Abstract
Background:
Coronavirus disease 2019 pandemic was expected to have traumatic effects and increase the anxiety levels of inflammatory bowel disease patients.
Methods:
We aimed to investigate the psychosocial effects of the coronavirus disease 2019 pandemic on patients with inflammatory bowel disease by revealing the risk perception for present disease, coping strategies, follow-up characteristics, and treatment adherence. This is a cross-sectional, web-based survey study including 798 inflammatory bowel disease patients who were followed at our outpatient clinic and 303 volunteer who did not have any known chronic diseases and were not health professionals were included as the control group.
Results:
In this study, 281 of the patients were diagnosed with Crohn’s disease and 215 with ulcerative colitis. The mean age of patients with Crohn’s disease, ulcerative colitis, and the control group were 40.9 ± 13.1, 42.3 ± 12.7, and 39.9 ± 11.6, respectively. Here, 119 (42%) of the Crohn’s disease cases, 116 (54%) of the ulcerative colitis cases, and 170 (56%) of the control group were male. Among the 3 groups, coronavirus disease 2019-related post-traumatic stress disorder rates (Impact of Event Scale-Revised > 33) and State-Trait Anxiety Inventory of current status of anxiety-related anxiety rates were not statistically different while State-Trait Anxiety Inventory of anxiety tendency-related constant anxiety was higher in inflammatory bowel disease patients than the control group (P < .017).
Conclusion:
Inflammatory bowel disease patients with anxiety have a lower quality of life, and this may worsen the clinical course of the disease. Coronavirus disease 2019 is a major source of stress for such a vulnerable population. During the pandemic, psychological support and mental health awareness should be made accessible to all individuals.
Keywords: Anxiety, COVID-19, inflammatory bowel disease, post-traumatic stress disorders, quality of life
Introduction
Coronavirus disease 2019 (COVID-19) is caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), and as of December 14, 2020, more than 70 million people worldwide have been infected with SARS-CoV-2 and 1.7 million people died.1 In Turkey, the first case was reported on March 11, 2020, and until January 5, 2021, 2 270 101 people were diagnosed with COVID-19 and 21 879 people died.2
Coronavirus disease 2019 pandemic forced governments to perform significant changes in the health care delivery systems. As many patients with COVID-19 need to be hospitalized, the hospitals started to intensively reduce routine appointments, elective surgeries, and endoscopic procedures.3 This disturbed machinery may have potential influences on patients with chronic diseases, especially on those who needed follow-up on a regular basis.
Inflammatory bowel disease (IBD) is an umbrella term, which describes disorders that involve different parts and layers of the gastrointestinal tract (GIT). It is known that the prevalence of post-traumatic stress disorders and anxiety levels has increased in IBD patients.4,5 The quality of life (QoL) is affected in IBD patients due to the chronic course of the disease, its relapsing nature, and the necessity of lifelong follow-up, and as a result, mental problems such as anxiety and depression can develop.6
The risk of severe infection and clinical outcomes related to COVID-19 in IBD patients is unclear. Although some studies have shown that the risk of contracting COVID-19 in IBD patients was not different from the general population,7 it can be predicted that the patients are at high mortality risk due to COVID-19 infection related to many factors such as disease activity, malnutrition, and the use of immunosuppressive drugs. Pharmacological agents such as corticosteroids, immunomodulators, and tumor necrosis factor-alpha (TNFα) inhibitors, which are commonly used in the treatment of IBD, may also frequently cause immunosuppression.8 In a study among 525 IBD patients from 33 countries, it has been reported that advanced age and systemic corticosteroid use were positively correlated with COVID-19-related death.9
In addition to these situations, which point to an increased risk of contracting COVID-19 in IBD patients and a worse course if caught, various measures taken including reprogramming of clinical controls, endoscopic procedures, and postponement of infusion appointments may be alarming.
In the present study, we aimed to investigate the psychosocial effects of the COVID-19 pandemic on patients with IBD by revealing the risk perception for present disease, coping strategies, outpatient clinical follow-up characteristics, and problems with treatment adherence. We hypothesize that the COVID-19 pandemic would increase the anxiety levels of IBD patients and would have traumatic effects on these patients.
MATERIALS AND METHODS
Participants and Procedure
This is a cross-sectional, web-based survey study including IBD patients who were followed at the Gastroenterology outpatient clinic of Cerrahpaşa School of Medicine. Healthy volunteers, who did not have any known chronic diseases and were not health professionals, were selected from the researchers’ close circle and social media platforms as the control group.
The study was designed using Google forms by researchers. Google account “https://forms.gle/FxpFQY6hDaUziGdW9” was set up and managed to collect survey responses. The questionnaire contained 3 parts: part I consisted of questions about sociodemographic information, current treatments of the patients, and personal thoughts about the pandemic. Part II and part III contained Impact of Event Scale-Revised (IES-R) and State-Trait Anxiety Inventory (STAI I-II), respectively. The contact information of the patients was accessed from the outpatient files.
An invitation letter explaining the work was sent to the participants by SMS between 1 May 2020 and August 30, 2020, only once for a person. People who wanted to participate in the survey approved by clicking on the study link, which was sent to them. The estimated time to complete the survey was between 15 and 20 mins.
Measures
Sociodemographic Data Form
This data form includes the questions about age, gender, marital status, education period, employment status, the number of household members, comorbidities and history of psychiatric disorders and treatment history, type of IBD, treatments, comorbidities, risk perception for COVID-19 and treatment difficulties experienced in the COVID-19 outbreak, compliance with social isolation, information, and compliance with rules.
