Abstract
A high prevalence of proximal femoral metastases persists in patients with cancer, particularly regarding lower extremity fractures. This study offers a detailed analysis of clinical characteristics of patients undergoing surgical treatment for pathological or impending fractures, enhancing treatment strategies for metastatic malignancies. A total of thirty patients who underwent treatment of impending and pathological fractures at Kindai University Hospital (Osakasayama, Japan) were included. The retrospective study comprised parameters including age, sex, fracture site, type of primary malignancy, number of metastases, pre-fracture Eastern Cooperative Oncology Group performance status (ECOG-PS) score, adjuvant therapy, treatment modality, operative time, blood loss, postoperative complications, Musculoskeletal Tumor Society (MSTS) score, outcome and follow-up period. Post-treatment MSTS scores were compared in cases of impending and pathological fractures, and between intramedullary nailing and other surgical procedures. In addition, one-year postoperative survival rates were calculated. Furthermore, operative time, blood loss and survival rates were compared between impending and pathological fractures. The participants' median age was 70.5 years, with disease sites primarily in the subtrochanteric femur, trochanteric femur, femoral diaphysis, femoral neck and other locations. Pathologies included multiple myeloma and unknown primary, lung, breast, kidney, liver, gastric, esophageal and uterine cancers. The median ECOG-PS score pre-fracture was 2. Treatment approaches involved radiotherapy, chemotherapy and a combination of both. Surgical interventions included intramedullary nailing (16 cases), endoprosthesis (1 case), bipolar head replacement (3 cases) and compression hip screw (3 cases), among others. A negative correlation (R=-0.63) existed between MSTS and pre-fracture ECOG-PS scores. The operative time was significantly shorter in impending than in pathological fractures, with impending fractures showing significantly lower blood loss. The treatment algorithm for malignant bone tumors of the lower extremity provided in the present study was efficient, potentially optimizing treatment strategies for such cases, and contributing to improved patient care and outcomes in oncology and orthopedic surgery.
Keywords: pathological fractures, impending fractures, malignancy, bone tumor, surgical treatment
Introduction
Approximately 10% of patients with primary malignancies develop proximal femoral metastases (1). Bone metastases, originating mainly from breast, kidney, thyroid, prostate or myeloma cancers, are often soluble or mixed in nature, posing a high risk of pathological fractures to this patient population (2). A previous study published an algorithm for treating long bone and pelvic metastases. The patients were categorized into four classes: i) Isolated lesion with good prognosis; ii, pathological fractures; iii, incisional fractures; and iv), other lesions (3). Important factors influencing the choice of treatment for long bones and the pelvis include prognosis, disease type, visceral metastases, time from disease onset, risk of pathologic fracture, and sensitivity to chemotherapy, hormonal therapy and irradiation. The role of orthopedic surgeons in evaluating patients with skeletal metastases is expected to increase over time as improved cancer treatments enhance survival (4).
In addition, pathological fractures are 3.5 times more likely to occur in the proximal femur than in the proximal humerus (5). However, studies describing cases of pathological or impending fractures of the lower extremities in patients with primary and metastatic malignancies are currently lacking. Therefore, the present study aimed to provide a detailed description of the clinical characteristics of patients who underwent surgical treatment of pathological or impending fractures.
Patients and methods
Patients
The study included 30 patients with impending and pathological fractures treated at the Department of Orthopedic Surgery at Kindai University Hospital (Osakasayama, Japan) between January 2019 and November 2023. Inclusion and exclusion criteria: Included were cases treated at the clinic during the period for whom the course of treatment could be followed. Excluded were cases for which the course of treatment could not be traced. Diagnosis: Impending and pathological fractures were diagnosed based on the Mirels' score (6). Number of patients: Impending and pathological fractures were observed in 12 and 18 cases, respectively.
Parameters
The retrospective survey covered the following parameters: Age, sex, fracture site, types of primary malignancy, number of metastases, pre-fracture Eastern Cooperative Oncology Group performance status score (ECOG-PS) (7), adjuvant therapy, treatment modality, operative time, blood loss, postoperative complications, Musculoskeletal Tumor Society (MSTS) score (8), outcome and follow-up period. Analytical methods: Post-treatment MSTS scores between cases of impending and pathological fractures, as well as between cases treated with intramedullary nailing and those undergoing other surgical procedures, were also compared. The postoperative one-year survival rate was calculated using the Kaplan-Meier test. In addition, the operative time, blood loss and survival rates were compared between impending and pathological fractures.
