Abstract
Background:
Although opioid prescribing has recently trended downward, opioid-related overdoses and deaths have drastically increased. Community pharmacists are accessible healthcare providers who are well-positioned to disseminate information on opioid safety and to educate and counsel on medication use, managing adverse events, and proper medication disposal. Patient callbacks facilitate appropriate medication usage. We developed an opioid callback program that provides a framework for pharmacists to follow up with patients with an opioid prescription.
Objectives:
This study aimed to (1) describe the development of the opioid callback initiative, and (2) report results from a pilot test in two community pharmacies.
Methods:
The opioid callback process and data collection forms were collaboratively developed with community pharmacists at each site. Data recorded on the opioid callback forms were descriptively analyzed and chi-square test of independence explored differences by pain durations related to opioid disposal, security, and safety. Participating pharmacy staff were interviewed to identify facilitators and barriers to implementation, as well as opportunities for improvement.
Results:
Forty-one opioid callbacks were attempted and 36 were completed (87.8%). Pharmacists were significantly more likely to discuss naloxone with patients with chronic pain (89.5%) compared to those with acute pain (46.2%). Pharmacists reported that the program successfully raised awareness of opioid disposal opportunities and safe opioid practices, including storage and naloxone ownership. They expressed patients’ willingness to answer questions and appreciation for the extra attention and care.
Conclusion:
Community pharmacists are well-positioned to address the opioid crisis as access points for medication questions, opioid safety education, opioid disposal, naloxone, and medications for people with an opioid use disorder. This study presents a proof of concept for a pharmacist-led opioid callback program. Expansion could help inform patients about how to use opioids safely, how to treat an opioid overdose, and where to dispose of unused medications.
Keywords: opioid epidemic, patient callbacks, community pharmacists, accessibility, safe opioid practices, opioid disposal
Background
In 2020, more than 142 million opioid prescriptions were dispensed in the United States.1 Although opioid prescribing has recently trended downward, opioid-related overdoses and deaths have drastically increased, highlighting the importance of disseminating information on the safe use and disposal of opioids.2,3 Nationally, roughly 29% of patients currently prescribed an opioid do not take their medication as directed.4 Patients not following prescribing instructions for opioids are considered to be misusing those medications and, as a result, are more likely to develop an opioid use disorder or experience severe harms such as overdose or death.5 Community pharmacists have expertise on medications and represent one of the most accessible health care providers. Therefore, they can play an important role in reducing opioid related harms.
Intervention
Patient callbacks represent one approach used by healthcare organizations to facilitate appropriate medication usage. Patient callbacks involve contacting patients after hospital discharge, medication initiation, or negative bacterial culture and can be effective for reviewing the discharge plan, counseling on new or changed medications, or to discontinuing antibiotics.6–13 Since antibiotic resistance is a global health concern that poses a serious threat to public health and safety,11 callbacks have been used prevalently as means to reduce this clinical issue. For example, post-hospital discharge callbacks, often nurse-led, have been shown to reduce return visits to the emergency department,7,8 discourage antibiotic use after a negative bacterial culture,10 and improve time to follow-up with primary care physicians.6
Community pharmacy staff routinely utilize reminder phone calls with patients for prescription refills and vaccination reminders9,14–23 and have 11 facilitated appropriate antibiotic use by using their clinical skills and awareness of prescription fill history to participate in patient antibiotic callbacks.8,9,11,12 Surprisingly, similar programs are not yet standard practice for opioid prescriptions despite the risks associated with prescription opioids and the opioid crisis being declared a US public health emergency.24–27 However, community pharmacists are well-positioned to perform opioid callbacks because they are accessible healthcare providers trained to educate and counsel on safe and effective medication use, managing adverse events, and proper medication disposal.28–30 These skills, also utilized when dispensing a medication, can be applied to educating patients about opioid safety and pain management, inquiring about unused opioids, and discussing the importance of opioid disposal for patient and public safety. Patient education and appreciation for opioid disposal are needed, since patients often are unaware of available medication disposal options and/or the risks and environmental impact of improper disposal.31–35 Evidence suggests that a similar approach with pharmacist-provided education about naloxone and opioid abuse prevention, including disposal education, increases naloxone prescriptions and access to medication disposal.36–38 We developed an opioid callback program that provided a framework for pharmacists to follow up with patients with an opioid prescription.
Objectives
This proof-of-concept study explored the feasibility and usability of a pharmacy opioid callback program. The study objectives were to (1) describe the development of the opioid callback initiative and (2) report results from a pilot test in two community pharmacies in one Midwest state.
Methods
The study was conceptualized as a mixed-methods design, consisting of data systematically collected during opioid callback interactions and brief interviews with participating pharmacists to evaluate this pilot project’ impact. The project was deemed quality improvement/program evaluation, not requiring Institutional Review Board review and oversight.
Pharmacy Recruitment
A total of 68 out of 352 community pharmacies completed a survey that inquired about their interest in piloting an opioid callback program.39 Of the 11 community pharmacies who indicated an interest, three pharmacies expressed initial willingness and two pharmacies ultimately agreed to participate in the opioid callback pilot.
