Abstract
Background
Patient involvement is crucial to the success of kidney transplants. This study aimed to investigate the knowledge, attitude, and practice (KAP) toward postoperative self-management among kidney transplant recipients.
Methods
A web-based cross-sectional study was conducted in Ruijin Hospital (Shanghai, China) between March 24, 2023, and April 15, 2023 in kidney transplant recipients. A questionnaire was designed to collect data about the characteristics of the participants and their KAP toward postoperative self-management. KAP scores were calculated based on participants' responses, using predefined scoring criteria tailored to evaluate each dimension of KAP effectively.
Results
A total of 483 valid questionnaires were collected, including 189 (39.13%) participants aged between 46 and 60 years. The mean score of knowledge, attitude and practice were 23.44 ± 4.87 (possible range: 0–28), 43.59 ± 2.65 (possible range: 10–50), 52.52 ± 4.64 (possible range: 0–58), respectively. The multivariate analysis showed knowledge scores (OR = 1.15, 95% CI = 1.10–1.20, p < 0.001), attitude scores (OR = 1.22, 95% CI = 1.12–1.32, p < 0.001) and undergone transplantation within 1 year (OR = 3.92, 95% CI = 1.60–9.63, p = 0.003) were independently associated with good practice. Knowledge scores (OR = 1.06, 95% CI = 1.02–1.10, p = 0.003), attitude scores (OR = 1.16, 95% CI = 1.08–1.25, p < 0.001), aged 16–35 years (OR = 0.38, 95% CI = 0.18–0.78, p = 0.009), underwent a single kidney transplant surgery (OR = 3.97, 95% CI = 1.28–12.38, p = 0.017) were independently associated with medication adherence.
Conclusions
Kidney transplant recipients had good knowledge, positive attitude and good practice toward postoperative self-management. Implementing personalized education, psychological support, and close monitoring strategies is recommended to optimize postoperative self-management in kidney transplant recipients.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12909-024-05631-8.
Keywords: Knowledge, Attitude, And practice, Postoperative self-management, Kidney transplant, Questionnaire, China
Background
The global incidence of end-stage renal disease (ESRD) is on the rise [1]. Renal transplantation stands as the optimal treatment for ESRD. Since its inaugural procedure in 1954, kidney transplantation has gained worldwide traction [2]. Among ESRD patients, living donor kidney transplantation is the favored option due to superior patient and graft survival rates [3]. This procedure holds prominence in the realm of solid organ transplants and serves as a pivotal intervention for individuals grappling with kidney failure. Despite successful surgical outcomes, ongoing self-management remains imperative to sustain the transplanted kidney's function and the patient's overall well-being [4].
Advancements in surgical techniques and immunosuppressants are boosting post-transplant survival rates while also reducing drug-related side effects. Postoperative self-management in kidney transplantation refers to recipients taking charge of their health post-surgery. This includes following medical instructions, taking immunosuppressants as directed, managing diet and weight, staying active, and attending regular medical check-ups. Self-management is vital to prevent rejection, reduce infections, and extend the life of the transplanted kidney. However, kidney transplant recipients still face significant risks like rejection, cardiovascular issues, and infections. Hence, rigorous postoperative care is necessary, involving strict medication and diet adherence. Kidney transplants often fail due to non-compliance with treatment, negatively impacting recipients' quality of life [5]. It was found that 20–37% of adult patients to be non-compliant, and non-compliance contributes to 50% of acute rejection cases and 15% of organ losses, resulting in short- and long-term physical and economic detriments [6, 7].
The Knowledge, Attitudes, and Practices (KAP) framework plays a pivotal role in unraveling the mechanisms of health education aimed at fostering behavioral changes among patients. This is achieved through the utilization of KAP questionnaires, which delve into an individual's understanding, beliefs, and actions. These KAP surveys offer a valuable tool for assessing the impact of intervention programs. Furthermore, a patient's KAP dimensions are consistently recognized as indispensable factors in effective disease management strategies [8, 9].
A previous study underscored the positive correlation between increased awareness and the presence of children in households with improved adherence to COVID-19 preventive measures among solid organ transplant (SOT) patients, while attitudes displayed a more limited impact [10]. In a separate study, researchers highlighted the moderate levels of kidney transplantation knowledge among both candidates and recipients, emphasizing the necessity for targeted health education interventions that consider demographic factors such as education, age, and fertility status to enhance knowledge within this cohort [11]. Despite the widely recognized importance of self-management after kidney transplantation, the impact of patients' knowledge, attitude, and practice on self-management has not been thoroughly studied. Exploring the knowledge, attitudes, and practices of kidney transplant recipients regarding postoperative self-management offers valuable insights into potential shortcomings and areas of concern, serving as a basis for refining postoperative care protocols.
Therefore, this study aimed to investigate the KAP toward postoperative self-management among kidney transplant recipients.
Methods
Study design and participants
This cross-sectional study was conducted at Ruijin Hospital between March 24, 2023, and April 15, 2023 among kidney transplant recipients. The inclusion criteria encompassed patients who underwent kidney transplantation (including graft failure and transplant nephrectomy cases), were on long-term oral immunosuppressive medication, and attended regular follow-up at the hospital's kidney transplant outpatient clinic. Exclusion criteria comprised recipients of multi-organ transplants such as heart, liver, or lung, as well as individuals who didn't provide informed consent.
Questionnaire and quality control
The questionnaire was developed with references to relevant literature [12–15] and guidelines ("Standardized Follow-Up after Kidney Transplantation (2019 edition) [16]"; "Expert Consensus on Perioperative Accelerated Recovery Management of Kidney Transplantation in China (2018 edition) [17]"). After completing the questionnaire, 34 kidney transplant recipients participated in the pretest. The Cronbach’s α was 0.923. We conducted confirmatory factor analysis simultaneously, showing CFI (comparative fit index) = 0.816 (> 0.8 is good), IFI (incremental fit index) = 0.830 (> 0.8 is good), TLI (Tucker-Lewis index) = 0.816 > 0.8 is good, RMSEA (root mean square error of approximation) = 0.054 (< 0.08 is good), and CMIN/DF (chi-square value/degrees of freedom) = 2.417 (1–3: excellent, 3–5: good).
The final questionnaire encompassed four distinct sections: demographic particulars (including gender, age, education, etc.), the knowledge dimension, the attitude dimension, and the practice dimension. The knowledge dimension encompassed a set of 14 items, each allocated a score of 2 for “Understand”, 1 for “Partially understand”, and 0 for “Do not understand”, thereby establishing a scoring continuum spanning 0 to 28 points. The attitude dimension consisted of 10 questions, evaluated via a five-point Likert scale that ranged from "very positive" (5 points) to "very negative" (1 point), thus offering a scoring spectrum of 10 to 50 points. The practice dimension gauged medication adherence using the Morisky Medication Adherence Questionnaire [18–20], comprising 8 items, and evaluated compliance with postoperative follow-up visits via a five-point Likert scale that ranged from "completely compliant" (5) to "completely non-compliant" (1). The comprehensive score range for the practice dimension spanned 0 to 58 points.
The electronic questionnaires were disseminated through a social media platform in China. The distribution was facilitated using a hyperlink generated through an online questionnaire software platform.
Sample size
According to the formula for calculating the sample size in cross-sectional surveys . In the formula, "n" represents the sample size for each group, "α" represents the type I error, which is typically set at 0.05, , δ represents the allowable error, typically set at 0.05, and "p" is set at 0.5 (as setting it at 0.5 maximizes the value and ensures a sufficiently large sample size). The calculated sample size "n" is 384. Considering an estimated questionnaire response rate of 80%, the final plan is to collect 480 valid questionnaires.
