Abstract
Regional anesthesia has benefits beyond just treating acute postoperative pain. Interfascial plane blocks, which have been very popular with ultrasound in recent years, function primarily by administering a high volume of a local anesthetic to the fascial plane. Contrary to traditional peripheral nerve blocks, the targeted nerve or structure in interfacial plane blocks is not fully defined, and the indications have not been fully revealed yet. Anatomical, cadaveric, and radiological studies show how effective the interfascial plane blocks play a role. This review focuses on the benefits, techniques, indications, and complications of interfascial plane blocks in the context of breast, thoracic, and orthopedic surgery.
Keywords: Interfascial plane block, acute pain, multimodal analgesia, postoperative analgesia
Main Points
Regional anesthesia is a crucial component of multimodal analgesia in relieving acute postoperative pain.
Interfascial plane blocks have become very popular in the last decade with the use of ultrasonography in regional anesthesia practice.
In cases where neuraxial analgesia cannot be applied or is contraindicated, interfascial plane blocks may be an alternative technique for appropriate surgical procedures.
Interfascial plane blocks show similar efficacy to neuraxial analgesia, which is the gold standard in postoperative analgesia.
Introduction
Regional anesthesia is a true component of anesthesia, and they are inseparable. Especially in the last 2 or 3 decades, the practice of regional anesthesia regimens has changed considerably. While there were neuraxial techniques at the beginning,1 later on, there was application of extremity blocks with a stimulator.2 In the following times, facial blocks with pop-ups3 showed up in the practice of regional anesthesia. However, now anesthesiologists go far beyond just performing extremity and neuraxial blocks. Today, by using ultrasound, we can see not only the nerves but also the facial planes where the nerves are located, and USG-guided facial plane blocks have become very popular applications.4
When we look at the facial plane blocks that start with Transversus Abdominis Plane (TAP) and become popular with erector spinae plane (ESP), we see many blocks defined differently for each plane and various nomenclatures.5-7 The answer to the question of whether facial planes used to deliver local anesthetics (LAs) to target nerves can provide anesthesia/analgesia or provide some perks beyond anesthesia/analgesia is still unknown. Contrary to traditional peripheral nerve blocks, the targeted nerve or structure within interfacial plane blocks is not fully defined, and the indications have not been revealed yet. After this point, the question of “What changes future will bring” appears. It would not be difficult to predict what awaits us and what the future of regional anesthesia will hold in this era when the concepts of artificial intelligence, machine learning, and deep learning have roles in our lives now.8
In this review, we will not proceed through the names of the blocks, and we will list the types of regional anesthesia that can be used for different types of surgeries.
Breast and Thoracic Surgery
Innervation of the breast and the axilla is provided by nerves originating from different regions.9 The lateral and median pectoral nerves originating from the brachial plexus provide most of the motor and proprioceptive innervation of the pectoralis major and minor muscles. In the axillary area, intercostobrachial nerves and thoracodorsal and thoracic longus nerves are involved. The second leading nerve group that provides sensory innervation of the breast tissue are the anterior and lateral divisions of the T2-T6 intercostal nerves. The intercostal nerves are a continuation of the ventral rami of the spinal nerve roots and extend from the intervertebral foramen to the sternum. It gives off the lateral cutaneous branch at the midaxillary line which perforates through the intercostal and serratus muscles and divides into posterior and anterior branches which supply the posterolateral and anterolateral chest wall, respectively. The terminal anterior cutaneous nerves provide the sensation of the sternal, parasternal region, and medial half of the breast. The innervation is made complex by multiple anastomosis between adjacent spinal/intercostal nerves. The midline has cross innervation from the contralateral anterior cutaneous divisions of corresponding intercostal nerves. The supraclavicular nerves arising from the superficial cervical plexus provide cutaneous innervation to the superior aspect of the breast.10 While blockade of intercostal nerves is essential for thoracic surgery, other branches coming from the brachial plexus are also required to be blocked in breast surgery for effective postoperative analgesia.
Epidural anesthesia and thoracic paravertebral block (TPVB) are the gold standard analgesic methods for breast and thoracic surgery; nevertheless, ultrasound-guided (USG) fascial plane blocks have also become popular in recent years. Intertransverse process block, ESP block (ESPB), retrolaminar block (RLB) applied from the paraspinal region, rhomboid intercostal sub-serratus plane (RISS) block applied from the parascapular region, superficial and deep serratus anterior plane (SAP) blocks (SAPBs), interpectoral plane block, and pectoserratus plane (PSP) block applied from the chest wall area are some of them. In addition, the superficial and deep parasternal intercostal plane (PIP) blocks are used for sternotomy and sternal surgery and also as a complementary block in patients undergoing breast surgery.
Retrolaminar Block
The retrolaminar block was first described in 2006 as a simple alternative to TPVB.11 The aim of the RLB is to only touch the bony vertebral lamina, rather than puncturing the superior costotransverse ligament and entering the paravertebral space. In the USG RLB, local anesthetic is injected into the fascial plane between the posterior surface of the thoracic lamina and the paraspinal muscles (Figure 1). In cadaveric studies, it has been shown that the dye solution spreads anteriorly and spreads to the paravertebral and epidural areas.12 It has been shown in clinical studies to provide effective postoperative analgesia in breast surgery and thoracic surgery.13,14 In a study conducted on patients who underwent modified radical mastectomy, comparing continuous RLB with paravertebral block (PVB), continuous RLB had a similar effect to PVB except for the first 24 hours.15 Furthermore, in a clinical study comparing ESPB and RLB performed with 20 mL of 0.375% levobupivacaine for breast surgery, ESPB was found to be equivalent to and not superior to RLB for postoperative analgesia.16 For thoracic surgery, there are 2 different studies comparing RLB with PVB and epidural block. In a retrospective study evaluating 192 minor video-assisted thoracic surgery (VATS) patients, RLB were non-inferior to epidural block.14 However, in another study, PVB and RLB were compared in VATS, postoperative pain scores and opioid consumption were lower in patients who underwent PVB.17
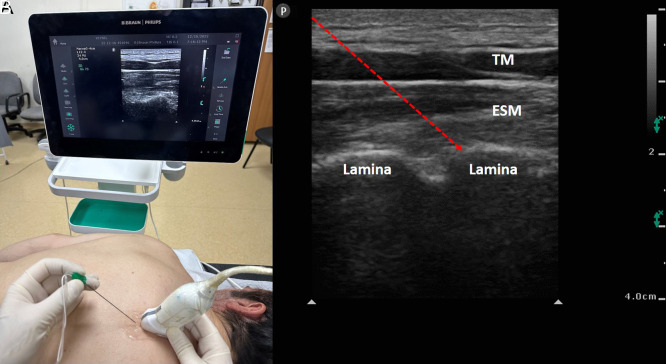
Figure 1. A, B.
(A) Patient and ultrasound probe position for retrolaminar block procedure. (B) Sonographic anatomy of the block. ESM, erector spinae muscle; TM, trapezius muscle; red arrow, needle.
