A 15 year old girl in the north of England is recovering this week after a heart transplant operation sanctioned by a High Court judge despite her refusal to undergo it.
The teenager, identified as M, had only a week to live, and her parents had consented to the operation. But M, who had been fit and healthy until she developed heart failure in May, had learnt only two days earlier that a transplant was her only chance of survival and insisted she did not want to have it.
The transplant team at Freeman hospital in Newcastle upon Tyne could not begin to look for a heart until they knew the operation could go ahead. The High Court family division judge on duty was contacted and he insisted that the girl must first be given the chance to make representations to him. He located a local solicitor who specialises in children’s cases, who agreed to go to the hospital and talk to M. She told him that she was “depressed” at the prospect of taking treatment for life, and worried that she would be “different” with someone else’s heart. Her words were relayed to the official solicitor, who took the view that she was overwhelmed by the discovery that she had a fatal illness and lacked the capacity to weigh up all the considerations and make an informed decision. The judge accepted his recommendation that the surgeons be allowed to treat her in accordance with their clinical judgment.
The case highlights the illogical state of the law on under 18s and consent. Under the Family Law Reform Act, children of 16 and over can give a valid consent to medical treatment, and the case brought some years ago by Victoria Gillick questioning provision of contraception for under 16s without parental consent confirmed that they have the same right if they have the maturity to weigh up all the factors. But in a later case, in 1991, the appeal court held that the court can override the refusal of a minor.
Dr Vivienne Nathanson, head of health policy and research at the BMA, said: “Doctors find these situations very difficult because all their instincts are to provide life saving treatment, but equally, they are very reluctant to override the wishes of an unwilling patient who may not recover as well if treatment has been imposed.” She added: “The legal and ethical position on young people and consent is complicated and confused. We are currently working on new guidance on informed consent which we hope will help clarify the decision making process.”
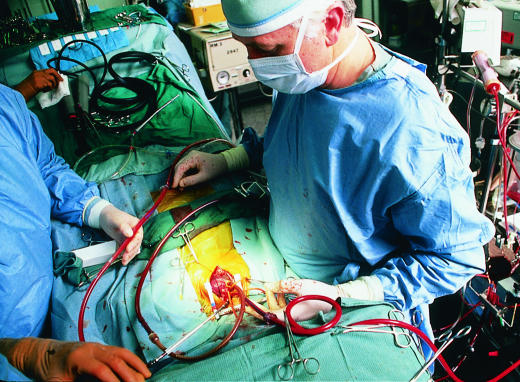
Figure.
ALEXANDER TSIARAS/SPL
Heart transplantation doctors were advised to act on their clinical judgment and overrule lack of consent in a teenager