Abstract
INTRODUCTION
Multiple composite indices of small area socioeconomic characteristics have been used to examine how neighborhood characteristics influence cancer care, but there is little consensus regarding how to employ them. The objective of this scoping review is to summarize the use of these indices in cancer literature and their association with outcomes.
METHODS
A search was conducted to identify studies from 2015 to 2021 that investigated cancer incidence, stage at diagnosis, and mortality that used area-based indices of deprivation as an independent variable. Studies were screened and assessed for eligibility. Data were extracted regarding the geospatial and statistical use of these indices.
RESULTS
Forty-five studies met all inclusion criteria. Nineteen (42.3%) had an area level of analysis at the census tract level, 15 (33.3%) county level, six (13.3%) block group level, and five (11.1%) ZIP code level. Eighteen unique indices were utilized in total, with four indices used most frequently. Of the studies that used their indices ordinally, three studies defined high and low deprivation dichotomously, 10 utilized tertiles, 13 quartiles, and 15 quintiles. Thirty-four (76.0%) studies showed a significant association between area deprivation and cancer-related outcomes.
CONCLUSIONS
Neighborhood deprivation indices are most commonly used at the census tract level and ordinally as quintiles. Despite variance in methodology, there is a strong indication that deprived areas are at adverse odds of cancer related outcomes. Further work investigating deprivation in the context of cancer can inform drivers of inequity and identify potential targets for care delivery and policy interventions.
Introduction
Inequity in cancer care has been well established by patient socioeconomic status, insurance coverage, race, and geography.1,2,3,4 Increasingly, studies have looked to incorporate area measures of socioeconomic factors that capture the overall resources in which patients and providers may reside. Rather than looking at single measures as an estimate of local area socioeconomic factors (i.e., median income at zip-code level), composite indices are one of these tools used to more broadly capture multiple factors into a single measure.
There is limited consensus regarding how to employ neighborhood-level indices.1 What remains unclear is which geographic levels are utilized most frequently, which measures are commonly used, and which cancer outcomes are evaluated. Some studies geocode patient cohorts to the county as the geographic level of analysis to establish neighborhood socioeconomic status (SES), whereas others utilize census tracts - subdivisions of a county with an average capita of 4,000 ideally homogenous residents. Research has also analyzed neighborhood SES by census block group, which are subdivisions of census tract’s covering a contiguous area of roughly 1,500 residents, also ideally socioeconomically homogenous.5 Variability also exists in the methodology used to construct the indices, particularly in choice of neighborhood characteristics used to define deprivation and statistical analysis of those characteristics.2–4,6–12 The variability in methods challenges interpretation of results and cross-comparison between studies using different indices. ‘Poverty’ within one index may be defined as a measure of percentage of persons below the federal poverty level, whereas a different index may use percentage of persons below 200% the poverty level.
The objective of this study is to summarize 1) which neighborhood level methods and indices are most used and the criteria used to characterize each method, 2) determine commonly used geographic area-level of analysis, and 3) characterize how literature is quantitatively defining deprivation or neighborhood SES. We hope to provide researchers with a resource to reference during their own study design, and to encourage further review of neighborhood deprivation as a tool to incorporate social determinants of health on disease presentation, intervention, and outcome.
Methods
The authors followed criteria for conducting a scoping review.13 A scoping review is a literature review method used to synthesize existing literature within a field to clarify working definitions and conceptual boundaries.14 Scoping reviews may be of particular use when a field of literature has not been thoroughly reviewed or, there exists heterogeneity in a research method’s application.15 Relevant studies were identified that investigated incidence, stage at diagnosis, and mortality for various cancers that used multivariable, area-based level indices of deprivation or neighborhood SES as an independent variable.
Searching
A search was conducted in PubMed and was limited from January 1, 2015 to June 1, 2021. The search utilized a query including keywords “socioeconomic deprivation,” “socioeconomic status,” “social deprivation,” “social vulnerability,” “small area deprivation,” “area deprivation,” or “neighborhood deprivation” - combined with “measurement,” “measure,” “index,” or “deprivation index” - combined with “cancer” – combined with “incidence,” “stage,” or “mortality.”
Inclusion and Exclusion Criteria
Studies were included in the study if they (1) were published in English language, (2) studied a population exclusively in the United States, (3) indexed multiple measures of SES defined at the area level, (4) had a small area level of analysis conducted at either the county, ZIP code, census tract, or block group level, and (5) had at least one study objective investigating cancer incidence, stage at diagnosis, or mortality. Studies were excluded if they were published in a language other than English, were a systematic review, scoping review, or clinical trial, or if the full text was not available even when full effort was made to obtain it.
Authors conducted an initial review of the identified studies from PubMed screening for inclusion and exclusion criteria. Following this review, the full text of the remaining potential studies were reviewed by authors and studies that did not meet the inclusion criteria were excluded.
Extracting and Charting the Results
After reviewing all included articles, details about each study’s use of its area level deprivation measurement were recorded. The authors recorded every cancer-related outcome investigated in each study (e.g., incidence, stage at diagnosis, and/or mortality) and the geographic area of the study’s population (e.g., nationwide, multi-state, single state, metropolitan area). Data regarding the specific use of the deprivation or neighborhood SES index were extracted including the small area level of analysis (e.g. county, ZIP code, census tract, block group), whether the index used was custom developed for the study or a priori based on a validated index, whether the study analyzed the index score as a continuous score or ordinal variable, and if ordinal, how the study employed an ordinal rank (e.g. tertiles, quartiles, quintiles). The authors also recorded whether there was a statistically significant correlation between the study outcome and the index used.