Opioid Callback Data Collection Process
The opioid callback program was piloted in two independently-owned community pharmacies in two mid-sized cities in a Midwestern state– PharmacyA (Aug-Oct 2021) and PharmacyB (July 2021). The program was originally piloted for 30 days, but PharmacyA opted to extend the program using student pharmacists for 90 days. To optimize the opioid callback experience, we utilized an iterative process to develop potential opioid callback scripts and scenarios (e.g., a one-time callback or multiple callbacks). Community pharmacists provided feedback about the likely feasibility and usability of the draft scripts/scenarios in their setting.
Prior to the project start, our team worked with each pharmacy to collaboratively develop data collection forms to guide the callback interaction. While both pharmacies would collect the same information, the forms were individually formatted to fit seamlessly within each pharmacy’s workflow (Appendix A). Following the pilot test, pharmacists mailed back their data collection forms, and information included on the forms was compiled for analysis. Figure 1 describes the opioid callback process.
Figure 1.
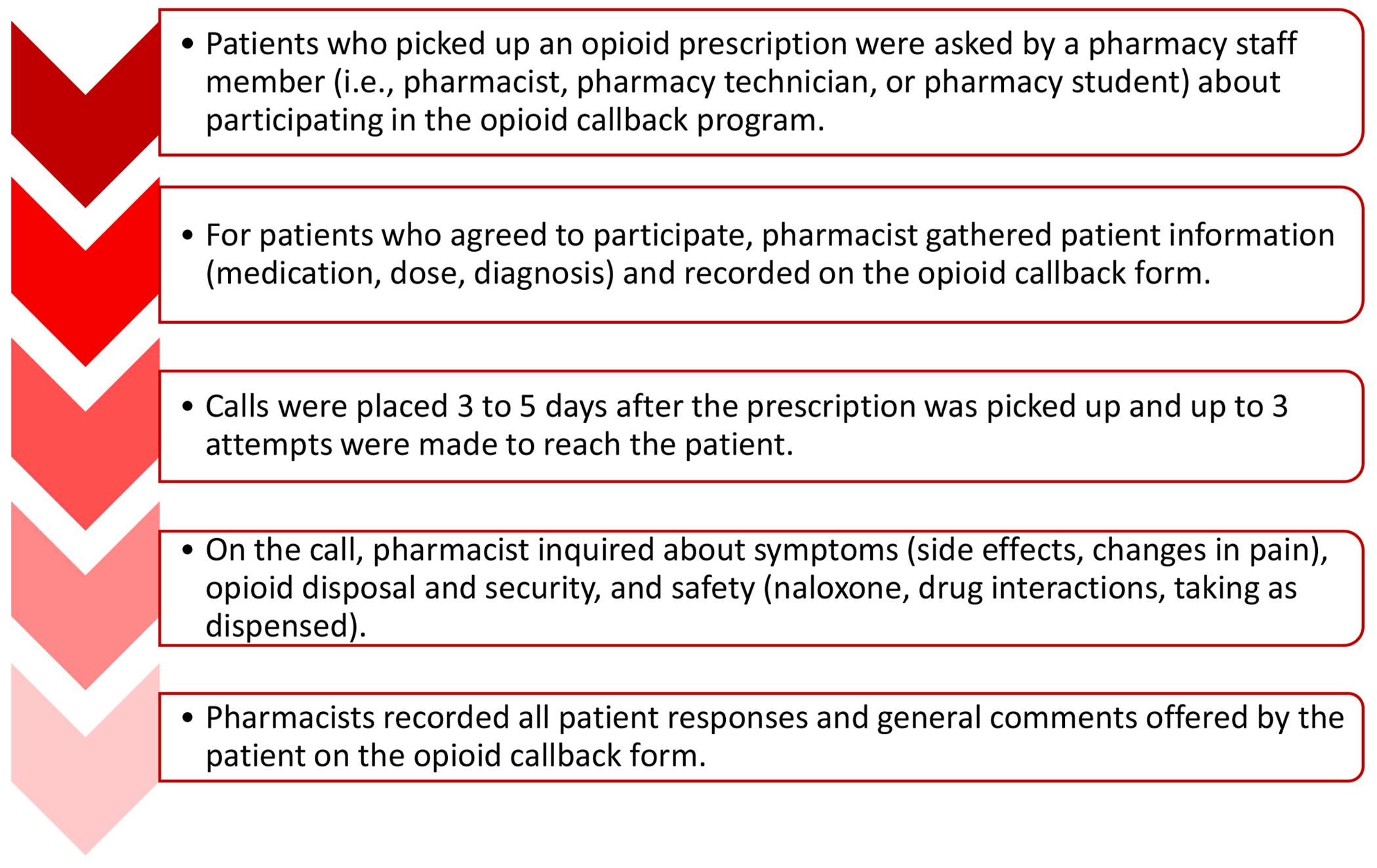
Process Associated with the Opioid Callback Pilot Program
Pharmacist Interviews
Pharmacy staff were invited to participate in a semi-structured follow-up interview about a month after piloting the program. These interviews sought to identify implementation facilitators and barriers, as well as opportunities for improvement (see Appendix B). JHF conducted all interviews by phone. Interviews, lasting an average of 16 minutes (5-39 minutes), were audio-recorded with permission and professionally transcribed for analysis.
