Most food is now produced by large farms, processed industrially, and sold in supermarkets and multinational food outlets. Modern food production has reduced the cost and increased the variety of food available, but this centralisation of the food supply presents an opportunity for foodborne pathogens and toxins to infect and poison large numbers of consumers.1 Furthermore, the globalisation of food trade means that food can become contaminated in one country and cause outbreaks of foodborne illness in another.2–4 Modern food production is so complex that a systematic approach is needed to identify the hazards at each point in the food chain.
Summary points
The centralisation and globalisation of foods increase the likelihood of pandemics of foodborne disease
People in developing countries are at greater risk from naturally occurring toxicants, foodborne disease, and contaminants in the food chain
The hazard critical control point concept is essential for assessing and managing risk
Special consideration is needed with regard to fish and shellfish
Concerted action needs to be taken to prohibit the use of antibiotics as growth promoters in animal production
Internationally agreed food standards are essential to facilitate trade in food between areas with food surplus and those with food deficit
Methods
I made an electronic search of the Medline database between January 1990 and May 1999, using the search terms food poisoning and epidemiology, food additives and adverse effects, pesticides and poisoning, and food contamination. Statistical information on the incidence of food poisoning and adverse reactions was obtained from the Public Health Laboratory Services; Centers for Disease Control and Prevention, Atlanta; and the UK Department of Health. Data on food surveillance was obtained from the Ministry of Agriculture, Fisheries, and Food. Information on risk assessment was derived from working papers of the WHO/FAO Codex Alimentarius Commission and the European Commission Scientific Committee for Food.
Hazards from food
An important development in improving food safety has been the application of the hazard critical control point concept (HACCP), which is a systematic approach to identifying, assessing, and controlling hazards, borrowed from the aerospace industry.5 It can be applied to all sectors of the food chain from primary production through food processing, manufacture, distribution, and retailing, to the point of consumption. Its strength is that it focuses on identifying the main avenues of risk and tackling them (box).
Seven steps of HACCP
Analyse hazards: potential hazards associated with a food and measures to control those hazards are identified
Identify critical control points: these are points in the food chain at which the potential hazard can be controlled or eliminated
Establish preventive measures with critical limits for each control point: for a cooked food, for example, this might include setting the minimum cooking temperature and time required to ensure the elimination of any microbes
Establish procedures to monitor the critical control points
Establish corrective actions to be taken when monitoring shows that a critical limit has not been met
Establish procedures to verify that the system is working properly
Establish effective record keeping to document the HACCP system: this would include records of hazards and their control methods, the monitoring of safety requirements, and action taken to correct potential problems
Adapted from the USA National Food Safety Initiative6
A food hazard is defined as “a biological, chemical or physical agent in, or condition of, food with the potential to cause an adverse health effect.”7 The acute hazards resulting from the consumption of food, such as allergy and food poisoning, are much easier to document than are the chronic harmful effects. The hazards associated with nutritional deficiency or nutritional imbalance (table 1) are recognised to be of great public health importance but are beyond the scope of this paper.
Table 1.