Erector Spinae Plane Block
Ultrasound-guided ESPB was first reported by Forero et al18 and was described for chronic thoracic neuropathic pain in 2016. Erector spinae plane block has since been widely used both in the management of acute postoperative pain and chronic pain.5,6,19-31 The ESPB can be applied in a wide area from the cervical to the sacral region along the erector spinae muscle (ESM). It is typically performed by administering local anesthetic between the tips of the vertebral transverse processes and the ESM (Figure 2). The local anesthetic spreads in the cranio-caudal direction to the 3-6 vertebral levels, but the medial-to-lateral spread is limited to the attachments of the ESM to the ribs and thoracolumbar fascia. Though the mechanism of spread into the paravertebral space from an ESPB is unclear, it is postulated from cadaveric studies using high-resolution computed tomography (CT), the spread is through the inter-transverse connective tissue along the dorsal rami and accompanying blood vessels. The local anesthetic spreads anteriorly from the injected plane, passes into the paravertebral area and affects the dorsal and ventral rami of the spinal nerves, and hence provides sensory and sympathetic blockade.32 There are many studies and subsequent meta-analyses showing the effectiveness of ESPB in breast surgery and thoracic surgery. Thirty-two articles including 6 randomized controlled studies in a review evaluating ESPB compared with tumescent anesthesia or no block in breast surgery found ESPB can decrease postoperative pain and opioid consumption.33 In another meta-analysis of 14 randomized controlled studies comparing ESPB and without a block for postoperative analgesia in breast and thoracic surgery patients, it was shown that ESPB not only significantly improved pain scores up to 24 hours at postoperative time points but also reduced 24-hour opioid consumption. Furthermore, when ESPB was compared with PVB, the analgesic efficacy of ESPB was similar to PVB in pain scores, 24-hour opioid consumption, and postoperative nausea and vomiting (PONV)rates.34 Erector spinae plane block is also used in the treatment of chronic pain in the thoracic region with recurrent blocks or catheter applications. It is effective in cancer pain involving a single hemithorax or postherpetic neuralgia.35,36
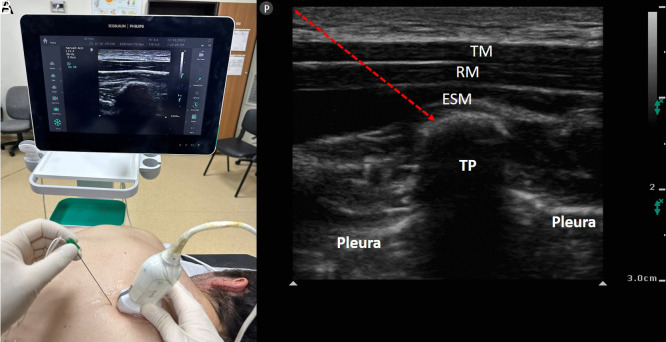
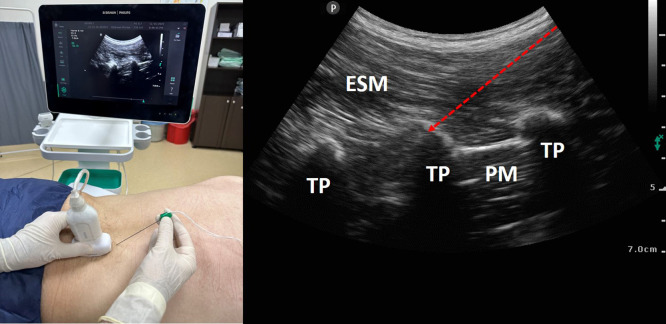
Figure 2. A, B.
(A) Patient and ultrasound probe position for thoracic erector spinae plane block procedure. (B) Sonographic anatomy of the block. ESM, erector spinae muscle; RM, rhomboid muscle; TM, trapezius muscle; TP, transverse process; red arrow, needle.
Rhomboid Intercostal Block
The rhomboid intercostal block (RIB) is performed in the area known as the auscultation triangle in the posterior chest wall region. The RIB is performed with the injection of local anesthetic in the plane between the rhomboid and the intercostal muscles. The RIB provides anesthesia between T2 and T7 dermatomes (Figure 3). The recent modification of this block, which is named the RISS block, affects T2-T11 dermatomes. Considering the dermatomal areas where it is effective, this block can be used in breast and axillary surgery, thoracic surgery, and upper abdominal surgery. There are publications showing the effectiveness of RIB in modified radical mastectomy, breast reduction surgery, and in the treatment of chronic pain after breast surgery.37-39 For the thoracic region, its effectiveness has been demonstrated in VATS and multiple rib fractures in the lateral region.40-43 A meta-analysis of studies that evaluated RIB and no block in patients undergoing breast and thoracic surgery showed that patients who underwent RIB had lower pain scores, opioid consumption, and PONV rates.44 In another study comparing the efficacy of RISS, ESP, and SAPB in patients undergoing VATS, it was identified that the patients who underwent RIB and ESPBs had lower opioid consumption and dynamic pain scores in the first 24 hours postoperatively compared to SAPB.45
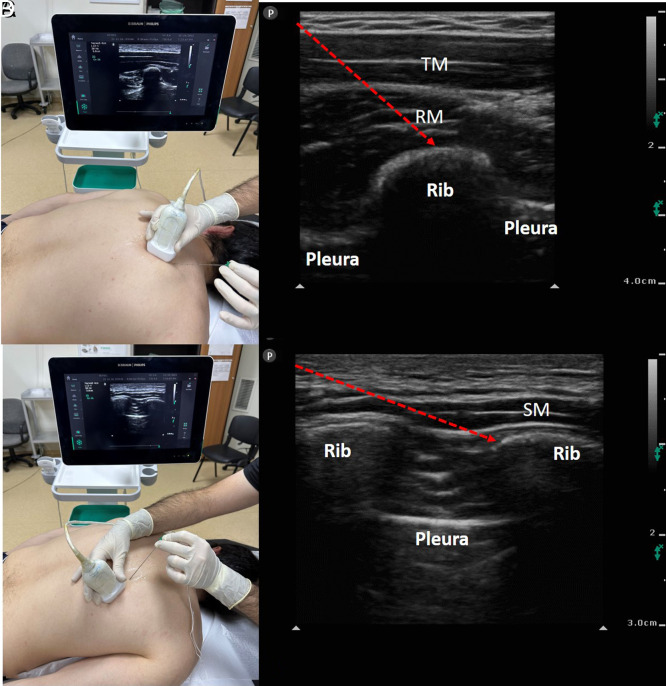
Figure 3. A-D.
(A–C) Patient and ultrasound probe position for rhomboid intercostal sub-serratus block procedure. (B–D) Sonographic anatomy of the block. RM, rhomboid muscle; SM, serratus muscle; TM, trapezius muscle; red arrow, needle.
Serratus Anterior Plane Block
This block is performed by injecting LA between the serratus anterior muscle and the rib (deep SAPB) or between the serratus anterior muscle and the latissimus dorsi muscle (superficial SAPB) in the area where the fourth ribs intersect with the midaxillary line (Figure 4). In the SAPB, T2-T8 intercostal nerves and long thoracic and thoracodorsal nerves are blocked. The SAPB has mainly been shown to be effective in oncological breast surgery, breast reduction surgery, thoracic surgery, anterolateral rib fractures, and chest wall chronic pain treatment.46-49 Blanco et al.50 in a small study on female volunteers, compared superficial and deep SAPB. Each volunteer was given 2 injections with a deep SAPB on one side and a superficial SAPB on the other, with LA and gadolinium. In the dermatological examination and magnetic resonance imaging performed 30 minutes after the injection, it was observed that a large area of thoracic dermatomes was anesthetized in all patients. In their study, a larger area and a longer duration of sensory loss were reported in the superficial SAP compared to the deep SAP. There are many randomized controlled studies showing the efficacy of SAPB in breast and thoracic surgery. In a meta-analysis of studies evaluating the efficacy of SAP in breast cancer surgery, it was shown that SAPB reduces intraoperative fentanyl consumption, reduces postoperative analgesic requirements, and reduces postoperative nausea and vomiting. When compared to TPVB, SAPB was not worse for the all evaluated parameters.48 Similarly, in a meta-analysis evaluating the efficacy of SAPB in thoracic surgery, SAPB reduced both pain scores and postoperative 24-hour opioid consumption, in addition, there was a lower incidence of PONV in the SAPB group.51
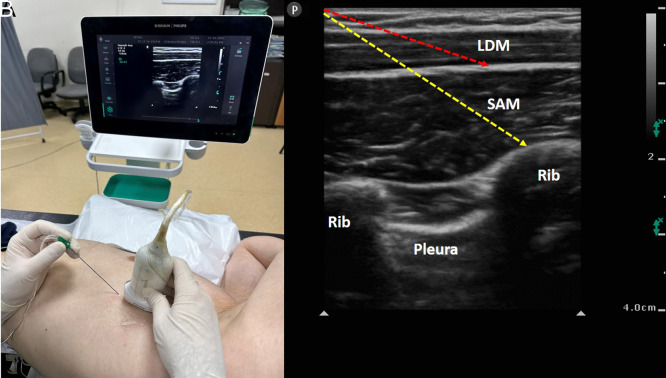
Figure 4. A, B.
(A) Patient and ultrasound probe position for serratus anterior plane block procedure. (B) Sonographic anatomy of the block. LDM, latissimus dorsi muscle; SAM: serratus anterior muscle; red arrow, needle direction for superficial serratus anterior plane block; yellow arrow, needle direction for deep serratus anterior plane block.
