Abstract
Cell surface molecules that can act as virus receptors may exert an important selective pressure on RNA viral quasispecies. Large population passages of foot-and-mouth disease virus (FMDV) in cell culture select for mutant viruses that render dispensable a highly conserved Arg-Gly-Asp (RGD) motif responsible for integrin receptor recognition. Here, we provide evidence that viability of recombinant FMDVs including a Asp-143→Gly change at the RGD motif was conditioned by a number of capsid substitutions selected upon FMDV evolution in cell culture. Multiply passaged FMDVs acquired the ability to infect human K-562 cells, which do not express integrin αvβ3. In contrast to previously described cell culture-adapted FMDVs, the RGD-independent infection did not require binding to the surface glycosaminoglycan heparan sulfate (HS). Viruses which do not bind HS and lack the RGD integrin-binding motif replicate efficiently in BHK-21 cells. Interestingly, FMDV mutants selected from the quasispecies for the inability to bind heparin regained sensitivity to inhibition by a synthetic peptide that represents the G-H loop of VP1. Thus, a single amino acid replacement leading to loss of HS recognition can shift preferential receptor usage of FMDV from HS to integrin. These results indicate at least three different mechanisms for cell recognition by FMDV and suggest a potential for this virus to use multiple, alternative receptors for entry even into the same cell type.
RNA viruses mutate at rates of 10−3 to 10−5 misincorporations per nucleotide copied; as a consequence, they evolve as complex mutant distributions termed viral quasispecies (17, 19, 34, 35, 51, 52, 54). Evolution of RNA viral quasispecies does not occur by the steady accumulation of mutations as replication proceeds but rather proceeds as the outcome of population disequilibrium in response to population size variations and environmental modifications. This is reflected in frequent fitness variations of RNA viruses as they replicate in cell culture or in vivo (3, 12, 18, 27, 29, 33, 42, 64; reviewed in reference 16). Perturbation of equilibrium may lead to the rapid dominance of subsets of variants which were previously present at low frequency in the mutant spectrum. Expression at the cell surface of particular molecules which can act as receptors or coreceptors for the virus may have a major influence on the mutant distributions in viral quasispecies.
Foot-and-mouth disease virus (FMDV) has been used in our laboratory as a model system to study viral quasispecies evolution, including the molecular basis of fitness variations (21, 22) and changes in host cell tropism (3, 20). FMDV is an important animal pathogen that belongs to the aphthovirus genus of the Picornaviridae family (5, 55) and infects cattle and other cloven-hooved animals (artiodactyls) (2, 9). Integrin αvβ3 was the first molecule identified as a primary receptor for FMDV (4, 6, 24, 38). Recent evidence suggests that integrin αvβ3 is the functional receptor for FMDV infections of cattle (50). The integrin receptor recognition site includes a highly conserved Arg-Gly-Asp (RGD) triplet located on the highly mobile, exposed G-H loop of capsid protein VP1 (1, 30, 39, 41). Interestingly, this loop is also a major antigenic site for the virus (7, 53, 60; reviewed in reference 45). Studies of site-directed mutagenesis of infectious cDNA copies of the FMDV genome (40, 44, 49), inhibition of infectivity by synthetic peptides (48), and binding of antibodies to substituted peptides (63) have defined those amino acid residues which are involved in cell receptor recognition and antibody binding. In FMDV of serotype C (clone C-S8c1, derived from natural isolate C-Sta Pau Sp/70 [59]), the RGD motif is directly involved in both integrin recognition (30, 48) and binding of several neutralizing antibodies (31, 56, 61–63). In spite of being subjected to strong selective pressure by antibodies, the RGD triplet was invariant among natural FMDV isolates, in populations of FMDV C-S8c1 subjected to intense selection by neutralizing antibodies (8), and among 81 monoclonal antibody (MAb) escape mutants of FMDV C-S8c1 (43, 46, 47). In contrast, a viral population resulting from 100 serial cytologic passages of FMDV C-S8c1, termed FMDV C-S8c1p100, generated an altered repertoire of MAb-resistant (MAR) mutants that included variants with substitutions at the RGD motif (43, 56).
Cell surface heparan sulfate (HS) can substitute for FMDV integrin receptor, and FMDV variants with improved affinity for heparin are frequently selected after propagation in cell culture (3, 37, 50, 57). Very recently, the crystallographic structure of the FMDV capsid of serotype O1 complexed with heparin has been determined (25). Interaction with heparin often involves the acquisition of positively charged residues on the viral capsid (3, 25, 57).
In this study, we used a collection of natural and engineered FMDVs to provide evidence that some FMDV variants lacking the RGD necessitate additional capsid substitutions for infectivity and that they must use some alternative entry pathway which requires an interaction with neither integrin αvβ3 nor HS. The results suggest the potential use of at least three alternative receptors for entry of FMDV into the same cell type.
MATERIALS AND METHODS
Cells and viruses.
The origins of baby hamster kidney 21 (BHK-21) and Chinese hamster ovary (CHO) cell lines used in this study have been previously described (13, 15, 59). Human K-562 erythroleukemia cells were kindly provided by M. Fresno. BHK-21 cells were grown in Dulbecco's modified Eagle's medium (DMEM) (Gibco) supplemented with nonessential amino acids (Gibco) and 5% fetal calf serum (Gibco). K-562 cells were grown as suspension cultures in the same medium but in the presence of 10% fetal calf serum.
FMDV C-S8c1 is a plaque-purified derivative of the European serotype C natural isolate C1 Santa Pau-Spain 70 (59). FMDV C-S8c1p100c10 is a plaque-purified clone derived from a population obtained after 100 serial cytolytic passages of C-S8c1 in BHK-21 cells (C-S8c1p100) described in reference 43. FMDV C-S8c1p100RGG is a C-S8c1p100-derived MAR mutant with an Asp-143→Gly change at the integrin recognition Arg-Gly-Asp motif (43). FMDV C-S8c1p100c10 and C-S8c1p100 RGG differ only in one amino acid (VP1 position 143) in their capsids. The FMDV C-S8c1 population at passage 213, termed C-S8c1p213, was used to select MARLS, a MAR mutant which includes the alteration Leu-144→Ser in VP1 (13, 46). Procedures for infections of cell monolayers and plaque assays with FMDV have been previously described (15, 59).
Virus growth curves.
