Abstract
Introduction
Branch atheromatous disease (BAD)-related stroke is increasingly becoming a clinical entity and prone to early neurological deterioration (END) and poor prognosis. There are no effective regimens to reduce the disability caused by BAD-related stroke in acute phase. Recent studies have indicated the efficacy of tirofiban in acute ischaemic stroke; however, its efficacy has not been validated in patients with BAD-related stroke. Thus, we aim to test whether intravenous tirofiban initiated within 48 hours after the onset would improve the functional outcome in patients with acute BAD-related stroke, in comparison with the standard antiplatelet therapy based on the current guideline.
Methods and analysis
BRANT is a multicentre, randomised, open-label, blinded endpoint, parallel-controlled, phase III trial conducted in 21 hospitals in China. Participants aged 18–75 years with acute BAD-related stroke within 48 hours after the stroke onset are randomised in a 1:1 ratio to the tirofiban or control group. The treatment period is 48 hours in both groups. The primary outcome is the excellent functional outcome (modified Rankin Scale Score: 0–1) at 90 days. The secondary outcomes include END, major bleeding, stroke, death, functional status, serious adverse events and change in bleeding-related markers. Assuming the rates of the primary outcome to be 74% in the tirofiban group and 62% in the control group, a total of 516 participants are needed for 0.8 power (two-sided 0.05 alpha).
Ethics and dissemination
BRANT study has been approved by the Ethics Committee of the Peking Union Medical College Hospital (I-23PJ1242). Written informed consent is required for all the patients before enrolment. The results of the study will be published in a peer-reviewed journal.
Trial registration number
ClinicalTrials.gov (NCT06037889).
Keywords: Stroke, Prognosis, THERAPEUTICS
STRENGTHS AND LIMITATIONS OF THIS STUDY.
With the aid of MRI, this study focuses on the patients with acute branch atheromatous disease (BAD)-related stroke, which had been inappropriately classified as small-vessel occlusion or an undetermined aetiology by the Trial Org 10 172 in Acute Stroke Treatment system in previous studies.
The intervention will be initiated within 48 hours of onset, which is more in line with the timeliness of BAD treatment.
The lack of a double-blinded design is a limitation, but the endpoints are measured in a blinded manner.
Introduction
Branch atheromatous disease (BAD), first described conceptually by Caplan in 1989, is being confirmed as a clinical entity with the aid of advanced neuroimaging.1–3 BAD-related stroke, characterised by subcortical single infarct in penetrating artery territories without severe stenosis of the large parent artery, accounts for 20.4% of all ischaemic stroke cases in Asian populations.2 4 Differing from lacunar infarct due to lipohyalinosis, BAD-related stroke is caused by parent arterial plaque occlusion of the perforating orifice or proximal atherosclerotic occlusion of the perforating artery,1–3 which could be identified from small-vessel occlusion or stroke of undetermined source in the Trial Org 10 172 in Acute Stroke Treatment (TOAST) system.5 6
A high incidence of early neurological deterioration (END) has been observed in BAD-related stroke and is strongly associated with poor prognosis.7 8 The rate of END is higher in BAD-related stroke than in lacunar infarct (26.8%–37.5% vs 6.3%–18.6%), and thrombolysis itself cannot prevent the occurrence of END.7–9 In addition, it remains unclear whether intravenous thrombolysis could improve the clinical outcome of BAD-related stroke.10 The rate of disability can reach 61%.2 However, there are no high-level recommendations for the acute-phase treatment of BAD-related stroke, and no randomised controlled trial (RCT) has examined BAD as a separate disease. Current practice—based on the limited observational data and expert opinion—is heterogeneous, including the anticoagulant and mono/dual antiplatelet therapy, the efficacy of which is uncertain for BAD-related stroke.11 12
Tirofiban, a selective and reversible antagonist of glycoprotein IIb/IIIa inhibitors on platelets, might be more effective than conventional agents (such as aspirin or clopidogrel) by blocking the final common pathway of platelet aggregation at the pathophysiological level.13 In clinical studies, historical evidence has also reported that tirofiban increases the recanalisation rate and improves the functional prognosis in stroke patients with endovascular therapy without increasing bleeding risk.14–16 A large randomised trial of patients with stroke without large or medium-sized vessel occlusion also reported the efficacy of tirofiban.17 However, though an atherosclerotic mechanism is presumed to exist between BAD and large artery atherosclerosis, this evidence may not be generalised to BAD-related stroke, as retrospective data or small samples may introduce selection bias.14 18 Moreover, about 78.6%–90.9% of END occurs within 48 hours after the onset.19 20 Our preliminary results of a cohort with BAD-related stroke found that the median time from onset to END was 38 hours. We hypothesised that early tirofiban administration could improve the functional prognosis by preventing the occurrence of END. However, tirofiban was often prescribed after END in previous studies, which might cause irreversible ischaemic lesions and neurologic deficits.14 17 Thus, RCTs of acute BAD-related stroke are needed and have been requested by the researchers.3 4 In addition, we speculated that tirofiban should be initiated within 48 hours after onset to prevent the occurrence of END.
