemedicine. | Rho et al. 47 , Whitten et al. 85 , Sandberg et al. 75 |
| • I can easily record a patient's health condition with telemedicine services. | ||
| • Because of the precise record keeping of the patients in telemedicine, it enables me to provide proper healthcare service to my patients. |
Questions regarding marker variable 94
“Once I have come to a conclusion, I’m not likely to change my mind”; “I do not change my mind easily”; “My views are very consistent over time”.
Footnotes
Author's note: Siow-Kian Tan, School of Economics and Management, Xiamen University Malaysia, Sepang, Malaysia.
Contributorship: Siow-Hooi Tan: conceptualization, methodology, writing – review & editing, software, and funding acquisition. Chee-Kuan Wong: conceptualization and data collection. Yee-Yann Yap: writing - draft preparation, and methodology. Siow-Kian Tan: writing – review & editing and visualization.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical Approval: This study has obtained formal approval from the Medical Research Ethics Committee of University of Malaya Medical Centre (Approval Number: 2021111-10719). Informed written consent was obtained from all survey respondents prior to their participation. Respondents who participated in the survey were asked to read the ethical statement posted at the top of the form and proceed only if they agree. The collected data is treated with the utmost confidentiality.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was supported by Multimedia University (MMUI/220112).
Guarantor: Siow-Hooi Tan.
ORCID iD: Siow-Hooi Tan https://orcid.org/0000-0001-6366-5606
References
- 1.Ong AKS, Kurata YB, Castro SADG, et al. Factors influencing the acceptance of telemedicine in the Philippines. Technol Soc 2022; 70: 102040. [Google Scholar]
- 2.WHO. Global spending on health: rising to the pandemic’s challenges, https://apps.who.int/iris/handle/10665/365133 (2022).
- 3.ATA. Telehealth basics, https://www.americantelemed.org/resource/why-telemedicine/.
- 4.Smith AC, Thomas E, Snoswell CL, et al. Telehealth for global emergencies: implications for coronavirus disease 2019 (COVID-19). J Telemed Telecare 2020; 26: 309–313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pylypchuk Y, Barker W. Use of Telemedicine among Office-Based Physicians, 2021. Washington: DC: ONC Data Brief, no. 65. Office of the National Coordinator for Health Information Technology, 2023. [Google Scholar]
- 6.Rahman NA, Husin M, Dahian K, et al. Job satisfaction of public and private primary care physicians in Malaysia: analysis of findings from QUALICO-PC. Hum Resour Health 2019; 17: 82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.WHO. Global Health Workforce statistics database. World Health Organization, https://www.who.int/data/gho/data/themes/topics/health-workforce (2023).
- 8.MHM. 2023 Health facts: reference data for the year 2022, https://www.moh.gov.my/moh/resources/Penerbitan/Penerbitan Utama/HEALTH FACTS/Health_Facts_2022-updated.pdf (2023).
- 9.Lim HM, Sivasampu S, Khoo EM, et al. Chasm in primary care provision in a universal health system: findings from a nationally representative survey of health facilities in Malaysia. PLoS One 2017; 12: e0172229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lawrence K, Nov O, Mann D, et al. The impact of telemedicine on Physicians’ after-hours electronic health record “work outside work” during the COVID-19 pandemic: retrospective cohort study. JMIR Med Informatics 2022; 10: e34826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ng SW, Hwong WY, Husin M, et al. Assessing the availability of teleconsultation and the extent of its use in Malaysian public primary care clinics: cross-sectional study. JMIR Form Res 2022; 6: e34485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pang JS. New normal comes with big changes: Telemedicine to the fore. MIMS News, 12 May 2020.