Statistical analysis
Variables are presented as the mean ± standard deviation (S.D.). The MSTS scores of intramedullary nailing and other surgical procedures were compared using Student t-test. The ECOG-PS and MSTS scores were plotted and a correlation diagram was drawn. The coefficient of determination (R2) was calculated by drawing an approximation line to assess the correlation between ECOG-PS and MSTS scores. Pearson's correlation method was used to determine these correlations. The strength of the correlation was determined according to Pearson's correlation coefficient R as follows: Very strong, 1.0≥|R|≥0.7; strong, 0.7≥|R|≥0.5; moderate, 0.5≥|R|≥0.4; medium, 0.4≥|R|≥0.3; weak, 0.3≥|R|≥0.2; and no correlation, 0.2≥|R|≥0.0.
The operative time between impending and pathological fractures was compared using Student t-test. In addition, survival rates were compared between cases of impending and that of pathological fractures using Log-rank test. P<0.05 was considered to indicate statistical significance in all analyses. Analyses were performed using Stat Mate 5.05 (ATMS, Tokyo, Japan).
Results
Patient characteristics. The characteristics of the patients [including 13 male and 17 female participants; mean ± S.D. age, 70.5±9.82 (range, 47-83) years] are summarized in Table I and treatments were performed according to the algorithm depicted in Fig. 1.
Table I.
Characteristics of the study population (n=30).
| Factor | Value |
|---|---|
| Age, years | |
| Mean ± S.D. | 70.5±9.82 |
| ≤70 | 15(50) |
| >70 | 15(50) |
| Sex | |
| Male | 13(43) |
| Female | 17(57) |
| Fracture site | |
| Femoral neck | 5(17) |
| Femoral diaphysis | 5(17) |
| Intertrochanteric | 6(20) |
| Subtrochanteric | 10(33) |
| Bilateral intertrochanteric | 1(3) |
| Proximal tibia | 2(7) |
| Distal femur | 1(3) |
| Type of cancer | |
| Lung | 9(30) |
| Breast | 7(23) |
| Kidney | 3(10) |
| Multiple myeloma | 4(13) |
| Liver | 2(7) |
| Gastric | 2(7) |
| Unknown | 1(3) |
| Esophageal | 1(3) |
| Uterine | 1(3) |
| N. metastases | |
| ≤3 | 4(13) |
| >3 | 26(87) |
| ECOG-PS (mean) | 2 |
| <2 | 14(47) |
| 2-3 | 14(47) |
| >3 | 2(7) |
| Adjuvant therapy | |
| Radiotherapy | 2(7) |
| Chemotherapy | 15(50) |
| Chemotherapy and radiotherapy | 10(33) |
| None | 3(10) |
| Treatment modality | |
| Intramedullary nail | 16(53) |
| Endoprosthesis | 1(3) |
| Fixation with plate | 1(3) |
| Bipolar head arthroplasty | 3(10) |
| Fixation with CHS | 3(10) |
| Bilateral intermedullary nail | 2(7) |
| Conservative | 2(7) |
| Artificial bone stem | 1(3) |
| Rt. bipolar head arthroplasty, Lt. fixation with CHS | 1(3) |
| Operating time, min | |
| Total | 92.0±38.7 |
| Impending fractures | 83.1±21.9a |
| Pathological fractures | 113.8±44.3 |
| 0-100 | 17 |
| >100 | 11 |
| Blood loss, ml | |
| Total | 50.0 (20-447) |
| Impending fractures | 46.4 (20-435) |
| Pathological fractures | 132.6 (20-447) |
| 0-60 | 15 |
| >60 | 13 |
| MSTS score | |
| Intramedullary nailing | 19.9±8.8 |
| Other surgical procedures | 22.0±10.9 |
| 0-10 | 8(27) |
| 11-20 | 7(23) |
| 21-30 | 15(50) |
| Outcome | |
| AWD | 19(63) |
| DOD | 11(37) |
| Follow-up period, months | |
| Mean | 6.5 |
| Range | 1-150 |
Values are expressed as n (%), the mean ± S.D. or median (range).
aP<0.05 vs. pathological fractures. Rt, right side; Lt, left side; S.D., standard deviation; ECOG-PS, Eastern Cooperative Oncology Group score for performance status; CHS, compression hip screw; MSTS, Musculoskeletal Tumor Society; CDF, continuous disease-free; AWD, alive with disease; DOD, dead of disease.