Additionally, authors extracted data regarding the citing whitepaper, the socioeconomic dimensions included in the index, and the individual measures used to construct the index. If a specific index was used three or more times, it was noted as “most commonly used.”
Results
The PubMed query produced 897 studies. After title and abstract review, 172 studies were selected for full-text review, of which 45 met all inclusion and exclusion criteria (Supplementary Appendix A). The primary reason for exclusion (n=463) was the study of a non-United States patient population. Two hundred thirty-nine papers were excluded because they did not investigate an outcome specific to cancer incidence, stage at diagnosis, or mortality, 97 did not utilize a multi-variable area-level index of deprivation, 40 were systematic or scoping reviews, and 13 were duplicates. (Figure 1)
Figure 1.
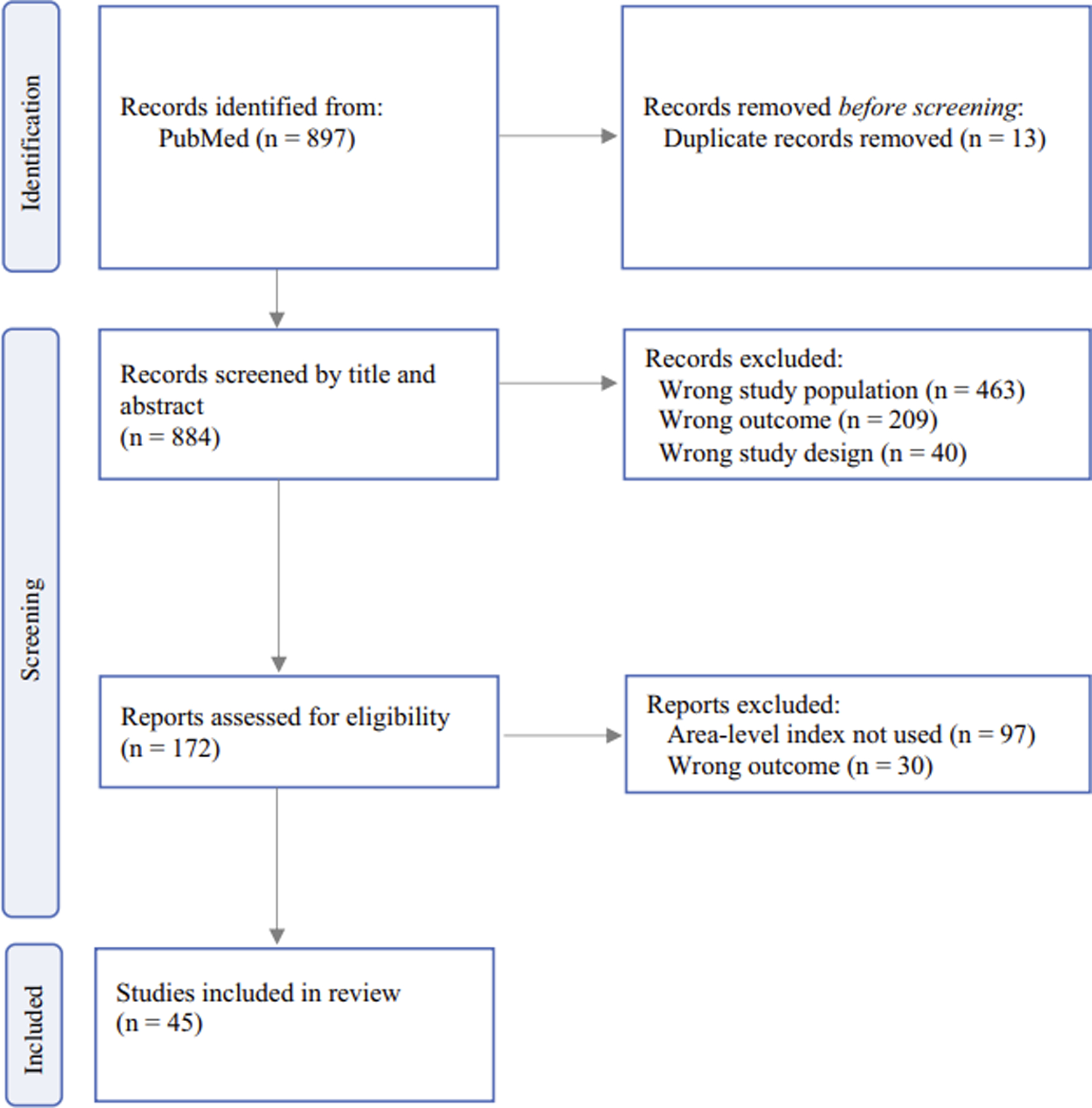
PRISMA 2020 flow diagram for included studies
Within the 45 included studies, there were 17 (33.3%) primary outcomes investigating cancer incidence, 12 (23.5%) investigating stage at diagnosis, and 22 (43.2%) investigating mortality (Table 1). Several observed more than one of the outcomes of interest, bringing the total of outcomes above 45. Ten studies (22.2%) used a nationwide cohort, 18 (40.0%) multi-state, 12 (26.7%) single state, and five (11.1%) metropolitan area. The area level of deprivation was at the county level in 19 (42.3%), ZIP code in five (11.1%), census tract in 19 (42.3%), and block group in six (13.3%). Of the indices used by the study authors, 39 (86.7%) were a priori methodologies cited by the authors, and six (13.3%) were custom developed. Thirty-six (80.0%) employed the indices as ordinal variables, six (13.3%) were used continuously, and three (6.7%) studies used indices as both ordinal and continuous (Table 1). Of the studies that used their indices ordinally, three studies defined high and low deprivation dichotomously, 10 utilized tertiles, 13 quartiles, and 14 quintiles. Nine studies utilized their indices as a continuous variable (Figure 2).
