Understanding the synergies between mental and brain health
Mental health and brain health have often been treated as separate realms. Across a range of levels, including research and grant calls, education and training, awareness, prevention, interventions, hospital and governmental programs, multisectoral initiatives, and clinical assessments, these two domains are typically considered independently. This divide is undoubtedly rooted in historical schisms between psychiatry and neurology1.
However, the intricate blending of mental and brain health involves multiple shared pathways that influence psychiatric and neurological disorders. Recent evidence suggests that the etiology of psychiatric and neurodegenerative disorders, traditionally classified separately, may partially originate in early neurodevelopment2. Early life events can increase vulnerability to conditions like depression and anxiety, and diseases like Huntington’s may start during embryonic development. The discovery of induced pluripotent stem cells has highlighted molecular and synaptic commonalities between these disorders, further challenging their traditional classification.
The World Health Organization definitions of mental health and brain health share some common themes, emphasizing the importance of well-being, functioning, and realizing one’s potential in different aspects of life. And although a triangulation between psychiatric, neurological, and whole-body health dimensions is beyond the scope of this work, recent studies indicate that poor body health leaves a significant overlapping imprint on neuropsychiatric disorders3. By tackling the connections between our genes and epigenetics, the impact of environmental pollutants and social determinants, the cumulative burden of lifestyle choices across our lifespan, and the shared neurocognitive and pathophysiological features, we can unravel the complex interplay between these two fields4,5.This piece aims to shed light on the emerging interdisciplinary efforts to understand, prevent, and treat these multifaceted disorders.
From genes to epigenomics
From shared genes to epigenetics, numerous commonalities exist between psychiatric and neurological disorders. Shared genes increase the risk for both types of diseases, such as the CACNA1C gene, which is linked to bipolar disorder, schizophrenia, or epilepsy, among other conditions. Copy number variations (CNVs) are structural variations in the genome (duplication or deletion of large DNA segments) implicated in multiple diseases. For instance, the 22q11.2 deletion is associated with schizophrenia, intellectual disability, Attention Deficit Hyperactive Disorder (ADHD), or Parkinson’s disease (PD). Different polygenic risk scores (PRS) that combine multiple genetic variants overlap between disorders, such as schizophrenia and Alzheimer’s disease (AD). Additionally, the genetic risk for ADHD disorder can predict cognitive decline and the development of AD disease in older adults6.
Epigenetic modifications7 (e.g., DNA methylation that regulates when and how specific genes are activated or deactivated) have been implicated in psychiatric and neurological disorders. Epigenomics involves the comprehensive analysis of epigenetic changes across many genes within a cell or throughout an entire organism. Social epigenomics, which explores the link between global epigenetic changes and environmental disparities, has revealed common mechanisms across diseases. These include the influence of social environment and stress on mental health-related gene methylation and the role of environmental factors in neurodegeneration-linked mitochondrial changes. Thus, genetic commonalities between psychiatric and neurological disorders may be vital to develop a more integrated approach.
From the exposome to social determinants of health
The exposome, a composite exposure to various environmental factors8, influences numerous biological pathways often disrupted across metabolic, cancerous, psychiatric, and neurological conditions. For example, environmental pollutants (heavy metals, pesticides, air pollution) have been linked to an increased risk of ADHD, PD, and AD. Poor nutrition, characterized by high sugar and saturated fat consumption, elevates the risk of depression and cognitive decline. Low socioeconomic status is associated with a heightened risk of psychiatric and neurological disorders, including depression, cognitive decline, and various forms of dementia. Social determinants of health, such as poverty, social isolation, discrimination, minority communities, and limited access to healthcare systems, further increase the risk of disorders like depression, cognitive decline, dementia, and others8. These shared environmental factors highlight the need for a more dimensional and transnosological approach to mental and brain health.
Lifestyle choices across the lifespan
Lifestyle and related modifiable factors represent the cumulative burden across the lifespan that impacts mental and brain health4,5. Some of the most significant commonalities include physical inactivity, sleep disturbances, substance abuse, stress, and obesity, which are associated with multiple psychiatric and neurological outcomes, including depression, anxiety, and cognitive decline. For example, sleep disturbances can contribute to the onset of numerous psychiatric disorders and, based on epidemiological studies, is a decisive risk factor for developing PD9. Thus, lifestyle factors may highlight the importance of healthy lifestyle habits5 for promoting mental and brain health.
