Abstract
Background
A large-scale industrial fire occurred in Rouen, France, in 2019. This study assessed the health-related quality of life of people exposed to its consequences 1 year later.
Methods
The study population comprised inhabitants of the exposed area and a non-exposed area. A representative sample was randomly selected using a stratified design. Data were collected using a standardized questionnaire to describe fire exposure and to calculate three health-related quality of life scores according to the SF12-v2 scale. After adjustment, descriptive and multivariate analyses were conducted.
Results
The sample comprised 4773 participants (response rate 47.7%). In the exposed area, the average mental, physical and overall health scores were 47.5, 52.0 and 73.8 out of 100, respectively. Mean mental and overall health scores were higher in the non-exposed area (49.0 and 76.0, respectively). After adjustment, a lower mental health score was associated with a higher number of perceived types of exposure, reaching −3.72 points [−5.41; −2.04] for five or more different types of perceived exposure. A lower mental health score was associated with soot deposits (−1.04 [−1.70; −0.39]), perceiving odours [(−2.04 [−3.22; −0.86]) up to the day of data collection], and having seen, heard or been awakened by the fire (−1.21 [−1.90; −0.52]). A slightly lower physical health score was associated with soot deposits (−0.57 [−1.07; −0.08]).
Conclusion
This study highlighted associations between exposure to the consequences of the industrial fire in Rouen and a deterioration of perceived health-related quality of life 1 year later, particularly the mental health dimension.
Introduction
On 26 September 2019, a large-scale industrial fire occurred in the warehouses of two companies in Rouen, France. As a result, a massive black smoke plume developed, and spread over several kilometres in a north-easterly direction, covering the regions of Normandy and Hauts-de-France. Approximately 9500 tons of chemical substances and various materials were burned, causing huge flames and barrel explosions. Debris from a smashed fibrocement roof was scattered over the surrounding area. The fire was extinguished nearly 12 h later. However, a smouldering fire lasted for some days. Soot deposits were observed after the fire, in addition to unpleasant persistent odours.1
Fortunately, no related deaths or injuries were reported. Local medical practitioners reported an increase in psychological disorders following the incident, including anxiety and stress.2 As a consequence, a medico-psychological unit was dispatched to help people in the days following the fire.3 During the month that followed the fire, a local epidemiological surveillance investigation was conducted.4 It highlighted a small increase in emergency care consultations for asthma and dyspnoea, as well as numerous reports to the local air quality monitoring organization regarding odours associated with otorhinolaryngological and ocular symptoms, bronchopulmonary irritation, general illness, and digestive tract disorders.
Several studies have highlighted the physical and mental health impact on people exposed to industrial or natural accidents.5,6 Belleville et al.5 showed that 1 year after the wildfires in Fort McMurray, Canada, in 2016, 38% of adult evacuees had a probable diagnosis of either post-traumatic stress, major depression, insomnia, generalized anxiety, or substance use disorder, or a combination of these conditions. Tjalvin et al.6 suggested that a year and a half after an oil tank explosion in western Norway in 2007, exposed workers had a higher Subjective Health Complaints Inventory score, and reported more self-reported mental and physical complaints than non-exposed workers.
The physical and mental health impacts of disasters can persist over the long term7 and exposure is associated with lower health-related quality of life (HRQL).8,9 A study conducted in Galicia, northwest Spain, showed that 1 year after the Prestige oil spill in 2002, residents living near the accident area, and those who were more exposed to the accident, had a lower mental health HRQL dimension score.8 Another study, also conducted in 2002, showed that 1 year after the World Trade Center Disaster and the subsequent American Airlines Flight 587 crash in 2001, exposure to cumulative disasters was associated with lower HRQL scores for general health, mental health and bodily pain.9 Other studies also highlighted the importance of assessing perceived health in areas affected by local environmental pollution.10–14
To our knowledge, few studies to date have assessed the impact of industrial fires or technological accidents on the HRQL of an exposed population, especially in the medium term. In order to assess the health impact of the fire in Rouen, an epidemiological surveillance tool called ‘The Post Fire 76 Health—“A study that listens to your health”’ was implemented among the general population in the affected area.15,16 The present analysis aimed to assess the associations between exposure to the fire and HRQL in the medium term (i.e. 1 year after the accident), as part of the cross-sectional study included in this tool.
Methods
Study area and population
‘The Post Fire 76 Health’ study took place in two areas of the Seine-Maritime department (a sub-regional administrative area) of the Normandy administrative region (Appendix 1). To make comparative analyses, the exposed area—the city of Rouen and its surroundings—was compared with a non-exposed area. For the latter, the city of Le Havre and its surroundings, located 70 kilometres northwest of Rouen, was chosen, because of its comparability in terms of territory and socioeconomic characteristics.17
In order to take into account the various types of exposure to the accident, geographical stratification was implemented on the exposed area based on environmental observations (Appendix 1). Four geographical strata were defined as follows: (i) a ‘proximity’ stratum, defined by a geographic criterion (0–700 and 700–1500 m from the site of the fire); (ii) a ‘South-West’ stratum, which covered the municipalities where at least six unpleasant odour complaints were reported in the 2 months following the fire18; (iii) a ‘Far North-East’ stratum, which covered the area directly under the plume of black smoke generated by the fire; (iv) a ‘Close North-East’ stratum, which covered all municipalities that met the inclusion criteria of strata (ii) and (iii). The exposed and non-exposed population included all adults residing in the exposed and non-exposed areas, respectively.
Sampling procedure
The Survey Division of the National Institute of Statistics and Economic (Insee) randomly selected a representative sample from the 2019 edition of the national fiscal database called ‘The Demographic Files on Households and Individuals’ (Fidéli).19 A simple random sampling procedure was used to select one adult per household from each of the four exposure strata described above.17 In total, a random sample of 10 777 adults—7999 in the exposed area and 2778 in the non-exposed area—were contacted to participate in the survey.