Table 1.
Characteristics of 45 studies using deprivation indices
| Characteristic | n (%) |
|---|---|
| Cancer related outcomesa | |
| Mortality | 22 (43.2) |
| Incidence | 17 (33.3) |
| Stage at Diagnosis | 12 (23.5) |
| Study area population | |
| Multi-state | 18 (40.0) |
| Single state | 12 (26.7) |
| Nationwide | 10 (22.2) |
| Multi-county metropolitan area | 5 (11.1) |
| Deprivation index area of analysis | |
| Census tract | 19 (42.3) |
| County | 15 (33.3) |
| Census block group | 6 (13.3) |
| ZIP Code | 5 (11.1) |
| Deprivation index methodology used by authors | |
| Previously validated in other studies | 39 (86.7) |
| Custom | 6 (13.3) |
| Statistical application of indices | |
| Ordinal | 36 (80.0) |
| Continuous | 6 (13.3) |
| Ordinal and continuous | 3 (6.7) |
Sum adds to more than 45 studies as several studies measured more than one outcome
Figure 2.
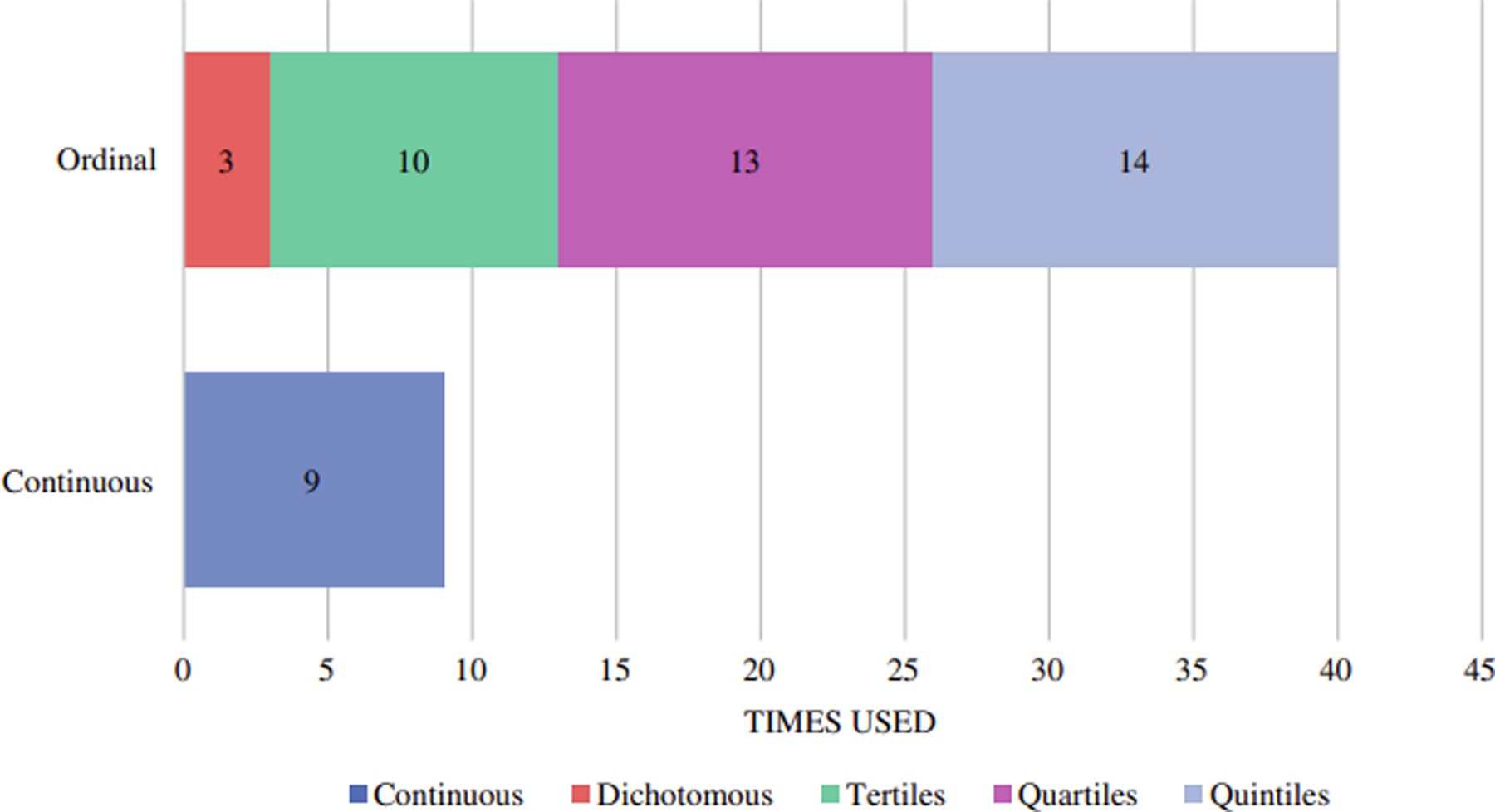
Statistical application of indices in all studies
Of the 18 unique indices across all studies, several stood out as the most utilized (Table 2). The National Cancer Institute (NCI) SES Index was most frequently used in nine of the studies. It is a census tract-based SES index using United States Census Bureau’s American Community Survey (ACS) measures and adopted by the National Cancer Institute (NCI) Surveillance, Epidemiology, and End Results (SEER) as a specialized database.4,12,16 Additionally, four studies modeled their own indices based on the criteria independent of the SEER database. The seven ACS measures included consist of percent working class, percent unemployed, percent of persons below 150% of the poverty level, median household income, education index (weighted school years), median house value, and median gross rent (Table 2).
