Abstract
Background
Surgical treatment of chronic rhinosinusitis with nasal polyps is an established treatment for medically resistant nasal polyp disease. Whether a nasal polypectomy with additional sinus dissection offers any advantage over an isolated nasal polypectomy has not been systematically reviewed.
Objectives
To assess the effectiveness of simple polyp surgery versus more extensive surgical clearance in chronic rhinosinusitis with nasal polyps.
Search methods
We searched the Cochrane Ear, Nose and Throat Disorders Group Trials Register; the Cochrane Central Register of Controlled Trials (CENTRAL 2014, Issue 1); PubMed; EMBASE; CINAHL; Web of Science; Cambridge Scientific Abstracts; ICTRP and additional sources for published and unpublished trials. The date of the search was 20 February 2014.
Selection criteria
Randomised and quasi‐randomised controlled trials in patients over 16 with chronic rhinosinusitis with nasal polyps, who have failed a course of medical management and who have not previously undergone any previous surgical intervention for their nasal disease. Studies compared nasal polypectomy with more extensive sinus clearance in this patient cohort.
Data collection and analysis
We used the standard methodological procedures expected by The Cochrane Collaboration.
Main results
We identified no trials which met our inclusion criteria. Six controlled trials (five randomised) met some but not all of the inclusion criteria and were therefore excluded from the review.
Authors' conclusions
We are unable to reach any conclusions as to whether isolated nasal polypectomy or more extensive sinus surgery is a superior surgical treatment modality for chronic rhinosinusitis with nasal polyps. There is a need for high‐quality randomised controlled trials to assess whether additional sinus surgery confers any benefit when compared to nasal polypectomy performed in isolation.
Keywords: Humans, Chronic Disease, Nasal Polyps, Nasal Polyps/complications, Nasal Polyps/surgery, Rhinitis, Rhinitis/complications, Rhinitis/surgery, Sinusitis, Sinusitis/complications, Sinusitis/surgery
Plain language summary
Surgical interventions for chronic rhinosinusitis with nasal polyps
Background
Benign nasal polyps are abnormal tissue growths inside the nasal passages and sinuses, often on both sides of the nose. They can cause a wide array of symptoms including blocked nose, poor sense of smell that can lead to a loss of taste, runny nose and nasal congestion. Sinuses are air‐filled cavities in the bones of the face, which are in continuity with the nasal passages. The first‐line treatment for nasal polyps is usually medical therapy in the form of steroids ‐ as sprays (topically) or by mouth (orally). In patients where this treatment has failed to relieve the symptoms, the polyps can be removed surgically. These surgical procedures are often not curative and patients may need to continue medical therapy or undergo further surgeries. A number of well‐established surgical techniques can be used to remove polyps. What has not been established is whether removing the nasal polyps and clearing out the sinuses offers any advantage in the control of the disease when compared to simply removing the polyps and leaving the sinuses unchanged. We sought evidence in the literature to establish whether there was any difference in patients who underwent nasal polyp removal alone versus those who had nasal polyps removed as well as opening up of the sinuses.
Study characteristics
No trials met our inclusion criteria. We did identify six controlled trials (five of which were randomised) in which some but not all of our inclusion criteria were met, but we had to exclude these studies from the review.
Key results
No trials met our inclusion criteria.
Quality of evidence
At present, we cannot comment on whether taking nasal polyps out alone or also opening up the sinuses at the same time is a better treatment for patients with this disease. There is a need for high‐quality randomised controlled trials to answer this question. This evidence is current to February 2014.
Background
Description of the condition
Nasal polyps are tumour‐like, hyperplastic swellings of the nasal mucosa, most commonly originating from within the ostiomeatal complex (Larsen 2004). They are a common problem; the prevalence is estimated at 0.2% to 4% in worldwide studies (Johansson 2003; Lange 2013; Min 1996). There is at least a 2:1 male to female predominance. The incidence of symptomatic nasal polyps increases with age, reaching a peak in individuals aged 50 to 59 years, and then declines (Larsen 2004). While polyps can be asymptomatic, they may produce symptoms such as nasal obstruction, congestion, facial pressure and anosmia, and are associated with significant reduction in quality of life (Radenne 1999). Nasal polyps are usually found in association with chronic rhinosinusitis (CRS), which is broadly divided into two phenotypes based on the presence (CRSwNP) or absence of polyps (CRSsNP) on examination. Chronic rhinosinusitis with nasal polyps is a chronic disease, with a clinical course often lasting over 20 years (Vento 2000).
Definition
Nasal polyps are considered a subgroup of chronic rhinosinusitis. The European Position Paper on Rhinosinusitis and Nasal Polyps defines these conditions clinically as inflammation of the nose and paranasal sinuses, associated with two or more of the following symptoms (Fokkens 2012):
blockage/congestion; discharge (anterior or post‐nasal drip); facial pain/pressure; reduction of smell; and
either endoscopic evidence of polyps; mucopurulent discharge from the middle meatus or oedema/mucosal obstruction primarily in the middle meatus; and/or mucosal changes within the ostiomeatal complex or sinuses on computed tomography (CT) imaging.
Chronic rhinosinusitis with nasal polyps is then further defined by the endoscopic visualisation of polyps bilaterally in the middle meatus. They are defined as chronic when symptoms persist for more than 12 weeks.
Histology
Histologically, polyps consist of extracellular oedema with an associated inflammatory cell infiltrate, with a surface covering of respiratory epithelium, often with areas of metaplasia (Larsen 1989). The inflammatory cells found are characterised by type 2 T‐helper cell (Th2) inflammation, predominantly eosinophils (Stoop 1993), in addition to mast cells, lymphocytes, neutrophils and plasma cells (Pawliczak 2005). Numerous inflammatory mediators, growth factors and adhesion molecules are increased, including interleukins (IL), particularly IL‐5, interferon Y, RANTES, granulocyte macrophage colony stimulating factor, eosinophilic cationic protein and p‐selectin (Bateman 2003).
Aetiology
Nasal polyps are thought to be a manifestation of chronic inflammation, where they represent the final common pathway of several disease processes, the trigger for which is still unknown. There are numerous theories including hereditary factors, anatomical factors, systemic and local allergy, and infection.
A positive family history of nasal polyps has been found in 14% of polyp patients (Greisner 1996), and nasal polyps have developed even when identical twins have been exposed to different environmental factors, suggesting a genetic link. Human leukocyte antigens (HLA) have been associated with an increased susceptibility to developing nasal polyps (Molnar‐Gabor 2000).
Anatomically, mucosal contact within the nose has been postulated to cause an inflammatory reaction or mucociliary stasis, with subsequent cytokine release leading to polyp formation (Stammberger 1991). However, mucosal contact also occurs without polyp formation (Jones 1997). Osteomeatal occlusion secondary to an anatomical abnormality or mucosal oedema has also been suggested as an initiator of inflammation.
The eosinophilia, mast cell degranulation and high immunoglobulin (Ig) E levels found in nasal polyps suggest that allergy is a factor in polyp formation. However, when 3000 atopic patients were assessed only 0.5% had nasal polyps on anterior rhinoscopy (although it is well understood that anterior rhinoscopy may underestimate polyp presence) (Caplin 1971). Similarly, objective measures of atopy (such as skin prick testing) were no more common in nasal polyp patients than in controls (Jamal 1987). A local allergic response within the nose may be responsible for nasal polyps, since it has been shown that total and specific IgE in polyp tissue correlates with the degree of eosinophilia, but is unrelated to positive skin prick tests (Bachert 2001). The allergens responsible may be bacterial, as bacterial‐specific IgE has been identified in patients with nasal polyps but not in those with allergic rhinitis (Calenoff 1993). Food‐based allergens may also be responsible, with positive intradermal tests for food allergens having been reported in 70% of chronic rhinosinusitis with nasal polyps patients (Collins 2006).