- 13.Thong HK, Kit Chung Wong D, Gendeh HS, et al. Perception of telemedicine among medical practitioners in Malaysia during COVID-19. J Med Life 2021; 14: 468–480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cobelli N, Cassia F, Zardini A, et al. Pharmacies providing health services: attitudes toward eHealth in Italy. J Retail Consum Serv 2024; 76: 103568. [Google Scholar]
- 15.Vidal-Silva C, Sánchez-Ortiz A, Serrano-Malebrán J, et al. Social influence, performance expectancy, and price value as determinants of telemedicine services acceptance in Chile. Heliyon 2024; 10: e27067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pereira FV, Tavares J, Oliveira T. Adoption of video consultations during the COVID-19 pandemic. Internet Interv 2023; 31: 100602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kabra G, Sangroya D. Understanding behavioral intention to use telemedicine in healthcare: Insights from medical practitioners. In: AIP Conference Proceedings. 2023.
- 18.Lu W, Wei D, Li C, et al. How to promote telemedicine patient adoption behavior for greener healthcare? J Clean Prod 2024; 434: 139884. [Google Scholar]
- 19.Xiong J, Zuo M. Factors influencing health care professionals’ adoption of mobile platform of medical and senior care in China. Inf Manag 2023; 60: 103798. [Google Scholar]
- 20.Ma Q, Sun D, Tan Z, et al. Usage and perceptions of telemedicine among health care professionals in China. Int J Med Inform 2022; 166: 104856. [DOI] [PubMed] [Google Scholar]
- 21.Wu D, Gu H, Gu S, et al. Individual motivation and social influence: a study of telemedicine adoption in China based on social cognitive theory. Heal Policy Technol 2021; 10: 100525. [Google Scholar]
- 22.Kamal SA, Shafiq M, Kakria P. Investigating acceptance of telemedicine services through an extended technology acceptance model (TAM). Technol Soc 2020; 60: 101212. [Google Scholar]
- 23.Yap Y-Y, Tan S-KS-H, Tan S-KS-H, et al. Integrating the capability approach and technology acceptance model to explain the elderly’s use intention of online grocery shopping. Telemat Informatics 2022; 72: 101842. [Google Scholar]
- 24.Attié E, Meyer-Waarden L. The acceptance and usage of smart connected objects according to adoption stages: an enhanced technology acceptance model integrating the diffusion of innovation, uses and gratification and privacy calculus theories. Technol Forecast Soc Change 2022; 176: 121485. [Google Scholar]
- 25.Wang Y, Meister DB, Gray PH. Social influence and knowledge management systems use: evidence from panel data. MIS Q 2013; 37: 299–313. [Google Scholar]
- 26.Ftouni R, AlJardali B, Hamdanieh M, et al. Challenges of telemedicine during the COVID-19 pandemic: a systematic review. BMC Med Inform Decis Mak 2022; 22: 207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Garavand A, Aslani N, Nadri H, et al. Acceptance of telemedicine technology among physicians: a systematic review. Informatics Med Unlocked 2022; 30: 100943. [Google Scholar]
- 28.Zailani S, Gilani MS, Nikbin D, et al. Determinants of telemedicine acceptance in selected public hospitals in Malaysia: clinical perspective. J Med Syst 2014; 38: 111. [DOI] [PubMed] [Google Scholar]
- 29.Zakerabasali S, Ayyoubzadeh SM, Baniasadi T, et al. Mobile health technology and healthcare providers: systemic barriers to adoption. Healthc Inform Res 2021; 27: 267–278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Du Y, Zhou Q, Cheng W, et al. Factors influencing adoption and use of telemedicine services in rural areas of China: mixed methods study. JMIR Public Heal Surveill 2022; 8: e40771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Davis FD, Bagozzi RP, Warshaw PR. User acceptance of computer technology: a comparison of two theoretical models. Manage Sci 1989; 35: 982–1003. [Google Scholar]
