Abstract
Introduction
One possible reason for the rapid proliferation of waterpipe (WP) smoking is the pervasive use of flavoured WP tobacco. To begin to understand the impact of WP tobacco flavours, the current study examined the impact of a preferred WP tobacco flavour compared with a non-preferred tobacco flavoured control on user’s smoking behaviour, toxicant exposure and subjective smoking experience.
Method
Thirty-six current WP smokers completed two, 45-minute ad libitum smoking sessions (preferred flavour vs non-preferred tobacco flavour control) in a randomised cross-over design. Participants completed survey questionnaires assessing subjective smoking experience, exhaled carbon monoxide (eCO) testing, and provided blood samples for monitoring plasma nicotine. WP smoking topography was measured continuously throughout the smoking session.
Results
While participants reported an enhanced subjective smoking experience including greater interest in continued use, greater pleasure derived from smoking, increased liking and enjoyment, and willingness to continue use after smoking their preferred WP tobacco flavour (ps <0.05), no significant differences were observed in nicotine and carbon monoxide boost between flavour preparations. Greater average puff volume (p=0.018) was observed during the nonpreferred flavour session. While not significant, measures of flow rate, interpuff interval (IPI), and total number of puffs were trending towards significance (ps <0.10), with decreased IPI and greater total number of puffs during the preferred flavour session.
Discussion
The current study is the first to examine flavours in WP smoking by measuring preferred versus control preparations to understand the impact on subjective experience, smoking behaviour and toxicant exposure. The pattern of results suggests that even this relatively minor manipulation resulted in significant changes in subjective experience. These results indicate a possible need for regulations restricting flavours in WP tobacco as with combustible cigarettes.
Waterpipe (WP) smoking, also known as shisha, narghile and hookah, is proliferating in the USA and internationally.1 2 From 2011 to 2014, WP smoking rates among emerging adults more than doubled while cigarette smoking rates decreased.1 Some research suggests WP smoking has overtaken cigarettes as the most frequently tried tobacco product among young adults3 with college student ever use rates between 30% and 50%.3–7 WP smoking lounges are likely to be placed close to college campuses and may be marketing specifically to this young adult population.8 Unfortunately, WP smoking is associated with many of the same toxicants and health effects as cigarette smoking.9–15
WP smoking is likely increasing for a number of reasons, including the pervasive belief that WP smoking is safe, particularly compared with cigarette smoking. Research suggests both WP smokers and non-smokers believe WP smoking is safer than cigarette smoking.6 16 Additionally, flavourants in the WP tobacco have likely played an important role in the propagation of WP smoking17 and the misbelief regarding the safety of WP smoking.18 Smokers incorrectly report that compared with unflavoured tobacco, the ‘fruit flavor makes it less harmful’.19
The majority of WP smokers report using flavoured tobacco20 and smokers emphasise the importance of flavours in WP smoking.17 In qualitative research, participants state that flavours in WP tobacco led to their initiation of WP smoking and increased the enjoyment associated with smoking, leading them to continue smoking WP.21
Regulatory bodies, including the US Food and Drug Administration (FDA), have expressed concern regarding the role of flavours and proposed regulations of WP tobacco. Moreover, flavours in tobacco cigarettes were banned by the FDA due to research indicating their role in smoking initiation and maintenance. However, WP tobacco was not included in the Family Smoking Prevention and Tobacco Control Act in 2009 and has therefore enjoyed an unregulated market. In the FDA’s new deeming regulation,22 WP is regulated under the Tobacco Control Act. This deeming rule precludes the sale of WP tobacco to individuals <18 years old and requires warning labels on WP tobacco; however, the FDA has not yet set restrictions on flavours in WP tobacco. While no experimental research has examined systematically the role of flavours in WP smoking, the cigarette and cigar literature implicate flavourants in initiation and maintenance of smoking. Specifically, flavours in tobacco have been shown to target youth and young adults and influence smoking initiation by appealing to naive and younger smokers.20,23–27 Flavours have also been shown to make smoking easier and more enjoyable, increasing initiation and smoking maintenance via increased nicotine dependence.28 29 In addition, smokers report flavours are an important part of their continued tobacco use and that flavours make smoking more satisfying.30 31 However, no research has explored experimentally the impact of flavours in WP tobacco smoking.
