Before 1948, building the hospital and community health service was primarily a local government responsibility and new investment depended on local authorities’ ability to meet the cost of borrowing. The “depressed areas,” which had the worst health status, were inevitably disadvantaged. Investment patterns during the interwar years contributed to the inequitable distribution of the infrastructure, which was, according the official historian of the NHS, a “ramshackle and largely bankrupt edifice.”1 The 1946 act led to the nationalisation of the inherited hospital infrastructure and the centralisation of the responsibility for financing its improvement within the ministry of health. NHS hospital building was to be financed by central government grants and funded out of general taxation and national insurance contributions.
The NHS initially made little impact on its inherited infrastructure problems because public sector investment in the postwar years was concentrated on education and housing. Aneurin Bevan, among others, suggested that spending controls could be evaded if hospital boards were allowed to borrow from the market, as they had before the war. But with funding now ultimately paid for out of general taxation, no rationale could be found for allowing boards to borrow at interest rates that would necessarily be higher than those incurred by central government (J Mohan, personal communication). Not until the mid-1950s did a gradual release of funding allow new hospital building in some areas that had a legacy of prewar planning inequities. Even so, the scale of investment fell a long way short of “complete replacement.”2
The principle of major hospital investment was finally adopted in the 1962 hospital plan. The plan was the first attempt to modernise the hospital infrastructure as a whole. But it remains unfulfilled, with only a third of the projected 224 schemes completed, a third partially completed, and a third not yet started. Investment in major developments was increasingly postponed as limited capital funds were spread ever more thinly. Between 1980 and 1997, only seven public schemes costing more than £25 million were completed.3
Summary points
The private finance initiative is a method of financing, not of funding. It allows the government to defer public spending—albeit at a much higher cost
Capital charges created a method of paying for private sector financing by using the revenue budget
The use of land sales and capital charges to fund investment means that local affordability, not national priorities, determines investment
The high costs of private sector financing have increased affordability problems at national and local level
The increased costs of the private finance initiative are being met from hospital closure programmes, reductions in services and capacity, subsidies from the Treasury, NHS block capital allocations, and trusts’ operational budgets
The private finance initiative transfers ownership and responsibility for providing services from the public to the private sector
The pattern of relatively low or declining capital investment has created severe problems. Today, the infrastructure still retains many pre-NHS features and a significant proportion of the stock predates the first world war. Capital spending has been insufficient to either replace or maintain outworn and outmoded buildings. The backlog of maintenance, now standing at £2.6bn, is partly the consequence and partly the cause of intensifying pressures on revenue. In 1996-7, one third of NHS trusts failed to meet at least one of their financial targets.4
Since 1992, most new capital investment has involved the private finance initiative (PFI). Under the private finance initiative the private sector designs, builds, finances, owns, and operates services. Hospitals funded by the private finance initiative are leased back to the public sector for periods of up to 60 years. Thirty one new hospitals are to be built; contracts for 12 have been signed to date (table 1). This paper shows how these hospitals, said by government to comprise “the largest hospital building programme in the history of the NHS,”5 will be funded through extensive hospital closures and resources generated by NHS trusts, not by new government funds.
Table 1.
First and second wave schemes financed by the private finance initiative, England
| Capital value* (£m) | |
|---|---|
| First wave | |
| Dartford and Gravesham NHS Trust | 94 |
| Carlisle Hospital NHS Trust | 65 |
| South Buckinghamshire NHS Trust | 45 |
| Norfolk and Norwich NHS Trust | 144 |
| North Durham Healthcare NHS Trust | 61 |
| Greenwich Healthcare NHS Trust | 84 |
| Calderdale Healthcare NHS Trust | 65 |
| South Manchester University Hospitals NHS Trust | 66 |
| South Tees Acute Hospitals NHS Trust | 96 |
| Wellhouse NHS Trust | 54 |
| Worcester Royal Infirmary NHS Trust | 85 |
| Bromley Hospitals NHS Trust | 118 |
| Hereford Hospitals NHS Trust | 62 |
| South Durham Healthcare NHS Trust | 41 |
| Swindon and Marlborough NHS Trust | 105 |
| Total first wave | 1184 |
| Second wave | |
| Schemes prioritised: | |
| Central Manchester Healthcare NHS Trust and Manchester Children’s Hospital NHS Trust | 127 |
| Dudley Group of Hospitals NHS Trust | 62 |
| West Berkshire Priority Care NHS Trust | 25 |
| Newcastle upon Tyne Hospitals NHS Trust | 59 |
| Walsgrave Hospitals NHS Trust and Coventry Healthcare NHS Trust | 174 |
| West Middlesex University Hospitals NHS Trust | 31 |
| London review schemes: | |
| University College London Hospitals NHS Trust | 160 |
| King’s Healthcare NHS Trust | 64 |
| St George’s Hospitals NHS Trust | 40 |
| Royal Hospitals NHS Trust | 250 |
| Total second wave and London review | 992 |
| Total first and second wave schemes | 2176 |
Estimated capital cost excluding financing costs.