Statistical analysis
SPSS 22.0 (IBM, Armonk, NY, USA) was used for the analysis. Continuous variables were represented by means and standard deviations (SD). The categorical variables were represented by n (%). Continuous variables shall be subject to the normality test first. If they conform to the Normal distribution, the comparison between the two groups shall be subject to the t-test. If they do not conform to the Normal distribution, the comparison between the two groups shall be subject to the Wilcoxon Mann Whitney test; Three or more groups of continuous variables conform to Normal distribution with uniform variance, and ANOVA is used for comparison among multiple groups; If it does not conform to Normal distribution, Kruskal Wallis analysis of variance is adopted. Univariate and multivariate logistic regression analyses were used to identify factors associated with good knowledge, positive attitude and good practice which was defined as the score exceeding mean of the score. Ordered univariate and multivariate logistic regression analyses were used to identify factors associated with medication compliance. Variables with P < 0.05 in the univariate analysis were entered into the multivariate analysis, and odds ratios (ORs) and 95% confidence intervals (95%CIs) were calculated. A two-sided P-value less than 0.05 was considered to be statistically significant.
Results
In this study, a total of 513 questionnaires were collected, out of which 30 duplicates and those lacking patients' informed consent were excluded, resulting in 483 valid questionnaires for analysis. Among the participants, 189 (39.13%) were aged between 46 and 60 years, while a substantial majority of 366 (75.78%) reported being married. With respect to residency, 305 (63.15%) participants were situated in urban areas. In terms of educational attainment, 226 (46.79%) participants held either a college or undergraduate degree. Regarding employment status, 195 (40.37%) participants were engaged in full-time employment. An impressive 471 (97.52%) participants had undergone a single kidney transplant surgery, with 348 (72.05%) surpassing the three-year mark since their initial transplant. Notably, 469 (97.10%) participants had availed themselves of education regarding post-kidney transplant precautions. In the context of complications, the data revealed that 304 (62.94%) participants reported an absence of complications, while 60 (12.42%) had experienced postoperative infections. Furthermore, underlying medical conditions were evident, with hypertension prevalent among 303 (62.73%) participants, and hyperlipidemia observed in 78 (16.15%) individuals (Table 1).
Table 1.
Demographic characteristics
| Variables | N (%) | Knowledge Score | Attitude Score | Practice Score | |||
|---|---|---|---|---|---|---|---|
| Mean ± SD | P | Mean ± SD | P | Mean ± SD | P | ||
| Total | 483 | 23.44 ± 4.87 | 43.59 ± 2.65 | 52.52 ± 4.64 | |||
| Gender | 0.005 | 0.031 | 0.085 | ||||
| Male | 309(63.98) | 22.97 ± 5.07 | 43.39 ± 22.72 | 52.25 ± 4.81 | |||
| Female | 174(36.02) | 24.28 ± 4.39 | 43.94 ± 2.49 | 53.00 ± 4.29 | |||
| Age, years | 0.010 | 0.288 | 0.981 | ||||
| 16–35 | 81(16.77) | 24.83 ± 4.10 | 43.09 ± 3.29 | 52.60 ± 5.18 | |||
| 36–45 | 168(34.78) | 23.66 ± 5.32 | 43.64 ± 2.76 | 52.58 ± 4.61 | |||
| 46–60 | 189(39.13) | 22.71 ± 4.81 | 43.76 ± 2.20 | 52.49 ± 4.47 | |||
| ≥ 61 | 45(9.32) | 23.22 ± 4.18 | 43.60 ± 2.66 | 52.28 ± 4.50 | |||
| Marital Status | 0.163 | 0.515 | 0.200 | ||||
| Married | 366(75.78) | 23.21 ± 5.00 | 43.66 ± 2.72 | 52.31 ± 4.69 | |||
| Single | 78(16.15) | 24.31 ± 4.22 | 43.28 ± 2.47 | 53.07 ± 4.75 | |||
| Divorced/Widowed | 39(8.07) | 23.90 ± 4.78 | 43.54 ± 2.36 | 53.38 ± 3.70 | |||
| Residence | 0.038 | 0.333 | 0.388 | ||||
| Rural area | 92(19.05) | 22.70 ± 5.45 | 43.63 ± 2.65 | 52.88 ± 4.75 | |||
| Urban area | 305(63.15) | 23.88 ± 4.59 | 43.48 ± 2.68 | 52.57 ± 4.49 | |||
| Suburban area | 86(17.81) | 22.71 ± 5.07 | 43.95 ± 2.56 | 51.95 ± 5.01 | |||
| Education | < 0.001 | 0.227 | 0.272 | ||||
| Elementary school or below | 12(2.48) | 19.25 ± 6.97 | 42.92 ± 1.16 | 51.31 ± 8.12 | |||
| Junior high school | 93(19.25) | 22.12 ± 6.00 | 43.38 ± 2.16 | 52.60 ± 5.02 | |||
| High school/Technical school | 137(28.36) | 23.57 ± 4.63 | 43.76 ± 2.74 | 52.78 ± 4.20 | |||
| College/Undergraduate | 226(46.79) | 24.27 ± 3.92 | 43.69 ± 2.76 | 52.55 ± 4.44 | |||
| Master’s degree or above | 15(3.11) | 21.40 ± 6.76 | 42.33 ± 3.50 | 50.17 ± 5.08 | |||
| Employment | 0.004 | 0.634 | 0.127 | ||||
| Full-time employment | 195(40.37) | 24.29 ± 4.39 | 43.78 ± 2.83 | 52.70 ± 4.75 | |||
| Unemployment | 58(12.01) | 22.88 ± 5.88 | 43.21 ± 2.36 | 53.17 ± 4.16 | |||
| Retired | 108(22.36) | 22.10 ± 5.00 | 43.48 ± 2.42 | 51.74 ± 4.83 | |||
| Self-employed/Freelancer/Part-time | 92(19.05) | 23.53 ± 4.71 | 43.68 ± 2.58 | 52.15 ± 4.58 | |||
| Homemaker/housewife | 24(4.97) | 22.88 ± 5.11 | 43.08 ± 3.23 | 53.85 ± 3.35 | |||
| Student | 6(1.24) | 26.33 ± 1.97 | 43.50 ± 1.64 | 54.83 ± 4.15 | |||
| Per capita income, China Yuan (CNY) | 0.077 | 0.040 | 0.863 | ||||
| ≤ 2000 | 58(12.01) | 22.71 ± 6.28 | 43.00 ± 2.76 | 52.36 ± 4.65 | |||
| 2001–5000 | 130(26.92) | 22.78 ± 5.17 | 43.26 ± 2.59 | 52.44 ± 4.76 | |||
| 5001–10000 | 143(29.61) | 23.45 ± 4.60 | 43.68 ± 2.34 | 52.34 ± 4.87 | |||
| 10,001–20000 | 80(16.56) | 24.48 ± 3.51 | 44.22 ± 2.30 | 53.03 ± 4.04 | |||
| > 20,000 | 72(14.91) | 24.06 ± 4.72 | 43.78 ± 3.41 | 52.56 ± 4.67 | |||
| Smoking habit | 0.107 | 0.445 | 0.172 | ||||
| Smoker | 33(6.83) | 22.73 ± 5.65 | 43.09 ± 2.94 | 51.10 ± 5.29 | |||
| Former smoker | 118(24.43) | 22.75 ± 4.83 | 43.75 ± 2.49 | 52.79 ± 4.28 | |||
| Non-Smoker | 332(68.74) | 23.76 ± 4.79 | 43.58 ± 2.68 | 52.57 ± 4.68 | |||
| Health Insurance | 0.187 | 0.839 | 0.018 | ||||
| Only social medical insurance | 426(88.20) | 23.46 ± 4.65 | 43.56 ± 2.67 | 52.48 ± 4.57 | |||
| Only commercial medical insurance | 5(1.04) | 23.60 ± 6.43 | 43.20 ± 3.03 | 51.70 ± 3.05 | |||
| Both social medical and commercial medical insurance | 49(10.14) | 23.63 ± 6.07 | 43.90 ± 2.61 | 53.39 ± 4.42 | |||