Data collection
Data collection was conducted between September and December 2020, 1 year after the industrial fire, using a standardized questionnaire. Participants were invited to complete the questionnaire online (self-administration) or by phone with a professional interviewer.
One section of the questionnaire focused in detail on participants’ exposure to the fire and its aftermath. The elements covered included perceiving odours and the duration of this perception, being located under the plume of black smoke and the duration of this exposure, observing soot deposits around their home, having directly seen the flames or the location of the fire, hearing the effects of the fire, and the presence of fibrocement roof debris in their surrounding environment. The residential area (exposed/non-exposed indicator variable) and the distance from the participant’s home to the industrial site where the fire occurred were also assessed as exposure variables.
HRQL was assessed for participants in the exposed and non-exposed areas using the French validated version of the 12-item version of the Medical Outcomes Study—Short Form Health Survey (SF-12v2).20,21 This instrument assesses self-reported HRQL over the preceding four weeks, by measuring eight domains as follows: physical functioning, physical role, bodily pain, general health, vitality, social functioning, emotional role, and mental health. From these, two scores are calculated: the Physical Component Summary (PCS) and the Mental Component Summary (MCS). Each of these scores ranges from 0 to 100 (the higher the value, the better is the perceived health state). For the purposes of this study, an unadjusted Overall Health Score (OHS) was also constructed by summing the 12 items of the SF-12v2, scaled also from 0 to 100.
The confounding variables were either provided by the Fidéli sampling database19 or declared by the participants in the survey questionnaire. They included socio-demographic factors (age at the time of data collection, gender, number of adults in the household, length of time living in the region, housing occupation status and social housing residence), socioeconomic factors (education level, perceived financial situation, disposable household income in deciles, socio-professional status, socio-professional category and employment status), self-reported health and lifestyle-related factors [pre-existing chronic disease, body mass index (BMI), smoking status, alcohol and tobacco consumption, social isolation, professional relationship with one of the involved companies], and three coronavirus disease (COVID-19)-related variables (possible COVID-19 infection, having had a difficult COVID-19-related lockdown experience, concerns about the COVID-19 pandemic).
Statistical analyses
In order to reflect the studied population as accurately as possible, all statistical data analyses took into account the study sampling design. Very few missing data were observed (≈ 2%) and were replaced using the multivariate imputation by chained equations method (MICE).17,22
In the descriptive analysis, the categorical variables were described by weighted percentages and their 95% confidence intervals (95% CI). Quantitative variables were described by their means and their 95% CI. The mean values of the three HRQL scores, along with their corresponding 95% CI, were depicted for each stratum.
Linear regression models with Gaussian distribution were used for the multivariate analysis. First, the SF-12v2 scores of participants in the exposed and non-exposed areas were compared. Second, the associations between the number of perceived exposures related to the fire and the three HRQL scores were analyzed for participants in the exposed area. Moreover, we assessed the associations between the types of perceived exposures (as described above) and the three scores of the SF-12v2 for participants in the exposed area.
We used the Akaike Information Criterion (AIC) for model selection. Some variables were forced into the models [age, gender, perceived financial situation, education level, social housing, number of adults in the household (for the three HRQL scores), social isolation (for the MCS only) and possible COVID-19 infection (for the PCS only)]. Interactions between the variables were also tested. The absence of collinearity between the variables included in the model was verified using the variance inflation factor (VIF).
Statistical analyses were performed using the ‘survey’ package in R software 4.0.4 and SAS software 7.1.
Ethical considerations
The survey received approval from the French council for statistical information (CNIS, no. 178/H03) and the Committee of Public Statistics (No. 2020_17077_DG75-L002). Personal data processing was performed in compliance with the General Data Protection Regulation (GDPR). Specifically, data collection was based on the participants’ consent (article 9.2.1 GDPR) and only pseudonymized data were used for the analyses.
Results
Descriptive results
The study sample comprised 4773 adults (3758 in the exposed area and 1015 in the non-exposed area), corresponding to a participation rate of 47.7% (50.2% and 40.2%, respectively). Two-thirds (64.3%) of the participants used self-administered the questionnaire online.
The main socio-demographic, socioeconomic, self-reported health and lifestyle, and COVID-19-related factors of both populations are presented in table 1. Half (53.2%) of the exposed population were women and mean age was 49.3 (±0.4) years. Overall, the characteristics of both populations were similar, although the exposed population had a higher level of education, higher-socio-professional jobs, and were more concerned by the COVID-19 pandemic. Additional descriptive analyses are presented in Appendix 2.
Table 1.