Social, affective, and cognitive impairments across diseases
Mental and brain health involve the harmonious coordination of cognitive, emotional, social, and behavioral functions5. Although neurocognitive deficits are commonly interpreted through disease-specific models, most diseases exhibit multiple cognitive deficits. It is difficult to attribute a single cognitive deficit exclusively to a particular brain dysfunction1,10,11. For instance, moral cognition deficits manifest in patients with various abnormalities and dysfunctions involving different genetic (i.e., Huntington’s disease), neuropsychiatric (i.e., autism), brain damage (i.e., frontal stroke), or hypometabolic (i.e., frontotemporal dementia)1 mechanisms. These suggest instantiations of the principle of degeneracy, where structurally different elements perform similar functions. In other words, diverse biological factors can lead to similar cognitive impairments across disorders.
Traditional neurocognitive theories often favor linear explanations, which fail to capture the dimensional complexity of psychiatric and neurological disorders10,11. Identifying cognitive commonalities may better reflect the underlying biology of these diseases. The Research Domain Criteria represent an initial attempt in psychiatry to promote the dimensional study of cognitive deficits across conditions4. Also, neurodegenerative disorders are classified based on specific proteinopathies and regional vulnerability, but symptoms commonly overlap. Cognitive sciences can benefit from more dimensional, transdiagnostic approaches to mental and brain disorders11,12.
Shared physiopathological mechanisms
Genes, the exposome, and lifestyle can increase the disease risk through multiple shared physiopathological pathways8 such as inflammation and neurotransmitter changes that impact neurological diseases (stroke, PD, AD) and psychiatric diseases (depression, schizophrenia)13. The emergence of omics biomarkers can revolutionize how we diagnose and understand multiple disorders. Microbiome, stress-related markers (i.e., oxidative stress, cortisol), astrocyte and microglia deficits, or deregulated insulin signaling represent other shared psychopathological processes across diseases12,13. These overlapping pathophysiological factors underscore the need for an integrated mental and brain health approach. This approach should consider transdiagnostic markers and numerous biological pathways for a personalized but dimensional clinical characterization12,13.
Computational neuroscience of mental and brain diseases
New models, such as predictive coding theories, allostatic overload, non-linear cascades, and synergistic approaches11,14, provide insights into the underlying mechanisms of mental and brain health and reveal how these pathophysiological features can be targeted for future dimensional interventions.
Predictive coding theories suggest that the brain constantly makes predictions about incoming sensory information and updates those predictions based on new information. Allostatic load refers to the cumulative wear and tear on the body and brain resulting from chronic environmental demands8, which helps understand various diseases. Predictive coding of allostatic interoception12 integrates the regulation of external demands with internal body signals, connecting multiple autonomic, biomarker, vascular, and brain measures of allostasis and interoception across psychiatric and neurological disorders11.
Computational synergetics combines computational modeling with experimental data to gain insights into the complex interactions between brain regions and systems14. By understanding the non-linear brain dynamics through hierarchy, synergy, and brain integration, these approaches can provide a more holistic, low-dimensional understanding of health and disease11. Similarly, these models allow for the integration of (a) external factors via order parameters; (b) genomic, transcriptomic, metabolomic, and proteomic influences at the organismic level; and (c) multimodal neuroimaging assessing different targets with spatial and temporal properties. Recent synergistic frameworks11,14 have been applied across various diseases, providing more dimensional mechanistic explanations.
These models are particularly relevant to a dimensional mental and brain health approach, as they allow for a more integrative understanding of the shared physiological mechanisms and brain dynamics underlying different psychiatric and neurological diseases. Such models, however, are highly dependent on data acquisition and analyses and can misclassify non-stereotypical samples. Thus, large multi-centric consortiums with standardized data collection, open code availability, and tailored-modeling must be a priority and can play a transformative role.
