Abstract
Background:
Use of postoperative radiographs after surgical management of supracondylar humerus (SCH) fractures is often based on rote practice rather than evidence. The purpose of this study was to determine the frequency with which 3-week postoperative radiographs at the time of pin removal altered management plans in pediatric SCH fractures that were intraoperatively stable after closed reduction and percutaneous pinning (CRPP).
Methods:
We prospectively recruited pediatric patients with SCH fractures managed by CRPP at our institution from June 2020 until June 2022, and reviewed retrospective data on pediatric SCH fractures managed surgically at our institution between April 2008 and March 2015. Patients were assessed for post-CRPP fracture alignment and stability. For prospective patients, we asked clinicians to document their management decision at the 3-week follow-up visit before evaluating the postoperative radiographs. Our primary outcome was change in management because of radiographic findings.
Results:
Overall, 1066 patients in the retrospective data and 446 prospectively recruited patients met the inclusion criteria. In the prospective group, radiographic findings altered management for 2 patients (0.4%). One patient had slow callus formation and 1 patient was identified as having cubitus varus. Altered management included prolonged immobilization or additional radiographic follow-up. Radiographic findings altered management in 0 (0%) of 175 type II fractures, in 2 (0.9%) of 221 type III fractures, and in 0 (0%) of 44 type IV fractures. We obtained similar findings from retrospective data.
Conclusion:
Rote use of 3-week postoperative radiographs after surgical management of SCH fractures that are intraoperatively stable has minimal utility. Eliminating rote postoperative radiographs for SCH fractures can decrease the time and financial burdens on families and health care systems without affecting patient outcomes.
Abstract
Contexte:
L’utilisation des radiographies postopératoires après la réduction chirurgicale des fractures supracondyliennes de l’humérus (SCH) se fonde souvent sur l’habitude plutôt que sur des données probantes. Cette étude avait pour but de déterminer la fréquence à laquelle les radiographies postopératoires après 3 semaines, au moment du retrait de l’embrochage, modifiaient la prise en charge des fractures SCH pédiatriques qui étaient stables à l’étape peropératoire, après réduction fermée et embrochage percutané (RFEP).
Méthodes:
Nous avons recruté de manière prospective des enfants ayant subi une fracture SCH traitée par RFEP dans notre établissement de juin 2020 à juin 2022, et passé en revue les données rétrospectives sur les fractures SCH pédiatriques traitées chirurgicalement dans notre établissement entre avril 2008 et mars 2015. Les jeunes ont été évalués en post-RFEP aux plans de l’alignement et de la stabilité des fractures. Pour le groupe prospectif, nous avons demandé aux médecins de documenter leurs décisions thérapeutiques à la visite de suivi après 3 semaines avant d’évaluer les radiographies postopératoires. Notre paramètre principal était tout changement de la prise en charge motivé par les résultats radiographiques.
Résultats;
En tout, 1066 jeunes de la cohorte rétrospective et 446 de la cohorte prospective répondaient aux critères d’inclusion. Dans le groupe prospectif, les résultats des radiographies ont modifié la prise en charge chez 2 enfants (0,4 %). L’un présentait une lente formation de callosité et l’autre, un cubitus varus. Les modifications de la prise en charge ont inclus la prolongation de l’immobilisation ou l’ajout d’examens radiographiques. Les résultats radiographiques ont modifié la prise en charge de 0 (0 %) fracture de type II sur 175, de 2 (0,9 %) fractures de type III sur 221, et de 0 (0 %) fracture de type IV sur 44. Nous avons fait des observations similaires pour la cohorte rétrospective.
Conclusion:
Les radiographies postopératoires de routine 3 semaines après une réduction chirurgicale des fractures SCH qui étaient stables à l’étape peropératoire sont peu utiles. Les éliminer ferait gagner du temps aux parents et aux systèmes de santé et tout en réduisant leurs dépenses, sans affecter les résultats de l’intervention.