Socio-demographic, socioeconomic, self-reported health and lifestyle, and COVID-19-related characteristics of participants in the exposed and non-exposed populations (N = 4773) ‘The Post Fire 76 Health—“A study that listens to your health”’
| Exposed population |
Non-exposed population |
|||
|---|---|---|---|---|
| n | % [95% CI] | n | % [95% CI] | |
| Gender | ||||
| Man | 1703 | 46.8 [45.0; 48.7] | 461 | 48.2 [44.9; 51.5] |
| Woman | 2061 | 53.2 [51.3; 55.0] | 554 | 51.8 [48.5; 55.1] |
| Level of education | ||||
| No schooling | 449 | 13.3 [12.0; 14.7] | 135 | 16.1 [13.5; 18.7] |
| Vocational training certificate | 475 | 13.5 [12.3; 14.8] | 146 | 15.0 [12.6; 17.4] |
| Middle-school diploma | 378 | 10.1 [8.9; 11.2] | 141 | 13.8 [11.5; 16.0] |
| High-school diploma | 738 | 18.6 [17.2; 20.1] | 216 | 20.8 [18.2; 23.4] |
| Post-secondary school diploma to 2-year third-level diploma | 615 | 14.4 [13.2; 15.6] | 173 | 16.6 [14.1; 19.0] |
| Bachelor’s to Doctorate degree | 1109 | 30.0 [28.4; 31.6] | 204 | 17.8 [15.4; 20.2] |
| Perceived financial comfort | ||||
| Comfortable | 668 | 17.9 [16.6; 19.3] | 188 | 17.3 [14.8; 19.7] |
| Getting by | 1431 | 36.2 [34.4; 37.9] | 442 | 42.3 [39.0; 45.5] |
| Just getting by, need to be careful | 1129 | 34.1 [32.3; 35.8] | 286 | 29.4 [26.3; 32.4] |
| Cannot make ends meet without going into debt | 436 | 11.9 [10.6; 13.1] | 99 | 11.1 [8.9; 13.3] |
| Smoking status | ||||
| Daily smoker | 614 | 16.3 [14.9; 17.7] | 158 | 16.6 [14.1; 19.2] |
| Occasional smoker | 279 | 7.1 [6.1; 8.0] | 52 | 5.5 [4.0; 7.1] |
| Ex-smoker | 884 | 22.9 [21.4; 24.4] | 247 | 22.9 [20.2; 25.6] |
| Non-smoker | 1987 | 53.7 [51.9; 55.6] | 558 | 54.9 [51.6; 58.2] |
| Alcohol consumption | ||||
| Daily | 181 | 5.5 [4.6; 6.4] | 69 | 6.8 [5.9; 7.6] |
| 4–6 times per week | 115 | 3.1 [2.5; 3.7] | 34 | 3.3 [2.1; 4.5] |
| 2–3 times per week | 559 | 14.4 [13.2; 15.7] | 148 | 13.4 [11.3; 15.6] |
| Once per week | 239 | 6.6 [5.7; 7.5] | 74 | 7.3 [5.6; 9.1] |
| One or several times per month | 1006 | 25.7 [24.1; 27.3] | 259 | 23.9 [21.1; 26.6] |
| Less than once per month | 648 | 17.9 [16.5; 19.3] | 169 | 18.1 [15.4; 20.7] |
| Never | 1016 | 26.8 [25.1; 28.4] | 262 | 27.2 [24.2; 30.2] |
| Social isolation | ||||
| Feeling very alone/alone | 534 | 14.9 [13.6; 16.3] | 109 | 11.6 [9.4; 13.8] |
| Feeling supported/very supported | 3230 | 85.1 [83.7; 86.5] | 906 | 88.4 [86.2; 90.59] |
| Possible COVID-19 infection | ||||
| No | 2987 | 79.5 [78.0; 80.9] | 827 | 81.2 [78.5; 83.8] |
| Yes, not certain | 350 | 9.2 [8.2; 10.3] | 69 | 6.8 [5.1; 8.5] |
| Yes, certain | 67 | 1.6 [1.2; 2.1] | 14 | 1.1 [0.5; 1.7] |
| Don’t know/refuse to answer | 360 | 9.7 [8.6; 10.8] | 105 | 10.9 [8.8; 13.0] |
| Difficult COVID-19-related lockdown experience | ||||
| Not difficult or a little difficult | 1258 | 33.4 [31.7; 35.2] | 406 | 39.8 [36.5; 40.0] |
| Moderately difficult | 1527 | 41.0 [39.2; 42.9] | 384 | 37.0 [33.9; 40.2] |
| Very difficult | 979 | 25.5 [23.9; 27.2] | 225 | 23.2 [20.3; 26.0] |
| Concerns about the COVID-19 pandemic | ||||
| Not or a little concerned | 499 | 13.5 [12.2; 14.7] | 147 | 14.2 [11.9; 16.4] |
| Moderately concerned | 1687 | 44.2 [42.4; 46.0] | 509 | 49.6 [46.3; 52.9] |
| Very concerned | 1578 | 42.4 [40.4; 44.2] | 359 | 36.3 [33.0; 39.5] |
| Mean | SD of mean | Mean | SD of mean | |
| Age (years) | 49.3 | 0.4 | 50.1 | 0.7 |
n, number of participants; %, weighted percentages; [95% CI], 95% confidence interval.
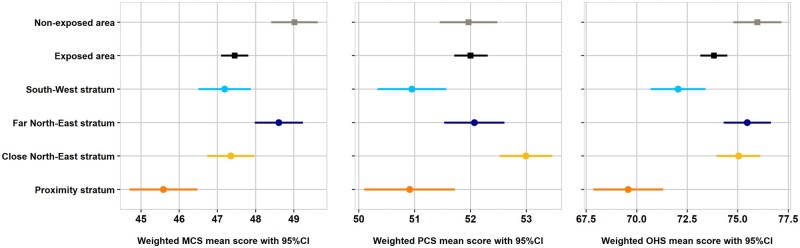
One year after the industrial fire, the mean MCS score of the exposed population was lower than that for the non-exposed population [47.5 (95% CI: 47.1; 47.8) vs. 49.0 (95% CI: 48.4; 49.6)]. Participants living in the proximity stratum had a lower MCS score [45.6 (95% CI: 44.7; 46.5)] than those living in more distant locations.
The observed mean PCS score was similar in both populations [(52.0 95% CI: 51.7; 52.3) and (52.0 95% CI: 51.4; 52.5) for those exposed and non-exposed, respectively], and was slightly lower among participants in the proximity stratum [50.9 (95% CI: 50.1; 51.7)].
