Acupuncture is the stimulation of special points on the body, usually by the insertion of fine needles. Originating in the Far East about 2000 years ago, it has made various appearances in the history of European and north American medicine. William Osler, for example, used acupuncture therapeutically in the 19th century. Acupuncture’s recent popularity in the West dates from the 1970s, when President Nixon visited China.
Background
In its original form acupuncture was based on the principles of traditional Chinese medicine. According to these, the workings of the human body are controlled by a vital force or energy called “Qi” (pronounced “chee”), which circulates between the organs along channels called meridians.
There are 12 main meridians, and these correspond to 12 major functions or “organs” of the body. Although they have the same names (such as liver, kidney, heart, etc), Chinese and Western concepts of the organs correlate only very loosely. Qi energy must flow in the correct strength and quality through each of these meridians and organs for health to be maintained. The acupuncture points are located along the meridians and provide one means of altering the flow of Qi.
Although the details of practice may differ between individual schools, all traditional acupuncture theory is based in the Daoist concept of yin and yang. Illness is seen in terms of excesses or deficiencies in various exogenous and endogenous pathogenic factors, and treatment is aimed at restoring balance. Traditional diagnoses are esoteric, such as “kidney-yang deficiency, water overflowing” or “damp heat in the bladder.”
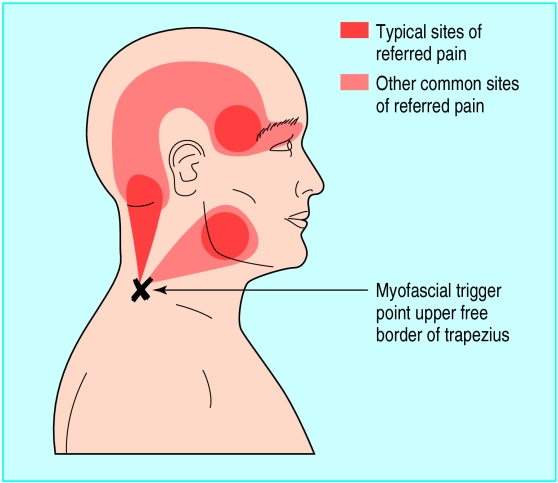
Many of the conventional health professionals who practise acupuncture have dispensed with such concepts. Acupuncture points are seen to correspond to physiological and anatomical features such as peripheral nerve junctions, and diagnosis is made in purely conventional terms. An important concept used by such acupuncturists is that of the “trigger point.” This is an area of increased sensitivity within a muscle which is said to cause a characteristic pattern of referred pain in a related segment of the body. An example might be tender areas in the muscles of the neck and shoulder which relate to various patterns of headache.
It is often implied that a clear and firm distinction exists between traditional and Western acupuncture, but the two approaches overlap considerably. Moreover, traditional acupuncture is not a single, historically stable therapy. There are many different schools—for example, Japanese practitioners differ from their Chinese counterparts by using mainly shallow needle insertion.
Acupressure involves firm manual pressure on selected acupuncture points. Shiatsu, a modified form of acupressure, was systematised as part of traditional Japanese medicine.
How does acupuncture work?
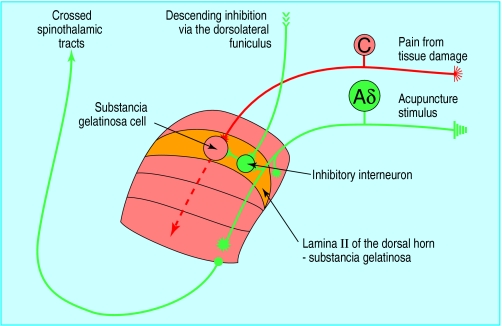
The effects of acupuncture, particularly on pain, are at least partially explicable within a conventional physiological model. Acupuncture is known to stimulate A delta fibres entering the dorsal horn of the spinal cord. These mediate segmental inhibition of pain impulses carried in the slower, unmyelinated C fibres and, through connections in the midbrain, enhance descending inhibition of C fibre pain impulses at other levels of the spinal cord. This helps explain why acupuncture needles in one part of the body can affect pain sensation in another region. Acupuncture is also known to stimulate release of endogenous opioids and other neurotransmitters such as serotonin. This is likely to be another mechanism for acupuncture’s effects, such as in acute pain and in substance misuse.