Impact of Event Scale-Revised (IES-R)
This scale includes a 22-item self-report questionnaire that is used to assess post-traumatic stress symptoms in relation to any event, with responses rated on a 5-point Likert-type scale (ranging from 0 to 4) developed by Weiss and Marmar.10 The IES-R, which scored the severity of the symptoms in the last 7 days, consists of 3 subscales: intrusion, avoidance, and hyperarousal. An increase in scale scores indicates the presence of higher symptoms of posttraumatic stress. Creamer et al11 defined the IES-R score cut-off value as 33, which indicates the presence of post-traumatic stress disorder (PTSD). In the present study, as in various others, it was used to measure stress after the COVID-19 pandemic.12,13 The validity and reliability of these scales in Turkish were evaluated by Corapcioglu et al.14 Cronbach’s alpha internal consistency reliability coefficients were found as 0.94 for the whole group and between 0.87 and 0.94 for the various study groups. We used the validated Turkish version of the questionnaire with one slight modification (we replaced the word “outbreak” for “event”).
State-Trait Anxiety Inventory (STAI)
STAI consists of a self-completed questionnaire of 40 items, which aims to measure the presence and severity of anxiety symptoms and general anxiety tendencies. STAI-S measures the current state of anxiety (temporary and influenced by the contingent situation), and STAI-T measures the anxiety tendency (how it feels “generally”). Each scale consists of 20 questions. The score for the STAI scales ranges from 20 to 80 points: no anxiety (0-20 points), mild (21-39 points), moderate (40-59 points), and severe anxiety (60-80 points). The validity and reliability of the Turkish version of the STAI was performed by Oner and Le Compte.15
Statistical Analysis
Statistical analyses were performed using the Statistical Package for the Social Sciences (SPSS) software (version 22.0, IBM Corp.; Armonk, NY, USA). Continuous variables are expressed as mean ± standard deviation (SD) and/or medians (interquartile range [IQR]). Student’s t-test or analysis of variance (ANOVA) was used to compare means between groups with normal data distribution. The results were evaluated at a 95% CI, a P-value < .05 was considered statistically significant.
Results
Characteristics of Participants
A total of 1200 IBD patients (600 CD and 600 UC) and 600 healthy controls were invited. Following the invitation, we collected 798 responses from the patients with CD, UC, and controls, 281 (response rate 46.8%), 215 (response rate 35.8%), and 303 (response rate 50.5%), respectively.
Patients with CD, UC, and the control group were comparable regarding mean age (40.9 ± 13.1, 42.3 ± 12.7, and 39.9 ± 11.6, respectively, P = .108) (Table 1). One hundred and nineteen (42%) CD patients, 116 (54%) UC cases, and 170 (56%) controls were male; the rate of female participants was significantly higher both in the UC and control groups compared to the CD group (P = .002).
Table 1.
Sociodemographic Characteristics of Participants
| Characteristics | Groups | P | |||
|---|---|---|---|---|---|
| IBD (n = 496) | CD (n = 281) | UC (n = 215) | Controls (n = 303) | ||
| Mean ± SD or n (%) | |||||
| Age | 41.54 ± 12.90 | 40.94 ± 13.06 | 42.32 ± 12.67 | 39.98 ± 11.62 | .086a* |
| .108a** | |||||
| Sex | |||||
| Female | 235 (47.4) | 119 (42) | 116 (54) | 170 (56) | .0017b* |
| Male | 261 (52.6) | 162 (58) | 99 (46) | 133 (44) | .002b** |
| Years of education | |||||
| <12 years | 322 (64.9) | 186 (66) | 136 (63) | 98 (32) | <.001b* |
| ≥12 years | 174 (35.1) | 95 (34) | 79 (37) | 205 (68) | .002b** |
| Marital status | |||||
| Single | 129 (26) | 79 (28) | 50 (23) | 61 (20) | .121b* |
| Married | 347 (70) | 189 (67) | 158 (74) | 225 (74) | .162c** |
| Divorced | 20 (4) | 13 (5) | 7 (3) | 17 (6) | |
| Employment status | |||||
| Unemployed | 230 (46.4) | 125 (45) | 105 (48.8) | 108 (36) | <.001* |
| Employed | 165 (33.3) | 88 (31) | 77 (35.8) | 177 (58) | <.001** |
| Temporary quit | 101 (20.4) | 68 (24) | 33 (15.3) | 18 (6) | |
| Living alone | |||||
| No | 483 (97.4) | 274 (97.5) | 209 (97) | 287 (95) | .051b* |
| Yes | 13 (2.6) | 7 (2.5) | 6 (3) | 16 (5) | .159b** |
| Smoking habits | |||||
| Currently | 118 (23.8) | 79 (28) | 39 (18) | 110 (36) | <.001b* |
| Never | 186 (37.5) | 87 (31) | 99 (46) | 125 (41) | <.001b** |
| Ex-smoker | 192 (38.7) | 115 (41) | 77 (36) | 68 (23) | |
| Comorbidities | |||||
| No | 255 (51.4) | 140 (50) | 115 (53.5) | 303 (100) | - |
| Yes | 241 (48.6) | 141 (50) | 100 (46.5) | 0 (0) | |
| Psychiatric disorders | |||||
| No | 461 (92.9) | 260 (92.5) | 201 (93.5) | 271 (89) | .083b* |
| Yes | 35 (7.1) | 21 (7.5) | 14 (6.5) | 32 (11) | .207b** |
| Psychiatric drugs using | |||||
| No | 461 (92.9) | 260 (92.5) | 201 (93.5) | 295 (97) | .009 c* |
| Yes | 35 (7.1) | 21 (7.5) | 14 (6.5) | 8 (3) | .018c** |
| Psychiatric treatment history | |||||
| Yes | 74 (14.9) | 47 (17) | 27 (13) | 44 (14.5) | .878b* |
| No | 422 (85.1) | 234 (83) | 188 (87) | 259 (85.5) | .426b** |
*Comparison between IBD and control groups. **Comparison between CD, UC, and control groups.
aOne-way ANOVA analysis; bPearson’s chi-square; cFisher’s exact chi-square analysis.