| No insurance | 3(0.62) | 17.33 ± 10.26 | 43.33 ± 0.58 | 44.92 ± 11.67 | |||
| Number of kidney transplant surgeries | 0.215 | 0.735 | 0.432 | ||||
| 1 | 471(97.52) | 23.40 ± 4.91 | 43.60 ± 2.66 | 52.55 ± 4.64 | |||
| 2 | 12(2.48) | 25.17 ± 2.92 | 43.33 ± 2.19 | 51.48 ± 4.45 | |||
| Time since first kidney transplant surgery, years | 0.255 | 0.452 | 0.003 | ||||
| < 1 | 43(8.90) | 24.12 ± 4.49 | 44.07 ± 2.30 | 54.44 ± 3.26 | |||
| 1–3 | 92(19.05) | 23.99 ± 4.88 | 43.49 ± 2.36 | 53.15 ± 4.64 | |||
| > 3 | 348(72.05) | 23.22 ± 4.91 | 43.56 ± 2.76 | 52.12 ± 4.71 | |||
| Post-kidney transplant precaution education | 0.008 | < 0.001 | < 0.001 | ||||
| Received education | 469(97.10) | 23.54 ± 4.78 | 43.69 ± 2.49 | 52.65 ± 4.46 | |||
| Did not receive education | 14(2.90) | 20.07 ± 6.78 | 40.14 ± 4.97 | 48.29 ± 7.88 | |||
| Family Experience with Kidney Transplant | 0.537 | 0.390 | 0.635 | ||||
| Yes | 11(2.28) | 22.55 ± 6.58 | 42.91 ± 2.66 | 51.86 ± 6.92 | |||
| No | 472(97.72) | 23.46 ± 4.83 | 43.61 ± 2.65 | 52.53 ± 4.58 | |||
| Current complications (Multiple choices) | |||||||
| None | 304(62.94) | 23.89 ± 4.58 | 43.99 ± 2.42 | 52.95 ± 4.58 | |||
| Postoperative infection | 60(12.42) | 23.03 ± 5.17 | 42.90 ± 2.38 | 52.60 ± 4.04 | |||
| Rejection reaction | 61(12.63) | 23.41 ± 5.65 | 42.85 ± 3.54 | 52.26 ± 4.61 | |||
| Transplanted kidney bleeding | 4(0.83) | 25.75 ± 4.50 | 43.00 ± 2.58 | 55.00 ± 2.45 | |||
| Ureteral stenosis | 11(2.28) | 20.45 ± 5.45 | 40.73 ± 5.78 | 49.73 ± 6.68 | |||
| Thromboembolic disease | 10(2.07) | 22.30 ± 4.97 | 44.30 ± 1.25 | 50.80 ± 4.92 | |||
| Osteoporosis | 53(10.97) | 21.40 ± 5.35 | 42.13 ± 2.37 | 50.73 ± 5.26 | |||
| Other | 71(14.70) | 23.00 ± 5.24 | 42.86 ± 3.29 | 52.23 ± 5.17 | |||
| Underlying medical conditions (Multiple choices) | |||||||
| None | 135(27.95) | 24.51 ± 4.31 | 43.79 ± 2.39 | 52.97 ± 4.32 | |||
| Hypertension | 303(62.73) | 22.99 ± 4.96 | 43.46 ± 2.73 | 52.38 ± 4.71 | |||
| Heart disease | 43(8.90) | 21.86 ± 6.01 | 43.00 ± 3.77 | 52.21 ± 5.37 | |||
| Hyperlipidemia | 78(16.15) | 22.12 ± 5.05 | 43.26 ± 2.72 | 51.41 ± 4.85 | |||
| Diabetes | 48(9.94) | 22.54 ± 5.12 | 42.90 ± 2.73 | 53.06 ± 4.63 | |||
| Neoplastic diseases | 10(2.07) | 26.60 ± 2.07 | 44.20 ± 2.62 | 53.13 ± 4.67 | |||
| Other | 36(7.45) | 21.94 ± 5.76 | 43.19 ± 3.19 | 52.31 ± 5.18 | |||
The mean score of knowledge, attitude and practice were 23.44 ± 4.87 (possible range: 0–28), 43.59 ± 2.65 (possible range: 10–50), 52.52 ± 4.64 (possible range: 0–58), respectively. Gender was linked to knowledge scores (p = 0.005), with females more likely to have higher knowledge scores. Age also played a role in knowledge scores (p = 0.010), with the 16–35 and ≥ 61 age groups more likely to exhibit increased knowledge scores compared to the 46–60 age group. Education (p < 0.001) and employment status (p = 0.004) were associated with knowledge scores, indicating that those with lower education levels and employed participants were less likely to have high knowledge scores. Per capita income demonstrated significance with attitude scores (p = 0.040), highlighting that individuals earning 10,001–20000 China Yuan (about $1,386 to $2,772 United States dollar) were more likely to possess positive attitudes. Health insurance influenced practice scores (p = 0.018), with those without insurance less likely to adopt recommended practices. Education on post-kidney transplant precautions associated with higher knowledge (p = 0.008), attitude (p < 0.001), and practice (p < 0.001) scores, emphasizing that educated individuals were more likely to excel in all three dimensions (Table 1).
The three knowledge items with the highest understanding rates were as follows: "Post-kidney transplant recipients are not recommended to use medications or foods that claim to enhance the immune system" (K7) with a correctness rate of 83.44%, "Post-kidney transplant, early mobilization is essential, with daily activity goals set to actively prevent deep vein thrombosis" (K8) with a correctness rate of 77.64%, and "Post-kidney transplant recipients should adhere to regular follow-up and routine examinations. In case of any discomfort, especially fever or oliguria, timely medical consultation is necessary" (K14) with a correctness rate of 94.41%. The three items with the lowest correctness rates were "Post-kidney transplant recipients are prone to complications such as pleural effusion, atelectasis, and lung infections. Early respiratory function exercises are effective methods to increase respiratory muscle strength, promote lung expansion, and reduce postoperative complications" (K9) with a correctness rate of 37.47%, "Respiratory function exercise methods include diaphragmatic breathing, lip-pursued breathing, and using a respiratory training device" (K10) with a correctness rate of 41.41%, and "Post-transplant bone diseases are relatively common, with osteoporosis being a prominent condition. Supplementing vitamin D has a beneficial effect on bone mineral density in adult kidney transplant recipients" (K5) with a correctness rate of 59.01% (Supplementary Table 1).
A significant majority of the patients (97.10%) strongly agreed or agreed that kidney transplantation had brought them a new lease on life, invoking gratitude and cherishment (A1). Similarly, a substantial proportion (91.51%) expressed their belief in the importance of following medical advice and dietary management after kidney transplantation (A5). Furthermore, an overwhelming number of patients (96.69%) affirmed their understanding of the significance of adhering to immunosuppressive medications and monitoring drug concentrations in their blood (A6). On a related note, a substantial majority (91.72%) acknowledged the importance of maintaining good mental health in the context of post-kidney transplant self-management (A7). It is noteworthy, however, that a notable segment of patients (38.92%) reported feeling substantial pressure due to the potential for rejection reactions and complications following transplantation (A2) (Supplementary Table 2).