FMDV single-step growth curves were determined by infecting BHK-21 cell monolayers (106 cells) at a multiplicity of infection of 5 PFU/cell. Virus was allowed to adsorb at 37°C for 1 h; then monolayers were washed once with 0.1 M phosphate buffer (pH 6.0), washed twice with DMEM, and further incubated in 2 ml of DMEM–2% fetal calf serum. At different times after infection, samples were taken for titration of infectivity on BHK-21 cell monolayers as previously described (59). For K-562 cells growing in suspension, virus adsorption was performed in 250 μl of culture medium (2 × 106 cells) at a multiplicity of infection of 2 PFU/cell, with gentle rocking at 37°C for 1 h. Cells were washed with 0.1 M phosphate buffer (pH 6.0) before further incubation in 2 ml of culture medium. Samples were centrifuged for 5 min at 1,500 × g before titration of infectivity.
cDNA synthesis, PCR amplification, and nucleotide sequencing.
Viral RNA extraction, cDNA synthesis, and reverse transcription-PCR (RT-PCR) amplification were performed as previously described (21). Consensus nucleotide sequences were determined on PCR-amplified DNA either in an automated sequencer (ABI373) or by using a Thermo Sequenase cycle sequencing kit (Amersham). The oligonucleotides used for RT-PCR and nucleotide sequencing have been previously described (3).
Heparin-Sepharose binding assay and selection of FMDV variants with decreased affinity for heparin.
Heparin-Sepharose binding assays and selection of FMDV variants with decreased affinity for heparin were performed as previously described (3).
Construction of full-length cDNA of FMDV O1K encoding type C capsid proteins, in vitro transcription, and cell transfection.
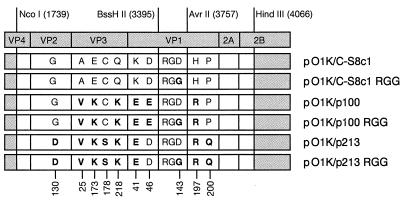
The numbering of FMDV genomic residues is as described in reference 21. The adenosine residue of the first functional AUG initiation codon is at nucleotide 1039; the capsid-coding region spans nucleotides 1642 to 3834. Amino acid residues have been numbered independently for each protein. The procedure used for construction of full-length chimeric cDNAs of FMDV O1K encoding type C capsid proteins was previously described (3). The region transferred to the O1K genetic background spans Ser-33 of VP4 to Lys-62 of protein 2B and corresponds to FMDV genomic positions 1739 and 4066 (NcoI-HindIII fragment) (Fig. 1). The BssHII-AvrII fragment encoding the VP1 G-H loop of FMDV C-S8c1p100RGG (genomic positions 3395 to 3757) was used to substitute an Arg-Gly-Gly (RGG, VP1 positions 141 to 143) sequence for the RGD integrin-binding domain in the FMDV cDNAs (Fig. 1).
FIG. 1.
Schematic representation of the capsid-coding region of chimeric FMDVs. Genomic regions of FMDV of serotype C (white boxes) are inserted in the full-length cDNA of type O1K FMDV (3, 65). Origins of the viruses used for construction of chimeric DNA and procedures employed for the preparation of plasmids are detailed in Materials and Methods. Restriction sites and numbering refer to the C-S8c1 genome (21). Positions at which amino acid residues differ among the compared chimeric genomes are indicated at the bottom. The amino acid sequence of protein VP4 is conserved among the FMDVs of serotypes O and C analyzed here. Boldface letters correspond to amino acid residues which differ from the parental C-S8c1.
In vitro transcription was performed as previously described (3). The RNA concentration was estimated by agarose gel electrophoresis and ethidium bromide staining. RNA transcripts (0.1 to 1 μg) were introduced into BHK-21 cells by the Lipofectin method or by electroporation (37). RNA from chimeric viruses resulting from one round of replication after transfection was retrotranscribed, and the regions encoding the capsid proteins and neighboring genomic regions were sequenced. In all chimeric constructs, the expected nucleotide sequences corresponding to serotype O FMDV were identified in the regions around those encoding the capsid proteins.
Synthetic peptides.
Peptide A15 (YTASARGDLAHLTTT), representing amino acid residues 136 to 150 of the G-H loop of VP1 of C-S8c1, and its variant peptide A15-RGG (YTASARGGLAHLTTT), in which an RGG was substituted for the RGD sequence, were synthesized by solid-phase procedures as described previously (11, 48). The peptides were at least 90% pure as determined by high-performance liquid chromatography. Peptides were dissolved in phosphate-buffered saline containing 1 mM CaCl2 and 0.5 mM MgCl2 at neutral pH, and their concentration was determined by amino acid analysis (48). Assays of inhibition of infectivity by synthetic peptides were carried out essentially as described previously (30, 48).
RESULTS
FMDV replication independent of the RGD in VP1 is conditioned by capsid alterations.
To test the possible requirement of the RGD triplet in cell recognition by FMDV variants of serotype C that differ in the degree of adaptation to BHK-21 cells, a number of chimeric viruses were constructed by cloning the capsid-coding region of FMDV C-S8c1, and of several cell culture-adapted derivatives, into a full-length cDNA of FMDV strain O1K (65). Constructs included viruses with the capsid of C-S8c1 (construct pO1K/C-S8c1), C-S8c1p100 (pO1K/p100), and C-S8c1p213 (pO1K/p213). We constructed a second set of chimeras that were identical to the former set except that they encoded a VP1 G-H loop with RGG instead of RGD; they were named pO1K/C-S8c1RGG, pO1K/p100RGG, and pO1K/p213RGG, respectively (Fig. 1). Production of progeny virus was determined upon transfection of BHK-21 cells with RNA transcripts from each construct. Transfection with RNA transcripts derived from cDNAs pO1K/p100, pO1K/p213, and their corresponding RGG variants resulted in cytopathologic changes at about 24 h posttransfection that were indistinguishable for transcripts expressing RGD or RGG in the G-H loop of VP1. In contrast, cytopathologic changes were observed at about 48 h after transfection with transcripts derived from pO1K/C-S8c1, and no cytopathic effect was observed upon transfection with pO1K/C-S8c1 RGG. Infectivity for BHK-21 cells was confirmed for viral progeny derived from each transfection except in the case of pO1K/C-S8c1 RGG, as expected from the lack of cytopathology. All recombinant progeny maintained their chimeric nature after a second round of replication in BHK-21 cells, as evidenced by RT-PCR amplification of progeny RNA and nucleotide sequencing. Progeny viruses were all neutralized by serotype C-specific MAbs directed to antigenic site D (39). The requirement for infectivity of an RGD triplet in an FMDV capsid with the sequence context of FMDV C-S8c1 was confirmed by a second series of experiments involving electroporation of BHK-21 cells with RNA transcribed from plasmid pO1K/C-S8c1 RGG. When 106 BHK-21 cells were electroporated with 1 μg of RNA, progeny virus was obtained (with a delay of about 24 h with respect to parallel transfections with RNA from pO1K/C-S8c1); it included mutation G-3635→A (amino acid change Gly-143→Asp in VP1), which implied a true reversion to restore the RGD triplet. Identical reversion was obtained upon electroporation of a pO1K/C-S8c1RGG variant which included mutation G-3067→A (amino acid replacement Glu-173→Lys in VP3). This marker mutation was maintained in the RGD-containing revertant progeny, ruling out possible contamination artifacts in the rescuing of infectious virus. These results suggest that Asp-143→Gly is lethal in the sequence context of the capsid of C-S8c1 but not in the context of the capsid of C-S8c1p100 or C-S8c1p213.