Infection may trigger immunologic events leading to the development of chronic rhinosinusitis with nasal polyps. Staphylococcus aureus has been found to colonise the nose in two‐thirds of patients with nasal polyps, compared with less than a third of controls and patients with chronic rhinosinusitis without nasal polyps (van Zele 2004). IgE antibodies have been found in nasal polyp tissue that are specific to Staphylococcus aureus enterotoxins SE‐A and B (Bachert 2001), indicating that superantigens are likely to be involved in the pathogenesis. Superantigens are toxins of microbial or viral origin that target the immune system, triggering polyclonal T‐cell proliferation and activation. They have the ability to bypass conventional restrictions of the immune system triggering massive cytokine release. Therefore they could induce IgE synthesis leading to eosinophilic inflammation. Colonisation, however, does not always lead to production of superantigens and other factors must be involved (Zhang 2005).
True type 1 allergic fungal sinusitis is characterised by diffuse nasal polyposis. The increasingly widespread demonstration of fungi in the nasal cavity and sinuses in patients with chronic rhinosinusitis has led to the suggestion that fungal colonisation may play an aetiological role in all polyps (Ponikau 1999), recruiting eosinophils and leading to release of inflammatory mediators. However, fungi may be found in normal subjects and the majority of polyp patients lack positive skin prick tests to fungal allergens (Drake‐Lee 1984).
There are clear associations between chronic rhinosinusitis with nasal polyps and other diseases. The prevalence of nasal polyps in asthmatic patients is reported to be as high as 13%. However, in those patients with nasal polyps, the prevalence of asthma is as high as 45% (Rugina 2002). There is an even stronger association in patients with aspirin hypersensitivity and bronchial asthma; more than 90% of these patients have severe nasal polyposis. This association is now referred to as aspirin‐exacerbated respiratory disease (AERD), having been previously termed 'Samter's triad' (Samter 1968). Nasal polyps are also associated with cystic fibrosis, ciliary dyskinesis syndromes (Kartagener's syndrome, Young's syndrome) and eosinophilic granulomatosis with polyangiitis (EGPA, Churg Strauss syndrome).
In summary, nasal polyps are likely to represent the end result of many different mechanisms and the search for a single aetiological factor may be in vain. Regardless of trigger, the end result is a failure to mount an appropriate immune response to antigens in the nose and sinuses, resulting in chronic inflammation (Chin 2013).
Description of the intervention
The management of chronic rhinosinusitis with nasal polyps involves both medical and surgical approaches and remains a controversial subject. A variety of intranasal corticosteroids form the mainstay of conservative management, with good evidence for their efficacy. A number of randomised, placebo‐controlled trials document statistically significant improvements in subjective symptom scores, polyp size and objective nasal flow rates following topical steroid use (Kalish 2012). Symptoms of nasal obstruction can be controlled in anywhere from 50% up to 80% of patients. However, clinical studies indicate that the management of anosmia is poor, especially when compared with systemic steroids. Adverse effects from nasal steroids are few, and range from epistaxis to headaches and dizziness. Using the more modern formulations, such as fluticasone or mometasone, there is minimal systemic absorption and the dose is well below that required for adrenal suppression. A meta‐analysis to assess the effectiveness of topical steroids has shown that intranasal corticosteroids are effective in the treatment of rhinosinusitis and that prior sinus surgery and direct sinus delivery methods enhance their effectiveness (Snidvongs 2011).
The use of systemic steroids (often termed medical polypectomy) has also shown to be effective. Two randomised controlled trials comparing placebo to systemic steroids show benefit with oral prednisolone (Alobid 2012; Vaidyanathan 2011). Unlike topical therapy, systemic steroids appear to be effective in improving the sense of smell (van Camp 1994). However, there is a high rate of recurrence of symptoms once oral steroids are stopped (Lildholdt 1989). The use of oral steroids is limited by their toxicity, with adverse effects including weight gain, immunosuppression and adrenal suppression. Using a combination of topical and intermittent oral steroids, reasonable symptom control can be achieved in the majority of patients (Slavin 1997). A Cochrane review supports the use of systemic steroids in the treatment of nasal polyposis (Martinez‐Devesa 2011)
Alternative preparations used in the management of polyposis are reported in the literature, but lack the evidence base of corticosteroids. It has been suggested that treatment with the leukotriene inhibitors has resulted in improvement and resolution of polyps, particularly in patients with aspirin sensitivity (Parnes 2002). Macrolide antibiotics have been proposed to have therapeutic activity based on their anti‐inflammatory properties. Long‐term, low‐dose macrolide antibiotic treatment has been shown to reduce IL‐8 production in nasal polyps and decrease their size (Yamada 2000). However, subgroup analysis of a placebo‐controlled trial suggests benefit is limited to patients with normal levels of IgE (Cervin 2014). New approaches, particularly targeting eosinophilic recruitment, are evolving. Interleukins, particularly IL‐5 and eotaxin (but also IL‐13 and IL‐8) may play a major role in polyposis (Bachert 2000). IL‐5 is essential for maturation of eosinophils in the bone marrow and orchestrates their migration into the tissues. Blockage of IL‐5 and eotaxin production, chemokine receptors and other sites in the inflammatory pathway using neutralising monoclonal antibodies is currently being investigated in patients with asthma, rhinitis and nasal polyps. While these approaches may offer alternatives to corticosteroid treatment or surgery, at present large‐scale controlled trials are lacking.
Surgery
In cases of marked mechanical obstruction of the airways or chronic disease unresponsive to maximal medical therapy, surgical intervention is the treatment of choice (Slavin 1997). Occlusion of the nasal passages by large polyps may be treated by simple polypectomy to restore patency of the nasal airway. The spectrum of surgical options ranges from simple polypectomy using a snare or forceps, surgery entering into the sinuses, through to radical 'nasalisation' of the sinuses. Simple polypectomy has been reported since the times of Hippocrates (Vancil 1969), but is associated with an extraordinarily high recurrence rate; as high as 75% in an eight‐year follow‐up study (Larsen 1997). Considerable changes have taken place over the last two decades in the surgical approach to nasal polyposis (Stammberger 1999). The advent of the endoscope enables earlier detection and more precise surgical treatment of polyposis. The concept of functional endoscopic sinus surgery (FESS) developed in relation to the management of chronic rhinosinusitis, and is aimed at restoring the physiological properties of the nose and allowing drainage of the infected sinuses by removing polyps and other causes of obstruction from the ethmoid sinuses and lateral nasal wall. Such endoscopic surgical techniques have been applied in polyposis and have been reported to be associated with lower rates of recurrence than simple polypectomy (Lanza 1992), although the value of different surgical techniques remains controversial. Stammberger initially described tailoring the extent of surgery undertaken to the limits of the disease found at operation (Stammberger 1991). Further modification in this technique has resulted in the concept of the 'minimally invasive sinus technique' (Catalano 2004), a technique characterised by conservative dissection using powered instrumentation, preservation of the mucosa and the avoidance of surgery to the middle meatus. At the other end of the spectrum, some surgeons advocate 'nasalisation' ‐ radical surgery removing all the bony lamellae of the ethmoid labyrinth, forming a large middle meatal antrostomy and opening the sphenoid sinuses (Jankowski 1997). It is possible that the widespread mucosal inflammation may be better treated in the postoperative period with topical therapies if wide access has been achieved by more extensive surgery (Chin 2013). While most surgeons probably operate between these two extremes, there is limited evidence comparing the techniques. Surgical management of any extent is associated with the risk of haemorrhagic, orbital or intracranial complications. The risk of major complications was found to be small (0.03%) in a prospective cohort study (Hopkins 2006), but must be considered when embarking on surgical treatment.