The American Academy of Orthopaedic Surgeons’ 2012 clinical practice guideline for the treatment of pediatric supracondylar humerus (SCH) fractures recommended surgical reduction with wire fixation for displaced fractures (moderate-strength recommendation). 1 However, the guideline did not provide recommendations for optimal postoperative management.1 Given that SCH fractures are the most common surgically managed pediatric fracture and require resource-intensive procedures that need expertise from multiple disciplines, postoperative management should be scrutinized to optimize resource utilization without affecting patient outcomes. Recent literature has questioned the utility of postoperative radiographs in surgically managed SCH fractures.2–6 However, these were retrospective studies. The purpose of this study was to determine the frequency with which 3-week postoperative radiographs at time of pin removal altered management plans in surgically managed pediatric SCH fractures that were intraoperatively stable after closed reduction and percutaneous pinning (CRPP) using retrospective and prospective data.
Methods
Retrospective review
We retrospectively reviewed all pediatric SCH fractures managed surgically at our pediatric academic tertiary care hospital between April 1, 2008, and March 31, 2015. We excluded fractures associated with bone cysts, abnormal lesions, or nonaccidental injury, as well as referrals for revision surgery or treatment failures after initial non-operative management. We also excluded fractures with postoperative follow-up and wire removal outside our institution.
We reviewed medical and radiologic records for demographics (e.g., age, sex), fracture characteristics (e.g., extension v. flexion, severity of displacement, intra-articular extension, open fracture), and reduction and fixation characteristics (e.g., closed v. open reduction, number of wires, presence of medial wire). We determined time from the surgery to wire and immobilization removal. Additional intervention after pin removal because of radiographic findings was the primary outcome variable of interest.
Prospective review
We prospectively recruited all patients with SCH fractures treated with CRPP at our institution between June 15, 2020, and June 26, 2022. Patients were treated according to our institution’s standard operative and postoperative protocols. The surgeon assessed patients for inclusion into the standard postoperative pathway based on post-CRPP fracture alignment and stability. After fixation, fracture stability was assessed using dynamic fluoroscopic examination; the sagittal plane was assessed while flexing and extending the elbow, and the coronal plane was assessed while applying varus and valgus forces across the elbow. At our institution, open reduction for malalignment is only considered if a closed reduction fails to achieve 1 of the following 4 parameters: less than or equal to 30% translation in the coronal plane, less than or equal to 30% in the sagittal plane, anterior humeral line intersecting the capitellum, or carrying angle in normal range and similar to the uninjured side. Open fractures, fractures treated with open reduction, and fractures that have questionable intraoperative stability are excluded from the standard postoperative pathway and managed with an individualized management plan, which could include an early follow-up visit with radiographs at postoperative day 7–10.
Fractures that qualify for the standard postoperative pathway are followed up in a fracture clinic at our institution around 3 weeks after surgery. At the 3-week follow-up visit, patients have their splint and pins removed and then undergo elbow radiographs. The clinician present at the fracture clinic (i.e., nurse practitioner, resident, fellow, or orthopedic surgeon) evaluates patients clinically before viewing the postoperative follow-up radiograph.
For this study, the clinician documented their plan after seeing each patient (immobilization, range of motion exercises, activity limitation, follow-up, consultations). After documenting their plan, the clinician evaluated the radiographs and documented if their plan changed because of radiographic findings. All patients were seen for a 12-week follow-up visit in the fracture clinic for a clinical assessment without routine radiographs.
Data analysis
We reviewed medical records for patient demographics, fracture characteristics, and reduction and fixation characteristics. We identified complications, including nerve palsies, vascular injuries, compartment syndrome, infections, and revision surgeries. We reviewed 3-week postoperative radiographs to evaluate bridging callus formation. Intervention after pin removal because of radiographic findings was the primary outcome variable of interest (e.g., additional immobilization, radiographs ordered at 12-wk visit). We used descriptive statistics to describe the demographic characteristics and the proportion of patients who had a change to their management plan because of postoperative radiographs.