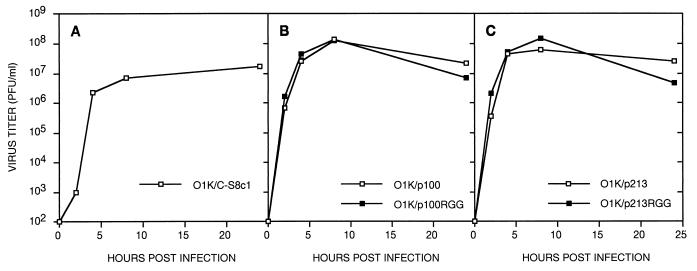
The replication capacity of FMDV recombinants O1K/p100 and O1K/p213 was indistinguishable from that of the corresponding mutants lacking the RGD motif (Fig. 2). Variants with the capsid of multiply passaged FMDV reached titers about 10-fold higher than that of FMDV O1K/C-S8c1. The presence of RGG sequence characterizing recombinant FMDV variants O1K/p100RGG and O1K/p213RGG was confirmed by sequencing of the viral genomes collected at 24 h postinfection. These results suggest that the presence of RGG instead of RGD in C-S8c1p100 or C-S8c1p213 does not affect significantly the infectivity of these viruses for BHK-21 cells.
FIG. 2.
Replication of recombinant FMDV variants in BHK-21 cells. Monolayers of BHK-21 cells were infected with chimeric viruses harboring the capsid of C-S8c1 (A), C-S8c1p100 and its RGG derivative (B), or C-S8c1p213 and its RGG derivative (C) at a multiplicity of infection of 5 PFU per cell. Procedures for the infection in liquid culture and titration of infectivity are described in Materials and Methods. Each value represents the mean of triplicate assays.
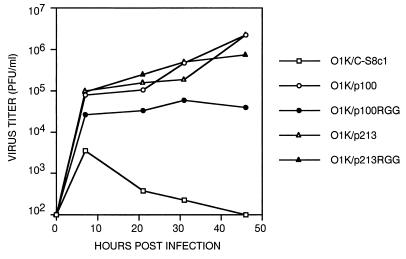
Replication of recombinant FMDV variants in K-562 cells.
Human K-562 erythroleukemia cells express undetectable levels of integrin αvβ3 (14) and are resistant to FMDV infection unless cells are transfected with cDNAs encoding this integrin (50). K-562 cells failed to sustain the replication of FMDV O1K/C-S8c1 (viral titers of <103 PFU/ml at 20 to 40 h postinfection). In contrast, FMDV O1K/C-S8c1p100 and O1K/C-S8c1p213, either the version with RGD or the version with RGG, replicated in K-562 cells, with viral titers in the range of 5 × 104 to 1 × 106 PFU/ml at 20 to 40 h postinfection (Fig. 3). This result suggests that multiply passaged FMDV C-S8c1p100 and C-S8c1p213 replicate without the need of integrin αvβ3.
FIG. 3.
Replication of recombinant FMDV variants in K-562 cells. Cells were infected with the indicated chimeric viruses at a multiplicity of infection of 2 PFU per cell. Procedures for infection of the suspension cultures and titration of infectivity are described in Materials and Methods. Each value represents the mean of duplicate assays.
Binding to HS is not required for cell recognition by type C FMDV variants that lack the RGD motif.
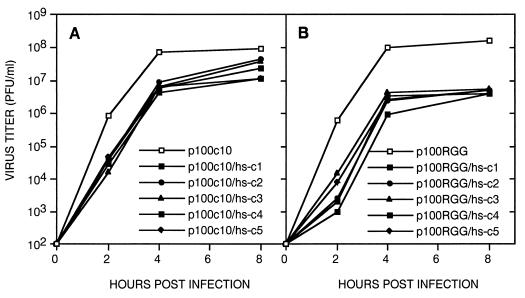
Recent evidence suggests that adaptation of FMDV to cell culture conditions results in the selection of variant viruses able to utilize the glycosaminoglycan HS as an alternative receptor molecule (3, 37, 50, 57). To determine the implication of HS glycosaminoglycan in cell recognition by FMDV mutants that lack the RGD motif, variant viruses with decreased affinity for heparin were selected from FMDV populations C-S8c1p100c10 and C-S8c1p100RGG. After five rounds of selection for negative binding to heparin-Sepharose beads (3), five FMDV clones unable to bind heparin were isolated from each subpopulation, and their capsid-coding regions were sequenced. Loss of heparin binding in C-S8c1p100c10 was associated with a single amino acid replacement which was either Lys-173→Glu in VP3 (two clones, including c1) or Arg-197→His at the C-terminal region of VP1 (three clones). Loss of heparin binding in C-S8c1p100RGG was associated with the Lys-173→Glu change in VP3 in each of the five clones analyzed. The two amino acid substitutions involved in loss of heparin binding were mediated by true reversions of two mutations (A-3067→G in the VP3-coding region and G-3797→A in the VP1-coding region) that had been acquired by FMDV C-S8c1 in the course of 100 serial passages in BHK-21 cells (Fig. 1). FMDV C-S8c1p100RGG/hs-c1 infected wild-type and mutant pgsA-745 and pgsD-677 CHO cells, with viral titers reaching 104 PFU/ml in all cases. Viral yields were 103-fold lower than those produced by the parental virus able to bind heparin, but the difference was independent of the expression of HS in the CHO cells. Upon infection of BHK-21 cells, the viral yield by clones which were defective in heparin binding was only 2- to 15-fold lower than the yield of their corresponding parental C-S8c1p100c10 and C-S8c1p100RGG populations (Fig. 4). The presence of the RGD or RGG motif and of the mutations associated with loss of heparin binding was confirmed by RT-PCR amplification and nucleotide sequencing of the RNA of progeny virus at 8 h postinfection. Likewise, none of the progeny from infections with five C-S8c1p100RGG/hs− clones regained binding to heparin. As expected, the progeny of the parental C-S8c1p100 RGG maintained its heparin binding. Therefore, high FMDV yields can be produced in BHK-21 cells by FMDV that binds neither to integrin αvβ3 nor to HS.