However, certain aspects of traditional acupuncture, which have some empirical support, resist conventional explanation. In one unreplicated study, for example, blinded assessment of the tenderness of points on the ear had high agreement with the true location of chronic pain in distant parts of the body. Changes in the electrical conductivity of acupuncture points associated with a particular organ have also been recorded in patients with corresponding conventional diseases. There are no known anatomical or physiological explanations for these observations.
What happens during a treatment?
Traditional acupuncturists supplement a detailed, multisystem case history with observations that are said to give information about the patient’s state of health. These include examination of the shape, coating, and colour of the tongue; the colour of the face; and the strength, rhythm, and quality of the pulse. Both Western and traditional practitioners may palpate to identify points at which pressure causes tenderness or pain.
Typically, between four and 10 points are needled during an acupuncture session. The needles are usually left in place for 10-30 minutes, although some practitioners needle for only a few seconds or minutes. Needles may be stimulated by manual twirling or a small electrical current. Lasers are sometimes used to stimulate acupuncture points instead of needles. Acupuncture needles are extremely fine and do not hurt in the same way as, say, an injection. Patients may even be unaware that a needle has been inserted. However, some acupuncturists attempt to produce a sensation called “de Qi”—a sense of heaviness, soreness, or numbness at the point of needling. This is said to be a sign that an acupuncture point has been correctly stimulated. Many patients say that they find acupuncture a relaxing or sedating experience.
Traditional acupuncturists may use various adjunctive therapies, including moxibustion (the burning of a herb just above the surface of the skin), massage, cupping, herbal preparations, exercises, and dietary modification.
A typical course of acupuncture treatment for a chronic condition would be six to 12 sessions over a three month period. This might be followed by “top up” treatments every two to six months.
Therapeutic scope
Acupuncture was developed as a relatively global system of medicine. Some current textbooks refer to treating conditions as varied as diarrhoea, the common cold, and tinnitus. As practised in Europe and north America, acupuncture is primarily a treatment for benign, chronic disease and for musculoskeletal injury. The most common presenting complaints found in surveys of acupuncture practice include back pain, arthritis, headache, asthma, hay fever, anxiety, fatigue, menstrual disorders, and digestive disorders. Acupuncture is also used in drug and alcohol rehabilitation, particularly in the United States.
Research evidence
There is good research evidence that acupuncture has effects greater than placebo. Randomised trials have found that true acupuncture is more effective in relieving pain than a “sham” technique, such as inserting needles away from true points. Of the numerous studies on nausea, a condition that readily lends itself to placebo controlled trials, almost all show that stimulating true acupuncture points is more effective that stimulating false points. Studies showing that acupuncture can affect anaesthetised animals provides further evidence that its effects probably cannot be explained purely in psychological terms.
Key studies of efficacy
Systematic reviews
Vickers AJ. Can acupuncture have specific effects on health? A systematic review of acupuncture antiemesis trials. J R Soc Med 1996;89:303-11
White AR, Rampes H. Acupuncture for smoking cessation. In: Cochrane Collaboration. The Cochrane Library. Issue 2. Oxford: Update Software, 1998
Randomised controlled trials
Johansson K, Lindgren I, Widner H, Wiklund I, Johansson BB. Can sensory stimulation improve the functional outcome in stroke patients? Neurology 1993;43:2189-92
Vincent CA. A controlled trial of the treatment of migraine by acupuncture. Clin J Pain 1989;5:305-12
It is less clear whether acupuncture has clinically important benefits in the conditions for which it is typically used. Much of the research evidence comes from hospital based studies of acute conditions such as postoperative pain rather than studies of chronic conditions in primary care. Moreover, most trials have had small numbers of patients and only short term follow up. Overall, evidence from several randomised controlled trials supports the use of acupuncture in pain conditions, particularly migraine, headache, and postoperative pain. Such trials also provide evidence of an effect of acupuncture in substance misuse, nausea, and stroke. Trials of acupuncture in asthma and hay fever have produced conflicting results. Systematic reviews and randomised controlled trials suggest that acupuncture is probably not of benefit for stopping smoking, tinnitus, or obesity. Data on fatigue, digestive disorders, and anxiety are insufficient.