Risks associated with food hazards
| Food hazards | Risk level |
|
|---|---|---|
| Developing countries | Developed countries | |
| Nutritional deficiency | High | Low |
| Nutritional imbalance (for example, obesity, excess intakes of salt, saturated and trans fats) | Moderate | High |
| Natural occurring toxicants in food (for example, alkaloids, legume toxins, cyanogenic glycosides) | High | Low |
| Microbiological contamination (bacteria, viruses, parasites, mould, and algal toxins) | Very High | Moderate |
| Contaminants in food (heavy metals, organic chemicals) | Moderate | Low |
Risk is defined as “a function of the probability of an adverse health effect and the severity of that effect, consequential to a hazard(s) in food.”7 Risk analysis consists of three components: risk assessment, risk management, and risk communication. Risk assessment is the science of understanding hazards, how likely they are to occur, and the consequences if they do occur. The process involves identifying and characterising the hazards, assessing exposure, and characterising the risk (box). Risk management is the process of weighing policy alternatives in the light of the results of risk assessment and, if required, selecting and implementing appropriate control options, including regulatory measures. It is essential that the risk assessment and risk management processes are transparent and separated, as one is scientific and the other is political. Risk communication is defined as “the interactive exchange of information and opinions concerning risk among risk assessors, risk managers, consumers and other interested parties.”7 It is perhaps this last stage that is hardest to deal with, as the distinction between risk assessment and risk management becomes blurred. A major barrier to risk communication is a general lack of understanding by the public of relative risk as opposed to absolute risk.8 Furthermore, public perception of risk is distorted by media reporting.9
Risk analysis framework
Risk assessment
Hazard identification
Hazard characterisation
Exposure assessment
Risk characterisation
Risk management
Assess policy alternatives
Select and implement appropriate options
Interactive exchange of information and opinions
Risk communication
Naturally occurring toxicants in food
Naturally occurring toxicants are ubiquitous in plants.10 People in developing countries are at much greater risk from naturally occurring toxicants because they have a limited dietary repertoire, they may out of necessity eat food which would otherwise be regarded as unfit for human consumption, and they may lack the resources to process it effectively into a safe form.11,12 Naturally occurring toxicants pose a relatively low risk to health in developed countries because effective food processing and a varied diet decreases exposure. Two exceptions to this rule are the toxicants present in wild mushrooms and herbal products.10
Microbiological hazards
The effects of foodborne infection are not restricted to the gastrointestinal tract, as illustrated by viral hepatitis, tuberculosis, and haemolytic-uraemic syndrome caused by Escherischia coli O157. Microbiological contamination of food and water is the main cause of diarrhoea, which contributes to about 3 million deaths among children aged under 5 (mainly in developing countries).13 Foodborne parasitic diseases are also a major public health problem in developing countries but not in developed countries. In addition, mycotoxins such as aflatoxin are known to present acute and chronic health hazards, particularly in tropical countries. In developed countries routine surveillance of mycotoxins,14 controls on the imports of potentially contaminated materials, use of fungicides, and good storage conditions minimise exposure to mycotoxins. Algal toxins that accumulate in the marine food chain are a considerable hazard for some fish eating populations. Ciguatera is a sporadic form of human poisoning caused by the consumption of contaminated subtropical and tropical marine finfish (barracuda, grouper, snappers, mackerel) that causes neuropathy and can be fatal.15 Red tides of toxic algae known to cause paralytic and diarrhoetic shellfish poisoning affect waters around the British Isles between the months of May and August.16 Monitoring programmes minimise exposure of the population to these algal toxins.
The US National Food Safety Initiative attributes 9000 deaths and between 6.5 million and 33 million episodes of illness annually to foodborne microbial illness.6 In England and Wales, 300 deaths and 35 000 hospital admissions are attributed annually to infectious gastrointestinal diseases.17 Laboratory reports indicate that campylobacter, salmonella, rotavirus A, and small round structured viruses are the most commonly detected pathogens. Surveillance reports underestimate the true incidence of infectious gastrointestinal disease by two orders of magnitude; it is estimated that there are 9.4 million cases of infectious gastrointestinal disease in England each year.17 Table 2 shows the number of outbreaks reported by cause in the United Kingdom.
Table 2.
Infectious intestinal disease general outbreaks in England and Wales18
| Organism | No of outbreaks
|
||||||
|---|---|---|---|---|---|---|---|
| 1992 (n=372) | 1993 (n=456) | 1994 (n=486) | 1995 (n=833) | 1996 (n=734) | 1997 (n=561) | 1998 (n=570)* | |
| Clostridium perfringens | 32 | 36 | 22 | 25 | 22 | 28 | 11 |
| Salmonella enteritidis PT 4 | 94 | 108 | 60 | 73 | 61 | 79 | 44 |
| Salmonella enteritidis | 18 | 15 | 14 | 12 | 22 | 44 | 24 |
| Salmonella typhimurium | 22 | 19 | 20 | 19 | 18 | 20 | 7 |
| Salmonella virchow | 5 | 2 | 6 | 6 | 1 | 2 | 0 |
| Other salmonellas | 18 | 4 | 7 | 9 | 11 | 9 | 6 |
| Scombrotoxin | 1 | 2 | 8 | 9 | 6 | 7 | 4 |
| Campylobacter | 5 | 6 | 9 | 4 | 8 | 10 | 15 |
| Clostridium difficile | 4 | 8 | 36 | 32 | 30 | 9 | 23 |
| Cryptosporidium | 9 | 8 | 6 | 6 | 5 | 9 | 3 |
| Escherichia coli O157 | 5 | 8 | 5 | 10 | 10 | 16 | 11 |
| Rotavirus | 5 | 8 | 17 | 23 | 31 | 12 | 16 |
| Shigella sonnei | 28 | 14 | 4 | 0 | 4 | 1 | 1 |
| Small round structured virus | 55 | 133 | 154 | 367 | 314 | 128 | 197 |
| Other | 11 | 11 | 24 | 22 | 23 | 6 | 2 |
| Unknown | 53 | 73 | 92 | 215 | 163 | 181 | 206 |
Data for 1998 are provisional.