FIG. 4.
Replication in BHK-21 cells of FMDV clones unable to bind heparin. p100c10 and p100RGG denote FMDV C-S8c1p100c10 and C-S8c1p100RGG, respectively; their origins are described in Materials and Methods. The five clones selected for the inability to bind heparin, termed hs-c1 through hs-c5, were selected as detailed in the text (3). Infections of BHK-21 cell monolayers were carried out at a multiplicity of infection of 5 PFU per cell. Procedures for infection in liquid culture and titration of infectivity are described in Materials and Methods. One representative experiment of three is shown for the parental p100c10 and p100RGG viruses.
Evidence for flexibility in FMDV receptor recognition.
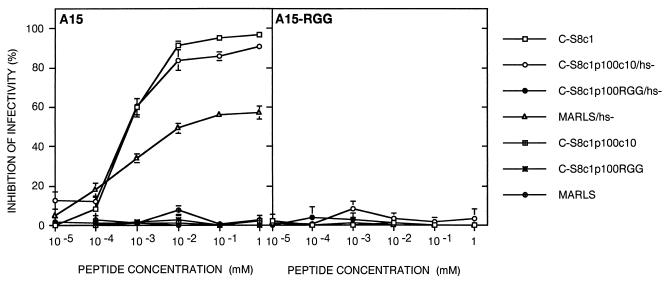
Synthetic peptides representing the G-H loop of VP1 of FMDV C-S8c1 are strong inhibitors of the infectivity of C-S8c1 for BHK-21 cells, presumably by competing with virus for binding to an integrin receptor (30, 48). Peptide A15, representing VP1 positions 136 to 150 of C-S8c1, did not inhibit the infectivity of C-S8c1p100c10 or C-S8c1p100RGG (Fig. 5). Interestingly, partial inhibition of infectivity by peptide A15 was observed with clones from C-S8c1p100c10 deficient in heparin binding. The clonal populations used were those harboring the single amino acid replacement (Lys-173 → Glu in VP3) associated with loss of heparin binding, as determined by nucleotide sequencing of the capsid-coding region. The inhibition reached 90%, approaching the maximum inhibition of infectivity attained with C-S8c1 in parallel assays (50% inhibitory concentration of ≈1 μM). In contrast, no inhibition by peptide A15 was observed with clones deficient in heparin binding derived from C-S8c1p100RGG. None of the variants tested were inhibited by a variant version of peptide A15 which included RGG instead of RGD in its sequence (Fig. 5). The ability to regain sensitivity to inhibition by peptide A15 concurrently with loss of heparin-binding capacity is not unique to FMDV C-S8c1p100; it was also noted with a heparin binding-deficient clone selected from FMDV MARLS, a MAR mutant isolated from population FMDV C-S8c1p213 described previously (3). In the case of MARLS, however, the maximum inhibition by peptide A15 was 58% (Fig. 5). These results suggest that FMDV capsid structures selected upon propagation on BHK-21 cells have retained the ability to interact with their integrin receptor in an RGD-dependent manner and are able to switch to integrin use when their HS binding pathway is impeded. Internalization of FMDV RGG variants involves a mechanism which does not implicate integrin αvβ3 or HS for cell recognition and entry. Thus, FMDV can use multiple alternative receptor molecules for infection of cells, and even for one defined cell type it may shift to using one receptor class when the use of another receptor is inhibited.
FIG. 5.
Inhibition of FMDV infectivity by peptides A15 and A15 with RGG instead of RGD. The amino acid sequences of peptides A15 and A15-RGG are given in Materials and Methods. BHK-21 cell monolayers (about 5 × 105 cells) were treated with the indicated concentration of peptide A15 or A15-RGG for 45 min at room temperature and further incubated in the presence of FMDV (50 to 150 PFU) for 45 min at 37°C. The monolayers were washed with 0.1 M phosphate buffer (pH 6.0) and overlaid with agar containing medium as described in Materials and Methods. The FMDVs used in different experiments are listed in the right; hs- denotes a clone selected for its inability to bind heparin. Origins of the viruses and procedures for selection of clones and infectivity assays are described in Materials and Methods. Each value is the average of three determinations. Standard deviations are indicated.
DISCUSSION
The RGD integrin-binding motif is highly conserved among representatives of the aphthovirus genus, and isolates of each FMDV serotype were found to bind purified integrin αvβ3 in an RGD-dependent manner (38). Evidence of integrin molecules being involved in the internalization of FMDV was initially provided by peptide inhibition experiments (4, 24) and then by inhibition of infectivity by antibodies to αvβ3 (6), and the use of cell lines modified to express αvβ3 (50). In spite of virus-integrin interaction being essential for the infectivity of FMDV isolated from cattle (50), FMDV harbors the evolutionary potential to render dispensable the RGD motif upon replication in cell culture (43). FMDV populations propagated in BHK-21 cells may generate a different repertoire of antigenic variants, including some with substitutions at the RGD motif (43, 58). In the present study, we have constructed infectious FMDV clones to document that dispensability of the RGD motif is conditioned to a number of amino acid replacements in the FMDV capsid. The Asp-143→Gly change was lethal in the context of the capsid proteins of C-S8c1, while the same replacement yielded viable viruses in the context of the capsid protein of C-S8c1p100 and C-S8c1p213. Therefore, it was the amino acid replacements in the viral capsid (Fig. 1) selected upon serial passages of FMDV C-S8c1 in BHK-21 cells that enabled the virus to find an alternative pathway for entry into cells and to render the RGD nonessential for infectivity. In the electroporation experiments, an average of 105 RNA molecules were introduced per BHK-21 cell, allowing revertants to arise in all experiments. Since the progeny from the electroporation was distinct from the input genome, the FMDV RNAs encoding RGG behave as quasi-infectious genomes, as defined by Gmyl et al. (26; reviewed in reference 28).