The examination of patients' behaviors within their treatment regimen revealed that in relation to medication-related practices, 43.06% occasionally forgot to adhere to their prescribed medication schedule (Item 1), 7.66% reported instances of missing medication days in the preceding two weeks (Item 2), and 13.87% acknowledged instances of reducing or discontinuing their medication when confronted with a deterioration of symptoms (Item 3). Notably, a substantial 82.40% of patients (P1) affirmed their commitment to following the doctor's advice for regular follow-up visits. Additionally, an impressive 89.65% (P2) promptly sought medical attention in case of discomfort. Furthermore, patients reported adherence to dietary and lifestyle recommendations, with percentages ranging from 61.08% (P3) to 76.81% (P4). Patients also demonstrated their dedication to psychological well-being and self-care practices, with up to 68.74% (P10) prioritizing maintaining a calm mindset (Supplementary Table 3). The results of the binary classification analysis for each dimension are presented in Supplementary Table 4.
The multivariate analysis showed that females (OR = 2.06, 95% CI = 1.25–3.39, p = 0.005) and retired (OR = 0.35, 95% CI = 0.18–0.69, p = 0.002) were independently associated with good knowledge (> 23.44) (Table 2). The multivariate analysis showed that knowledge scores (OR = 1.05, 95% CI = 1.01–1.09, p = 0.016), females (OR = 1.63, 95% CI = 1.08–2.46, p = 0.020), unemployed (OR = 0.52, 95% CI = 0.28–0.98, p = 0.041), full-time homemakers or housewives (OR = 0.38, 95% CI = 0.17–0.87, p = 0.021), and did not receive education on post-kidney transplant precautions (OR = 0.09, 95% CI = 0.01–0.69, p = 0.021) were independently associated with positive attitude (> 43.59) (Table 3). The multivariate analysis showed that knowledge scores (OR = 1.15, 95% CI = 1.10–1.20, p < 0.001), attitude scores (OR = 1.22, 95% CI = 1.12–1.32, p < 0.001) and undergone transplantation within 1 year (OR = 3.92, 95% CI = 1.60–9.63, p = 0.003) were independently associated with good practice (> 52.52) (Table 4).
Table 2.
Univariate and multivariate analysis for good knowledge (> 23.44)
| Variables | Univariate Analysis | Multivariate Analysis | ||||
|---|---|---|---|---|---|---|
| OR | 95%CI | P | OR | 95%CI | P | |
| Gender | ||||||
| Male | Ref | Ref | ||||
| Female | 1.72 | 1.17, 2.54 | 0.006 | 2.06 | 1.25, 3.39 | 0.005 |
| Age, years | ||||||
| 16–35 | Ref | Ref | ||||
| 36–45 | 0.74 | 0.42, 1.31 | 0.298 | 0.74 | 0.40, 1.39 | 0.355 |
| 46–60 | 0.46 | 0.27, 0.81 | 0.007 | 0.64 | 0.33, 1.24 | 0.186 |
| ≥ 61 | 0.40 | 0.19, 0.86 | 0.018 | 1.00 | 0.36, 2.79 | 0.995 |
| Marital Status | ||||||
| Married | Ref | Ref | ||||
| Single | 1.73 | 1.02, 2.92 | 0.040 | 1.14 | 0.62, 2.09 | 0.669 |
| Divorced/Widowed | 1.23 | 0.62, 2.42 | 0.551 | 0.99 | 0.48, 2.05 | 0.986 |
| Residence | ||||||
| Rural area | 0.67 | 0.42, 1.07 | 0.096 | 0.66 | 0.37, 1.17 | 0.152 |
| Urban area | Ref | Ref | ||||
| Suburban area | 0.62 | 0.38, 1.00 | 0.049 | 0.62 | 0.37, 1.06 | 0.081 |
| Education | ||||||
| Elementary school or below | 0.39 | 0.12, 1.27 | 0.119 | 0.65 | 0.18, 2.33 | 0.513 |
| Junior high school | 0.56 | 0.34, 0.91 | 0.020 | 0.79 | 0.43, 1.44 | 0.438 |
| High school/Technical school | 0.77 | 0.50, 1.19 | 0.237 | 1.00 | 0.62, 1.61 | 0.990 |
| College/Undergraduate | Ref | Ref | ||||
| Master’s degree or above | 0.48 | 0.17, 1.37 | 0.170 | 0.36 | 0.12, 1.10 | 0.072 |
| Employment | ||||||
| Full-time employment | Ref | Ref | ||||
| Unemployment | 0.80 | 0.44, 1.46 | 0.460 | 1.00 | 0.50, 2.00 | 0.995 |
| Retired | 0.40 | 0.25, 0.65 | < 0.001 | 0.35 | 0.18, 0.69 | 0.002 |
| Self-employed/Freelancer/Part-time | 0.78 | 0.47, 1.30 | 0.336 | 0.93 | 0.53, 1.64 | 0.805 |
| Homemaker/housewife | 1.05 | 0.46, 2.36 | 0.912 | 0.77 | 0.31, 1.88 | 0.566 |
| Student | ||||||
| Per Capita Income, CNY | 1.24 | 0.66, 2.32 | 0.508 | |||
| ≤ 2000 | 0.70 | 0.44, 1.13 | 0.148 | |||
| 2001–5000 | Ref | |||||
| 5001–10000 | 1.24 | 0.70, 2.17 | 0.463 | |||
| 10,001–20000 | 1.40 | 0.78, 2.54 | 0.261 | |||
| Smoking habit | ||||||
| Smoker | 0.72 | 0.35, 1.49 | 0.381 | 0.99 | 0.45, 2.16 | 0.973 |
| Former smoker | 0.62 | 0.41, 0.95 | 0.030 | 0.83 | 0.51, 1.37 | 0.469 |
| Non-Smoker | Ref | Ref | ||||
| Health Insurance | ||||||
| Only social medical insurance | 2.76 | 0.25, 30.67 | 0.409 | |||
| Only commercial medical insurance | 3.00 | 0.15, 59.89 | 0.472 | |||
| Both social medical and commercial medical insurance | 4.53 | 0.38, 53.93 | 0.232 | |||
| No insurance | Ref | |||||
| Number of kidney transplant surgeries | ||||||
| 1 | Ref | |||||
| 2 | 2.12 | 0.57, 7.93 | 0.264 | |||
| Time since first kidney transplant surgery, years | ||||||
| < 1 | 1.79 | 0.90, 3.55 | 0.096 | |||
| 1–3 | 1.39 | 0.86, 2.23 | 0.178 | |||
| > 3 | Ref | |||||
| Post-kidney transplant precaution education | ||||||
| Received education | Ref | |||||
| Did not receive education | 0.38 | 0.12, 1.14 | 0.083 | |||
| Family Experience with Kidney Transplant | ||||||
| Yes | Ref | |||||
| No | 1.20 | 0.36, 4.00 | 0.761 | |||
Table 3.
