Most patients admitted to intensive care require some form of respiratory support. This is usually because of hypoxaemia or ventilatory failure, or both. The support offered ranges from oxygen therapy by face mask, through non-invasive techniques such as continuous positive airways pressure, to full ventilatory support with endotracheal intubation.
Oxygen therapy
Oxygen is given to treat hypoxaemia. Patients should initially be given a high concentration. The amount can then be adjusted according to the results of pulse oximetry and arterial blood gas analysis. The dangers of reducing hypoxic drive have been overemphasised; hypoxaemia is more dangerous than hypercapnia. The theoretical dangers of oxygen toxicity are unimportant if the patient is hypoxaemic.
Oxygen is usually given by face mask, although nasal prongs or cannulas may be better tolerated. A fixed performance, high flow, air entrainment mask can provide a known fractional inspired oxygen concentration (Fio2) within the range 0.24-0.60. The fractional inspired oxygen concentration is not known with the more common variable performance masks. The maximum concentration is 0.6 unless a reservoir bag is added to the mask.
Non-invasive respiratory support
If the patient remains hypoxaemic on high flow oxygen (15 l/min) continuous positive airways pressure (CPAP) may be used. The technique improves oxygenation by recruiting underventilated alveoli and so is most successful in clinical situations where alveoli are readily recruited, such as acute pulmonary oedema and postoperative atelectasis. It is also helpful in immunocompromised patients with pneumonia. As intubation is avoided the risks of nosocomial pneumonia are reduced. The continuous positive airways pressure mask often becomes uncomfortable and gastric distension may occur. Patients must therefore be cooperative, able to protect their airway, and have the strength to breathe spontaneously and cough effectively.
Indications for intubation and ventilation
Protect the airway—for example, facial trauma or burns, unconscious patient
Treat profound hypoxaemia—for example, pneumonia, cardiogenic pulmonary oedema, acute respiratory distress syndrome
Postoperative care—for example, after cardiothoracic surgery and other major, complicated, or prolonged surgery
Allow removal of secretions—for example, myasthenia gravis, Guillain-Barré syndrome
Rest exhausted patients—for example, severe asthma
Avoid or control hypercapnia—for example, acute brain injury, hepatic coma, chronic obstructive airways disease
Non-invasive ventilation refers to ventilatory support without tracheal intubation. This can be used as a first step in patients who require some ventilatory support and who are not profoundly hypoxaemic. Ventilation through a nasal or face mask may avoid the need for intubation, especially in exacerbations of chronic obstructive airways disease. Some patients with chronic ventilatory failure rely on long term non-invasive ventilation. It may also have a place during weaning from conventional ventilation. External negative pressure ventilation, historically provided by an “iron lung,” is now provided by a cuirass system.
Ventilatory support
Endotracheal intubation and ventilation is the next step in the management of respiratory failure. Clinical symptoms and signs are generally more useful than arterial blood gas analysis or measurements of peak expiratory flow rate and vital capacity in deciding the need for intubation.. However, some findings confirm the imminent need for ventilation. These include hypoxaemia in patients receiving maximum oxygen therapy (Pao2<8 kPa, or Sao2<90%), hypercapnia with impairment of conscious level, and a falling vital capacity in patients with neuromuscular disorders.
Indicators of respiratory distress
Tachypnoea, dyspnoea
Sweating
Tachycardia and bounding pulse
Agitation, restlessness, diminished conscious level, unwilling to lie flat
Use of accessory muscles, intercostal recession
Abdominal paradox (abdomen moves inward during inspiration)
Respiratory alternans (thoracic movement then abdominal movement)
Cyanosis or pallor
Management of the airway
Endotracheal intubation can be extremely hazardous in critically ill patients with respiratory and often cardiovascular failure. Continuous monitoring, particularly of heart rate and blood pressure, is essential and resuscitation drugs must be immediately available.
Potential problems during intubation
Hypotension
Reduced intrinsic sympathetic drive
Reduced cardiac output
Severe hypoxaemia
Regurgitation and aspiration of gastric contents
Arrhythmias
Electrolyte disturbances, especially hyperkalaemia after suxamethonium
Hypotension follows induction of anaesthesia because of the direct cardiovascular effects of the drugs given. Unconsciousness also reduces intrinsic sympathetic drive. Positive pressure ventilation reduces venous return to the heart and reduces cardiac output.