The mechanism of surgery in improving symptom control in chronic rhinosinusitis with nasal polyps is unclear. Eosinophilic chronic rhinosinusitis, typically associated with nasal polyps, does not appear to be a disease where obstruction of the sinus drainage at the ostiomeatal complex is key to the pathophysiology (Snidvongs 2013). Therefore, it is not clear that surgery to the ostiomeatal complex or sinuses will offer additional benefit over removing those polyps that obstruct the nasal cavity. The lack of high‐quality evidence to guide surgeons in planning the extent of surgery performed leads to significant variation in practice (Sinonasal Audit 2006).
Staging and outcome assessment
As curative treatment is hard to achieve in polyposis, management is primarily aimed at reducing symptom severity. It is therefore important to include a measurement of health‐related quality of life when assessing the severity of disease or outcome of treatment. The duration and severity of individual symptoms may be measured numerically, or using visual analogue scales. In addition, there are now many validated questionnaires available that may measure general health, or disease‐specific quality of life. Several instruments have been designed and validated to measure disease‐specific quality of life in sinonasal disease and some examples are shown in Table 1.
1. Health‐related quality of life instruments for rhinosinusitis.
| Instrument | Details |
| Rhinosinusitis Outcome Measure (RSOM‐31) (Piccirillo 1995) | 31 items in 7 domains: nasal, eye, ear, sleep, general, practical and emotional problems. 2 rating scales: magnitude and importance of each item. Each item is measured on a 0 to 10 cm visual analogue scale (VAS). The minimal important difference (MID) is greater than 1. Time‐consuming and complex scoring system |
| 20‐item Sinonasal Outcome Test (SNOT‐20) (Piccirillo 2002) | 20‐item modification of RSOM‐31, in 5 domains. Patients rate the magnitude of each item and the 5 most important items. Each item is rated on a 6‐point scale (0 = no problem, 5 = most serious problem) (range 0 to 100). Complex scoring system because of weighting for important symptoms. Excludes nasal blockage and anosmia |
| 22‐item Sinonasal Outcome Test (SNOT‐22) (Hopkins 2009) | Modification of SNOT‐20, including nasal blockage and anosmia. Patients rate the magnitude of each item. Each item is rated on a 6‐point scale (0 = no problem, 5 = most serious problem) (range 0 to 110). Excludes weighting for most important symptoms. The minimal important difference (MID) is greater than 8.9 |
Alternatively, severity may be measured using clinical indicators of disease. Polyps are graded by convention as: grade I ‐ confined to the middle meatus; grade II ‐ extending below the level of the middle turbinate; and grade III ‐ causing total obstruction. Endoscopic examination may assess the condition of the nasal mucosa and demonstrate recurrent disease following treatment. The Lund‐Mackay staging system generates a simple numeric score from the CT scan (and hence is available only when such imaging is performed) and may be used to stage the extent of inflammatory disease within the sinuses on cross‐sectional imaging (Lund 1997). The total score ranges from 0 to 24. The Lund‐Mackay score in 'normal' individuals in the absence of symptoms or signs of chronic rhinosinusitis has been found to be four. The score does not reflect the extent of polyps in the nasal cavity, but some studies have found an association between the score and the likelihood of recurrence following treatment (Kennedy 1992).
Nasal obstruction may be estimated using peak nasal inspiratory flow rates, acoustic rhinometry (which measures the cross‐sectional area of the nasal cavity) or rhinomanometry (which measures nasal resistance), although the correlation between such measurements and subjective symptoms of blockage is poor in some studies.
Revision surgery rates or recurrent topical steroid usage may be used as evidence of treatment failure.
A discrepancy between 'subjective' symptomatic improvement reported by patients following surgical treatment for polyposis and 'objective' endoscopic evidence of resolution of disease in response to surgery has been described (Kennedy 1992). The ideal study should therefore include both patient‐based and clinical measures of outcome.
Why it is important to do this review
In summary, both the aetiology and the most effective management of chronic rhinosinusitis with nasal polyps remain unknown. Studies have shown that patients with chronic sinusitis report poorer quality of life scores than patients with conditions including angina, congestive heart failure and chronic back pain (Glicklich 1995). In the US, chronic sinusitis has been shown to account for 12 million doctor visits and 70 million restricted activity days annually (Adams 1999). Different surgical techniques may achieve different outcomes, incur differing financial costs (met by either the patient or health care provider) and be associated with higher or lower risks of complications and rates of revision surgery. This is a chronic and common problem, which is currently treated in a variety of ways and hence merits review to identify the optimum treatment.
The comparison of medical versus surgical interventions for chronic rhinosinusitis with nasal polyps is assessed in a separate Cochrane review (Rimmer 2014).
Objectives
To assess the effectiveness of simple polyp surgery versus more extensive surgical clearance in chronic rhinosinusitis with nasal polyps.
Methods
Criteria for considering studies for this review
Types of studies
Randomised controlled trials, where the unit of randomisation is the patient. We excluded any randomised studies in which the patient acts as their own control, i.e. one side of the nose is treated with one surgical technique and the other side is treated with another ('split‐nose' studies). This can introduce a high risk of bias, as ongoing inflammation on one side may affect the rate of recurrence on the contralateral side, thus confounding a particular surgical technique. Additionally, patient‐reported outcome tools become more difficult for patients to complete as they are doing so on an 'each nostril' basis.
As the mean time between revision procedures has been shown to be six years in a large, multicentre cohort study (Sinonasal Audit 2006), included studies should ideally have a follow‐up period of many years. However, we planned to include all studies, but to clearly state follow‐up time and, where multiple time points were reported, we would analyse only the longest follow‐up data in each study.
Types of participants
Patients over 16 with chronic rhinosinusitis with nasal polyps confirmed by direct visualisation (preferably, but not exclusively with an endoscope). We did not consider duration of polyposis as an inclusion criterion.
We excluded studies involving patients under 16 and patients undergoing revision surgery. We also excluded patients with known malignancy and those with unilateral polyps shown to be inverting papillomas.
As patients should ideally be managed medically prior to considering surgical treatment, all patients enrolled in included trials should have failed an acceptable trial of topical steroid therapy prior to being randomised. However, we considered all studies as long as pre‐operative treatment was the same in all patients.
Types of interventions
Simple polypectomy versus more extensive surgery entering the sinuses.
Simple polypectomy may be defined as the removal of polyps alone, without intentionally entering the sinuses or enlarging the natural ostia. We accept that during the removal of polyps, the sinuses may be inadvertently entered. More extensive surgery involves ventilation and extirpation of the sinus complexes in addition to the removal of polyps. This usually progresses in a stepwise manner, but may vary from limited surgery to the middle meatus through to radical clearance of all the sinuses (nasalisation). In the UK, the extent of surgery is usually tailored to the severity of mucosal disease demonstrated on cross‐sectional imaging. If possible, additional sinus surgery may be subdivided into surgery involving only the ostiomeatal complexes, surgery to the ethmoids and surgery extending beyond the ethmoids (these subdivisions are arbitrary and could be adjusted). Surgery may also vary in its approach (intranasal, sublabial or external), illumination (headlamp, microscope or endoscope) and removal technique. Removal may be performed using snare, forceps, laser or mechanical microdebrider. We planned to look at these as subgroups if the data allowed, but the technique was not expected to be as important as the extent of surgery undertaken.
In addition, we planned (if such studies existed) to consider studies where patients were randomised to surgery entering the sinuses of differing extent (for example, surgery involving only the ostiomeatal complex versus nasalisation).