The mean OHS was lower in the exposed population [73.8 (95% CI: 73.2; 74.5) vs. (76.0 95% CI: 74.8; 77.2)]. Participants in the proximity stratum had a lower mean OHS [69.6 (95% CI: 67.9; 71.3)] than participants in other strata (figure 1).
Figure 1.
SF-12v2 scores of the participants per area (exposed/non-exposed) and per stratum (SouthWest/Far North-East/Close North-East/Proximity) (weighted mean, 95% confidence interval [95% CI], N = 4773). MCS, mental component summary; PCS, physical component summary; OHS, overall health score. ‘The Post Fire 76 Health—“A study that listens to your health”’.
Multivariate analysis results
Mental health
The mean MCS score of the non-exposed area was slightly higher than that of the exposed area, with a significant difference of 0.69 points (table 2).
Table 2.
Adjusted comparisons of SF-12v2 scores between participants in the exposed and non-exposed area (N = 4773) ‘The Post Fire 76 Health—“A study that listens to your health”’
| MCS |
PCS |
OHS |
||||
|---|---|---|---|---|---|---|
| Regression coefficient [95% CI]a | P-valuea | Regression coefficient [95% CI]b | P-valueb | Regression coefficient [95% CI]c | P-valuec | |
| Exposed/NON-exposed area | ||||||
| Participants in the exposed area | Reference | Reference | Reference | |||
| Participants in the non-exposed area | 0.69 [0.05; 1.34] | 0.036 | 0.08 [−0.43; 0.59] | 0.771 | 0.98 [−0.20; 2.16] | 0.104 |
MCS, mental component summary; PCS, physical component summary; OHS, overall health score.
Adjusted for age, gender, number of adults in the household, length of time living in the region, social housing, education level, perceived financial situation, pre-existing chronic disease, BMI, social isolation, possible COVID-19 infection, having had a difficult COVID-19-related lockdown experience, and having concerns about the COVID-19 pandemic.
Adjusted for age, gender, number of adults in the household, social housing, education level, perceived financial situation, BMI, pre-existing chronic disease, smoking status, alcohol consumption, social isolation, and possible COVID-19 infection.
Adjusted for age, gender, number of adults in the household, length of time living in the region, social housing, education level, perceived financial situation, BMI, pre-existing chronic disease, smoking status, alcohol consumption, social isolation, possible COVID-19 infection, having had a difficult COVID-19-related lockdown experience, and having concerns about the COVID-19 pandemic.
Perceiving two, three, four and five or more exposures in the exposed area was significantly associated with a lower MCS score than not perceiving any exposure, with a difference of 1.73, 2.24, 3.10 and 3.72 points, respectively.
In the exposed area, observing soot deposits around one’s home was statistically associated with a lower MCS score (difference of 1.04 points), compared with not perceiving soot deposits. Perceiving odours related to the fire for the modalities for ‘several weeks’ and ‘up to the day of data collection’ were significantly associated with a lower MCS score compared with not perceiving these odours (difference of 1.65 points and of 2.04 points, respectively).
Having heard, seen or been awakened by the fire was associated with a lower MCS score (difference of 1.21 points) (table 3).
Table 3.
Associations between the number of perceived exposures related to the fire and the SF-12v2 scores and associations between the various types of perceived exposures related to the fire and the SF-12v2 scores in the exposed area (n = 3758) ‘The Post Fire 76 Health—“A study that listens to your health”’
| MCS |
PCS |
OHS |
||||
|---|---|---|---|---|---|---|
| Regression coefficient [95% CI]a | P-valuea | Regression coefficient [95% CI]b | P-valueb | Regression coefficient [95% CI]c | P-valuec | |
| Number of perceived exposures in the exposed area | ||||||
| None | Reference | Reference | Reference | |||
| One | −1.04 [−2.40; 0.32] | 0.133 | 0.85 [−0.31; 2.02] | 0.151 | 0.07 [−2.33; 2.47] | 0.954 |
| Two | −1.73 [−3.08; −0.38] | 0.012 | 0.54 [−0.63; 1.70] | 0.367 | −1.35 [−3.68; 0.99] | 0.258 |
| Three | −2.24 [−3.64; −0.85] | 0.002 | 0.29 [−0.88; 1.46] | 0.625 | −2.47 [−4.91; −0.04] | 0.047 |
| Four | −3.10 [−4.68; −1.52] | <0.0001 | −0.76 [−2.05; 0.52] | 0.245 | −5.29 [−8.00; −2.57] | 0.0001 |
| Five or more | −3.72 [−5.41; −2.04] | <0.0001 | −0.81 [−2.17; 0.56] | 0.247 | −6.27 [−9.18; −3.35] | <0.0001 |
| Observing soot deposits around one's home | ||||||
| No | Reference | Reference | Reference | |||
| Yes | −1.04 [−1.70; −0.39] | 0.002 | −0.57 [−1.07; −0.08] | 0.024 | −2.30 [−3.42; −1.17] | <0.0001 |
| Duration of exposure to odours | ||||||
| None | Reference | – | – | Reference | ||
| A few hours | −0.83 [−2.48; 0.83] | 0.329 | – | – | 0.28 [−2.73; 3.29] | 0.856 |
| Several days | −0.76 [−1.86; 0.34] | 0.176 | – | – | −0.31 [−2.28; 1.66] | 0.758 |
| Several weeks | −1.65 [−2.73; −0.57] | 0.003 | – | – | −1.58 [−3.52; 0.35] | 0.109 |
| Several months | −1.12 [−2.27; 0.04] | 0.059 | – | – | −1.59 [−3.66; 0.48] | 0.132 |
| Up to the day of data collection | −2.04 [−3.22; −0.86] | 0.001 | – | – | −2.73 [−4.84; −0.63] | 0.011 |
| Heard, seen or been awakened by the fire | ||||||
| No | Reference | Reference | Reference | |||
| Yes | −1.21 [−1.90; −0.52] | 0.001 | −0.47 [−0.98; 0.03] | 0.068 | −2.37 [−3.56; −1.18] | 0.0001 |
MCS, mental component summary; PCS, physical component summary; OHS, overall health score.
