Abstract
Objective:
Do-Not-Attempt-Resuscitation orders originated in the early 1960s with the establishment of advanced cardiopulmonary resuscitation. These orders aim to limit therapeutic efforts in cases where it may be futile. The decision not to resuscitate a patient is a process that involves a series of ethical, legal, and clinical considerations. Still, it also requires a process in which priority is given to the patients and their autonomy. The objective of this study was to describe the knowledge and attitudes of physicians working in Chile toward Do-Not-Attempt-Resuscitation orders.
Methods:
A cross-sectional study was conducted, in which a digital questionnaire was sent to physicians from different regions of Chile. Quantitative variables were analyzed using measures of central tendency and dispersion (e.g., median and interquartile range), while qualitative variables were evaluated using frequencies and percentages.
Results:
Four hundred and thirty-one physicians completed the survey. 85.4% were familiar with the ethical and legal guidelines for cardiopulmonary resuscitation and the rights and duties of the patient. 39.2% believed that patients should have the final decision Do-Not-Attempt-Resuscitation orders, especially if they themselves requested not to be resuscitated. 87.7% mentioned that the Do-Not-Attempt-Resuscitation orders should be reassessed if the patient’s prognosis improves. In addition, it was found that the decision not to resuscitate was not always discussed with the patient or their family.
Conclusions:
The study revealed an ethical conflict regarding Do-Not-Attempt-Resuscitation orders and their management by Chilean physicians. Therefore, it is necessary to create recommendations and provide training to guide professionals in this process, which should also involve patients and their families.
Keywords: Terminal care, hospice care, resuscitation orders, physicians, Chile
Introduction
Do-Not-Attempt-Resuscitation (DNAR) orders are specific medical instructions that indicate that cardiopulmonary resuscitation (CPR) should not be performed if a patient stops breathing or their heart stops beating.1,2 These orders are established in writing and are usually written by a doctor. DNAR orders are ideally created before an emergency occurs and allow patients to decide whether or not they wish to receive CPR in the event of an emergency situation.3–5 However, it is essential to note that DNAR orders refer specifically to CPR and do not include instructions on other medical treatments, such as palliative care.6–8
In Chile, for example, the 2012 Law 20584 (also known as the Law of Duties and Rights of Patients) was enacted in Chile on April 24, 2012. This law aims to regulate the rights and duties of people about actions linked to their health care and recognizes that patients have the right to information and to refuse treatment as long as it does not lead to the artificial acceleration of death. This refusal can be verbal but must be in writing for surgeries and invasive procedures. Also, in the case of a terminal illness, individuals have the right to grant or deny their will to undergo procedures that artificially prolong life. 9
When comparing with other countries in the South American region that share similar customs and culture, it should be noted that in several of these countries, end-of-life care is regulated, and, in addition, Colombia has legislation on euthanasia.
In Colombia, end-of-life care is regulated through Law 1733 of 2014, which proposes patients’ rights at the end of life. Also, ruling C-233 of 2014 indicates the value of advance directives. Resolutions 1216 of 2015 and 2565 of 2018 contemplate the right of patients to know the advance directive document and its content. Resolution 229 of 2020 also indicates the Charter of Rights and Duties guidelines, where the fundamental right to die with dignity is established.10,11
In the case of Cuba, the limitation of therapeutic effort is legally based on the constitutional postulates regarding the protection of human dignity. Furthermore, it conforms to the Cuban health system’s ethical recommendations; therefore, limiting therapeutic effort is considered good clinical practice. For Cuba, euthanasia and medically assisted suicide are not modalities of dignified death but rather illicit actions that compromise the right to life. Nor are they forms of limitation of therapeutic effort. 12
In Argentina, a qualitative study in which 31 oncology and palliative care professionals were interviewed about planning end-of-life care for patients found that more communication tools must be needed to address these types of conversations with patients. It was also evident that providing information about the diagnosis and prognosis to patients and family members is difficult. Health professionals are reluctant to openly discuss these issues with patients, especially those with advanced oncological diseases, evidencing practices of concealment or incomplete disclosure of information, which limits the possibility of patients being informed about their condition and deciding according to their preferences. Also, the legal requirements for the preparation of advance directive documents (which, according to Argentine legislation, must be countersigned by a notary public) act as structural barriers. 13
The decision not to resuscitate a patient is a process that involves a series of ethical, legal, and clinical considerations. Still, it also requires a process in which priority is given to the patients and their autonomy. Given the above, the objective of this study was to describe the knowledge and attitudes of physicians working in Chile toward DNAR orders.
Methods
This study was prepared following the STROBE (Strengthening the reporting of observational studies in epidemiology) recommendations for writing observational studies papers.
Study design
This observational, descriptive, cross-sectional study sought to describe the knowledge and attitudes of doctors working in Chile toward DNAR orders.
Setting
The questionnaire was distributed in July 2022, and a period of 6 months, until December 2022, was designated to receive responses. The questionnaire was presented at two virtual conferences on bioethics and the QR code was available for access. Publications were made on social networks (Instagram, Twitter, and LinkedIn), and medical groups on Facebook invited people to participate in the study. Different medical associations were also asked to disseminate the questionnaire.
Participants
Physicians who graduated from national or foreign universities authorized to practice in Chile were selected. It was also considered that they worked in different health institutions and agreed to participate. Physicians who performed mainly administrative tasks (without healthcare contact during the last 2 years) or worked only in telemedicine were excluded.
Variables
Variables for participant characterization, such as age, gender, professional category, medical specialty, years of experience, and region of origin, were included. Other variables inquired about knowledge regarding guidelines for resuscitation (Guidelines for CPR published in 2020 by the American Heart Association for CPR and emergency cardiovascular care). 14 The patient’s rights and duties law “Law 20-584”—“Article 14.- Every person has the right to grant or deny their will to undergo any procedure or treatment linked to their health care” and “Article 16- The person who is informed that their health condition is terminal, has the right to grant or deny their will to undergo any treatment that has the effect of artificially prolonging their life, without prejudice to maintaining ordinary support measures.” 9 And finally, awareness of the World Medical Association’s (WMA) declaration on euthanasia and assisted suicide (in which the WMA reiterates its strong commitment to the principles of medical ethics and that the utmost respect for human life must be maintained. They oppose euthanasia and physician-assisted suicide). 15 Variables also covered various scenarios in which discussions about not resuscitating a patient had occurred.
Data sources
Data collection was carried out through an online questionnaire named “Knowledge and Attitudes of Physicians toward DNAR orders.” This questionnaire was taken from Bremer et al. 16 who carried out an adaptation and validation of previous questionnaires.17–19 The questionnaire is divided into four sections and has 35 questions. The first section contains general questions to characterize the population under study, such as age, years of work experience, city where they work, etc. Section two contains questions about participants’ experience with DNAR decisions and information about them to the patient. The third part contains questions about the experience of DNAR decisions and information about them to patients’ relatives. Finally, the fourth part contains questions about opinions about an advance decision to refrain from attempting resuscitation in case of sudden cardiac arrest. The entire questionnaire and its sections can be found in Annex 1.