Capital expenditure since 1974
By the mid-1970s, the wave of capital investment that had inaugurated the hospital plan for the NHS was effectively at an end. The squeeze on capital was reflected across all government departments in which, between 1974 and 1998, total net annual capital expenditure fell from £28.8bn to £3.3bn in 1998 prices.6
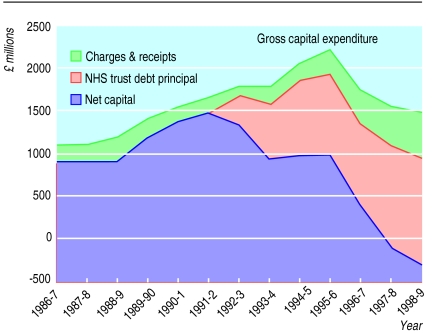
In the NHS in 1997-8 and 1998-9 there was negative capital investment on hospital and community health services (table 2). All capital investment is being met from funds internally generated from land sales and capital charges (figure).
Table 2.
Financing of hospital and community health services (HCHS) capital expenditure, 1986-7 to 1998-9
| Financial year | HCHS capital (£m) | Charges and receipts from land sales (£m) | Internally generated resources* (£m) | Net HCHS capital expenditure (£000) |
|---|---|---|---|---|
| 1986-7 | 1051 | 149 | 902 | |
| 1987-8 | 1106 | 201 | 905 | |
| 1988-9 | 1191 | 280 | 912 | |
| 1989-90 | 1423 | 232 | 1191 | |
| 1990-1 | 1551 | 178 | 1372 | |
| 1991-2 | 1639 | 169 | 1470 | |
| 1992-3 | 1785 | 113 | 363 | 1309 |
| 1993-4 | 1782 | 213 | 674 | 895 |
| 1994-5 | 2049 | 208 | 890 | 951 |
| 1995-6 | 1996 | 282 | 930 | 984 |
| 1996-7 | 1711 | 393 | 1000 | 318 |
| 1997-8 | 1514 | 446 | 1207 | −139 |
| 1998-9 | 1449 | 561 | 1236 | −348 |
Internally generated resources refers to “that element of trusts’ capital expenditure which they fund from their charges to health care purchasers.” Expenditure in excess of internally generated resoruces is funded through loans from the secretary of state for health (trust external financing). Only the latter constitutes additional government expenditure.
A recovery in capital spending was announced by the Treasury in the comprehensive spending review 1998: “With additional capital resources from land sales and receipts and investment through the PFI, the total capital investment will be nearly £8 billion over the three year period (1999-2002).”8However, the NHS capital expenditure plans show that total net capital investment over the next three years (1998-2002) will be less than £1.5 billion. The NHS capital budget will therefore continue to be made up of funds largely generated from within the NHS, namely land sales and elements of the capital charges.
Land sales and receipts
The 1970s economic crisis led to attempts to find sources of financing other than government borrowing. In 1973, regional health authorities were allowed for the first time to use proceeds from land sales for investment.9 Despite depressed prices in the late 1980s, land sales have become an increasingly important source of capital funding. In 1998-9, they accounted for over a third of NHS capital expenditure, masking the real decline in new funding for investment (table 2).