Figure 1.
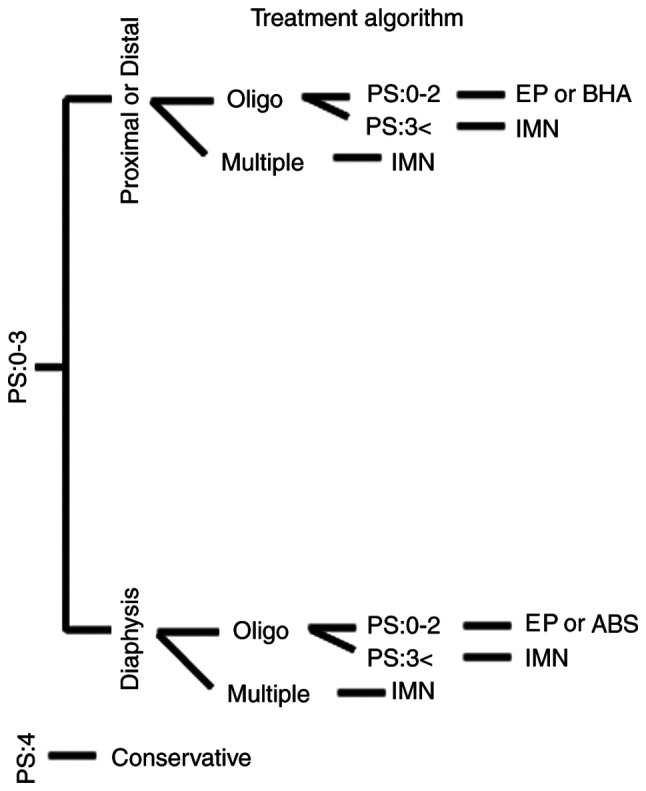
Tree diagram showing the treatment algorithm for lower leg malignancy at our hospital. Oligo, oligo metastasis in whole body; Multiple, multiple metastases in whole body; PS, performance status; EP, endoprosthesis; BHA, bipolar head arthroplasty; IMN, intermedullary nail; ABS, artificial bone stem.
As indicated in Table I, disease sites included the subtrochanteric region of the femur (n=10), intertrochanteric region of the femur (n=6), femoral diaphysis (n=5), femoral neck (n=5), bilateral intertrochanteric femoral region (n=1), proximal tibia (n=2) and distal femur (n=1). Pathological conditions included cases of lung cancer (n=9), breast cancer (n=7), kidney cancer (n=3), multiple myeloma (n=4), liver cancer (n=2), gastric cancer (n=2), unknown primary cancer (n=1), uterine cancer (n=1) and esophageal cancer (n=1). The number of metastases was ≤3 in 4 cases and >3 in 26 cases. The median ECOG-PS before fracture was 2 (range, 0-4; <2, n=20; 2-3, n=15; and >3, n=2 cases; Table I). Adjuvant therapy comprised radiotherapy in two cases, chemotherapy in 15 cases and a combination of radiotherapy and chemotherapy in 10 cases (Table I). Surgical procedures included intramedullary nailing (n=16), endoprosthesis (n=1), bipolar head arthroplasty (n=3), compression hip screw (CHS) (n=3), conservative treatment (n=2), bilateral intramedullary nailing (n=2), artificial bone stem (n=1), combined intramedullary nail and plate fixation (n=1), right-sided artificial head replacement (n=1) and left-sided CHS (n=1) (Table I).
Algorithm and planning
The algorithm was as follows: First, the ECOG-PS was determined. In cases of PS 4, conservative treatment was indicated; for PS 0-3, the fracture location was considered; and in addition, for PS 0-3, the number of metastases was focused on. In cases of distal or proximal involvement, the number of metastases was determined. In cases of multiple metastases, intramedullary nailing was considered. In cases of oligometastases and a PS of 3, intramedullary nailing was performed. In cases of oligometastases and a PS of 0-2, reconstruction with endoprosthesis or bipolar head arthroplasty was performed.
Similarly, in cases of PS of 0-3 in the diaphysis, the number of metastases was assessed. In cases of multiple metastases, intramedullary nailing was considered. In cases of oligo metastases and PS of 3, intramedullary nails were used. In cases of oligo metastases and PS of 0-2, reconstruction was performed using endoprosthesis or artificial bone stem. Furthermore, the procedure plan was decided by two oncologic surgeons (SN and KH).