The BRANT study aims to establish the efficacy and safety of intravenous tirofiban for improving the functional outcome in patients with acute BAD-related stroke.
Methods
Design
This is a multicentre, randomised, open-label, blinded endpoint, parallel-controlled phase III trial. The BRANT study began enrolment on 9 November 2023, and the anticipated date of study completion is 31 October 2025.
Patient population
BRANT will enrol 516 participants with BAD-related stroke within 48 hours of onset from 21 centres in China.
Inclusion criteria
Age: 18–75 years old.21 22
Acute ischaemic stroke.
Time from onset to randomisation ≤48 hours; if onset time is unknown, time from last known well to randomisation ≤48 hours.
-
Meet the following BAD diagnostic imaging criteria:
Diffusion-weighted imaging (DWI) infarcts: single (isolated) deep (subcortical) infarcts.
-
The culprit arteries are either lenticulostriate artery (LSA) or paramedian pontine artery (PPA), and the infarct lesion on DWI conforms to one of the following characteristics (A/B):
LSA: ‘Comma-like’ infarct lesions with ‘fan-shaped’ extension from bottom to top in the coronary position; or ≥3 layers (layer thickness 5–7 mm) on the axial DWI brain images.
PPA: The infarct lesion extends from the deep pons to the ventral pons on the axial DWI brain images.
3. No more than 50% stenosis on the parent artery of the criminal artery (ie, corresponding basilar or middle cerebral artery) (confirmed by magnetic resonance angiography (MRA)/CT angiography (CTA)/digital subtraction angiography (DSA)).
Signed informed consent by the patient or legally authorised representatives.
Exclusion criteria
Transient ischaemic attack (TIA).
Intracranial haemorrhagic diseases, vascular malformations, aneurysms, brain abscesses, malignant space-occupying lesions or other non-ischaemic intracranial lesions detected by baseline CT/MRI, or MRA/CTA/DSA.
Presence of ≥50% stenosis in extracranial artery in tandem relationship ipsilateral to the lesion.
Cardiogenic embolism: atrial fibrillation, myocardial infarction, heart valve disease, dilated cardiomyopathy, infective endocarditis, atrioventricular block disease, heart rate <50 beats per minute.
Have received or plan to receive endovascular therapy or thrombolysis after onset.
Stroke of other clear causes, for example, moyamoya disease, arterial entrapment, vasculitis, etc.
Modified Rankin Scale score ≥2 before onset.
Use of tirofiban within 1 week before or after onset.
Low platelets (<100×109 /L), or prothrombin time >1.3 times of the upper normal limit, or international normalised ratio >1.5 or other systemic haemorrhagic tendencies such as haematological disorders.
Elevation of alanine aminotransferase or aspartate aminotransferase >1.5 times the upper normal limit.
Glomerular filtration rate <60 mL/min/1.73 m2.
Known malignant tumours.