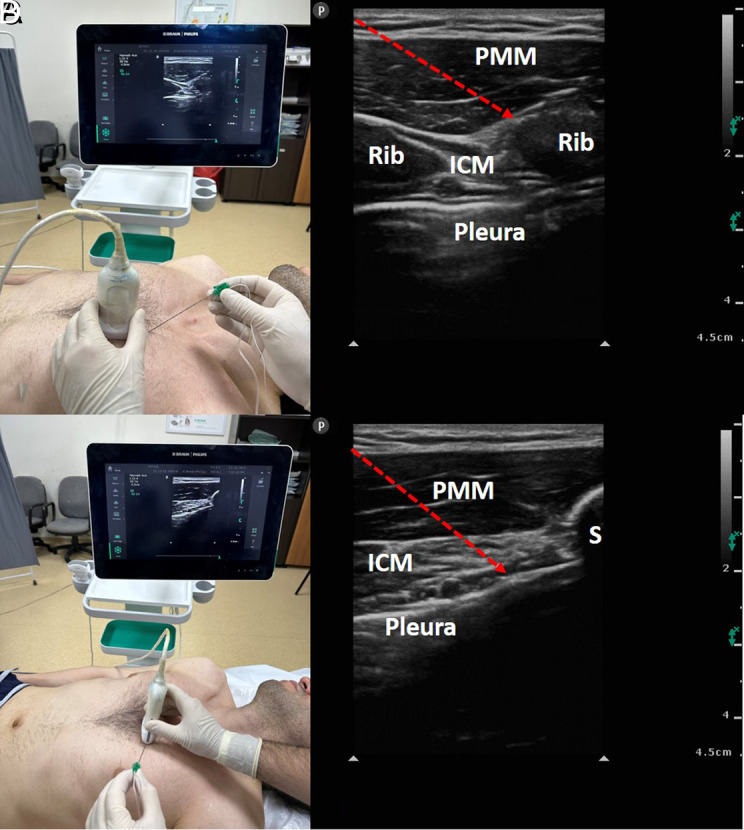
Interpectoral Plane Block and Pectoserratus Plane Block
Interpectoral plane block (previously known as PECS-I block) is applied by injecting LA between the pectoralis major and pectoralis minor muscles (Figure 5). This injection point is the fascial plane where the pectoral branch of the thoraco-acromial artery and the lateral pectoral nerve are located. The medial pectoral nerve is located in the inferolateral region of this injection point. The pectoral nerves have no cutaneous innervation, they only innervate the pectoral muscles. But it is still used to manage pain caused by stretching or injury of the pectoral muscles.52 Pectoserratus plane block (formerly called PECS-II block) is performed by injecting LA between the pectoralis minor and serratus anterior muscles at the intersection of the third or fourth rib in the anterior axillary line. The dermatomal area affected by the PSP block is similar to the SAPB and it is covered the intercostobrachial nerve, long thoracic nerve, and third-sixth intercostal nerves.53 Interpectoral plane and PSP blocks were first described as an alternative to paravertebral block, providing effective analgesia in breast surgery. And also it was widely used in thoracic surgery, cardiac surgery, and post-surgical chronic pain management. In a meta-analysis that included 1026 patients and 16 studies, in patients undergoing mastectomy and other breast surgery, comparing the effects of PSP block and no block, the meta-analysis provided moderate-to-high evidence that PSP blocks provide postoperative analgesia after breast surgery.54 In another meta-analysis comparing PSP block with control, LA infiltration, ESPB, and paravertebral block in breast cancer surgery, PSP block reduces intraoperative and postoperative opioid consumption compared to control and ESPB, and PSP provides better pain relief compared to paravertebral block.55 Furthermore, PSP blocks not only reduce the effect on acute postoperative pain but also reduce the incidence of chronic pain after breast surgery.56 For thoracic surgery, it has been shown to be effective as a part of multimodal analgesia in thoracoscopic surgery and minimally invasive pectus excavatum surgery.57,58
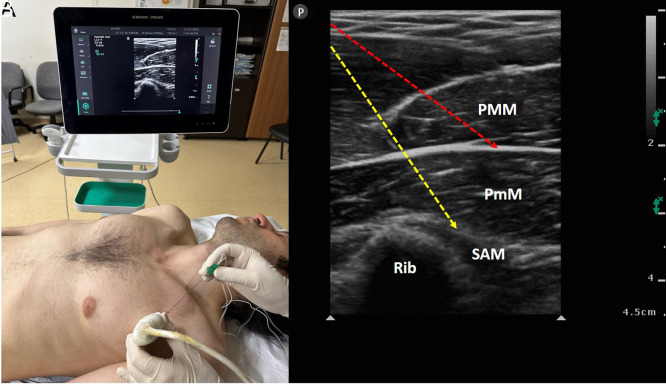
Figure 5. A, B.
(A) Patient and ultrasound probe position for interpectoral plane block and pectoserratus plane block procedure. (B) Sonographic anatomy of the block. PMM, pectoralis major muscle; PmM, pectoralis minor muscle; SAM, serratus anterior muscle; red arrow, needle direction for interpectoral plane block; yellow arrow, needle direction for pectoserratus plane block procedure.
Parasternal Intercostal Plane Block
Parasternal intercostal plane blocks are performed with local anesthetic injection between the internal intercostal muscles and the pectoralis major muscle (superficial PIP) (Figure 6A and B) or between the internal intercostal muscles and the transverse thoracic muscle (deep PIP) (Figure 6C and D) in the parasternal area at the level of the third and fourth ribs. It blocks the anterior cutaneous branches of the 2-6 intercostal nerves. These blocks are frequently used for postoperative analgesia in sternal surgery and cardiac surgery with sternotomy. Parasternal intercostal plane blocks are also used in combination with other lateral wall blocks (SAPB, pectoserratus block) to provide complete analgesia in breast surgery.59-62
Figure 6. A-D.
(A) Patient and ultrasound probe position for superficial parasternal intercostal plane block. (B) Sonographic anatomy of the superficial parasternal intercostal plane block. (C) Patient and ultrasound probe position for deep parasternal intercostal plane block. (D) Sonographic anatomy of the deep parasternal intercostal plane block. PMM, pectoralis major muscle; red arrow, needle direction.
Orthopedic Surgery
Pain management is a critical issue after orthopedic surgery. Patients may suffer moderate-to-severe pain due to bone and muscle operations in orthopedic surgeries.63 Regional anesthesia techniques are used for this aim as a part of multimodal analgesia. Techniques such as interscalene nerve block and epidural analgesia (EA) are gold standard methods; however, they have complications such as diaphragmatic paralysis for interscalene block (ISB), and dural puncture, hypotension, headache for EA.64-66 In addition, they have some technical difficulties in applications. Therefore, simple and safe methods are needed in daily applications. The rising star “interfascial plane blocks” are very popular in anesthesia practice nowadays. Thanks to the use of ultrasound novel plane blocks have been described recently.7 In this section, our aim is to refer to fascial plane blocks that can be used for postoperative analgesia management following orthopedic surgeries.
Erector Spinae Plane Block
The LA is performed between the transverse process and ESM into the plane deep into the ESM (Figure 7). The LA runs a long way in the deep fascia of ESM. Erector spinae plane block provides a large sensorial blockade due to this plane contains dorsal and ventral rami.5,6,25,32,67-69 In addition, it has been reported that ESPB spreads epidural and paravertebral spaces.31 Since ESPB has these features, it was classified as a paraspinal block. High-thoracic/cervical ESPB may be used for pain relief after arthroscopic shoulder surgery, upper extremity surgery, shoulder disarticulation surgery, and for chronic shoulder pain.70-73 The sensorial innervation of the shoulder and upper extremity is provided by the C4-C8 segments of the brachial plexus. It has been reported that the T2-level ESPB spreads over the C4-C8 in CT images. The ESPB may be an alternative analgesic technique in patients with pulmonary comorbidities after shoulder surgery due to its phrenic nerve-sparing effect. Ma et al74 performed high-thoracic ESPB for proximal humerus surgery and total shoulder arthroplasty surgery, and they reported that ESPB has a motor-sparing effect. Diwan et al75 reported ESPB as a phrenic nerve-sparing block for shoulder surgeries. Ekinci et al71 performed ESPB for upper extremity surgery and they reported low pain scores and no additional analgesic drug needed. Ciftci et al70 performed T2-level ESPB for arthroscopic shoulder surgery in their randomized study, and they reported that ESPB provided better pain relief compared to the sham group. Kapukaya et al76 compared the ESPB and ISB after arthroscopic shoulder surgery, and they reported ISB in the first 4 hours postoperatively. The ESPB may be a better choice for patients undergoing shoulder surgery, especially in patients with pulmonary insufficiency and anatomical difficulties. Although many studies show that lumbar ESPB is effective in hip surgery,69,77 some studies argued that it is not effective.78 For lumbar ESP to be effective in hip surgery, it must be done at L3 and below levels, and the volume of LA must be high.