Table 2.
American Community Survey variables utilized in commonly used indices
| Dimension | Variable | NCI SES Index | NDI | ADI | SVI |
|---|---|---|---|---|---|
| Poverty and Wealth | Median household income | ||||
| Per capita income | |||||
| Median house value | |||||
| Percent owner-occupied housing units (home ownership rate) | |||||
| Median monthly mortgage | |||||
| Median gross rent | |||||
| Percent of families below the poverty level | |||||
| Percent population below 150% poverty level | |||||
| Percent of households with public assistance income | |||||
| Income disparitya | |||||
| Education | Percent aged ≥ 25 years with < 9 years education | ||||
| Percent aged ≥ 25 years with < high school diploma | |||||
| Educational indexb | |||||
| Employment | Percent working class | ||||
| Percent unemployed | |||||
| Percent of males in management and professional occupations | |||||
| Percent of employed persons ≥16 years of age in white-collar occupations | |||||
| Housing Quality | Percent of households with more than one person per room (crowding) | ||||
| Percent of households without a motor vehicle | |||||
| Percent of households without a telephone | |||||
| Percent of occupied housing units without complete plumbing | |||||
| Percent of persons in group quarters | |||||
| Percent housing in structures with 10 or more units | |||||
| Percent mobile homes | |||||
| Housing Composition | Percent of single-parent households with children < 18 years of age | ||||
| Percent persons aged 65 and older | |||||
| Percent persons aged 17 and younger | |||||
| Percent non-institutionalized population with a disability | |||||
| Minority Status and Language | Percent minority (all persons except white, non - Hispanic) | ||||
| Percent persons (age 5+) who speak English “less than well” |
Log of 100 * the ratio of the number of households with <$10,000 in income to the number of households with $50,000 or more in income
Percent with less than high school graduate, high school only and more than high school as calculated: (Less than HS grad * 9) + (HS only *12) + (More than HS grad * 16)
The Neighborhood Deprivation Index (NDI) was used in seven studies.7 The NDI is validated at the census tract level, and uses eight ACS measures: percent of individuals below the federal poverty level, percent of households with public assistance income, percent aged ≥ 25 years with < high school diploma, percent unemployed, percent of males in management and professional occupations, percent of households with more than one person per room (crowding), and percent of single-parent households with children < 18 years of age (Table 2).
The Area Deprivation Index (ADI) was used in six studies.10 Based on 17 ACS measures, the ADI is validated at the block group level.6 Specific ACS measures include median household income, median house value, percent owner-occupied housing units (home ownership rate), median monthly mortgage, median gross rent, percent of families below the poverty level, percent population below 150% poverty level, income disparity, percent aged ≥ 25 years with < nine years education, percent aged ≥ 25 years with < high school diploma, percent unemployed, percent of employed persons ≥16 years of age in white-collar occupations, percent of households with more than one person per room (crowding), percent of households without a motor vehicle percent of households without a telephone, percent of occupied housing units without complete plumbing, and percent of single-parent households with children < 18 years of age (Table 2).
The Social Vulnerability Index (SVI), developed by the CDC, was used in three studies.11 Based on 15 ACS measures, the SVI is validated at both the census tract and county level. Specific measures include per capita income, percent of families below the poverty level, percent aged ≥ 25 years with < high school diploma, percent unemployed, percent of households with more than one person per room (crowding), percent of households without a motor vehicle, percent of persons in group quarters, percent housed in structures with 10 or more units, percent mobile homes, percent of single-parent households with children < 18 years of age, percent persons aged 65 and older, percent persons aged 17 and younger, percent non-institutionalized population with a disability, percent minority (all persons except white, non-Hispanic), and percent persons five years or older who speak English “less than well” (Table 2).
The usage of the NCI SES Index, NDI, ADI, and SVI and their distribution amongst cancer specific outcomes, study population, area level of analysis, and statistical significance is shown in Figure 3. Notably, studies using the NCI SES Index and NDI more often used census tracts as their level of analysis. Despite being validated at the block group and census tract level respectively, the ADI was most often used at the ZIP code level, and the SVI at the county level. The NCI SES Index was primarily used in the study of nationwide, multi-state, and single state populations. The ADI had equal distribution of use amongst nationwide, multi-state, and single state study populations. The NDI was used primarily to study nationwide and multi-state populations, and a large minority studied metropolitan areas. All studies using NCI SES Index, ADI, NDI, and SVI found a statistically significant correlation between their outcomes and their indices, except for two studies using ADI (Figure 3).
Figure 3.