Adjusted for age, gender, number of adults in the household, length of time living in the region, social housing, education level, perceived financial situation, BMI, pre-existing chronic disease, social isolation, possible COVID-19 infection, having had a difficult COVID-19-related lockdown experience, and having concerns about the COVID-19 pandemic.
Adjusted for age, gender, number of adults in the household, social housing, education level, perceived financial situation, BMI, pre-existing chronic disease, smoking status, alcohol consumption, social isolation and possible COVID-19 infection.
Adjusted for age, gender, number of adults in the household, length of time living in the region, social housing, education level, perceived financial situation, BMI, pre-existing chronic disease, smoking status, alcohol consumption, social isolation, possible COVID-19 infection, having had a difficult COVID-19-related lockdown experience, and having concerns about the COVID-19 pandemic.
Physical health
No significant difference was observed between the exposed and the non-exposed areas concerning the PCS score (table 2). Furthermore, no significant associations were observed between the perceived number of exposures related to the fire and the PCS score (table 3).
When assessing the types of exposures in the exposed area, only exposure to soot deposits was significantly associated with a slightly lower PCS score (difference of 0.57 points) (table 3).
Overall health
No difference for the OHS was observed when comparing the exposed and non-exposed areas (table 2).
On the contrary, perceiving three, four, and five or more exposures related to the fire in the exposed area was significantly associated with a lower OHS than not perceiving any exposure (difference of 2.47, 5.29, and 6.27 points, respectively) (table 3).
Observing soot deposits around one’s home was significantly related to lower mean OHS, (difference of 2.30 points). Participants, who perceived odours up to the day of data collection had a lower OHS (mean difference of 2.73 points) compared with participants who did not perceive odours. Finally, having heard, seen or been awakened by the fire was associated with a significantly lower OHS (difference of 2.37 points) (table 3).
Discussion
This study aimed to assess the HRQL of people exposed to the consequences of a large-scale industrial fire in the medium term. Our results suggest that 1 year after the event, experiencing several types of exposure, smelling odours (especially for a long time), observing soot deposits around one’s home, and having heard, seen, or been awakened by the accident, were all negatively associated with participants’ HRQL. This result is most probably due to an impact on participants’ mental health, which was evaluated with the MCS score of the SF-12v2.
The HRQL scores for inhabitants in the proximity stratum were lower than those for inhabitants in the other three strata. This can be explained by the fact that people residing near the site of the fire may have experienced the consequences of the fire more intensely and/or for a longer duration. They may also have had a lower socioeconomic level and more difficulties in coping with this kind of situation. These possibilities echo existing literature and underline the importance of the impact of this type of an accident on HRQL and in particular on the mental health component, despite the fact that no related deaths or injuries were reported.8,23,24
Mental health
The present study showed that participants in the exposed area had a significantly lower MCS score than persons in the non-exposed area one year after the fire. This result is consistent with data from various scientific studies showing the health impact of catastrophic events and their consequences on mental health in the short, medium and long terms.7,24–26
A lower MCS score was strongly associated with the number of perceived exposures to the fire. Specifically, reporting two or more exposures was associated with a significantly and monotonously lower MCS score. These results are also in line with existing literature which shows an association between the intensity or number of exposures and the risk of psychopathology, usually a dose–response type relationship.8,25,27,28
Observing soot deposits around one’s home was associated with a lower MCS score. Seeing soot highlighted the quantity of pollution generated by the fire and its persistence in the environment, even after the dispersion of the plume of black smoke. This experience may have worried inhabitants, thereby creating a negative effect on the exposed population’s mental health.
A lower MCS score was also associated with perceiving unpleasant odours ‘for several weeks’ and ‘up to the day of data collection. This result is also consistent with the scientific literature. The olfactory sense is linked to the emotional system.29 Mental health disorders such as anxiety and depression have previously been associated with the duration of residence in an environment with unpleasant odours and olfactory discomfort.11 A study conducted following the 2010 Deepwater Horizon oil spill in the Gulf of Mexico also showed that exposure to odours was associated with depression.30
In our study, participants who reported seeing or hearing the fire had a lower MCS score than those who did not. This reflects findings in a study conducted among residents of Fort McMurray 18 months following the 2016 wildfires, showed a significant association between witnessing burning homes and depression.31
Physical health
We found no significant association between either the number or type of exposure to the fire and physical health 1 year after the event, assessed using the PCS from the SF-12v2. The only exception was for people who observed soot deposits around their home. This sub-group had a slightly lower PCS score (−0.57 points) than people who did not observe soot deposits.
The presence of soot deposits could be an indicator of the level of exposure to fumes whether visible or not. Globally, air pollution may be associated with effects on physical health.32,33 Exposure to soot deposits and the duration of exposure to chemical pollution and environmental nuisances from the fire may probably not have been sufficient to cause physical problems detectable in the medium term by our study, which was exclusively based on self-reported health. The absence of significant results on perceived physical health might also be explained by the fact that this industrial accident did not lead to injuries likely to induce physical sequelae.
Overall health
Observing soot deposits and having heard, seen or been awakened by the fire were associated with a lower OHS. In addition, the OHS gradually decreased as the number of perceived nuisances and the duration of perceived odours increased.
Considering the respective effects of perceived exposure to the industrial fire on the MCS and PCS, this overall deterioration in health was mainly due to the negative impact we observed on mental health.