Given the importance and impact of flavours in cigarette smoking, experimental research examining the role of flavours in WP smoking is needed urgently. The current study is an important first step and examined users’ (1) WP smoking behaviours/topography, (2) exposure to toxicants such as carbon monoxide and nicotine, and (3) subjective smoking experience while smoking a preferred flavour WP tobacco compared with a non-preferred, tobacco-flavoured control. It was hypothesised that smoking the preferred flavour preparation would be associated with increased puff time, puff duration, flow rate, total number of puffs, total inhaled volume, maximum puff volume, and decreased interpuff interval (IPI), resulting in increased nicotine uptake and smoke exposure. It was also hypothesised that preferred flavour WP tobacco would be associated with an overall enhanced smoking experience, including greater interest in future use, compared with the control flavour.
METHOD
Sample
Participants were 36 current WP smokers recruited from a major metropolitan area via flyers, word of mouth and online advertisements (eg, Craigslist) from June to December 2015. Potential participants were screened for eligibility via telephone using the following eligibility criteria: (1) intended to smoke WP in the next 6 months, (2) were current WP smokers as indicated by smoking WP ≥1 time in the past month,32 (3) were ≥18 years old, (4) spoke and understood English, (5) denied current or past chronic health issues (eg, cycstic fibrosis, chronic obstructive pulmonary disease, asthma, lung or heart disease) and (6) were not currently pregnant or breastfeeding or had plans of becoming pregnant or beginning breastfeeding at any point during the study. All participants completed written informed consent procedures.
Laboratory procedures
The current study used a randomised cross-over design in which current WP smokers completed two 45 min WP smoking sessions. During each session, participants smoked either a preferred WP tobacco product or a non-preferred tobacco flavoured control product. Sessions were separated by a minimum 48 hours washout period to mitigate the impact of carryover effects. Session order was counterbalanced within participant. Presession tobacco abstinence was required for each session and was verified by exhaled carbon monoxide (eCO) testing on arrival (eCO <10 ppm). For female participants, absence of pregnancy was confirmed with a urine test at each visit.
Smoking sessions were conducted in a controlled laboratory setting in a room under negative pressure. Participants were seated in a comfortable chair while watching one of several prescreened movies of their choice. Participants were not allowed to eat, drink, or use their phone or other electronic devices during the WP smoking sessions. Initially, one piece of charcoal was lit and placed on the WP Additional charcoals were added and recorded on request from the participant. WP smoking topography was measured continuously throughout the session. Blood samples and eCO were collected immediately pre-WP and post-WP smoking session. Participants were compensated $50 for the first session and $60 for the second session for a total of $110 for study completion.
Materials
An Egyptian King Tut WP was used throughout study procedures. The WP had a stainless steel stem attached to the glass base (86 centimeters total). Six centimeters of the WP stem was submerged in 1200 mL of distilled water within the base. A glazed ceramic bowl (6 cm. diameter with five cm holes to allow air flow) was placed on top of the WP stem. The bowl was filled with 10 g of WP tobacco and covered with a circular sheet of aluminium foil with prepunched holes. Charcoals were coconut briquettes. Each charcoal was preweighed before being lit and placed on top of the perforated aluminium foil. Traditional leather hoses, interfaced with the topography machine, were used for each session. A new, prepackaged, disposable mouthpiece was provided for each participant, consistent with typical WP lounge practices. All procedures were consistent with existing laboratory studies of WP tobacco smoking.33 34 For the preferred flavour WP tobacco session, participants chose from a selection of 11 flavoured and sweetened Al Fahker WP tobacco including the pipe flavour. We planned to exclude participants who chose the pipe flavour as their preferred flavour; however, no participant chose this flavour. Flavoured WP tobacco options included watermelon (n=17), strawberry (n=4), apple (n=3), pineapple (n=3), orange (n=1), berry (n=1), cherry (n=1), lemon (n=1), vanilla (n=1) and grape (n=1). Preferred flavour options were pretested to confirm similar nicotine content as the control WP tobacco (preferred flavour =0.11–0.22%; non-preferred flavour=0.15%). Al Fahker Pipe flavour WP tobacco was used as the non-preferred tobacco-flavoured control because it does not include characterising flavours, is similar to a regular tobacco flavour and no participants indicated it as their preferred WP tobacco flavour.
Measures
Demographics
Participants completed demographic measures assessing age, gender and ethnicity.
Current WP smoking
Past month WP smoking was assessed via a self-report item adapted from Heinz and colleagues ( ‘How many sessions of hookah did you smoke in the past month?’).6 Response choices included 0, 1–2, 3–5, 6–9, 10–15, 16–20 or 21 or more sessions.