Univariate and multivariate analysis for positive attitude (> 43.59)
| Variables | Univariate Analysis | Multivariate Analysis | ||||
|---|---|---|---|---|---|---|
| OR | 95%CI | P | OR | 95%CI | P | |
| Knowledge score | 1.07 | 1.03, 1.11 | 0.001 | 1.05 | 1.01, 1.09 | 0.016 |
| Gender | ||||||
| Male | Ref | Ref | ||||
| Female | 1.55 | 1.07, 2.26 | 0.021 | 1.63 | 1.08, 2.46 | 0.020 |
| Age, years | ||||||
| 16–35 | Ref | |||||
| 36–45 | 1.25 | 0.73, 2.13 | 0.411 | |||
| 46–60 | 1.35 | 0.80, 2.27 | 0.265 | |||
| ≥ 61 | 1.31 | 0.63, 2.71 | 0.473 | |||
| Marital Status | ||||||
| Married | Ref | |||||
| Single | 0.85 | 0.52, 1.38 | 0.500 | |||
| Divorced/Widowed | 0.59 | 0.30, 1.15 | 0.121 | |||
| Residence | ||||||
| Rural area | 0.97 | 0.61, 1.55 | 0.906 | |||
| Urban area | Ref | |||||
| Suburban area | 1.40 | 0.87, 2.28 | 0.167 | |||
| Education | ||||||
| Elementary school or below | 0.44 | 0.13, 1.51 | 0.192 | |||
| Junior high school | 0.73 | 0.45, 1.18 | 0.198 | |||
| High school/Technical school | 0.90 | 0.59, 1.37 | 0.614 | |||
| College/Undergraduate | Ref | |||||
| Master’s degree or above | 0.59 | 0.20, 1.71 | 0.330 | |||
| Employment | ||||||
| Full-time employment | Ref | Ref | ||||
| Unemployment | 0.46 | 0.25, 0.84 | 0.011 | 0.52 | 0.28, 0.98 | 0.041 |
| Retired | 0.78 | 0.48, 1.24 | 0.292 | 0.82 | 0.50, 1.34 | 0.425 |
| Self-employed/Freelancer/Part-time | 0.88 | 0.53, 1.44 | 0.610 | 1.02 | 0.61, 1.71 | 0.930 |
| Homemaker/housewife | 0.47 | 0.21, 1.03 | 0.060 | 0.38 | 0.17, 0.87 | 0.021 |
| Student | ||||||
| Per Capita Income, CNY | 0.60 | 0.32, 1.12 | 0.111 | |||
| ≤ 2000 | 0.72 | 0.45, 1.17 | 0.184 | |||
| 2001–5000 | 10.56 | 0.89, 2.72 | 0.118 | |||
| 5001–10000 | 10.46 | 0.82, 2.60 | 0.194 | |||
| 10,001–20000 | ||||||
| Smoking habit | ||||||
| Smoker | 0.75 | 0.36, 1.54 | 0.427 | |||
| Former smoker | 1.12 | 0.74, 1.71 | 0.596 | |||
| Non-Smoker | Ref | |||||
| Health Insurance | ||||||
| Only social medical insurance | 2.00 | 0.18, 22.22 | 0.573 | |||
| Only commercial medical insurance | 1.33 | 0.07, 26.62 | 0.851 | |||
| Both social medical and commercial medical insurance | 2.08 | 0.18, 24.51 | 0.559 | |||
| No insurance | Ref | |||||
| Number of kidney transplant surgeries | ||||||
| 1 | Ref | |||||
| 2 | 1.00 | 0.32, 3.16 | 0.994 | |||
| Time since first kidney transplant surgery, years | ||||||
| < 1 | 1.25 | 0.66, 2.36 | 0.495 | |||
| 1–3 | 0.83 | 0.52, 1.32 | 0.429 | |||
| > 3 | Ref | |||||
| Post-kidney transplant precaution education | ||||||
| Received education | Ref | Ref | ||||
| Did not receive education | 0.07 | 0.01, 0.57 | 0.012 | 0.09 | 0.01, 0.69 | 0.021 |
| Family Experience with Kidney Transplant | ||||||
| Yes | Ref | |||||
| No | 1.20 | 0.36, 3.99 | 0.766 | |||
Table 4.
Univariate and multivariate analysis for good practice (> 52.52)
| Variables | Univariate Analysis | Multivariate Analysis | ||||
|---|---|---|---|---|---|---|
| OR | 95%CI | P | OR | 95%CI | P | |
| Knowledge score | 1.17 | 1.12, 1.23 | < 0.001 | 1.15 | 1.10 | < 0.001 |
| Attitude score | 1.28 | 1.17, 1.39 | < 0.001 | 1.22 | 1.12 | < 0.001 |
| Gender | ||||||
| Male | Ref | |||||
| Female | 1.37 | 0.94, 2.00 | 0.106 | |||
| Age, years | ||||||
| 16–35 | Ref | |||||
| 36–45 | 0.89 | 0.51, 1.53 | 0.666 | |||
| 46–60 | 0.74 | 0.43, 1.25 | 0.260 | |||
| ≥ 61 | 0.74 | 0.35, 1.54 | 0.416 | |||
| Marital Status | ||||||
| Married | Ref | |||||
| Single | 1.59 | 0.95, 2.66 | 0.078 | |||
| Divorced/Widowed | 1.59 | 0.79, 3.19 | 0.193 | |||
| Residence | ||||||
| Rural area | 1.36 | 0.83, 2.20 | 0.219 | |||
| Urban area | Ref | |||||
| Suburban area | 0.79 | 0.49, 1.28 | 0.346 | |||
| Education | ||||||
| Elementary school or below | 0.98 | 0.30, 3.18 | 0.972 | |||
| Junior high school | 0.93 | 0.57, 1.51 | 0.759 | |||
| High school/Technical school | 1.07 | 0.70, 1.66 | 0.744 | |||
| College/Undergraduate | Ref | |||||
| Master’s degree or above | 0.47 | 0.16, 1.35 | 0.161 | |||
| Employment | ||||||
| Full-time employment | Ref | Ref | ||||
| Unemployment | 1.05 | 0.57, 1.94 | 0.865 | 1.42 | 0.71, 2.84 | 0.319 |
| Retired | 0.54 | 0.33, 0.86 | 0.010 | 0.80 | 0.47, 1.36 | 0.407 |
| Self-employed/Freelancer/Part-time | 0.74 | 0.45, 1.23 | 0.250 | 0.82 | 0.47, 1.43 | 0.484 |
| Homemaker/housewife | 1.40 | 0.61, 3.21 | 0.432 | 2.03 | 0.79, 5.23 | 0.141 |
| Student | ||||||
| Per Capita Income, CNY | 1.08 | 0.58, 2.01 | 0.797 | |||
| ≤ 2000 | 0.92 | 0.57, 1.49 | 0.736 | |||
| 2001–5000 | Ref | |||||
| 5001–10000 | 1.42 | 0.81, 2.50 | 0.223 | |||
| 10,001–20000 | 1.20 | 0.67, 2.14 | 0.531 | |||
| Smoking habit | ||||||
| Smoker | 0.52 | 0.25, 1.07 | 0.075 | |||
| Former smoker | 1.14 | 0.74, 1.75 | 0.552 | |||
| Non-Smoker | Ref | |||||
| Health Insurance | ||||||
| Only social medical insurance | 2.66 | 0.24, 29.51 | 0.427 | |||
| Only commercial medical insurance | 1.33 | 0.07, 26.62 | 0.851 | |||
| Both social medical and commercial medical insurance | 5.54 | 0.46, 66.32 | 0.177 | |||
| No insurance | Ref | |||||
| Number of kidney transplant surgeries | ||||||
| 1 | Ref | |||||
| 2 | 0.71 | 0.22, 2.22 | 0.553 | |||
| Time since first kidney transplant surgery, years | ||||||
| < 1 | 4.28 | 1.85, 9.87 | 0.001 | 3.92 | 1.60, 9.63 | 0.003 |
| 1–3 | 1.29 | 0.81, 2.07 | 0.282 | 1.18 | 0.70, 1.98 | 0.534 |
| > 3 | Ref | Ref | ||||
| Post-kidney transplant precaution education | ||||||
| Received education | Ref | |||||
| Did not receive education | 0.52 | 0.18, 1.54 | 0.239 | |||
| Family Experience with Kidney Transplant | ||||||
| Yes | Ref | |||||
| No | 0.52 | 0.14, 1.98 | 0.337 | |||
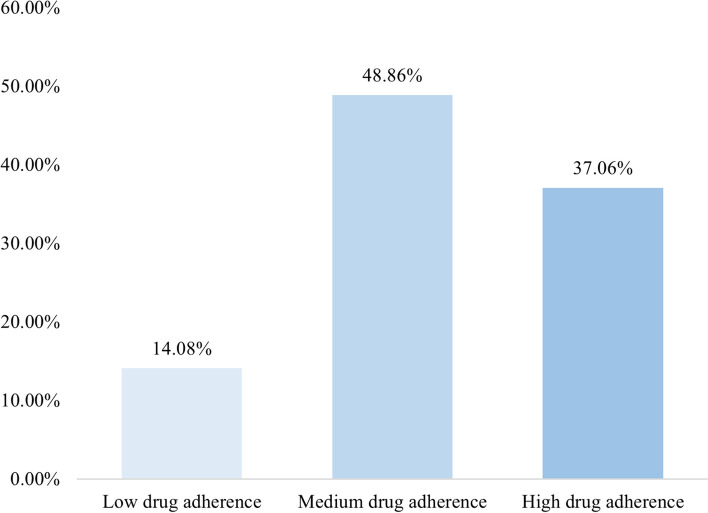
The multivariate analysis showed that knowledge scores (OR = 1.06, 95% CI = 1.02–1.10, p = 0.003), attitude scores (OR = 1.16, 95% CI = 1.08–1.25, p < 0.001), aged 16–35 years (OR = 0.38, 95% CI = 0.18–0.78, p = 0.009), underwent a single kidney transplant surgery (OR = 3.97, 95% CI = 1.28–12.38, p = 0.017) were independently associated with medication adherence (Table 5). Medication Adherence Status is shown in Fig. 1.