Data Analysis
Pharmacists use clinical decision-making based on disease state to select the education/awareness issues when dispensing prescriptions.40 Acute and chronic pain conditions, and resulting opioid prescriptions, may prompt pharmacists to discuss different patient-related issues, such as counseling on opioid disposal for patients with acute pain.41–43 Therefore, we classified patients based on pain duration (I.e., length of the pain experience) - having either acute or chronic pain using information from the opioid callback forms. A patient was determined to have acute pain when the prescription indicated the opioid was prescribed for acute pain or the patient was taking the medication for an acute pain condition (e.g., surgery, a car accident, or acute pancreatitis). Patients were categorized with chronic pain when the prescription stated it was for chronic pain or the patient was taking the medication for a chronic pain condition (e.g., chronic back pain, degenerative nerve pain, neuropathic arthritis, or cancer pain). The analysis excluded patients who did not respond to callback attempts or whose pain duration could not be determined.
A codebook was developed from the semi-structured interview guide topics, including general reactions, workflow, disposal awareness, safety awareness, and recommendations for the callback program. SH deductively coded interviewee responses into relevant themes. Representative quotes were selected for each theme to describe the impact of, and recommended changes to, the pilot program.
In addition to descriptive statistics, the chi-square test of independence explored differences by pain durations related to opioid disposal, security, and safety. A sensitivity analysis determined whether excluding one of the pharmacies, due to its comparatively low number of participants, would affect our findings. All analyses were conducted using IBM SPSS Statistics v.28.0.1.0.
Results
Opioid Callbacks
Forty-one opioid callbacks were attempted (averaging 1.4 calls per patient) and 36 were completed (87.8%); five patients did not answer callback attempts. Appendix C describes information collected during the opioid callback. Pain durations were determined for 34 (94.4%) patients, nine of which were derived from the prescription. The final sample consisted of 31 patients from PharmacyA and three from PharmacyB. Table 1 revealed a significant difference in frequency of naloxone being discussed with patients based on pain duration, with pharmacists being more likely to discuss naloxone with patients identified as having chronic pain (89.5%) compared to those with acute pain (46.2%). No other significant differences emerged. The sensitivity analysis revealed no change in results.
Table 1.
Comparison of Items Discussed with Patients by Pain Duration1
| Items Discussed with Patient | Acute Pain (n=15) |
Chronic Pain (n=19) |
Total (n=34) |
Chi-Square |
|---|---|---|---|---|
|
|
||||
| n (%) | n (%) | n (%) | ||
| Medications Storage Location | 5.102 (p=0.164) | |||
|
| ||||
| Contained, Locked | 1 (9.1%) | 6 (33.3%) | 7 (25.0%) | |
|
| ||||
| Contained, Monitored2 | 0 (0.0%) | 2 (11.1%) | 2 (7.1%) | |
|
| ||||
| Contained, Unlocked3 | 6 (54.5%) | 4 (22.2%) | 10 (35.7%) | |
|
| ||||
| Uncontained, Unlocked4 | 3 (27.3%) | 6 (33.3%) | 9 (32.1%) | |
|
| ||||
| Disposal Options Discussed | 0.552 (p=0.457) | |||
|
| ||||
| Yes | 11 (78.6%) | 12 (66.7%) | 23 (71.9%) | |
|
| ||||
| No | 3 (21.4%) | 6 (33.3%) | 9 (28.1%) | |
|
| ||||
| Naloxone as a Rescue Medication Discussed | 7.166 (p=0.007) | |||
|
| ||||
| Yes | 6 (46.2%) | 17 (89.5%) | 23 (71.9%) | |
|
| ||||
| No | 7 (53.8%) | 2 (10.5%) | 9 (28.1%) | |
|
| ||||
| Drug Interaction Discussed | 3.406 (p=0.092) | |||
|
| ||||
| Yes | 10 (71.4%) | 18 (94.7%) | 28 (84.8%) | |
|
| ||||
| No | 4 (28.6%) | 1 (5.3%) | 5 (15.2%) | |
|
| ||||
| Take Medication as Directed Discussed | 0.050 (p=0.823) | |||
|
| ||||
| Yes | 13 (92.9%) | 18 (94.7%) | 31 (93.9%) | |
|
| ||||
| No | 1 (7.1%) | 1 (5.3%) | 2 (6.1%) | |
|
| ||||
| Side Effects | 4.577 (p=0.334) | |||
|
| ||||
| None | 7 (63.6%) | 13 (72.2%) | 20 (69.0%) | |
|
| ||||
| Drowsiness | 3 (27.3%) | 2 (11.1%) | 5(17.2%) | |
|
| ||||
| Dizziness | 1 (9.1%) | 0 (0.0%) | 1 (3.4%) | |
|
| ||||
| Constipation | 0 (0.0%) | 2 (11.1%) | 2 (6.9%) | |
|
| ||||
| Drowsiness/Dizzy | 0 (0.0) | 1 (5.6%) | 1 (3.4%) | |
|
| ||||
| Change in Pain Intensity | 1.595 (p=0.451) | |||
|
| ||||
| Unchanged | 1 (9.1%) | 4 (22.2%) | 5 (17.2%) | |
|
| ||||
| Improved | 10 (90.9%) | 13 (72.2%) | 23 (79.3%) | |
|
| ||||
| Worsened | 0 (0.0%) | 1 (5.6%) | 1 (3.4%) | |
|
| ||||
| Average Number of Call Attempts | (p=0.885) | |||
|
| ||||
| 1.3 calls (0.46 SE) | 1.2 calls (0.55 SE) | 1.2 calls (0.50 SE) | ||
Instances where numbers do not add up to category total sample are due to non-response in that criteria and could not be determined. Items discussed when medication picked-up by patient, during the opioid callback, or both.