- 32.Kelman HC. Compliance, identification, and internalization: three processes of attitude change. J Conflict Resolut 1958; 2: 51–60. [Google Scholar]
- 33.Cobelli N, Cassia F, Donvito R. Pharmacists’ attitudes and intention to adopt telemedicine: integrating the market-orientation paradigm and the UTAUT. Technol Forecast Soc Change 2023; 196: 122871. [Google Scholar]
- 34.Klingberg A, Sawe HR, Hammar U, et al. m-Health for burn injury consultations in a low-resource setting: an acceptability study among health care providers. Telemed e-Health 2020; 26: 395–405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Schmitz A, Díaz-Martín AM, Guillén MJY. Modifying UTAUT2 for a cross-country comparison of telemedicine adoption. Comput Human Behav 2022; 130: 107183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Arfi WB, Nasr IB, Kondrateva G, et al. The role of trust in intention to use the IoT in eHealth: application of the modified UTAUT in a consumer context. Technol Forecast Soc Change 2021; 167: 120688. [Google Scholar]
- 37.Rajak M, Shaw K. An extension of technology acceptance model for mHealth user adoption. Technol Soc 2021; 67: 101800. [Google Scholar]
- 38.Yamin MAY, Alyoubi BA. Adoption of telemedicine applications among Saudi citizens during COVID-19 pandemic: an alternative health delivery system. J Infect Public Health 2020; 13: 1845–1855. [DOI] [PubMed] [Google Scholar]
- 39.Kim E, Han S. Investigating the digital health acceptance of Korean baby boomers: comparative study of telemedicine and wearable healthcare devices. Heal Policy Technol 2023; 12: 100727. [Google Scholar]
- 40.Cobelli N, Cassia F, Burro R. Factors affecting the choices of adoption/non-adoption of future technologies during coronavirus pandemic. Technol Forecast Soc Change 2021; 169: 120814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Upadhyay N, Kamble A, Navare A. Virtual healthcare in the new normal: Indian healthcare consumers adoption of electronic government telemedicine service. Gov Inf Q 2023; 40: 101800. [Google Scholar]
- 42.Ahmed MH, Awol SM, Kanfe SG, et al. Willingness to use telemedicine during COVID-19 among health professionals in a low income country. Informatics Med Unlocked 2021; 27: 100783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Yuen KF, Chua JY, Li X, et al. The determinants of users’ intention to adopt telehealth: health belief, perceived value and self-determination perspectives. J Retail Consum Serv 2023; 73: 103346. [Google Scholar]
- 44.Hubona GS, Geitz S. External variables, beliefs, attitudes and information technology usage behavior. In: Proceedings of the Thirtieth Hawaii International Conference on System Sciences. IEEE Comput. Soc. Press, pp. 21–28. [Google Scholar]
- 45.Rouidi M, Elouadi AE, Hamdoune A, et al. TAM-UTAUT and the acceptance of remote healthcare technologies by healthcare professionals: a systematic review. Informatics Med Unlocked 2022; 32: 101008. [Google Scholar]
- 46.Alexandra S, Handayani PW, Azzahro F. Indonesian Hospital telemedicine acceptance model: the influence of user behavior and technological dimensions. Heliyon 2021; 7: e08599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Rho MJ, Choi I, young , et al. Predictive factors of telemedicine service acceptance and behavioral intention of physicians. Int J Med Inform 2014; 83: 559–571. [DOI] [PubMed] [Google Scholar]