The emergence of new foodborne pathogens such as E coli O157, which has been detected in the faeces of up to 15% of British cattle, is of particular concern as beef is often consumed undercooked or rare. Intensive poultry production is linked to the epidemic of Salmonella enteridis phage type 4 that has emerged in Europe and the United States: S enteritidis can be detected in 1% of eggs and in about a fifth of all poultry.19 There is, however, some evidence that application of the hazard critical control point concept in poultry production is leading to a decline in S enteritidis infections in the United States and Europe.20 Providing that poultry and eggs are cooked properly, the risk of food poisoning is low. Poor food hygiene and inadequate processing, particularly within the home, contribute to causing infectious intestinal disease but cannot be blamed for food poisoning outbreaks associated with shellfish, especially molluscs, which are particularly linked to viral infections.
Hazards from food production
Technological inputs (selective breeding, fertilisers, herbicides, pesticides, fungicides, etc) into farming have increased the efficiency of food production. However, inappropriate animal feeding practices and the use of agrochemicals may pose hazards to human health. Foodborne exposure to agricultural and environmental chemicals results in much public concern in the United Kingdom. Owing to exquisitely sensitive methods of detection, trace amounts of potentially harmful chemicals can be detected in many foods. However, the levels of human exposure to these chemicals are generally well below the tolerable daily intakes in the United Kingdom.14,21,22 In most developed countries the use and application of agrochemicals is carefully regulated, monitored, and reviewed. The appropriate use of agrochemicals in food production is a not a great hazard to human health.
The safety assessment of genetically modified foods poses a new challenge. The classical toxicological approach used for chemicals, which involves feeding animals intakes 100 times the amounts likely to be consumed by humans to demonstrate toxic effects, is not appropriate when applied to foods that may contribute up to 20% of the dietary intake. The UK Advisory Committee on Novel Foods and Processes considers each genetically modified food to ensure that there are no hazards associated with the method used to transfer the gene, that the genetic modification is stable, that the processing of the food denatures the DNA, that there are no new allergens, and that the food is substantially equivalent in terms of chemical composition to the unmodified parent organism. Few genetically modified foods have been approved for food use in the United Kingdom (box), but many more have been approved and been in the food chain for a few years in Canada and United States.
Genetically modified foods approved for use in Britain23
Genetically modified foods:
Improved baker’s yeast (1990)
Improved brewer’s yeast (1991)
Processed products from glyphosate tolerant soybeans (1995)
Oil from glufosinate tolerant rapeseed (1995)
Oil from glyphosate tolerant rapeseed (1996)
Flavr Savr tomato paste (1995) and fresh Flavr Savr tomato (1996)
Processed products from glufosinate tolerant and BT toxin containing maize (1997)
Oil from bromoxynil tolerant cotton seed (1997)
Food ingredients made from genetically modified micro-organisms:
Chymosin (rennet)—currently used to make most cheese in the United Kingdom (1991, 1992)
Amylase—used to clear haze in fruit juice (1994)
Riboflavin (1997)
The potential environmental and health risks from genetically modified foods have been discussed elsewhere.24 No adverse reactions in humans to approved genetically modified foods have yet been reported. The continued use of antibiotics as growth promoters for poultry and pigs is of concern25 because it has resulted in the emergence of multidrug resistant strains of pathogenic bacteria such as quinolone resistant Campylobacter jejuni26 and Salmonella enterica serotype tymphomurium DT104.27 The sewage sludge generated from intensive poultry and pig meat production might be an important origin for the spread of antibiotic resistant genes and pathogenic bacteria into the food chain. The process of feeding infected bovine and ovine offal to cattle was responsible for the epidemic of bovine spongiform encephalopathy in the United Kingdom and is almost certainly responsible for new variant Creutzfeld-Jakob disease, although the exact mode of transmission remains uncertain.28 The S enteritidis and bovine spongiform encephalopathy epidemics underscore the importance of applying the hazard critical control point concept to the production of food animals.