There is little reliable information on the relative effectiveness of the various Western and traditional forms of acupuncture.
Safety of acupuncture
As with all complementary medicine, the absence of a formal system for reporting adverse effects means that acupuncture’s safety is difficult to assess. However, it seems to be a relatively safe form of treatment with a low incidence of serious adverse events. An extensive worldwide literature search identified only 193 adverse events (including relatively minor events such as bruising and dizziness) over 15 years. The more serious events were usually related to poor practice—for example, cases of hepatitis B infection typically involved bad hygiene and unregistered practitioners.
A prospective study of over 55 000 acupuncture treatments given in a college for medically trained acupuncturists confirms that acupuncture is probably safe in qualified hands. Only 63, mostly minor, adverse events were identified, and no cases of serious adverse events such as pneumothorax, infection, or spinal lesions were reported, although these have been described in the literature.
Adverse events related to acupuncture
| Reported adverse events | No of cases* |
|---|---|
| Forgotten needles (all later retrieved without sequelae) | 16 |
| Transient hypotension | 13 |
| Burn injury (such as caused by moxibustion) | 6 |
| Ecchymosis with pain | 6 |
| Ecchymosis without pain | 5 |
| Malaise | 5 |
| Minor haemorrhage | 3 |
| Aggravation of complaint | 3 |
| Suspected contact dermatitis | 3 |
| Pain in the puncture region | 2 |
| Fall from bed | 1 |
From Yamashita H, Tsukayama H, Tanno Y, Nishijo K. Adverse events related to acupuncture [letter]. JAMA 1998;280:1563-4
*Total number of treatments was 55 291, from November 1992 to October 1997
Indwelling “press” needles are commonly used in the treatment of addiction and should be used with care. They have been associated with infections, such as perichondritis. Systemic infection seems to be very uncommon, but acupuncture should probably be avoided in patients with valvular heart defects. Deep needling is contraindicated in patients with bleeding disorders or taking anticoagulant drugs.
Practitioners
Acupuncturists without a background in conventional health care tend to work in private practice and treat a wide variety of conditions. About 2000 doctors and physiotherapists practise acupuncture, but they rarely specialise in it and generally use it as an adjunctive treatment when appropriate. Most offer treatment mainly directed at musculoskeletal and other painful conditions and are usually based in pain clinics or in general practice.
Organisations concerned with regulation and training in acupuncture
British Medical Acupuncture Society
For doctors only
Newton House, Whitley, Warrington WA4 4JA. Tel: 01925 730727. Fax: 01925 730492. Email: bmasadmin@aol.com. URL: www.medical-acupuncture.co.uk
British Acupuncture Council
Park House, 206-208 Latimer Road, London W10 6RE. Tel: 0181 964 0222. Fax: 0181 964 0333. Email: info@acupuncture.org.uk. URL: www.acupuncture.org.uk
Acupuncture Association of Chartered Physiotherapists
Chartered Society of Physiotherapists, 14 Bedford Row, London WC1R 4ED. Tel: 0171 242 1941
Training
Professional acupuncturists train for up to 3-4 years full time and may acquire university degrees on completion of their training. Some complete further training in the principles and practice of Chinese herbalism. All accredited acupuncture training courses include conventional anatomy, physiology, pathology, and diagnosis. Research and audit skills are also taught.
Medical acupuncturists generally have fewer training hours in acupuncture techniques—a course of several weekends in which they learn a small range of simple techniques is typical. Other conventional healthcare disciplines run courses for their own members, ranging from basic introductions to two year training in advanced acupuncture.
Regulation
Professional acupuncturists have a single regulatory body, the British Acupuncture Council (BAcC), with about 1500 members. The council aims to achieve statutory regulation, although no final decisions have been made. All members have undergone a training independently accredited by the British Acupuncture Accreditation Board. Physiotherapists are regulated by the Acupuncture Association of Chartered Physiotherapists (AACP). Although many doctors practise some basic acupuncture without an official qualification, the British Medical Acupuncture Society offers a Certificate of Basic Competence and a Diploma of Medical Acupuncture for appropriately trained doctors.