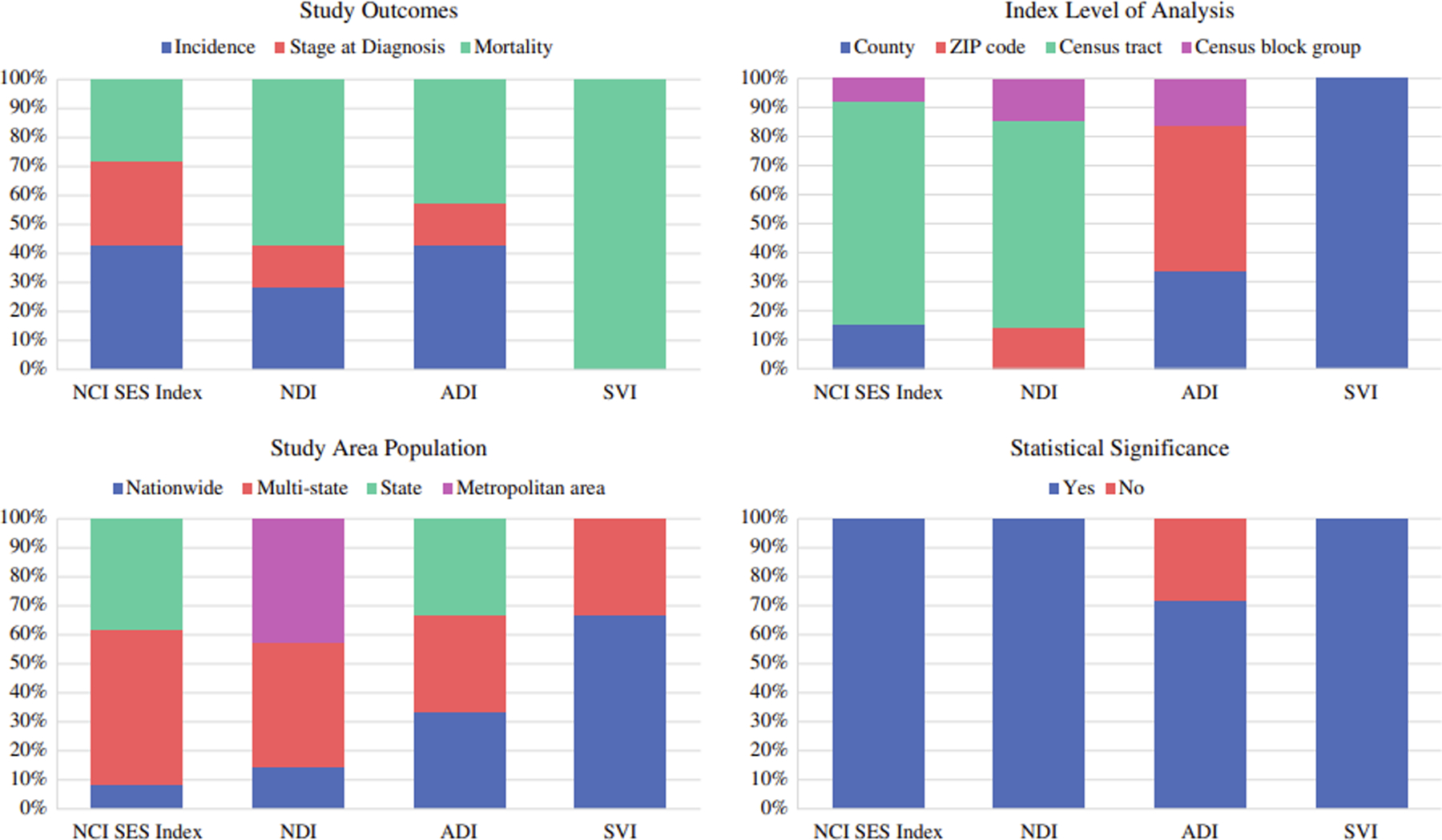
Distribution of study outcomes, population, levels of analysis, and significance among commonly used indices
Discussion
This review summarizes the recent state of American studies using neighborhood deprivation measures and their effects on cancer and related outcomes. Of the 45 studies on cancer care, most defined neighborhood deprivation using ACS measures of poverty and wealth, education, employment, housing quality, housing composition, and minority status and language. The most common geographic level of analysis was at the census tract level. Overall, we identified 18 unique composite indices measuring deprivation or neighborhood SES. The NCI SES Index, NDI, ADI, and SVI were among the most commonly employed indices, and their use varied greatly concerning the study populations and geographic level of analysis. Although each method differed slightly in construction and statistical application, a significant association between area-level socioeconomic status and outcomes was demonstrated in in 34 of 45 (76%) of studies.
Socioeconomic indices have demonstrated the ability to reflect a neighborhood’s multidimensional SES with robustness, validity, and explanatory power, more so than single measures of area-level characteristics. Indices can be useful in documenting the effect of neighborhood characteristics on disease presentation and outcome.6,7,17 However, the practical definition of a neighborhood varied between the county, ZIP code, census tract, and block group. There are nuanced use cases for differing geographic levels of analysis. Counties tend to remain socio-politically and geographically stable over time. In contrast, census tracts and block groups are subject to changes every centennial census.6,18 When used temporally, counties can provide appropriate social, political, and community context while mitigating the risk of encountering changing smaller geographic levels.6,19
Our review finds that defining neighborhoods by the census tract is in line with existing literature and there are reasons to support this approach. Census tracts are a small, relatively homogenous subdivision of a county, theoretically comprised of people with similar economic statuses and living conditions.3 They are small enough to offer a more precise definition of a neighborhood, but are just large enough to avoid unmasking individuals compared to data at the block group level.20 Census block groups, on the other hand, have been demonstrated to perform just as well at correlating neighborhood SES with cancer related outcomes, and provide a close approximation of SES characteristics measured at the level of the individual.2–4,21 The extent to which block groups provide meaningful information that larger geographic scales cannot may “differ for different area characteristics or across larger contexts (e.g. cities/metro areas).”3 If there are differences between populations at a smaller geographic scale, the use of block groups may be more appropriate.