Hazards from the industrial processing of food
The benefits of modern food processing are often taken for granted: increased availability of food, decreased cost, and convenience. Food processing is essential to feed a large urban population: it destroys naturally occurring toxicants and inhibits the growth and spread of pathogenic and spoilage organisms. Raw or unpasteuerised milk and eggs are an important cause of food poisoning in both the United Kingdom and the United States.2,29,30
In processed foods, food additives act as preservatives and processing aids and replace the colour and nutrients lost during processing. The safety and use of food additives is strictly controlled by legislation. Allegations widely reported in the media a decade ago that food additives are a major cause of food allergy have not been substantiated.9 The hazards of allergic reactions to naturally occurring foodstuffs such as nuts, shellfish, and soy are much greater. Peanut allergy may affect 1-2% of the UK population31; it tends to be lifelong and can result in life threatening anaphylaxis.32 In the United Kingdom, products containing even traces of peanuts need to be clearly labelled. It is a paradox that peanut allergy is virtually unknown in tropical countries, where peanuts are eaten almost daily. One explanation for this could be that frequent infections in childhood dampen the response to allergens.
The mass packaging of food is an important barrier against microbiological contamination. However, the hazards resulting from the leaching of potentially accumulatively toxic compounds (such as vinyl chloride, phthalates, dioxins) from packaging material into foods, especially those with a high fat content, are currently being assessed.22
Challenge of the future
Advances in technology have enabled world food supply to keep pace with population growth. However, each technology has its own risks. The world population is forecast to double over the next 50 years, and food production must increase to meet demands. The availability of water is a major constraint on food production in many parts of the world, and efforts will be needed to conserve water for food production. Biotechnology could help achieve the goal of sustainable development, which recognises the need for technology without environmental damage. An efficient food industry and distribution system can also decrease waste.
To achieve a safe food supply it is necessary to apply the hazard critical control point concept and risk analysis to the food chain and to enact legislation, where appropriate, to ensure that training is undertaken and practices are followed and that monitoring and surveillance occur. Education is also needed to alert consumers to risks from food and how to minimise them. Special consideration is needed for fish and shellfish as they are particularly prone to both environmental and microbiological contamination.22,33 Global warming could dramatically change the geographical distribution of algal toxins. Finally, internationally agreed food standards are essential to facilitate trade between countries. All of these challenges require a sophisticated infrastructure, which in some parts of the world, particularly Africa, is being destroyed by war.
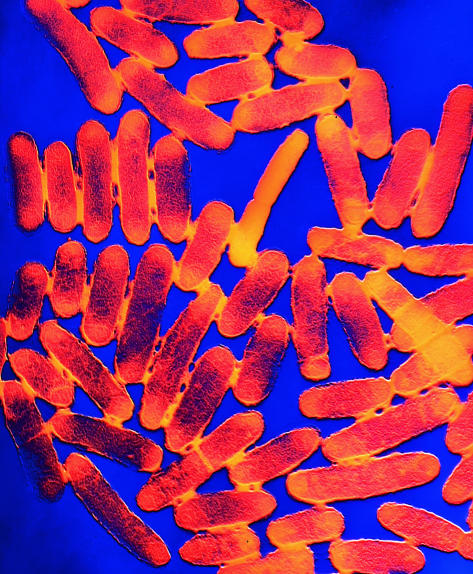
Figure.