A call for a more integrated agenda
Recognizing the commonalities between these fields, including shared genetic, environmental, lifestyle factors, neurocognitive and pathophysiological pathways, is crucial for a more comprehensive approach to mental and brain health4,5. Considering the mental and brain health spectrum, more effective prevention and intervention strategies can be developed. Embracing dimensional and transdiagnostic principles can foster excellence in practice and counter the downsides of sub-specialization. Moreover, a more integrated approach can help break down the silos between different disciplines and fields, potentially leading to more innovative research, awareness, scientific diplomacy, and advocacy.
By working together across disciplines, we can achieve a more comprehensive and holistic understanding of mental and brain health and disease, which is critical for developing neurotechnologies. Similarly, by developing interventions that target shared neurocognitive mechanisms and reduce allostatic load, individuals may be able to reduce their risk of developing both these disorders. A call for more interdisciplinary, integrative, and multi-sectorial initiatives is essential to combine dimensional and transnosological approaches in research, prevention, clinical assessments, interventions, actionable policies, and strategies for reducing stigma and increasing awareness. This cooperation can help us better understand, prevent, and treat these multifaceted disorders, ultimately improving individual and societal outcomes. It is time to embrace a shared understanding of mental and brain health and disease.
Figure 1.
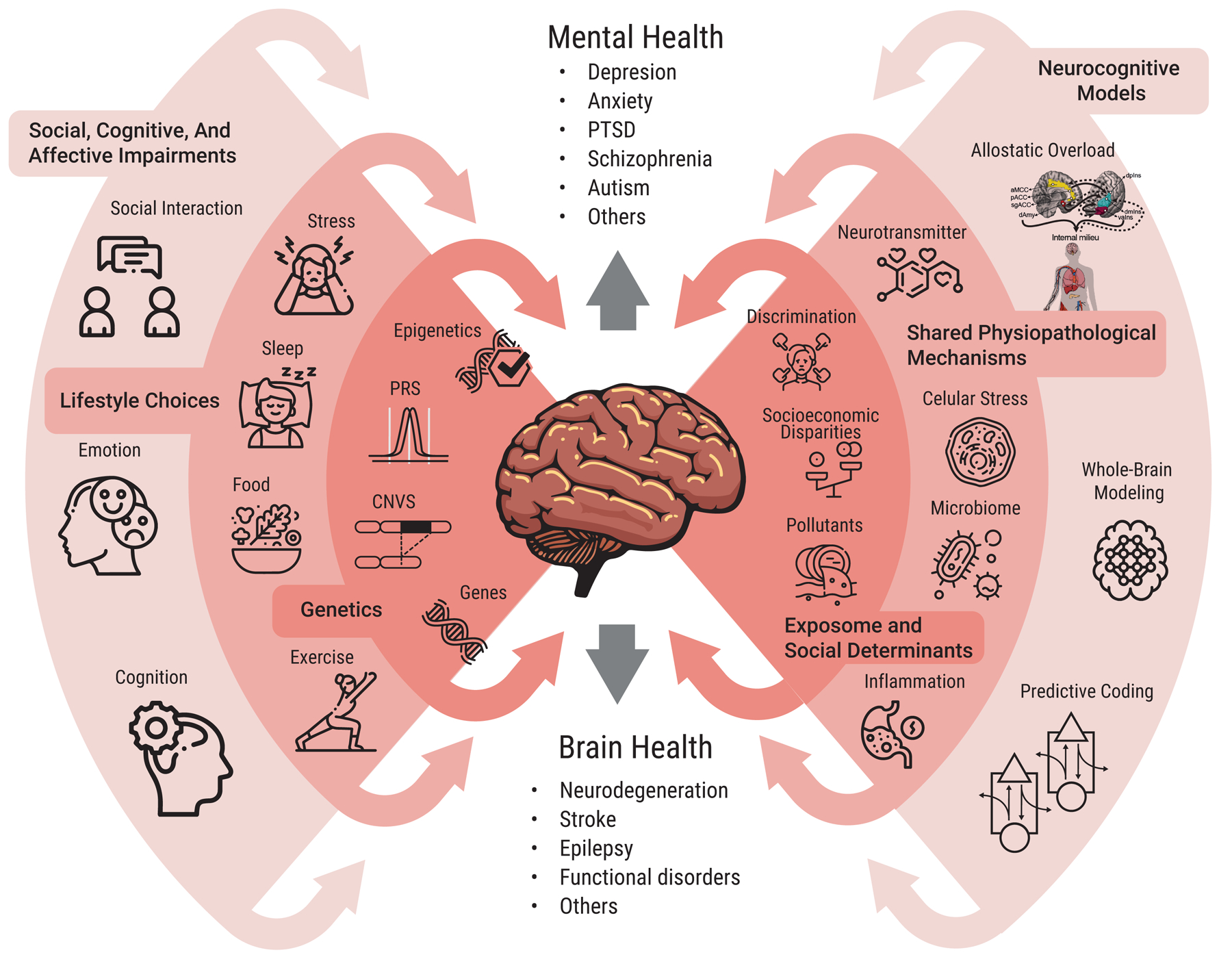
Common and interconnected levels of analysis across mental health and brain health fields and diseases. The circles illustrate the interlinked dimensions of mental and brain health, emphasizing the shared dimensions encompassing genetics, environmental exposome and social determinants, lifestyle choices, neurocognitive models, physiopathological mechanisms, as well as social, cognitive and affective impairments. This conceptual representation underscores the importance of considering these multiple shared processes in an interdisciplinary and integrative approach to understanding, preventing, and treating mental and brain disorders. Abbreviations: Copy number variations (CNVS), polygenic risk scores (PRS), post-traumatic stress disorder (PTSD).
Acknowledgments
Funding