Capital charges
Since 1996-7, the bulk of NHS capital expenditure has been financed by resources generated internally by the hospital and community health service sectors (table 3). The NHS and Community Care Act 1990 fundamentally altered the financing of capital investment and paved the way for the private finance initiative through the capital charging system. Hospitals had been funded separately for revenue and capital expenditure; capital needs were met by capital grants. In a major break with the past, the 1990 act made capital financing the responsibility of the trusts, not the government.10It imposed new financial duties on NHS trusts, modelled on the relation between a private sector corporation and its bankers and shareholders. The duties require trusts to pay for the use of capital. In effect, hospitals are being taxed to provide capital.11
Table 3.
NHS sources of finance, 1993-4 to 2000
| Year | Total NHS expenditure (£m) | Public* (%) | Charges (%) | Miscellaneous† (%) | Capital refunds‡ |
|---|---|---|---|---|---|
| 1993-4 | 31 275 | 94.7 | 3.1 | 1.1 | 1.2 |
| 1994-5 | 33 266 | 94.5 | 2.4 | 1.0 | 2.2 |
| 1995-6 | 34 878 | 94.3 | 2.3 | 1.0 | 2.5 |
| 1996-7 | 36 330 | 93.7 | 2.1 | 1.2 | 3.0 |
| 1997-8 | 38 110 | 94.2 | 2.1 | 1.0 | 2.7 |
| 1998-9 | 41 369 | 88.3 | 2.1 | 1.7 | 7.9 |
| 1999-2000 | 43 068 | 91.9 | 2.1 | 4.0 | 2.0 |
| 2000-1 | 45 680 | 91.9 | 2.1 | NA | NA |
NA=not available.
General taxation and national insurance contributions.
Mostly health authority land sales.
Defined as “repayments of principal on trusts’ interest bearing debt.” They are voted as appropriations in aid by parliament. As refunds are ultimately funded through taxation, they do not constitute an additional source of public expenditure.
The capital charging regime obliges trusts to make an annual surplus of income over expenditure equal to 6% of the value of their assets and to make a charge for depreciation. Previously, depreciation, interest, dividend, and debt repayment did not feature in hospital accounts because these were not charged, and no revenue was allocated to finance the cost of capital. The new charges required hospitals for the first time to set aside a proportion of annual income to pay for capital.
Under the capital charging system, all hospital capital, including buildings and equipment inherited from earlier periods, is defined as a liability with government as creditor and sole shareholder. The liability corresponds to the value of the assets and is calculated on the basis of replacement cost, which is considerably higher than the original cost. New investment is funded through loans issued by the secretary of state for health and serves to increase the liability. The 6% charge is paid to the government on the value of the assets, both old and new, used in healthcare delivery.
Capital charges are recovered by trusts in the prices charged to NHS purchasers for the provision of services, and thus ultimately out of the revenue budget for hospital and community health services. The hospital and community health services revenue budget is adjusted so that the amount paid by trusts in capital charges is matched by allocations to NHS purchasers. But at the local level there is no direct relation between charges paid out and purchasers’ contributions. Some trusts are therefore disadvantaged under the charging system, and this has been a factor in trust deficits.
The capital charging system has allowed the government to substitute the circulation of debt for the issue of new capital in the public sector. The impact on the finances of the NHS of this circulation of debt, and any receipts on land and property sales, can be seen in table 3: capital refunds represent a return to government from revenue. In 1998-9, capital refunds from internally generated resources accounted for 7% of the entire NHS budget.
Capital refunds, like land sales, disguise the extent to which funding for capital investment has been withdrawn. The NHS must generate efficiency savings to fund new investment.
Implications of government’s capital investment plans
PFI—the only game in town
In the absence of new capital, NHS trusts have no other recourse but to pursue the private finance initiative to finance new investments. The introduction of capital charges provides a funding stream within the revenue budget to pay for private sector finance.
Local affordability rather than national priority
The capital charging system forces regions and trusts to consider the affordability of new capital investments. Where affordability was formerly a matter ofallocating to the regions the capital voted by parliament each year it is now about how much of their annual revenue trusts can afford to spend on capital.
