We report and review how physician leaders in the state of Indiana created new state-funded residency programs to help address their growing shortage of physicians and to expand access to healthcare in rural Indiana.
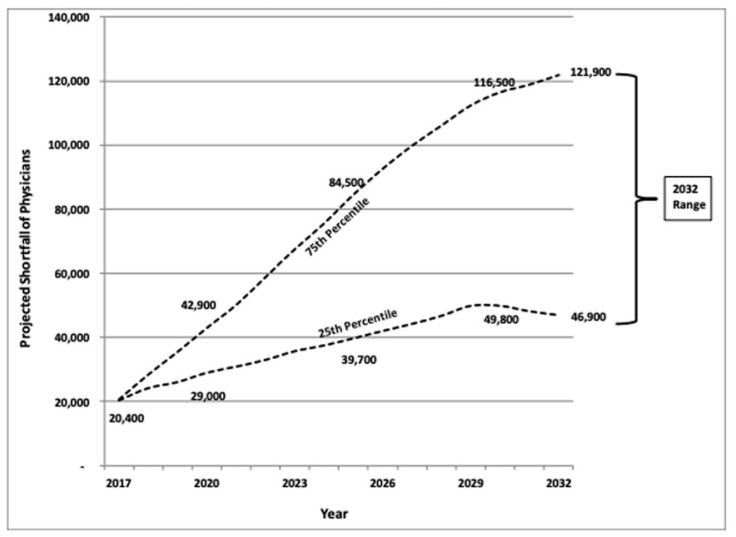
Here in the United States, we have a large and growing shortage of physicians. Importantly, a significant number of physicians are planning to retire early,1 with 21.8% of respondents in one survey reportedly considering early retirement.2 One reports suggests: “The U.S. is facing a shortage of up to 124,000 physicians by 2034, including as many as 48,000 primary care doctors.”3 Post-pandemic burnout, liability concerns, private equity and “productivity” pressures, onerous bureaucratic regulations, and governmental interference in the practice of medicine are some commonly cited reasons for physicians leaving their practices. Two major avenues to address the pipeline for our physician workforce include: expanding our workforce with foreign graduates and international medical graduates,4,5 and increasing federal funding of graduate medical education (GME) for residency and fellowship training.6,7
Our federal government is the primary funder of GME, including Medicare, Medicaid, the Health Resources Services Administration (HRSA), and the Veterans Administration (VA) funds;8 since 1997, the number of Medicare-funded GME positions had been capped at 1996 levels.6 In 2021, the US Congress finally passed a bill to add 1000 new residency slots starting in fiscal year 2023, with no more than 250 slots per year.9 This was the first increase to GME slots since 1997, and while a step in the right direction, this will not be nearly enough to address current and anticipated physician workforce shortages. The first round of awards for new residency slots were released in February 2023, with 200 new slots added, only two of which were in Missouri.8
In the meantime, new medical schools continue to be built while medical school class sizes continue to expand. This imbalance between the number of available residency positions and the number of graduating medical students each year, results in some medical students who are “unmatched” and need to find other solutions. According to the AMA, “nearly 8,500 medical school graduates did not initially match into a residency slot last year” and “just over 5,000 of these unmatched students were able to scramble” into a program they did not initially apply for; however, “more than 3,000 students failed to locate an available position and, as a result, were unable to begin training and provide physician care to their communities.” 10 Many who do not match plan to apply again in the next year, while spending some time in either research or other avenues for professional development (and also addressing their educational debt burdens).
Exhibit ES-1.
