The secretary of state is due to announce the results of an inquiry into beds in England. This review seems to have been in response to a perception that hospitals were experiencing increased difficulty in coping with emergency pressures and that the reduction in beds had gone too far—a fact apparently supported by a plateauing in the downward trend in the number of beds. The hospital sector, especially in the NHS, has long been a focus from all sides for rhetoric and emotive political appeals. In terms of numbers of both hospitals and beds, the NHS has been shrinking for most of its life. The bed stock of NHS in England peaked in 1957-8 and has declined since. In the more recent past, official statistics on hospital services in this country have been plentiful, yet they are rarely presented together in an easily accessible and unified form. It is the objective of this paper, therefore, to provide a concise summary of key trends and statistics in the sector that will be of use to policymakers, analysts, researchers, and practitioners. We present data on hospital provision in both the public and the private sectors, and on productivity in the NHS hospital sector. The implications of the most significant trends are discussed, and a number of lessons are suggested for audiences both within the United Kingdom and abroad. The analysis starts in 1982, the year of a major administrative reorganisation within the NHS, and shortly before the Griffiths Report,1 which ushered in the concept of “general management” in the NHS. NHS data reporting conventions in all areas changed in 1987, including a move in reporting from calendar years to financial years, the replacement of “deaths and discharges” with the “finished consultant episode,” and changes to the definition of certain specialty groupings.
Summary points
Since the early 1980s, the NHS hospital infrastructure in England has shrunk dramatically but inpatient activity has grown by over two thirds
The number of private sector nursing home beds has increased massively, so the overall bed stock in England has actually risen slightly since the early 1980s
Productivity has improved substantially and hospital capacity for treating patients and providing interventions has increased dramatically
NHS hospital infrastructure and bed provision in England
In 1991, after the introduction of the NHS internal market and the establishment of NHS hospital trusts, the Department of Health stopped recording the number of hospitals in England. It is therefore no longer possible to establish from official sources how many hospitals the NHS operates in England; the data show only the number of trusts, and many trusts operate two or more separate hospital sites. Between 1978 and 1990-1, the total number of hospital sites offering inpatient or residential accommodation operated by the NHS was reduced from 2063 to 1624. A small increase in the number of psychiatric hospitals (from 410 to 477) reflected a growth in the number of small psychiatric units and took place in parallel with sweeping closures of larger facilities. In contrast, most of the 506 non-psychiatric hospitals that closed during this period had less than 250 beds. During this 12 year period, an average of 42 non-psychiatric inpatient facilities closed each year.
Data on the number of NHS beds in England are still available in centralised form, allowing a more contemporary analysis. The number of available beds shows a continuous downward trend over the past decade, with over two fifths of the 1982 bed stock closed by 1997-8. Table 1 shows the relative reduction in bed capacity across the main specialty groups. Closures of beds in wards specialising on mental illness and learning disability during this period (overwhelmingly the result of the long term policy of deinstitutionalisation) account for over 55% of the total bed reduction observed, while “acute” beds registered the slowest rate of reduction.
Table 1.
Change in numbers of NHS beds in England, 1982 to 1994-51 9
| Year | All specialties | Acute care | Geriatrics | Mental illness | Mental handicap | Maternity care |
|---|---|---|---|---|---|---|
| 1982 | 348 104 | 143 535 | 55 646 | 83 831 | 46 983 | 18 108 |
| 1994-5 | 211 812 | 108 008 | 36 795 | 41 827 | 13 211 | 11 971 |
| % change | −39 | −25 | −34 | −50 | −72 | −34 |
Translated into terms of numbers of beds per 1000 population, over the same period the total available beds (all specialties) declined by 47%, from 7.4 per 1000 to 3.9 per 1000 in England. The number of acute beds declined from 3.1 to 2.2 per 1000 population, a reduction of nearly 29%; reductions in acute beds have slowed considerably in the last four years.
Trends in inpatient activity and productivity
The mirror image of the sustained closure of hospital beds throughout the period in question has been the sustained increase in total inpatient activity. Over a 15 year period from 1982 the NHS in England was able to increase by over two thirds the number of patients it treated as inpatients or day cases—while reducing the number of beds by two fifths. Table 2 summarises the change in activity over this period for all specialties and general and acute specialties (total acute activity including geriatric medicine, excluding new births). The interaction of rising inpatient activity with a reducing bed stock is captured vividly in one single indicator—the throughput rate (cases per bed), which more than doubled in the 15 years after 1982.
Table 2.
Change in NHS inpatient and day case activity in England, 1982 to 1994-5
| Inpatient cases (000s) | Day cases (000s) | Total cases (000s) | Total cases per 1000 population | Throughput per bed | |
|---|---|---|---|---|---|
| All specialties | |||||
| 1982 | 5720 | 707 | 6 427 | 137.3 | 16.4 |
| 1994-5 | 8065 | 2474 | 10 539 | 216.4 | 38.1 |
| % change | 41 | 250 | 64 | 58 | 132 |
| General and acute specialties | |||||
| 1982 | 4709 | 685 | 5 394 | 115.2 | 23.7 |
| 1994-5 | 6210 | 2439 | 8 649 | 177.6 | 42.9 |
| % change | 32 | 256 | 60 | 54 | 81 |
It is immediately obvious that a dramatic increase in the scale of day case activity (both surgical and medical) has been a key contributor to this upward trend and that inpatient treatment has also increased substantially in volume. Overall, day case activity, which constituted 11% of total activity in 1982, had risen to make up 26.6% of total workload in all specialties by 1997-8, and accounted for greatly higher proportions of total activity in several acute specialties, particularly surgery.