The capsid of FMDV C-S8c1p100 or C-S8c1p213, but not that of the parental C-S8c1, enabled virus replication in K-562 cells which do not express integrin αvβ3 (14). Thus, other cell surface molecules such as HS (50) must act as receptors for the FMDVs adapted to BHK-21 cells. RGD-mediated interactions of FMDV capsid with α5β1 or other integrin molecules expressed at the surface of K-562 cells (14) could be partially responsible for FMDV internalization in this particular cell line and perhaps also for a limited viral production seen in infections with O1K/C-S8c1 (Fig. 3). Yet the absence of detectable differences between virus production on K-562 cells by recombinant variants differing only at the RGD sequence suggests that recognition of K-562 cells by FMDV occurs mainly through RGD-independent mechanisms.
Binding to heparin is a phenotypic trait that characterizes many cell culture-adapted FMDV variants, and virus interaction with cell surface HS may constitute a major step toward FMDV adaptation to cell culture (3, 37, 50, 57). However, several lines of evidence obtained with FMDV of serotype C support the existence of alternative pathways for FMDV adaptation to cells in culture. We previously reported that variants that were highly adapted to BHK-21 cells, including C-S8c1p100RGG, displayed enhanced affinity for heparin, but unexpectedly, binding to cell surface HS was not required for efficient replication in glycosaminoglycan-deficient CHO cells (3). In the present study, we have shown that biological selection allowed a complete reversion of the heparin-binding phenotype of FMDV variants that lack the RGD motif. These variants infected cells via a mechanism which is independent of integrin αvβ3 or HS. These results imply the existence of at least three different pathways for entry of FMDV into host cells. It is noteworthy that while the multiply passaged FMDVs used HS as a receptor, they maintained the potential to interact and use integrin αvβ3 as a receptor (Fig. 5). The potential for simultaneous use of at least three alternative receptors for entry into the same cell types confers functional flexibility on FMDV to modulate receptor usage in response to environmental modifications (differential expression of the various types of receptors on cells, blocking of receptor recognition by antibody binding, presence of inhibitors of one of the alternative entry pathways, etc.). It must be emphasized that not only can genetic changes in the virus prompt usage of one receptor in preference over another receptor, but the same capsid may be driven to use one or another entry pathway.
There is increasing evidence that picornaviruses, as well as many other RNA viruses, may use a number of alternative receptors for attachment and entry into cells (10, 23, 32, 36). The results of expansion of receptor usage of FMDV C-S8c1 reported here pose a number of interesting questions. One relates to neutralization by antibodies which bind to the RGD motif (13, 43, 61, 63) of viruses which do not use integrin αvβ3 as their receptor. A number of possible mechanisms are now under investigation.
The dispensability of the RGD as a receptor recognition triplet may greatly expand the repertoire of antigenic variants mapping within site A of FMDV. In addition to a number of replacements previously identified among MAb-resistant mutants of C-S8c1p100 (43), we have recently identified highly unusual variants including one with a GGG triplet instead of the RGD (56). This suggests that viruses which use the same surface site for receptor recognition and antibody binding harbor the potential of coevolution of cell tropism and antigenicity and may undergo expansions of the repertoire of antigenic variants when the site ceases to be essential for entry into the cell. Finally, several multiply passaged FMDVs display an expanded host range, exemplified by the acquisition of infectivity for CHO cells (3, 57) and human K-562 cells (50) (Fig. 3). Given the potential relevance of this expansion for FMDV to become a new emergent pathogen for animal species other than artiodactyls, the cell tropism of a number of additional FMDV variants is currently under investigation.
ACKNOWLEDGMENTS
We are indebted to Peter Mason and Barry Baxt for fruitful collaboration and discussions, Cristina Escarmís and Mauricio G. Mateu for valuable suggestions, Wendy F. Ochoa for neutralization experiments, and M. Dávila and G. Gómez Mariano for expert technical assistance.
Work in Madrid was supported by grants PM 97-0060-C02-01, FAIR 5PL97-3665, and Fundación Ramón Areces. E.Baranowski was supported by a postdoctoral fellowship from Ministerio de Educación y Cultura, and C.R.-J. was supported by a fellowship from Comunidad Autónoma de Madrid. Work in Barcelona was supported by grant PB97-0873. A visit of E.Baranowski to Plum Island Animal Disease Center was supported by a fellowship under the OECD Co-Operative Research Programme: Biological Resource Management for Sustainable Agricultural Systems.
