The patients
Case 1
Ms H, a 21 year old woman, consulted with a one day history of sore throat. She did not complain of cough or of any other associated respiratory symptom. On examination she was feverish (38°C), with exudate on her tonsils and tender cervical lymph nodes. A textbook of diagnostic strategies suggests that this collection of symptoms and signs increases the likelihood of her having group A β haemolytic streptococcus infection to over 40%.1 She was treated with a seven day course of penicillin, and a throat swab was taken to confirm infection with group A β haemolytic streptococcus. Four days later the swab result confirmed the presence of group A β haemolytic streptococcus which was sensitive to penicillin. Nine days after the initial consultation Ms H returned complaining of continuing symptoms of sore throat and requesting further antibiotics. She still had inflamed tonsils but with no exudate; her cervical lymphadenopathy had persisted. In view of her positive throat swab she was given a further course of penicillin. Serology for infectious mononucleosis was negative. A subsequent consultation confirmed that her sore throat had settled two days after the second consultation.
Case 2
Ms D, a 17 year old woman, consulted with a two day history of sore throat and blocked nose. Examination revealed an inflamed pharynx with some exudate, but the patient was otherwise well. She had been treated with two consecutive courses of antibiotics for a similar illness in 1997. She was keen to have antibiotics again. After some negotiation a compromise was reached: antibiotics were not prescribed, but a throat swab was taken. A week later the swab result confirmed group A haemolytic streptococcus (non-β) reported as sensitive to penicillin, and a letter with a prescription was sent to Ms D after contact by telephone failed. One week after this the patient complained to the practice manager that she still had a sore throat. Her sister had been seen the day before (by a different doctor) with the same symptoms and was prescribed antibiotics immediately. An appointment to see the doctor concerned to discuss the complaint was made, but the patient failed to attend.
The clinical question
We were unsettled by these two cases and wished to be clear about a rational and evidence based approach to sore throat, a common condition in general practice. The two cases presented two clinical problems. Firstly, does the use of a throat swab improve diagnostic accuracy? Secondly, do antibiotics improve symptoms and reduce complications?
Search strategy
We adopted a pragmatic approach when looking for evidence concerning diagnosis and treatment. We initially looked, therefore, for systematic reviews of primary studies. We found a recently updated systematic review on sore throat in the Cochrane Library2 and a review on the topic in the Drug and Therapeutics Bulletin.3 We also knew of a recently published randomised controlled trial.4,5 Other references cited in this report are taken from the citations in these studies.
Is a throat swab a good diagnostic test?
The throat swab is currently recommended as a diagnostic aid in patients with sore throat.3 The quoted sensitivity (26-30%) and specificity (73-80%), however, are low when compared with the “gold standard” of a rise in antistreptolysin O titre.6 The antistreptolysin O titre is probably the best predictor for the presence of group A β haemolytic streptococcus, the most common bacterial pathogen causing sore throat, as the association with definite cases of rheumatic fever and high initial level of antistreptolysin O titre or rise in antistreptolysin O titre is 100%.7 The low predictive value of throat swabs is probably due to a high symptomless carriage rate of group A β haemolytic streptococcus (ranging from 6% to 40%).7 Although antistreptolysin O titre may be a better gold standard, it is not suitable for routine use because of delay, cost, and the inconvenience of serial titres. As the first case illustrates, if the throat culture is positive it is difficult not to prescribe further antibiotics.
What are the benefits and risks of prescribing antibiotics?
The rationale behind treating people with sore throat with antibiotics is to reduce symptoms and the likelihood of developing suppurative and non-suppurative complications.
Symptom relief
The Cochrane review reports that 90% of all (treated and untreated) patients are well one week after the onset of symptoms.2 Those treated with antibiotics for sore throat, headache, and fever have reduced symptoms on day three. The maximum benefit is at three and a half days, when the symptoms of half the treated patients have already settled.
Suppurative complications
Quinsy is rare in general practice.8 Most randomised controlled trials exclude patients at high risk of suppurative complications. Despite these exclusions, the Cochrane review shows that the rate of complication with quinsy is significantly reduced with antibiotics.2 However, this finding is based on a single trial reported in 1951 that contributed 15 of the 19 patients with quinsy in the untreated group.
Non-suppurative complications
Rheumatic fever is similarly rare in general practice. In trials from the 1950s, however, treatment of exudative tonsillitis with penicillin did reduce the incidence of subsequent rheumatic fever.2 Moreover, patients who have developed complications (either suppurative or non-suppurative) may not have had a preceding sore throat, and of those with prior symptoms, only a minority will seek medical help.7,8
Disadvantages of prescribing antibiotics
The risks of prescribing antibiotics have been well described. These include the common side effects of antibiotics (diarrhoea, rashes, candidiasis, unplanned pregnancy secondary to oral contraceptive failure) and the rare occurrence of anaphylaxis. Another consequence is to “medicalise” the condition of sore throat, resulting in increasing reattendance for future episodes of this condition.5 Furthermore, there is evidence that by treating patients positive for group A β haemolytic streptococcus, the modest benefits of treatment at the beginning of the episode of illness may be negated because of increased likelihood of such an infection recurring.9 When the direct costs of prescribing and the impact on bacterial resistance are also considered, the use of antibiotics is clearly not a risk free strategy.
The informed decision
Using a throat swab as a diagnostic test in primary care may medicalise the condition and encourage prescribing.6 Guidelines from the United States and the United Kingdom recommend prescribing antibiotics in patients in whom group A β haemolytic streptococcus has been identified.10,11 We believe that this advice ignores the fact that no satisfactory diagnostic test can identify these patients.