Types of outcome measures
We analysed the following outcomes in the review, but they were not used as a basis for including or excluding studies.
Primary outcomes
Disease severity, as measured by patient‐reported disease‐specific symptom scores. This includes rating of nasal obstruction and other sinonasal symptoms (using visual analogue scales or other methods).
Health‐related quality of life, using disease‐specific health‐related quality of life scores, such as the Sinonasal Outcome Test‐22 (SNOT‐22) (Table 1).
Health‐related quality of life, using generic quality of life scores, such as the SF‐36.
Secondary outcomes
Endoscopic appearances (there is no single accepted endoscopic grading system).
Complications from surgery or medical treatment: epistaxis, infection, orbital complications, intracranial complications, intolerance to medication or other medication side effects.
Recurrence rate; if available we used the disease‐free interval.
Objective physiological measures: nasal peak flow, nasal volume, nasal cross‐sectional area, nasal nitric oxide (nNO), ciliary function.
Olfactory tests.
We did not consider postoperative medication use, as this may be either reactive to recurrence or prophylactic.
Search methods for identification of studies
We conducted systematic searches for randomised controlled trials. There were no language, publication year or publication status restrictions. The date of the search was 20 February 2014.
Electronic searches
We searched the following databases from their inception for published, unpublished and ongoing trials: the Cochrane Ear, Nose and Throat Disorders Group Trials Register; the Cochrane Central Register of Controlled Trials (CENTRAL 2014, Issue 1); PubMed; EMBASE; CINAHL; LILACS; KoreaMed; IndMed; PakMediNet; CAB Abstracts; Web of Science; ISRCTN; ClinicalTrials.gov; ICTRP, Google Scholar and Google. In searches prior to 2013, we also searched BIOSIS Previews 1926 to 2012 and CNKI.
We modelled subject strategies for databases on the search strategy designed for CENTRAL. Where appropriate, we combined subject strategies with adaptations of the highly sensitive search strategy designed by The Cochrane Collaboration for identifying randomised controlled trials and controlled clinical trials (as described in theCochrane Handbook for Systematic Reviews of Interventions Version 5.1.0, Box 6.4.b. (Handbook 2011). Search strategies for major databases including CENTRAL are provided in Appendix 1
Searching other resources
We scanned the reference lists of identified publications for additional trials and contacted trial authors where necessary. In addition, we searched PubMed, TRIPdatabase, The Cochrane Library and Google to retrieve existing systematic reviews relevant to this systematic review, so that we could scan their reference lists for additional trials. We searched for conference abstracts using the Cochrane Ear, Nose and Throat Disorders Group Trials Register.
Data collection and analysis
Selection of studies
The Cochrane ENT Group's Trials Search Co‐ordinator used reference management software to merge search results and remove duplicate records of the same report. Two authors (Rishi Sharma (RS) and Claire Hopkins (CH)) independently examined titles and abstracts to remove obviously irrelevant reports. We retrieved the full text of any reports potentially meeting the inclusion criteria and examined these independently to determine study eligibility. Where necessary we contacted/attempted to contact study authors to obtain additional information to clarify study eligibility. We identified and linked multiple reports of the same study, or excluded them if duplicated or not relevant. We discussed study selection and there were no differences to resolve.
Data extraction and management
Two authors (RS and CH) independently extracted data from the studies using a standardised data form. The data categories collected were:
source;
eligibility;
methods;
participants;
interventions;
outcomes;
results; and
key conclusions of the study authors.
We discussed the extracted data; there were no disagreements between the authors involved.
Assessment of risk of bias in included studies
RS and Raj Lakhani (RL) were to undertake assessment of the risk of bias of the included trials independently, taking the following into consideration, as guided by theCochrane Handbook for Systematic Reviews of Interventions (Handbook 2011):
sequence generation;
allocation concealment;
blinding;
incomplete outcome data;
selective outcome reporting; and
other sources of bias.
We planned to use the Cochrane 'Risk of bias' tool in RevMan 5 (RevMan 2014), which involves describing each of these domains as reported in the trial and then assigning a judgement about the adequacy of each entry: high, low or unclear (or unknown) risk of bias.
Measures of treatment effect
Where data were comparable we planned to pool to give a summary measure of effect. We intended to use the risk ratio or odds ratio for dichotomous data and for continuous data the mean difference (for data from the same scale) or standardised mean difference (for data from different scales).
Unit of analysis issues
The units of randomisation and analysis in the included trials should be at the level of the individual. We excluded studies in which each individual trial participant acted as their own control (i.e. one side of the nose was randomised to a specific surgical technique and the other side another surgical technique) (see Types of studies). Where studies presented results at multiple time points during follow‐up (e.g. one month, six months and one year), we planned to only analyse the longest follow‐up from each study, as we were looking at a chronic disease and wished to avoid the risk of multiplicity of analysis.
Dealing with missing data
Where data were missing, we planned to attempt to contact the original investigators to request the missing data. Where this was not possible we would have assumed that the data were missing at random and analysed on an intention‐to‐treat (ITT) basis, as this is more likely to reflect real life when patients do not attend for follow‐up review.
Assessment of heterogeneity
We planned to evaluate studies for clinical and methodological heterogeneity on the basis of the treatment protocols used and the outcomes measured in each. A meta‐analysis would be considered appropriate if treatment protocols were broadly comparable and the appropriate outcome data were available. We planned to examine statistical heterogeneity visually, using confidence intervals where available, or using the I2 statistic and the Chi2 test.
Assessment of reporting biases
We addressed publication bias by including trial databases in the electronic search, looking for published, unpublished and ongoing trials. Where potentially eligible but unpublished trials were identified, we contacted the authors to ask for results (where available). We addressed multiple publication bias by combining papers that described different results from the same study, and by excluding papers that reported results that had already been published. We addressed language bias by including all languages in the search strategy and obtaining a translation when necessary. We addressed outcome reporting bias by assessing the risk of bias from within‐study selective reporting and selective under‐reporting of data.
Data synthesis
We planned to analyse data on an intention‐to‐treat (ITT) basis. Where data were comparable we planned to pool data to give a summary measure of effect. The risk ratio or odds ratio was to be used for dichotomous data and for continuous data the mean difference (for data from the same scale) or standardised mean difference (for data from different scales). We planned to use study risk of bias in a sensitivity analysis.
If meta‐analysis was possible, we planned to use the fixed‐effect model in the absence of significant heterogeneity and the random‐effects model if heterogeneity was present.
Subgroup analysis and investigation of heterogeneity
We planned to examine statistical heterogeneity using the I2 statistic and the Chi2 test. We intended to explore clinical heterogeneity by subgroup analysis as appropriate. Potential subgroups included:
nasal polyps in asthma patients;
cystic fibrosis;
aspirin‐exacerbated respiratory disease;
allergic fungal rhinosinusitis.
If the data allowed, we planned to carry out analyses separately for the different types of treatment, as well as considering surgical treatment as a whole.
Sensitivity analysis
We planned to use study risk of bias in a sensitivity analysis, if required.
Results
Description of studies
Results of the search
Our electronic searches retrieved a total of 3014 records, which reduced to 1896 after duplicates were removed. After screening of titles and/or abstracts we were left with six studies for further assessment. Following assessment of the full text, we excluded all six studies (Jankowski 2006; Kuehnemund 2002; Sauer 2007; Selivanova 2003; Venkatachalam 1998; Wadwongtham 2003) (see Excluded studies).
We identified no ongoing studies and no studies are currently awaiting assessment.
See Figure 1 (PRISMA flow chart of search history).
1.
