Few areas of clinical medicine are changing as rapidly as intensive care. Greater understanding of the pathophysiology of disease processes, technological innovations, targeted pharmaceutical and “nutriceutical” interventions, and the use of specialised audit and scoring methods to improve patient classification and monitor disease progression have all contributed to changes in practice in the past decade. This article considers developments that may affect patient management in the next 10 years.
Prevention
There is an increasing appreciation of the need to prevent critical illness with proactive care rather than to offer reactive support once organ failure is established. This has considerable resource implications, although savings should be made through reduced requirement for intensive care. Emphasis should be placed on identifying patients at risk, with early recognition of physiological disturbances and prompt correction to avoid subsequent major complications.
Maintenance of organ perfusion
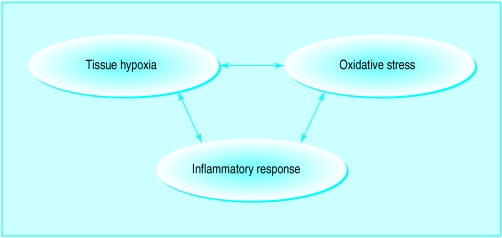
The concept of a perioperative tissue oxygen debt resulting in organ dysfunction, which need not be clinically manifest until several days after an operation, is now accepted. Many high risk patients cannot mount an adequate haemodynamic response to the stress of surgery, and this may be compounded by unrecognised hypovolaemia and poor organ perfusion. Tissue hypoxia and reperfusion injury both fuel the subsequent systemic inflammatory response.
Several recent studies have shown a strong relation between intraoperative haemodynamic deterioration and postoperative complications. Significant improvements in outcome and reductions in hospital stay have been achieved by optimising perioperative circulatory function using fluid loading with or without vasoactive drugs, and guided by monitoring of cardiac output.
Ward supervision
The hospital mortality of patients admitted to intensive care from general wards (40-45%) is significantly higher than that of patients admitted directly from either accident and emergency (30%) or the operating theatre (20%). This is partly because of delays in recognising problems and suboptimal treatment.
Attempts are being made to improve patient care in general wards and thereby pre-empt the need for intensive care. The Liverpool Hospital in New South Wales, Australia, has recently pioneered medical emergency teams. These are expert teams that can be called by medical or nursing staff when patients meet predetermined physiological criteria or give cause for concern. The high dependency unit is also being proposed as a means of improving the management of high risk patients.
Immunological and genetic manipulation
Individual susceptibility to the effects of inflammatory activation may be determined genetically, and this raises the possibility of assessment before procedures such as major elective surgery. For example, septic patients homozygous for the tumour necrosis factor B2 allele had higher plasma tumour necrosis factor-α concentrations, organ failure scores, and mortality than heterozygous septic patients. Drugs may be developed to boost or suppress the inflammatory response in high risk patients.
The degree of acquired endogenous immunity may also be important. For example, patients with high titres of endogenous endotoxin antibodies have better outcomes after cardiac surgery; passive or active immunisation programmes may therefore be effective.
Pharmaceutical advances
Modulating the inflammatory response
Patients may develop (multiple) organ dysfunction after insults such as infection and trauma. Increasing awareness of the roles of endotoxin and other toxins; endogenous proinflammatory, vasoactive, and anti-inflammatory mediators; tissue hypoxia; and subsequent reperfusion injury has led to drugs targeted against these pathophysiological mechanisms.