WP dependence
WP dependence was measured via the Lebanon Waterpipe Dependence Scale-11 (LWDS-11).35 The LWDS-11 is an 11-item self-report measure of WP dependence and comprises four subscales: physiological dependence, negative reinforcement, psychological craving and positive reinforcement. Scores > 10 indicate clinically significant WP dependence.35
Other product use
Participants reported on current use of other tobacco, nicotine and combustible products including electronic cigarettes, vapour devices, cigarettes, smokeless tobacco, nicotine replacement therapy (NRT; eg, lozenge, patch, inhaler, nasal spray, gum) and marijuana. Current use was indicated by product use during the previous 30 days as measured via a dichotomous (yes/no) self-report item (‘Have you used product in the last 30 days?’).
Outcome measures
WP smoking topography
Smoking topography was measured via a pressure flow sensor integrated into the WP hose near the base.36 37 Measures of WP topography included total puff time, puff duration, IPI, number of puffs, total volume inhaled, average puff volume and average flow rate. WP smoking topography was measured throughout each session.
Plasma nicotine boost
Blood draws occurred presmoking and postsmoking session at each visit. Plasma nicotine concentrations were analysed by gas chromatography-mass spectrometry, consistent with previously published methods.38
Exhaled carbon monoxide boost
Participants were assessed for exposure to carbon monoxide (a biomarker of smoke exposure and a cardiovascular toxicant) via a Covita handheld exhaled carbon monoxide (eCO) detector to confirm smoking abstinence at the beginning of each study visit. Postsession eCO was also assessed.
Subjective smoking experience
Following each WP smoking session, participants responded to the following subjective smoking experience items assessing the recently consumed product (preferred versus control tobacco flavour): pleasantness, desire/urge to smoke, need, want, liking, enjoyment, pleasure from use, satisfaction, interest in continued use and willingness to smoke the recently consumed product (see online Supplementary Appendix A). All items were presented on a Visual Analogue Scale (VAS) ranging from 0 (‘not at all’) to 100 (‘extremely’) presented as a 100 mm line on the computer. Participants placed a hash mark on the line that corresponded to a number along the line.
Data analysis
Data were analysed consistent with previous WP smoking laboratory studies.39–41 Means were calculated for all outcome measures (ie, measures of smoking topography, plasma nicotine boost, eCO and subjective experience items) and compared by session (preferred versus control flavour) using two-tailed paired samples t tests. For eCO measures, carbon monoxide boost was calculated by subtracting the presession eCO measure from the postsession eCO measure. Only seven participants had presession plasma nicotine measures above the limit of quantitation (LOQ). For those below the LOQ, one half of the LOQ (0.5 ng/ mL) was assumed for their presession value. Similar to eCO boost, nicotine boost was calculated by subtracting the presession nicotine value from the postsession value. Significance was set at p<0.05. All analyses were conducted in SPSS Statistics, V.22.0 (IBM, Armonk, New York, USA). One participant did not return for the second session and therefore is missing data for the flavoured session. Four participants are missing topography data for one session and one participant is missing topography data for both sessions due to instrument malfunction.
RESULTS
Participant demographics
Participants (n=36) had a mean age of 26.69 (SD=4.83) years and ranged from 18 years to 38 years of age and were primarily male (n=22; 61.1%). Twenty (55.6%) participants identified as Caucasian, five identified (13.9%) as African-American/black, four identified (11.1%) as Asian and seven participants identified (19.4%) as other. The majority (n=15; 41.7%) of participants reported one to two WP smoking sessions during the past month, with 50% (n=18) reporting more than two sessions and 8.3% (n=3) reporting no WP smoking during the past 30 days. The three participants who reported no WP smoking during the past 30 days, were still eligible per the IRB protocol as they self-reported past 30 days WP use at the time of screening. Participants denying WP smoking in the past month at presession did not differ significantly from other participants on measures of WP smoking frequency or duration and were therefore retained in analyses. Mean LWDS-11 was 8.67 (SD=3.30). In terms of other current tobacco, nicotine or combustible product use, participants endorsed past 30 days use of cig-a-like e-cigarettes (n=3; 0.8%), tank style e-cigarettes (n=9; 25%), combustible cigarettes (n=9; 25%), smokeless tobacco (n=1;2.8%) and marijuana (n=10;27.8%). All participants denied current NRT use. Of the 36 participants, 33 (91.7%) reported past 30 days use of any tobacco product. Participants used an average of 2.3 (SD=0.7) and 2.2 (SD=0.6) charcoals during the control flavour and preferred flavour session, respectively.
WP smoking topography
All WP smoking topography data are shown in table 1. No significant differences in topography were observed between preferred and control flavour sessions except for average puff volume (p=0.018). Average puff volume was statistically significantly greater when participants smoked the non-preferred WP tobacco flavour compared with the preferred flavour. In addition, several topography indices were trending towards significance (p<0.10), including average flow rate, IPI and total number of puffs.