Length of stay in hospital
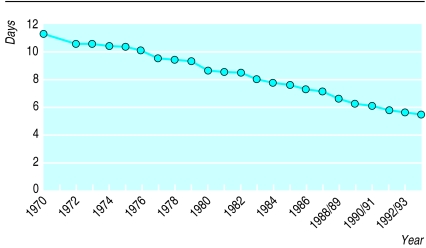
Inpatient length of stay has shown a long term downward trend for nearly 50 years. In all specialties, mean length of stay was 49.3 days in 1949; 37.6 days in 1959; 25.6 days in 1969; and 19.8 days in 1979. Figure 1 shows the downward trend in length of stay in the acute specialties since 1970. The difficulties posed by the apparently inexorable progress of length of stay towards zero have been commented on,2,3 and it is generally suggested that the rate of decrease in length of stay must sooner or later decelerate as a natural “floor” is approached in terms of external constraints (critically in the area of “bed blocking” and the ability of social services to establish effective care packages).
Figure 1.
Length of hospital stay in acute specialties since 1970
Alongside the growth in day cases, one of the critical mechanisms by which throughput has been increased and total inpatient activity expanded has been the fact that length of stay has consistently fallen at a faster rate than the number of beds (see table 3). This has been equivalent to an effective increase in bed capacity—falling length of stay has freed more bed days than bed closures have eliminated, and these “extra” bed days have allowed more admissions to take place. It can been argued that, in effect, a “bed” is now more likely to be available than it was in 1982 and that this increased supply helps to explain the more recent phenomenon of rising emergency admissions.4 Similarly, there is reason to believe that a substantial portion of the growth in day case activity has represented “new” activity that hitherto would not have been performed and hence does not represent a substitution for inpatient activity.5
Table 3.
Average annual change in number of beds and length of stay in acute services. Values are percentages
| Period | Beds | Length of stay |
|---|---|---|
| 1982 to 1993-4 | −2.06 | −3.10 |
| 1982 to 1986 | −1.82 | −3.02 |
| 1987-8 to 1990-1 | −3.06 | −4.17 |
| 1991-2 to 1993-4 | −1.57 | −2.29 |
Trends in private sector provision
Private sector provision of acute hospital services encompasses independent, privately owned and operated hospitals as well as NHS “pay beds,” and obtaining consistent data on provision or activity in either segment of the sector is complex. Since the NHS reforms of 1991, NHS hospital trusts no longer need to report routinely on their pay beds, with the effect that the Department of Health is no longer able to monitor private activity taking place in NHS facilities. This section therefore examines briefly the main trends in bed provision in the independently owned or operated acute sector and in the nursing home sector, using data for the period 1984 to 1996-7.
The private healthcare sector is important in two main areas—elective surgery and continuing care. In 1984, private and voluntary hospitals and nursing homes accounted for some 7.5% of total healthcare spending in the United Kingdom as a whole, which had risen to 18.8% in 1991, largely because of the growth of the nursing home sector (see table 4).6
Table 4.
Changes in private sector provision6 10
| Institutions | Acute hospitals | Acute beds | Nursing home beds | |
|---|---|---|---|---|
| 1984 | 1491 | 200 | 10 067 | 32 831 |
| 1994-5 | 5676 | 245 | 11 363 | 173 961 |
| % change | 281 | 23 | 13 | 430 |
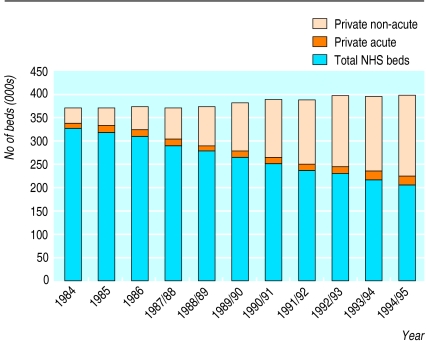
Immediately visible is the massive growth of the nursing home sector relative to the private acute hospital sector. However, independent acute bed provision has grown (by 4% in terms of beds, although this is down from a peak in 1992-3) during a period in which, as we have seen, the NHS acute bed stock declined rapidly. The explosive growth of the nursing home sector during this period has been of an entirely different magnitude. Private acute care beds now make up only 5.3% of all private beds—the remainder are to be found in nursing homes. Increasingly, the nursing home sector has taken on patients who, 10 or more years ago, would probably have been cared for in NHS continuing care beds in hospitals; indeed, the NHS is a key source of financing for patients cared for in the private nursing home sector. It would not be valid to argue that nursing homes have directly substituted for NHS beds; the complex interface with social care, local authorities, and private demand makes analysis of this issue complex, and activity data on the nursing home sector are not readily available. The growth in the number of nursing home beds has been so great, however, that, when all private (acute plus nursing home) beds are added to total NHS beds, it can be seen that the “broad” measure of total bed stock in England has actually risen since the early 1980s (fig 2).