A review of the questionnaire was carried out by three experts in the construction of questions to ensure that there were no common errors, such as confusing or ambiguous questions, guaranteeing content validity. Then, a pilot test was carried out with 22 participants (5.1% of the calculated sample size).
Bias
This study may have a selection bias as a probabilistic sampling with a classic random method was not conducted. Nonetheless, efforts were made to have a sample size representative of the study population.
In addition, classification bias refers to an error in the classification of variables, which results in an overestimation or underestimation of the true value and can affect the validity and interpretation of the study results. To reduce classification bias in this study, clear inclusion criteria were set to minimize subjectivity and error in classification. A previously validated instrument was also used to reduce classification bias. In addition, using an online questionnaire that automatically generates a database reduces human error when classifying responses.
Confounding bias can occur when the presence of a third so-called confounding variable can partially or fully explain an observed association between an exposure variable and an outcome variable. This confounding variable may distort the magnitude or direction of the association between the exposure and the outcome, generating biased results. Different methods, such as statistical adjustment or group matching, can be used to control for confounding bias. The goal is to minimize the influence of confounding variables and obtain a more precise estimate of the true association between the exposure and the outcome of interest. In this case, an adjustment was made for gender to reduce the appearance of this bias.
Study size
The sample was selected by intention, but a sample size calculation was performed, taking into account the known number of health professionals registered with the Ministry of Health of Chile (53,490). Thus, the representative target sample size was 384 physicians.
The formula to calculate the sample size of a proportion was used. 20
where,
Z = 1.962 (since the security is 95%)
p = expected proportion. Starting from the fact that the population under study are doctors who work in Chile, p represents the proportion (prevalence) of those physicians whose attitudes toward DNARs are known. The value of that proportion is needed to calculate the sample size. This value is obtained from previous work in the population. If it is not known what the value of this proportion may be (as in this case), and knowing that the value must be between 0 and 1, the average value must be considered, that is, 0.5. The explanation is that in the mathematical model, the ratio of p versus q(1–p), the maximum value of this product is reached when p is equal to 0.5.
q = 1–p (in this case, 1–0.5 = 0.5)
d = precision (in this case, we want 5% = 0.05)
Then, substituting the data into the formula
Quantitative variables
Whether the variables followed the normal distribution was evaluated using the Kolmogorov–Smirnov test. 21 Then, measures of central tendency, such as the mean or median, were calculated depending on whether the variables were symmetric or asymmetric. Measures of dispersion, such as the standard deviation and the interquartile range, were also calculated.
Statistical analysis
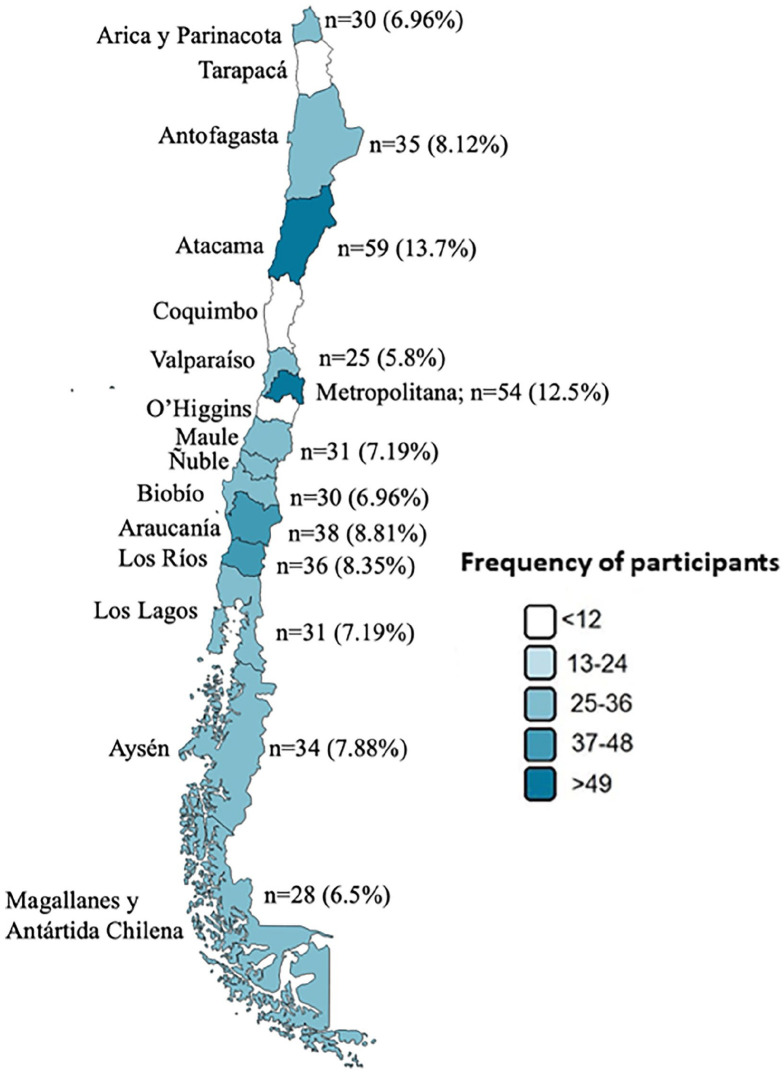
The data were analyzed with IBM-SPSS statistical software (IBM Corp. Released 2023. IBM SPSS Statistics for Windows, Version 29.0.2.0 Armonk, NY: IBM Corp). Nominal variables were coded using numbers, and an analysis was performed using frequencies and percentages. A stratification by gender was also carried out to observe the differences, both in the characterization variables and in the presentation variables of knowledge and attitudes toward DNAR orders. Tables were also created to summarize the analyzed data, and a georeferencing map was generated to illustrate the participants’ regions of origin, because Chile is a long and narrow country that stretches along the western edge of South America. It spans a wide range of latitudes, resulting in diverse landscapes and climates.
This study employed a data collection format that did not request personal identification data, and questionnaires were anonymized. Therefore, it was considered compliant with the guidelines of Council for International Organizations of Medical Sciences (CIOMS), 22 the Helsinki Declaration, and data protection laws, posing no direct risk to participants other than the potential impact of learning the obtained results. Written informed consent was obtained from participants, and the study was reviewed and approved by the Universidad Internacional de la Rioja Ethics Committee with registration number “2023-2612.”