Contained, monitored medications were stored with a caregiver or out of reach of children.
Contained, unlocked medications were stored in a drawer, cabinet, or pillbox.
Uncontained, unlocked medications were stored on a counter or bedside table.
Only PharmacyA recorded call attempts. We reported mean and standard error and utilized a t-test to examine differences based on self-reported pain duration.
Interviews
Four pharmacists were interviewed, one at PharmacyA (RPh1) and three at PharmacyB (RPh2, RPh3, RPh4). Additionally, we interviewed one student pharmacist (SPh1) who performed opioid callbacks at PharmacyA as part of their experiential education.
General Reactions to Opioid Callback Program
Overall, pharmacists reported that patients were willing to answer questions and demonstrated appreciation for the extra attention and care. As RPh1 commented: “I don’t think anybody was…angry that we were asking or felt like they were being accused of something.” Although some patients expressed gratitude for the education about opioid alternatives for pain management, RPh3 also was pleased “that we are recommending other forms of pain relief or pain management.” RPh4 described one patient, who expressed hesitancy about filling their opioid prescription and was directed to an over-the-counter pain reliever first – “[The patient] didn’t pick [the opioid prescription] up the first day, had me hold it and wait…Then came back the second day when the alternatives weren’t enough.”
SPh1 noted some patients’ initial “apprehension” or “defensiveness” about the callback, emphasizing that the introductory message of the call could significantly affect the patient’s response. When SPh1 explained that the callback’s purpose was to better serve the patient and to improve safety, it became a more positive experience for the patient.
Assessing patient awareness about opioid disposal and opioid safety
Disposal awareness was considered the most valuable callback topic to RPh2, as this was most patients’ introduction to the existence of opioid disposal opportunities. RPh3 reported that “nobody really had any idea about how to dispose of it properly…they were very concerned about disposing of it properly.” Patients were interested in learning different ways to dispose of left-over opioids and appreciated the pharmacist taking time to inform them. RPh1 also mentioned that PharmacyA included with every opioid prescription “a half sheet that had the different locations in town where opioid could be disposed of.”
Perceptions about safety awareness showed more variation. The program was seen as successful at ensuring patients’ awareness of naloxone and opioid safety while also prompting education where needed. The form “made sure everyone was on an even playing field,” reported RPh4. RPh1 even said that the intervention led to naloxone nasal spray dispensing. However, that same pharmacist did not feel the program was influential for chronic opioid-use patients. RPh2 recalled that an opioid-naïve patient “didn’t think that he needed Narcan necessarily, but we did talk about it.”
Impact on Workflow
Most interviewees believed this program did not affect the workflow significantly. A few felt they were already doing some of the steps and that this could be integrated well into their current process. RPh1 noted that the continued operation relies on having pharmacy interns. Overall, respondents expressed uncertainty about integrating the opioid callback into current employee workloads.
Recommended Changes
SPh1 recommended condensing the form. Respondents suggested considering information that the pharmacists could have beforehand, such as acute versus chronic use, to reduce the questions posed to patients. SPh1 also suggested adding checkboxes to the callback form for common side-effects (e.g., nausea, vomiting, insomnia, drowsiness, and constipation), which standardizes and streamlines the data collection process and would capture more accurate side-effects profiles.
RPh1 shared that, while the pain assessment form “was a nice guide,” it was not more helpful than “clinical judgement as to where to take those questions.” Instead of asking the patient if pain has improved or worsened, SPh1 recommended asking if pain is controlled. SPh1 also suggested asking the patient’s pain goal to better assess pain treatment efficacy.
A theme throughout the interviews was the need for different approaches for acute versus chronic opioid use patients. Acute use patients were considered more receptive to the program and thankful for the pharmacists’ effort. It was recommended by SPh1 to “focus more on…the acute patients first because I think that’s where we’re going to see the greatest return on our investment…The first thing we need to do is prevent future occurrences.” In addition, RPh2 suggested that “something to discuss is having just Narcan on hand, not necessarily for them but for anyone that might get into it.”