- 48.Saigi-Rubió F, Jiménez-Zarco A, Torrent-Sellens J. Determinants of the intention to use telemedicine: evidence from primary care physicians. Int J Technol Assess Health Care 2016; 32: 29–36. [DOI] [PubMed] [Google Scholar]
- 49.Kim J, DelliFraine JL, Dansky KH, et al. Physicians’ acceptance of telemedicine technology: an empirical test of competing theories. Int J Inf Syst Change Manag 2010; 4: 210. [Google Scholar]
- 50.Malhotra Y, Galletta D. A multidimensional commitment model of volitional systems adoption and usage behavior. J Manag Inf Syst 2005; 22: 117–151. [Google Scholar]
- 51.Venkatesh V, Morris MG, Davis GB, et al. User acceptance of information technology: toward a unified view. MIS Q 2003; 27: 425. [Google Scholar]
- 52.Lu Z, Cui T, Tong Y, et al. Examining the effects of social influence in pre-adoption phase and initial post-adoption phase in the healthcare context. Inf Manag 2020; 57: 103195. [Google Scholar]
- 53.Venkatesh V, Davis FD. A theoretical extension of the technology acceptance model: four longitudinal field studies. Manage Sci 2000; 46: 186–204. [Google Scholar]
- 54.Deutsch M, Gerard HB. A study of normative and informational social influences upon individual judgment. J Abnorm Soc Psychol 1955; 51: 629–636. [DOI] [PubMed] [Google Scholar]
- 55.Goh JM, Gao G(Gordon), Agarwal R. Evolving work routines: adaptive routinization of information technology in healthcare. Inf Syst Res 2011; 22: 565–585. [Google Scholar]
- 56.Tong Y, Tan C-H, Teo H-H. Direct and indirect information system use: a multimethod exploration of social power antecedents in healthcare. Inf Syst Res 2017; 28: 690–710. [Google Scholar]
- 57.Cialdini RB, Goldstein NJ. Social influence: compliance and conformity. Annu Rev Psychol 2004; 55: 591–621. [DOI] [PubMed] [Google Scholar]
- 58.Bagozzi RP, Dholakia UM. Intentional social action in virtual communities. J Interact Mark 2002; 16: 2–21. [Google Scholar]
- 59.Cheung CMK, Lee MKO. A theoretical model of intentional social action in online social networks. Decis Support Syst 2010; 49: 24–30. [Google Scholar]
- 60.Lewis W, Agarwal R, Sambamurthy V. Sources of influence on beliefs about information technology use: an empirical study of knowledge workers. MIS Q 2003; 27: 657. [Google Scholar]
- 61.Moore GC, Benbasat I. Development of an instrument to measure the perceptions of adopting an information technology innovation. Inf Syst Res 1991; 2: 192–222. [Google Scholar]
- 62.Kummer T-F, Schäfer K, Todorova N. Acceptance of hospital nurses toward sensor-based medication systems: a questionnaire survey. Int J Nurs Stud 2013; 50: 508–517. [DOI] [PubMed] [Google Scholar]
- 63.Jeng DJ-F, Tzeng G-H. Social influence on the use of clinical decision support systems: revisiting the unified theory of acceptance and use of technology by the fuzzy DEMATEL technique. Comput Ind Eng 2012; 62: 819–828. [Google Scholar]
- 64.Chong AYL, Blut M, Zheng S. Factors influencing the acceptance of healthcare information technologies: a meta-analysis. Inf Manag 2022; 59: 103604. [Google Scholar]
- 65.Liang H, Xue Y, Wu L. Ensuring Employees’ IT compliance: carrot or stick? Inf Syst Res 2013; 24: 279–294. [Google Scholar]
- 66.Li C-Y. Persuasive messages on information system acceptance: a theoretical extension of elaboration likelihood model and social influence theory. Comput Human Behav 2013; 29: 264–275. [Google Scholar]
- 67.Podsakoff PM, Bommer WH, Podsakoff NP, et al. Relationships between leader reward and punishment behavior and subordinate attitudes, perceptions, and behaviors: a meta-analytic review of existing and new research. Organ Behav Hum Decis Process 2006; 99: 113–142. [Google Scholar]