History of trauma or major surgical intervention within 6 weeks prior to onset.
History of intracranial haemorrhage.
Active or recent history (within 30 days prior to onset) of clinical bleeding (eg, gastrointestinal bleeding).
Malignant hypertension (systolic blood pressure >200 mm Hg or diastolic blood pressure >120 mm Hg).
Life expectancy ≤6 months.
Contraindications of 3T MRI examination.
Pregnant or lactating women.
Have participated in another clinical trial within 3 months prior to the date of informed consent or are participating in another clinical trial.
Randomisation
Participants will be randomised in a 1:1 ratio using a dynamic block randomisation method via an independent central website. The block sizes were set to 6, 8 and 12. The allocation sequence is stored on the central website and the participant will be assigned to the tirofiban or control group in a 1:1 ratio according to the order of enrolment.
Intervention
Tirofiban group: intravenous tirofiban will be administered immediately after randomisation for a total duration of 48 hours with a loading dose of 0.4 µg/kg/min×30 min, followed by a maintenance dose of 0.1 µg/kg/min×47.5 hours (figure 1).
Figure 1.
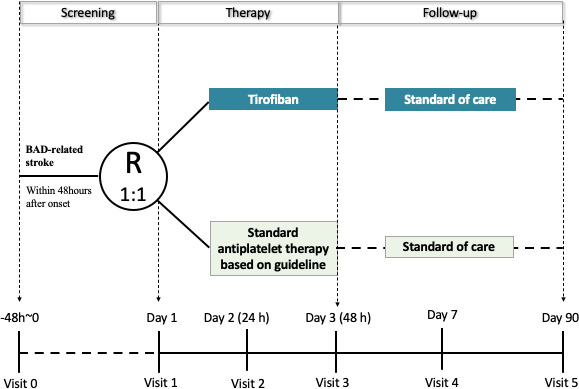
Study flow. BAD, branch atheromatous disease.
Control group: standard antiplatelet therapy based on the Chinese stroke guidelines will be initiated after randomisation for a total duration of 48 hours, as the two following types: (1) aspirin 150–300 mg per day, or (2) aspirin 100 mg per day plus clopidogrel 75 mg per day.23 Its initiation will be determined based on the last administration time of antithrombotic drugs; however, the drug should be administered as soon as possible.
After a 48-hour treatment period in both groups, the standard of care, including an antithrombotic regimen, will be performed based on current guidelines and recorded in detail (figure 1).
Primary outcomes
The primary outcome is an excellent functional outcome at 90 days, defined as a modified Rankin Scale score of 0-1.24 The primary outcome will be measured by the qualified evaluators who are blinded to all procedures.
Secondary outcomes
Secondary efficacy outcomes include END, National Institutes of Health Stroke Scale (NIHSS) score, Barthel Index score, ischaemic stroke, stroke, TIA, a composite event of new-onset stroke, myocardial infarction and all-cause death. Excellent functional outcome at 7 days is also listed as a secondary efficacy outcome. Safety outcomes include major bleeding as defined by the PLATO criteria, adverse events, all-cause death and changes in bleeding-related markers.25 The evaluators will not be aware of the treatment assignment after randomisation. All the clinical and safety events will be re-examined by the independent Clinical Event Committee (CEC), which will be blinded during all the procedures.
Considering the predictive value of END, we adopted the widely used and conservative definition of END for the BRANT study.26 The presence of END is determined by an increase of ≥4 points in the NIHSS or an increase of ≥2 points in the NIHSS motor score. The NIHSS motor score refers to bilateral upper and lower extremity mobility scores. The baseline NIHSS score for the calculation of END is the first clinician evaluated and recorded NIHSS score after onset. The time frame for postrandomisation END is within 7 days of randomisation.