Despite the collective use of census based geographic areas, our review found a noticeable number of studies defining neighborhoods at the ZIP code level. ZIP codes are used for the efficient delivery of mail, are more conceptual than geographic, and generally do not “respect political or census statistical boundaries.”2 ZIP code measures have been shown to deficiently detect cancer mortality and incidence gradients across neighborhood SES.2,4 Geocoding health data to the tract or block group level may offset the convenience of using potentially less accurate ZIP code data.4
Included studies did not discuss rationale for their use of geographic area. However, most studies are confined to the geographic areas provided by specific datasets. SEER was the most used dataset, and it only provides data at the zip-code or census tract level. Other administrative data like HCUP National Inpatient Sample can only provide ZIP-code data, and state cancer registries may provide more granular data, some down to the level of block group. The use of smaller areas of analysis can lead to statistical challenges such as Modifiable Areal Unit Problem and use of larger areas can lead to overlook significant sociodemographic variation., with dozens of block groups within a given county, for instance.6,22 It may be advisable for more cancer databases to provide such geographic data for further flexibility among researchers to choose area levels based on study frameworks while also maintaining protection of patient confidentiality.
Our review demonstrates that there is variation in how indices are evaluated quantitatively. The finding that indices are most commonly defined ordinally as quintile groupings is in line with statistical theory. Studies suggest that neighborhood SES should not be considered a linear scale. A national sample of 5% of all Medicare beneficiaries found that that the most deprived neighborhoods made up the top 15% of the distribution.23 Suggesting that deprivation is associated with a “threshold effect,” similar in theory to what is considered a “dose response” relation such that there is some point at which residents can no longer compensate, and “additional disadvantage leads to increasingly adverse outcomes.”7,23 Quintile grouping appears to be a safe and reliable way to distribute a study cohort and draw meaningful conclusions while avoiding a “dose response.” However, tertiles may be more appropriate to use when sample size is limited; researchers should consider such nuances during study design phase.16,18
Our study revealed that 18 unique neighborhood SES indices were used in just 45 studies, each comprising different neighborhood measures and statistical modeling. This variation defines the primary challenges of neighborhood and cancer studies today, inconsistency. Among the four most commonly used indices – NCI SES Index, NDI, ADI, SVI – 30 different variables are used, ranging from seven variables in the NCI SES Index to 17 in the ADI. While these studies have consistently confirmed the effects of neighborhood deprivation on cancer related outcomes, the collective findings can be challenging to compare and interpret due to the variety of methods used to measure neighborhood level deprivation. Despite the convergence of the research community to use the four commonly identified indices, they all differ substantially. For example, The NCI SES Index is weighted heavily on the variables included in the poverty/wealth, education, and employment domains, while bearing no weight from variables regarding housing or minority status and language as seen in the SVI. Furthermore, despite both sharing inclusion of poverty/wealth variables, the dimensions are defined differently. The NCI SES Index includes measures: median household income median house value, median gross rent, and percent population below 150% poverty level, whereas the SVI only consists of variables: per capita income and percent of families below the poverty level.
Literature demonstrates that these differences matter, and that the selection of variables may depend on the health outcome and population of interest. For example, Yu and colleagues compared the NCI SES Index to an index developed by Krieger in a SEER registry study.16 The Krieger Index included variables regarding housing, car ownership, and crowded living quarters while the NCI SES index did not. As a result, the NCI SES index gave lower ranks (less deprivation) than the Krieger Index to rural communities, who were more likely to own a car, live in a house, and live in less crowded spaces. They concluded that though there is not yet a consensus definition of neighborhood SES, the NCI SES index may provide a simplified definition broadly applicable across geographic areas.16 A study included in this review offered a solution to this issue of choice of index selection while studying liver cancer incidence in the Pennsylvania State Cancer Registry.24 By introducing a Bayesian geoadditive approach, they were able to visually assess how neighborhood liver cancer risk changed with the inclusion and exclusion of different neighborhood SES indices, eventually finding a model best fit by combining the NCI SES index criteria with Krieger’s Index of the Concentration of Extremes (ICE) – Income model.25 This combination was able to attenuate relative risk and geographic disparities after neighborhood SES adjustment.24 There is utility in all indices, so researchers may benefit from considering multiple neighborhood SES measures statistically and geospatially to determine which group of measures impact the target study population, and provide rationale for the measure selection.