Local affordability versus population needs
Under the capital charging regime, a trust must consider the effect of new investment on its annual costs. Any change in the value of assets will affect revenue. This can be shown by comparing hospital building plans before and after 1990. The Norfolk and Norwich regional plan originally proposed a second district general hospital of 900 beds to provide a total of 1600 beds in the area. After the introduction of capital charges the plan was revised to a single site scheme providing a total of 1000 beds. Similarly, at Hereford the outline business case formally approved by the NHS Executive in January 1995 was predicated on a requirement of 351 beds plus 47 maternity beds, but all four options were found to be unaffordable to the trust because the construction would impose unaffordable capital charge equivalents.
PFI—the higher cost option
In principle, investment through the private finance initiative has the same effect as capital charging. The only formal difference between the private finance initiative and public procurement is that under the former, annual payments for capital are made to the private sector and not to the Treasury. However, there is a crucial practical difference between the two types of procurement. The private finance initiative has proved to be more expensive than traditional public procurement, with the result that trusts have found that charges paid to the private sector will finance a considerably smaller facility than would have been the case had they been paid to the Treasury.
There are two reasons for the higher costs. Firstly, asset bases have increased in cost and in many cases almost doubled, compared with the current value of the estate they were intended to replace.12As a result, annual payments under the private finance initiative absorb a higher proportion of trusts’ incomes than current capital charges. Secondly, the payments, equivalent to the rental charge, to the private sector are higher than those made to government under capital charging. Payments to the private sector (the unitary payment) consist of an availability fee and a service fee. The availability fee covers construction costs, rolled up interest, and life cycle maintenance and is equivalent to the rental charge; the service fee covers facilities management services such as cleaning, lighting, and laundry. In the first wave of private finance initiative schemes, the rental payments/availability fees ranged from 11.2% to 18.5% of construction costs, compared with the 6% charge made by the Treasury (table 4).12 As a result, the proportion of trusts’ incomes spent on charges for capital will more than double in hospitals funded by the private finance initiative. The private finance initiative is associated with higher rates of return on more expensive asset bases, and trusts have been unable to replace like with like for the same annual cost (table 4).
Table 4.
Capital costs and annual payments of private finance initiative (PFI) hospitals
| NHS trust | Annual income 1996-7 (£m) | Current asset base 1996-7 (£m) | PFI construction costs (£m) | 1996-7 annual capital costs* (£m) | PFI availability payment (£m) | Availability fee as % of income | Availability fee as % of construction costs |
|---|---|---|---|---|---|---|---|
| Calderdale | 72.7 | 35.2 | 64.6 | 4.7 | 9.0 | 12.4 | 13.5 |
| Carlisle Hospitals | 46.3 | 19.6 | 64.7 | 2.7 | 8.0 | 17.3 | 12.4 |
| Greenwich | 95.2 | 55.0 | 84.0 | 8.7 | 11.0 | 11.5 | 13.1 |
| Norfolk and Norwich | 122.1 | 19.0 | 143.5 | 12.7 | 15.6 | 12.8 | 15.5 |
| North Durham | 59.0 | 24.9 | 61.0 | 3.6 | 7.1 | 12.0 | 11.6 |
| Wellhouse | 83.6 | 105.0 | 54.0 | 5.2 | 10.0 | 12.0 | 18.5 |
Interest, dividends, depreciation, rental.
Most private finance initiative schemes involve centralising hospitals on a single, usually cheaper, site and releasing land for sale. However, even with land sales and subsidies, the requirements of the private sector meant that the costs of each new hospital built under the private finance initiative exceeded the prevailing capital charges. As a result, the trusts had to radically revise their plans (downwards).
Bridging the affordability gap
The scale of new investment is constrained by hospitals’ ability to generate resources to pay for the new asset. The higher costs have created an affordability gap—the gap between what the trust and purchasers can afford and the private sector charges. There are, potentially, four sources a trust can tap to pay the private sector:
The revenue used by trusts to pay for capital charges
The proceeds of selling assets
Cost savings in service delivery
Income generation (retailing, private patients, etc).13
These sources have proved insufficient and the government has stepped in to ease affordability problems by providing external subsidy from the Treasury (the “smoothing mechanism”), by redirecting capital intended for NHS trusts remaining in public ownership,14 and by allowing private finance initiative trusts to retain without charge the proceeds of sales of their assets. However, increased costs arising from the private finance initiative have also required a diversion of hospital budgets from staffing to capital payments and have led to major downward revisions in the planned capacity of hospitals.