Table 1.
Waterpipe smoking topography measures by preparation (n=30*)
| Non-preferred control flavour | Preferred flavour | df | t | p | |||
|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | df | t | p | |
| Total smoke time, min | 46.09 | 2.01 | 45.74 | 1.35 | 29 | 0.899 | 0.376 |
| Cumulative puffing time, min | 6.82 | 3.79 | 8.06 | 7.80 | 29 | −1.10 | 0.281 |
| Average puff duration, s | 3.43 | 1.54 | 3.16 | 1.48 | 29 | 1.39 | 0.176 |
| Average flow rate, L/min | 13.7 | 4.4 | 12.3 | 3.9 | 29 | 2.01 | 0.054 |
| Average IPI, s | 24.73 | 13.75 | 21.54 | 12.57 | 29 | 1.70 | 0.099 |
| Total number of puffs | 133 | 76 | 159 | 121 | 29 | −1.76 | 0.090 |
| Total inhaled volume, L | 90.4 | 51.2 | 80.7 | 43.6 | 29 | 1.14 | 0.263 |
| Average puff volume, L | 0.79 | 0.43 | 0.65 | 0.39 | 29 | 2.50 | 0.018 |
| Maximum puff volume, L | 1.70 | 0.54 | 1.82 | 1.37 | 29 | −0.51 | 0.614 |
6 participants were missing topography data for one or both WP sessions.
df, degrees of freedom; IPI, interpuff interval.
Exhaled carbon monoxide
Mean eCO concentration for the preferred WP tobacco flavour preparation increased from 4.2 ppm (SD=4.6) presession to 23.1 ppm (SD=16.7) after the smoking session, resulting in an overall change in concentration of 18.8 ppm (SD=15.1). For the control flavour WP preparation, mean eCO increased by 23.6 ppm (SD=25.5) from 3.6 ppm (SD=3.5) presession to 27.2 ppm (SD=27.0) at postsession. No statistically significant difference in the observed change in eCO was seen between each preparation t(32) = 1.37, p=0.180.
Plasma nicotine
Mean presession plasma nicotine concentration for the preferred WP tobacco flavour was 0.98 ng/mL (SD=1.28) and increased to 9.58 ng/mL(SD=6.54) at postsession. For the control flavour, mean presession plasma nicotine concentration was 1.10 ng/mL (SD=1.58) and increased to 8.99 (SD=6.07) at postsession. While this trend follows the predicted direction, these differences were not statistically significant, t(31) = −0.72, p=0.479. There was no significant difference in the increase of nicotine concentration between preferred (M=8.48 ng/mL, SD=6.38) versus control (M=7.98 ng/mL, SD=5.63) flavour conditions, t(31) =0.60, p=0.550.
Subjective smoking experience.
Measures of subjective smoking experience collected after each smoking session revealed significant differences between the two tobacco preparations. Figure 1 depicts mean ratings for all subjective smoking experience items. Significant differences were observed between groups for the following indices: pleasantness of product, liking of product, enjoyment of product, pleasure from product use, product satisfaction, interest in continued use and willingness to smoke the recently consumed product. For each of these items, values were greater when smoking the preferred tobacco flavour preparation (ps<0.05) versus the control flavour preparation. There were no observed differences between groups for need and want items.
Figure 1.