Discussion
To the authors knowledge, this study was the first to explore the feasibility of a community pharmacy opioid callback intervention. Our approach generally followed the structure of other community pharmacy callback initiatives.9,11,12 The median number of calls (1 call) to reach a patient did not differ from antibiotic callbacks.44 Time to conduct calls was only reported by one pharmacy, with the average duration (7.5 minutes) being 4.2 minutes longer than a pharmacy antibiotic callback.11 The longer time may reflect the difference between what a pharmacist needs to discuss with a patient regarding the prescribed medication. Even given this longer call time, pharmacists indicated that the opioid callback, like antibiotic callbacks, did not significantly change their workflow.11,44
Although outcomes (i.e., disposal, naloxone co-prescriptions, and safety) were common across the two pharmacies, each pharmacy implemented the callback program consistent with their workflow. Although pharmacists generally were receptive to the opioid callback program, systematic opioid callback seemed more likely at community pharmacies where residents/students can complete the task. The student pharmacist noted that explaining the purpose of the callback to the patient early in the callback improved the experience, aligning with past findings of effective communication and clear explanations for treatments on patient satisfaction.45 An initial statement about the program’s goal to improve opioid safety may improve patients’ experience and willingness to change their medication behaviors.
Patient assignment to pain duration categories was determined retrospectively based on information notated on the opioid callback form, but reviewing patients’ medication profiles (e.g., access to electronic health records) could have yielded different allocations. In this opioid callback program pilot, pharmacists discussed the same callback items with acute or chronic pain patients equally, except for naloxone use, which was discussed more with chronic pain patients. In the follow-up interviews, pharmacists expressed a need to differentiate approaches for acute or chronic opioid use patients, even focusing exclusively on acute pain patients because they may be more receptive to discussing safe opioid use. Incorporating into the callback form a recitation about the risks that opioids can pose for people beyond the patient may help patients appreciate naloxone’s importance and decide to acquire the opioid-reversal agent. Further research on these points, including the effect of pain duration on callback time, are warranted.
While naloxone as a rescue medication was discussed in our study, this pilot program did not reference other naloxone-specific interventions such as using educational brochures or distributing naloxone when an opioid medication is picked-up at the pharmacy. A recent study suggests that a follow-up phone, even if not completed, is associated with a greater likelihood that an order for a naloxone rescue kit will be agreed to by the patient, especially among non-white patients.46 The intervention impact on naloxone uptake for chronic versus acute pain patients remains unexplored.
Only 21% of patients participating in the opioid callback program stored medications in a locked container. This finding is consistent with previous research.33–35,47 In a pediatric-based study, parents were unconcerned with children accessing prescriptions in the house, with the primary reasons for nonuse of locked containers being access or a lack of thought about medication storage.48 Safely securing opioid medications is an important issue that needs to be promoted.
In our study, 70% of patients discussed opioid disposal options with the pharmacist. These findings align with prior research on awareness and use of appropriate opioid disposal.32–35,47 For orthopedic patients, the provision of a disposal packet when medications are dispensed increased the likelihood of disposal of unused medications or planned disposal.49 Even when patients report about medication disposal, the mechanisms are not appropriate. For example, in a project interviewing women who have underdone post-cesarean sections, 88% of women with leftover opioids reported disposing of the medications, but 20.7% of those disposed of the medications by flushing them, which contributes to environmental and human health risks associated with pharmaceutical pollution.50,51
While results were promising, this pilot project has several limitations. First, the project sample size was small and focused only on the callback and not prescription dispensing. Second, the conversation during the call was not observed, and may not have reflected complete fidelity to the callback data collection form but rather be guided by pharmacists’ judgement about what to discuss with the patient; similarly, it was not possible to determine that callbacks occurred for each opioid dispensed during the pilot time periods. Third, one pharmacy completed 92% of the opioid callbacks and opinions were limited to the pharmacist and pharmacy resident, so generalizability of the results to other community pharmacies is limited. Fourth, it was not possible to account for patients with more complete pain needs (i.e., acute or chronic pain). Finally, this study focused on pharmacists’ perspectives, so explorations of patient and provider perspectives are needed to gain a more complete understanding of the benefit of implementing an opioid callback program in pharmacies.
Disseminating the opioid callback program to more community pharmacies should include a comprehensive and consistent assessment of patient pain levels—acute versus chronic—to support these pilot findings. Opportunities exist for additional pharmacist-led patient educational initiatives regarding the importance of securing medications and opioid disposal options, either alone or with interventions (e.g., provision of lock boxes or disposal packets) provided when medications are dispensed.
Conclusion
Community pharmacists are well-positioned to help address the opioid crisis. This study presents a proof of concept for the feasibility of a pharmacist-led opioid callback program to raise awareness of opioid disposal opportunities and safe opioid practices, including storage and naloxone ownership. Expanding this promising opioid callback initiative, individually or combined with other initiatives, could inform patients about using opioids safely, treating an opioid overdose, and disposing of unused medications. It is only through the transdisciplinary, widespread, adoption of a variety of systemic interventions, including pharmacy-based opioid callback programs, that opioid-related morbidity and mortality can be more effectively mitigated.
Supplementary Material
Key Points.
Background:
Community pharmacists are widely accessible and uniquely qualified to offer guidance to patients on proper medication use and availability for patient follow-up once a medication is administered.
One acceptable approach used by community pharmacies to facilitate appropriate medication usage is patient callbacks.
Evidence suggests that pharmacist-provided education about naloxone and opioid abuse prevention, including disposal education, increases naloxone prescriptions and access to medication disposal.
Findings:
Proof of concept regarding the effectiveness of a community pharmacy based opioid callback program to raise awareness of appropriate opioid medication use, opioid disposal opportunities and safe opioid practices, including storage and naloxone ownership.