Results
Taking into account the participation of doctors in the two bioethics conferences and the reach on social networks (views, likes, reposts), it was calculated that the questionnaire had a reach of approximately 5000 doctors and taking into account that the questionnaire was answered by 431 subjects, an average response of 14.4% was estimated. However, the calculated sample size was met and exceeded (the representative target sample size was 384 physicians). The median age was 38 years (IQR 17). Regarding gender, 52.7% (n = 227) were women, 45.9% (n = 198) were men, and the remaining 1.4% (n = 6) identified as another gender. In the professional category, 81.9% (n = 353) were specialist physicians, and 18.1% (n = 78) were general physicians. Within the specialties, 18.8% (n = 81) were emergency physicians, 13.7% (n = 59) were intensive care physicians, 13.2% (n = 57) were internal medicine physicians, and the remaining professionals belonged to specialties such as surgery, family medicine, anesthesiology, among others. The median years of experience as a physician were 11 years (IQR 14) (Table 1).
Table 1.
Baseline characteristics of the study population.
| Variables | Female | Male | Other gender | |||
|---|---|---|---|---|---|---|
| Median | IQR | Median | IQR | Median | IQR | |
| Age | 38 | 14 | 40 | 23 | 26 | 5 |
| Years of professional experience | 8 | 10 | 15 | 14 | 4 | 2 |
| Frequency | % | Frequency | % | Frequency | % | |
| Professional category | ||||||
| Physicians with specialty (Medical specialist) | 180 | 79.3 | 173 | 87.4 | 0 | 0 |
| General practitioners (before specialist residency) | 47 | 20.7 | 25 | 12.6 | 6 | 100 |
| Total | 227 | 100 | 198 | 100 | 6 | 100 |
| Medical specialties | ||||||
| Emergencies (Medical specialist) | 50 | 22 | 31 | 15.7 | 0 | 0 |
| General medicine (before specialist residency) | 47 | 20.7 | 25 | 12.6 | 6 | 100 |
| Internal medicine (Medical specialist) | 41 | 18.1 | 16 | 8.1 | 0 | 0 |
| Intensive care (Medical specialist) | 18 | 7.9 | 41 | 20.7 | 0 | 0 |
| Epidemiology (Medical specialist) | 13 | 5.7 | 0 | 0 | 0 | 0 |
| Anesthesiology (Medical specialist) | 11 | 4.8 | 7 | 3.5 | 0 | 0 |
| Gynecology and obstetrics (Medical specialist) | 11 | 4.8 | 0 | 0 | 0 | 0 |
| Family medicine (Medical specialist) | 10 | 4.4 | 11 | 5.6 | 0 | 0 |
| Psychiatry (Medical specialist) | 10 | 4.4 | 0 | 0 | 0 | 0 |
| Physical medicine and rehabilitation (Medical specialist) | 9 | 4.0 | 0 | 0 | 0 | 0 |
| Infectious diseases (Medical specialist) | 7 | 3.1 | 1 | 0.5 | 0 | 0 |
| Surgery (Medical specialist) | 0 | 0 | 21 | 10.6 | 0 | 0 |
| Ophthalmology (Medical specialist) | 0 | 0 | 13 | 6.6 | 0 | 0 |
| Neurology (Medical specialist) | 0 | 0 | 11 | 5.6 | 0 | 0 |
| Oncology (Medical specialist) | 0 | 0 | 11 | 5.6 | 0 | 0 |
| Pediatrics (Medical specialist) | 0 | 0 | 10 | 5.1 | 0 | 0 |
| Total | 227 | 100 | 198 | 100 | 6 | 100 |
Participants were asked about the region where they worked, and it was found that 13.7% (n = 59) worked in Atacama, 12.5% (n = 54) in the metropolitan region; the regions of La Aracucanía ranked third, with 8.81% (n = 38) of participants, and the remaining percentage was distributed among other regions of the country (Figure 1).
Figure 1.
Distribution of participants according to region of origin. Participation representation is shown in colors according to ranges calculated following the Sturges Rule.
Source: Figure created by the authors.
They were asked if they were familiar with the guidelines for CPR, with 85.4% (n = 368) stating that they were aware of them. The patient’s rights and duties law in force in Chile, specifically Article 14, regarding the expression of informed consent, was declared known by 97% of participants. Article 16, which mentions the right to grant or deny consent to any treatment that artificially prolongs life, was declared known by 97.5% (n = 420) of participants. In addition, 85.8% (n = 370) mentioned being familiar with the World Medical Association’s (WMA) declaration on euthanasia and assisted suicide. 46.2% (n = 199) responded that neither the patient’s rights and duties law nor the AMA declaration had been socialized in their workplace.
Seventy-seven percent (n = 332) of participants expressed that they had participated in a discussion leading to a decision not to resuscitate a patient at some point, and 76.3% (n = 329) had been the professional making the decision. Physicians were asked about the number of patients per 100 treated with a valid DNAR order. The median found was five patients, with an IQR of 18. Furthermore, the median number of patients per 100 treated with a DNAR order who knew this information was five individuals, with an IQR of 20.
Based on the latest discussion about a specific DNAR decision that the physicians participated in, when asked if the decision DNAR was discussed with the patient, 38.3% (n = 165) stated that it was. The prognosis of the disease was explained in 61.5% (n = 265) of cases. In 12.1% (n = 52) of cases, the patient initiated the discussion about the process leading to the decision DNAR, and in 26.2% (n = 113) of cases, the patient himself requested not to be resuscitated.
When the decision DNAR was made without the patient’s involvement, the patient was informed in 26.7% (n = 115) of cases. Therefore, professionals were asked if it was ethically correct not to inform the patient or family about this decision; 70.1% (n = 302) considered this practice inappropriate. Fifty-eight percent (n = 250) responded that, to avoid not discussing the decision with the patient, the discussion about DNAR orders should be initiated well in advance. Also, 80.7% (n = 348) said that the patient’s opinion should be sought, provided they are capable of participating in the conversation (Table 2). In addition, stratification of the questions was carried out by 5-year age periods, finding that doctors between 26 and 30 years old were the ones who answered the most surveys: 26.2% (n = 113), followed by the age range of 36–40 years old 18.1% (n = 78), and so on until reaching the age range with the lowest participation, which was 46–50 years old 3.25% (n = 14). All of the responses stratified by the different age ranges are shown in Table 3.
Table 2.