Some immunotherapeutic drugs tested in randomised, controlled phase II or III trials in human sepsis
Methylprednisolone
Hyperimmune immunoglobulin
Endotoxin antibody
Bactericidal permeability increasing protein
Tumour necrosis factor antibody
Soluble tumour necrosis factor receptor antibody
Interleukin-1 receptor antagonist
Platelet activating factor antagonists
Bradykinin antagonists
Ibuprofen
Antithrombin III
Activated protein c
N-acetyl cysteine
Procysteine
Nitric oxide synthase inhibitor (l-monomethyl nG-arginine (l-NMMA))
Most effort to date has been expended on modulating the inflammatory response with immunotherapeutic drugs aimed against endotoxins or mediators such as the cytokines, tumour necrosis factor, and interleukin-1. Unfortunately, the promising results shown in both laboratory and small patient groups have yet to be reproduced in large multicentre trials. Paradoxically, this has helped to clarify some of the problems of study design that exist when looking at such a heterogeneous population. But many other issues remain—for instance, when to give the drug and the balance between blocking and enhancing the inflammatory response. These difficulties are compounded by enormous variation in the pattern of response between patients. This variation may be due to coexisting illness or to genetic predisposition.
In future there may be targeted treatment guided by appropriate immunological markers which can be measured at the bedside. Identification of genetically high risk patients will allow them to have closer monitoring, and drugs may also be developed to modulate their inflammatory response.
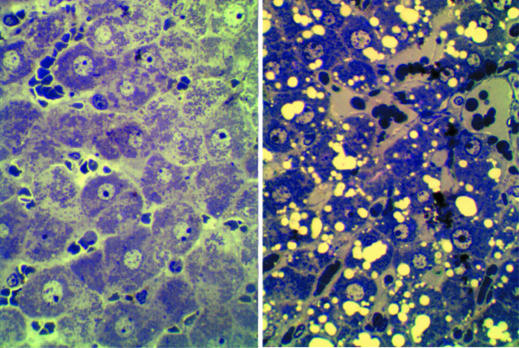
Reducing cellular injury
Recognition of the importance of hypoxia in the pathogenesis of cellular injury has stimulated development of various drugs that are either protective or augment tissue oxygenation—for example, by shifting the oxyhaemoglobin dissociation curve or enhancing cellular oxygen use. Specific channels, receptors, and signalling pathways are activated by tissue hypoxia; antagonism or stimulation of these may prove beneficial.
Treatments are also being developed to prevent the damage caused to cell membranes, protein, DNA, and mitochondria by raised intracellular concentrations of calcium and excessive production of reactive oxygen and nitrogen species (superoxide, hydroxyl radical, nitric oxide, etc).
Modifying vascular tone and function
Nitric oxide is associated with profound hypotension in hyperinflammatory syndromes such as sepsis. Inhibitors of the synthesising enzyme (nitric oxide synthase) or its effector pathways have been well studied. A recent large multicentre study of a nitric oxide synthase inhibitor was, however, terminated prematurely because of adverse outcome. Nevertheless, drugs that modify vascular tone and the microcirculation by acting on the endothelium (including leucocyte and platelet interactions), smooth muscle tone, and rheology could optimise microvascular distribution of blood flow and tissue perfusion, thereby reducing tissue damage.
Other drugs being tried in intensive care
Drugs to improve gas exchange
Sedatives or analgesics that are short acting despite prolonged administration
Specific vasoactive drugs
Neuroprotective drugs for use after neurosurgery or cardiothoracic surgery, head trauma, or cardiorespiratory arrest
New antibiotics to deal with increasingly multiresistant micro-organisms
Anabolic hormones (some with immunomodulatory effects) such as growth factors which can hasten rehabilitation
In the long term, a cocktail of the agents described above, rather than any single drug, is likely to be used to prevent, attenuate, or treat hypoxic, infectious, and other insults that lead to multiple organ failure.
Blood substitutes
Artificial haemoglobin and fluorocarbon solutions carry much higher amounts of oxygen than equivalent volumes of standard plasma or crystalloid solutions. These have been in development for several decades as an alternative to blood in emergency situations and peroperatively (for example, for Jehovah’s witnesses). Problems such as nephrotoxicity and inadequate release of oxygen to tissues have delayed their introduction into routine use, although recent advances have largely overcome these difficulties—for example, diasprin cross linkage of haemoglobin molecules and liposome encapsulation. Multicentre trials are now in progress in various potential applications. The first artifical haemoglobins are likely to be commercially available within a year.