Study protocol and data management
A study flowchart is shown in figure 1 and online supplemental table S1. At visit 1, the trained investigators will recruit the patients based on the screening age, onset time, MRI and other enrolment criteria (ie, intracranial artery and ECG). The investigator will then explain the BRANT study to the patient in detail, including the contents of each visit and the interventions. After obtaining written informed consent, the participants will be assigned to the tirofiban or control groups via a central website-based randomisation system. The patients are encouraged to undergo on-site follow-up at 90 days. Demographic, clinical, radiological, laboratory and clinical event data at each visit (online supplemental table S1) will be collected and stored in an electronic case report form (CRF) via a secure website. All CRFs will be checked by the local investigators for completeness and correction prior to data entry. The data will be checked dynamically by the principal investigator (JN) with the aid of research assistants.
bmjopen-2023-082141supp001.pdf (39.3KB, pdf)
Data monitoring board
An independent Data Security Monitoring Board (DSMB), including academic experts and statisticians, has been established to protect the interests of the participants during the study. The DSMB will review the overall implementation of the clinical study regularly and dynamically assess the risks and benefits, particularly the unexpected adverse events. The DSMB reports to the Executive Committee and provides professional advice.
Sample size estimates
Based on the previous studies and clinical practice, we assumed the rates of the primary outcome to be 62% and 74% in the control and tirofiban groups, respectively.2 14–16 18 27–29 Thus, 234 participants per arm are needed for a two-sided test at alpha 0.05 and power 0.8. Considering a dropout rate of 10%, 516 patients will be required.
Statistical analyses
According to the principle of intention-to-treat analysis, all the participants who are randomised into groups with more than one efficacy evaluation will be included in the full analysis set. The estimation of missing values will be conducted by the carry-over based on last observation carried forward estimation method. The proportion of excellent functional outcomes at 90 days will be compared using the χ2 tests and shown as frequency (percentage). Most secondary outcome analyses will also use the primary outcome analysis strategy. Survival data will be calculated using the Kaplan-Meier method to estimate the survival rate in each group, and efficacy will be assessed using the log-rank test. HRs and 95% CIs will be calculated using the Cox proportional hazards model. Non-survival data will be analysed using the χ2 test, and ORs and 95% CIs will be calculated using Logistic regression model. Continuous variables will be compared between the two groups using the Student’s t-test or Wilcoxon rank-sum test. The influence of covariables will be evaluated using subgroup analysis. No interim analysis is planned in this trial. All analyses will be performed using SAS V.9.4, and a two-sided p<0.05 is considered significant.
Patient and public involvement statement
None.
Ethics and dissemination
The BRANT study was approved by the Ethics Committee of Peking Union Medical College Hospital (I-23PJ1242) on 20 July 2023. Written informed consent is required from all the patients before enrolment. BRANT will be carried out according to Good Clinical Practice and the Declaration of Helsinki. The protocol amendments will be reported to the institutional ethics committee. The trial sponsor is Peking Union Medical College Hospital. The trial results will be published in a peer-reviewed journal.
Discussion
The BRANT study is a multicentre RCT that addresses the important treatment dilemma of improving the functional outcomes of BAD-related stroke.
BAD was first proposed by Caplan in 1989 to be distinct from lacunar infarct.1 However, in the past three decades, most clinical studies have classified BAD as small-vessel occlusion or undetermined aetiology based on the TOAST system.4 5 Few studies focused on acute BAD-related stroke, probably due to discrepant definitions.3 Recently, an increasing number of observational studies found distinct clinical, radiologic and prognostic features that patients with BAD-related stroke are prone to END and poor prognosis.2 30
Owing to the limitations of neuroimaging techniques, the perforating artery, such as the LSA or PPA, cannot be directly visualised. Radiological diagnosis is based on the vascular territory, dimension or shape of the lesion,3 31 which results in huge variations among BAD definitions. With the aid of neuroimaging and clinical practice, Asian neurologists proposed the radiological diagnosis criteria for BAD.32 33 Our previous study also found that ≥4 consecutive slices on the axial view are more effective than the transversal diameter in differentiating atherosclerotic mechanisms of single subcortical infarction in the LSA territory.34 Considering the generalisation and diagnostic accuracy of our study, we used ≥3 consecutive layers on the axial DWI series instead of lesion diameter to define BAD-related stroke in the LSA territory.35 Because obtaining direct evidence of the LSA and PPA is currently not technically feasible, our inclusion criteria based on MRI show considerable accuracy and representativeness.