Physicians’ responses regarding knowledge of ethical and legal guidelines on resuscitation and DNAR orders in patients, stratified by gender. The questions could be answered as yes, no, or uncertain (this last category was set for the participant to mark if they did not remember the situation, there was no clear decision, or the situation was not presented).
| Variables | Female | Male | Other gender | |||
|---|---|---|---|---|---|---|
| Frequency | % | Frequency | % | Frequency | % | |
| Do you understand the ethical and legal guidelines for CPR? | ||||||
| Yes | 188 | 82.8 | 174 | 87.9 | 6 | 100 |
| No | 39 | 17.2 | 24 | 12.1 | 0 | 0 |
| Are you familiar with the patient’s rights and responsibilities act? | ||||||
| Yes | 216 | 95.2 | 198 | 100 | 6 | 100 |
| No | 11 | 4.8 | 0 | 0 | 0 | 0 |
| Do you know the WMA statement on euthanasia and medically assisted suicide? | ||||||
| Yes | 179 | 78.9 | 185 | 93.4 | 6 | 100 |
| No | 48 | 21.1 | 13 | 6.6 | 0 | 0 |
| Have you ever been involved in a discussion that led to a decision DNAR a patient? | ||||||
| Yes | 152 | 67 | 174 | 87.9 | 6 | 100 |
| No | 75 | 33 | 24 | 12.2 | 0 | 0 |
| Have you ever made a decision not to resuscitate a patient? | ||||||
| Yes | 163 | 71.8 | 166 | 83.8 | 0 | 0 |
| No | 64 | 28.2 | 32 | 16.2 | 6 | 100 |
| Was the decision DNAR discussed with the patient? | ||||||
| Yes | 101 | 44.5 | 58 | 29.3 | 6 | 100 |
| No | 40 | 17.6 | 95 | 48 | 0 | 0 |
| Uncertain | 86 | 37.9 | 45 | 22.8 | 0 | 0 |
| Was the prognosis of the disease discussed with the patient? | ||||||
| Yes | 141 | 62.1 | 118 | 59.6 | 6 | 100 |
| No | 22 | 9.7 | 27 | 13.6 | 0 | 0 |
| Uncertain | 64 | 28.2 | 53 | 26.8 | 0 | 0 |
| Was the patient asked about their opinion in the process that led to the decision of DNAR? | ||||||
| Yes | 94 | 41.4 | 60 | 30.3 | 6 | 100 |
| No | 59 | 26 | 98 | 49.5 | 0 | 0 |
| Uncertain | 74 | 32.6 | 40 | 20.2 | 0 | 0 |
| Was it the patient himself who initiated the discussion about DNAR? | ||||||
| Yes | 39 | 17.2 | 13 | 6.6 | 0 | 0 |
| No | 124 | 54.6 | 140 | 70.7 | 4 | 66.7 |
| Uncertain | 64 | 28.2 | 45 | 22.8 | 2 | 33.3 |
| Was it the patient himself who requested not to be resuscitated? | ||||||
| Yes | 76 | 33.5 | 31 | 15.7 | 6 | 100 |
| No | 87 | 38.3 | 130 | 65.7 | 0 | 0 |
| Uncertain | 64 | 28.2 | 37 | 18.7 | 0 | 0 |
| If the decision DNAR was made without patient participation, was the patient informed of the decision once it was made? | ||||||
| Yes | 65 | 28.6 | 45 | 22.7 | 5 | 83.3 |
| No | 64 | 28.2 | 87 | 43.9 | 1 | 16.7 |
| Uncertain | 98 | 43.2 | 66 | 33.4 | 0 | 0 |
| Do you think there are patients who want to be informed that the responsible physician has made a decision DNAR but in practice they do not receive that information? | ||||||
| Yes | 156 | 68.7 | 185 | 93.4 | 6 | 100 |
| No | 43 | 18.9 | 0 | 0 | 0 | 0 |
| Uncertain | 28 | 12.3 | 13 | 6.6 | 0 | 0 |
| Do you think there are patients who are informed that the responsible physician has made a decision DNAR, but those patients did not want to receive that information? | ||||||
| Yes | 124 | 54.6 | 164 | 82.8 | 4 | 66.7 |
| No | 58 | 25.6 | 10 | 5.1 | 0 | 0 |
| Uncertain | 45 | 19.8 | 24 | 12.1 | 2 | 33.3 |
| Total | 227 | 100 | 198 | 100 | 6 | 100 |
Table 3.
Physicians’ responses regarding knowledge of ethical and legal guidelines on resuscitation and DNAR orders in patients, stratified by age ranges (in 5-year periods). The questions could be answered as yes, no, or uncertain (this last category was set for the participant to mark if they did not remember the situation, there was no clear decision, or the situation was not presented).
| Answers | Age in ranges | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| 26–30 | 31–35 | 36–40 | 41–45 | 46–50 | 51–55 | 56–60 | 61–65 | 66–70 | |
| Do you understand the ethical and legal guidelines for CPR? | |||||||||
| Yes | 102 (90.3%) | 59 (89.4%) | 67 (85.9%) | 45 (80.4%) | 14 (100%) | 45 (81.8%) | 11 (45.8%) | 7 (100%) | 18 (100%) |
| No | 11 (9.7%) | 7 (10.6%) | 11 (14.1%) | 11 (19.6%) | 0 (0%) | 10 (18.2%) | 13 (54.2%) | 0 (0%) | 0 (0%) |
| Total | 113 (100%) | 66 (100%) | 78 (100%) | 56 (100%) | 14 (100%) | 55 (100%) | 24 (100%) | 7 (100%) | 18 (100%) |
| Are you familiar with the patient’s rights and responsibilities act? | |||||||||
| Yes | 113 (100%) | 66 (100%) | 67 (85.9%) | 56 (100%) | 14 (100%) | 55 (100%) | 24 (100%) | 7 (100%) | 18 (100%) |
| No | 0 (0%) | 0 (0%) | 11 (14.1) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) |
| Total | 113 (100%) | 66 (100%) | 78 (100%) | 56 (100%) | 14 (100%) | 55 (100%) | 24 (100%) | 7 (100%) | 18 (100%) |
| Do you know the WMA statement on euthanasia and medically assisted suicide? | |||||||||
| Yes | 106 (93.8%) | 46 (69.7%) | 67 (85.9%) | 43 (76.8%) | 14 (100%) | 45 (81.8%) | 24 (100%) | 7 (100%) | 18 (100%) |
| No | 7 (6.2%) | 20 (30.3%) | 11 (14.1%) | 13 (23.2%) | 0 (0%) | 10 (18.2%) | 0 (0%) | 0 (0%) | 0 (0%) |
| Total | 113 (100%) | 66 (100%) | 78 (100%) | 56 (100%) | 14 (100%) | 55 (100%) | 24 (100%) | 7 (100%) | 18 (100%) |
| Have you ever been involved in a discussion that led to a decision DNAR a patient? | |||||||||
| Yes | 89 (78.8%) | 59 (89.4%) | 50 (64.1%) | 45 (80.4%) | 14 (100%) | 39 (70.9%) | 11 (45.8%) | 7 (100%) | 18 (100%) |
| No | 24 (21.2%) | 7 (10.6%) | 28 (35.9%) | 11 (19.6%) | 0 (0%) | 16 (29.1%) | 13 (54.2%) | 0 (0%) | 0 (0%) |
| Total | 113 (100%) | 66 (100%) | 78 (100%) | 56 (100%) | 14 (100%) | 55 (100%) | 24 (100%) | 7 (100%) | 18 (100%) |
| Have you ever made a decision not to resuscitate a patient? | |||||||||