Our study has several limitations. First, because of its cross-sectional design, no causal relationships between exposure to the fire and HRQL could be established. This limitation likely reflects bidirectional associations. Second, data collection occurred 1 year after the industrial fire. Hence, accounts of perceived exposures were susceptible to recall bias, although the latter is limited in the context of large-scale disasters and accidents. Residents close to the fire area may have overestimated the intensity of their exposure and/or the effects of the fire.34 However, the SF-12v2 survey looks at the 4 weeks preceding a study interview, which limits recall bias for HRQL measures.20,21 Finally, data may have been subject to desirability bias for participants who completed the questionnaire by phone with the assistance of a professional interviewer.35
There are also several study strengths. First, the sampling strategies, the number of people included, and the statistical analyses used made it possible to obtain a representative sample and to reach good statistical power.17 Second, besides defining geographical strata, we assessed the exposure not only by using binary variables, but also by evaluating the duration of certain exposures. This approach acknowledges the difficulties of measuring different exposures after a disaster.36 Third, the literature has highlighted the effect of the COVID-19 pandemic on mental and physical health.37,38 In our study, by including a non-exposed population, we were able to take this potential effect into consideration and to compare the results with the exposed population. Fourth, we used a validated psychometric scale to measure participants’ HRQL. This meant that we could reliably assess participants’ self-perceived health.20,21 The monotonous dose–response associations we found between a lower MCS score and a higher number of exposures reflect the potential impact of this fire on exposed people’s health. Finally, the consistency of the results obtained, as well as the observed deterioration of mental health but not physical health, as one might have expected for this accident, underlines the internal validity of our study.
In conclusion, the present study highlighted significant associations between the number and types of exposures related to the industrial fire in Rouen in September 2019 and the local population’s HRQL, mainly the mental health dimension, 1 year after the event.
These associations underline the importance of assessing medium term HRQL and self-perceived health—especially the mental dimension—following such an event.
Furthermore, our results highlight various actions to implement when preparing an effective response to similar future industrial accidents. These include: (i) paying particular attention to residents near the accident, (ii) training health professionals on the toxic and psychological effects observed after such events, (iii) taking into account all exposures, in particular odours, in the communication and the health management of the event, (iv) informing health professionals during the event about known exposures, observed health effects and their management, and finally, (v) informing the general population about all potential effects and actions to take in the event of such an accident.16
Supplementary Material
Acknowledgements
The authors are most grateful to all the study participants from Rouen and Le Havre for their involvement, Mélanie Martel for her help in designing the survey and administering the questionnaires to Travelers, as well as all members of health advisor groups and the scientific council, in particular: Marcel Calvez, Michel Chadelaud, Alain Rouzies, André Cicolella, Yvon Graïc, Patrick Daimé, Bruno Burel, Martine Fleury, Robert Garnier, Anne Maître, Maria Melchior, Olivier Borraz, and Jean-Claude Pairon. Finally, we would like to thank IPSOS Observer, and Jude Sweeney (Milan, Italy) for his careful copyediting of the manuscript.
Contributor Information
Maria El Haddad, Data Science Division, French National Public Health Agency, Saint Maurice, France.
Abdelkrim Zeghnoun, Data Science Division, French National Public Health Agency, Saint Maurice, France.
Jean-Baptiste Richard, Data Science Division, French National Public Health Agency, Saint Maurice, France.
Abdessattar Saoudi, Data Science Division, French National Public Health Agency, Saint Maurice, France.
Gaëlle Pédrono, Data Science Division, French National Public Health Agency, Saint Maurice, France.
Anne-Laure Perrine, Data Science Division, French National Public Health Agency, Saint Maurice, France.
Yvon Motreff, Non-Communicable Diseases and Trauma Division, French National Public Health Agency, Saint Maurice, France; Department of Social Epidemiology, Inserm, Sorbonne Université, Institut Pierre Louis d’Epidémiologie et de Santé Publique (IPLESP), Paris, France.
Myriam Blanchard, Regional Division, French National Public Health Agency, Normandy, France.
Pauline Morel, Regional Division, French National Public Health Agency, Normandy, France.
Emmanuelle Le Lay, International Scientific Division, French National Public Health Agency, Saint Maurice, France.
Franck Golliot, Regional Division, French National Public Health Agency, Saint Maurice, France.
Pascal Empereur-Bissonnet, Regional Division, French National Public Health Agency, Saint Maurice, France.
Supplementary data
Supplementary data are available at EURPUB online.
Funding
This study was conducted by Santé publique France, which is the French Public Health Agency. Santé publique France is funded by the French Ministry of Health.
Data availability
Data are available upon request from the authors.
Conflicts of interest: None declared.
Key points.
The large-scale industrial fire in 2019 in Rouen, France, had a negative impact on HRQL observed 1 year later in the exposed population, especially for inhabitants who were close to the site of fire when it occurred.
The deterioration of mental and overall health in persons in the exposed area was monotonously associated with the number of perceived exposures.
Perceiving odours (especially over a long time), observing soot deposits around one’s home, and having seen, heard or been awakened by the fire, were all negatively associated with the mental health dimension of quality of life in people living in the exposed area.
Only observing soot deposits around one’s home was associated with a slightly lower physical health score among inhabitants of the exposed area.
Several actions could be taken when future similar industrial accidents occur such as paying particular attention to residents near the accident, training health professionals on the potential toxic and psychological effects, and taking into account all exposures in communications to the general population, including perceptible exposures such as odours.