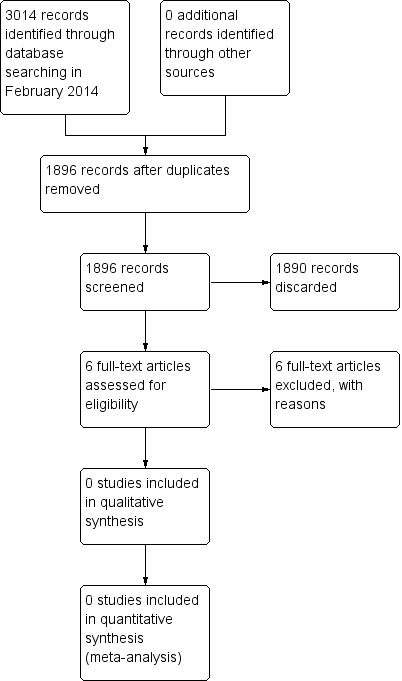
Process for sifting search results and selecting studies for inclusion.
Included studies
We included no studies in the review.
Excluded studies
We excluded six studies from the review. See Characteristics of excluded studies.
Jankowski 2006 was a retrospective study comparing radical endoscopic nasalisation and functional endoscopic ethmoidectomy in patients with nasal polyposis performed by two different surgeons. This was not a randomised study and also reported outcome when comparing two techniques that involved entering the sinuses during the operation. Outcomes were measured five years after the study (recall bias) and there was a significant rate of attrition.
Kuehnemund 2002 was a prospective, randomised trial comparing extended versus limited endonasal sinus surgery in patients suffering from chronic rhinosinusitis. The methodology had some failings in that two groups of surgeons conducted the surgeries, introducing a possible confounder. Additionally, the symptom score questionnaire they used was not a validated form such as SNOT‐22. The major reason that this study could not be included, however, was that the pathology analysed was chronic rhinosinusitis, which again did not necessarily include patients with nasal polyposis. However, apart from the weaknesses identified the study addresses an important area and would benefit from further study.
Sauer 2007 and Selivanova 2003 were prospective randomised controlled trials comparing powered instrumentation with standard instruments in the surgical treatment of chronic rhinosinusitis. The methodology in both studies appears fairly robust but these studies could not be included as the surgical methods analysed are outside the scope of this review and the pathology investigated did not necessarily include patients with nasal polyposis. The question investigated by these researchers is important, however, and further work in this area would be useful.
Venkatachalam 1998 was a randomised study that compared functional endoscopic sinus surgery with conventional (non‐endoscope assisted) techniques for the treatment of nasal polyposis. They did not directly compare simple polypectomy and more extensive sinus surgery with polypectomy. This study could therefore not be included in this review.
Wadwongtham 2003 reported results from a double‐blind randomised controlled trial involving patients with 'chronic' maxillary sinusitis (clinical and radiological evidence, but of unknown duration) and nasal polyposis. They did not specify what preoperative treatment had been received or whether maximal medical therapy had been used, did not standardise postoperative care and did not use standardised reporting measures. The study used each side of the patient's nose as their own control in a 'split‐nose' design. We thus excluded this from the review on this basis.
Risk of bias in included studies
No studies are included in the review.
Effects of interventions
No studies are included in the review.
Discussion
Summary of main results
No studies met the inclusion criteria for this review.
Overall completeness and applicability of evidence
This review cannot answer the clinical question addressed. We are unable to draw any conclusions regarding the effectiveness of isolated nasal polypectomy compared with more extensive sinus dissection for chronic rhinosinusitis with nasal polyps.
Potential biases in the review process
We used a comprehensive search strategy for this review. The search should have identified all relevant studies as we used broad search terms, included all languages and searched trial databases to ensure that any unpublished studies were found. However, it is still possible that some studies could have been missed. We contacted authors where necessary to obtain unpublished data. Two authors independently reviewed the search results to minimise selection bias. Two authors extracted data independently and were in agreement throughout, limiting bias. However, the authors were not blinded to the authors of the studies, which is a potential source of bias.
There were no marginal decisions during the review process. However, we did make some changes to the protocol: we further developed the methods section regarding study selection and clarified our outcome measures (see Differences between protocol and review).
Agreements and disagreements with other studies or reviews
We excluded several studies in the process of this review (see Characteristics of excluded studies). Kuehnemund 2002 performed a prospective, randomised study comparing extended versus limited approach endonasal sinus surgery. The patient cohort of 65 patients that they examined comprised patients with chronic rhinosinusitis as diagnosed by an unvalidated symptom score, imaging and failure of medical management. The limited approach surgery was characterised by infundibulotomy, opening of the bulla and middle meatal antrostomy and was applied to 32 patients, whereas the extended approach included infundibulotomy, opening of the ethmoids, sphenoids and frontal recess, middle meatal antrostomy and reduction of the middle turbinate, and was applied to 33 patients. Postoperative care was standardised between the groups. Their primary outcome measures were saccharine transport time (STT), endoscopic findings and symptom scores. The authors reported that there was improvement in endoscopy findings and STT in both groups at six months. The symptom score improved up to six months and then deteriorated in long‐term follow‐up. No statistical difference could be identified between groups.
Jankowski 2006 undertook a retrospective five‐year study of 76 patients with nasal polyposis who underwent either what was termed 'nasalisation' (ethmoidectomy removing all bony lamellae and mucosa within the ethmoids, large antrostomy, sphenoidotomy, frontal recess opening and middle turbinate removal) or 'functional ethmoidectomy' (a tailored approach leaving non‐diseased cells intact and proceeding to further dissection only in the presence of disease). Thirty‐nine patients underwent 'nasalisation' and 37 underwent 'functional ethmoidectomy'. Patients were asked to complete a 10‐point visual analogue scale (VAS), where 10 was deemed a 'normal' nose and '0' was no improvement from their symptoms prior to surgery and endoscopic evaluation. This study reported an improvement in the VAS score of 8.41 (± 0.4) in the nasalisation group against 5.69 (± 0.83) in the ethmoidectomy group (P value < 0.002). Nasal polyp recurrence was also reported as lower in the nasalisation group compared with ethmoidectomy (Chi² = 10.41, P value < 0.01).
Wadwongtham 2003 undertook a prospective randomised controlled study comparing intranasal polypectomy with intranasal polypectomy, uncinectomy and middle meatal antrostomy in 60 patients. The study did not specify whether patients had trialled maximal medical therapy prior to surgery and postoperative medication regimes were not reported. No validated symptom scoring was used in this study. No mention was made of whether other sinuses (ethmoidal, frontal, sphenoid) were entered during the surgical procedure. Postoperatively the patients were packed with umbilical tape, which was left for between three and five days before being removed. This leads to a high risk of bias, as the length of postoperative packing was not standardised, and could also lead to bias by altering the surgical results by potentially enlarging the maxillary sinus ostium. The study interventions do not match the objective as on one side the uncinate process is removed and on the other a middle meatal antrostomy is created. The latter would not be classified as more extensive surgical clearance as it is the smallest adjunct to an intranasal polypectomy and if the other sinuses have not been addressed only a minimal change in approach has been compared.
Of the remaining three studies that we reviewed in full text and excluded, one compared endoscopic versus non‐endoscopic nasal polypectomy (Venkatachalam 1998) and the other two compared powered versus non‐powered instruments in the endoscopic treatment of chronic rhinosinusitis with or without polyps (Sauer 2007; Selivanova 2003).
These studies highlight a number of problems with the evidence relating to this topic. Firstly, these trials recruited patients with chronic rhinosinusitis but patients in this group do not necessarily have nasal polyposis and a clear demarcation of those patients with polyps should be made. Secondly, most studies lacked an adequate, validated symptom score, such as SNOT‐22, which we have established as our primary outcome measure.