| Yes | 83 (73.5%) | 59 (89.4%) | 61 (78.2%) | 45 (80.4%) | 14 (100%) | 39 (70.9%) | 11 (45.8%) | 7 (100%) | 10 (55.6%) |
| No | 30 (26.5%) | 7 (10.6%) | 17 (21.8%) | 11 (19.6%) | 0 (0%) | 16 (29.1%) | 13 (54.2%) | 0 (0%) | 8 (44.4%) |
| Total | 113 (100%) | 66 (100%) | 78(100%) | 56 (100%) | 14 (100%) | 55 (100%) | 24 (100%) | 7 (100%) | 18 (100%) |
| Was the decision DNAR discussed with the patient? | |||||||||
| Yes | 64 (56.6%) | 35 (53%) | 15 (19.2%) | 23 (41.1%) | 0 (0%) | 21 (38.2%) | 0 (0%) | 7 (100%) | 0 (0%) |
| No | 17 (15%) | 24 (36.4%) | 11 (14.1%) | 22 (39.3%) | 14 (100%) | 18 (32.7%) | 11 (45.8%) | 0 (0%) | 18 (100%) |
| Uncertain | 32 (28.3%) | 7 (10.6%) | 52 (66.7%) | 11 (19.6%) | 0 (0%) | 16 (29.1%) | 13 (54.2%) | 0 (0%) | 0 (0%) |
| Total | 113 (100%) | 66 (100%) | 78 (100%) | 56 (100%) | 14 (100%) | 55 (100%) | 24 (100%) | 7 (100%) | 18 (100%) |
| Was the prognosis of the disease discussed with the patient? | |||||||||
| Yes | 71 (62.8%) | 46 (69.7%) | 50 (64.1%) | 34 (60.7%) | 7 (50%) | 39 (70.9%) | 11 (45.8%) | 7 (100%) | 0 (0%) |
| No | 10 (8.8%) | 0 (0%) | 11 (14.1%) | 11 (19.6%) | 7 (50%) | 0 (0%) | 0 (0%) | 0 (0%) | 10 (55.6%) |
| Uncertain | 32 (28.3%) | 20 (30.3%) | 17 (21.8%) | 11 (19.6%) | 0 (0%) | 16 (29.1%) | 13 (54.2%) | 0 (0%) | 8 (44.4%) |
| Total | 113 (100%) | 66 (100%) | 78 (100%) | 56 (100%) | 14 (100%) | 55 (100%) | 24 (100%) | 7 (100%) | 18 (100%) |
| Was the patient asked about their opinion in the process that led to the decision of DNAR? | |||||||||
| Yes | 54 (47.8%) | 35 (53%) | 31 (39.7%) | 23 (41.1%) | 0 (0%) | 10 (18.2%) | 0 (0%) | 7 (100%) | 0 (0%) |
| No | 17 (15%) | 24 (36.4%) | 30 (38.5%) | 22 (39.3%) | 14 (100%) | 29 (52.7%) | 11 (45.8%) | 0 (0%) | 10 (55.6%) |
| Uncertain | 42 (37.1%) | 7 (10.6%) | 17 (21.8%) | 11 (19.6%) | 0 (0%) | 16 (29.1%) | 13 (54.2%) | 0 (0%) | 8 (44.4%) |
| Total | 113 (100%) | 66 (100%) | 78 (100%) | 56 (100%) | 14 (100%) | 55 (100%) | 24 (100%) | 7 (100%) | 18 (100%) |
| Was it the patient himself who initiated the discussion about DNAR? | |||||||||
| Yes | 29 (25.7%) | 13 (19.7%) | 0 (0%) | 10 (17.9%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) |
| No | 52 (46%) | 46 (69.7%) | 48 (61.5%) | 35 (62.5%) | 14 (100%) | 39 (70.9%) | 11 (45.8%) | 7 (100%) | 18 (100%) |
| Uncertain | 32 (28.3%) | 7 (10.6%) | 30 (38.5%) | 11 (19.6%) | 0 (0%) | 16 (29.1%) | 13 (54.2%) | 0 (0%) | 0 (0%) |
| Total | 113 (100%) | 66 (100%) | 78 (100%) | 56 (100%) | 14 (100%) | 55 (100%) | 24 (100%) | 7 (100%) | 18 (100%) |
| Was it the patient himself who requested not to be resuscitated? | |||||||||
| Yes | 52 (46%) | 24 (36.4%) | 7 (9%) | 23 (41.1%) | 0 (0%) | 0 (0%) | 0 (0%) | 7 (100%) | 0 (0%) |
| No | 37 (32.7%) | 35 (53%) | 41 (52.6%) | 22 (39.3%) | 14 (100%) | 39 (70.9%) | 11 (45.8%) | 0 (0%) | 18 (100%) |
| Uncertain | 24 (21.2%) | 7 (10.6%) | 30 (38.5%) | 11 (19.6%) | 0 (0%) | 16 (29.1%) | 13 (54.2%) | 0 (0%) | 0 (0%) |
| Total | 113 (100%) | 66 (100%) | 78 (100%) | 56 (100%) | 14 (100%) | 55 (100%) | 24 (100%) | 7 (100%) | 18 (100%) |
| If the decision DNAR was made without patient participation, was the patient informed of the decision once it was made? | |||||||||
| Yes | 35 (31%) | 22 (33.3%) | 15 (19.2%) | 10 (17.9%) | 0 (0%) | 21 (38.2%) | 0 (0%) | 7 (100%) | 0 (0%) |
| No | 23 (20.4%) | 11 (16.7%) | 35 (44.9%) | 35 (62.5%) | 14 (100%) | 18 (32.7%) | 11 (45.8%) | 0 (0%) | 10 (55.6%) |
| Uncertain | 55 (48.6%) | 33 (50%) | 28 (35.9%) | 11 (19.6%) | 0 (0%) | 16 (29.1%) | 13 (54.2%) | 0 (0%) | 8 (44.4%) |
| Total | 113 (100%) | 66 (100%) | 78 (100%) | 56 (100%) | 14 (100%) | 55 (100%) | 24 (100%) | 7 (100%) | 18 (100%) |
| Do you think there are patients who want to be informed that the responsible physician has made a decision DNAR but in practice they do not receive that information? | |||||||||
| Yes | 113 (100%) | 55 (83.3%) | 58 (74.4%) | 33 (58.9%) | 14 (100%) | 38 (69.1%) | 11 (45.8%) | 7 (100%) | 18 (100%) |
| No | 0 (0%) | 0 (0%) | 20 (25.6%) | 23 (41.1%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) |
| Uncertain | 0 (0%) | 11 (16.7%) | 0 (0%) | 0 (0%) | 0 (0%) | 17 (30.9%) | 13 (54.2%) | 0 (0%) | 0 (0%) |
| Total | 113 (100%) | 66 (100%) | 78 (100%) | 56 (100%) | 14 (100%) | 55 (100%) | 24 (100%) | 7 (100%) | 18 (100%) |
| Do you think there are patients who are informed that the responsible physician has made a decision DNAR, but those patients did not want to receive that information? | |||||||||
| Yes | 77 (68.1%) | 66 (100%) | 45 (57.7%) | 32 (57.1%) | 14 (100%) | 34 (61.85) | 11 (45.8%) | 7 (100%) | 8 (44.4%) |
| No | 13 (11.5%) | 0 (0%) | 22 (28.2%) | 13 (23.2%) | 0 (0%) | 10 (18.2%) | 0 (0%) | 0 (0%) | 10 (55.6%) |
| Uncertain | 23 (20.4%) | 0 (0%) | 11 (14.1%) | 11 (19.6%) | 0 (0%) | 11 (20%) | 13 (54.2%) | 0 (0%) | 0 (0%) |
| Total | 113 (100%) | 66 (100%) | 78 (100%) | 56 (100%) | 14 (100%) | 55 (100%) | 24 (100%) | 7 (100%) | 18 (100%) |
Physicians were asked if DNAR orders should be discussed with family members; 76.3% (n = 329) agreed to do so, and 77.7% (n = 95) also considered discussing the prognosis of the disease relevant. When asked if family members have the opportunity to participate in such discussions, 72.2% (n = 311) responded affirmatively. However, only 22% (n = 95) stated that family members initiate discussions about DNAR orders. Forty-five percent (n = 194) stated that it is not always necessary to seek the opinion of family members to consider a DNAR orders, and 71.5% (n = 308) said that the family should not be allowed to make the final decision on non-resuscitation; instead, other medical and ethical assessments should be considered.