- 68.Sims HP. Further thoughts on punishment in organizations. Acad Manag Rev 1980; 5: 133. [Google Scholar]
- 69.Trevino LK. The social effects of punishment in organizations: a justice perspective. Acad Manag Rev 1992; 17: 647–676. [Google Scholar]
- 70.Malik MAR, Butt AN, Choi JN. Rewards and employee creative performance: moderating effects of creative self-efficacy, reward importance, and locus of control. J Organ Behav 2015; 36: 59–74. [Google Scholar]
- 71.Karahanna E, Straub DW, Chervany NL. Information technology adoption across time: a cross-sectional comparison of Pre-adoption and post-adoption beliefs. MIS Q 1999; 23: 183. [Google Scholar]
- 72.Bulgurcu B, Cavusoglu H, Benbasat I. Information security policy compliance: an empirical study of rationality-based beliefs and information security awareness. MIS Q 2010; 34: 523. [Google Scholar]
- 73.Bagozzi RP, Lee K-H. Multiple routes for social influence: the role of compliance, internalization, and social identity. Soc Psychol Q 2002; 65: 226. [Google Scholar]
- 74.Johnston AC, Warkentin M, Siponen M. An enhanced fear appeal rhetorical framework: leveraging threats to the human asset through sanctioning rhetoric. MIS Q 2015; 39: 113–134. [Google Scholar]
- 75.Sandberg J, Trief PM, Izquierdo R, et al. A qualitative study of the experiences and satisfaction of direct telemedicine providers in diabetes case management. Telemed e-Health 2009; 15: 742–750. [DOI] [PubMed] [Google Scholar]
- 76.Adenuga KI, Iahad NA, Miskon S. Towards reinforcing telemedicine adoption amongst clinicians in Nigeria. Int J Med Inform 2017; 104: 84–96. [DOI] [PubMed] [Google Scholar]
- 77.Hung S-Y, Ku Y-C, Chien J-C. Understanding physicians’ acceptance of the medline system for practicing evidence-based medicine: a decomposed TPB model. Int J Med Inform 2012; 81: 130–142. [DOI] [PubMed] [Google Scholar]
- 78.McKee GB, Pierce BS, Donovan EK, et al. Examining models of psychologists’ telepsychology use during the COVID-19 pandemic: a national cross-sectional study. J Clin Psychol 2021; 77: 2405–2423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Bandura A. Self-efficacy mechanism in human agency. Am Psychol 1982; 37: 122–147. [Google Scholar]
- 80.Venkatesh V, Davis FD. A model of the antecedents of perceived ease of use: development and test. Decis Sci 1996; 27: 451–481. [Google Scholar]
- 81.Zobair KM, Sanzogni L, Sandhu K. Expectations of telemedicine health service adoption in rural Bangladesh. Soc Sci Med 2019; 238: 112485. [DOI] [PubMed] [Google Scholar]
- 82.Deng Z, Liu S. Understanding consumer health information-seeking behavior from the perspective of the risk perception attitude framework and social support in mobile social media websites. Int J Med Inform 2017; 105: 98–109. [DOI] [PubMed] [Google Scholar]
- 83.Rahi S, Khan MM, Alghizzawi M. Factors influencing the adoption of telemedicine health services during COVID-19 pandemic crisis: an integrative research model. Enterp Inf Syst 2021; 15: 769–793. [Google Scholar]
- 84.Venkatesh V. Determinants of perceived ease of use: integrating control, intrinsic motivation, and emotion into the technology acceptance model. Inf Syst Res 2000; 11: 342–365. [Google Scholar]
- 85.Whitten P, Doolittle G, Mackert M. Providers’ acceptance of telehospice. J Palliat Med 2005; 8: 730–735. [DOI] [PubMed] [Google Scholar]
- 86.Bhatia R. Telehealth and COVID-19: using technology to accelerate the curve on access and quality healthcare for citizens in India. Technol Soc 2021; 64: 101465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Palmas W, Teresi J, Weinstock RS, et al. Acceptability to primary care providers of telemedicine in diabetes case management. J Telemed Telecare 2008; 14: 306–308. [DOI] [PubMed] [Google Scholar]