Further reading
Filshie J, White A. Medical acupuncture. Edinburgh: Churchill Livingstone, 1997
Maciocia G. The foundations of Chinese medicine. Edinburgh: Churchill Livingstone, 1989
Kaptchuk T. Chinese medicine: the web that has no weaver. London: Rider, 1983
Acupuncture Resource Research Centre website. www.demon.co.uk/acupuncture/arrc.html
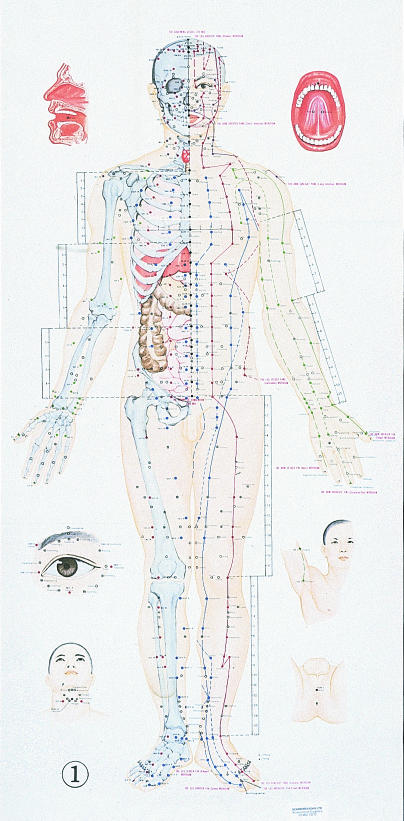
Figure.
Acupuncture meridians run superficially and longitudinally. Both traditional and Western acupuncturists identify acupuncture points by their location on the meridians—for example, gall bladder 30 or large intestine 4
Figure.
Trigger points, and their characteristic patterns of referred pain, can be treated by direct needling at the trigger point. This concept is also used in musculoskeletal medicine, with trigger points being treated by manipulative techniques
Figure.
The neuronal connections which are thought to mediate the effects of acupuncture on pain
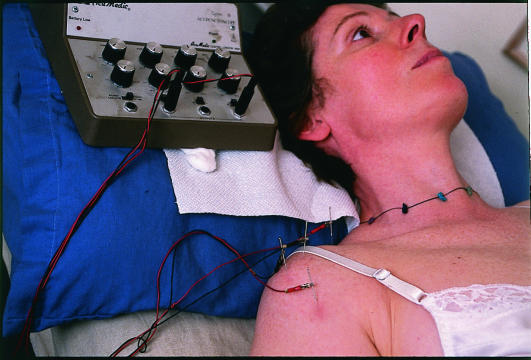
Figure.
A typical traditional acupuncture session includes a physical assessment of yin-yang energy status with methods such as pulse and tongue diagnosis
Figure.
Using electricity to stimulate acupuncture points is thought to augment the therapeutic effect of needling and is used particularly in treating chronic pain
Figure.
On balance, research evidence supports the use of acupuncture in treating substance misuse. Auricular acupuncture is often used for this purpose
Acknowledgments
The chart of acupuncture points is reproduced with permission of Medicine and Health Publishing, Hong Kong, and was supplied by Scarboroughs. The diagrams showing trigger points and neuronal connections mediating acupuncture’s effects were supplied by Mike Cummings of the British Medical Acupuncture Society. The picture of tongue examination is reproduced with permission of Mark de Fraye/Science Photo Library. The picture of auricular acupuncture is reproduced with permission of AP/Shane Young. The picture of electrically stimulated acupuncture is reproduced with permission of BMJ/Ulrike Preuss.
Footnotes
The ABC of complementary medicine is edited and written by Catherine Zollman and Andrew Vickers. Catherine Zollman is a general practitioner in Bristol, and Andrew Vickers will shortly take up a post at Memorial Sloan-Kettering Cancer Center, New York. At the time of writing, both worked for the Research Council for Complementary Medicine, London. The series will be published as a book in Spring 2000.