Total Projected Physician Shortfall Range, 2017–2032
Source: The Complexities of Physician Supply and Demand
Meanwhile, our physician workforce is lacking adequate primary care physicians, with a need for 44,000 additional primary care physicians in the US by 2035.11 In a 2016 report, the Health Resources Services Administration projected that Missouri would need 5,150 primary care physicians but only have 3,930 available, for a 23.7% deficit.12 According to AAMC, only 24.1% of active physicians who graduated from an MD- or DO-granting school in Missouri were in practice in Missouri in 2020 (7,360 out of 30,530 total medical school graduates).13 This number rises to 55.7% of active physicians who graduated from an MD- or DO-granting school in Missouri and completed GME in Missouri, who were also in practice in Missouri in 2020 (3,415 out of 6,130 total medical school and residency graduates).13
With six medical schools (A.T. Still University – Kirksville College of Osteopathic Medicine in Kirksville [ATSU COM]; Kansas City University College of Osteopathic Medicine [KCU COM]; Saint Louis University School of Medicine [SLU SOM]; University of Missouri – Columbia [MU]; University of Missouri – Kansas City [UMKC]; and Washington University [WUSTL SOM] in St. Louis), Missouri is clearly a net exporter of medical education, with more graduating medical students than in-state residency positions available. According to the Association of American Medical Colleges (AAMC), more than half (54–55%) of individuals who were in residency training from 2012 through 2021 have been practicing in the state where they completed their residency training.14–15
As many have said before, local and state governments are indeed the “incubators of democracy.” Indeed, several states (including Utah,16,17 Virginia,18,19 and Indiana20) have successfully secured funding from their state legislatures for new residency positions in their state. In 2023, the Missouri State Legislature similarly passed House Bill 1162 to establish a graduate medical education grant program,21 which is now being implemented by our Missouri Department of Health and Senior Services. For those states who have not yet established state funding of GME positions, Indiana and other states are demonstrating how to think outside of the box and implement state funding of GME positions to address our growing access-to-care issues nationwide. Below is a summary of our interview of one physician leader in Indiana.
Indiana’s Story
In the early 2010s, Indiana hospitals and medical schools were facing a problem: they were graduating more medical students per year than the number of residency spots they had available. In addition, most residency positions were located centrally, around the Indianapolis area. Hospitals in other areas of the state had few residency slots or were resident-naïve. As the majority of physicians tend to practice in the location of their residency training,14–15 Indiana’s physician leaders were looking for a solution that could not only improve care in the state, but also retain the students they had worked so hard to train.
Luckily, Indiana was in a positive financial position: through good fiscal discipline and management, the state government had a revenue surplus. Physician leaders introduced and lobbied for legislation to create state-funded residency positions in Indiana. “The goal was to provide some state grants as seed money and partial funding for new residency positions, particularly in primary care, which was listed to include family medicine, internal medicine, psychiatry, ob/gyn, and emergency medicine,” according to Heidi Dunniway, MD, Regional Chief Medical Officer of Ascension St. Vincent.
In 2015, this legislation was successfully passed, creating the Indiana Graduate Medical Education (GME) Board12 to oversee this program. The aim of the board was to fund new primary care residency program positions at licensed hospitals and qualifying non-profit organizations. This board, comprised of a broad representation of physicians and business/community leaders from around the state who were appointed by the governor, worked to implement residency positions that were not federally funded, provide startup funding for new residency programs, and develop the infrastructure for expansion of existing residency programs and establishment of new ones. The GME board comprised five different consortiums by location: Indianapolis, Lafayette, Muncie, Northwest Indiana, and Southwest Indiana.
The Southwest Indiana GME Consortium (SIGMEC) showed how successful such a program can be, and may be a role model for other states and regions who wish to implement state-funded residency program expansion. SIGMEC includes Good Samaritan Hospital (Vincennes, Indiana), Ascension St. Vincent Hospital (Evansville, Indiana), Deaconess Hospital (Evansville, Indiana), and Memorial Hospital and Health Care Center (Jasper, Indiana). Two of their four hospitals were residency-naïve and thus had no caps to the number of Medicare-funded GME spots that they could apply for. In Evansville, they have two level 2 trauma centers with a population of 800,000 in their catchment area serving a 200-mile radius. At three hours from Indianapolis, two hours from Louisville (KY), two hours from Nashville (TN), and three and a half hours away from St. Louis (MO), many of their residents don’t want to travel for medical care but it can be tough to get physicians.