Figure 7. A, B.
(A) Patient and ultrasound probe position for lumbar erector spinae plane block procedure. (B) Sonographic anatomy of the block. ESM, erector spinae muscle; PM, psoas muscle; TP, transverse process; red arrow, needle.
Deep Supraspinatus Muscle Plane Block
Kose et al79 described the deep supraspinatus muscle plane block (DSMPB), which involves the injection of LA into the plane between the supraspinatus muscle and the posterior scapula (Figure 8). They performed the DSMPB on the lateral aspect of the scapula below the muscle. Deep supraspinatus muscle plane block targets the suprascapular nerve branches.79,80 The suprascapular nerve innervates the cephalad cutaneous part of the shoulder. Kose et al79 performed DSMPB on a patient with chronic shoulder pain. They reported pain relief and a pain-free period of 12 weeks. Kose et al81 performed a radiological evaluation of DSMPB, and they reported significant radiocontrast spread within the whole supraspinous fossa and partially spread into the infraspinous fossa. Additionally, dye spread in the supraspinous fossa has been reported in their cadaveric investigation.82 Altiparmak et al83 performed DSMPB for post-laparoscopic shoulder pain, and they reported effective analgesia in their patient. Öksüz et al84 performed DSMPB for rescue analgesia after shoulder surgery, and they reported pain relief after the block. The DSMPB may be performed for acute and chronic shoulder pain.
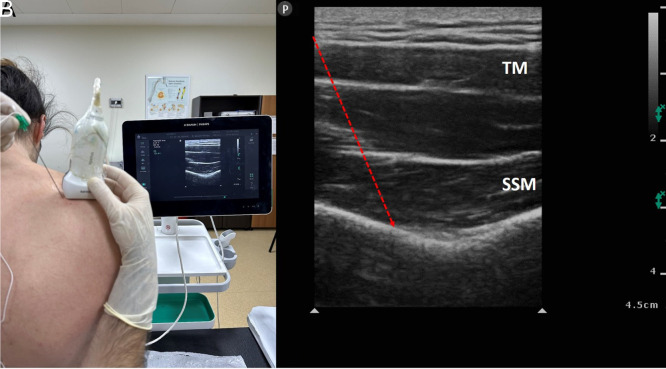
Figure 8. A, B.
(A) Patient and ultrasound probe position for deep supraspinatus muscle plane block procedure. (B) Sonographic anatomy of the block. SSM, supraspinatus muscle; TM, trapezius muscle; red arrow, needle.
Serratus Anterior Plane Block
Serratus anterior plane block was first defined by Blanco et al50 in 2013. Blanco et al performed LA between latissimus dorsi and serratus anterior muscles at the level of fourth-fifth ribs for SAPB. Serratus anterior plane block provides analgesia in the hemithorax. Serratus anterior plane block is commonly used for analgesia after thoracic surgeries, pain relief in rib fractures, and breast surgeries.40,47,49,85 Serratus anterior plane block may be also used in shoulder surgery with an adequate thoracic sensorial blockade. Demir et al86 compared ISB and ISB + SAPB in patients who underwent arthroscopic shoulder surgery. In their randomized study, they performed 30 mL LA in the 2 groups. They reported that SAPB + ISB increased the quality of surgical anesthesia and reduced the need for intraoperative sedo-analgesia. Serratus anterior plane block may be used with ISB for anesthesia management during shoulder surgery.
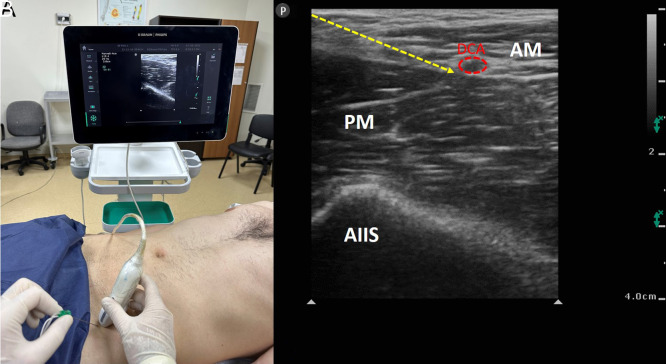
Pericapsular Nerve Group Block
Pericapsular nerve group (PENG) block was first described by Girón-Arango et al87 in 2018. They performed PENG block for hip fracture in 5 patients. They reported reduced pain scores compared to baseline and no motor weakness of the quadriceps muscle. Pericapsular nerve group is performed into the fascial plane between the psoas tendon and pubic ramus with an in-plane approach by using a convex probe (Figure 9). The anatomical landmarks are the anterior inferior iliac spine, pubic ramus, iliopubic eminence, iliopsoas muscle and tendon, the femoral artery, and pectineus muscle. Pericapsular nerve group block targets the articular branches of the hip capsule. The anterior hip capsule is mainly innervated by the articular branches of the femoral nerve and accessory obturator nerve. Pericapsular nerve group mainly provides analgesia for the anterior part of the hip.87 However, in a cadaveric study, it was reported that PENG may spread to the joint surface and posterior of the hip.88 It was reported that a high-volume PENG block may act as a lumbar plexus block.89 Ahiskalioglu et al90 used the PENG for surgical anesthesia of the medial thigh. Ciftci et al91 reported that high-volume PENG may result in motor blockade due to the spread of the femoral nerve and obturator nerve. Pericapsular nerve group block may be effectively used for postoperative analgesia management in patients who underwent hip surgery. In addition, by using high volumes, PENG can be an alternative method for postoperative analgesia after knee surgery.
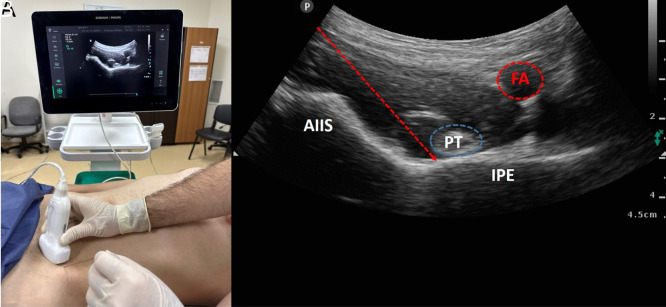
Figure 9. A, B.
(A) Patient and ultrasound probe position for pericapsular nerve group block procedure. (B) Sonographic anatomy of the block. AIIS, anterior inferior iliac spine; FA, femoral artery; IPE, iliopubic eminence; PT, psoas muscle tendon; red arrow, needle.
Suprainguinal Fascia Iliaca Block
Fascia iliaca block (FIB) contains the injection of LA in the plane between the fascia iliaca and the iliacus muscle (Figure 10), which includes the femoral nerve and lateral femoral cutaneous nerve (LFCN).92 It is used for the anesthesia/analgesia of the hip, knee, and thigh.93 Ultrasound-guided FIB has 2 approaches: suprainguinal and infrainguinal approaches. Hebbard et al93 reported that LA is injected directly into the iliac fossa during suprainguinal fascia iliaca block (SFIB). The needle is directed under the fascia iliaca from below the inguinal ligament. Thus, the needle tip passes superior to the ligament. It has been shown that injection with suprainguinal technique leads to a wide spread in the iliac fossa of cadavers. The SFIB may allow lower LA volumes to block the femoral nerve and LFCN in patients. In the literature, SFIB has been used for total hip arthroplasty, knee surgery, and pediatric knee/hip surgery.94-98 The SFIB and PENG may be used for ease of positioning during spinal anesthesia in patients with hip fractures.99
Figure 10. A, B.