REFERENCES
- 1.Acharya R, Fry E, Stuart D, Fox G, Rowlands D, Brown F. The three-dimensional structure of foot-and-mouth disease virus at 2.9 Å resolution. Nature. 1989;337:709–716. doi: 10.1038/337709a0. [DOI] [PubMed] [Google Scholar]
- 2.Bachrach H L. Foot-and-mouth disease virus. Annu Rev Microbiol. 1968;22:201–244. doi: 10.1146/annurev.mi.22.100168.001221. [DOI] [PubMed] [Google Scholar]
- 3.Baranowski E, Sevilla N, Verdaguer N, Ruiz-Jarabo C, Beck E, Domingo E. Multiple virulence determinants of foot-and-mouth disease virus in cell culture. J Virol. 1998;72:6362–6372. doi: 10.1128/jvi.72.8.6362-6372.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Baxt B, Becker Y. The effect of peptides containing the arginine-glycine-aspartic acid sequence on the adsorption of foot-and-mouth disease virus to tissue culture cells. Virus Genes. 1990;4:73–83. doi: 10.1007/BF00308567. [DOI] [PubMed] [Google Scholar]
- 5.Belsham G J. Distinctive features of foot-and-mouth disease virus, a member of the picornavirus family; aspects of virus protein synthesis, protein processing and structures. Prog Biophys Mol Biol. 1993;60:241–260. doi: 10.1016/0079-6107(93)90016-D. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Berinstein A, Roivainen M, Hovi T, Mason P W, Baxt B. Antibodies to the vitronectin receptor (integrin αvβ3) inhibit binding and infection of foot-and-mouth disease virus to cultured cells. J Virol. 1995;69:2664–2666. doi: 10.1128/jvi.69.4.2664-2666.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bittle J L, Houghten R A, Alexander H, Shinnick T M, Sutcliffe J C, Lerner R A, Rowlands D J, Brown F. Protection against foot-and-mouth disease by immunization with a chemically synthesized peptide predicted from the viral nucleotide sequence. Nature. 1982;298:30–33. doi: 10.1038/298030a0. [DOI] [PubMed] [Google Scholar]
- 8.Borrego B, Novella I S, Giralt E, Andreu D, Domingo E. Distinct repertoire of antigenic variants of foot-and-mouth disease virus in the presence or absence of immune selection. J Virol. 1993;67:6071–6079. doi: 10.1128/jvi.67.10.6071-6079.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brown F. Foot-and-mouth disease. In: Nicholson B H, editor. Synthetic vaccines. Oxford, England: Blackwell Scientific Publications; 1994. pp. 416–432. [Google Scholar]
- 10.Byrnes A P, Griffin D E. Binding of Sindbis virus to cell surface heparan sulfate. J Virol. 1998;72:7349–7356. doi: 10.1128/jvi.72.9.7349-7356.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Carreño C, Roig X, Cairo J, Camarero J, Mateu M G, Domingo E, Giralt E, Andreu D. Studies on antigenic variability of C strains of foot-and-mouth disease virus by means of synthetic peptides and monoclonal antibodies. Int J Pept Protein Res. 1992;39:41–47. doi: 10.1111/j.1399-3011.1992.tb01554.x. [DOI] [PubMed] [Google Scholar]
- 12.Carrillo C, Borca M, Moore D M, Morgan D O, Sobrino F. In vivo analysis of the stability and fitness of variants recovered from foot-and-mouth disease virus quasispecies. J Gen Virol. 1998;79:1699–1706. doi: 10.1099/0022-1317-79-7-1699. [DOI] [PubMed] [Google Scholar]
- 13.Charpentier N, Dávila M, Domingo E, Escarmís C. Long-term, large-population passage of aphthovirus can generate and amplify defective noninterfering particles deleted in the leader protease gene. Virology. 1996;223:10–18. doi: 10.1006/viro.1996.0450. [DOI] [PubMed] [Google Scholar]
- 14.Danen E, Aota S-I, van Kraats A, Yamada K, Ruiter D, van Muijen G. Requirement for the synergy site for cell adhesion to fibronectin depends on the activation state of integrin α5β1. J Biol Chem. 1995;270:21612–21618. doi: 10.1074/jbc.270.37.21612. [DOI] [PubMed] [Google Scholar]
- 15.Domingo E, Dávila M, Ortín J. Nucleotide sequence heterogeneity of the RNA from a natural population of foot-and-mouth disease virus. Gene. 1980;11:333–346. doi: 10.1016/0378-1119(80)90073-6. [DOI] [PubMed] [Google Scholar]
- 16.Domingo E, Escarmís C, Menédez-Arias L, Holland J J. Viral quasispecies and fitness variations. In: Domingo E, Webster R G, Holland J J, editors. Origin and evolution of viruses. London, England: Academic Press; 1999. pp. 141–161. [Google Scholar]
- 17.Domingo E, Holland J J. RNA virus mutations and fitness for survival. Annu Rev Microbiol. 1997;51:151–178. doi: 10.1146/annurev.micro.51.1.151. [DOI] [PubMed] [Google Scholar]
- 18.Duarte E, Clarke D, Moya A, Domingo E, Holland J J. Rapid fitness losses in mammalian RNA virus clones due to Muller's ratchet. Proc Natl Acad Sci USA. 1992;89:6015–6019. doi: 10.1073/pnas.89.13.6015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Eigen M, Biebricher C K. Sequence space and quasispecies distribution. In: Domingo E, Holland J J, Ahlquist P, editors. RNA genetics. Vol. 3. Boca Raton, Fla: CRC Press, Inc.; 1988. pp. 211–245. [Google Scholar]
- 20.Escarmís C, Carrillo E C, Ferrer M, García Arriaza J F, López N, Tami C, Verdaguer N, Domingo E, Franze-Fernández M T. Rapid selection in modified BHK-21 cells of foot-and-mouth disease virus variant showing alterations in cell tropism. J Virol. 1998;72:10171–10179. doi: 10.1128/jvi.72.12.10171-10179.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Escarmís C, Dávila M, Charpentier N, Bracho A, Moya A, Domingo E. Genetic lesions associated with Muller's ratchet in an RNA virus. J Mol Biol. 1996;264:255–267. doi: 10.1006/jmbi.1996.0639. [DOI] [PubMed] [Google Scholar]
- 22.Escarmís C, Dávila M, Domingo E. Multiple molecular pathways for fitness recovery of an RNA virus debilitated by operation of Muller's ratchet. J Mol Biol. 1999;285:495–505. doi: 10.1006/jmbi.1998.2366. [DOI] [PubMed] [Google Scholar]
- 23.Evans D J, Almond J W. Cell receptors for picornaviruses as determinant of cell tropism and pathogenesis. Trends Microbiol. 1998;6:198–202. doi: 10.1016/s0966-842x(98)01263-3. [DOI] [PubMed] [Google Scholar]