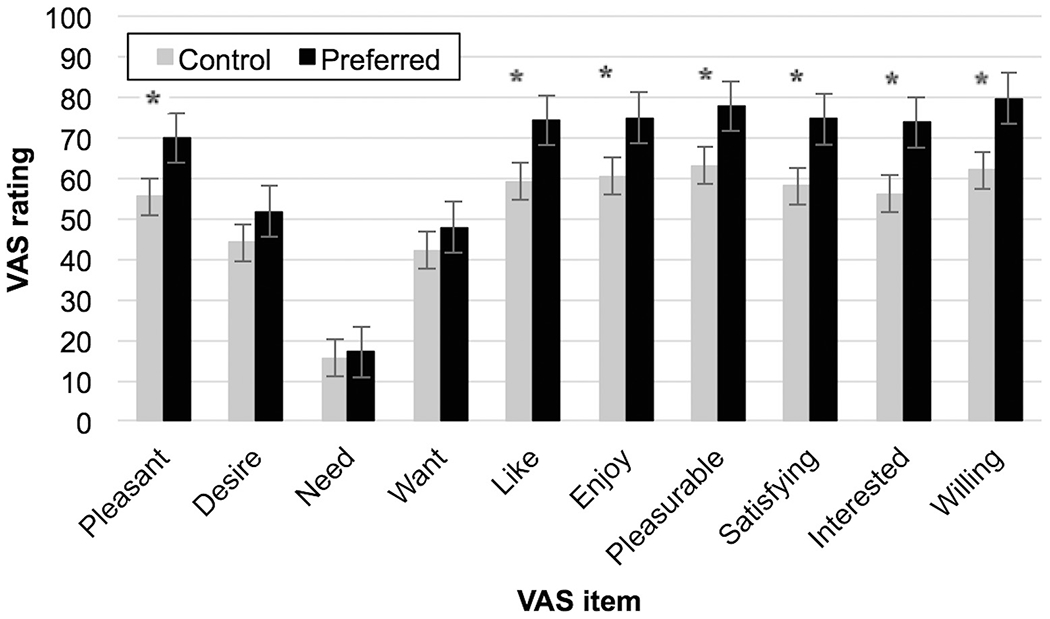
Subjective smoking experience items by WP smoking preparation. VAS ranges from 0 to 100 for each item; * indicates significant differences for that item between groups. VAS, Visual Analogue Scale. Mean(±SEM) data for subjective smoking experience items between preferred and control flavour.
DISCUSSION
The current study is the first to investigate the impact of flavour preference on WP tobacco smoking behaviours, toxicant exposure and subjective smoking experience. The results indicate that smoking a preferred WP tobacco preparation positively enhances the subjective experience of WP smoking and is associated with a greater willingness and interest in continuing to smoke WP. These findings provide further support for the role of flavours in the initiation and continued use of WP smoking, with participants reporting greater liking, enjoyment, satisfaction, interest in continued use and willingness to use their preferred flavour WP tobacco compared with the non-preferred control. The extant literature suggests these are important components of tobacco initiation and maintenance leading to increased nicotine dependence.28 29 Moreover, with these findings suggesting that even a slight change from a preferred to a non-preferred tobacco flavour results in a significant effect on user experience and willingness to continue to smoke WP it stands to reason that these results would be amplified with greater alterations to WP tobacco flavours and sweeteners (ie, unflavoured and unsweetened tobacco). FDA restrictions on characterising flavours and sweeteners may have a substantial impact on WP smoking prevalence in the USA.
Interestingly, while trending in the hypothesized direction for some topography variables, no significant differences in smoking topography were observed between the two different preparations of tobacco, with the exception of greater average puff volume when participants smoked the non-preferred control WP preparation as compared with the preferred WP tobacco. While unexpected, this finding is consistent with mixed topography results in studies examining mentholated cigarettes,42 even when users consistently report enhanced satisfaction and pleasure with menthol versus non-menthol use.43 44 While the control preparation was a plain tobacco flavour, both WP preparations still contained sweeteners and flavourants, which have been implicated in improved taste and increased smoking patterns.17 As would be expected, the lack of difference in most topography measures resulted in no significant difference in users’ exposure to carbon monoxide or nicotine uptake when smoking the preferred versus non-preferred flavour. Overall and consistent with previous research,13 33 36 39 40 45 46 users inhaled an average of 86 060 mL (SD=49.38) of smoke (equal to smoking approximately 172.12 cigarettes), experienced a nicotine boost of 8.29 ng/mL (SD=5.85) and eCO boost of 21.2 ppm (SD=20.77) indicating significant exposure to harmful tobacco-related constituents and addictive nicotine.
While the current study addresses important gaps in the WP smoking literature, it has several limitations. The study examined preferred flavours compared with a pipe flavoured WP tobacco product. While the flavour was non-preferred, a truly unflavoured preparation was unavailable in the US market at the time of the study. Overall differences in topography, subjective effects, carbon monoxide exposure and nicotine uptake between groups may be amplified with the inclusion of a truly unflavoured preparation. Second, both preparations were sweetened with molasses and glycerin; therefore, the data cannot be used to form conclusions regarding unsweetened WP tobacco. Another limitation of the current study is that it may not capture differences between WP smokers with high versus lower levels of dependence. The majority of participants in this study were regular WP smokers, but did not report high levels of dependence. Existing research suggests high and low frequency WP smokers differ in terms of their attitudes and beliefs about WP smoking47 as well as in their smoking patterns and behaviours.46 For this reason, the current study may not generalise to more frequent or nicotine dependent WP smokers. Finally, the current study was a highly controlled in-laboratory study of smoking behaviour. The results may differ outside the laboratory setting or when peers are present during the smoking session.48 However, given the current lack of understanding in flavour preferences on these outcomes, laboratory studies establishing whether differences might exist are a crucial first step in understanding the effects of flavours on WP smoking.