(A) Patient and ultrasound probe position for suprainguinal fascia iliaca block procedure. (B) Sonographic anatomy of the block. AIIS, anterior inferior iliac spine; AM, abdominal muscles; DCA, deep circumflex iliac artery; FA, femoral artery; PM, psoas muscle; yellow arrow, needle.
Footnotes
Peer-review: Externally peer-reviewed.
Author Contributions: Concept – A.A., A.M.Y.; Design – S.T., E.O.A.; Supervision – M.N., B.B.; Materials – M.E.A.; Data Collection and/or Processing – E.C.C.; Literature Review – B.C., M.E.A., E.C.C.; Writing Manuscript – A.M.Y., A.A.; Critical Review – S.T., A.A.
Declaration of Interests: The authors have no conflicts of interest to declare.
Funding: The authors declared that this study has received no financial support.
References
- 1. Brill S, Gurman GM, Fisher A. A history of neuraxial administration of local analgesics and opioids. Eur J Anaesthesiol. 2003;20(9):682 689. ( 10.1017/s026502150300111x) [DOI] [PubMed] [Google Scholar]
- 2. Orebaugh SL, Williams BA, Vallejo M, Kentor ML. Adverse outcomes associated with stimulator-based peripheral nerve blocks with versus without ultrasound visualization. Reg Anesth Pain Med. 2009;34(3):251 255. ( 10.1097/AAP.0b013e3181a3438e) [DOI] [PubMed] [Google Scholar]
- 3. Rafi AN. Abdominal field block: a new approach via the lumbar triangle. Anaesthesia. 2001;56(10):1024 1026. ( 10.1046/j.1365-2044.2001.02279-40.x) [DOI] [PubMed] [Google Scholar]
- 4. Hebbard P, Fujiwara Y, Shibata Y, Royse C. Ultrasound-guided transversus abdominis plane (TAP) block. Anaesth Intensive Care. 2007;35(4):616 617. [PubMed] [Google Scholar]
- 5. Tulgar S, Ahiskalioglu A, De Cassai A, Gurkan Y. Efficacy of bilateral erector spinae plane block in the management of pain: current insights. J Pain Res. 2019;12:2597 2613. ( 10.2147/JPR.S182128) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Tulgar S, Aydin ME, Ahiskalioglu A, De Cassai A, Gurkan Y. Anesthetic techniques: focus on lumbar erector spinae plane block. Local Reg Anesth. 2020;13:121 133. ( 10.2147/LRA.S233274) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Elsharkawy H, Pawa A, Mariano ER. Interfascial plane blocks: back to basics. Reg Anesth Pain Med. 2018;43(4):341 346. ( 10.1097/AAP.0000000000000750) [DOI] [PubMed] [Google Scholar]
- 8. Ahiskalioglu A, Yayik AM, Karapinar YE, Tulgar S, Ciftci B. From ultrasound to artificial intelligence: a new era of the regional anesthesia. Minerva Anestesiol. 2022;88(7-8):640 642. ( 10.23736/S0375-9393.22.16456-4) [DOI] [PubMed] [Google Scholar]
- 9. Chin KJ, Versyck B, Pawa A. Ultrasound-guided fascial plane blocks of the chest wall: a state-of-the-art review. Anaesthesia. 2021;76(suppl 1):110 126. ( 10.1111/anae.15276) [DOI] [PubMed] [Google Scholar]
- 10. Smeele HP, Bijkerk E, van Kuijk SMJ, Lataster A, van der Hulst RRWJ, Tuinder SMH. Innervation of the female breast and nipple: a systematic review and meta-analysis of anatomical dissection studies. Plast Reconstr Surg. 2022;150(2):243 255. ( 10.1097/PRS.0000000000009306) [DOI] [PubMed] [Google Scholar]
- 11. Pfeiffer G, Oppitz N, Schöne S, Richter-Heine I, Höhne M, Koltermann C. Analgesia of the axilla using a paravertebral catheter in the lamina technique. Anaesthesist. 2006;55(4):423 427. ( 10.1007/s00101-005-0969-0) [DOI] [PubMed] [Google Scholar]
- 12. Yang HM, Choi YJ, Kwon HJ, O J, Cho TH, Kim SH. Comparison of injectate spread and nerve involvement between retrolaminar and erector spinae plane blocks in the thoracic region: a cadaveric study. Anaesthesia. 2018;73(10):1244 1250. ( 10.1111/anae.14408) [DOI] [PubMed] [Google Scholar]
- 13. Onishi E, Murakami M, Nishino R, Ohba R, Yamauchi M. Analgesic effect of double-level retrolaminar paravertebral block for breast cancer surgery in the early postoperative period: a placebo-controlled, randomized clinical trial. Tohoku J Exp Med. 2018;245(3):179 185. ( 10.1620/tjem.245.179) [DOI] [PubMed] [Google Scholar]
- 14. Nobukuni K, Hatta M, Nakagaki T, Yoshino J, Obuchi T, Fujimura N. Retrolaminar versus epidural block for postoperative analgesia after minor video-assisted thoracic surgery: a retrospective, matched, non-inferiority study. J Thorac Dis. 2021;13(5):2758 2767. ( 10.21037/jtd-21-238) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Murouchi T, Yamakage M. Retrolaminar block: analgesic efficacy and safety evaluation. J Anesth. 2016;30(6):1003 1007. ( 10.1007/s00540-016-2230-1) [DOI] [PubMed] [Google Scholar]
- 16. Sotome S, Sawada A, Wada A, Shima H, Kutomi G, Yamakage M. Erector spinae plane block versus retrolaminar block for postoperative analgesia after breast surgery: a randomized controlled trial. J Anesth. 2021;35(1):27 34. ( 10.1007/s00540-020-02855-y) [DOI] [PubMed] [Google Scholar]
- 17. Wang Q, Wei S, Li S.et al. Comparison of the analgesic effect of ultrasound-guided paravertebral block and ultrasound-guided retrolaminar block in uniportal video-assisted thoracoscopic surgery: a prospective, randomized study. BMC Cancer. 2021;21(1):1229. ( 10.1186/s12885-021-08938-7) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Forero M, Adhikary SD, Lopez H, Tsui C, Chin KJ. The erector spinae plane block: a novel analgesic technique in thoracic neuropathic pain. Reg Anesth Pain Med. 2016;41(5):621 627. ( 10.1097/AAP.0000000000000451) [DOI] [PubMed] [Google Scholar]
- 19. Ciftci B, Ekinci M, Celik EC, Yayik AM, Aydin ME, Ahiskalioglu A. Ultrasound-guided erector spinae plane block versus modified-thoracolumbar interfascial plane block for lumbar discectomy surgery: a randomized, controlled study. World Neurosurg. 2020;144:e849 e855. ( 10.1016/j.wneu.2020.09.077) [DOI] [PubMed] [Google Scholar]
- 20. Yayik AM, Ahiskalioglu A, Çelik EC, Ay A, Ozenoglu A. Continuous erector spinae plane block for postoperative analgesia of multiple rib fracture surgery: case report. Braz J Anesthesiol. 2019;69(1):91 94. ( 10.1016/j.bjan.2018.08.001) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Ahiskalioglu A, Yayik AM, Celik EC, Ahiskalioglu EO, Emsen M. Two plane two block for surgical anesthesia: ultrasound-guided serratus and erector spinae plane blocks. J Clin Anesth. 2018;47:19 20. ( 10.1016/j.jclinane.2018.03.004) [DOI] [PubMed] [Google Scholar]
- 22. Yayik AM, Cesur S, Ozturk F.et al. Postoperative analgesic efficacy of the ultrasound-guided erector spinae plane block in patients undergoing lumbar spinal decompression surgery: a randomized controlled study. World Neurosurg. 2019;126:e779 e785. ( 10.1016/j.wneu.2019.02.149) [DOI] [PubMed] [Google Scholar]
- 23. Cesur S, Yayik AM, Ozturk F, Ahiskalioglu A. Ultrasound-guided low thoracic erector spinae plane block for effective postoperative analgesia after lumbar surgery: report of five cases. Cureus. 2018;10(11):e3603. ( 10.7759/cureus.3603) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Cesur S, Ay AN, Yayık AM, Naldan ME, Gürkan Y. Ultrasound-guided erector spinae plane block provides effective perioperative analgesia and anaesthesia for thoracic mass excision: a report of two cases. Anaesth Crit Care Pain Med. 2019;38(2):189 190. ( 10.1016/j.accpm.2018.01.002) [DOI] [PubMed] [Google Scholar]