The 2012 European Position Paper on Rhinosinusitis and Nasal Polyps is the only recent evidence‐based systematic review on the aetiology, management and treatment of CRS with and without nasal polyps, and it agrees with this review that randomised controlled trials are needed to investigate minimal versus more extensive endoscopic sinus surgery (Fokkens 2012).
Authors' conclusions
Implications for practice.
As we identified no trials that met the inclusion criteria for the review, there is currently no available evidence to support either nasal polypectomy or more extensive sinus clearance as a superior surgical modality in the treatment of chronic rhinosinusitis with nasal polyps.
Implications for research.
As surgery forms the mainstay of practice for medically resistant nasal polyp disease, randomised controlled trials would be desirable to determine whether more extensive sinus dissection offers any advantage over endoscopic polypectomy alone, ideally in chronic rhinosinusitis with nasal polyps patients who have undergone standardised pre‐ and postoperative medical care. In order to reduce heterogenous outcome data and allow subsequent meta‐analyses, trials should preferably utilise outcome measures similar to those that form the basis of this review. Despite our increasing understanding of the pathophysiology of the disease, isolated polypectomy is still likely to be practised, as factors such as reduced skill and time needed to perform the procedure, limited equipment, reduced complications and lower cost of isolated polypectomy will be incentives for some surgeons to perform this in preference to more extensive sinus dissection.
History
Protocol first published: Issue 1, 2008 Review first published: Issue 11, 2014
| Date | Event | Description |
|---|---|---|
| 4 November 2008 | Amended | Converted to RevMan 5 format |
Acknowledgements
The authors wish to acknowledge the support of Jenny Bellorini and the editorial panel of the Cochrane Ear, Nose and Throat Disorders Group.
Appendices
Appendix 1. Search strategies
| PubMed | EMBASE (Ovid) | CINAHL (EBSCO) |
| #1 "Nasal Polyps"[MeSH] #2 "Polyps"[MeSH] #3 polyp* [tiab] #4 #2 OR #3 #5 "Nose"[MeSH] #6 nose* [tiab] OR nasal* [tiab] OR nasi [tiab] OR intranasal* [tiab] OR sinonasal* [tiab] OR paranasal* [tiab] #7 #5 OR #6 #8 #4 AND #7 #9 #1 OR #8 | 1 Nose Polyp/ 2 exp Polyp/ 3 polyp*.tw. 4 3 or 2 5 exp Nose/ 6 (nose* or nasal* or nasi or intranasal* or sinonasal* or paranasal*).tw 7 6 or 5 8 4 and 7 9 8 or 1 | S1 (MH "Nasal Polyps") S2 (MH "Polyps") S3 TX polyp* S4 (MH "Nose+") S5 TX nose* OR nasal* OR nasi OR intranasal* OR sinonasal* OR paranasal* S6 (S2 OR S3) AND (S4 OR S5) S7 S1 OR S6 |
| Web of Science | CAB Abstracts (Ovid) | ISRCTN |
| #1 TS=polyp* #2 TS=(nose* OR nasal* OR nasi OR intranasal* OR sinonasal* OR paranasal*) #3 #2 AND #1 |
1 polyp*.tw. 2 exp Nose/ 3 (nose* or nasal* or nasi or intranasal* or sinonasal* or paranasal*).tw. 4 3 or 2 5 4 and 1 | (nose OR nasal) AND polyp% |
Characteristics of studies
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Jankowski 2006 | ALLOCATION Non‐randomised |
| Kuehnemund 2002 | ALLOCATION Randomised controlled trial PARTICIPANTS Patients with chronic rhinosinusitis; only a few patients had nasal polyps. We aimed to analyse those with nasal polyps alone |
| Sauer 2007 | ALLOCATION Randomised controlled trial PARTICIPANTS Patients with chronic rhinosinusitis with and without polyps INTERVENTIONS Powered versus non‐powered sinus surgery therefore outside the remit of the review |
| Selivanova 2003 | ALLOCATION Randomised controlled trial PARTICIPANTS Patients with chronic rhinosinusitis with and without polyps INTERVENTIONS Powered versus non‐powered sinus surgery therefore outside the remit of this review |
| Venkatachalam 1998 | ALLOCATION Randomised controlled trial PARTICIPANTS Patients with chronic rhinosinusitis INTERVENTIONS Endoscope‐assisted versus non‐endoscope‐assisted sinus surgery, therefore outside the remit of this review |
| Wadwongtham 2003 | ALLOCATION: Randomised controlled trial comparing large middle meatal antrostomy with undisturbed maxillary sinus ostium in endoscopic sinus surgery in patients with 'chronic' maxillary sinusitis and nasal polyposis. The study used the each side of the patient as their own control in a 'split‐nose' design and was thus excluded |
Differences between protocol and review
The title has changed from 'Surgical interventions for nasal polyps' to 'Surgical interventions for chronic rhinosinusitis with nasal polyps', in accordance with current terminology (Fokkens 2012).
We have further developed the Methods section regarding study selection. Initially, the primary outcome was "symptom scores"; we have expanded this into "disease severity, as measured by patient‐reported disease‐specific symptom scores", "health‐related quality of life, using disease‐specific health‐related quality of life scores" and "health‐related quality of life, using generic quality of life scores". The fourth secondary outcome was originally "physiological measures of nasal airway resistance, cross‐sectional area, olfaction or ciliary function"; we have divided this into two separate secondary outcomes. The first is "objective physiological measures: nasal peak flow, nasal volume, nasal cross‐sectional area, nasal nitric oxide (nNO), ciliary function" and the second is "olfactory tests". This was done because olfactory tests are by definition subjective.
We have also added the clarifying statement, "We analysed the following outcomes in the review, but they were not used as a basis for including or excluding studies", reflecting current standards.
We have explicitly stated that studies with a 'split‐nose' design (i.e. one side of the nose is treated with one surgical technique and the other side is treated with another) were excluded from the review due to their high risk of bias, as ongoing inflammation on one side may affect the rate of recurrence on the contralateral side, thus confounding a particular surgical technique.
We have adopted the Cochrane 'Risk of bias' tool for study quality assessment (Handbook 2011).
We have provided more detail on data synthesis methods.
Contributions of authors
CH: background literature search, development of protocol, data search and analysis, senior author.
RS: data extraction, literature review and analysis, preparation of written review, contact author.
RL/JR: data extraction, literature review and analysis, preparation of written review.
Sources of support
Internal sources
NIHR/Cochrane Incentive Scheme Award 2013, UK.