IBD, inflammatory bowel disease; CD, Crohn’s disease; UC, ulcerative colitis; SD, standard deviation.
Approximately half of the patients in the IBD group had at least 1 comorbidity. The most common comorbidity was rheumatological diseases (rheumatoid arthritis/ankylosing spondylitis; 25.7%), followed by hypertension (13.2%), diabetes mellitus (10.7%), and chronic obstructive pulmonary disease (9.5%), respectively.
COVID-19 Outbreak-Related Characteristics of the Patients and Perceptions of COVID-19 Infection Risk
There was no significant difference between CD, UC, and control groups in terms of frequency of COVID-19 diagnosis and hospitalization rate due to COVID-19 (Table 2). In addition to patients with CD and UC, healthy controls also found COVID-19 very dangerous (P = .748) (data not shown). Therewith, it was observed that almost all participants in the 3 groups paid attention to social isolation rules (CD: 98.9%, UC: 99.5%, and control group: 98.7%) (Table 2).
Table 2.
The Characteristics and Risk Perception of Participants During the COVID-19 Outbreak
| Questions |
CD (n = 281) | UC (n = 215) | Controls (n = 303) | P |
|---|---|---|---|---|
| n (%) or Median | ||||
| Have you been diagnosed with COVID-19? | ||||
| Yes | 6 (2) | 4 (2) | 1 (1) | .135c |
| No | 275 (98) | 211 (98) | 302 (99) | |
| Have you been hospitalized due to COVID-19? | ||||
| Yes | 2 (1) | 1 (0.5) | 1 (1) | .836c |
| No | 279 (99) | 214 (99.5) | 302 (99) | |
| Has anyone in your family been diagnosed with COVID-19? | ||||
| Don’t know | 20 (7) | 25 (12) | 0 (0) | <.001c |
| Yes | 31 (11) | 19 (9) | 41 (13.5) | |
| No | 230 (82) | 171 (79) | 262 (86.5) | |
| Have you lost a family member due to COVID-19? | ||||
| Yes | 1 (1) | 1 (0.5) | 2 (1) | .999c |
| No | 280 (99) | 214 (99.5) | 301 (99) | |
| How serious do you consider the COVID-19 outbreak? | ||||
| Exaggerated | 7 (3) | 5 (2) | 10 (3) | .748b |
| Very dangerous | 203 (72) | 161 (75) | 211 (70) | |
| Partially dangerous | 71 (25) | 49 (23) | 82 (27) | |
| Did you pay attention to the social isolation rules during the COVID-19 outbreak? | ||||
| Yes | 278 (99) | 214 (99.5) | 299 (99) | .682c |
| No | 3 (1) | 1(0.5) | 4 (1) | |
aOne-way ANOVA analysis; bPearson’s chi-square; cFisher’s exact chi-square analysis.
Follow-Up Characteristics of IBD Patients During the Pandemic and Factors That Increase the Risk of Being Affected by COVID-19 at a Traumatic Level
During the study period, 51% of the outpatient clinic appointments were delayed and IBD patients came to their last outpatient clinic visits 5.53 ± 7.78 months ago and 48% of them stated that they considered these situations related to the outbreak as a problem. Only 34% of the patients received information about their treatments with telemedicine. It was observed that 149 patients (30%) had thought of discontinuing their medication, but the rate of adherence to current treatment was still 84.8%. It was found that 75 participants (15%) discontinued one or more of their medications. Rates of discontinuation in patients receiving immunosuppressant drugs and 5-ASA are 12.6% vs 8.9%, respectively. Discontinuation rates according to the routes of administration (per-os vs parenteral) are 10.6% vs 12.6%, respectively. When we divide the patients into 2 groups as those who have to come to the hospital to receive their intravenous treatment (infliximab, vedolizumab) and those who were able to make a visit with telemedicine and administer subcutaneous formulations by themselves at home (adalimumab, ustekinumab, and certolizumab), discontinuation rates are 14.2% vs 9.7%, respectively.
Among the patient group, 77% of the respondents stated that their risk of contracting COVID-19 was higher compared to healthy people, and if they do contract to disease, 83.2% thought the disease would be fatal. COVID-19 infection was “extremely dangerous” according to 73% of the patients. Also, 312 patients (63%) stated that they followed the information about the pandemic on social media and 51% on TV (data not shown).
In both CD and UC groups, the risk of being affected by COVID-19 outbreak at a traumatic level was significantly increased by “having difficulties obtaining drugs from the pharmacy” (OR = 2.04, P = .041; CI: 1.03-4.04, OR = 2.87, P = .005; CI: 1.39-5.96, respectively. Factors associated with treatment variables that increase the risk of being affected by the COVID-19 outbreak at a traumatic level are given in Table 3.
Table 3.