Patients with chronic pain were more likely to discuss safe opioid practices related to naloxone ownership and its importance as a rescue medication during the opioid callback with the pharmacist.
Community pharmacists found an opioid callback was acceptable to patients and easily integrated into existing workflows.
Funding:
This manuscript was supported by funding from NIDA-funded research (R01DA052975-01A1, Drs. McGovern and Ford, principal investigators). NIDA had no role in the preparation of or the decision to submit this report for publication. The statements made here are those of the authors.
Footnotes
Conflicts of Interest: The authors declare no relevant conflicts of interest or financial relationships.
Previous presentations of the work: An early draft of the results was presented at the 2022 American Pharmacy Association Annual Conference in San Antonio, Texas.
References
- 1.Centers for Disease Control and Prevention. U.S. Opioid Dispensing Rate Map. Available at: https://www.cdc.gov/drugoverdose/rxrate-maps/index.html#print. Published 2021. Accessed April 14, 2023.
- 2.American Medical Association. Report shows decreases in opioid prescribing, increase in overdoses. Available at: https://www.ama-assn.org/press-center/press-releases/report-shows-decreases-opioid-prescribing-increase-overdoses. Published 2021. Accessed April 14, 2023.
- 3.Centers for Disease Control and Prevention. CDC’s Efforts to Prevent Overdoses and Substance Use-Related Harms - 2022-2024. Available at: https://www.cdc.gov/drugoverdose/prevention/pdf/CDC-Efforts-to-Prevent-Overdoses_2022-2024.pdf. Published 2022. Accessed April 14, 2023.
- 4.Oelhaf RC, Del Pozo E, Azadfard M. Opioid Toxicity. In: StatPearls. Treasure Island (FL): StatPearls Publishing; January 1, 2023. [Google Scholar]
- 5.Substance Abuse and Mental Health Services Administration. Key substance use and mental health indicators in the United States: Results from the 2020 National Survey on Drug Use and Health (HHS Publication No. PEP21-07-01-003, NSDUH Series H-56). Rockville, MD: Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration. Retrieved from https://www.samhsa.gov/data/. Published 2021. Accessed April 14, 2023. [Google Scholar]
- 6.Biese K, Lamantia M, Shofer F, et al. A randomized trial exploring the effect of a telephone call follow-up on care plan compliance among older adults discharged home from the emergency department. Acad Emerg Med. 2014;21(2):188–195. doi: 10.1111/acem.12308 [DOI] [PubMed] [Google Scholar]
- 7.Luciani-McGillivray I, Cushing J, Klug R, Lee H, Cahill JE. Nurse-led call back program to improve patient follow-up with providers after discharge from the emergency department. J Patient Exp. 2020;7(6):1349–1356. doi: 10.1177/2374373520947925 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dudas V, Bookwalter T, Kerr KM, Pantilat SZ. The impact of follow-up telephone calls to patients after hospitalization. Am J Med. 2001;111(9B):26S–30S. doi: 10.1016/s0002-9343(01)00966-4 [DOI] [PubMed] [Google Scholar]
- 9.Beaucage K, Lachance-Demers H, Ngo TT, et al. Telephone follow-up of patients receiving antibiotic prescriptions from community pharmacies. Am J Health Syst Pharm. 2006;63(6):557–563. doi: 10.2146/ajhp050177 [DOI] [PubMed] [Google Scholar]
- 10.Ostrow O, Prodanuk M, Foong Y, et al. Decreasing misdiagnoses of urinary tract infections in a pediatric emergency department. Pediatrics. 2022;150(1):e2021055866. doi: 10.1542/peds.2021-055866 [DOI] [PubMed] [Google Scholar]
- 11.Paravattil B, Zolezzi M, Nasr Z, et al. An interventional call-back service to improve appropriate use of antibiotics in community pharmacies. Antibiotics. 2021;10(8):986. doi: 10.3390/antibiotics10080986 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Salmany SS, Ratrout L, Amireh A, et al. The impact of pharmacist telephone calls after discharge on satisfaction of oncology patients: a randomized controlled study. J Oncol Pharm Pract. 2018;24(5):359–364. doi: 10.1177/1078155217709616 [DOI] [PubMed] [Google Scholar]
- 13.Aloy-Prósper A, Pellicer-Chover H, Balaguer-Martínez J, Llamas-Monteagudo O, Peñarrocha-Diago M. Patient compliance to postoperative instructions after third molar surgery comparing traditional verbally and written form versus the effect of a postoperative phone call follow-up a: a randomized clinical study. J Clin Exp Dent. 2020;12(10):e909–e915. doi: 10.4317/jced.56680 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hess R. Impact of automated telephone messaging on zoster vaccination rates in community pharmacies. J Am Pharm Assoc (2003). 2013;53(2):182–187. doi: 10.1331/JAPhA.2013.12222 [DOI] [PubMed] [Google Scholar]