Table 5.
Univariate and multivariate analysis for medication adherence
| Variables | Univariate Analysis | Multivariate Analysis | ||||
|---|---|---|---|---|---|---|
| OR | 95%CI | P | OR | 95%CI | P | |
| Knowledge score | 1.07 | 1.03,1.11 | < 0.001 | 1.06 | 1.02, 1.10 | 0.003 |
| Attitude score | 1.20 | 1.12,1.29 | < 0.001 | 1.16 | 1.08, 1.25 | < 0.001 |
| Gender | ||||||
| Male | 0.82 | 0.58,1.17 | 0.274 | |||
| Female | Ref | |||||
| Age, years | ||||||
| 16–35 | 0.47 | 0.23,0.94 | 0.032 | 0.38 | 0.18, 0.78 | 0.009 |
| 36–45 | 0.75 | 0.40,1.40 | 0.366 | 0.62 | 0.32, 1.19 | 0.149 |
| 46–60 | 0.98 | 0.52,1.81 | 0.936 | 0.84 | 0.44, 1.59 | 0.587 |
| ≥ 61 | Ref | Ref | ||||
| Marital Status | ||||||
| Married | 1.43 | 0.76, 2.69 | 0.264 | |||
| Single | 1.63 | 0.78, 3.39 | 0.191 | |||
| Divorced/Widowed | ||||||
| Residence | ||||||
| Rural | 0.98 | 0.56, 1.72 | 0.952 | |||
| Urban | 1.10 | 0.69, 1.73 | 0.694 | |||
| Suburban | Ref | |||||
| Education | ||||||
| Elementary school or below | 0.87 | 0.21, 3.71 | 0.518 | |||
| Junior high school | 1.10 | 0.39, 3.11 | 0.856 | |||
| High school/Technical school | 1.37 | 0.50,3.78 | 0.855 | |||
| College/Undergraduate | 1.39 | 0.51,3.75 | 0.543 | |||
| Master’s degree or above | Ref | |||||
| Employment | ||||||
| Employed (full time) | 0.89 | 0.43, 1.84 | 0.748 | |||
| Unemployed | 0.85 | 0.37, 1.97 | 0.705 | |||
| Retired | 0.91 | 0.42, 1.96 | 0.802 | |||
| Self-employed/Freelancer/Part-time | 0.62 | 0.28, 1.35 | 0.227 | |||
| Full-time homemaker/housewife | Ref | |||||
| Student | ||||||
| Per Capita Income, CNY | 0.83 | 0.49, 1.43 | 0.507 | |||
| ≤ 2000 | 0.55 | 0.28, 1.06 | 0.076 | |||
| 2001–5000 | 0.76 | 0.44, 1.31 | 0.316 | |||
| 5001–10000 | 0.93 | 0.51, 1.71 | 0.821 | |||
| 10,001–20000 | Ref | |||||
| Smoking habit | ||||||
| Yes | 1.00 | 0.51, 1.97 | 0.998 | |||
| Former smoker | 0.87 | 0.58, 1.30 | 0.496 | |||
| No | ||||||
| Health Insurance | ||||||
| Only social medical insurance (e.g., employee medical insurance, “New Rural Cooperative Medical System,” “Urban Resident Basic Medical Insurance) | 0.52 | 0.06, 4.80 | 0.566 | |||
| Only commercial medical insurance | 0.42 | 0.03, 6.75 | 0.543 | |||
| Both social medical insurance and commercial medical insurance | 0.36 | 0.04, 3.51 | 0.380 | |||
| No insurance | Ref | |||||
| Times of kidney transplant surgeries | ||||||
| 1 | 3.12 | 1.04, 9.34 | 0.042 | 3.97 | 1.28, 12.38 | 0.017 |
| 2 | Ref | Ref | ||||
| For your first kidney transplant, how long has it been since the surgery | ||||||
| < 1 year | 1.74 | 0.94, 3.20 | 0.076 | |||
| 1–3 years | 1.45 | 0.93, 2.24 | 0.100 | |||
| 3 years or more | Ref | |||||
| Education on post-kidney transplant precautions | ||||||
| Yes | 2.88 | 1.04, 7.96 | 0.041 | 1.48 | 0.50, 4.38 | 0.474 |
| No | Ref | |||||
| Do other members of your family have experience with kidney | ||||||
| Yes | 0.41 | 0.13, 1.29 | 0.128 | |||
| No | Ref | |||||
Fig. 1.
Medication adherence status
Discussion
Kidney transplant recipients exhibited good knowledge, positive attitude and good practice toward postoperative self-management. To enhance the efficacy of postoperative self-management among kidney transplant recipients, it is advisable to integrate tailored educational interventions, psychological support mechanisms, and vigilant monitoring strategies.
The assessment of knowledge, attitude, and practice scores provides a comprehensive understanding of patients' management of post-kidney transplant care. While reasonable mean scores for knowledge and positive attitude signify foundational awareness and motivation to adhere to care recommendations, there exists room for improvement in the practice domain. Although patients possess knowledge and positive attitudes, effective translation into consistent actions necessitates targeted interventions. These findings are consistent with similar studies on chronic disease management and self-care [21, 22]. The observed correlation between higher education and improved knowledge scores supports existing research highlighting education's role in health literacy [23–25].
The demographic distribution of participants in this study reflects trends observed in previous research on kidney transplant recipients. Studies consistently show that the majority of transplant recipients fall within the age range of 46 to 60 years, likely due to the higher incidence of kidney diseases in older adults [26, 27]. The prevalence of married participants aligns with research indicating that social support, often provided by spouses, positively impacts post-transplant outcomes [28, 29]. Similarly, the higher educational attainment observed here corresponds with literature highlighting education's influence on health behaviors and adherence [30]. This demographic profile offers insights into the population under investigation, where participants' predominant age range of 46 to 60 years and their married status could reflect the prevalence of kidney disease and transplantation among middle-aged individuals. The concentration of participants in urban areas might indicate better access to healthcare facilities and transplant centers. Moreover, the prevalence of higher educational attainment suggests that educational background could play a role in patients' understanding and engagement in post-transplant care.