Factors Associated with Treatment Variables That Increase the Risk of Being Affected by COVID-19 Outbreak at a Traumatic Level According to the IES-R Total Score (Above 33 Points)
| Questions | Groups | |||||
|---|---|---|---|---|---|---|
| CD (n = 281) | UC (n = 215) | |||||
| OR | 95% CI (LL-UL) | P | OR | 95% CI (LL-UL) | P | |
| Missing outpatient clinic appointment (yes) | 1.17 | 0.61-0.64 | .64 | 1.23 | 0.59-2.54 | .583 |
| Missing this appointment is a problem (yes) | 3.01 | 1.52-0.002 | .002 | 0.85 | 0.39-1.87 | .692 |
| Have you been able to consult your doctor about how to continue treatment during the COVID-19 outbreak? (yes) | 1.32 | 0.69-0.406 | .406 | 0.72 | 0.31-1.66 | .439 |
| Are medical treatment of IBD a risk for COVID-19? | 0.35 | 0.10-0.099 | .099 | 1.67 | 0.30-9.35 | .560 |
| Did you think about stopping the medications? (yes) | 1.30 | 0.64-0.467 | .467 | 1.09 | 0.50-2.41 | .825 |
| Have IBD medical treatment been discontinued? (no) | 0.81 | 0.32-0.664 | .664 | 0.40 | 0.16-1.03 | .057 |
| Did you have any problems during the procurement of these medicines from the pharmacy? (yes) | 2.04 | 1.03-0.041 | .041 | 2.87 | 1.39-5.96 | .005 |
| Do you think you have a higher risk of getting COVID-19 infection than healthy people? (yes) | 1.23 | 0.45-0.693 | .693 | 3.10 | 0.92-10.51 | .069 |
| If you get COVID-19 infection, do you think this infection will progress worse for you than healthy people? (yes) | 5.19 | 0.99-0.051 | .051 | 2.51 | 0.63-9.99 | .192 |
CD, Crohn’s disease; UC, ulcerative colitis; OR, odds ratio; LL, lower limit; UL, upper limit; CD; X2 (10, N = 281) = 34.53, P < .001, Cox-Snell R2 = 0.12, Nagelkerke R2 = 0.18, overall percentage = 80.1. UC; X2 (10, N = 215) = 30.08, P = .001, Cox-Snell R2 = 0.13, Nagelkerke R2 = 0.20, overall percentage = 77.2.
Comparison of Psychiatric Scale Scores (IES-R and STAI I-II) Between Groups
For all 3 groups, COVID-19-related PTSD rates (IES-R > 33) and STAI-S-related anxiety rates were not different, while STAI-T-related constant anxiety was significantly different (P < .017) (Figure 1). STAI-T scores were higher in both CD and UC groups than in the control group.
Figure 1.
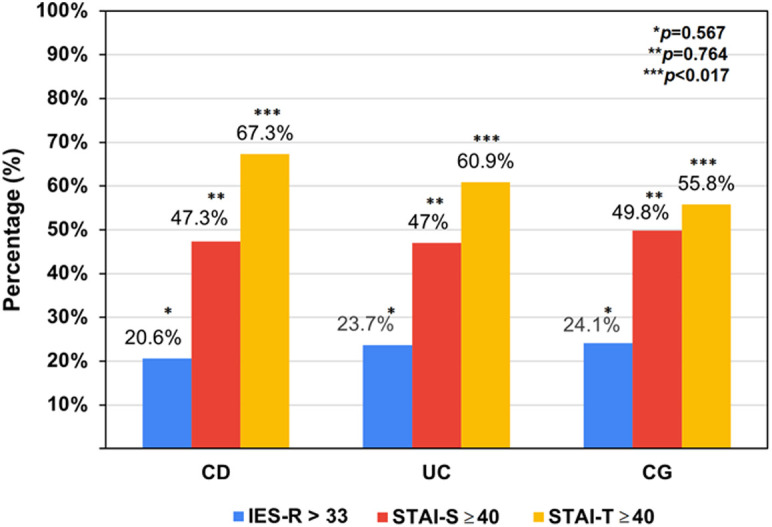
Trauma and anxiety rates according to IES-R and STAI scales among the groups evaluated in the study. IES-R, Impact of Event Scale-Revised; STAI, State-Trait Anxiety Inventory.
In the UC group, perception of COVID-19 as a dangerous disease (OR: 3.06, P = .047; CI: 1.01-9.26) was found to increase the risk of being affected by COVID-19 at a traumatic level. Age, level of education, marital status, and psychiatric disorders history were not associated with PTSD (Table 4).
Table 4.