- 25. Tulgar S, Ahiskalioglu A, Aydin ME, Jadon A, Forero M, Gürkan Y. Lumbar erector spinae plane block: a miracle or self-persuasion? Reg Anesth Pain Med. 2021;46(7):638 639. ( 10.1136/rapm-2020-102336) [DOI] [PubMed] [Google Scholar]
- 26. Aydın T, Balaban O, Ahiskalioglu A, Alici HA, Acar A. Ultrasound-guided erector spinae plane block for the management of herpes zoster pain: observational study. Cureus. 2019;11(10):e5891. ( 10.7759/cureus.5891) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Aydin ME, Tekin E, Ahiskalioglu EO.et al. Erector spinae plane block vs non-steroidal anti-inflammatory drugs for severe renal colic pain: a pilot clinical feasibility study. Int J Clin Pract. 2021;75(3):e13789. ( 10.1111/ijcp.13789) [DOI] [PubMed] [Google Scholar]
- 28. Ahiskalioglu A, Kocak AO, Doymus O, Sengun E, Celik M, Alici HA. Erector spinae plane block for bilateral lumbar transverse process fracture in emergency department: a new indication. Am J Emerg Med. 2018;36(10):1927.e3-1927.e4. ( 10.1016/j.ajem.2018.06.072) [DOI] [PubMed] [Google Scholar]
- 29. Kilicaslan A, Aydin A, Kekec AF, Ahiskalioglu A. Sacral erector spinae plane block provides effective postoperative analgesia for pelvic and sacral fracture surgery. J Clin Anesth. 2020;61:109674. ( 10.1016/j.jclinane.2019.109674) [DOI] [PubMed] [Google Scholar]
- 30. Ahiskalioglu A, Aydin ME, Alici HA. (MS 19311) Ultrasound guided erector spinae plane block as a safe and effective method to treat herpes zoster pain. Am J Emerg Med. 2019;37(6):1192 1194. ( 10.1016/j.ajem.2018.12.006) [DOI] [PubMed] [Google Scholar]
- 31. Celik M, Tulgar S, Ahiskalioglu A, Alper F. Is high volume lumbar erector spinae plane block an alternative to transforaminal epidural injection? Evaluation with MRI. Reg Anesth Pain Med. 2019. ( 10.1136/rapm-2019-100514) [DOI] [PubMed] [Google Scholar]
- 32. Chin KJ, El-Boghdadly K. Mechanisms of action of the erector spinae plane (ESP) block: a narrative review. Can J Anaesth. 2021;68(3):387 408. ( 10.1007/s12630-020-01875-2) [DOI] [PubMed] [Google Scholar]
- 33. ElHawary H, Abdelhamid K, Meng F, Janis JE. Erector spinae plane block decreases pain and opioid consumption in breast surgery: systematic review. Plast Reconstr Surg Glob Open. 2019;7(11):e2525. ( 10.1097/GOX.0000000000002525) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Huang W, Wang W, Xie W, Chen Z, Liu Y. Erector spinae plane block for postoperative analgesia in breast and thoracic surgery: a systematic review and meta-analysis. J Clin Anesth. 2020;66:109900. ( 10.1016/j.jclinane.2020.109900) [DOI] [PubMed] [Google Scholar]
- 35. Tekin E, Ahiskalioglu A, Aydin ME, Sengun E, Bayramoglu A, Alici HA. High-thoracic ultrasound-guided erector spinae plane block for acute herpes zoster pain management in emergency department. Am J Emerg Med. 2019;37(2):375.e1-375.e3. ( 10.1016/j.ajem.2018.10.028) [DOI] [PubMed] [Google Scholar]
- 36. Yayik AM, Karapinar YE, Ozgodek HB, Tor IH, Ahiskalioglu A. Bilevel opposite direction ESP block with indwelling catheter in the management of severe lung cancer pain. Interv Pain Med. 2022;1(4):100144. ( 10.1016/j.inpm.2022.100144) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Yayik AM, Ahiskalioglu A, Ates I, Ahiskalioglu EO, Cinal H. Ultrasound guided bilateral rhomboid intercostal block for breast reduction surgery. J Clin Anesth. 2019;57:38 39. ( 10.1016/j.jclinane.2019.03.001) [DOI] [PubMed] [Google Scholar]
- 38. Altıparmak B, Korkmaz Toker M, Uysal AI, Dere Ö, Uğur B. Evaluation of ultrasound-guided rhomboid intercostal nerve block for postoperative analgesia in breast cancer surgery: a prospective, randomized controlled trial. Reg Anesth Pain Med. 2020;45(4):277 282. ( 10.1136/rapm-2019-101114) [DOI] [PubMed] [Google Scholar]
- 39. Piraccini E, Calli M, Taddei S, Maitan S. Erector spinae plane block and rhomboid intercostal block for the treatment of post-mastectomy pain syndrome. Saudi J Anaesth. 2020;14(4):517 519. ( 10.4103/sja.SJA_203_20) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Yayik AM, Aydin ME, Tekin E, Ulas AB, Ahiskalioglu A. An alternative plane block for multiple rib fractures: Rhomboid Intercostal and Sub-Serratus block (RISS). Am J Emerg Med. 2019;37(12):2263.e5-2263.e7. ( 10.1016/j.ajem.2019.158429) [DOI] [PubMed] [Google Scholar]
- 41. Deng W, Liu F, Jiang CW, Sun Y, Shi GP, Zhou QH. Continuous rhomboid intercostal block for thoracoscopic postoperative analgesia. Ann Thorac Surg. 2022;114(1):319 326. ( 10.1016/j.athoracsur.2021.06.068) [DOI] [PubMed] [Google Scholar]
- 42. Longo F, Piliego C, Martuscelli M.et al. Rhomboid intercostal and subserratus plane block for intubated uniportal video-assisted thoracoscopic surgery lobectomy. J Clin Anesth. 2020;65:109881. ( 10.1016/j.jclinane.2020.109881) [DOI] [PubMed] [Google Scholar]
- 43. Kozanhan B, Semerkant T, Esme H, Canitez A, İyisoy MS. Evaluation of rhomboid intercostal and subserratus plane block under direct vision for postoperative analgesia in thoracic surgeries: a prospective, randomized controlled trial. Eur J Cardiothorac Surg. 2022;62(6). ( 10.1093/ejcts/ezac498) [DOI] [PubMed] [Google Scholar]
- 44. Chen R, Su S, Shu H. Efficacy and safety of rhomboid intercostal block for analgesia in breast surgery and thoracoscopic surgery: a meta-analysis. BMC Anesthesiol. 2022;22(1):71. ( 10.1186/s12871-022-01599-4) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Zhang JG, Jiang CW, Deng W, Liu F, Wu XP. Comparison of rhomboid intercostal block, erector spinae plane block, and serratus plane block on analgesia for video-assisted thoracic surgery: a prospective, randomized, controlled trial. Int J Clin Pract. 2022;2022:6924489. ( 10.1155/2022/6924489) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Ahiskalioglu A, Alici HA, Yayik AM, Celik M, Oral Ahiskalioglu E. Ultrasound guided serratus plane block for management of acute thoracic herpes zoster. Anaesth Crit Care Pain Med. 2017;36(5):323 324. ( 10.1016/j.accpm.2017.01.008) [DOI] [PubMed] [Google Scholar]
- 47. Ahiskalioglu A, Yayik AM, Demir U.et al. Preemptive analgesic efficacy of the ultrasound-guided bilateral superficial serratus plane block on postoperative pain in breast reduction surgery: a prospective randomized controlled study. Aesthet Plast Surg. 2020;44(1):37 44. ( 10.1007/s00266-019-01542-y) [DOI] [PubMed] [Google Scholar]
- 48. Li ZH, Hong WJ, Guo XL.et al. Serratus plane block in breast cancer surgery: a systematic review and meta-analysis. Clin Breast Cancer. 2023;23(1):e1 e13. ( 10.1016/j.clbc.2022.10.009) [DOI] [PubMed] [Google Scholar]