In addition, our study uses simplified operationalised criteria to exclude cardiogenic embolism and patients with these comorbidities will not be included. Some conditions seem general, which is a limitation of our study; however, this facilitates the researcher’s ability to complete the screening within a limited timeframe with low inconsistency.
We set a 90-day excellent functional outcome instead of END or new-onset stroke as the primary outcome for the following reasons: (1) historical evidence indicated that tirofiban improved the functional outcome of ischaemic stroke;14 17 (2) END is an intermediate indicator;7 (3) the 90-day rate of recurrent stroke is 1.8% in our preliminary analysis of a BAD-related stroke cohort and probably less than 3.8% in other cohorts,30 which is relatively low. Thus, the BRANT study will provide direct evidence on how to reduce the disability caused by BAD, which is the major challenge in current clinical practice.
As oral mono antiplatelet therapy is unethical and against Chinese stroke guidelines for patients with NIHSS ≤3, there are two types of antiplatelet therapy in the control group.23 A double-blind design would markedly increase the complexity of the trial procedure. Therefore, we selected a prospective randomised open-blinded end-point design for BRANT. Independent senior neurologists who will be blinded to the procedure information have been trained to evaluate the primary outcome. An independent CEC has been established to centrally re-examine all the clinical events after randomisation. Some local investigators may know the treatment allocation; however, all evaluators of the subjective indicators will be blinded to the treatment allocation.
Supplementary Material
Footnotes
Contributors: SL and JN designed the study. SL drafted the manuscript. DZ designed the statistical method. YS, LZ, YZ and BP critically revised the study protocol and the manuscript. The entire project will be supervised by JN.
Funding: This study is funded by the National High Level Hospital Clinical Research Funding (2022-PUMCH-D-007).
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, conduct, reporting or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Ethics statements
Patient consent for publication
Not applicable.
References
- 1. Caplan LR. Intracranial branch atheromatous disease: a neglected, Understudied, and UNDERUSED concept. Neurology 1989;39:1246–50. 10.1212/wnl.39.9.1246 [DOI] [PubMed] [Google Scholar]
- 2. Kwan MW-M, Mak W, Cheung RT-F, et al. Ischemic stroke related to intracranial branch atheromatous disease and comparison with large and small artery diseases. J Neurol Sci 2011;303:80–4. 10.1016/j.jns.2011.01.008 [DOI] [PubMed] [Google Scholar]
- 3. Petrone L, Nannoni S, Del Bene A, et al. Branch atheromatous disease: a clinically meaningful, yet Unproven concept. cerebrovascular diseases. Cerebrovasc Dis 2016;41:87–95. 10.1159/000442577 [DOI] [PubMed] [Google Scholar]
- 4. Kim BJ, Kim JS. Ischemic stroke subtype classification: an Asian viewpoint. J Stroke 2014;16:8–17. 10.5853/jos.2014.16.1.8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Uchiyama S, Toyoda K, Kitagawa K, et al. Branch atheromatous disease diagnosed as Embolic stroke of undetermined source: a sub-analysis of NAVIGATE ESUS. Int J Stroke 2019;14:915–22. 10.1177/1747493019852177 [DOI] [PubMed] [Google Scholar]
- 6. Wen L, Feng J, Zheng D. Heterogeneity of single small subcortical infarction can be reflected in lesion location. Neurol Sci 2013;34:1109–16. 10.1007/s10072-012-1187-6 [DOI] [PubMed] [Google Scholar]