Upon its creation, SIGMEC’s first step was to hire an independent consultant to do a needs-assessment of regional hospitals, to see what could be supported clinically and financially. Dr. Dunniway stressed the critical importance of this vital step, to determine the rural locations that had the greatest disparities in access to care, and to identify resident-naïve hospitals that may benefit from new residency programs. The needs assessment also included an analysis of which parts of the state were failing to recruit and retain physicians, and gaps were noted in the rural areas outside of Indianapolis. After the needs-assessment, development of individual residency programs began. In the initial stages, each hospital participating in SIGMEC contributed $1 million, and another $250,000 was allocated from the state GME Board. This initial investment helped fund the search for new program directors and residency coordinators, as well as enable the necessary infrastructure to establish new residency programs. Some hospitals were found to be unable to support particular residency programs on their own, and would also need specialty rotations in other hospitals. Establishing some of these residency programs also required a culture change, getting nursing and ancillary services on-board with the educational mission of these programs.
As each resident began their training, the programs also received approximately $45,000 annually per resident from SIGMEC and/or state funding. While the initial cost to join this program may appear steep, this should be viewed as an investment in the community. After initial investment from the hospital and SIGMEC, these resident-naïve programs can become sustainable long-term through securing new federal GME funding. Dr. Dunniway also explained that by introducing resident physicians to these underserved local rural areas, those areas were empowered to recruit and retain those physicians and provide more and better care to those communities.
Indiana’s early numbers are promising. SIGMEC (comprising Good Samaritan, Jasper Memorial, Ascension, and Deaconess) now has 56 new internal medicine residents (Ascension and Good Samaritan), 20 psychiatry residents at Good Samaritan (also doing rotations at Ascension and Deaconness), and 15 family medicine residents at Jasper (also doing rotations at Ascension and Deaconness). The psychiatry residency has graduated their second class (five psychiatry residents) this year, and the family medicine residency in Jasper graduated their second class (five family medical residents) also this year. In Evansville Indiana, six out of their 16 graduating internal medical residents will be staying on as faculty in their region of rural Central and Southwestern Indiana (while four others have matched into fellowship). If one considers the costs associated with recruiting six new internists to rural Indiana, this program is already seeing a significant return on investment, and increasing access to medical care in their local communities. As their current physician workforce is undergoing attrition (due to burnout, relocations, changes in life circumstances), they are looking to continue to bring in new physicians—and they have already cut their locums costs by over $1 million per year at Ascension alone.
The benefits to the consortium’s hospitals stretch beyond the raw numbers of increasing residency positions, as well as increasing physician recruitment and retention. Programs are now seeing an increase in award-winning research, bringing academic recognition to the hospitals. “We’ve got a ton of research going on —clinical, case presentations, etc.” said Dr. Dunniway. “Our residents have been phenomenal in terms of the meetings they have presented at. The cases they’ve been written up have been published multiple times, and their posters have won top poster presentation awards at national meetings like the American College of Physicians (ACP).”
Lessons
Dr. Dunniway has several points of advice for states wishing to create similar programs. First, she recommends having strong physician leadership in the state legislature: “Physicians in our legislature were key to gaining support with our legislature and governor, planting seeds for the legislation that made this possible.” In addition to physician leadership in the Indiana state legislature, US Representative Larry Bucshon is a cardiothoracic surgeon from southwest Indiana who also played a key role in advocating for their state’s commitment to GME.
Once funding was secured, a needs-assessment was crucial to identifying the locations that were most likely to support new residency programs, especially resident-naïve hospitals that could build new programs and secure federal GME funding. While creating new GME programs is not an easy, “it’s just amazing what a start-up program can do with the right energy behind it. It’s not without its challenges, but it’s been a fantastic process.”