- 49. Sulak M, Ahiskalioglu A, Yayik A.et al. The effect of ultrasound-guided serratus plane block on the quality of life in patients undergoing modified radical mastectomy and axillary lymph node dissection: a randomized controlled study. Anaesthesiol Intensive Ther. 2022;54(1):48 55. ( 10.5114/ait.2022.114203) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Blanco R, Parras T, McDonnell JG, Prats-Galino A. Serratus plane block: a novel ultrasound-guided thoracic wall nerve block. Anaesthesia. 2013;68(11):1107 1113. ( 10.1111/anae.12344) [DOI] [PubMed] [Google Scholar]
- 51. Liu X, Song T, Xu HY, Chen X, Yin P, Zhang J. The serratus anterior plane block for analgesia after thoracic surgery: a meta-analysis of randomized controlled trails. Med (Baltim). 2020;99(21):e20286. ( 10.1097/MD.0000000000020286) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Chin KJ. Thoracic wall blocks: from paravertebral to retrolaminar to serratus to erector spinae and back again - a review of evidence. Best Pract Res Clin Anaesthesiol. 2019;33(1):67 77. ( 10.1016/j.bpa.2019.02.003) [DOI] [PubMed] [Google Scholar]
- 53. Blanco R, Fajardo M, Parras Maldonado T. Ultrasound description of Pecs II (modified Pecs I): a novel approach to breast surgery. Rev Esp Anestesiol Reanim. 2012;59(9):470 475. ( 10.1016/j.redar.2012.07.003) [DOI] [PubMed] [Google Scholar]
- 54. Grape S, Jaunin E, El-Boghdadly K, Chan V, Albrecht E. Analgesic efficacy of PECS and serratus plane blocks after breast surgery: a systematic review, meta-analysis and trial sequential analysis. J Clin Anesth. 2020;63:109744. ( 10.1016/j.jclinane.2020.109744) [DOI] [PubMed] [Google Scholar]
- 55. Elshanbary AA, Zaazouee MS, Darwish YB.et al. Efficacy and safety of pectoral nerve block (pecs) compared with control, paravertebral block, erector spinae plane block, and local anesthesia in patients undergoing breast cancer surgeries: a systematic review and meta-analysis. Clin J Pain. 2021;37(12):925 939. ( 10.1097/AJP.0000000000000985) [DOI] [PubMed] [Google Scholar]
- 56. De Cassai A, Bonanno C, Sandei L, Finozzi F, Carron M, Marchet A. PECS II block is associated with lower incidence of chronic pain after breast surgery. Korean J Pain. 2019;32(4):286 291. ( 10.3344/kjp.2019.32.4.286) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Sertcakacilar G, Kose S. Bilateral PECS II block is associated with decreased opioid consumption and reduced pain scores for up to 24 hours after minimally invasive repair of pectus excavatum (Nuss procedure): a retrospective analysis. J Cardiothorac Vasc Anesth. 2022;36(10):3833 3840. ( 10.1053/j.jvca.2022.06.001) [DOI] [PubMed] [Google Scholar]
- 58. Luo G, Zhu J, Ni H.et al. Pretreatment with pectoral nerve block II is effective for reducing pain in patients undergoing thoracoscopic lobectomy: a randomized, double-blind, placebo-controlled trial. BioMed Res Int. 2021;2021:6693221. ( 10.1155/2021/6693221) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Aydin ME, Ahiskalioglu A, Ates I.et al. Efficacy of ultrasound-guided transversus thoracic muscle plane block on postoperative opioid consumption after cardiac surgery: a prospective, randomized, double-blind study. J Cardiothorac Vasc Anesth. 2020;34(11):2996 3003. ( 10.1053/j.jvca.2020.06.044) [DOI] [PubMed] [Google Scholar]
- 60. Aydin ME, Medetoglu EN, Yazici K, Colak A, Ahiskalioglu A. A combination of serratus and transverse thoracic muscle plane blocks as the main anesthetic method for a high-risk patient with pericardial tamponade. J Clin Anesth. 2021;71:110204. ( 10.1016/j.jclinane.2021.110204) [DOI] [PubMed] [Google Scholar]
- 61. Ahiskalioglu A, Kucun T, Yayik AM, Ulas AB, Ates İ. Ultrasound-guided transversus thoracis muscle plane block provides effective postoperative analgesia for pediatric open pectus carinatum surgery: first report. Pain Med. 2021;22(5):1233 1235. ( 10.1093/pm/pnaa250) [DOI] [PubMed] [Google Scholar]
- 62. Song WQ, Wang W, Yang YC.et al. Parasternal intercostal block complementation contributes to postoperative pain relief in modified radical mastectomy employing pectoral nerve block I and serratus-intercostal block: a randomized trial. J Pain Res. 2020;13:865 871. ( 10.2147/JPR.S237435) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Roberts M, Brodribb W, Mitchell G. Reducing the pain: a systematic review of postdischarge analgesia following elective orthopedic surgery. Pain Med. 2012;13(5):711 727. ( 10.1111/j.1526-4637.2012.01359.x) [DOI] [PubMed] [Google Scholar]
- 64. Hussain N, Goldar G, Ragina N, Banfield L, Laffey JG, Abdallah FW. Suprascapular and interscalene nerve block for shoulder surgery: a systematic review and meta-analysis. Anesthesiology. 2017;127(6):998 1013. ( 10.1097/ALN.0000000000001894) [DOI] [PubMed] [Google Scholar]
- 65. Bos EME, Hollmann MW, Lirk P. Safety and efficacy of epidural analgesia. Curr Opin Anaesthesiol. 2017;30(6):736 742. ( 10.1097/ACO.0000000000000516) [DOI] [PubMed] [Google Scholar]
- 66. Kim KS, Ahn JH, Yoon JH, Ji HT, Kim IS. Hemidiaphragmatic paresis following interscalene brachial plexus block with 2-point injection technique. Pain Phys. 2021;24(8):507 515. [PubMed] [Google Scholar]
- 67. De Cassai A, Bonvicini D, Correale C, Sandei L, Tulgar S, Tonetti T. Erector spinae plane block: a systematic qualitative review. Minerva Anestesiol. 2019;85(3):308 319. ( 10.23736/S0375-9393.18.13341-4) [DOI] [PubMed] [Google Scholar]
- 68. Tulgar S, Ahiskalioglu A, Thomas DT, Gurkan Y. Should erector spinae plane block applications be standardized or should we revise nomenclature? Reg Anesth Pain Med. 2020;45(4):318 319. ( 10.1136/rapm-2019-100910) [DOI] [PubMed] [Google Scholar]
- 69. Ahiskalioglu A, Tulgar S, Celik M, Ozer Z, Alici HA, Aydin ME. Lumbar erector spinae plane block as a main anesthetic method for hip surgery in high risk elderly patients: initial experience with a magnetic resonance imaging. Eurasian J Med. 2020;52(1):16 20. ( 10.5152/eurasianjmed.2020.19224) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Ciftci B, Ekinci M, Gölboyu BE.et al. High thoracic erector spinae plane block for arthroscopic shoulder surgery: a randomized prospective double-blind study. Pain Med. 2021;22(4):776 783. ( 10.1093/pm/pnaa359) [DOI] [PubMed] [Google Scholar]
- 71. Ekinci M, Ciftci B, Atalay YO. An alternative technique for effective pain management in upper extremity surgery: erector spinae plane block. Minerva Anestesiol. 2020;86(3):358 360. ( 10.23736/S0375-9393.19.14080-1) [DOI] [PubMed] [Google Scholar]
- 72. Hamadnalla H, Elsharkawy H, Shimada T, Maheshwari K, Esa WAS, Tsui BCH. Cervical erector spinae plane block catheter for shoulder disarticulation surgery. Can J Anaesth. 2019;66(9):1129 1131. ( 10.1007/s12630-019-01421-9) [DOI] [PubMed] [Google Scholar]
- 73. Forero M, Rajarathinam M, Adhikary SD, Chin KJ. Erector spinae plane block for the management of chronic shoulder pain: a case report. Can J Anaesth. 2018;65(3):288 293. ( 10.1007/s12630-017-1010-1) [DOI] [PubMed] [Google Scholar]