Figure 2.
Availability of beds in England, 1984 to 1994-5
Hospital based ambulatory care
In comparison with the profound changes in inpatient services discussed above, hospital based ambulatory care activity in England has been notable mainly for its lack of dramatic change over the last decade. Outpatient activity increased steadily, by some 16.8%, between 1982 and 1997-8 in all specialties, rising from around 35.6 million attendances to 41.6 million.7 Over the same period, total attendances at accident and emergency departments have remained essentially static, fluctuating narrowly around a mean of approximately 13.6 million attendances per year (287 attendances per 1000 population).
Key themes
Undeniably, over the 1980s and 1990s the productivity of the hospital sector in England has improved. Between 1982 and 1997-8, over two thirds more hospital patients were treated using over two fifths fewer beds; length of stay continued to drop steadily as practice changed, and the uptake of day case treatments accelerated massively. In effect, productivity has improved so substantially that the capacity of the English NHS hospital sector to treat more patients and provide more interventions has increased dramatically despite a large reduction in its physical infrastructure.
The pace of change in the hospital sector was at its fastest in the late 1980s, before the introduction of the 1991 NHS reforms. During 1986 to 1990-1 the rates of decrease in bed numbers and length of stay, and of increase in inpatient activity and throughput, were fastest. Only the rate of increase of day case treatment has accelerated more rapidly after 1991 (by a factor of four to five times its previous rate of growth).
The strong suggestion of an important interaction between the growth of the nursing home sector and the ability of the NHS to reduce the hospital bed stock should not be lost on those seeking to reform the hospital sector elsewhere. In particular, it may be necessary to substitute beds for beds (albeit low tech, low dependency beds) rather than simply be able to make beds “disappear” from the system entirely.
Finally, substantial increases in inpatient and day case admissions have taken place alongside more gentle increases in the volume of first attendances in the hospital ambulatory care sector. One viable interpretation of this trend is that improvements in therapeutic technology are as likely (if not even more likely) to increase the likelihood of admission to hospital as they are to shift treatment out of secondary care. Certainly, the “average” English person is now substantially more likely to be admitted to hospital than he or she was in 1982, but only marginally more likely to attend an outpatient department. Evidence from Scotland shows that the increasing likelihood of admission to hospital reflects both an increase in single admissions (more individuals admitted to hospital) and an increase in multiple repeat admissions (more admissions of the same individuals)8—but in the absence of linked record systems the English data cannot support such an analysis.
The maintenance and design of appropriate indicators and information systems for health service reform is a key lesson of the British experience. Some of the decentralising trends embodied in the 1991 reform package led to growing ignorance at central government level of what, elsewhere in the world, might be regarded as fundamental (and simple) information. Thus, the Department of Health collects a wide array of complex and sophisticated performance information from around the country9,10—but it is not possible from these routine data sources to say how many hospitals are run by the NHS in England, or how many of these hospitals operate an accident and emergency department. Some people might argue that the ability to say “This information is no longer collected centrally” has proved to be useful for governments and civil servants. Whether or not this is fair, those designing reform packages for the health sector elsewhere might wish to ensure that they have access to such vital, basic information if an effective ability to monitor the success of reform is to be retained.
Figure.
Lock Hospital, Hyde Park Corner, London, in 1831
References
- 1.Department of Health and Social Security. NHS management enquiry. London: DHSS; 1983. (Griffiths report.) [Google Scholar]
- 2.Vetter N. The hospital—from centre of excellence to community support. London: Chapman and Hall; 1995. [Google Scholar]
- 3.Appleby J. Data briefing: the English patient. Health Serv J. 1997;107:36–37. [PubMed] [Google Scholar]
- 4.Edwards N. The wrong side of the bed. Health Serv J. 1997;107:26–27. [PubMed] [Google Scholar]
- 5.Edwards N. Day for night. Health Serv J. 1996;106:24–27. [PubMed] [Google Scholar]
- 6.Laing’s . Laing’s review of private healthcare 1993. London: Laing and Buisson; 1993. [Google Scholar]
- 7.Department of Health. Outpatients and ward attenders for England. London: Government Statistical Service; 1990. , 1995, 1996, 1998. [Google Scholar]
- 8.Kendrick S. Emergency admissions: what is driving the increase? Health Serv J. 1995;105:26–28. [PubMed] [Google Scholar]
- 9.Department of Health. Bed availability for England. London: Government Statistical Service; 1990. , 1995, 1996, 1998. [Google Scholar]
- 10.Department of Health. London: HMSO; 1990. Private hospitals, homes and clinics registered under section 3 of the Nursing Homes Act 1975. , 1995, 1996, 1998. [Google Scholar]