Ethics approval
We obtained approval from the Hospital for Sick Children Research Ethics Board (no. 1000064579) for the retrospective phase of the study and Quality Improvement Project Approval from the Hospital for Sick Children for the prospective phase.
Results
Retrospective review
We retrospectively identified 1066 patients with supracondylar humerus fractures, of whom 1017 met the inclusion criteria. Patient demographics can be found in Table 1. On average, wires were removed 23.02 (standard deviation [SD] 3.29) days after surgery. Only 2 (0.2%) patients had prolonged elbow immobilization because of inadequate callus formation, identified on radiographic assessment after wire removal. The first patient was a 2-year-old female with a Gartland type III fracture managed with closed reduction. The second patient was a 11-year-old female with a Gartland type IV fracture managed with open reduction. Both patients had closed fractures and no other notable demographic, fracture, or management characteristics that may have affected healing.
Table 1.
Characteristics of patients and fractures from retrospective review
| Characteristic | No. (%) of patients* n = 1017 |
|---|---|
| Age, yr | |
| Mean ± SD | 5.4 ± 2.6 |
| Median (range) | 5 (0–15) |
| Sex | |
| Female | 488 (48.0) |
| Male | 529 (52.0) |
| Fracture type | |
| Gartland II | 364 (35.8) |
| Gartland III | 592 (58.2) |
| Gartland IV | 55 (5.4) |
| Flexion type | 1 (0.1) |
| Unspecified | 5 (0.5) |
| Associated injuries | |
| Ipsilateral forearm fracture | 34 (3.3) |
| Open fracture | 12 (1.2) |
| Nerve palsy identified preoperatively | 164 (16.1) |
| Vascular injury requiring vascular surgery intervention | 2 (0.2) |
| Compartment syndrome | 3 (0.3) |
| Open reduction | 30 (2.9) |
SD = standard deviation.
Unless indicated otherwise.
Prospective study
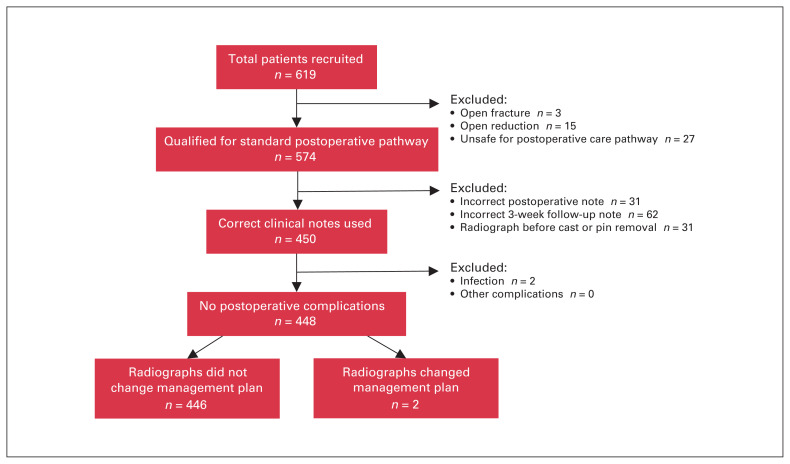
We prospectively recruited 619 patients with SCH fracture who underwent CRPP between June 15, 2020, and June 26, 2022 (Figure 1). Patients who did not meet the inclusion criteria were 3 with an open fracture, 15 treated with open reduction, and 27 who did not qualify for the standard postoperative care pathway after CRPP, leaving 574 patients who qualified for the standard postoperative pathway. Of these, we excluded 31 patients for missing or incorrect postoperative study documentation, 62 patients for a missing or incorrect study documentation from the 3-week postoperative visit, and 31 patients for whom radiographs were taken before cast or pin removal. The appropriate study documentation was used for the remaining 450 patients. We excluded 2 patients identified to have developed an infection on clinical examination. Overall, 448 patients met the inclusion criteria and were included in the analysis (Figure 1).