Operating time, blood loss and score
The operating time (mean ± S.D.) was 92.0±38.7 min and the numbers of patients with operating times in different ranges were as follows: 0-100 min, n=17; and >100 min, n=11 cases. The mean blood loss was 50.0 (range, 20-447) ml as shown in Table I. The overall total MSTS score was 569. The MSTS score was as follows: 0-10, 8 cases; 11-20, 7 cases; and 21-30, 15 cases. In addition, the MSTS score was 19.9±8.8 for intramedullary nailing and 22.0±10.9 for other surgical procedures (P=0.23), as shown in Table I, with a negative moderate correlation between MSTS score and pre-fracture ECOG-PS (R=-0.63; Fig. 2).
Figure 2.
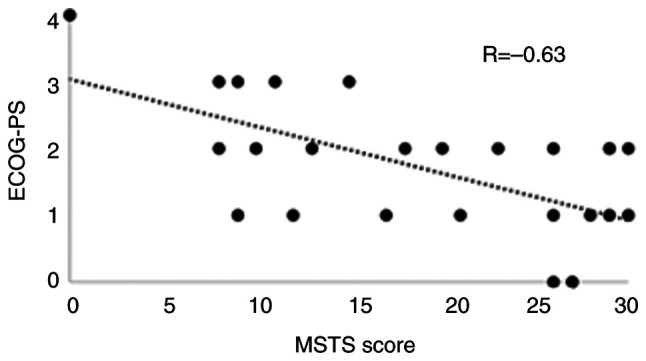
Graphs showing the negative correlation between the MSTS score and ECOG-PS (r=-0.63). ECOG-PS, Eastern Cooperative Oncology Group score for performance status; CHS, compression hip screw; MSTS, Musculoskeletal Tumor Society.
Complications and outcomes
Postoperative complications included one case of implant failure following the replacement of an intramedullary nail with an endoprosthesis. The median follow-up period was 6.5 (range, 1-150) months, with outcomes categorized as alive with disease in 19 cases and dead of disease in 11 cases, as shown in Table I. The one-year postoperative overall survival rate was 48.8% (Fig. 3).
Figure 3.
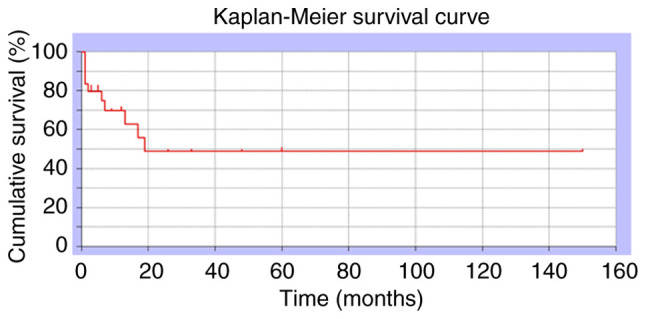
Kaplan-Meier curves showing the survival rate of all cases in the current study. The 1-year survival rate was 48.8%.
Comparison of impending fractures with pathological fractures
Furthermore, the operative time for patients with impending fractures was significantly shorter than that for patients with pathological fractures (83.1±21.9 vs. 113.8±44.3 min, respectively; P=0.015), as shown in Table I. The amount of blood loss was as follows: 0-60 ml, n=15 cases; and >60 ml, n=13 cases. The amount of blood loss [mean (range)] of patients with impending fractures and pathological fracture was 46.4 (20-435) and 132.6 (20-447) ml, respectively, as shown in Table I. No significant difference was observed in the 1-year survival between patients with incisional fractures and those with pathological fractures (54.6 and 43.6%, respectively; P=0.85) (Fig. 4).
Figure 4.
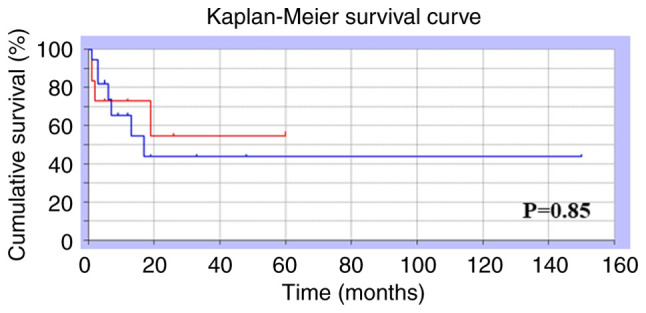
Comparison of survival rate among patients with impending fracture and pathological fracture. Kaplan-Meier curves for cases of impending fracture (red line) and pathological fracture (blue line). There was no significant difference in 1-year survival for patients with incisional fractures compared to those with pathological fractures (54.6 and 43.6%, respectively; P=0.85).