Very ill patients have, because of exclusion on clinical grounds, been poorly represented in randomised controlled trials.2,4 These patients may be the individuals most likely to benefit from antibiotics. For the vast majority of patients with a sore throat, however, the trade-off between risks and benefits from antibiotics is, at best, marginal.
These diagnostic and therapeutic dilemmas ignore the patient’s perspective. In the United Kingdom, most patients consult for reassurance and information; only a minority expect to receive antibiotics. Doctors often prescribe antibiotics to maintain good relationships with their patients. What patients require is consistent information that addresses their concerns and beliefs.12,13 Our cases illustrate that the priority in consultations should be to elicit patients’ concerns and provide sufficient information for a joint management decision to be reached.
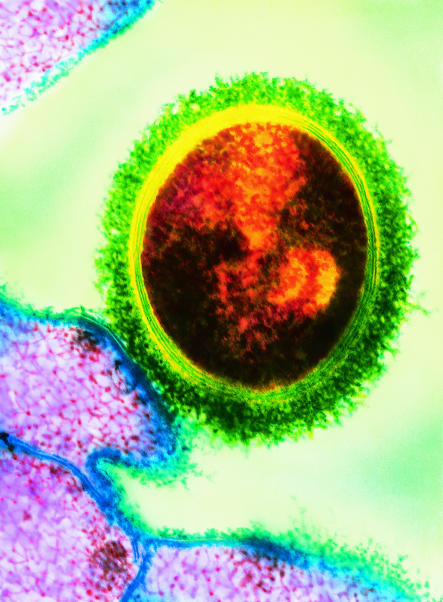
Figure.
DR IMMO RANTALA/SCIENCE PHOTO LIBRARY
Group A β haemolytic streptococcus bacteria are the most common cause of sore throat. But is the use of throat swabs and antibiotics always appropriate?
Acknowledgments
We thank Chris Salisbury, Debbie Sharp, Paul Little, Andy Ness, and Rob Heyderman for helpful comments on this case report.
Footnotes
Funding: AG is funded by the South and West regional office of NHS Executive on a research studentship.
Competing interests: None declared.
References
- 1.Komaroff A. Sore throat in adult patients. In: Panzer R, Black E, Griner P, editors. Diagnostic strategies for common medical problems. Philadelphia: American College of Physicians; 1991. pp. 186–195. [Google Scholar]
- 2.Del Mar C, Glasziou P Cochrane Collaboration, editors. Cochrane Library. Issue 3. Oxford: Update Software; 1998. Antibiotics for the symptoms and complications of sore throat. [Google Scholar]
- 3.Diagnosis and treatment of streptococcal sore throat. Drugs Ther Bull. 1995;33:9–12. doi: 10.1136/dtb.1995.3329. [DOI] [PubMed] [Google Scholar]
- 4.Little P, Williamson I, Warner G, Gould G, Gantley M, Kinmonth AL. Open randomised trial of prescribing strategies in managing sore throat. BMJ. 1997;314:722–727. doi: 10.1136/bmj.314.7082.722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Little P, Gould C, Williamson I, Warner G, Gantley M, Kinmonth AL. Reattendance and complications in a randomised trial of prescribing strategies for sore throat: the medicalising effect of prescribing antibiotics. BMJ. 1997;315:350–352. doi: 10.1136/bmj.315.7104.350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Del Mar C. Managing sore throat: a literature review. I. Making the diagnosis. Med J Aust. 1992;156:572–575. [PubMed] [Google Scholar]
- 7.Valkenburg H, Haverkorn M, Goslings W, Lorrier J, de Moor C, Maxted W. Streptococcal pharyngitis in the general population. II. The attack rate of rheumatic fever and acute glomerulonephritis in patients not treated with penicillin. J Infect Dis. 1971;124:348–358. doi: 10.1093/infdis/124.4.348. [DOI] [PubMed] [Google Scholar]
- 8.Little P, Williamson I. Sore throat management in general practice. Fam Pract. 1996;13:317–321. doi: 10.1093/fampra/13.3.317. [DOI] [PubMed] [Google Scholar]
- 9.Pichichero M, Disney F, Talpey W, Green JL, Francis AB, Roghmann KJ, et al. Adverse and beneficial effects of immediate treatment of group A beta-hemolytic streptococcal pharyngitis with penicillin. Pediatr Infect Dis J. 1987;6:635–643. doi: 10.1097/00006454-198707000-00004. [DOI] [PubMed] [Google Scholar]
- 10.Standing Medical Advisory Committee. The path of least resistance. London: Stationery Office; 1998. [Google Scholar]
- 11.Bisno A, Gerber M, Gwaltney J, Kaplan E, Schwartz R. Diagnosis and management of group A streptococcal pharyngitis: a practice guideline. Clin Infect Dis. 1997;25:574–583. doi: 10.1086/513768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kai J. Parents’ difficulties and information needs in coping with acute illness in preschool children: a qualitative study. BMJ. 1996;313:987–990. doi: 10.1136/bmj.313.7063.987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Butler CC, Rollnick S, Pill R, Maggs-Rapport F, Stott N. Understanding the culture of prescribing: a qualitative study of general practitioners’ and patients’ perceptions of antibiotics for sore throats. BMJ. 1998;317:637–642. doi: 10.1136/bmj.317.7159.637. [DOI] [PMC free article] [PubMed] [Google Scholar]