Fig. 1.
Description of prospective study cohort.
Patient demographics can be found in Table 2. The mean age was 6.3 years. There were 197 females (44.0%) and 251 males (56.0%). Of the 448 patients, 125 (27.9%) had a Gartland type IIa fracture, 50 (11.2%) patients had a type IIb fracture, 221 (49.3%) had a Gartland type III fracture, 44 (9.8%) had a Gartland type IV fracture, and 8 (1.8%) had a flexion-type fracture. Thirty-nine patients had nerve palsies identified preoperatively, an additional 4 patients had nerve palsies identified after surgery but before discharge, and 9 patients had nerve palsies identified at the 3-week postoperative visit. Twenty-seven patients had a perfused but pulseless hand identified during preoperative examination, with an additional 20 instances identified immediately after surgery; all resolved without requiring direct intervention. There were no instances of compartment syndrome.
Table 2.
Characteristics of patients and fractures from prospective review
| Characteristic | No. (%) of patients* n = 448 |
|---|---|
| Age, yr | |
| Mean ± SD | 6.3 ± 2.4 |
| Median (range) | 6 (0.9–15.8) |
| Sex | |
| Female | 197 (44.0) |
| Male | 251 (56.0) |
| Fracture type | |
| Gartland IIa | 125 (27.9) |
| Gartland IIb | 50 (11.2) |
| Gartland III | 221 (49.3) |
| Gartland IV | 44 (9.8) |
| Flexion type | 8 (1.8) |
| Associated injuries and complications† | |
| Ipsilateral forearm fracture | 8 (1.8) |
| Perfused, pulseless hand identified preoperatively | 27 (6.0) |
| Perfused, pulseless hand identified immediately postoperatively | 20 (4.5) |
| Nerve palsy identified preoperatively | 39 (8.7) |
| Nerve palsy identified after surgery, before discharge | 4 (0.9) |
| Nerve palsy identified at 3-wk visit | 9 (2.0) |
SD = standard deviation.
Unless indicated otherwise.
Open fractures and fractures that required open reduction were excluded from prospective analysis.
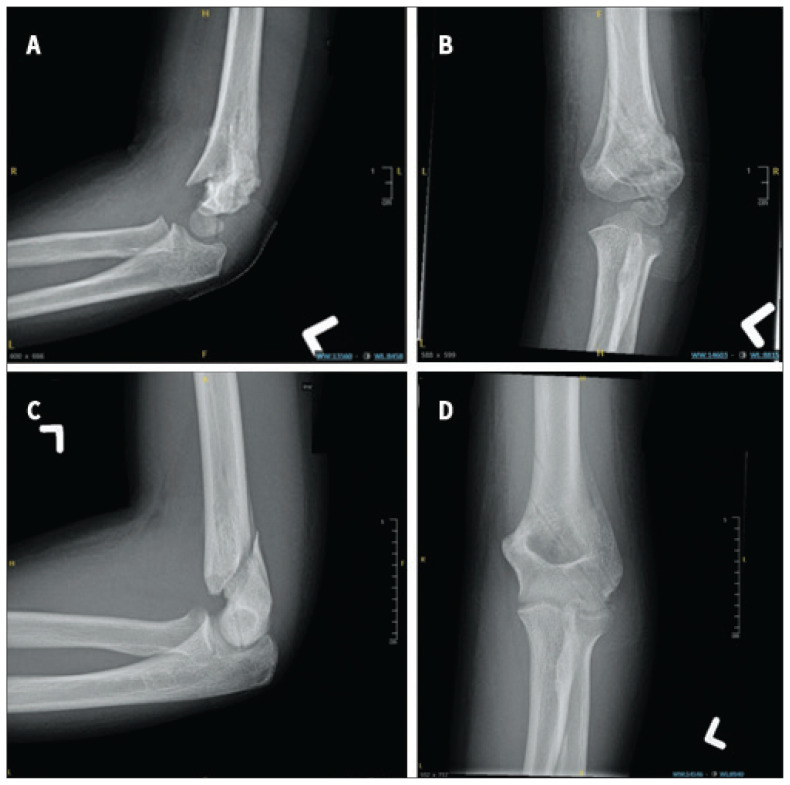
On average, wires were removed 22.98 (SD 2.90) days after surgery. Two patients (0.4%) had their management plans altered because of 3-week postoperative radiographs (Table 3). Both patients had a Gartland type III fracture. Patient 1 was found to have cubitus varus on radiographic assessment, and their management plan was changed by adding radiographs at their 12-week postoperative visit to assess for improvement in angulation and healing. Patient 2 had delayed callus formation on radiographic assessment, and the standard management plan was altered by adding a radiographic assessment at a 6-week postoperative visit to assess for fracture healing. Radiographs of both patients can be found in Figure 2. Radiographs altered management in 0 (0%) of 175 type II fractures, in 2 (0.9%) of 221 type III fractures, and in 0 (0%) of 44 type IV fractures. Of note, no 3-week postoperative radiographs showed unacceptable healing among the 31 patients excluded because of missing or incorrect postoperative study documentation and the 62 patients excluded because of missing or incorrect 3-week postoperative visit study documentation.