The variability in the accuracy of knowledge items emphasizes the significance of targeted educational interventions, aligning with analogous findings in studies concentrating on patient education for chronic disease management [31]. Notably, challenges in comprehending certain items, including respiratory exercises and post-transplant bone health, resonate with the intricate nature of medical information, potentially necessitating simplified and patient-centric explanations [32]. The identification of individual knowledge items with varying correctness rates serves to highlight sectors warranting focused patient education endeavors. Items with elevated correctness rates denote effective communication of general post-transplant precautions. In contrast, the struggles in grasping specific elements like respiratory exercises and post-transplant bone health accentuate opportunities for fortifying patient education in these domains. By addressing these gaps through tailored educational strategies, a more comprehensive level of patient knowledge can be achieved.
The participants' favorable attitudes towards kidney transplantation and their adherence to medical advice align with the recognized positive influence of transplantation on patients' quality of life [33, 34]. Correspondingly, the acknowledgment of pressure stemming from potential complications resonates with the psychological burden commonly faced by transplant recipients, as indicated by qualitative research [35, 36]. The positive attitudes exhibited by patients towards kidney transplantation and their dedication to medical guidance and dietary management signify their recognition of the procedure's benefits, playing a pivotal role in effective post-transplant care. Nevertheless, a notable subset of patients encountering pressure due to potential complications accentuates the psychological challenges associated with transplantation. Introducing psychological support into the care regimen stands as a potential strategy to alleviate these concerns and foster overall well-being.
The documented cases of medication non-adherence, encompassing instances of forgetting medication schedules, underscore well-established difficulties encountered in managing chronic diseases [37]. Additionally, the notable dedication to follow-up appointments and timely medical attention mirrors findings that underscore the pivotal role of healthcare provider-patient relationships in enhancing patient engagement [38]. Through an examination of medication-related behaviors, insights into challenges pertaining to adhering to prescribed regimens emerge. The occurrences of missed medication schedules and doses illuminate specific areas necessitating interventions aimed at bolstering adherence. Moreover, the elevated rates of commitment demonstrated in follow-up visits and the prompt pursuit of medical care serve as encouraging indications of robust patient engagement. Notably, the adherence to dietary and lifestyle recommendations further underscores patients' active involvement in their care.
The pertinence of gender, age, retirement status, education, and employment in shaping knowledge, attitude, practice, and medication adherence aligns cohesively with existing research that underscores socio-demographic factors as pivotal predictors of health-related behaviors [39]. The multivariate analyses conducted in this study provide a thorough understanding of the intricate factors that exert influence over various dimensions of patient care. These insightful findings subsequently facilitate the customization of interventions based on the unique characteristics of individual patients. The observed impact of gender, age, retirement status, educational level, and employment status across knowledge, attitude, practice, and medication adherence further underscores the imperative of addressing a diverse array of patient needs.
This study had several limitations. Firstly, the cross-sectional design restricts our ability to infer causality or establish temporal relationships between variables. Secondly, the reliance on self-reported data might introduce recall bias or social desirability bias, potentially compromising the accuracy of responses. Thirdly, the study's focus on a single hospital may limit the generalizability of the findings to broader populations. Moreover, the use of an online survey could exclude individuals without internet access or those less comfortable with digital interfaces, potentially omitting significant demographic groups. Importantly, the underrepresentation of younger adults, particularly those aged 20 and below, in our study population suggests a need for caution in extrapolating our findings to this subgroup.
Conclusions
Kidney transplant recipients had good knowledge, positive attitude and good practice toward postoperative self-management. Targeted educational modules to address knowledge gaps, integrated psychosocial support, adherence strategies, and patient engagement are recommended. Emphasizing follow-up, lifestyle compliance, adopting a holistic care approach with specialists, and establishing ongoing assessment mechanisms are also recommended.
Supplementary Information
Acknowledgements
None.
Abbreviations
- KAP
Knowledge, attitude, and practice
- ESRD
End-stage renal disease
- SOT
Solid organ transplant
- CNY
China Yuan
Authors’ contributions
Xiqian Huang carried out the studies, participated in collecting data, and drafted the manuscript. Beihua Xi performed the statistical analysis and participated in its design. Chengjie Xuan, Yi Bao, and Lin Wang participated in acquisition, analysis, or interpretation of data and draft the manuscript. All authors read and approved the final manuscript.
Funding
None.
Availability of data and materials
All data generated or analysed during this study are included in this published article and its supplementary information files.
Declarations
Ethics approval and consent to participate
This work has been carried out in accordance with the Declaration of Helsinki (2000) of the World Medical Association. This study has been approved by Ethics Committee of Ruijin Hospital (No. 2021–385), and informed consent was obtained from each patient.
Consent for publication
Not applicable.
Competing interests
The authors report that they have no relationships relevant to the contents of this paper to disclose.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Xiqian Huang and Beihua Xi are co-first authors.
References
- 1.Liu FX, Rutherford P, Smoyer-Tomic K, Prichard S, Laplante S. A global overview of renal registries: a systematic review. BMC Nephrol. 2015;16:31. doi: 10.1186/s12882-015-0028-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chaudry M, Gislason GH, Fosbøl EL, Køber L, Gerds TA, Torp-Pedersen C. Hypertension, cardiovascular disease and cause of death in Danish living kidney donors: matched cohort study. BMJ Open. 2020;10(11):e041122. doi: 10.1136/bmjopen-2020-041122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zhang W, Li J, Qi G, Tu G, Yang C, Xu M. Myeloid-derived suppressor cells in transplantation: the dawn of cell therapy. J Transl Med. 2018;16(1):19. doi: 10.1186/s12967-018-1395-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nielsen C, Agerskov H, Bistrup C, Clemensen J. 'The hospital and everyday life are two worlds': patients' and healthcare professionals' experiences and perspectives on collaboration in the kidney transplantation process. Nurs Open. 2019;6(4):1491–1500. doi: 10.1002/nop2.349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kim S, Ju MK, Son S, Jun S, Lee SY, Han CS. Development of video-based educational materials for kidney-transplant patients. PLoS One. 2020;15(8):e0236750. doi: 10.1371/journal.pone.0236750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.De Geest S, Dobbels F, Fluri C, Paris W, Troosters T. Adherence to the therapeutic regimen in heart, lung, and heart-lung transplant recipients. J Cardiovasc Nurs. 2005;20(5 Suppl):S88–98. doi: 10.1097/00005082-200509001-00010. [DOI] [PubMed] [Google Scholar]
- 7.Denhaerynck K, Dobbels F, Cleemput I, Desmyttere A, Schäfer-Keller P, Schaub S, et al. Prevalence, consequences, and determinants of nonadherence in adult renal transplant patients: a literature review. Transpl Int. 2005;18(10):1121–1133. doi: 10.1111/j.1432-2277.2005.00176.x. [DOI] [PubMed] [Google Scholar]