- 88.Compeau DR, Higgins CA. Computer self-efficacy: development of a measure and initial test. MIS Q 1995; 19: 189. [Google Scholar]
- 89.Martínez A, Everss E, Rojo-Álvarez JL, et al. A systematic review of the literature on home monitoring for patients with heart failure. J Telemed Telecare 2006; 12: 234–241. [DOI] [PubMed] [Google Scholar]
- 90.O’Reilly CA, Chatman J. Organizational commitment and psychological attachment: the effects of compliance, identification, and internalization on prosocial behavior. J Appl Psychol 1986; 71: 492–499. [Google Scholar]
- 91.Vandenberg RJ, Self RM, Seo JH. A critical examination of the internalization, identification, and compliance commitment measures. J Manage 1994; 20: 123–140. [Google Scholar]
- 92.Chin WW. The partial least squares approach to structural equation modelling. In: Marcoulides GA. (ed.) Modern methods for business research. Mahwah, NJ: Lawrence Erlbaum Associates Publishers, 1998, pp.295–336. [Google Scholar]
- 93.Lindell MK, Whitney DJ. Accounting for common method variance in cross-sectional research designs. J Appl Psychol 2001; 86: 114–121. [DOI] [PubMed] [Google Scholar]
- 94.Malhotra NK, Kim SS, Patil A. Common method variance in IS research: a comparison of alternative approaches and a reanalysis of past research. Manage Sci 2006; 52: 1865–1883. [Google Scholar]
- 95.Hair JF, Risher JJ, Sarstedt M, et al. When to use and how to report the results of PLS-SEM. Eur Bus Rev 2019; 31: 2–24. [Google Scholar]
- 96.Petter S, Straub D, Rai A. Specifying formative constructs in information systems research. MIS Q 2007; 31: 623. [Google Scholar]
- 97.Cenfetelli B. Interpretation of formative measurement in information systems research. MIS Q 2009; 33: 689. [Google Scholar]
- 98.Hair JFJ, Sarstedt M, Hopkins L, et al. Partial least squares structural equation modeling (PLS-SEM). Eur Bus Rev 2014; 26: 106–121. [Google Scholar]
- 99.Henseler J, Ringle CM, Sinkovics RR. The use of partial least squares path modeling in international marketing. In: Sinkovics RR, Ghauri PN. (eds) Advances in international marketing. Bingley, UK: Emerald Group, 2009, pp.277–320. [Google Scholar]
- 100.Franke G, Sarstedt M. Heuristics versus statistics in discriminant validity testing: a comparison of four procedures. Internet Res 2019; 29: 430–447. [Google Scholar]
- 101.Hair JF, Sarstedt M, Ringle CM, et al. Advanced issues in partial least squares structural equation modeling. Thousand Oaks, CA: Sage Publications, 2017. [Google Scholar]
- 102.Shmueli G, Sarstedt M, Hair JF, et al. Predictive model assessment in PLS-SEM: guidelines for using PLSpredict. Eur J Mark 2019; 53: 2322–2347. [Google Scholar]
- 103.Hair JF, Hult GTMTM, Ringle C, et al. A primer on partial least squares structural equation modeling (Pls-Sem). Thousand Oaks, CA: Sage Publications, 2016. [Google Scholar]
- 104.Aldholay AH, Isaac O, Abdullah Z, et al. The role of transformational leadership as a mediating variable in DeLone and McLean information system success model: the context of online learning usage in Yemen. Telemat Informatics 2018; 35: 1421–1437. [Google Scholar]
- 105.Chau PYK, Hu PJ-H. Investigating healthcare professionals’ decisions to accept telemedicine technology: an empirical test of competing theories. Inf Manag 2002; 39: 297–311. [Google Scholar]
- 106.Hoque MR, Bao Y. Cultural influence on adoption and use of e-health: evidence in Bangladesh. Telemed e-Health 2015; 21: 845–851. [DOI] [PubMed] [Google Scholar]