Table 3.
Characteristics of patients with management plan alterations because of radiographic findings
| Patient | Age, yr | Sex | Supracondylar humerus fracture type | Radiographic finding that prompted change in management | Change in management plan |
|---|---|---|---|---|---|
| 1 | 3.08 | Female | III | Varus angulation with anterior spike because of rotation | Repeat radiograph at 12-week follow-up |
| 22 | 13.67 | Female | III | Slow callus formation | Repeat radiograph after 3 weeks |
Fig. 2.
Radiographs of prospectively recruited patients who had management plan alterations because of postoperative radiographic assessment. Radiographs from patient 1 showed (A) malrotation at the fracture site and (B) varus alignment in the coronal plane at time of wire and immobilization removal. Radiographs from patient 2 showed (C) questionable bridging callus in the sagittal plane in a near skeletally mature patient with (D) an unstable fracture pattern.
On examination of 3-week postoperative radiographs after pin and cast removal, 126 (100%) type IIa fractures, 49 (98%) type IIb fractures, 213 (97%) type III fractures, and 43 (98%) type IV fractures had bridging callus formation on at least 3 cortices (Table 4). One (2%) type IIb fracture, 6 (3%) type III fractures, and 1 (2%) type IV fracture had visible bridging calluses on 2 cortices. Only 1 type III fracture (patient 2) had bridging callus formation on fewer than 2 cortices.
Table 4.
Number of cortices with bridging callus formation identified on 3-week postoperative radiographs
| Fracture type | No. (%) of patients | ||||
|---|---|---|---|---|---|
| 4 cortices n = 408 |
3 cortices n = 31 |
2 cortices n = 8 |
1 cortex n = 1 |
0 cortices n = 0 |
|
| IIa | 122 (96.8) | 4 (3.2) | 0 | 0 | 0 |
| IIb | 47 (94.0) | 2 (4.0) | 1 (2.0) | 0 | 0 |
| III | 191 (86.8) | 22 (10.0) | 6 (2.7) | 0 | 1 (0.4) |
| IV | 41 (93.2) | 2 (4.5) | 1 (2.3) | 0 | 0 |
| Flexion | 7 (87.5) | 1 (12.5) | 0 | 0 | 0 |
Discussion
Supracondylar humerus fractures are exceedingly common pediatric injuries, with an estimated incidence of 308 per 100 000 people per year.7 These fractures need resource-intensive procedures with expertise from many disciplines, including emergency department physicians, orthopedic surgeons, orthopedic nurse practitioners, orthopedic technologists, anesthesiologists, radiographers, and radiologists. The primary objective of this study was to determine the frequency with which postoperative radiographs at time of pin removal altered management plans for pediatric SCH fractures managed by CRPP.