LAMR/A B DOWSETT/SPL
E coli O157 has been detected in the faeces of up to 15% of British cattle
Editorials by Brundtland and Pershagen
Footnotes
Competing interests: TABS has been paid for participating in workshops on food safety by ILSI Europe and acts as a consultant to Seven Seas Ltd and the Nutrasweet Information Service.
References
- 1.Hennessy TW, Hedberg CW, Slutsker L, White KE, Besser-Wiek JM, Moen ME, et al. A national outbreak of Salmonella enteritidis infections from ice cream. N Engl J Med. 1996;334:1281–1286. doi: 10.1056/NEJM199605163342001. [DOI] [PubMed] [Google Scholar]
- 2.Kaferstein FK, Motarjemi Y, Bettcher DW. Foodborne disease control: a transnational challenge. Emerg Infect Dis. 1997;3:503–510. doi: 10.3201/eid0304.970414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Herwaldt BL, Ackers ML. An outbreak in 1996 of cyclosporiasis associated with imported raspberries. The Cyclospora Working Group. N Engl J Med. 1997;336:1548–1556. doi: 10.1056/NEJM199705293362202. [DOI] [PubMed] [Google Scholar]
- 4.Hutin YJ, Pool V, Cramer EH, Nainan GV, Weth H, Williams IT, et al. A multistate, foodborne outbreak of hepatitis A. National Hepatitis A Investigation Team. N Engl J Med. 1999;340:595–602. doi: 10.1056/NEJM199902253400802. [DOI] [PubMed] [Google Scholar]
- 5.FAO/WHO (Food and Agriculture Organisation/World Health Organisation) Codex Alimentarius Commission. Risk Assessment. Rome: FAO; 1996. (CL96/21 Gen.) [Google Scholar]
- 6.US National Food Safety Initiative. www.foodsafety.gov/ (accessed 1 June 1999).
- 7.European Commission Scientific Committee for Food. Opinion on principles for the development of risk assessment of microbiological hazards under the hygiene of foodstuffs directive. Brussels: European Commission,1997. (93/43/EEC; expressed on 13 June 1997.)
- 8.Calman KC, Royston G. Risk language and dialects. BMJ. 1997;315:939–942. doi: 10.1136/bmj.315.7113.939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sanders T, Bazalgette P. The food revolution. London: Bantam; 1991. [Google Scholar]
- 10.Sanders TAB. Overview of bioactive compounds in foods. Biochem Soc Trans. 1996;24:771–775. doi: 10.1042/bst0240771. [DOI] [PubMed] [Google Scholar]
- 11.Bhat RV, Shetty PH, Amruth RP, Sudershan RV. A foodborne disease outbreak due to the consumption of moldy sorghum and maize containing fumonisin mycotoxins. J Toxicol Clin Toxicol. 1997;35:249–255. doi: 10.3109/15563659709001208. [DOI] [PubMed] [Google Scholar]
- 12.Haque A, Hossain M, Wouters G, Lambein F. Epidemiological study of lathyrism in northwestern districts of Bangladesh. Neuroepidemiology. 1996;15:83–91. doi: 10.1159/000109893. [DOI] [PubMed] [Google Scholar]
- 13.Motarjemi Y, Kaferstein FK. Global estimation of foodborne diseases. World Health Stat Q. 1997;50:5–11. [PubMed] [Google Scholar]
- 14.Ministry of Agriculture, Fisheries, and Food. Food chemical surveillance. Annual report 1997. London: MAFF; 1998. [Google Scholar]
- 15.Ting JY, Brown AF, Pearn JH. Ciguatera poisoning: an example of a public health challenge. Aust NZ J Public Health. 1998;22:140–142. doi: 10.1111/j.1467-842x.1998.tb01158.x. [DOI] [PubMed] [Google Scholar]
- 16.Scoging A, Bahl M. Diarrhetic shellfish poisoning in the UK. Lancet. 1998;352:117. doi: 10.1016/S0140-6736(98)85023-X. [DOI] [PubMed] [Google Scholar]
- 17.Wheeler JG, Sethi D, Cowden JM, Wall PG, Rodrigues LC, Tompkin DS, et al. Studies of infectious intestinal disease in England: rates in the community, presenting in general practice, and reported to national surveillance. BMJ. 1999;318:1046–1050. doi: 10.1136/bmj.318.7190.1046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Outbreak Reports to CDSC April 20, 1999. www.phls.co.uk/ (accessed 1 June 1999).