Despite these limitations, this research begins to fill an important gap in the WP smoking literature, as it is the first to examine the impact of a preferred versus non-preferred WP tobacco flavour in a controlled laboratory setting and highlights the importance of flavours in WP smoking. Future research should incorporate and compare an unflavoured WP tobacco preparation as well as unsweetened preparations in order to investigate the effects of these flavourants on smoking behaviour, toxicant exposure and subjective smoking experience. Such comparisons would allow for a more complete understanding of the impact of flavours in WP tobacco smoking. As the pattern of results in the current research suggests, flavours strongly affect overall satisfaction of WP use. As seen with the ban of flavours other than menthol in tobacco cigarettes by the FDA it seems likely that restricting flavours in WP smoking would reduce willingness and interest in initiation and continued use. Additionally, given the broad range of smoking frequency and WP dependence among US WP smokers, additional research is needed to understand whether these findings differ among highly dependent and more frequent WP smokers.
Supplementary Material
What is already known on this subject?
Waterpipe (WP) smoking is rapidly increasing, particularly among young adults.
WP smoking is associated with many of the same negative health outcomes as cigarette smoking.
The majority of WP smokers report smoking flavoured tobacco and emphasise the importance of flavours in WP smoking
What important gaps in knowledge exist on this topic?
No research has explored experimentally the impact of flavours in waterpipe tobacco smoking.
What this study adds
This study is the first to experimentally investigate the impact of a preferred versus non-preferred waterpipe (WP) tobacco flavour on subjective smoking experience, smoking patterns and toxicant exposure.
Participants reported a greater overall subjective smoking experience when smoking their preferred WP tobacco flavour compared with the non-preferred control WP tobacco.
Acknowledgements
The authors would like to thank Leslie Chandler, RN, MS, CTTS for her contributions to the study and for her assistance with phlebotomy. Dr. Wagener’s effort was partially supported by National Institute on Drug Abuse of the National Institutes of Health under Award Number R03 DA041928 and the Center for Tobacco Products of the U.S. Food and Drug Administration. Dr. Eissenberg’s and Dr. Shihadeh’s efforts were supported by the National Institute on Drug Abuse of the National Institutes of Health under Award Number P50DA036105 and the Center for Tobacco Products of the U.S. Food and Drug Administration. Eleanor Leavens’ effort was supported by the National Institute on Drug Abuse of the National Institutes of Health under Award Number F31 DA04252. The content is solely the responsibility of the authors and does not necessarily represent the views of the NIH or the FDA.
Funding
Intramural funds to TLW were used to complete this study. Part of TLW’s salary support is provided by the Oklahoma Tobacco Research Center, which is provided funding from the Oklahoma Tobacco Settlement Endowment Trust.
Footnotes
Competing interests None declared.
Ethics approval The University of Oklahoma Health Sciences Center Institutional Review Board.
REFERENCES
- 1.Arrazola RA, Singh T, Corey CG, et al. Tobacco use among middle and high school students - United States, 2011-2014. MMWR Morb Mortal Wkly Rep 2015;64:381–5. [PMC free article] [PubMed] [Google Scholar]
- 2.Johnston LD, O.M P. M, Miech RA, et al. Monitoring the future national results on drug use: 1975-2013: overview, key findings on adolescent drug use. Ann Arbor: Institute for Social Research, The University of Michigan, 2014. [Google Scholar]
- 3.Barnett TE, Smith T, He Y, et al. Evidence of emerging hookah use among university students: a cross-sectional comparison between hookah and cigarette use. BMC Public Health 2013; 13:302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Meier EM, Tackett AP, Miller MB, et al. Which nicotine products are gateways to regular use? First-tried tobacco and current use in college students. Am J Prev Med 2015;48(Suppl 1):S86–93. [DOI] [PubMed] [Google Scholar]
- 5.Sutfin EL, McCoy TP, Reboussin BA, et al. Prevalence and correlates of waterpipe tobacco smoking by college students in North Carolina. Drug Alcohol Depend 2011;115(1–2):131–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Heinz AJ, Giedgowd GE, Crane NA, et al. A comprehensive examination of hookah smoking in college students: use patterns and contexts, social norms and attitudes, harm perception, psychological correlates and co-occurring substance use. Addict Behav 2013;38:2751–60. [DOI] [PubMed] [Google Scholar]