From our initial retrospective review of 1017 patients, we identified only 2 patients (0.2%) who required additional elbow immobilization after pin removal based on radiologic findings of inadequate healing. Of note, review of these radiographs by the senior author could not identify signs of delayed or nonunion.
Given the limitations of retrospective studies, we further prospectively evaluated 448 patients with SCH fractures managed with CRPP. Only 2 patients (0.4%) had alterations to their management plans based on radiographic findings, a frequency lower than that reported by Garg and colleagues (1%),3 Karalius and colleagues (3.5%),4 and Acosta and colleagues (3.3%–5%).2 Both patients had type III fractures and the only management alteration was an additional radiograph at a future date. No patients required additional immobilization or interventions. Furthermore, radiographs after pin and cast removal consistently showed robust bridging callus formation; more than 97% of all type IIa, IIb, III, and IV fractures had bridging callus formation on at least 3 cortices, and only 1 patient had callus formation on fewer than 2 cortices. Although 40 patients were identified to have a nerve palsy at time of pin removal, none required alterations to management based on radiographic findings. A subset of patients was referred to physiotherapy, occupational therapy, or plastic surgery for follow-up based on clinical assessment alone.
Our findings are in keeping with many recently published studies that question the need for postoperative radiographic follow-up. Garg and colleagues3 did not suggest definitive elimination of radiograph assessment at the time of wire removal, but identified that radiographs at pin removal did not alter management and showed stable fracture reduction with good signs of healing for type II fractures. Karalius and colleagues4 suggested that Gartland type II fractures may not need any follow-up radiographs. Tuomilehto and colleagues6 found that postoperative radiography did not alter management or outcomes and supported clinical evaluation instead.
Our data suggest the minimal utility of 3-week postoperative radiographs at time of pin removal after surgical management of pediatric SCH fractures. Based on our data and the available literature, postoperative radiographs of closed pediatric type II and III SCH fractures that are intraoperatively stable after CRPP may be eliminated without risk of patient harm. We found that, when intraoperative radiographs were used to confirm fracture stability with operatively managed SCH fractures, the 3-week postoperative radiographs failed to alter management in 99.6% of cases. Rote ordering of radiographs at the time of wire removal or beyond for intraoperatively stable SCH fractures to determine further immobilization, nonunion, or malunion should be discouraged. Given the amount of periosteal disruption in type IV fractures, radiographs at time of pin removal may be useful to assess adequate callus formation and determine if additional immobilization is required. As such, we continue to obtain radiographs at the 3-week follow-up for type IV fractures at our institution. However, we concede that this practice is not based in evidence. By eliminating unnecessary postoperative radiographs for most SCH fractures, we can substantially reduce the time and financial burdens on families and the health care system without affecting patient outcomes.
Limitations
Clinicians viewing radiographs after already making a management decision may lead to confirmation bias and deter from changing management. However, this was not evident based on patient outcomes. Review of 3-week postoperative radiographs demonstrated substantial callus formation for nearly all patients. Patients were also followed clinically at a 12-week postoperative visit, with no patients requiring additional surgical management and only 1 patient with a varus or valgus carrying angle greater than 10 degrees. Our results may be limited by their generalizability to other hospitals. Our institution is a specialized pediatric academic tertiary care hospital with a team of experienced surgeons who manage several hundred SCH fractures annually. Surgical outcomes at our institution may not be representative of all patients with type II or III SCH fractures treated with CRPP. However, the directives that our institution previously set for acceptable reduction after CRPP may standardize patients who are eligible for elimination of postoperative radiographs.8 In addition, intraoperatively stable SCH fractures managed at our institution were not routinely followed up at 1 week after surgery. Although forgoing a postoperative radiograph at this time point may miss scenarios where earlier alterations to management are needed, studies have shown that early postoperative radiographic follow-up does not alter management or patient outcomes and may be eliminated in pediatric SCH fractures managed with CRPP.2,5,9
We did not calculate a comprehensive savings analysis, including health care resource savings from radiograph expenses, clinician time, and facility fees; savings from lost productivity resulting from parents missing work and patients missing school because of radiograph wait times; and reduced radiation exposure. Further investigation may be warranted.