Ventilation and gas exchange
The increasing use of mechanical ventilation was the driving force behind the creation of intensive care units. Over the past 30 years ventilators have become more sophisticated, with various techniques incorporated to minimise iatrogenic trauma and facilitate patients’ tolerance and weaning. Particular attention has been applied to non-invasive modes of ventilation such as biphasic positive airways ventilation through a nasal or face mask, high frequency oscillation, and negative pressure ventilation with a cuirass ventilator. Continued developments will reduce the need for tracheal intubation—for example, in those with acute-on-chronic respiratory failure. Computer controlled ventilation, in which the ventilator constantly adjusts to changes in lung compliance and blood gas measurements, is another recent development.
There has also been considerable enthusiasm for locally applied agents that improve gas exchange or reduce lung injury. These include inhaled nitric oxide, nebulised epoprostenol, and nebulised artificial surfactants. Although these agents produce short term improvement in many patients with acute respiratory failure, only surfactants in neonatal respiratory distress have been shown to improve outcome. A novel concept is to attenuate the degree of lung fibrosis in conditions such as the acute respiratory distress syndrome by using specific inhibitors instilled into the lung—for example, thrombin inhibitors.
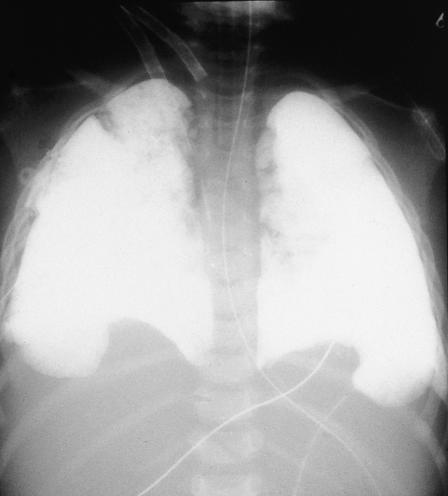
Finally, trials of liquid ventilation are ongoing. The lungs are filled with a fluorocarbon to functional residual capacity—that is, when a fluid meniscus is seen in the endotracheal tube on end expiration—and are ventilated through this medium. Early results have been highly encouraging in terms of gas exchange, bronchial lavage, surfactant-like properties, and anti-inflammatory properties and suggest that the technique will improve outcome.
Nutrition
Increasing awareness of the importance of nutrition and avoiding malnutrition has encouraged earlier introduction of feeding for critically ill patients. Recent laboratory studies have shown various nutrients to have positive immunomodulatory effects, including glutamine, polyunsaturated fatty acids, and arginine. “Immunoenhanced” diets have been given to intensive care patients, surgical patients, burn patients, and those having bone marrow transplantation. Reduced morbidity and, occasionally, mortality have been shown, although confirmatory large scale multicentre studies are awaited.
Other areas under investigation include the concept of protecting the gastrointestinal surface with probiotic bacteria. Shortening the catabolic phase of injury and enhancing anabolism by infusion of growth hormone and insulin growth factor-1 was recently tested but produced an adverse outcome.
Monitoring
Treatment in intensive care should always be guided by adequate monitoring. Advances have enabled cardiorespiratory function to be monitored continuously and, increasingly, by non-invasive or minimally invasive techniques. These techniques are being continually refined and some are now being commercially marketed. Further efforts are being made to measure regional organ perfusion (and its adequacy) through tissue or arteriovenous oxygen or carbon dioxide pressure, lactate concentration, or other markers such as the cytochrome aa3 redox state, and hepatic clearance of indocyanine green.
Examples of new monitoring techniques
| Variable | Monitoring |
|---|---|
| Arterial blood gas concentrations and pH | Continuous by intra-arterial catheters Intermittent by portable devices |
| Cardiac output | Intraoesophageal probes, surface electrodes, or via radial arterial cannulas |
| Gastric mucosal carbon dioxide pressure (index of tissue perfusion) | Continuous through nasogastric catheter |
Although the importance of raised plasma concentrations of circulating inflammatory mediators such as interleukin-6 and procalcitonin is not yet fully understood, kits are being developed to allow measurement at the bedside. The results may be used to predict sepsis or to indicate the correct timing for giving immunomodulating drugs.