- 7.Primack BA, Shensa A, Kim KH, et al. Waterpipe smoking among U.S. university students. Nicotine Tob Res 2013;15:29–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kates FR, Salloum RG, Thrasher JF, et al. Geographic proximity of waterpipe smoking establishments to colleges in the u.s. Am J Prev Med 2016;50:e9–e14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Al Rashidi M, Shihadeh A, Saliba NA. Volatile aldehydes in the mainstream smoke of the Narghile waterpipe. Food Chem Toxicol 2008;46:3546–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Monzer B, Sepetdjian E, Saliba N, et al. Charcoal emissions as a source of CO and carcinogenic PAH in mainstream narghile waterpipe smoke. Food Chem Toxicol 2008;46:2991–5. [DOI] [PubMed] [Google Scholar]
- 11.Sepetdjian E, Shihadeh A, Saliba NA. Measurement of 16 polycyclic aromatic hydrocarbons in Narghile waterpipe tobacco smoke. Food Chem Toxicol 2008;46:1582–90. [DOI] [PubMed] [Google Scholar]
- 12.Shihadeh A Investigation of mainstream smoke aerosol of the argileh water pipe. Food Chem Toxicol 2003;41:143–52. [DOI] [PubMed] [Google Scholar]
- 13.Cobb CO, Sahmarani K, Eissenberg T, et al.Acute toxicant exposure and cardiac autonomic dysfunction from smoking a single narghile waterpipe with tobacco and with a “healthy” tobacco-free alternative. Toxicol Lett 2012;215:70–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.El-Zaatari ZM, Chami HA, Zaatari GS. Health effects associated with waterpipe smoking. Tob Control 2015;24(Suppl 1):i31–i43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rammah M, Dandachi F, Salman R, et al. In vitro effects of waterpipe smoke condensate on endothelial cell function: a potential risk factor for vascular disease. Toxicol Lett 2013;219:133–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Smith SY, Curbow B, Stillman FA. Harm perception of nicotine products in college freshmen. Nicotine Tob Res 2007;9:977–82. [DOI] [PubMed] [Google Scholar]
- 17.Rastam S, Ward KD, Eissenberg T, et al. Estimating the beginning of the waterpipe epidemic in Syria. BMC Public Health 2004;4:32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hammal F, Wild TC, Nykiforuk C, et al. Waterpipe (Hookah) Smoking Among Youth and Women in Canada is New, not Traditional. Nicotine Tob Res 2016;18:757–62. [DOI] [PubMed] [Google Scholar]
- 19.Roskin J, Aveyard P. Canadian and english students’ beliefs about waterpipe smoking: a qualitative study. BMC Public Health 2009;9:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Villanti AC, Richardson A, Vallone DM, et al. Flavored tobacco product use among U.S. young adults. Am J Prev Med 2013;44:388–91. [DOI] [PubMed] [Google Scholar]
- 21.Nakkash RT, Khalil J, Afifi RA. The rise in Narghile (shisha, hookah) waterpipe tobacco smoking: a qualitative study of perceptions of smokers and non smokers. BMC Public Health 2011;11:315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Food and Drug Administration, HHS. Deeming Tobacco Products to be subject to the federal Food, Drug, and Cosmetic Act, as Amended by the Family Smoking Prevention and Tobacco Control Act; Restrictions on the Sale and Distribution of Tobacco Products and Required Warning Statements for Tobacco Products. Final rule. Fed Regist 2016;81:28973. [PubMed] [Google Scholar]
- 23.Carpenter CM, Wayne GF, Pauly JL, et al. New cigarette brands with flavors that appeal to youth: tobacco marketing strategies. Health Aff 2005;24:1601–10. [DOI] [PubMed] [Google Scholar]
- 24.Klausner K Menthol cigarettes and smoking initiation: a tobacco industry perspective. Tob Control 2011;20(Suppl 2):ii12–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Klein SM, Giovino GA, Barker DC, et al. Use of flavored cigarettes among older adolescent and adult smokers: United states, 2004--2005. Nicotine Tob Res 2008;10:1209–14. [DOI] [PubMed] [Google Scholar]
- 26.Lewis MJ, Wackowski O. Dealing with an innovative industry: a look at flavored cigarettes promoted by mainstream brands. Am J Public Health 2006;96:244–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.King BA, Dube SR, Tynan MA. Flavored cigar smoking among U.S. adults: findings from the 2009-2010 national adult tobacco survey. Nicotine Tob Res 2013;15:608–14. [DOI] [PubMed] [Google Scholar]