References
- 1. Bureau d’analyse des risques et pollutions industriels (Barpi). Incendie sur deux sites industriels aux zones d’entreposage mitoyennes. 26 septembre 2019. Rouen et Petit-Quevilly (Seine-Maritime), France. [Fire on two industrial sites with adjoining storage areas. September 26, 2019. Rouen and Petit-Quevilly (Seine-Maritime), France.]. Ministère de la Transition écologique, Direction générale de la prévention des risques, France, 2020. [Google Scholar]
- 2. Assemblé Nationale. Rapport d’information sur l’incendie d’un site industriel à Rouen. [Information report on the fire at an industrial site in Rouen.] no. 2689. Paris Assemblée Nationale, France, 2020. [Google Scholar]
- 3. Prieto N, Cheucle E, Faure P, et al. [Defusing of victims of the terrorist attacks in Paris. Elements of assessment one-month post-event]. Encephale 2018;44:118–21. [DOI] [PubMed] [Google Scholar]
- 4. Blanchard M, Leduc G, Sinno-Tellier S, et al. Early health impact assessment of a major industrial fire at a chemical plant on September 26, 2019, Rouen, France. Environnement Risques Santé 2021;20:171–80. [Google Scholar]
- 5. Belleville G, Ouellet M-C, Lebel J, et al. Psychological symptoms among Evacuees from the 2016 Fort McMurray Wildfires: a population-based survey one year later. Front Public Health 2021;9:655357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Tjalvin G, Hollund BE, Lygre SH, et al. Subjective health complaints among workers in the aftermath of an oil tank explosion. Arch Environ Occup Health 2015;70:332–40. [DOI] [PubMed] [Google Scholar]
- 7. van der Velden PG, Wong A, Boshuizen HC, Grievink L. Persistent mental health disturbances during the 10 years after a disaster: four-wave longitudinal comparative study. Psychiatry Clin Neurosci 2013;67:110–8. [DOI] [PubMed] [Google Scholar]
- 8. Sabucedo JM, Arce C, Senra C, et al. Symptomatic profile and health-related quality of life of persons affected by the Prestige catastrophe. Disasters 2010;34:809–20. [DOI] [PubMed] [Google Scholar]
- 9. Fernandez WG, Galea S, Miller J, et al. Health status among emergency department patients approximately one year after consecutive disasters in New York City. Acad Emerg Med 2005;12:958–64. [DOI] [PubMed] [Google Scholar]
- 10. Daniau C, Dor F, Eilstein D, et al. [Study of self-reported health of people living near point sources of environmental pollution: a review. First part: health indicators]. Rev Epidemiol Sante Publique 2013;61:375–87. [DOI] [PubMed] [Google Scholar]
- 11. Daniau C, Dor F, Eilstein D, et al. [Study of self-reported health of people living near point sources of environmental pollution: a review. Second part: analysis of results and perspectives]. Rev Epidemiol Sante Publique 2013;61:388–98. [DOI] [PubMed] [Google Scholar]
- 12. Daniau C, Wagner V, Salvio C, et al. Perceived state of health of the population living near a chemical industrial platform: salindres]. Environnement Risques Sante 2018;17:583–95. [Google Scholar]
- 13. Martin S, Guillam MT, Cassagne E, et al. Étude des perceptions des habitants de la Vallée-de-Seine (Yvelines) relatives à leur environnement et leur santé: phase quantitative. [Study of the perceptions of residents of the Vallée-de-Seine (Yvelines) relating to their environment and their health: quantitative phase.]. Rev Épidémiol Santé Publique 2016;64:S249. [Google Scholar]
- 14. Nijrolder I, van der Velden PG, Grievink L, Yzermans CJ. Symptom attribution and presentation in general practice after an extreme life event. Fam Pract 2011;28:260–6. [DOI] [PubMed] [Google Scholar]
- 15. Golliot F, Blanchard M, Empereur-Bissonnet P, et al. Évaluation de l’impact sanitaire de l’incendie industriel survenu à Rouen. Dispositif d’études « Santé post-incendie 76 ». [Assessment of the health impact of the industrial fire that occurred in Rouen. “The Post Fire 76 Health” study.]. Environnement Risques Santé 2021;20:164–70. [Google Scholar]
- 16. Empereur-Bissonnet P, Perrine AL, Pédrono G, et al. Santé Post Incendie 76 – Une Étude à L’écoute de Votre Santé. Étude Épidémiologique Par Questionnaire Sur L’incendie Industriel du 26 Septembre 2019 à Rouen (France). Rapport Principal. [“The Post Fire 76 Health” – a study that listens to your health. Epidemiological study by questionnaire on the industrial fire of September 26, 2019 in Rouen (France). Main Report]. Saint-Maurice: Santé publique France, 2021: 81. [Google Scholar]
- 17. Richard J, Perrine A, Zeghnoun A, et al. Santé Post-Incendie 76: une étude à l’écoute de votre santé. Bilan méthodologique. [“The Post Fire 76 Health”: a study that listens to your health. Methodological review.] Santé publique France, France, 2022. [Google Scholar]
- 18. Atmo Normandie. Incendie Lubrizol et NL Logistique: bilan des mesures de polluants et d’odeurs dans l’air ambiant et les retombées atmosphériques. [Lubrizol and NL Logistics fire: assessment of measurements of pollutants and odors in ambient air and atmospheric fallout.] Rapport no. 2520-001. Rouen: Atmo Normandie, France, 2021. Available at: http://www.atmonormandie.fr/Media/Files/Publication-Atmo-Normandie/rapports/2021/Rapport-Lubrizol-NL-Logistique (May 2021, date last accessed). [Google Scholar]
- 19. Insee. Fichier démographique d’origine fiscale sur les logements et les personnes (Fideli). [Demographic file of fiscal database on households and Individuals (Fidéli)]. Montrouge, France, 2020. Available at: https://www.insee.fr/fr/information/3897375 (March 2024, date last accessed). [Google Scholar]
- 20. Ware J Jr, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care 1996;34:220–33. [DOI] [PubMed] [Google Scholar]
- 21. Gandek B, Ware JE, Aaronson NK, et al. Cross-validation of item selection and scoring for the SF-12 Health Survey in nine countries: results from the IQOLA Project. International Quality of Life Assessment. J Clin Epidemiol 1998;51:1171–8. [DOI] [PubMed] [Google Scholar]