- 15.Rickles NM, Svarstad BL, Statz-Paynter JL, Taylor LV, Kobak KA. Pharmacist telemonitoring of antidepressant use: effects on pharmacist-patient collaboration. J Am Pharm Assoc (2003). 2005;45(3):344–353. doi: 10.1331/1544345054003732 [DOI] [PubMed] [Google Scholar]
- 16.Nietert PJ, Tilley BC, Zhao W, et al. Two pharmacy interventions to improve refill persistence for chronic disease medications: a randomized, controlled trial. Med Care. 2009;47(1):32–40. doi: 10.1097/MLR.0b013e3181808c17 [DOI] [PubMed] [Google Scholar]
- 17.Stolpe S, Choudhry NK. Effect of automated immunization registry-based telephonic interventions on adult vaccination rates in community pharmacies: a randomized controlled trial. J Manag Care Spec Pharm. 2019;25(9):989–994. doi: 10.18553/jmcp.2019.25.9.989 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Odegard PS, Christensen DB. MAP study: RCT of a medication adherence program for patients with type 2 diabetes. J Am Pharm Assoc (2003). 2012;52(6):753–762. doi: 10.1331/JAPhA.2012.11001 [DOI] [PubMed] [Google Scholar]
- 19.Kooij MJ, Heerdink ER, van Dijk L, van Geffen EC, Belitser SV, Bouvy ML. Effects of Telephone Counseling Intervention by Pharmacists (TelCIP) on medication adherence; results of a cluster randomized trial. Front Pharmacol. 2016;7:269. doi: 10.3389/fphar.2016.00269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Elliott RA, Boyd MJ, Tanajewski L, et al. ‘New Medicine Service’: supporting adherence in people starting a new medication for a long-term condition: 26-week follow-up of a pragmatic randomised controlled trial. BMJ Qual Saf. 2020;29(4):286–295. doi: 10.1136/bmjqs-2018-009177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kooy MJ, Van Geffen EC, Heerdink ER, Van Dijk L, Bouvy ML. Patients’ general satisfaction with telephone counseling by pharmacists and effects on satisfaction with information and beliefs about medicines: Results from a cluster randomized trial. Patient Educ Couns. 2015;98(6):797–804. doi: 10.1016/j.pec.2015.02.020 [DOI] [PubMed] [Google Scholar]
- 22.Margolis KL, Asche SE, Dehmer SP, et al. Long-term outcomes of the effects of home blood pressure telemonitoring and pharmacist management on blood pressure among adults with uncontrolled hypertension: follow-up of a cluster randomized clinical trial. JAMA Netw Open. 2018;1(5):e181617. doi: 10.1001/jamanetworkopen.2018.1617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Margolis KL, Asche SE, Bergdall AR, et al. Effect of home blood pressure telemonitoring and pharmacist management on blood pressure control: a cluster randomized clinical trial. JAMA. 2013;310(1):46–56. doi: 10.1001/jama.2013.6549 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Preuss CV, Kalava A, King KC. Prescription of Controlled Substances: Benefits and Risks. In: StatPearls. StatPearls Publishing; 2023. Accessed July 26, 2023. Available at: http://www.ncbi.nlm.nih.gov/books/NBK537318/ [Google Scholar]
- 25.U.S. Department of Health and Human Services Press Office. HHS Acting Secretary Declares Public Health Emergency to Address National Opioid Crisis. Published 2017. Accessed July 26, 2023. Available at: https://public3.pagefreezer.com/browse/HHS.gov/31-12-2020T08:51/https:/www.hhs.gov/about/news/2017/10/26/hhs-acting-secretary-declares-public-health-emergency-address-national-opioid-crisis.html
- 26.Blanco C, Wiley TRA, Lloyd JJ, Lopez MF, Volkow ND. America’s opioid crisis: the need for an integrated public health approach. Transl Psychiatry. 2020;10:167. doi: 10.1038/s41398-020-0847-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Volkow ND, Blanco C. The changing opioid crisis: development, challenges and opportunities. Mol Psychiatry. 2021;26(1):218–233. doi: 10.1038/s41380-020-0661-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.National Association of Chain Drug Stores. Pharmacies. The face of neighborhood healthcare. Available at: https://www.nacds.org/community-spotlight/. Published 2023. Accessed April 14, 2023.
- 29.Agency for Healthcare Research and Quality Patient Safety Network. The Pharmacist’s Role in Medication Safety. Available at: https://psnet.ahrq.gov/primer/pharmacists-role-medication-safety. Published 2019. Accessed April 14, 2023.