Most studies did not provide reason for use of index versus individual measures. Understanding a study’s causal framework can be important when considering the use of indices or individual measures. The use of individual measures may have value in situations that help us understand how certain aspects of SES are associated with outcomes or test a specific hypothesis. For example, individual measures of transportation may be more important to use if the outcome of interest is travel to high-volume hospitals, or a measure of food availability may be more appropriate to use if investigating surgical outcomes of esophagectomy26–29 However, use of individual measures risk making inferences based on the inclusion of one variable without concurrently considering the system of factors that contribute to the deprived community, which can produce incomplete conclusions. The use of an index may more accurately reflect the multidimensional nature of a community’s SES.6,30
Across multiple different methodologies, there is a strong indication that deprived areas are at adverse odds of cancer related outcomes. Composite indices can be used for a variety of reasons to target these disparities. Indices can be used to evaluate risk adjustment while controlling confounding factors, identify and locate areas of geospatial disparity to target for quality assessment at the state or local level, or further investigate the drivers of racial disparities and inequity by controlling for community factors in the context of interpersonal racism.31–33Our study has some important limitations. First, the aim of our review was to provide an overview of recent use cases of neighborhood deprivation and cancer research. There are cancer related studies prior to 2015 that utilized neighborhood deprivation measures that were not included in our analysis. However, we believe that our review offered a timely glimpse at the current trends of indices and captures sufficient studies for a robust review. Additionally, we did not consider analyzing the strength of statistical methods to construct indices. Neighborhood level indices are often developed using factor analysis, principal component analysis, or z-score summation. While all methods may produce meaningful indices for specific applications and populations, there are fundamental differences in each approach and the indices may not maintain validity with other uses. Dissecting this generalizability of indices was not within the scope of this review but warrants additional evaluation. Finally, we did not have all cancer-related outcomes in our inclusion criteria and as such there may be additional indices used with other cancer research.
Further work in determining a more robust approach to quantifying deprivation in the context of cancer will enhance our understanding of which measures offer the most weight in adverse cancer outcomes and can further inform future health care delivery and policy. The increased use of common deprivation methods may help create a more uniform and refined definition of neighborhood deprivation and direct future studies investigating cancer and area level socioeconomic characteristics.
Supplementary Material
References
- 1.Krieger N, Williams DR, Moss NE. Measuring social class in US public health research: concepts, methodologies, and guidelines. Annu Rev Public Health. 1997;18:341–378. [DOI] [PubMed] [Google Scholar]
- 2.Krieger N, Chen JT, Waterman PD, Soobader MJ, Subramanian SV, Carson R. Geocoding and monitoring of US socioeconomic inequalities in mortality and cancer incidence: does the choice of area-based measure and geographic level matter?: the Public Health Disparities Geocoding Project. Am J Epidemiol. 2002;156(5):471–482. [DOI] [PubMed] [Google Scholar]
- 3.Diez-Roux AV, Kiefe CI, Jacobs DR Jr, et al. Area characteristics and individual-level socioeconomic position indicators in three population-based epidemiologic studies [published correction appears in Ann Epidemiol. 2001 Aug;30(4):924. Roux AV [corrected to Diez-Roux]]. Ann Epidemiol. 2001;11(6):395–405. [DOI] [PubMed] [Google Scholar]
- 4.Yost K, Perkins C, Cohen R, Morris C, Wright W. Socioeconomic status and breast cancer incidence in California for different race/ethnic groups. Cancer Causes Control. 2001;12(8):703–711. [DOI] [PubMed] [Google Scholar]
- 5.Census Bureau, U., 2022. Glossary. [online] Census.gov. Available at: <https://www.census.gov/programs-surveys/geography/about/glossary.html#par_textimage_13> [Accessed 10 February 2022]. [Google Scholar]
- 6.Singh GK. Area deprivation and widening inequalities in US mortality, 1969–1998. Am J Public Health. 2003;93(7):1137–1143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Messer LC, Laraia BA, Kaufman JS, et al. The development of a standardized neighborhood deprivation index. J Urban Health. 2006;83(6):1041–1062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Saldana-Ruiz N, Clouston SA, Rubin MS, Colen CG, Link BG. Fundamental causes of colorectal cancer mortality in the United States: understanding the importance of socioeconomic status in creating inequality in mortality. Am J Public Health. 2013;103(1):99–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rubin MS, Clouston S, Link BG. A fundamental cause approach to the study of disparities in lung cancer and pancreatic cancer mortality in the United States. Soc Sci Med. 2014;100:54–61. [DOI] [PubMed] [Google Scholar]
- 10.Kind AJH, Buckingham W. Making Neighborhood Disadvantage Metrics Accessible: The Neighborhood Atlas. N Engl Jl Med, 2018. 378: 2456–2458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Atsdr.cdc.gov. 2015. CDC/ATSDR’s Social Vulnerability Index (SVI). [online] Available at: <https://www.atsdr.cdc.gov/placeandhealth/svi/index.html>.
- 12.SEER. n.d. Census Tract-level SES and Rurality Database - SEER*Stat. [online] Available at: <https://seer.cancer.gov/seerstat/databases/census-tract/index.html>.