When questioned about whether the patient’s wish to receive resuscitation should always be respected, regardless of the clinical situation, 39.2% (n = 169) answered affirmatively. However, when a decision DNAR a patient has been made and the patient’s condition improves, 87.7% (n = 378) mentioned that the DNAR orders should be reassessed. 80.5% (n = 347) considered that some patients want to know if they have DNAR orders; conversely, 67.7% (n = 292) believe that some patients do not want to know this information, and it is still communicated to them.
Discussion
According to the study results, the majority of participants (85.4%) were familiar with the guidelines for CPR, as well as the patient’s rights and duties law in force in Chile (97.5%) and the WMA’s declaration on euthanasia and assisted suicide (85.8%). However, about 46% of participants responded that these texts had not been socialized in their workplace, indicating a lack of dissemination and training on these topics in some work environments. The study by Bremer et al. 16 using this same questionnaire, identified that 35% of participants had read the resuscitation guidelines, while 63% had heard about them. Therefore, in this first aspect, our study showed higher percentages of knowledge of the guidelines and legal documents regarding cardiovascular resuscitation despite the age of the participants in Chile being lower (38 years versus 42 years). It is not known whether age can be an influential factor, but it is notable since it could be considered that the older the age, the greater the knowledge of the guidelines, but this is not entirely clear; it will remain a question for future research to seek the relationship between age with the percentage of knowledge of the ethical-legal guides and documents regarding CPR.
It is essential to emphasize that knowledge of ethical and legal guidelines for resuscitation and patient rights is crucial for healthcare professionals, as it can make the difference between care guided by good clinical practice and a purely paternalistic approach.23,24 Regarding the lack of dissemination and training in some workplaces, clinical simulation can be a useful tool for training in these matters, allowing professionals to practice and enhance their skills in a controlled and safe environment.25–27
This study also indicated that a proportion of physicians (77%) have been involved in discussions leading to the decision DNAR a patient, and most of the time, this decision is made without the patient’s participation (only 36% of the time it was discussed with the patient). These findings align with those reported by other authors, who state that the suspension and withdrawal of treatments in hospitalized patients are among the most frequent decisions for patients with a poor prognosis.28–30 A study by Blanco et al. 31 reported that the most frequent ethical problems for Spanish internists are precisely those related to end-of-life care, including the establishment of DNAR orders. Furthermore, a study carried out in Japan by Nakagawa et al. 32 reported that the proportion of patients with a DNAR order who had been involved in the decision process of their DNAR order was ⩽25% at 81% of the hospitals, 25–50% at 12%, 50–75% at 1%, and ⩾75% at 6%.
A previous study in Chile by Morales et al. 33 in which a questionnaire was sent to doctors working in pediatric intensive care units, reported that 98% (n = 124) of those surveyed had made decisions to limit therapeutic effort. Among these decisions, the most frequent was the DNAR order (n = 119). When these types of decisions are made, only 27% of the participants said that a document is written that the family signs, and 31% indicated that it is done only on some occasions. That is, family participation was documented about 50% of the time in these authors’ study. In our study, about 75% considered discussing the DNAR order’s prognosis and intention with family members.
The results suggest a need to improve communication and patient involvement in decision-making regarding DNAR orders. Following the recommendations of the bioethics working group of the Spanish Society of Intensive Care, the relationship between a patient and their healthcare professional is based on mutual trust, generated through sincerity in communication. The patient has control over who should be informed about their situation and is the owner of that information.34–36 In their study, Quenot et al. 37 emphasize the importance of ensuring that discussions fully consider the opinions and reflections of all those involved in patient management, as well as obtaining the patient’s opinion, either directly or through advance directive documents, or from the family, who is presumed to know the patient best and can provide information closest to what the patient’s decision would be.
Although the majority (76.3%) of respondents in this study favored allowing family participation in these decisions, a significant proportion differs from this practice. In this regard, some studies have pointed out that including the family helps the patient and improves the grieving process, making care more approachable, perceived as higher quality, and warmer.38–40 In the study by Bremer et al. 16 the DNAR decision (67%) and the patient’s prognoses (77%) were discussed with family members. In comparison, their opinions were considered to a lesser degree (58%) compared to the patient’s opinion. This situation is similar to what we reported in the present study.
This work also revealed a lack of consensus among surveyed physicians regarding whether the patient’s desire to receive CPR should always be respected. Despite an increase in the development of advance care planning documents in recent years, Cuevas et al.’s study 41 identified that only 50% of patients are aware of the existence of such documents, and only about 5% have filled them out.
This study is easily generalizable to other countries since the questionnaire is available in full text in English and Spanish, has been used previously, and only requires adapting the first questions according to the laws and guides governing aspects related to the DNAR orders and CPR guides in each country. We firmly believe that conducting studies of this type demonstrates the current situation in each region and is the fundamental basis for building care systems that consider the opinions of patients and their families, especially in aspects as sensitive as care at the end of life. We invite other authors to develop this study in their countries and publish their experiences to continue advancing in a kind of health that involves not only physical aspects but also other items relevant to comprehensive health care.