Multiple Logistic Regression Analysis Results Associated with Increasing the Risk of Being Affected by COVID-19 at a Traumatic Level According to IES-R Total Score (>33 Points)
| Characteristics | CD (n = 281) | UC (n = 215) | Controls (n = 303) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| P | OR | 95% CI (LL-UL) | P | OR | 95% CI (LL-UL) | P | OR | 95% CI (LL-UL) | |
| Age | 0.95 | 1.00 | 0.97-1.03 | .298 | 0.98 | 0.94-1.02 | .827 | 1.00 | 0.97-1.03 |
| Gender (Female) | 0.41 | 1.36 | 0.66-2.83 | .166 | 1.85 | 0.77-4.44 | .025 | 2.19 | 1.11-4.34 |
| Level of education (<12 years) | 0.23 | 1.71 | 0.71-4.08 | .149 | 2.11 | 0.77-5.83 | .779 | 0.90 | 0.45-1.83 |
| Marital status (Single) | 0.66 | 1.22 | 0.51-2.97 | .133 | 0,45 | 0.16-1.28 | .314 | 0.65 | 0.29-1.49 |
| Psychiatric disorders (No) | 0.46 | 2.36 | 0.25-22.59 | .468 | 2.78 | 0.18-43.77 | .785 | 1.16 | 0.41-3.27 |
| Psychiatric drugs using (No) | 0.99 | 1.01 | 0.11-9.39 | .257 | 0.20 | 0.01-3.24 | .116 | 7.02 | 0.62-79.98 |
| COVID-19 perception (Dangerous) | 0.42 | 1.44 | 0.60-3.45 | .047 | 3.06 | 1.01-9.26 | .027 | 2.41 | 1.11-5.27 |
CD, Crohn’s disease; UC, ulcerative colitis; OR, odds ratio; LL, lower limit; UL, upper limit. CH; X2 (13, N = 281) = 89.19, P < .001, Cox-Snell R2 = 0.27, Nagelkerke R2 = 0.43, overall percentage = 82.9. ÜKH; X2 (13, N = 215) = 73.67, P < .001, Cox-Snell R2 = 0.29, Nagelkerke R2 = 0.44, overall percentage = 85.1. KG; X2 (10, N = 303) = 92.14, P < .001, Cox-Snell R2 = 0.6, Nagelkerke R2 = 0.39, overall percentage = 84.2.
When we divide the patients into 2 groups according to the routes of drug administration (i.v. vs s.c.), no significant differences were observed in psychiatric scale scores (Table 5).
Table 5.
Comparison of IES-R, STAI-S and STAI-T Scores Between IBD Patients According to Treatment Characteristics
|
|
Treatment Modality I | Treatment Modality II | ||||||
|---|---|---|---|---|---|---|---|---|
| Intravenous (n = 127) | Subcutaneous (n = 72) | t | P | Oral (n = 295) | Intravenous + Subcutaneous (n = 199) | t | P | |
| IES-R total (mean ± SD) | 22.90 ± 12.67 | 24.51 ± 12.69 | −0.86 | .389 | 24.18 ± 15.88 | 23.48 ± 12.67 | 0.52 | .603 |
| Intrusion (mean ± SD) | 6.76 ± 5.07 | 7.28 ± 5.74 | −0.67 | .507 | 7.56 ± 6.52 | 6.94 ± 5.31 | 1.10 | .272 |
| Avoidance (mean ± SD) | 11.12 ± 5.58 | 11.76 ± 4.24 | −0.85 | .35 | 10.81 ± 5.54 | 11.35 ± 5.13 | −1.10 | .273 |
| Hyperarousal (mean ± SD) | 5.02 ± 4.38 | 5.47 ± 4.68 | −0.68 | .499 | 5.82 ± 5.66 | 5.19 ± 4.49 | 1.32 | .188 |
| STAI-S | 40.02 ± 11.31 | 38.68 ± 11.55 | 0.79 | .428 | 39.41 ± 12.27 | 39.53 ± 11.38 | −0.12 | .908 |
| STAI-T | 44.50 ± 10.37 | 45.63 ± 9.96 | −0.74 | .458 | 44.25 ± 11.58 | 44.91 ± 10.21 | −0.65 | .518 |
The mean IES-R, STAI-S, and STAI-T scores were comparable among men and women diagnosed with CD. Comparison of the mean scores of IES-R, STAI-S, and STAI-T among the participants by gender was shown in Table 6.
Table 6.
Comparison of the Mean Scores of IES-R, STAI-S, and STAI-T Among the Participants by Gender
| IES-R total | Intrusion | Avoidance | Hyperarousal | STAI-S | STAI-T | |
|---|---|---|---|---|---|---|
| I-CD (mean ± SD) | ||||||
| Male | 22.8 ± 13.2 | 6.9 ± 5.7 | 11.1 ± 5 | 4.9 ± 4.6 | 38.2 ± 11.4 | 43.4 ± 10.6 |
| Female | 24 ± 14.7 | 7.3 ± 6 | 11 ± 5.7 | 5.8 ± 5.2 | 40.9 ± 11.8 | 45.8 ± 10.5 |
| Total | 23.4 ± 13.9 | 7 ± 5.8 | 11 ± 5.3 | 5.3 ± 4.9 | 39.4 ± 11.6 | 44.4 ± 10.6 |
| t | 0.71 | 0.59 | −0.21 | 1.55 | 1.93 | 1.90 |
| II-UC (mean ± SD) | ||||||
| Male | 21.8 ± 15.9 | 6.7 ± 6.2 | 9.9 ± 6 | 5.1 ± 5.4 | 38.9 ± 13.3 | 43.1 ± 12.1 |
| Female | 26.9 ± 14.9 | 8.5 ± 6.4 | 11.8 ± 4.8 | 6.6 ± 5.7 | 39.9 ± 11.4 | 45.9 ± 11.1 |
| Total | 24.6 ± 15.6 | 7.66 ± 6.3 | 10.97 ± 5.4 | 5.9 ± 5.6 | 39.5 ± 12.3 | 44.6 ± 11.6 |
| t | 2.44* | 2.10* | 2.52* | 1.96 | 0.60 | 1.80 |
| III-controls (mean ± SD) | ||||||
| Male | 22.5 ± 13.1 | 7.2 ± 5.3 | 11.5 ± 5.6 | 3.8 ± 4.3 | 37.4 ± 10.2 | 38.9 ± 8.8 |
| Female | 27.5 ± 14.4 | 9.4 ± 6.1 | 12.3 ± 5.5 | 5.8 ± 5.1 | 41.4 ± 11.6 | 43.9 ± 10.2 |
| Total | 25.3 ± 14.0 | 8.4 ± 5.8 | 11.9 ± 5.5 | 4.9 ± 4.8 | 39.7 ± 11.2 | 41.7 ± 9.9 |
| t | 3.10** | 3.34** | 1.15 | 3.67** | 3.14** | 4.51** |
CD, Crohn’s disease; UC, ulcerative colitis; SD, standard deviation.