- 13.Peters MD, Godfrey CM, Khalil H, McInerney P, Parker D, Soares CB. Guidance for conducting systematic scoping reviews. Int J Evid Based Healthc. 2015;13(3):141–146. [DOI] [PubMed] [Google Scholar]
- 14.Davis K, Drey N, Gould D. What are scoping studies? A review of the nursing literature. Int J Nurs Stud. 2009;46(10):1386–1400. [DOI] [PubMed] [Google Scholar]
- 15.Arksey H and O’Malley L, 2005. Scoping studies: towards a methodological framework. International Journal of Social Research Methodology, 8(1), pp.19–32. [Google Scholar]
- 16.Yu M, Tatalovich Z, Gibson JT, Cronin KA. Using a composite index of socioeconomic status to investigate health disparities while protecting the confidentiality of cancer registry data. Cancer Causes Control. 2014;25(1):81–92. [DOI] [PubMed] [Google Scholar]
- 17.Pruitt SL, Shim MJ, Mullen PD, Vernon SW, Amick BC 3rd. Association of area socioeconomic status and breast, cervical, and colorectal cancer screening: a systematic review. Cancer Epidemiol Biomarkers Prev. 2009;18(10):2579–2599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jayasekera J, Onukwugha E, Cadham C, et al. An ecological approach to monitor geographic disparities in cancer outcomes. PLoS One. 2019;14(6):e0218712. Published 2019 Jun 21. doi: 10.1371/journal.pone.0218712 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Song S, Duan Y, Huang J, et al. Socioeconomic Inequalities in Premature Cancer Mortality Among U.S. Counties During 1999 to 2018. Cancer Epidemiol Biomarkers Prev. 2021;30(7):1375–1386. [DOI] [PubMed] [Google Scholar]
- 20.Chakravarthy R, Stallings SC, Velez Edwards DR, et al. Determinants of stage at diagnosis of HPV-related cancer including area deprivation and clinical factors. J Public Health (Oxf). 2022;44(1):18–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wheeler DC, Czarnota J, Jones RM. Estimating an area-level socioeconomic status index and its association with colonoscopy screening adherence. PLoS One. 2017;12(6):e0179272. Published 2017 Jun 8. doi: 10.1371/journal.pone.0179272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Meliker JR, Jacquez GM, Goovaerts P, Copeland G, Yassine M. Spatial cluster analysis of early stage breast cancer: a method for public health practice using cancer registry data. Cancer Causes Control. 2009. Sep;20(7):1061–9. doi: 10.1007/s10552-009-9312-4. Epub 2009 Feb 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kind AJ, Jencks S, Brock J, et al. Neighborhood socioeconomic disadvantage and 30-day rehospitalization: a retrospective cohort study. Ann Intern Med. 2014;161(11):765–774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ortiz AG, Wiese D, Sorice KA, et al. Liver Cancer Incidence and Area-Level Geographic Disparities in Pennsylvania-A Geo-Additive Approach. Int J Environ Res Public Health. 2020;17(20):7526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Krieger N, Waterman PD, Spasojevic J, Li W, Maduro G, Van Wye G. Public Health Monitoring of Privilege and Deprivation With the Index of Concentration at the Extremes. Am J Public Health. 2016;106(2):256–263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Siegel J, Engelhardt KE, Hornor MA, Morgan KA, Lancaster WP. Travel distance and its interaction with patient and hospital factors in pancreas cancer care. Am J Surg. 2021. Apr;221(4):819–825. doi: 10.1016/j.amjsurg.2020.08.023. Epub 2020 Aug 25. [DOI] [PubMed] [Google Scholar]
- 27.Siegel JB, Allen S, Engelhardt KE, Morgan KA, Lancaster WP. Travel distance and overall survival in hepatocellular cancer care. Am J Surg. 2021. Sep;222(3):584–593. doi: 10.1016/j.amjsurg.2020.12.052. Epub 2020 Dec 31. [DOI] [PubMed] [Google Scholar]
- 28.Fong AJ, Lafaro K, Ituarte PHG, Fong Y. Association of Living in Urban Food Deserts with Mortality from Breast and Colorectal Cancer. Ann Surg Oncol. 2021. Mar;28(3):1311–1319. doi: 10.1245/s10434-020-09049-6. Epub 2020 Aug 25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fay KA, Maeder ME, Emond JA, Hasson RM, Millington TM, Finley DJ, Phillips JD. Residing in a food desert is associated with an increased risk of readmission following esophagectomy for cancer. J Thorac Dis. 2022. Jun;14(6):1854–1868. doi: 10.21037/jtd-21-1637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Singh GK, Miller BA, Hankey BF. Changing area socioeconomic patterns in U.S. cancer mortality, 1950–1998: Part II--Lung and colorectal cancers. J Natl Cancer Inst. 2002. Jun 19;94(12):916–25. doi: 10.1093/jnci/94.12.916. [DOI] [PubMed] [Google Scholar]
- 31.Chang HY, Hatef E, Ma X, Weiner JP, Kharrazi H. Impact of Area Deprivation Index on the Performance of Claims-Based Risk-Adjustment Models in Predicting Health Care Costs and Utilization. Popul Health Manag. 2021. Jun;24(3):403–411. doi: 10.1089/pop.2020.0135. Epub 2020 Sep 10. [DOI] [PubMed] [Google Scholar]
- 32.Ghirimoldi FM, Schmidt S, Simon RC, Wang CP, Wang Z, Brimhall BB, Damien P, Moffett EE, Manuel LS, Sarwar ZU, Shireman PK. Association of Socioeconomic Area Deprivation Index with Hospital Readmissions After Colon and Rectal Surgery. J Gastrointest Surg. 2021. Mar;25(3):795–808. doi: 10.1007/s11605-020-04754-9. Epub 2020 Sep 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Krieger N, Singh N, Waterman PD. Metrics for monitoring cancer inequities: residential segregation, the Index of Concentration at the Extremes (ICE), and breast cancer estrogen receptor status (USA, 1992–2012). Cancer Causes Control. 2016. Sep;27(9):1139–51. doi: 10.1007/s10552-016-0793-7. Epub 2016 Aug 8. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