- 19.Fisher IST. Salmonella enteritidis in western Europe 1995-98—a surveillance report from Enter-net. Eurosurveillance. 1999;4:56. doi: 10.2807/esm.04.05.00072-en. [DOI] [PubMed] [Google Scholar]
- 20.Hogue A, White P, Guard-Petter J, Schlosser W, Gast R, Ebel E, et al. Epidemiology and control of egg-associated Salmonella enteritidis in the United States of America. Rev Sci Tech. 1997;16:542–553. doi: 10.20506/rst.16.2.1045. [DOI] [PubMed] [Google Scholar]
- 21.Ministry of Agriculture, Fisheries, and Food/Health and Safety Executive. Annual report of the Working Party on Pesticide Residues 1994. London: HMSO; 1995. (Supplement to the Pesticide Register 1995.) [Google Scholar]
- 22.Ministry of Agriculture, Fisheries, and Food. Food chemical surveillance: annual report 1998. London: MAFF Publications; 1999. [Google Scholar]
- 23.Ministry of Agriculture, Fisheries, and Food. Annual report of the Advisory Committee on Novel Foods and Processes, 1997. London: MAFF Publications; 1998. [Google Scholar]
- 24.Jones L. Genetically modified foods. BMJ. 1999;318:581–584. doi: 10.1136/bmj.318.7183.581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ministry of Agriculture, Fisheries, and Food. A review of antimicrobial resistance in the food chain. A technical report for MAFF, July 1998. www.maff.gov.uk/food/resist.pdf (accessed 1 June 1999.) [DOI] [PubMed]
- 26.Smith KE, Besser JM, Hedberg CW, Leano FT, Bender JB, Wickland JH, et al. Quinolone-resistant Campylobacter jejuni infections in Minnesota, 1992-1998. N Engl J Med. 1999;340:1525–1532. doi: 10.1056/NEJM199905203402001. [DOI] [PubMed] [Google Scholar]
- 27.Glynn MK, Bopp C, Dewitt W, Dabney P, Moktar M, Angulo FJ. Emergence of multidrug-resistant Salmonella enterica serotype tymphomurium DT104 infections in the United States. N Engl J Med. 1998;338:1333–1338. doi: 10.1056/NEJM199805073381901. [DOI] [PubMed] [Google Scholar]
- 28.Johnson RT, Gibbs CJ., Jr Creutzfeldt-Jakob disease and related transmissible spongiform encephalopathies. N Engl J Med. 1998;339:1994–2004. doi: 10.1056/NEJM199812313392707. [DOI] [PubMed] [Google Scholar]
- 29.Djuretic T, Wall PG, Nichols G. General outbreaks of infectious intestinal disease associated with milk and dairy products in England and Wales: 1992 to 1996. Commun Dis Rep CDR Rev. 1997;7:R41–R45. [PubMed] [Google Scholar]
- 30.Headrick ML, Korangy S, Bean NH, Angulo SF, Potter ME, Klontz KC. The epidemiology of raw milk-associated foodborne disease outbreaks reported in the United States, 1973 through 1992. Am J Public Health. 1998;88:1219–1221. doi: 10.2105/ajph.88.8.1219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tariq SM, Stevens M, Matthews S, Ridout S, Twiselton R, Hide DW. Cohort study of peanut and tree nut sensitisation by age of 4 years. BMJ. 1996;313:514–517. doi: 10.1136/bmj.313.7056.514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Committee on Toxicity of Chemicals in Food, Consumer Products and the Environment. Peanut allergy. London: Department of Health; 1998. [Google Scholar]
- 33.Ahmed FE, editor. Seafood safety. Washington, DC: National Academy Press; 1991. (Committee on Evaluation of the Safety of Fishery Products.) [PubMed] [Google Scholar]