- 7. Duan Z, Fu C, Chen B, et al. Lesion patterns of single small subcortical infarct and its association with early neurological deterioration. Neurol Sci 2015;36:1851–7. 10.1007/s10072-015-2267-1 [DOI] [PubMed] [Google Scholar]
- 8. Jeong H-G, Kim BJ, Yang MH, et al. Neuroimaging markers for early neurologic deterioration in single small subcortical infarction. Stroke 2015;46:687–91. 10.1161/STROKEAHA.114.007466 [DOI] [PubMed] [Google Scholar]
- 9. Park M-G, Oh EH, Kim B-K, et al. Intravenous tissue plasminogen activator in acute branch atheromatous disease: does it prevent early neurological deterioration. J Clin Neurosci 2016;33:194–7. 10.1016/j.jocn.2016.04.011 [DOI] [PubMed] [Google Scholar]
- 10. Wu X, Liu Y, Nie C, et al. Efficacy and safety of intravenous Thrombolysis on acute branch atheromatous disease: a retrospective case-control study. Front Neurol 2020;11:581. 10.3389/fneur.2020.00581 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Wang Q, Chen C, Chen XY, et al. Low-molecular-weight heparin and early neurologic deterioration in acute stroke caused by large artery occlusive disease. Arch Neurol 2012;69:1454–60. 10.1001/archneurol.2012.1633 [DOI] [PubMed] [Google Scholar]
- 12. Yi X, Zhou Q, Wang C, et al. Aspirin plus Clopidogrel may reduce the risk of early neurologic deterioration in ischemic stroke patients carrying Cyp2C19*2 reduced-function Alleles. J Neurol 2018;265:2396–403. 10.1007/s00415-018-8998-1 [DOI] [PubMed] [Google Scholar]
- 13. Schwarz M, Meade G, Stoll P, et al. Conformation-specific blockade of the integrin Gpiib/Iiia: a novel antiplatelet strategy that selectively targets activated platelets. Circ Res 2006;99:25–33. 10.1161/01.RES.0000232317.84122.0c [DOI] [PubMed] [Google Scholar]
- 14. Wu C, Sun C, Wang L, et al. Low-dose Tirofiban treatment improves neurological deterioration outcome after intravenous Thrombolysis. Stroke 2019;50:3481–7. 10.1161/STROKEAHA.119.026240 [DOI] [PubMed] [Google Scholar]
- 15. Pan X, Zheng D, Zheng Y, et al. Safety and efficacy of Tirofiban combined with Endovascular treatment in acute ischaemic stroke. Eur J Neurol 2019;26:1105–10. 10.1111/ene.13946 [DOI] [PubMed] [Google Scholar]
- 16. Yang J, Wu Y, Gao X, et al. Intraarterial versus intravenous Tirofiban as an adjunct to Endovascular Thrombectomy for acute ischemic stroke. Stroke 2020;51:2925–33. 10.1161/STROKEAHA.120.029994 [DOI] [PubMed] [Google Scholar]
- 17. Zi W, Song J, Kong W, et al. Tirofiban for stroke without large or medium-sized vessel occlusion. N Engl J Med 2023;388:2025–36. 10.1056/NEJMoa2214299 [DOI] [PubMed] [Google Scholar]
- 18. Liu B, Zhang H, Wang R, et al. Early administration of Tirofiban after Urokinase-mediated intravenous Thrombolysis reduces early neurological deterioration in patients with branch atheromatous disease. J Int Med Res 2020;48. 10.1177/0300060520926298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Audebert HJ, Pellkofer TS, Wimmer ML, et al. Progression in Lacunar stroke is related to elevated acute phase parameters. Eur Neurol 2004;51:125–31. 10.1159/000077012 [DOI] [PubMed] [Google Scholar]
- 20. Kim YS, Lee K-Y, Koh S-H, et al. The role of matrix metalloproteinase 9 in early neurological worsening of acute Lacunar infarction. Eur Neurol 2006;55:11–5. 10.1159/000091137 [DOI] [PubMed] [Google Scholar]
- 21. Januzzi JL, Sabatine MS, Wan Y, et al. Interactions between age, outcome of acute coronary syndromes, and Tirofiban therapy. Am J Cardiol 2003;91:457–61. 10.1016/s0002-9149(02)03247-2 [DOI] [PubMed] [Google Scholar]