While Indiana and Missouri are two distinct states, they share several similarities that suggest that Indiana’s success may be a model for Missouri. Indiana’s population of 6.8 million (#17 in the US) is very similar to Missouri’s population of 6.2 million (#19 in the US), but with a higher population density of 189 (#16 in the US) vs 88.2 (#30 in the US) people per square mile. Many parallels can be seen between the demographics, major industries, politics, geography, and challenges of both states. Like Missouri, Indiana is comprised of a few cities scattered like islands amid large rural agricultural areas. As with much of the Midwest, agriculture, energy, manufacturing, and pharmaceuticals are the other pillars of Indiana’s economy. Racial diversity is mostly confined to urban areas, while most of the rural population is white. Indiana University is also home to the largest medical school in the country (with 338 graduating medical students22 in 2022).
Similar to Indiana, Missouri is a rural agricultural state in the Midwest which serves as a net exporter of medical education. With passage of House Bill 1162 in 2023 (and increased funding for this program in 2024), Missouri is now in an excellent position to follow in Indiana’s footsteps, by expanding existing residency programs with state funding. In the coming years, there may be also be an interest in enabling creation of new GME programs to residency-naïve hospitals. Through these initiatives, our state of Missouri will hopefully recruit and retain more physicians who will put down roots and remain in the area, generate new research and innovation, and increase access to medical care for underserved rural and urban populations.
Footnotes
Albert L. Hsu, MD, (pictured), is at the Reproductive Medicine and Fertility Center, Department of Obstetrics, Gynecology and Women’s Health, University of Missouri - Columbia, School of Medicine, Columbia, Missouri (MU SOM COMO). Amanda E. Hull, MD, is an Ob/Gyn resident and Lacey E. Raper, MA, is a medical student at MU SOM COMO. Eric A. Millican, MD, is at the Department of Dermatology, University of Utah, Salt Lake City, Utah.
References
- 1.The Complexities of Physician Supply and Demand: Projections from 2019 to 2034. Association of American Medical Colleges (AAMC); [accessed 07/04/23]. at https://www.aamc.org/media/54681/download?attachment. see 9-10. [Google Scholar]
- 2.Doximity 2021 Physician Compensation Report. Dec, 2021. [accessed 07/04/23]. at https://c8y.doxcdn.com/image/upload/v1/Press%20Blog/Research%20Reports/Doximity-Compensation-Report-2021.pdf. see page 15 for early retirement citation.
- 3.1,000 new GME slots are coming CMS must not hamper their use. the American Medical Association; [accessed 07/04/23]. at https://www.ama-assn.org/education/gme-funding/1000-new-gme-slots-are-coming-cms-must-not-hamper-their-use,3/16/22. [Google Scholar]
- 4.AMA Council on Medical Education Report 4 (A-21) on “Expediting Entry of Qualified International Medical Graduate (IMG) Physicians to US Medical Practice,”. [accessed 07/04/23]. at https://www.ama-assn.org/system/files/a21-cme-04.pdf.
- 5.IMG toolkit: Types of visas & FAQs. [accessed 07/04/23.]. at https://www.ama-assn.org/education/international-medical-education/international-medical-graduates-img-toolkit-types-visas.
- 6.AMA Council on Medical Education Report 1 (I-15) on “Sources of Funding for Graduate Medical Education,”. [accessed 07/04/23.]. at https://www.ama-assn.org/system/files/2021-06/i15-cme-01.pdf.
- 7.AMA Council on Medical Education Report 6 (I-19) on “Veterans Health Administration Funding of Graduate Medical Education,”. [accessed 07/04/23.]. at https://www.ama-assn.org/system/files/2020-04/cme-report-6-i19-annotated.pdf.
- 8.Congressional Research Service. Federal Support for Graduate Medical Education: An Overview. Dec 27, 2018. at https://crsreports.congress.gov/product/pdf/R/R44376.
- 9.S.186 – 117th Congress 2021–2022 Consolidated Appropriations Act (CAA), 2021 S. 186. at < https://www.cms.gov/medicare/medicare-fee-for-service-payment/acuteinpatientpps/dgme>.