Strengths and limitations
Among the limitations of this study is the cross-sectional design, which lacks the capacity to establish causal relationships. In addition, the results may be influenced by sample selection, as several regions of the country were not represented in this study. Although the response rate was 14.4% and a priori could be considered a risk in estimating the data, using a probabilistic sample size with a sample calculation can help mitigate this bias (this was done), at least about participation, since the minimum sample size was reached and exceeded. However, this study should be considered a pioneer in addressing this topic, as there are no similar studies in the region. In addition, these results suggest the need to prioritize discussion within the medical community to establish a standardized guideline or consensus recommendations on the approach to DNAR orders. It is crucial to emphasize the need to consider the reevaluation of DNAR orders in case the patient shows improvement.
Conclusions
There is a need to improve communication and patient involvement in decision-making regarding DNAR orders. It is also crucial to ensure that discussions take into account the opinions and reflections of all involved in patient management, including the patient and their family. Furthermore, it becomes evident the necessity of establishing a guideline or a consensus of recommendations regarding DNAR orders and communication with patients and their families concerning these decisions. The importance of respecting patients’ preferences regarding the communication of these decisions is emphasized, along with considering the reevaluation of DNAR orders in case of patient improvement.
Supplemental Material
Supplemental material, sj-docx-1-smo-10.1177_20503121241259285 for Knowledge and attitudes of physicians in Chile toward Do-Not-Attempt-Resuscitation orders: A cross-sectional nation-wide study by Yelson Alejandro Picón-Jaimes, Ivan David Lozada-Martinez, Sabrina Rahman and Maria Belén Cantón Álvarez in SAGE Open Medicine
Supplemental material, sj-docx-2-smo-10.1177_20503121241259285 for Knowledge and attitudes of physicians in Chile toward Do-Not-Attempt-Resuscitation orders: A cross-sectional nation-wide study by Yelson Alejandro Picón-Jaimes, Ivan David Lozada-Martinez, Sabrina Rahman and Maria Belén Cantón Álvarez in SAGE Open Medicine
Acknowledgments
None.
Footnotes
Author contributions: Y.A.P.J., I.D.L.M., and M.B.C.A. contributed to methodology and validation. Y.A.P.J., I.D.L.M., S.R., and M.B.C.A. contributed to writing original draft, and review and editing. Y.A.P.J., I.D.L.M., and S.R. contributed to investigation and resources.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethics approval: The study was reviewed and approved by the Universidad Internacional de la Rioja Ethics Committee with registration number “2023-2612.”
Informed consent: Written informed consent was obtained from participants.
Trial registration: Not applicable.
ORCID iD: Sabrina Rahman  https://orcid.org/0000-0002-4057-3116
https://orcid.org/0000-0002-4057-3116
Supplemental material: Supplemental material for this article is available online.
References
- 1. Emanuel EJ. Euthanasia. Historical, ethical, and empiric perspectives. Arch Intern Med 1994; 154(17): 1890–1901. [DOI] [PubMed] [Google Scholar]
- 2. Knipe M, Hardman JG. I. Past, present, and future of “Do not attempt resuscitation” orders in the perioperative period. Br J Anaesth 2013; 111(6): 861–863. [DOI] [PubMed] [Google Scholar]
- 3. Wagemans AM, van Schrojenstein Lantman-de Valk HM, Proot IM, et al. Do-not-attempt-resuscitation orders for people with intellectual disabilities: dilemmas and uncertainties for ID physicians and trainees. The importance of the deliberation process. J Intellect Disabil Res 2017; 61(3): 245–254. [DOI] [PubMed] [Google Scholar]
- 4. Thomas RH, Schuster-Bruce M. Do not attempt resuscitation orders, ethics and the Mental Capacity Act. Br J Hosp Med (Lond) 2011; 72(5): 259–263. [DOI] [PubMed] [Google Scholar]
- 5. Fritz Z, Fuld J. Ethical issues surrounding do not attempt resuscitation orders: decisions, discussions and deleterious effects. J Med Ethics 2010; 36(10): 593–597. [DOI] [PubMed] [Google Scholar]
- 6. Dignam C, Brown M, Thompson CH. Moving from “Do Not Resuscitate” orders to standardized resuscitation plans and shared-decision making in hospital inpatients. Gerontol Geriatr Med 2021; 7: 23337214211003431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Tanabe R, Hongo T, Mandai Y, et al. Emotional work stress reactions of emergency medical technicians involved in transporting out-of-hospital cardiac arrest patients with “do not attempt resuscitation” orders. Resuscitation 2022; 173: 61–68. [DOI] [PubMed] [Google Scholar]
- 8. Mockford C, Fritz Z, George R, et al. Do not attempt cardiopulmonary resuscitation (DNACPR) orders: a systematic review of the barriers and facilitators of decision-making and implementation. Resuscitation 2015; 88: 99–113. [DOI] [PubMed] [Google Scholar]
- 9. Chilean National Congress. Law 20584, https://www.bcn.cl/leychile (2012, accessed 22 December 2023).
- 10. Saboga M, Pamela F. Medicina familiar, principios bioéticos y final de la vida en Colombia. Rev Cuba Med Gen Integral 2023; 39(2): e2243. [Google Scholar]
- 11. Cárdenas Cárdenas JL. Factores determinantes para la toma de decisiones complejas en pacientes con enfermedades crónicas avanzadas: Una mirada desde los cuidados paliativos. Acta Med Colomb 2021; 47(2). [Google Scholar]
- 12. Momblanc LC, Estupiñan YP, de los Ángeles Feal Fernández M. La adecuación del esfuerzo terapéutico en el ordenamiento jurídico cubano. Rev Cuba Med Intensiva Emerg 2023; 21(4): e951. [Google Scholar]
- 13. Macchi MJ, Pérez M, del V, Alonso JP. Planificación de los cuidados en el final de la vida. Perspectivas de profesionales de oncología y cuidados paliativos. Sex Salud Soc (Rio J) 2020; (35): 218–236. [Google Scholar]
- 14. Merchant RM, Topjian AA, Panchal AR, et al. Part 1: executive summary: 2020 American heart association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation 2020; 142(16_suppl_2): S337–S357. [DOI] [PubMed] [Google Scholar]
- 15. WMA declaration on euthanasia and physician-assisted suicide, https://www.wma.net/policies-post/declaration-on-euthanasia-and-physician-assisted-suicide/ (2019, accessed 25 February 2024).