- 22. Li L, Geraghty OC, Mehta Z, et al. Age-specific risks, severity, time course, and outcome of bleeding on long-term antiplatelet treatment after vascular events: a population-based cohort study. The Lancet 2017;390:490–9. 10.1016/S0140-6736(17)30770-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Chinese Society of Neurology, Cerebrovascular disease group of Chinese Society of Neurology . Chinese guidelines for diagnosis and treatment of acute ischemic stroke 2018. Chin J Neurol 2018;51 9:666–82. [Google Scholar]
- 24. van Swieten JC, Koudstaal PJ, Visser MC, et al. Interobserver agreement for the assessment of handicap in stroke patients. Stroke 1988;19:604–7. 10.1161/01.str.19.5.604 [DOI] [PubMed] [Google Scholar]
- 25. Wallentin L, Becker RC, Budaj A, et al. Ticagrelor versus Clopidogrel in patients with acute coronary syndromes. N Engl J Med 2009;361:1045–57. 10.1056/NEJMoa0904327 [DOI] [PubMed] [Google Scholar]
- 26. Seners P, Turc G, Oppenheim C, et al. Incidence, causes and predictors of neurological deterioration occurring within 24 H following acute ischaemic stroke: a systematic review with pathophysiological implications. J Neurol Neurosurg Psychiatry 2015;86:87–94. 10.1136/jnnp-2014-308327 [DOI] [PubMed] [Google Scholar]
- 27. Wang H, Li X, Liu C, et al. Effects of oral antiplatelet agents and Tirofiban on functional outcomes of patients with non-disabling minor acute ischemic stroke. J Stroke Cerebrovasc Dis 2020;29:104829. 10.1016/j.jstrokecerebrovasdis.2020.104829 [DOI] [PubMed] [Google Scholar]
- 28. Lin J, Han Z, Wang C, et al. Dual therapy with Clopidogrel and aspirin prevents early neurological deterioration in ischemic stroke patients carrying Cyp2C19*2 reduced-function Alleles. Eur J Clin Pharmacol 2018;74:1131–40. 10.1007/s00228-018-2468-7 [DOI] [PubMed] [Google Scholar]
- 29. Albers GW, Marks MP, Kemp S, et al. Thrombectomy for stroke at 6 to 16 hours with selection by perfusion imaging. N Engl J Med 2018;378:708–18. 10.1056/NEJMoa1713973 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Zhang C, Wang Y, Zhao X, et al. Distal single subcortical infarction had a better clinical outcome compared with proximal single subcortical infarction. Stroke 2014;45:2613–9. 10.1161/STROKEAHA.114.005634 [DOI] [PubMed] [Google Scholar]
- 31. Yamamoto Y, Ohara T, Hamanaka M, et al. Characteristics of intracranial branch atheromatous disease and its association with progressive motor deficits. J Neurol Sci 2011;304:78–82. 10.1016/j.jns.2011.02.006 [DOI] [PubMed] [Google Scholar]
- 32. Adachi T, Takagi M. The clinical differences between Lacunar infarction and branch atheromatous disease. Nihon Rinsho 2006;64 Suppl 8:155–9. [PubMed] [Google Scholar]
- 33. Zhou LX. Ni J.Advances in branch atheromatous disease. Chinese Stroke Journal 2020;15:1351. [Google Scholar]
- 34. Cao Y, Zhang M, Zhou L, et al. Consecutive slides on axial view is more effective than Transversal diameter to differentiate mechanisms of single subcortical Infarctions in the Lenticulostriate artery territory. Front Neurol 2019;10:336. 10.3389/fneur.2019.00336 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. SPS3 Investigators, Benavente OR, Hart RG, et al. Effects of Clopidogrel added to aspirin in patients with recent Lacunar stroke. N Engl J Med 2012;367:817–25. 10.1056/NEJMoa1204133 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2023-082141supp001.pdf (39.3KB, pdf)