Conclusion
When intraoperative radiographs were used to confirm fracture stability with operatively managed SCH fractures, 3-week postoperative radiographs failed to alter management in nearly all cases. Our results suggest that rote 3-week postoperative radiographs of closed pediatric SCH fractures that are intraoperatively stable after CRPP can be eliminated without affecting patient outcomes.
Footnotes
Presented at the 2023 annual meetings of the Pediatric Orthopaedic Society of North America and the Canadian Orthopaedic Society.
Competing interests: None declared.
Contributors: Eliane Rioux Trottier, Stanley Moll, Unni Narayanan, and Mark Camp contributed to the conception and design of the work. George Zhao, Kelvin Ng, Anne Murphy, Stanley Moll, Steven Morrison, and Daniel Pincus contributed to data acquisition, analysis, and interpretation. George Zhao drafted the manuscript. All of the authors revised it critically for important intellectual content, gave final approval of the version to be published, and agreed to be accountable for all aspects of the work.
Funding: This study was supported by grants from the Canadian Orthopaedic Foundation and the SickKids Perioperative Services Summer Studentship. Mark Camp is supported by OrthoPediatrics and SeaSpine.
References
- 1.Howard A, Mulpuri K, Abel MF, et al. The treatment of pediatric supracondylar humerus fractures. J Am Acad Orthop Surg 2012;20:320–7. [DOI] [PubMed] [Google Scholar]
- 2.Acosta AM, Li YJ, Bompadre V, et al. The utility of the early postoperative follow-up and radiographs after operative treatment of supracondylar humerus fractures in children. J Pediatr Orthop 2020;40:218–22. [DOI] [PubMed] [Google Scholar]
- 3.Garg S, Bloch N, Cyr M, et al. Routine radiographs at time of pin removal after closed reduction and percutaneous pinning for type 2 supracondylar humerus fractures do not change management: a retrospective cohort study. J Child Orthop 2016;10:329–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Karalius VP, Stanfield J, Ashley P, et al. The utility of routine postoperative radiographs after pinning of pediatric supracondylar humerus fractures. J Pediatr Orthop 2017;37:e309–12. [DOI] [PubMed] [Google Scholar]
- 5.Thompson RM, Hubbard EW, Elliott M, et al. Is less more? Assessing the utility of early clinical and radiographic follow-up for operative supracondylar humerus fractures. J Child Orthop 2018;12:502–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tuomilehto N, Kivisaari R, Sommarhem A, et al. Outcome after pin fixation of supracondylar humerus fractures in children: postoperative radiographic examinations are unnecessary. Acta Orthop 2017;88:109–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Houshian S, Mehdi B, Larsen MS. The epidemiology of elbow fracture in children: analysis of 355 fractures, with special reference to supracondylar humerus fractures. J Orthop Sci 2001;6:312–5. [DOI] [PubMed] [Google Scholar]
- 8.Narayanan U, Wood W. Best trauma paper at the 2017 POSNA Annual Meeting “acceptable reduction” for supracondylar humerus fractures in children. Pediatric Orthopaedic Society of North America meeting 2017. 2017 Oct. 13; Barcelona. [Google Scholar]
- 9.Karamitopoulos MS, Dean E, Littleton AG, et al. Postoperative radiographs after pinning of supracondylar humerus fractures: are they necessary? J Pediatr Orthop 2012;32:672–4. [DOI] [PubMed] [Google Scholar]