Tracheostomies are usually done electively when intubation is likely to be prolonged (over 14 days). They may also be done for the patient’s comfort and to facilitate weaning from the ventilator. Tracheostomy is often done as a percutaneous procedure in intensive care. Complications of tracheostomy include misplacement or displacement of the tube, bleeding, infection, failure of the stoma to heal, and tracheal stenosis. However, because patients tolerate a tracheostomy much better than an orotracheal tube, sedation can usually be reduced, weaning is more rapid, and the stay in intensive care is reduced. A minitracheostomy may help with tracheal toilet in patients with copious secretions and poor cough effort.
Ventilator strategy
The choice of ventilatory mode and settings such as tidal volume, respiratory rate, positive end expiratory pressure (PEEP), and the ratio of inspiratory to expiratory time depends on the patient’s illness. In asthma, for example, a prolonged expiratory phase may be required for lung deflation, whereas in patients with atelectasis or other forms of reduced lung volume the emphasis is towards recruiting alveoli with positive end expiratory pressure or a prolonged inspiratory phase.
Lung protective ventilation strategy
The strategy aims to maintain alveolar volume by
Using lung recruitment manoeuvres and positive end expiratory pressure to maximise and maintain alveolar volume
Avoiding alveolar overdistension by limiting tidal volume or airway pressure, or both
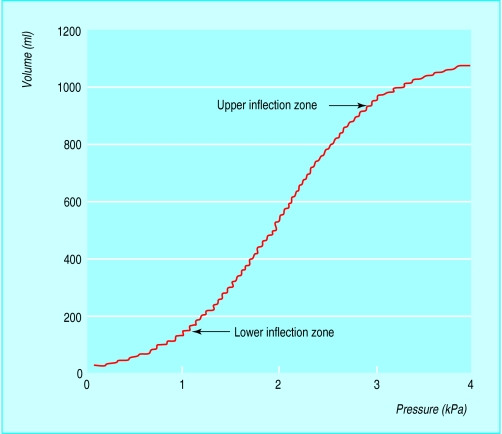
Damage to lungs can be exacerbated by mechanical ventilation, possibly because of overdistension of alveoli and the repeated opening and collapse of distal airways. Some evidence exists for benefit from a lung protective ventilatory strategy using positive end expiratory pressure or prolonged inspiration to maintain alveolar volume, and limiting tidal volumes and peak airway pressures. This may result in increased arterial carbon dioxide pressure (permissive hypercapnia). Serial measurements of airway pressure and tidal volume allow lung compliance to be optimised. Compliance indicates alveolar recruitment, and reduces the risks of overdistension.
Methods of ventilation
No consensus exists on the best method of ventilation. In volume controlled methods the ventilator delivers a preset tidal volume. The inspiratory pressure depends on the resistance and compliance of the respiratory system. In pressure controlled ventilation the delivered pressure is preset. Tidal volume varies according to the resistance and compliance of the respiratory system. Pressure controlled ventilation has become popular for severe acute respiratory distress syndrome as part of the lung protective strategy. As well as limiting peak airway pressure, the distribution of gas may be improved within the lung. Pressure controlled ventilation is often used with a long inspiratory phase (inverse ratio ventilation) to maintain adequate alveolar recruitment.
In high frequency techniques gas is delivered to the airway by oscillation or jet ventilation. The tidal volumes achieved are small but gas exchange still occurs. The role of high frequency techniques in respiratory support is not yet established.
Methods of ventilation that allow the patient to breathe spontaneously are thought to be advantageous. Modern ventilators have sensitive triggers and flow patterns that can adapt to the patient’s needs, thus reducing the work of breathing. In synchronised intermittent mandatory ventilation a set number of breaths are delivered by the ventilator and the patient can breathe between these breaths. This method is often used during weaning, often with pressure support, by which the ventilator enhances the volume of each spontaneous breath up to a predetermined positive pressure. Biphasic airway pressure is similar to continuous positive airways pressure ventilation but pressure is set at two levels. The ventilator switches between the levels, thus augmenting alveolar ventilation.