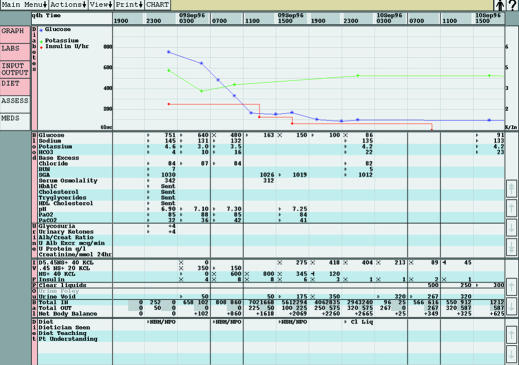
Finally, paperless monitoring with sophisticated computers interfaced with physiological monitors, fluid infusion pumps and drainage sets, pathology laboratories, and pharmacy should not only facilitate data collection and patient management but provide a sophisticated and comprehensive database for audit and research. Early versions are already in operation in over 100 intensive care units worldwide, but continual refinement and technological advances should produce widespread uptake of these systems.
Audit, guidelines, and evidence based medicine
The scoring systems for physiological abnormality, therapeutic intervention, organ dysfunction, and predicting outcome are far more complex than in any other specialty. Indeed, many intensive care units are now employing dedicated audit staff to collect these data. The data are being incorporated into national and international databases, enabling better definition of patient populations and disease progression. Variations in case mix between units are being taken into account, and this will allow quality issues to be explored in far greater detail than at present.
Clinical governance is likely to lead to local, regional, national, or even international, practice guidelines. These will be evidence based where possible. However, the current paucity of conclusive large scale, randomised controlled trial data, and the logistical, ethical, and financial difficulties in conducting such studies, will often oblige these to be consensus led.
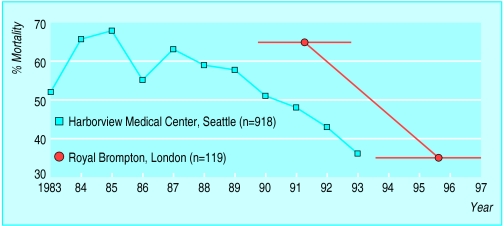
Figure.
Outcome from acute respiratory distress syndrome has improved over the past 15 years. Data from Milberg JA et al. Improved survival of patients with acute respiratory distress syndrome. JAMA 1995;306-9 and Abel SJ et al. Reduced mortality in association with the acute respiratory distress syndrome. Thorax 1998;53:292-4
Figure.
Factors responsible for organ dysfunction
Figure.

Outcome from intensive care is related to source of admission
Figure.

Genetic factors may affect survival of patients with septicaemia
Figure.
Effects of hypoxia on rat liver
Figure.

Blood substitutes will be available shortly for clinical care
Figure.
Continuous intra-arterial blood gas monitoring
Figure.
Radiograph of patient receiving liquid ventilation
Figure.
Immunonutrition
Figure.
Measurement of gastric mucosal pco2, a marker of organ perfusion
Figure.

Continuous monitoring of cardiac output by oesophageal Doppler ultrasonograph
Figure.
Computerised monitoring system
Footnotes
Rod Little is professor, North West Injury Research Centre, University of Manchester.
The ABC of intensive care is edited by Mervyn Singer, reader in intensive care medicine, Bloomsbury Institute of Intensive Care Medicine, University College London and Ian Grant, director of intensive care, Western General Hospital, Edinburgh. The series was conceived and planned by the Intensive Care Society’s council and research subcommittee.
The radiograph was provided by Dr R Hirschl, the oesophageal Doppler monitor by Deltex, continuous air tonometer by Datex-Ohmeda, the picture of the computerised monitoring system by Hewlett Packard, and the blood gas analyser by Diametrics