- 74. Ma W, Sun L, Ngai L.et al. Motor-sparing high-thoracic erector spinae plane block for proximal humerus surgery and total shoulder arthroplasty surgery: clinical evidence for differential peripheral nerve block? Can J Anaesth. 2019;66(10):1274 1275. ( 10.1007/s12630-019-01442-4) [DOI] [PubMed] [Google Scholar]
- 75. Diwan S, Nair A. Erector spinae plane block for proximal shoulder surgery: a phrenic nerve sparing block! Turk J Anaesthesiol Reanim. 2020;48(4):331 333. ( 10.5152/TJAR.2019.55047) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Kapukaya F, Ekinci M, Ciftci B.et al. Erector spinae plane block vs interscalene brachial plexus block for postoperative analgesia management in patients who underwent shoulder arthroscopy. BMC Anesthesiol. 2022;22(1):142. ( 10.1186/s12871-022-01687-5) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Townsend D, Siddique N, Kimura A.et al. Lumbar erector spinae plane block for total hip arthroplasty comparing 24-hour opioid requirements: a randomized controlled study. Anesthesiol Res Pract. 2022;2022:9826638. ( 10.1155/2022/9826638) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Chan A, Ng TKT, Tang BYH. Single-shot lumbar erector spinae plane block in total hip replacement: a randomized clinical trial. Anesth Analg. 2022;135(4):829 836. ( 10.1213/ANE.0000000000006162) [DOI] [PubMed] [Google Scholar]
- 79. Kose SG, Kose HC, Tulgar S, Akkaya T. Deep supraspinatus muscle plane block: a novel ultrasound-guided technique for the blockade of suprascapular nerve branches. J Clin Anesth. 2021;70:110187. ( 10.1016/j.jclinane.2021.110187) [DOI] [PubMed] [Google Scholar]
- 80. Ciftci B, Ahiskalioglu A, Ekinci M, Alici HA. Deep supraspinatus muscle plane block: is it just a new description of an old technique? J Clin Anesth. 2021;73:110333. ( 10.1016/j.jclinane.2021.110333) [DOI] [PubMed] [Google Scholar]
- 81. Kose SG, Kose HC, Tulgar S, Thomas DT, Akkaya T. Radiological evaluation and unexpected sensorial block in a patient undergoing ultrasound-guided deep supraspinatus muscle plane block. J Clin Anesth. 2021;71:110248. ( 10.1016/j.jclinane.2021.110248) [DOI] [PubMed] [Google Scholar]
- 82. Altiparmak B, Ciftci B, Tekin B, Sakul BU, Alici HA. Is the deep supraspinatus muscle plane block and suprascapular nerve block the same approach? A cadaveric nomenclature study. Korean J Anesthesiol. 2022;75(2):193 195. ( 10.4097/kja.21513) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Altıparmak B, Korkmaz Toker M, Uysal Aİ, Akgün G, Gümüş Demirbilek S. Deep supraspinatus muscle plane block: a new indication for the novel block. J Clin Anesth. 2021;72:110291. ( 10.1016/j.jclinane.2021.110291) [DOI] [PubMed] [Google Scholar]
- 84. Öksüz G, Arslan M, Bilal B, Gişi G, Yavuz C, Çalışır F. Ultrasound-guided deep supraspinatus muscle plane block for rescue analgesia after shoulder surgery. J Clin Anesth. 2021;71:110247. ( 10.1016/j.jclinane.2021.110247) [DOI] [PubMed] [Google Scholar]
- 85. Ekinci M, Ciftci B, Gölboyu BE, Demiraran Y, Bayrak Y, Tulgar S. A randomized trial to compare serratus anterior plane block and erector spinae plane block for pain management following thoracoscopic surgery. Pain Med. 2020;21(6):1248 1254. ( 10.1093/pm/pnaa101) [DOI] [PubMed] [Google Scholar]
- 86. Demir U, Yayik AM, Köse M, Aydin ME, Ates İ, Ahiskalioglu A. Does the serratus plane block added to the interscalene block improve the quality of anesthesia in arthroscopic shoulder surgery? A prospective randomized study. Cureus. 2020;12(4):e7648. ( 10.7759/cureus.7648) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Girón-Arango L, Peng PWH, Chin KJ, Brull R, Perlas A. Pericapsular nerve group (PENG) block for hip fracture. Reg Anesth Pain Med. 2018;43(8):859 863. ( 10.1097/AAP.0000000000000847) [DOI] [PubMed] [Google Scholar]
- 88. Yamak Altinpulluk E, Galluccio F, Salazar C.et al. Peng block in prosthetic hip replacement: a cadaveric radiological evaluation. J Clin Anesth. 2020;65:109888. ( 10.1016/j.jclinane.2020.109888) [DOI] [PubMed] [Google Scholar]
- 89. Ahiskalioglu A, Aydin ME, Celik M, Ahiskalioglu EO, Tulgar S. Can high volume pericapsular nerve group (PENG) block act as a lumbar plexus block? J Clin Anesth. 2020;61:109650. ( 10.1016/j.jclinane.2019.109650) [DOI] [PubMed] [Google Scholar]
- 90. Ahiskalioglu A, Aydin ME, Ahiskalioglu EO, Tuncer K, Celik M. Pericapsular nerve group (PENG) block for surgical anesthesia of medial thigh. J Clin Anesth. 2020;59:42 43. ( 10.1016/j.jclinane.2019.06.021) [DOI] [PubMed] [Google Scholar]
- 91. Ciftci B, Ahiskalioglu A, Altintas HM, Tekin B, Sakul BU, Alici HA. A possible mechanism of motor blockade of high volume pericapsular nerve group (PENG) block: a cadaveric study. J Clin Anesth. 2021;74:110407. ( 10.1016/j.jclinane.2021.110407) [DOI] [PubMed] [Google Scholar]
- 92. Jones MR, Novitch MB, Hall OM.et al. Fascia iliaca block, history, technique, and efficacy in clinical practice. Best Pract Res Clin Anaesthesiol. 2019;33(4):407 413. ( 10.1016/j.bpa.2019.07.011) [DOI] [PubMed] [Google Scholar]
- 93. Hebbard P, Ivanusic J, Sha S. Ultrasound-guided supra-inguinal fascia iliaca block: a cadaveric evaluation of a novel approach. Anaesthesia. 2011;66(4):300 305. ( 10.1111/j.1365-2044.2011.06628.x) [DOI] [PubMed] [Google Scholar]
- 94. Aliste J, Layera S, Bravo D.et al. Randomized comparison between pericapsular nerve group (PENG) block and suprainguinal fascia iliaca block for total hip arthroplasty. Reg Anesth Pain Med. 2021;46(10):874 878. ( 10.1136/rapm-2021-102997) [DOI] [PubMed] [Google Scholar]
- 95. Nassar H, Hasanin A, Sewilam M.et al. Transmuscular quadratus lumborum block versus suprainguinal fascia iliaca block for hip arthroplasty: a randomized, controlled pilot study. Local Reg Anesth. 2021;14:67 74. ( 10.2147/LRA.S308964) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Sanllorente-Sebastián R, Arroyo-García B, Avello-Taboada R. Ultrasound suprainguinal fascia iliaca block in knee surgery. J Anesth. 2020;34(3):476. ( 10.1007/s00540-020-02754-2) [DOI] [PubMed] [Google Scholar]
- 97. Aksu C, Gürkan Y. Suprainguinal fascia iliaca block for pediatric hip surgeries. Reg Anesth Pain Med. 2019. ( 10.1136/rapm-2019-100520) [DOI] [PubMed] [Google Scholar]
- 98. Alrayashi W, Zurakowski D, Sullivan CA.et al. The effect of suprainguinal fascia iliaca block on the recovery of patients after arthroscopic hip surgery. Paediatr Anaesth. 2019;29(8):829 834. ( 10.1111/pan.13663) [DOI] [PubMed] [Google Scholar]
- 99. Jadon A, Mohsin K, Sahoo RK, Chakraborty S, Sinha N, Bakshi A. Comparison of supra-inguinal fascia iliaca versus pericapsular nerve block for ease of positioning during spinal anaesthesia: a randomised double-blinded trial. Indian J Anaesth. 2021;65(8):572 578. ( 10.4103/ija.ija_417_21) [DOI] [PMC free article] [PubMed] [Google Scholar]



 Content of this journal is licensed under a
Content of this journal is licensed under a