Grants from Takeda CW2680521 partially support IA; ANID/FONDECYT Regular (1210195 and 1210176); ANID/FONDAP/15150012; and ReDLat, supported by the National Institutes of Health and the Fogarty International Center (FIC), National Institutes of Aging (R01 AG057234), Alzheimer’s Association (SG-20-725707), Rainwater Charitable Foundation - and Global Brain Health Institute)]. The contents of this publication are solely the author’s responsibility and do not represent the official views of these institutions.
Footnotes
This Comment highlights the intertwined nature of mental and brain health and disease. Common genetic, environmental, and lifestyle factors contribute to psychiatric and neurological disorders, which partially share neurocognitive and pathophysiological mechanisms. A call for a more dimensional, interdisciplinary approach can accelerate the development of robust approaches to research, prevention, and intervention.
Competing interests
The authors declare no competing interests.
References
- 1.Ibanez A, et al. World psychiatry : official journal of the World Psychiatric Association (WPA) 2014; 13(2): 148–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Thibaut F Dialogues in clinical neuroscience 2018; 20(4): 251–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tian YE, et al. JAMA Psychiatry 2023; 10.1001/jamapsychiatry.2023.0791. [DOI] [Google Scholar]
- 4.Craske MG, et al. Nature Mental Health 2023; 1(1): 12–24. [Google Scholar]
- 5.Avan A, Hachinski V. Alzheimer’s & dementia : the journal of the Alzheimer’s Association 2022; 18(7): 1396–407. [DOI] [PubMed] [Google Scholar]
- 6.Leffa DT, et al. Mol Psychiatry 2023; 28(3): 1248–55. [DOI] [PubMed] [Google Scholar]
- 7.Qureshi IA, Mehler MF. Handb Clin Neurol 2018; 147: 43–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vermeulen R, et al. Science 2020; 367(6476): 392–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hsiao YH, et al. J Sleep Res 2017; 26(5): 623–8. [DOI] [PubMed] [Google Scholar]
- 10.Ibanez A, et al. Social Neuroscience 2016; 10.1080/17470919.2016.1245214. [DOI] [Google Scholar]
- 11.Ibanez A Trends in cognitive sciences 2022; 26(12): 1031–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Migeot JA, et al. Trends Neurosci 2022; 45(11): 838–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Khansari PS, Sperlagh B. Inflammopharmacology 2012; 20(3): 103–7. [DOI] [PubMed] [Google Scholar]
- 14.Luppi AI, et al. Nat Rev Neurosci 2022; 23(12): 767–8. [DOI] [PubMed] [Google Scholar]