- 28.Giovino GA, Villanti AC, Mowery PD, et al. Differential trends in cigarette smoking in the USA: is menthol slowing progress? Tob Control 2015;24:28–37. [DOI] [PubMed] [Google Scholar]
- 29.Yerger VB. Menthol’s potential effects on nicotine dependence: a tobacco industry perspective. Tob Control 2011;20(Suppl 2):ii29–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Levin ED, Behm F, Rose JE. The use of flavor in cigarette substitutes. Drug Alcohol Depend 1990;26:155–60. [DOI] [PubMed] [Google Scholar]
- 31.Feirman SP, Lock D, Cohen JE, et al. Flavored tobacco products in the United States: A systematic review assessing use and attitudes. Nicotine Tob Res 2016;18:739–49. [DOI] [PubMed] [Google Scholar]
- 32.Maziak W, Ben Taleb Z, Jawad M, et al. ; Expert Panel on Waterpipe Assessment in Epidemiological Studies. Consensus statement on assessment of waterpipe smoking in epidemiological studies. Tob Control 2016:tobaccocontrol-2016-052958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cobb CO, Shihadeh A, Weaver MF, et al. Waterpipe tobacco smoking and cigarette smoking: a direct comparison of toxicant exposure and subjective effects. Nicotine Tob Res 2011;13:78–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Maziak W, Rastam S, Shihadeh AL, et al. Nicotine exposure in daily waterpipe smokers and its relation to puff topography. Addict Behav 2011;36:397–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Salameh P, Waked M, Aoun Z. Waterpipe smoking: construction and validation of the lebanon waterpipe dependence scale (LWDS-11). Nicotine Tob Res 2008;10:149–58. [DOI] [PubMed] [Google Scholar]
- 36.Shihadeh A, Saleh R. Polycyclic aromatic hydrocarbons, carbon monoxide, “tar”, and nicotine in the mainstream smoke aerosol of the narghile water pipe. Food Chem Toxicol 2005;43:655–61. [DOI] [PubMed] [Google Scholar]
- 37.Shihadeh A, Azar S, Antonios C, et al. Towards a topographical model of Narghile water-pipe cafe smoking: a pilot study in a high socioeconomic status neighborhood of Beirut, Lebanon. Pharmacol Biochem Behav 2004;79:75–82. [DOI] [PubMed] [Google Scholar]
- 38.Jacob P, Wu S, Yu L, et al. Simultaneous determination of mecamylamine, nicotine, and cotinine in plasma by gas chromatography-mass spectrometry. J Pharm Biomed Anal 2000;23:653–61. [DOI] [PubMed] [Google Scholar]
- 39.Eissenberg T, Shihadeh A. Waterpipe tobacco and cigarette smoking: direct comparison of toxicant exposure. Am J Prev Med 2009;37:518–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Maziak W, Rastam S, Ibrahim I, et al. CO exposure, puff topography, and subjective effects in waterpipe tobacco smokers. Nicotine Tob Res 2009;11:806–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Shihadeh A, Salman R, Jaroudi E, et al. Does switching to a tobacco-free waterpipe product reduce toxicant intake? A crossover study comparing CO, NO, PAH, volatile aldehydes, “tar” and nicotine yields. Food Chem Toxicol 2012;50:1494–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Yerger VB, McCandless PM. Menthol sensory qualities and smoking topography: a review of tobacco industry documents. Tob Control 2011;20(Suppl 2):ii37–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kreslake JM, Wayne GF, Connolly GN. The menthol smoker: tobacco industry research on consumer sensory perception of menthol cigarettes and its role in smoking behavior. Nicotine Tob Res 2008;10:705–15. [DOI] [PubMed] [Google Scholar]
- 44.Okuyemi KS, Ebersole-Robinson M, Nazir N, et al. African-American menthol and nonmenthol smokers: differences in smoking and cessation experiences. J Natl Med Assoc 2004;96:1208–11. [PMC free article] [PubMed] [Google Scholar]
- 45.Blank MD, Cobb CO, Kilgalen B, et al. Acute effects of waterpipe tobacco smoking: a double-blind, placebo-control study. Drug Alcohol Depend 2011;116(1–3):102–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Cobb CO, Blank MD, Morlett A, et al. Comparison of puff topography, toxicant exposure, and subjective effects in low- and high-frequency waterpipe users: a double-blind, placebo-control study. Nicotine Tob Res 2015;17:667–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Asfar T, Ward KD, Eissenberg T, et al. Comparison of patterns of use, beliefs, and attitudes related to waterpipe between beginning and established smokers. BMC Public Health 2005;5:19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ramôa CP, Shihadeh A, Salman R, et al. Group waterpipe tobacco smoking increases smoke toxicant concentration. Nicotine Tob Res 2016;18:770–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