* P < .05; ** P < .01.
Post hoc analysis results (adjusted P value in Turkey correction).
Intrusion scores
Group I versus Group III, P < .05; Group I females versus Group III females, P < .05.
STAI-T scores
Group I versus Group III, P < .01; Group II versus Group III, P < .01; Group I males versus Group III males, P < .01; Group II males versus Group III males, P < .01.
The remaining P values did not show statistical significance.
Discussion
The COVID-19 pandemic has the potential to cause negative emotional, cognitive, and behavioral reactions in individuals due to its uncertain nature, rapid spread and life-threatening, lack of specific treatment, and also requiring restrictions and isolation measures in daily and social life activities. In the present study, we investigated the psychological effects of the COVID-19 outbreak on IBD patients. We found that almost a quarter of the patients with IBD were affected by COVID-19 at a traumatic level, half of these patients had instant anxiety and about 60% of the patients had a level of anxiety that requires clinical support.
Patients with chronic diseases and the elderly have a higher risk of being infected with SARS-CoV-2 and the higher mortality rates.16 This is not only the concern of medical professionals but also the people with chronic disease partly because of very close follow-up of any medical consequences of COVID-19 by written and social media. Therefore, these patients are expected to have more concerns about the pandemic. Supporting this, recent studies have shown that individuals with chronic diseases develop more psychiatric symptoms during the COVID-19 pandemic.17
We have shown that patients with CD and UC seem to be reacting the same way to the pandemic, revealing similar levels of anxiety, fear of contracting COVID-19, and adherence to medications. This finding is not surprising because CD and UC patients tend to react similarly to difficult situations and have similar mental health profiles prior to the COVID-19 pandemic era.18
In our study, both patients with CD and UC have significantly higher trait anxiety levels (64.5%) higher than the control group. Similar results have been observed in previous studies evaluating anxiety levels in IBD patients. In a study with 1156 IBD patients, a significant proportion of the participants (48.4%) experienced anxiety during the pandemic.19 Similarly, half of the IBD patients presented moderate (37%) to severe (14.5%) anxiety in another study.20 Among 200 IBD patients, 62% of the cases showed moderate to high level of anxiety in the pandemic.21 This may be related to the increasing concerns of IBD patients about disease control during the pandemic process due to disruptions in health care, such as the difficulty in applying to the outpatient clinic and inpatient admissions and the lack of access to pharmacies.
We did not find a significant difference in “state” anxiety levels between IBD and controls. Our findings suggest that patients with IBD may be more resilient than we expected towards unexpected stressful events such as the ongoing COVID-19 pandemic. This could be related to “a positive adaptive behavior.” The fact that IBD patients are often receiving immunosuppressants, such as azathioprine and TNF-α inhibitors, which are associated with an increased risk of infection, may partially explain their perceptions of personal danger. Maybe IBD patients, because of the immunosuppression treatments, were already paying more attention to social isolation rules and hygiene rules before the pandemic.
The prevalence of PTSD in IBD patients has increased because they have been trying to deal with similar traumatic events for years. Having an incurable disease, lifelong follow-up requirement, potential side effects of treatment, recurrent surgeries, and remittent diarrhea episodes may have negative effects on mental health in IBD patients.22 There are only a few studies in the literature on this subject. In a study from Switzerland consisting of 468 CD patients, 19% scored above the diagnostic cut-off for PTSD.23
There were no significant differences between patients with CD and UC and the controls in terms of PTSD rates. Similarly, Poyraz et al24 showed that the severity of PTSD symptoms did not change depending on the presence of chronic disease in the COVID-19 pandemic era. Due to the chronic relapsing/remitting nature of IBD, most probably our patient group was partially prepared for the things that might go wrong and in addition, they do not react differently to the pandemic conditions than the normal population.
Among our IBD patients, the rate of medication adherence was 84%. Similarly, it was reported that 30.7% of IBD patients discontinue or delay their medications during the pandemic.25 In another study, most patients had a fear of contracting COVID-19, but in 3815 IBD patients, 96% continued their treatments.26 Putting all these together, most probably IBD patients are more afraid of relapse of their diseases that might occur when they stop taking their medications than they fear of COVID-19.
It was shown that anxiety disorders are more frequent in women in general27 and also in the pandemic era.28 In our study, while female controls had a significantly increased risk of being affected by COVID-19 at a traumatic level, there was no difference regarding PTSD rates between men and women in UC and CD groups. In addition, the elderly (especially >65 years) have an increased risk of disease contact.28 Parallel to all these findings, we expected to find that levels of anxiety would increase by age. However, we found no statistically significant difference in terms of PTSD and anxiety scores by age. It shows that the effect of gender and age on anxiety may disappear when there are concerns about chronic illness.
It was previously shown that social media platforms were the main source for gathering information about the pandemic.29 Similarly, in our patient group, most of the patients followed the news regarding the pandemic on social media and TV.