- 22. Azur MJ, Stuart EA, Frangakis C, Leaf PJ. Multiple imputation by chained equations: what is it and how does it work? Int J Methods Psychiatr Res 2011;20:40–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Institut de veille sanitaire. Conséquences sanitaires de l’explosion survenue à l’usine “AZF”, le 21 septembre 2001. Rapport final sur les conséquences sanitaires dans la population toulousaine. [Health consequences of the explosion that occurred at the “AZF” factory on September 21, 2001. Final report on the health consequences among Toulouse population.] Saint-Maurice: Institut de veille sanitaire, 2006. Available at: https://www.santepubliquefrance.fr/regions/occitanie/documents/rapport-synthese/2006/consequences-sanitaires-de-l-explosion-survenue-a-l-usine-azf-le-21-septembre-2001.-rapport-final-sur-les-consequences-sanitaires-dans-la-popula (March 2024, date last accessed). [Google Scholar]
- 24. Gissurardóttir ÓS, Hlodversdóttir H, Thordardóttir EB, et al. Mental health effects following the eruption in Eyjafjallajökull volcano in Iceland: a population-based study. Scand J Public Health 2019;47:251–9. [DOI] [PubMed] [Google Scholar]
- 25. Goldmann E, Galea S. Mental health consequences of disasters. Annu Rev Public Health 2014;35:169–83. [DOI] [PubMed] [Google Scholar]
- 26. Hahn MB, Van Wyck R, Lessard L, Fried R. Compounding effects of social vulnerability and recurring natural disasters on mental and physical health. Disaster Med Public Health Prep 2021;16:1013–21. [DOI] [PubMed] [Google Scholar]
- 27. McFarlane AC, Williams R. Mental health services required after disasters: learning from the lasting effects of disasters. Depress Res Treat 2012;2012:970194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Adams RE, Boscarino JA. Stress and well-being in the aftermath of the world trade center attack: the continuing effects of a communitywide disaster. J Community Psychol 2005;33:175–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Bushdid C, Topin J, Golebiowski J. Quand l’atmosphère sent le soufre. Perception des pollutions odorantes. When the atmosphere smells like sulfur. Perception of malodors. Pollution Atmosphérique 2017;234(3). Available at: http://lodel.irevues.inist.fr/pollution-atmospherique/index.php?id=5245. [Google Scholar]
- 30. Kwok R, McGrath J, Lowe S, et al. Mental health indicators associated with oil spill response and clean-up: cross-sectional analysis of the GuLF STUDY cohort. Lancet Public Health 2017;2:e560–e567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Moosavi S, Nwaka B, Akinjise I, et al. Mental health effects in primary care patients 18 months after a major wildfire in Fort McMurray: risk increased by social demographic issues, clinical antecedents, and degree of fire exposure. Front Psychiatry 2019;10:683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Yang BY, Qian Z, Howard SW, et al. Global association between ambient air pollution and blood pressure: a systematic review and meta-analysis. Environ Pollut 2018;235:576–88. [DOI] [PubMed] [Google Scholar]
- 33. Liu Y, Pan J, Zhang H, et al. Short-term exposure to ambient air pollution and asthma mortality. Am J Respir Crit Care Med 2019;200:24–32. [DOI] [PubMed] [Google Scholar]
- 34. Grimm A, Hulse L, Preiss M, Schmidt S. Behavioural, emotional, and cognitive responses in European disasters: results of survivor interviews. Disasters 2014;38:62–83. [DOI] [PubMed] [Google Scholar]
- 35. McHorney CA, Kosinski M, Ware JE Jr. Comparisons of the costs and quality of norms for the SF-36 health survey collected by mail versus telephone interview: results from a national survey. Med Care 1994;32:551–67. [DOI] [PubMed] [Google Scholar]
- 36. Bongers S, Janssen NA, Reiss B, et al. Challenges of exposure assessment for health studies in the aftermath of chemical incidents and disasters. J Expo Sci Environ Epidemiol 2008;18:341–59. [DOI] [PubMed] [Google Scholar]
- 37. Chan-Chee C, eacute O, Lasbeur L, et al. , editors. The mental health of the French facing the Covid-19 crisis: prevalence, evolution and determinants of anxiety disorders during the first two weeks of lockdown (CoviPrev study, 23-25 March and 30 March-1 April, 2020), Santé publique France, France, 2020.
- 38. Carvalho-Schneider C, Laurent E, Lemaignen A, et al. Follow-up of adults with noncritical COVID-19 two months after symptom onset. Clin Microbiol Infect 2021;27:258–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data are available upon request from the authors.
Conflicts of interest: None declared.
Key points.
The large-scale industrial fire in 2019 in Rouen, France, had a negative impact on HRQL observed 1 year later in the exposed population, especially for inhabitants who were close to the site of fire when it occurred.
The deterioration of mental and overall health in persons in the exposed area was monotonously associated with the number of perceived exposures.
Perceiving odours (especially over a long time), observing soot deposits around one’s home, and having seen, heard or been awakened by the fire, were all negatively associated with the mental health dimension of quality of life in people living in the exposed area.
Only observing soot deposits around one’s home was associated with a slightly lower physical health score among inhabitants of the exposed area.
Several actions could be taken when future similar industrial accidents occur such as paying particular attention to residents near the accident, training health professionals on the potential toxic and psychological effects, and taking into account all exposures in communications to the general population, including perceptible exposures such as odours.