- 30.York AS. Role of the pharmacist in proper medication disposal. US Pharm. 2011;36(7):52–55. Available at: https://www.uspharmacist.com/article/role-of-the-pharmacist-in-proper-medication-disposal. Accessed April 14, 2023. [Google Scholar]
- 31.Maeng DD, Tom LA, Wright EA. Patient characteristics and healthcare utilization patterns associated with unused medications among medicare patients. Res Social Adm Pharm. 2017;13(6):1090–1094. doi: 10.1016/j.sapharm.2016.11.003 [DOI] [PubMed] [Google Scholar]
- 32.Kearney M, Reynolds L, Blitzstein S, Chapin K, Massey P. Primary prevention of prescription drug misuse among culturally and linguistically diverse suburban communities. J Community Health. 2019;44(2):238–248. doi: 10.1007/s10900-018-0579-9 [DOI] [PubMed] [Google Scholar]
- 33.Reddy A, de la Cruz M, Rodriguez EM, et al. Patterns of storage, use, and disposal of opioids among cancer outpatients. Oncologist. 2014;19(7):780–785. doi: 10.1634/theoncologist.2014-0071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.de la Cruz M, Reddy A, Balankari V, et al. The impact of an educational program on patient practices for safe use, storage, and disposal of opioids at a comprehensive cancer center. Oncologist. 2017;22(1):115–121. doi: 10.1634/theoncologist.2016-0266 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cooper JN, Lawrence AE, Koppera S, et al. Effect of drug disposal bag provision on families’ disposal of children’s unused opioids. J Am Pharm Assoc (2003). 2021;61(1):109–114.e2. doi: 10.1016/j.japh.2020.10.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Shafer E, Bergeron N, Smith-Ray R, Robson C, O’Koren R. A nationwide pharmacy chain responds to the opioid epidemic. J Am Pharm Assoc (2003). 2017;57(2S):S123–S129. doi: 10.1016/j.japh.2016.12.075 [DOI] [PubMed] [Google Scholar]
- 37.Duvivier H, Gustafson S, Greutman M, et al. Indian Health Service pharmacists engaged in opioid safety initiatives and expanding access to naloxone. J Am Pharm Assoc (2003). 2017;57(2S):S135–S140. doi: 10.1016/j.japh.2017.01.005 [DOI] [PubMed] [Google Scholar]
- 38.Oliva EM, Christopher MLD, Wells D, et al. Opioid overdose education and naloxone distribution: Development of the Veterans Health Administration’s national program. J Am Pharm Assoc (2003). 2017;57(2S):S168–S179.e4. doi: 10.1016/j.japh.2017.01.022 [DOI] [PubMed] [Google Scholar]
- 39.Ford JH, Gilson AM, Bryan G, Augustine C, Gassman M, Mott DA. Community pharmacy-based injectable naltrexone service delivery models and best practices. Res Social Adm Pharm. 2021;17(7):1332–1341. doi: 10.1016/j.sapharm.2020.10.004 [DOI] [PubMed] [Google Scholar]
- 40.Watt S. Clinical decision-making in the context of chronic illness. Health Expect. 2000;3(1):6–16. doi: 10.1046/j.1369-6513.2000.00076.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Buffington DE, Lozicki A, Alfieri T, Bond TC. Understanding factors that contribute to the disposal of unused opioid medication. J Pain Res. 2019;12:725–732. doi: 10.2147/JPR.S171742 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Dyson MP, Dong K, Sevcik W, et al. Quantifying unused opioids following emergency and ambulatory care: a systematic review and meta-analysis. J Am Coll Emerg Physicians Open. 2022;3(5):e12822. Published 2022. Sep 30. doi: 10.1002/emp2.12822 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Yang C, Stilley JAW, Bedy SC, Goddard KB, Sampson CS. Leftover narcotic analgesics among emergency department patients and methods of disposal. J Am Coll Emerg Physicians Open. 2020;1(6):1486–1492. doi: 10.1002/emp2.12161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Dumkow LE, Beuschel TS, Brandt KL. Expanding Antimicrobial Stewardship to Urgent Care Centers Through a Pharmacist-Led Culture Follow-up Program. Infect Dis Ther. 2017;6(3):453–459. doi: 10.1007/s40121-017-0168-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Entwistle V, Prior M, Skea ZC, Francis JJ. Involvement in treatment decision-making: its meaning to people with diabetes and implications for conceptualisation. Soc Sci Med. 2008;66(2):362–375. doi: 10.1016/j.socscimed.2007.09.001 [DOI] [PubMed] [Google Scholar]
- 46.Hoefling AD, Ash LR, Linneman TW. Impact of pharmacist contact via telephone vs letter on rate of acquisition of naloxone rescue kits by patients with opioid use disorder. Subst Abus. 2021;42(4):625–629. doi: 10.1080/08897077.2020.1809606 [DOI] [PubMed] [Google Scholar]
- 47.Bicket MC, Long JJ, Pronovost PJ, Alexander GC, Wu CL. Prescription opioids commonly unused after surgery: a systematic review. JAMA Surg. 2017;152(11):1066–1071. doi: 10.1001/jamasurg.2017.0831 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Webb AC, Nichols MH, Shah N, Monroe KW. Effect of lock boxes and education on safe storage of medications. Inj Epidemiol. 2020;7(Suppl 1):21. doi: 10.1186/s40621-020-00257-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Roberts S, Peyatt NO, Bunkley D. At your disposal: a pilot for safely discarding medication in postoperative patients. J Am Pharm Assoc (2003). 2022;62(1):237–240. doi: 10.1016/j.japh.2021.08.004 [DOI] [PubMed] [Google Scholar]
- 50.Loomis EA, McNaughton D, Genord C. A quality improvement initiative addressing safe opioid prescribing and disposal postcesarean delivery. Pain Manag Nurs. 2022;23(2):174–179. doi: 10.1016/j.pmn.2021.02.002 [DOI] [PubMed] [Google Scholar]
- 51.Wilkinson JL, Boxall ABA, Kolpin DW, et al. Pharmaceutical pollution of the world’s rivers. Proc Natl Acad Sci USA. 2022;119(8):e2113947119. doi: 10.1073/pnas.2113947119 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