Monitoring ventilatory therapy
Pulse oximetry and measurement of end tidal carbon dioxide concentration allow continuous monitoring of oxygenation and ventilation. End tidal carbon dioxide concentration is roughly equal to arterial carbon dioxide partial pressure in normal subjects but may differ widely in critically ill patients with ventilation-perfusion mismatch. Nevertheless, monitoring end tidal carbon dioxide may be useful in neurointensive care, when transferring critically ill patients, and for confirming tracheal intubation. Adequacy of ventilation should be confirmed regularly by arterial blood gas analysis. Tolerance to ventilation can be assessed using a simple scale.
Ventilation assessment scale
Tolerates ventilation
Tolerates ventilation most of the time; some transient desaturation or coughing on manoeuvres such as tracheal suction, turning, etc
Moderate desaturation on coughing or above manoeuvres that resolves spontaneously
Severe or prolonged desaturation on coughing or above manoeuvres that requires intervention
Intolerant of mechanical ventilation, requires manual intervention
Paralysed
Preparation for weaning from the ventilator
Ensure
Clear airway
Adequate oxygenation
Adequate carbon dioxide clearance
Control of
Precipitating illness
Fever and infection
Pain
Agitation
Depression
Optimisation of
Nutritional state
Electrolytes (potassium, phosphate, magnesium)
Beware
Excessive carbon dioxide production from overfeeding
Sleep deprivation
Acute left heart failure
Weaning from the ventilator
Several techniques are available for weaning. All are likely to fail unless the patient is well prepared. Clinical assessment is the most important issue in deciding when to wean a patient from the ventilator. The factors considered are similar to the indications for respiratory support. The patient should be adequately oxygenated (Pao2>8 kPa with fractional inspired oxygen <0.6); be able to maintain normocapnia; be able to meet the increased work of breathing; and be conscious and responsive. Weaning techniques allow the patient to breathe spontaneously for increasing periods or to gradually reduce the level of ventilatory support. Recently weaned patients should continue to be closely monitored for secondary deterioration. Patients are extubated after they are weaned from the ventilator and can breathe unaided. Patients also need to be able to protect their airway once it is no longer protected by an endotracheal tube. This means they must be alert, able to swallow without aspiration, and able to cough well enough to clear secretions.
Other aspects of respiratory support
Humidification
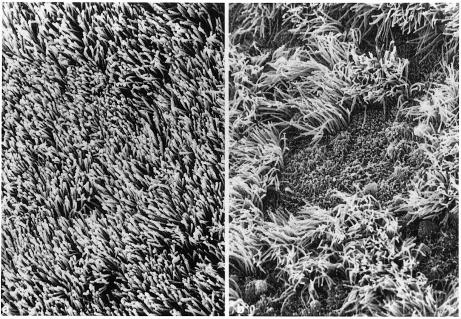
Inadequate humidification of inspired gases destroys the ciliated epithelium lining the upper airway. This stops secretions from being cleared from the lungs and increases the risk of infection. Piped medical oxygen and air are completely dry. The upper airway may not be able to supply enough heat and moisture to fully saturate them, especially when much of the upper airway is bypassed by tracheal intubation. Additional humidification is therefore necessary.
Physiotherapy
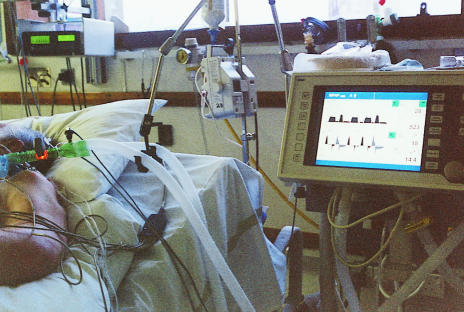
Patients who are intubated cannot clear secretions effectively because of reduced conscious level, poor cough effort, and discomfort. Regular chest physiotherapy and tracheal suction are essential.
Position
Regular turning to avoid pressure sores also helps mobilise and clear secretions. Patients who are too unstable to be turned regularly may benefit from being nursed on special beds that allow some degree of rotation.
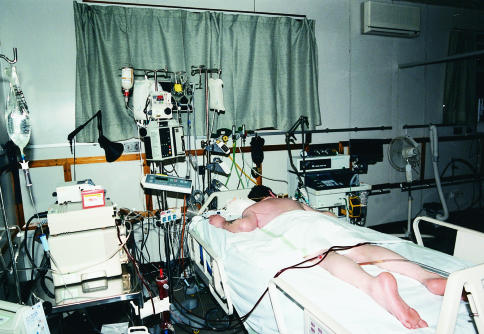
Patients with resistant hypoxaemia may benefit from being turned prone. The improved oxygenation probably results from normalisation of pleural pressure gradients within the lung.