- 8.Fenwick EK, Man REK, Gan ATL, Aravindhan A, Tey CS, Soon HJT, et al. Validation of a new diabetic retinopathy knowledge and attitudes questionnaire in people with diabetic retinopathy and diabetic macular edema. Transl Vis Sci Technol. 2020;9(10):32. doi: 10.1167/tvst.9.10.32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Qi JY, Zhai G, Wang Y, Liang YB, Li D, Wen L, et al. Assessment of knowledge, attitude, and practice regarding diabetic retinopathy in an urban population in Northeast China. Front Public Health. 2022;10:808988. doi: 10.3389/fpubh.2022.808988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wang L, Abualfoul M, Oduor H, Acharya P, Cui M, Murray A, et al. A cross-sectional study of knowledge, attitude, and practice toward COVID-19 in solid organ transplant recipients at a transplant center in the United States. Front Public Health. 2022;10:880774. doi: 10.3389/fpubh.2022.880774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ma H, Hu M, Wan J. Kidney transplant-related knowledge and influencing factors in Chinese kidney transplant candidates and recipients: a cross-sectional study. Front Public Health. 2023;11:1027715. doi: 10.3389/fpubh.2023.1027715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Çetin Ç, Cebeci F. Effects of web-based educational intervention on self-management in kidney recipients. Exp Clin Transplant. 2018;16 Suppl 1(Suppl 1):117–118. doi: 10.6002/ect.TOND-TDTD2017.P9. [DOI] [PubMed] [Google Scholar]
- 13.Chan M, Patwardhan A, Ryan C, Trevillian P, Chadban S, Westgarth F, et al. Evidence-based guidelines for the nutritional management of adult kidney transplant recipients. J Renal Nutr. 2011;21(1):47–51. doi: 10.1053/j.jrn.2010.10.021. [DOI] [PubMed] [Google Scholar]
- 14.Ranahan M, Von Visger J, Kayler LK. Describing barriers and facilitators for medication adherence and self-management among kidney transplant recipients using the information-motivation-behavioral skills model. Clin Transplant. 2020;34(6):e13862. doi: 10.1111/ctr.13862. [DOI] [PubMed] [Google Scholar]
- 15.Zhang W, Zeng L, Li J, Deng X, Jin M, Chen Z, et al. Construction and reliability and validity tests of the dietary self-management ability scale for kidney transplant recipients. Ann Palliat Med. 2020;9(2):352–358. doi: 10.21037/apm.2020.03.07. [DOI] [PubMed] [Google Scholar]
- 16.Fu YX. Standardized follow-up after kidney transplantation (2019 edition) Organ Transplant. 2019;10(06):667–671. [Google Scholar]
- 17.Wu JY, Lei WH. Expert consensus on perioperative accelerated recovery management of kidney transplantation in China (2018 edition) Chin J Transplant (Electronic Edition) 2018;12(04):151–156. [Google Scholar]
- 18.Bress AP, Bellows BK, King JB, Hess R, Beddhu S, Zhang Z, et al. Cost-effectiveness of intensive versus standard blood-pressure control. N Engl J Med. 2017;377(8):745–755. doi: 10.1056/NEJMsa1616035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Berlowitz DR, Foy CG, Kazis LE, Bolin LP, Conroy MB, Fitzpatrick P, et al. Effect of intensive blood-pressure treatment on patient-reported outcomes. N Engl J Med. 2017;377(8):733–744. doi: 10.1056/NEJMoa1611179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Morisky DE, Ang A, Krousel-Wood M, Ward HJ. Predictive validity of a medication adherence measure in an outpatient setting. J Clin Hypertens (Greenwich) 2008;10(5):348–354. doi: 10.1111/j.1751-7176.2008.07572.x. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 21.Jaffar A, Mohd-Sidik S, Nien FC, Fu GQ, Talib NH. Urinary incontinence and its association with pelvic floor muscle exercise among pregnant women attending a primary care clinic in Selangor, Malaysia. PLoS One. 2020;15(7):e0236140. doi: 10.1371/journal.pone.0236140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Usman HB, AlSahafi A, Abdulrashid O, Mandoura N, Al Sharif K, Ibrahim A, et al. Effect of health education on dengue fever: a comparison of knowledge, attitude, and practices in public and private high school children of Jeddah. Cureus. 2018;10(12):e3809. doi: 10.7759/cureus.3809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Baek S, Lee O. Developing Korean children's physical activity health literacy: Literate, Empowered, Active, Doer program (LEAD) Int J Qual Stud Health Well Being. 2019;14(1):1648940. doi: 10.1080/17482631.2019.1648940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ligita T, Wicking K, Francis K, Harvey N, Nurjannah I. How people living with diabetes in Indonesia learn about their disease: a grounded theory study. PLoS One. 2019;14(2):e0212019. doi: 10.1371/journal.pone.0212019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Liu J, Li Y. The visual movement analysis of physical education teaching considering the generalized hough transform model. Comput Intell Neurosci. 2022;2022:3675319. doi: 10.1155/2022/3675319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Artzi-Medvedik R, Kob R, Fabbietti P, Lattanzio F, Corsonello A, Melzer Y, et al. Impaired kidney function is associated with lower quality of life among community-dwelling older adults: the screening for CKD among older people across Europe (SCOPE) study. BMC Geriatr. 2020;20(Suppl 1):340. doi: 10.1186/s12877-020-01697-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zhang S, Zhang Y, Zhang X, Luo C, Cao Y, Ji D, et al. Nitrative stress-related autophagic insufficiency participates in hyperhomocysteinemia-induced renal aging. Oxid Med Cell Longev. 2020;2020:4252047. doi: 10.1155/2020/4252047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Shahgholian N, Yousefi H. The lived experiences of patients undergoing hemodialysis with the concept of care: a phenomenological study. BMC Nephrol. 2018;19(1):338. doi: 10.1186/s12882-018-1138-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Xu H, Wang H, Yuan C, Zhai Q, Tian X, Wu L, et al. Identifying diseases that cause psychological trauma and social avoidance by GCN-Xgboost. BMC Bioinformatics. 2020;21(Suppl 16):504. doi: 10.1186/s12859-020-03847-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Li CC, Zhang ZW. Effect of precision health education on compliance behavior after extracorporeal shock wave lithotripsy. Comput Math Methods Med. 2022;2022:3306036. doi: 10.1155/2022/3306036. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 31.Lee W, Park JO, Hong SO, Kim Y. Bicycle injury prevention education using 360° virtual reality experiences of accidents and computer-based activity. Children (Basel) 2022;9(11):1623. doi: 10.3390/children9111623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mohan V, Joshi S, Mithal A, Kesavadev J, Unnikrishnan AG, Saboo B, et al. Expert consensus recommendations on time in range for monitoring glucose levels in people with diabetes: an Indian perspective. Diabetes Ther. 2023;14(2):237–249. doi: 10.1007/s13300-022-01355-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Broe MP, Galvin R, Keenan LG, Power RE. Laparoscopic and hand-assisted laparoscopic donor nephrectomy: a systematic review and meta-analysis. Arab J Urol. 2018;16(3):322–334. doi: 10.1016/j.aju.2018.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Shajari A, Ashrafi MM, Shajari H, Derakhshan A. Graft and patient survival rate among Iranian pediatric recipients of kidney transplantation: a systematic review and meta-analysis. Iran J Public Health. 2022;51(6):1232–1244. doi: 10.18502/ijph.v51i6.9666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Han A, Ahn S, Min SK, Ha J, Kim YS, Ahn C, et al. Value of perioperative genitourinary screening culture and colonization status in predicting early urinary tract infection after renal transplantation. PLoS One. 2018;13(4):e0196115. doi: 10.1371/journal.pone.0196115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zachciał J, Uchmanowicz I, Krajewska M, Banasik M. Adherence to immunosuppressive therapies after kidney transplantation from a biopsychosocial perspective: a cross-sectional study. J Clin Med. 2022;11(5):1381. doi: 10.3390/jcm11051381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ly HHV, Le NNM, Ha MTT, Diep HG, Lam AN, Nguyen TTT, et al. Medication adherence in Vietnamese patients with cardiovascular and endocrine-metabolic diseases. Healthcare (Basel) 2022;10(9):1734. doi: 10.3390/healthcare10091734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.King C, Collins D, Patten A, Nicolaidis C, Englander H. Trust in hospital physicians among patients with substance use disorder referred to an addiction consult service: a mixed-methods study. J Addict Med. 2022;16(1):41–48. doi: 10.1097/ADM.0000000000000819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sahin C, Courtney KL, Naylor PJ, E Rhodes R. Tailored mobile text messaging interventions targeting type 2 diabetes self-management: a systematic review and a meta-analysis. Digit Health. 2019;5:2055207619845279. doi: 10.1177/2055207619845279. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data generated or analysed during this study are included in this published article and its supplementary information files.