- 24.Fox G, Parry N, Barnett P V, McGlinn B, Rowlands D J, Brown F. The cell attachment site on foot-and-mouth disease virus includes the amino acid sequence RGD (argine-glycine-aspartic acid) J Gen Virol. 1989;70:625–637. doi: 10.1099/0022-1317-70-3-625. [DOI] [PubMed] [Google Scholar]
- 25.Fry E E, Lea S M, Jackson T, Newman J W, Ellard F M, Blakemore W E, Abu-Ghazaleh R, Samuel A, King A M, Stuart D. The structure and function of a foot-and-mouth disease virus-oligosaccharide receptor complex. EMBO J. 1999;18:543–554. doi: 10.1093/emboj/18.3.543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gmyl A P, Pilipenko E V, Maslova S V, Belov G A, Agol V I. Functional and genetic plasticities of the poliovirus genome: quasi-infectious RNAs modified in the 5′-untranslated region yield a variety of pseudorevertants. J Virol. 1993;67:6309–6316. doi: 10.1128/jvi.67.10.6309-6316.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Goudsmit J, De Ronde A, Ho D, Perelson A S. Human immunodeficiency virus fitness in vivo: calculations based on a single zidovudine resistance mutation at codon 215 of reverse transcriptase. J Virol. 1996;70:5662–5664. doi: 10.1128/jvi.70.8.5662-5664.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gromeier M, Wimmer E, Gorbalenya A E. Genesis, pathogenesis and evolution of picornaviruses. In: Domingo E, Webster R G, Holland J J, editors. Origin and evolution of viruses. London, England: Academic Press; 1999. pp. 287–343. [Google Scholar]
- 29.Harrigan P R, Bloor S, Larder B A. Relative replicative fitness of zidovudine-resistant human immunodeficiency type 1 isolates in vitro. J Virol. 1998;72:3773–3778. doi: 10.1128/jvi.72.5.3773-3778.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hernández J, Valero M L, Andreu D, Domingo E, Mateu M G. Antibody and host cell recognition of foot-and-mouth disease virus (serotype C) cleaved at the Arg-Gly-Asp (RGD) motif: a structural interpretation. J Gen Virol. 1996;77:257–264. doi: 10.1099/0022-1317-77-2-257. [DOI] [PubMed] [Google Scholar]
- 31.Hewat E A, Verdaguer N, Fita I, Blakemore W, Brookes S, King A, Newman J, Domingo E, Mateu M G, Stuart D. Structure of the complex of an Fab fragment of a neutralizing antibody with foot-and-mouth disease virus: positioning of a highly mobile antigenic loop. EMBO J. 1997;16:1492–1500. doi: 10.1093/emboj/16.7.1492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hoffman T L, Stephens E B, Narayan O, Doms R W. HIV type 1 envelope determinants for use of the CCR2b, CCR3, STRL33, and APJ coreceptors. Proc Natl Acad Sci USA. 1998;95:11360–11365. doi: 10.1073/pnas.95.19.11360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Holland J J, de la Torre J C, Clarke D K, Duarte E. Quantitation of relative fitness and great adaptability of clonal populations of RNA viruses. J Virol. 1991;65:2960–2967. doi: 10.1128/jvi.65.6.2960-2967.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Holland J J, de la Torre J C, Steinhauer D A. RNA viral population as quasispecies. Curr Top Microbiol Immunol. 1992;176:1–20. doi: 10.1007/978-3-642-77011-1_1. [DOI] [PubMed] [Google Scholar]
- 35.Holland J J, Spindler K, Horodyski F, Grabau E, Nichol S, Vande Pol S. Rapid evolution of RNA genomes. Science. 1982;215:1577–1585. doi: 10.1126/science.7041255. [DOI] [PubMed] [Google Scholar]
- 36.Hsu E C, Sarangi F, Iorio C, Sidhu M S, Udem S A, Dillehay D L, Xu W, Rota P A, Bellini W J, Richardson C D. A single amino acid change in the hemagglutinin protein of measles virus determines its ability to bind CD46 and reveals another receptor on marmoset B cells. J Virol. 1998;72:2905–2916. doi: 10.1128/jvi.72.4.2905-2916.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Jackson T, Ellard F M, Abu Ghazaleh R, Brookes S M, Blakemore W E, Corteyn A H, Stuart D I, Newman J W, King A M. Efficient infection of cells in culture by type O foot-and-mouth disease virus requires binding to cell surface heparan sulfate. J Virol. 1996;70:5282–5287. doi: 10.1128/jvi.70.8.5282-5287.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Jackson T, Sharma A, Ghazaleh R A, Blakemore W E, Ellard F M, Simmons D L, Newman J W, Stuart D I, King A M. Arginine-glycine-aspartic acid binding by foot-and-mouth disease viruses to the purified integrin αvβ3 in vitro. J Virol. 1997;71:8357–8361. doi: 10.1128/jvi.71.11.8357-8361.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lea S, Hernandez J, Blakemore W, Brocchi E, Curry S, Domingo E, Fry E, Abu-Ghazaleh R, King A, Newman J, Stuart D, Mateu M G. The structure and antigenicity of a type C foot-and-mouth disease virus. Structure. 1994;2:123–139. doi: 10.1016/s0969-2126(00)00014-9. [DOI] [PubMed] [Google Scholar]
- 40.Leippert M, Beck E, Weiland F, Pfaff E. Point mutations within the βG-βH loop of foot-and-mouth disease virus O1K affect virus attachment to target cells. J Virol. 1997;71:1046–1051. doi: 10.1128/jvi.71.2.1046-1051.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Logan D, Abu-Ghazaleh R, Blakemore W, Cyrry S, Jackson T, King A, Lea S, Lewis R, Newman J, Parry N, Rowlands D, Stuart D, Fry E. Structure of a major immunogenic site of foot-and-mouth disease virus. Nature. 1993;362:566–568. doi: 10.1038/362566a0. [DOI] [PubMed] [Google Scholar]
- 42.Martínez M A, Carrillo C, González-Candelas F, Moya A, Domingo E, Sobrino F. Fitness alteration of foot-and-mouth disease virus mutants: measurement of adaptability of viral quasispecies. J Virol. 1991;65:3954–3957. doi: 10.1128/jvi.65.7.3954-3957.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Martínez M A, Verdaguer N, Mateu M G, Domingo E. Evolution subverting essentiality: dispensability of the cell attachment Arg-Gly-Asp motif in multiply passaged foot-and-mouth disease virus. Proc Natl Acad Sci USA. 1997;94:6798–6802. doi: 10.1073/pnas.94.13.6798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Mason P W, Rieder E, Baxt B. RGD sequence of foot-and-mouth disease virus in essential for infecting cells via the natural receptor but can be bypassed and antibody-dependent enhancement pathway. Proc Natl Acad Sci USA. 1994;91:1932–1936. doi: 10.1073/pnas.91.5.1932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Mateu M G. Antibody recognition of picornaviruses and escape from neutralization: a structural view. Virus Res. 1995;38:1–24. doi: 10.1016/0168-1702(95)00048-u. [DOI] [PubMed] [Google Scholar]