Implications for equity
None of these measures represent an equitable system of resource allocation. Furthermore, the private finance initiative creates new inequities. Since trusts operating under the private finance initiative divert their capital charge payments from the public to the private sector, but continue, as they must, to charge purchasers for capital, the capital charge payment—one source of NHS funding—“leaks” out of the system. Moreover, when trusts dispose of assets to fund the new hospital they still remain liable for 6% capital charges on these “deferred” assets. In at least one case, Wellhouse, the charge has been waived.
As yet, little thought has been given to the financial implications of this for the NHS as a whole. Unless the government makes good the leakage of capital charges, trusts operating under the private finance initiative will draw funding from the system at the expense of providers remaining in public ownership. The capital charges system will continue to require the remaining NHS trusts to fund new investment in the private sector. From financing to resourcing, the playing field is tilted in favour of the private sector.
Conclusion
Postwar levels of capital investment have been insufficient to fund a national programme of hospital renewal or to maintain the ageing NHS estate. Funding declined substantially in the 1990s and in 1998-9 the government provided no new net capital. Since 1990, a growing proportion of capital investment has been generated out of trusts’ own revenue budgets. In the absence of new capital, trusts have no choice but to opt for the private finance initiative if they want to invest in their facilities and remain “competitive.” The private finance initiative is an expensive financial option and has brought with it severe affordability problems at both local and national level. The government has stepped in by providing external subsidies and diverting NHS resources intended for other services and other areas to pay for it. But these measures are insufficient and do not prevent major cuts in service. Under the private finance initiative the NHS pays more for less; paradoxically, the “largest hospital building programme in the history of the NHS” is being funded by the largest acute hospital closure programme.
Supplementary Material
Figure.
Financing of hospital and community health services capital expenditure, 1986-7 to 1998-97
Acknowledgments
We thank Dr John Mohan for comments on the historical section.
Footnotes
Competing interests: None declared.
References
- 1.Webster C. The health services since the war. Vol. 2. London: HMSO; 1990. pp. 261–262. [Google Scholar]
- 2.Webster C. The National Health Service, a political history. Oxford: Oxford University Press; 1998. Creation and consolidation; pp. 1–41. [Google Scholar]
- 3.Written answers. House of Commons official report (Hansard) 1997 July 16;298:col 534. (No 43.) (Document deposited in House of Commons library in response to parliamentary question 6555.)
- 4.House of Commons. NHS (England) summarised accounts 1996-97. London: Stationery Office, 1998.
- 5.Department of Health. Press release 98/318, 31 July 1998.
- 6.HM Treasury. Financial statement and budget report 1999-2000. London: Stationery Office; 1999. (Table B28: Historical series of government expenditure.) [Google Scholar]
- 7.Pollock AM, Gaffney D. The private cost of public health. Health Review 1998 Winter:20-1.
- 8.House of Commons Health Select Committee. Public expenditure, 1999. Minutes of evidence 1998 July 22:19.
- 9.Meara R. Unfreezing the assets: NHS estate management in the 1980s. London: King’s Fund; 1991. p. 6. . (King’s Fund Institute research report 11.) [Google Scholar]
- 10.Shaoul J. Charging for capital in the NHS trusts: to improve efficiency? Management Accounting Research. 1998;9:95–112. [Google Scholar]
- 11.Pollock AM, Gaffney DG. Capital charges: a tax on the NHS. BMJ. 1998;317:157–158. doi: 10.1136/bmj.317.7152.157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gaffney D, Pollock AM. Pump-priming the PFI: why are privately financed hospital schemes being subsidized? Public Money and Management, 1999 January-March:55-62.
- 13.Gaffney D, Pollock AM. Can the NHS afford the private finance initiative? London: BMA; 1997. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.