- 16. Bremer A, Årestedt K, Rosengren E, et al. Do-not-attempt-resuscitation orders: attitudes, perceptions and practices of Swedish physicians and nurses. BMC Med Ethics 2021; 22(1): 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Naess M. “Do-Not-Attempt-Resuscitation”-orders in ICCUs: a survey of attitudes and experiences of nurses in Norway. Intensive Crit Care Nurs 2009; 25(3): 140–146. [DOI] [PubMed] [Google Scholar]
- 18. Löfmark R, Nilstun T. Do-not-resuscitate orders—Should the patient be informed? J Intern Med 1997; 241(5): 421–425. [DOI] [PubMed] [Google Scholar]
- 19. Löfmark R, Nilstun T. Informing patients and relatives about do-not-resuscitate decisions. Attitudes of cardiologists and nurses in Sweden. J Intern Med 1998; 243(3): 191–195. [DOI] [PubMed] [Google Scholar]
- 20. Rodríguez del Águila MM, González-Ramírez AR. Sample size calculation. Allergol Immunopathol (Madr) 2014; 42(5): 485–492. [DOI] [PubMed] [Google Scholar]
- 21. Bishara AJ, Li J, Conley C. Informal versus formal judgment of statistical models: the case of normality assumptions. Psychon Bull Rev 2021; 28(4): 1164–1182. [DOI] [PubMed] [Google Scholar]
- 22. Pautas éticas internacionales para la investigación relacionada con la salud con seres humanos. COUNCIL FOR INTERNATIONAL ORGANIZATIONS OF MEDICAL SCIENCES, https://cioms.ch/publications/product/pautas-eticas-internacionales-para-la-investigacion-relacionada-con-la-salud-con-seres-humanos/ (2017, accessed 28 March 2024).
- 23. Gulino M, Patuzzo S, Baldelli I, et al. Bioethics in Italian medical and healthcare education. A pilot study. Acta Bio-Medica Atenei Parm 2019; 89(4): 519–531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Post SG, Wentz SW. Joining humanity and Science: medical humanities, compassionate care, and bioethics in medical education. Perspect Biol Med 2022; 65(3): 458–468. [DOI] [PubMed] [Google Scholar]
- 25. Haynes C, Yamamoto M, Dashiell-Earp C, et al. Continuity clinic practice feedback curriculum for residents: a model for ambulatory education. J Grad Med Educ 2019; 11(2): 189–195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Martins V, Santos C, Duarte I. Bioethics education and the development of nursing students’ moral competence. Nurse Educ Today 2020; 95: 104601. [DOI] [PubMed] [Google Scholar]
- 27. Mentzelopoulos SD, Slowther AM, Fritz Z, et al. Ethical challenges in resuscitation. Intensive Care Med 2018; 44(6): 703–716. [DOI] [PubMed] [Google Scholar]
- 28. García Caballero R, Herreros B, Real de Asúa D, et al. Withholding and withdrawing treatment in patients admitted in an Internal Medicine ward. Rev Calid Asist Organo Soc Espanola Calid Asist 2016; 31(2): 70–75. [DOI] [PubMed] [Google Scholar]
- 29. García-Caballero R, Herreros B, Real de Asúa D, et al. Limitation of therapeutic effort in patients hospitalised in departments of internal medicine. Rev Clin Esp 2018; 218(1): 1–6. [DOI] [PubMed] [Google Scholar]
- 30. Gross M. Cardiopulmonary resuscitation and do not attempt resuscitation and do not attempt resuscitation orders: legislation may be helpful. Clin Med Lond Engl 2002; 2(1): 80. [PubMed] [Google Scholar]
- 31. Blanco-Portillo A, García-Caballero R, Real de, Asúa D, et al. Which are the most prevalent ethical conflicts for Spanish internists? Rev Clínica Esp 2021; 221(7): 393–399. [DOI] [PubMed] [Google Scholar]
- 32. Nakagawa Y, Inokuchi S, Kobayashi N, et al. Do not attempt resuscitation order in Japan. Acute Med Surg 2017; 4(3): 286–292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Morales Valdés G, Alvarado Romero T, et al. Limitación del esfuerzo terapéutico en cuidados intensivos pediátricos: conocimiento y actitudes bioéticas del profesional médico. Rev Chil Pediatr 2016; 87(2): 116–120. [DOI] [PubMed] [Google Scholar]
- 34. Estella Á, Saralegui I, Rubio Sanchiz O, et al. Update and recommendations in decision making referred to limitation of advanced life support treatment. Med Intensiva 2020; 44(2): 101–112. [DOI] [PubMed] [Google Scholar]
- 35. Estella A, Martín MC, Hernández A, et al. End of life critical patients: a multicenter study in Spanish Intensive Care Units. Med Intensiva 2016; 40(7): 448–450. [DOI] [PubMed] [Google Scholar]
- 36. Lauridsen KG, Saraiva J, Løfgren B, et al. Full resuscitation or no resuscitation attempt: should we have a third option? Resuscitation 2022; 181: 68–69. [DOI] [PubMed] [Google Scholar]
- 37. Quenot JP, Ecarnot F, Meunier-Beillard N, et al. What are the ethical aspects surrounding the collegial decisional process in limiting and withdrawing treatment in intensive care? Ann Transl Med 2017; 5(S-4): S43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. León Delgado MX, Acero González ÁR, Buitrago Reyes LA, et al. Grief and palliative home-care services for patients at the end of life during the COVID-19 pandemic in Colombia: analysis from the relatives’ perspective. Rev Colomb Psiquiatr. Epub ahead of print 24 October 2022. DOI: 10.1016/j.rcp.2022.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Achury DM, Pinilla M. Nursing professional communication with the family of the terminal patienta. Enferm Univ 2016; 13(1): 55–60. [Google Scholar]
- 40. Bonete Román MC, Campos Rivera G. The death of children: ethical dilemmas about the limitation of therapeutic effort. J Healthc Qual Res 2023; 38(3): 180–185. [DOI] [PubMed] [Google Scholar]
- 41. Cuevas-Garcia J, Gil-Caravaca V, Osuna Carrillo de Albornoz E. Attitudes and beliefs towards advance directives and end-of-life care preferences among elderly population in a community health centre. Med Clínica 2023; 160(5): 222–223. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-smo-10.1177_20503121241259285 for Knowledge and attitudes of physicians in Chile toward Do-Not-Attempt-Resuscitation orders: A cross-sectional nation-wide study by Yelson Alejandro Picón-Jaimes, Ivan David Lozada-Martinez, Sabrina Rahman and Maria Belén Cantón Álvarez in SAGE Open Medicine
Supplemental material, sj-docx-2-smo-10.1177_20503121241259285 for Knowledge and attitudes of physicians in Chile toward Do-Not-Attempt-Resuscitation orders: A cross-sectional nation-wide study by Yelson Alejandro Picón-Jaimes, Ivan David Lozada-Martinez, Sabrina Rahman and Maria Belén Cantón Álvarez in SAGE Open Medicine