- 46.Mateu M G, Martínez M A, Capucci L, Andreu D, Giralt E, Sobrino F, Brocchi E, Domingo E. A single amino acid substitution affects multiple overlapping epitopes in the major antigenic site of foot-and-mouth disease virus of serotype C. J Gen Virol. 1990;71:629–637. doi: 10.1099/0022-1317-71-3-629. [DOI] [PubMed] [Google Scholar]
- 47.Mateu M G, Martínez M A, Rocha E, Andreu D, Parejo J, Giralt E, Sobrino F, Domingo E. Implications of a quasispecies genome structure: effect of frequent, naturally occurring amino acid substitutions on the antigenicity of foot-and-mouth disease virus. Proc Natl Acad Sci USA. 1989;86:5883–5887. doi: 10.1073/pnas.86.15.5883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Mateu M G, Valero M L, Andreu D, Domingo E. Systematic replacement of amino acid residues within an Arg-Gly-Asp-containing loop of foot-and-mouth disease virus: effect on cell recognition. J Biol Chem. 1996;271:12814–12819. doi: 10.1074/jbc.271.22.12814. [DOI] [PubMed] [Google Scholar]
- 49.McKenna T S C, Lubroth J, Reider E, Baxt B, Mason P W. Receptor binding-site-deleted foot-and-mouth disease (FMD) virus protects cattle from FMD. J Virol. 1995;69:5787–5790. doi: 10.1128/jvi.69.9.5787-5790.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Neff S, Carvalho D S, Rieder E, Mason P, Blystone S, Brown E, Baxt B. Foot-and-mouth disease virus virulent for cattle utilizes the integrin αvβ3 as its receptor. J Virol. 1998;72:3587–3594. doi: 10.1128/jvi.72.5.3587-3594.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Novella I S, Duarte E A, Elena S F, Moya A, Domingo E, Holland J J. Exponential increases of RNA virus fitness during large population transmission. Proc Natl Acad Sci USA. 1995;92:5841–5844. doi: 10.1073/pnas.92.13.5841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Nowak M A. What is a quasispecies? Trends Ecol Evol. 1992;7:118–121. doi: 10.1016/0169-5347(92)90145-2. [DOI] [PubMed] [Google Scholar]
- 53.Pfaff E, Mussgay M, Böhm H O, Schultz G E, Schaller H. Antibodies against a preselected peptide recognize and neutralize foot-and-mouth disease virus. EMBO J. 1982;1:869–874. doi: 10.1002/j.1460-2075.1982.tb01262.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Preston B D, Dougherty J P. Mechanisms of retroviral mutation. Trends Microbiol. 1996;4:16–21. doi: 10.1016/0966-842x(96)81500-9. [DOI] [PubMed] [Google Scholar]
- 55.Rueckert R R. Picornaviridae: the viruses and their replication. In: Fields B N, et al., editors. Fields virology. Philadelphia, Pa: Lippincott-Raven Publishers; 1996. pp. 609–654. [Google Scholar]
- 56.Ruiz-Jarabo C M, Sevilla N, Dávila M, Gómez-Mariano G, Baranowski E, Domingo E. Antigenic properties and population stability of a foot-and-mouth disease virus with an altered Arg-Gly-Asp receptor-recognition motif. J Gen Virol. 1999;80:1899–1909. doi: 10.1099/0022-1317-80-8-1899. [DOI] [PubMed] [Google Scholar]
- 57.Sá-Carvalho D, Rieder E, Baxt B, Rodarte R, Tanuri A, Mason P. Tissue culture adaptation of foot-and-mouth disease virus selects viruses that bind to heparin and are attenuated in cattle. J Virol. 1997;71:5115–5123. doi: 10.1128/jvi.71.7.5115-5123.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Sevilla N, Domingo E. Evolution of a persistent aphthovirus in cytolytic infections: partial reversion of phenotypic traits accompanied by genetic diversification. J Virol. 1996;70:6617–6624. doi: 10.1128/jvi.70.10.6617-6624.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Sobrino F, Dávila M, Ortin J, Domingo E. Multiple genetic variants arise in the course of replication of foot-and-mouth disease virus in cell culture. Virology. 1983;128:310–318. doi: 10.1016/0042-6822(83)90258-1. [DOI] [PubMed] [Google Scholar]
- 60.Strohmaier K, Franze R, Adam K H. Location and characterization of the antigenic portion of the FMDV immunizing protein. J Gen Virol. 1982;59:295–306. doi: 10.1099/0022-1317-59-2-295. [DOI] [PubMed] [Google Scholar]
- 61.Verdaguer N, Mateu M G, Andreu D, Giralt E, Domingo E, Fita I. Structure of the major antigen loop of foot-and-mouth disease virus complexed with a neutralizing antibody: direct involvement of the Arg-Gly-Asp motif in the interaction. EMBO J. 1995;14:1690–1696. doi: 10.1002/j.1460-2075.1995.tb07158.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Verdaguer N, Schoehn G, Ochoa W F, Fita I, Brookes S, King A, Domingo E, Mateu M G, Stuart D, Hewat E A. Flexibility of the major antigenic loop of foot-and-mouth disease virus bound to an Fab fragment of a neutralizing antibody: structure and neutralization. Virology. 1999;255:260–268. doi: 10.1006/viro.1998.9554. [DOI] [PubMed] [Google Scholar]
- 63.Verdaguer N, Sevilla N, Valero M L, Stuart D, Brocchi E, Andreu D, Giralt E, Domingo E, Mateu M G, Fita I. A similar pattern of interaction for different antibodies with a major antigenic site of foot-and-mouth disease virus: implication for intratypic antigenic variation. J Virol. 1998;72:739–748. doi: 10.1128/jvi.72.1.739-748.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Zennou V, Mammano F, Paulous S, Mathez D, Clavel F. Loss of viral fitness associated with multiple Gag and Gag-Pol processing defects in human immunodeficiency virus type 1 variants selected for resistance to protease inhibitors in vivo. J Virol. 1998;72:3300–3306. doi: 10.1128/jvi.72.4.3300-3306.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Zibert A, Maass G, Strebel K, Falk M M, Beck E. Infectious foot-and-mouth disease virus derived from a cloned full-length cDNA. J Virol. 1990;64:2467–2473. doi: 10.1128/jvi.64.6.2467-2473.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]