- 10.Medical students show leadership in call for more GME slots. the American Medical Association; [accessed 07/04/23.]. at https://www.ama-assn.org/education/gme-funding/medical-students-show-leadership-call-more-gme-slots,4/17/23. [Google Scholar]
- 11.Shaffer T. Primary Care Physician Supply for Missouri. Mo Med. 2016 Jul–Aug;113(4):293–300. [PMC free article] [PubMed] [Google Scholar]
- 12.State-level projections of Supply and Demand for Primary Care Practitioners, 2013–2025. Nov, 2016. at https://bhw.hrsa.gov/sites/default/files/bureau-health-workforce/data-research/primary-care-state-projections2013-2025.pdf.
- 13.Association of American Medical Colleges. State Physician Workforce Data Report. Jan, 2022. https://store.aamc.org/downloadable/download/sample/sample_id/506/- Table 4.1 for “Physicians Retained from Undergraduate Medical Education (UME), 2020” - Table 4.4 for “Physicians Retained from Undergraduate Medical Education (UME) and Graduate Medical Education (GME) Combined, 2020 - Table 4 2 for “Physicians Retained from Public Undergraduate Medical Education (UME), 2020”.
- 14.AAMC 2022 Report on Residents Executive Summary. Association of American Medical Colleges (AAMC); [accessed 07/04/23]. at https://www.aamc.org/data-reports/students-residents/data/report-residents/2022/executive-summary, in Am Fam Physician 2013; 88(10):704 AAMC. [Google Scholar]
- 15.Association of American Medical Colleges. Physician Retention in State of Residency Training, by State. https://www.aamc.org/data-reports/students-residents/data/table-c6-physician-retention-state-residency-training-state .
- 16. [accessed 2/1/23];Utah passes legislation to provide additional state funding for GME programs. 22 Apr 5; < Utah passes legislation to provide additional funding for GME programs ( osteopathic.org)>. [Google Scholar]
- 17.Utah state legislature bill, HB 0295“Physician Workforce Amendments,”. at https://le.utah.gov/~2022/bills/static/HB0295.html.
- 18.Virginia med students, residents help open 25 more GME spots. May 24, 17. at https://www.ama-assn.org/education/gme-funding/virginia-med-students-residents-help-open-25-more-gme-spots.
- 19.Graduate Medical Education. Virginia Medicaid Dept of Medical Assistance Services (DMAS); at https://www.dmas.virginia.gov/forproviders/rates-and-rate-setting/graduate-medical-education/ [Google Scholar]
- 20.Graduate Medical Education Board. the Indiana Commission for Higher Education; [accessed 07/04/23.]. at https://www.in.gov/che/boards-and-committees/graduate-medical-education-board/ [Google Scholar]
- 21.Missouri House Bill no 1162 (102nd General Assembly) [accessed 07/04/23.]. at https://house.mo.gov/billtracking/bills231/hlrbillspdf/2386H.03P.pdf.
- 22.2022 FACTS: Enrollment, Graduates, and MD-PhD Data. AAMC; [accessed 07/04/23.]. at https://www.aamc.org/data-reports/students-residents/data/2022-facts-enrollment-graduates-and-md-phd-data. [Google Scholar]
- 23.Blake Fagan E, MD, Finnegan Sean C, MS, Bazemore Andrew W, MD, MPH, Gibbons Claire B, PhD MPH, Petterson Stephen M., PhD Migration After Family Medicine Residency: 56% of Graduates Practice Within 100. Miles of Training Am Fam Physician. 2013;88(10):704. [PubMed] [Google Scholar]
- 24.Seifer SD, Vranizan K, Grumbach K. Graduate Medical Education and Physician Practice Location: Implications for Physician Workforce Policy. JAMA. 1995;274(9) [PubMed] [Google Scholar]
- 25.Quinn KJ, et al. Influencing Residency Choice and Practice Location through a Longitudinal Rural Pipeline Program. Academic Medicine. 2011 November;86(11):1397–1406. doi: 10.1097/ACM.0b013e318230653f. [DOI] [PubMed] [Google Scholar]
- 26.Figure from “A Growing Crisis: Physician Shortage,”. the Focus for Health Foundation; [accessed 5/20/24]. at https://www.focusforhealth.org/a-growing-crisis-physician-shortage/ [Google Scholar]