External sources
No sources of support supplied
Declarations of interest
Rishi Sharma: none declared
Raj Lakhani: none declared
Jo Rimmer: none declared
Claire Hopkins: none declared
New
References
References to studies excluded from this review
Jankowski 2006 {published data only}
- Jankowski R, Pigret D, Decroocq F, Blum A, Gillet P. Comparison of radical (nasalisation) and functional ethmoidectomy in patients with severe sinonasal polyposis. Revue de Laryngologie Otologie Rhinologie (Bord) 2006;127(3):131‐40. [PubMed] [Google Scholar]
Kuehnemund 2002 {published data only}
- Kuehnemund M, Lopatin A, Amedee RG, Mann WJ. Endonasal sinus surgery: extended versus limited approach. American Journal of Rhinology 2002;16(4):187‐92. [PubMed] [Google Scholar]
Sauer 2007 {published data only}
- Sauer M, Lemmens W, Vauterin T, Jorissen M. Comparing the microdebrider and standard instruments in endoscopic sinus surgery: a double‐blind randomised study. B‐ENT 2007;3(1):1‐7. [PubMed] [Google Scholar]
Selivanova 2003 {published data only}
- Selivanova O, Kuehnemund M, Mann WJ, Amedee RG. Comparison of conventional instruments and mechanical debriders for surgery of patients with chronic sinusitis. American Journal of Rhinology 2003;17(4):197‐202. [PubMed] [Google Scholar]
Venkatachalam 1998 {published data only}
- Venkatachalam VP, Bhat A. Comparative evaluation of endoscopic and conventional surgical techniques in the management of nasal polyposis. JK Practitioner 1998;5(4):295‐9. [Google Scholar]
Wadwongtham 2003 {published data only}
- Wadwongtham W, Aeumjaturapat S. Large middle meatal antrostomy vs undisturbed maxillary ostium in the endoscopic sinus surgery of nasal polyposis. Journal of the Medical Association of Thailand 2003;86 Suppl 2:S373‐8. [PubMed] [Google Scholar]
Additional references
Adams 1999
- Adams PF, Hendershot GE, Marano MA, Centers for Disease Control and Prevention/National Center for Health Statistics. Current estimates from the National Health Interview Survey, 1996. Vital and Health Statistics. Series 10, Data from the National Health Survey 1999;10(200):1‐203. [PubMed] [Google Scholar]
Alobid 2012
- Alobid I, Benitez P, Valero A, Munoz R, Langdon C, Mullol J. Oral and intranasal steroid treatments improve nasal patency and paradoxically increase nasal nitric oxide in patients with severe nasal polyposis. Rhinology 2012;50(2):171‐7. [DOI] [PubMed] [Google Scholar]
Bachert 2000
- Bachert C, Gevaert P, Holtappels G, Cuvelier C, Cauwenberge P. Nasal polyposis: from cytokines to growth. American Journal of Rhinology 2000;14(5):279‐90. [DOI] [PubMed] [Google Scholar]
Bachert 2001
- Bachert C, Gevaert P, Holappels G, Johansson SGO, Cauwenberge P. Total and specific IgE in nasal polyps is related to local eosinophilic inflammation. Journal of Allergy and Clinical Immunology 2001;107:607‐14. [DOI] [PubMed] [Google Scholar]
Bateman 2003
- Bateman ND, Fahy C, Woolford T. Nasal polyps: still more questions than answers. Journal of Laryngology and Otology 2003;117(1):1‐9. [DOI] [PubMed] [Google Scholar]
Calenoff 1993
- Calenoff E, McMahan JT, Herzon GD. Bacterial allergy in nasal polyposis. Archives of Otolaryngology ‐ Head and Neck Surgery 1993;119:830‐6. [DOI] [PubMed] [Google Scholar]
Caplin 1971
- Caplin I, Haynes JT, Spahn J. Are nasal polyps an allergic phenomenon?. Annals of Allergy 1971;29:631‐4. [PubMed] [Google Scholar]
Catalano 2004
- Catalano P. Minimally invasive sinus technique: should we consider it?. Current Opinion in Otolaryngology and Head and Neck Surgery 2004;12:34‐7. [DOI] [PubMed] [Google Scholar]
Cervin 2014
- Cervin A, Wallwork B. Efficacy and safety of long‐term antibiotics (macrolides) for the treatment of chronic rhinosinusitis. Current Allergy & Asthma Reports 2014;14(3):416. [DOI] [PubMed] [Google Scholar]
Chin 2013
- Chin D, Harvey RJ. Nasal polyposis: an inflammatory condition requiring effective anti‐inflammatory treatment. Current Opinion in Otolaryngology & Head and Neck Surgery 2013;21(1):23‐30. [DOI] [PubMed] [Google Scholar]
Collins 2006
- Collins MM, Loughran S, Davidson P, Wilson JA. Nasal polyposis: prevalence of positive food and inhalant skin tests. Otolaryngology ‐ Head and Neck Surgery 2006;135(5):680‐3. [DOI] [PubMed] [Google Scholar]
Drake‐Lee 1984
- Drake‐Lee AB, Lowe D, Swanston A, Grace A. Clinical profile and recurrence of nasal polyposis. Journal of Laryngology and Otology 1984;98(8):783‐93. [DOI] [PubMed] [Google Scholar]
Fokkens 2012
- Fokkens WJ, Lund VJ, Mullol J, Bachert C, Alobid I, Baroody F. European position paper on rhinosinusitis and nasal polyps. Rhinology 2012;23:1‐298. [PubMed] [Google Scholar]
Glicklich 1995
- Glicklich R, Metson R. The health impact of chronic sinusitis in patients seeking otolaryngologic care. Otolaryngology ‐ Head and Neck Surgery 1995;113:104‐9. [DOI] [PubMed] [Google Scholar]
Greisner 1996
- Greisner WA, Settipane GA. Hereditary factor for nasal polyps. Allergy and Asthma Proceedings 1996;17:283‐6. [DOI] [PubMed] [Google Scholar]
Handbook 2011
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Hopkins 2006
- Hopkins C, Browne J, Slack R, Lund V, Brown P, Meulen J. Complications of sinonasal surgery. Laryngoscope 2006;116(8):1494‐9. [DOI] [PubMed] [Google Scholar]
Hopkins 2009
- Hopkins C, Gillett S, Slack R, Lund VJ, Browne JP. Psychometric validity of the 22‐item Sinonasal Outcome Test. Clinical Otolaryngology 2009;34(5):447‐54. [DOI] [PubMed] [Google Scholar]
Jamal 1987
- Jamal A, Maran AGD. Atopy and nasal polyposis. Journal of Laryngology and Otology 1987;110:355‐8. [Google Scholar]
Jankowski 1997
- Jankowski R, Pigret D, Decrooq F. Comparison of functional results after ethmoidectomy for diffuse and sever nasal polyposis. Acta Oto‐Laryngologica 1997;117(4):601‐8. [DOI] [PubMed] [Google Scholar]
Johansson 2003
- Johansson L, Akerlund A, Holmberg K, Melén I, Bende M. Prevalence of nasal polyps in adults: the Skovde population based study. Annals of Otology, Rhinology, and Laryngology 2003;112(7):625‐9. [DOI] [PubMed] [Google Scholar]
Jones 1997
- Jones NS, Strobl A, Holland I. A study of CT findings in 100 patients with rhinosinusitis and 100 controls. Clinical Otolaryngology and Allied Sciences 1997;22:47‐51. [DOI] [PubMed] [Google Scholar]
Kalish 2012
- Kalish L, Snidvongs K, Sivasubramaniam R, Cope D, Harvey RJ. Topical steroids for nasal polyps. Cochrane Database of Systematic Reviews 2012, Issue 12. [DOI: 10.1002/14651858.CD006549.pub2] [DOI] [PubMed] [Google Scholar]
Kennedy 1992
- Kennedy DW. Prognostic factors, outcomes and staging in ethmoids sinus surgery. Laryngoscope 1992;102:S1‐18. [PubMed] [Google Scholar]
Lange 2013
Lanza 1992