British Society of Gastroenterology COVID-19 IBD Working Group divided patients into risk groups for COVID-19-related poor outcome. Risk groups were determined according to age, comorbid diseases, and the type of immunosuppressant agent used.29 Anxiety scores can be expected to be higher in the patient group receiving intravenous treatment because they had to come to the hospital for infusion. Interestingly, there was no significant difference in PTSD and anxiety scales according to treatment modality. In a study, similar to our work, no significant difference was found in anxiety scales between patients who received azathioprine, anti-TNF, and corticosteroid treatment.20 This shows that the patient group using drugs that are categorized as low risk for COVID-19 by the published guidelines (5-ASA and budesonide) may also be psychosocially affected by the pandemic at least as badly as patients receiving immunosuppressive therapy.
Our study has several limitations. All participants were asked questions that measure their current situation in a cross-sectional manner. It is not possible to effectively say whether this is due to the pandemic or the cross-sectional nature of the study due to the lack of data on the levels of the variables before the pandemic began. Despite the studies showing that anxiety level increases in patients with active disease,30 we did not evaluate the activity of the disease in our patients.
COVID-19 is a major source of stress for such a vulnerable population. Studies evaluating the effects of psychological stress on emotional states in patients with IBD are lacking. This study enabled us to evaluate how IBD patients in Turkey respond collectively to a major stressful event. Follow-up studies are also needed to understand the long-term psychological effects of the pandemic in patients with IBD.
Conclusion
Although no differently perceived from the healthy population, as one of the major sources of current global stress, COVID-19’s negative impact on IBD patients via anxiety may lower the QoL and worsen the clinical course of the disease.
During the pandemic, psychological support and mental health awareness should be made accessible to all individuals.
Footnotes
Ethics Committee Approval: The study was approved by the local ethics committee of İstanbul University-Cerrahpaşa, Cerrahpaşa School of Medicine (Decision No: 72185 dated June 15, 2020). All procedures were in accordance with ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent: All subjects have given their written informed consent.
Peer-review: Externally peer-reviewed.
Author Contributions: Consept – T.E., E.D., Ş.T.; Design – T.E., E.D., Ş.T.; Supervision – A.İ.H., A.F.Ç., Y.E., Ş.T.; Resources – T.E., E.D.; Materials – T.E., E.D.; Data Collection and/or Processing – O.K.B., E.A.K., U.Ö., S.C., Ö.D.; Analysis and/or Interpretation – T.E., E.D., A.İ.H.; Literature Search – T.E., E.D., Ö.D.; Writing Manuscript – T.E., E.D., A.İ.H., Ş.T.; Critical Review – M.T., Y.E., A.F.Ç., A.İ.H., Ş.T.
Declaration of Interest: The authors have no conflict of interest to declare.
Funding: The authors declared that this study has received no financial support.
References
- 1. . Park SE. Epidemiology, virology, and clinical features of severe acute respiratory syndrome -coronavirus-2 (SARS-CoV-2; coronavirus disease-19). Clin Exp Pediatr. 2020;63(4):119 124. 10.3345/cep.2020.00493) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. . Republic of Turkey Ministry of Health. Republic of Turkey Ministry of Health Corona Table. 2020. Available at: https://covid19.saglik.gov.tr/, Accessed December 9, 2020. [Google Scholar]
- 3. . Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497 506. 10.1016/S0140-6736(20)30183-5) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. . Stapersma L, van den Brink G, Szigethy EM, Escher JC, Utens EMWJ. Systematic review with meta-analysis: anxiety and depression in children and adolescents with inflammatory bowel disease. Aliment Pharmacol Ther. 2018;48(5):496 506. 10.1111/apt.14865) [DOI] [PubMed] [Google Scholar]
- 5. . Graff LA, Walker JR, Bernstein CN. Depression and anxiety in inflammatory bowel disease: a review of comorbidity and management. Inflamm Bowel Dis. 2009;15(7):1105 1118. 10.1002/ibd.20873) [DOI] [PubMed] [Google Scholar]
- 6. . Kubesch A, Boulahrout P, Filmann N, Blumenstein I, Hausmann J. Real-world data about emotional stress, disability and need for social care in a German IBD patient cohort. PLoS One. 2020;15(1):e0227309. 10.1371/journal.pone.0227309) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. . Singh AK, Jena A, Kumar MP, Sharma V, Sebastian S. Risk and outcomes of coronavirus disease (COVID-19) in patients with inflammatory bowel disease: a systematic review and meta-analysis. U Eur Gastroenterol J. 2021;9(2):159 176. 10.1177/2050640620972602) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. . Toruner M, Loftus EV, Harmsen WS, et al. Risk factors for opportunistic infections in patients with inflammatory bowel disease. Gastroenterology. 2008;134(4):929 936. 10.1053/j.gastro.2008.01.012) [DOI] [PubMed] [Google Scholar]
- 9. . Brenner EJ, Ungaro RC, Gearry RB, et al. Corticosteroids, but not TNF antagonists, are associated with adverse COVID-19 outcomes in patients with inflammatory bowel diseases: results from an international registry. Gastroenterology. 2020;159(2):481 491.e3. 10.1053/j.gastro.2020.05.032) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. . Weiss DS. The impact of event scale-revised. In: Wilson JP, Keane TM.eds. Assessing Psychological Trauma and PTSD. New York: Guilford Press; 1997:399 411. [Google Scholar]