Pharmacological adjuncts
Inhaled nitric oxide may improve oxygenation by dilating pulmonary vessels passing alongside ventilated alveoli. Although it is widely used, and often effective in increasing arterial oxygen tension in patients with acute respiratory distress syndrome, there is no evidence of improved survival. Nitric oxide remains unlicensed for this indication.
Steroids have a limited role in the acute management of ventilated patients except for treating the underlying disease—for example, asthma. However, there is evidence that they improve pulmonary function in the later, fibroproliferative, phase of acute respiratory distress syndrome.
Sedation
Ventilated patients generally require sedation to tolerate both ventilation and the presence of an endotracheal tube. The aim is for the patient to be comfortable at all times. In the past, ventilation could be controlled only if the patient was heavily sedated or even paralysed. Sophisticated ventilators now allow less sedation but patients still require analgesia for pain and relief of anxiety and distress.
Indications for analgesia and sedation
| • Allow effective ventilation | • Relieve distress |
| • Reduce oxygen demand | • Facilitate sleep |
| • Provide analgesia | • Provide amnesia |
| • Reduce anxiety | • Reduce depression |
Indications for muscle relaxants
Allow intubation and other procedures
Allow control of ventilation where respiratory drive is very high—for example, permissive hypercapnia
Treat certain diseases—for example, tetanus
Reduce oxygen demand while oxygenation is critical
Control carbon dioxide pressure and prevent increases in intracranial pressure—for example, in head injury
Patients have individual needs and different indications for analgesia and sedation. Muscle relaxants are now used infrequently. Compassionate care and effective communication help patients, but drugs are often necessary to keep them comfortable.
Assessment of sedation
+3 Agitated and restless
+2 Awake and uncomfortable
+1 Aware but calm
0 Roused by voice
−1 Roused by touch
−2 Roused by painful stimuli
−3 Cannot be roused
A Natural sleep
P Paralysed
Sedatives, however, have some adverse effects. The parent drug or active metabolites may accumulate because of renal failure and have prolonged action. There may also be circulatory effects—for example, hypotension. Tolerance sometimes occurs. Patients may develop withdrawal syndromes when the drug is stopped, while altered sleep patterns may produce sleep deprivation. Some patients develop ileus, which may impair feeding.
Because critically ill patients cannot usually say whether they are comfortable, anxiety, depression, and even pain may be difficult to assess. This assessment tends to be subjective and various scoring systems are used, most being based on the patient’s response to different stimuli.
Conclusion
Many patients who would previously have died from respiratory failure now survive. Improved understanding and management of acute lung injury will hopefully lead to further improvements in survival. Appropriate treatment of hypoxia, and early referral to intensive care before complications arise, will also hopefully improve the outcome of critically ill patients.
Figure.
Oxygen masks and nasal cannula
Figure.
Continuous positive airways pressure requires a tight fitting mask and appropriate valve and breathing system
Figure.

Hayek oscillator provides external negative pressure ventilation
Figure.
A tracheostomy is more comfortable than an orotracheal tube
Figure.
Pressure-volume curve showing upper and lower inflection points
Figure.
Biphasic airway pressure improves alveolar ventilation
Figure.
Inadequate humidification of inspired gases causes loss of tracheal and bronchial cilia (right), which reduces clearance of secretions from the lungs
Figure.
Physiotherapy is important to help clear secretions in ventilated patients
Figure.
Nursing patients in prone position may help resistant hypoxaemia
Acknowledgments
The picture of cilia is reproduced with permission from Konrad F, Schiener R, Marx T, Georgieff M. Intensive Care Medicine 1995;21:482-9.
Footnotes
Maire P Shelly is consultant in anaesthesia and intensive care and Peter Nightingale is director of intensive care, Withington Hospital, Manchester.
The ABC of intensive care is edited by Mervyn Singer, reader in intensive care medicine, Bloomsbury Institute of Intensive Care Medicine, University College London and Ian Grant, director of intensive care, Western General Hospital, Edinburgh. The series was conceived and planned by the Intensive Care Society’s council and research subcommittee.