- Lanza DE, Kennedy DW. Current concepts in surgical management of nasal polyposis. Journal of Allergy and Clinical Immunology 1992;90:543‐6. [DOI] [PubMed] [Google Scholar]
Larsen 1989
- Larsen P, Tos M. Nasal polyps: epithelium and goblet cell density. Laryngoscope 1989;99(12):1274‐80. [DOI] [PubMed] [Google Scholar]
Larsen 1997
- Larsen K, Tos M. A long‐term follow‐up study of nasal polyp patients after simple polypectomies. European Archives of Oto‐rhino‐laryngology 1997;254(Suppl 1):S85‐8. [DOI] [PubMed] [Google Scholar]
Larsen 2004
- Larsen P, Tos M. Origin of nasal polyps: an endoscopic autopsy study. Laryngoscope 2004;114(4):710‐9. [DOI] [PubMed] [Google Scholar]
Lildholdt 1989
- Lildholdt T. Surgical versus medical treatment of nasal polyps. Rhinology 1989;27(S8):31‐3. [PubMed] [Google Scholar]
Lund 1997
- Lund VJ, Kennedy DW. Staging for rhinosinusitis. Otolaryngology ‐ Head and Neck Surgery 1997;117:S35‐S40. [DOI] [PubMed] [Google Scholar]
Martinez‐Devesa 2011
- Martinez‐Devesa P, Patiar S. Oral steroids for nasal polyps. Cochrane Database of Systematic Reviews 2011, Issue 7. [DOI: 10.1002/14651858.CD005232.pub3] [DOI] [PubMed] [Google Scholar]
Min 1996
- Min YG, Jung HW, Kim HS, Park SK, Yoo KY. Prevalence and risk factors of chronic sinusitis in Korea: results of a nationwide survey. European Archives of Oto‐rhino‐laryngology 1996;253(7):435‐9. [DOI] [PubMed] [Google Scholar]
Molnar‐Gabor 2000
- Molnar‐Gabor E, Endreffy E, Rozsasi A. HLA‐DRB1, ‐DQA1, and ‐DQB1 genotypes in patients with nasal polyposis. Laryngoscope 2000;110(3 Pt 1):422‐5. [DOI] [PubMed] [Google Scholar]
Parnes 2002
- Parnes S. Targeting cysteinyl leukotrienes in patients with rhinitis, sinusitis and paranasal polyps. American Journal of Respiratory Medicine 2002;1(6):403‐8. [DOI] [PubMed] [Google Scholar]
Pawliczak 2005
- Pawliczak R, Lewandowska‐Polak A, Kowalski ML. Pathogenesis of nasal polyps: an update. Current Allergy and Asthma Reports 2005;5(6):463‐71. [DOI] [PubMed] [Google Scholar]
Piccirillo 1995
- Piccirillo JF, Edwards D, Haiduk A, Yonan C, Thawley SE. Psychometric and clinimetric validity of the 31‐item Rhinosinusitis Outcome Measure (RSOM‐31). American Journal of Rhinology 1995;9(6):297‐306. [Google Scholar]
Piccirillo 2002
- Piccirillo JF, Merritt MGJ, Richards ML. Psychometric and clinimetric validity of the 20‐Item Sino‐Nasal Outcome Test (SNOT‐20). Otolaryngology ‐ Head and Neck Surgery 2002;126(1):41‐7. [DOI] [PubMed] [Google Scholar]
Ponikau 1999
- Ponikau JU, Sherris DA, Kern EB. The diagnosis and incidence of allergic fungal sinusitis. Mayo Clinic Proceedings 1999;74:877‐84. [DOI] [PubMed] [Google Scholar]
Radenne 1999
- Radenne F, Lamblin C, Vandezande LM, Tillie‐Leblond I, Darras J, Tonnel AB, et al. Quality of life in nasal polyposis. Journal of Allergy and Clinical Immunology 1999;104(1):79‐84. [DOI] [PubMed] [Google Scholar]
RevMan 2014 [Computer program]
- The Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager (RevMan). Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Rimmer 2014
- Rimmer J, Fokkens W, Chong LY, Hopkins C. Medical versus surgical interventions for chronic rhinosinusitis with nasal polyps. Cochrane Database of Systematic Reviews 2014, Issue 11. [DOI: 10.1002/14651858.CD006991.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Rugina 2002
- Rugina M, Serrano E, Klossek JM, Crampette L, Stoll D, Bebear JP, et al. Epidemiological and clinical aspects of nasal polyps in France: the ORLI group experience. Rhinology 2002;40(2):75‐9. [PubMed] [Google Scholar]
Samter 1968
- Samter M, Beers RF. Intolerance to aspirin. Clinical studies and consideration of its pathogenesis. Annals of Internal Medicine 1968;68(5):975‐83. [DOI] [PubMed] [Google Scholar]
Sinonasal Audit 2006
- Hopkins C, Browne JP, Slack R, Lund V, Topham J, Reeves B, et al. The national comparative audit of surgery for nasal polyposis and chronic rhinosinusitis. Clinical Otolaryngology 2006;31(5):390‐8. [DOI] [PubMed] [Google Scholar]
Slavin 1997
- Slavin RG. Nasal polyps and sinusitis. JAMA 1997;278(22):1849‐54. [PubMed] [Google Scholar]
Snidvongs 2011
- Snidvongs K, Kalish L, Sacks R, Craig J, Harvey R. Topical steroid for chronic rhinosinusitis without polyps. Cochrane Database of Systematic Reviews 2011, Issue 8. [DOI: 10.1002/14651858.CD009274] [DOI] [PubMed] [Google Scholar]
Snidvongs 2013
- Snidvongs K, Chin D, Sacks R, Earls P, Harvey RJ. Eosinophilic rhinosinusitis is not a disease of ostiomeatal occlusion. Laryngoscope 2013;123(5):1070‐4. [DOI] [PubMed] [Google Scholar]
Stammberger 1991
- Stammberger H. Functional Endoscopic Sinus Surgery. The Messerklinger Technique. Toronto: BC Decker, 1991. [DOI] [PubMed] [Google Scholar]
Stammberger 1999
- Stammberger H. Surgical treatment of nasal polyps: past, present and future. Allergy 1999;Suppl 53:S7‐S11. [DOI] [PubMed] [Google Scholar]
Stoop 1993
- Stoop AE, Heijden HA, Biewenga J. Eosinophils in nasal polyps and nasal mucosa: an immunohistochemical study. Journal of Allergy and Clinical Immunology 1993;91(2):616‐22. [DOI] [PubMed] [Google Scholar]
Vaidyanathan 2011
- Vaidyanathan S, Barnes M, Williamson P, Hopkinson P, Donnan PT, Lipworth B. Treatment of chronic rhinosinusitis with nasal polyposis with oral steroids followed by topical steroids: a randomized trial. Annals of Internal Medicine 2011;154(5):293‐302. [DOI] [PubMed] [Google Scholar]
van Camp 1994
- Camp C, Clement PA. Results of oral steroid treatment in nasal polyposis. Rhinology 1994;32(1):5‐9. [PubMed] [Google Scholar]
van Zele 2004
- Zele T, Gevaert P, Watelet JB, Claeys G, Holtappels G, Claeys C, et al. Staphylococcus aureus colonization and IgE antibody formation to enterotoxins is increased in nasal polyposis. Journal of Allergy and Clinical Immunology 2004;114(4):981‐3. [DOI] [PubMed] [Google Scholar]
Vancil 1969
- Vancil ME. A historical survey of treatments for nasal polyposis. Laryngoscope 1969;79(3):435‐45. [DOI] [PubMed] [Google Scholar]
Vento 2000
- Vento SI, Ertama LO, Hytonen ML, Wolff CH, Malmberg CH. Nasal polyposis: clinical course during 20 years. Annals of Allergy, Asthma and Immunology 2000;85(3):209‐14. [DOI] [PubMed] [Google Scholar]
Yamada 2000
- Yamada T, Fujieda S, Mori S, Yamamoto H, Saito H. Macrolide treatment decreased the size of nasal polyps and IL‐8 levels in nasal lavage. American Journal of Rhinology 2000;14(3):143‐8. [DOI] [PubMed] [Google Scholar]
Zhang 2005
- Zhang N, Gevaert P, Zele T, Perez‐Novo C, Patou J, Holtappels G, et al. An update on the impact of Staphylococcus aureus enterotoxins in chronic sinusitis with nasal polyposis. Rhinology 2005;43(3):162‐8. [PubMed] [Google Scholar]