- 11. . Creamer M, Bell R, Failla S. Psychometric properties of the impact of event scale - revised. Behav Res Ther. 2003;41(12):1489 1496. 10.1016/j.brat.2003.07.010) [DOI] [PubMed] [Google Scholar]
- 12. . Wang C, Pan R, Wan X, et al. A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain Behav Immun. 2020;87:40 48. 10.1016/j.bbi.2020.04.028) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. . Alkhamees AA, Alrashed SA, Alzunaydi AA, Almohimeed AS, Aljohani MS. The psychological impact of COVID-19 pandemic on the general population of Saudi Arabia. Compr Psychiatry. 2020;102:152192. 10.1016/j.comppsych.2020.152192) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. . Çorapçioğlu A, Yargiç İ, Geyran P, Kocabaşoğlu N. Olaylarin etkisi ölçeği (IES-R) Türkçe versiyonunun geçerlilik ve güvenilirliği = Validity and reliability of Turkish Version of “Impact of Event Scale-Revised” (IES-R). Yeni Symp Psikiyatr Nöroloji ve Davraniş Bilim. Derg. 2006;44(1):14 22. [Google Scholar]
- 15. . Oner N, LeCompte A. Durumluk-Sürekli Kaygı El Kitabı (State-Trait Anxiety Inventory Handbook). Baski . 2. Istanbul: Boğaziçi Üniversitesi Yayınları; 1985. [Google Scholar]
- 16. . Pan L, Mu M, Yang P, et al. Clinical characteristics of COVID-19 patients with digestive symptoms in Hubei, China: a descriptive, cross-sectional, multicenter study. Am J Gastroenterol. 2020;115(5):766 773. 10.14309/ajg.0000000000000620) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. . Ozamiz-Etxebarria N, Dosil-Santamaria M, Picaza-Gorrochategui M, Idoiaga-Mondragon N. Stress, anxiety, and depression levels in the initial stage of the COVID-19 outbreak in a population sample in the northern Spain. Cad Saude Publica. 2020;36(4):e00054020. 10.1590/0102-311X00054020) [DOI] [PubMed] [Google Scholar]
- 18. . Choi K, Chun J, Han K, et al. Risk of anxiety and depression in patients with inflammatory bowel disease: a nationwide, population-based study. J Clin Med. 2019;8(5):654. 10.3390/jcm8050654) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. . Mosli M, Alourfi M, Alamoudi A, et al. A cross-sectional survey on the psychological impact of the COVID-19 pandemic on inflammatory bowel disease patients in Saudi Arabia. Saudi J Gastroenterol. 2020;26(5):263 271. 10.4103/sjg.SJG_220_20) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. . Trindade IA, Ferreira NB. COVID-19 pandemic’s effects on disease and psychological outcomes of people with inflammatory bowel disease in Portugal: a preliminary research. Inflamm Bowel Dis. 2021;27(8):1224 1229. 10.1093/ibd/izaa261) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. . Spagnuolo R, Larussa T, Iannelli C, et al. COVID-19 and inflammatory bowel disease: patient knowledge and perceptions in a single center survey. Medicina. 2020;56(8):407. 10.3390/medicina56080407) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. . Baumgart DC, Sandborn WJ. Inflammatory bowel disease: clinical aspects and established and evolving therapies. Lancet. 2007;369(9573):1641 1657. 10.1016/S0140-6736(07)60751-X) [DOI] [PubMed] [Google Scholar]
- 23. . Cámara RJ, Gander ML, Begré S, von Känel R. Swiss Inflammatory Bowel Disease Cohort Study Group. Post-traumatic stress in Crohn’s disease and its association with disease activity. Frontline Gastroenterol. 2011;2(1):2 9. 10.1136/fg.2010.002733) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. . Poyraz BÇ, Poyraz CA, Olgun Y, et al. Psychiatric morbidity and protracted symptoms after COVID-19. Psychiatry Res. 2021;295:113604. 10.1016/j.psychres.2020.113604) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. . Mir N, Cheesbrough J, Troth T, et al. COVID-19-related health anxieties and impact of specific interventions in patients with inflammatory bowel disease in the UK. Frontline Gastroenterol. 2021;12(3):200 206. 10.1136/flgastro-2020-101633) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. . D’Amico F, Rahier JF, Leone S, Peyrin-Biroulet L, Danese S. Views of patients with inflammatory bowel disease on the COVID-19 pandemic: a global survey. Lancet Gastroenterol Hepatol. 2020;5(7):631 632. 10.1016/S2468-1253(20)30151-5) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. . Sareen J, Erickson J, Medved MI, et al. Risk factors for post-injury mental health problems. Depress Anxiety. 2013;30(4):321 327. 10.1002/da.22077) [DOI] [PubMed] [Google Scholar]
- 28. . Wang Y, Di Y, Ye J, Wei W. Study on the public psychological states and its related factors during the outbreak of coronavirus disease 2019 (COVID-19) in some regions of China. Psychol Health Med. 2021;26(1):13 22. 10.1080/13548506.2020.1746817) [DOI] [PubMed] [Google Scholar]
- 29. . Grunert PC, Reuken PA, Stallhofer J, Teich N, Stallmach A. Inflammatory Bowel Disease in the COVID-19 Pandemic: the Patients’ Perspective. J Crohns Colitis. 2020;14(12):1702 1708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. . Tribbick D, Salzberg M, Ftanou M, et al. Prevalence of mental health disorders in inflammatory bowel disease: an Australian outpatient cohort. Clin Exp Gastroenterol. 2015;8:197 204. 10.2147/CEG.S77567) [DOI] [PMC free article] [PubMed] [Google Scholar]