Discussion
In the present study, the treatment outcomes of pathological or impending fractures in metastatic bone tumors were investigated and an algorithm was generated, with generally favorable results. The most frequently reported sites of pathological fractures include the femur, spine and pelvis (9). The preferred sites of pathological fractures in the lower extremities were the femoral neck (50%), trochanter (30%) and subtrochanter (20%) (10). Other studies have reported 47.5% in the femoral head and neck, 27.5% in the femoral metaphyseal area and 25% below the femoral metaphyseal area (11). In the present study, the subtrochanteric and trochanteric areas were more common than the femoral neck area.
Previous studies have reported that the most common primary sites leading to pathological femoral fractures were multiple myeloma, breast, renal, colorectal, thyroid and lung cancers (1). Specifically, multiple myeloma, breast, lung and kidney cancers were the predominant primary lesions, resulting in pathological fractures of the proximal femur (9,11). Of note, lung cancer was relatively common in the present study, potentially reflecting the specialized treatments for lung cancer provided by our oncology department. Furthermore, patients with prostate cancer were not specifically excluded. Bone metastases from prostate cancer generally manifest as osteosclerosis, potentially contributing to the lower incidence of pathological fractures compared to lung and kidney cancer, which commonly result in osteolytic metastases.
Fractures of the lower extremities are clinically more important than those of the upper extremities because of their weight-bearing nature (9). Recommendations for the fixation of pathological fractures vary depending on the anatomical site (9). Regarding femoral head and neck fractures, treatment options include hemiarthroplasty, total hip arthroplasty, endoprosthesis, or plate or nail fixation with void filler. Cephalomedullary nailing is a recommended treatment for intertrochanteric, subtrochanteric and diaphyseal fractures. In cases of distal third femoral shaft fractures, the recommended treatments involve locking plates or retrograde intramedullary nails (with careful consideration by a musculoskeletal oncologist to avoid proximal tumor spread). For supracondylar fracture, the recommended treatment option is a distal femur periarticular plate. A locking plate or endoprosthesis is recommended for proximal tibia fixation, and intramedullary nails for tibial shafts.
Tumor arthroplasty offers advantages, such as rapid stability, independence from the degree of fracture healing and minimal risk of local progression or implant failure (12). However, it presents certain drawbacks, including greater surgical invasiveness, bleeding, relative difficulty in muscle reconstruction and higher costs (12). Intramedullary nails have the advantages of relatively low surgical invasion, the possibility of additional radiation therapy and the ability to support load immediately after radiation (12). Disadvantages of intramedullary nails include the need for adequate bone stock, instability near the joint and the risk of implant fracture (12). Alternatively, plate fixation provides benefits such as muscle cuff preservation, strong fixation with locking screws, fixation of distal fractures and a relatively large operative field allowing for visual resection of the tumor (12). Its disadvantages include the need for large incisions, longer surgical procedures and lack of prophylactic fixation of the entire bone (12). Intramedullary nails were used in the present study. Our approach involves reconstructing pathological fractures of the femoral neck using either artificial head replacement or tumor arthroplasty. The choice is based on tumor spread, prognosis, invasiveness and patient's rehabilitation potential, including load-bearing capacity. With regard to pathological fractures of the femoral condyle and the subtrochanteric region, reconstruction using an intramedullary nail was performed in anticipation of postoperative radiotherapy. Impending fractures of the femoral neck or transverse condyle were treated with bipolar head arthroplasty, intramedullary nails or CHS plates. The reconstruction method was selected based on a comprehensive evaluation of postoperative radiotherapy, fixation stability and the amount of lesion removed. Both types of fixation demonstrated generally good functional prognosis. However, poor prognosis was observed when rehabilitation did not progress as expected due to the patient's general condition.
In the present study, a protocol and treatment were followed that resulted in the predominant use of intramedullary nails. Previous studies have reported MSTS scores of 6.4-25.2 after implant use for pathological fractures (11-13). The findings of the present study align with, and corroborate the general recommendation of our surgical indications.
Complications have been reported in 9-20% of cases involving intramedullary nails (14,15). The primary complications include deep infection, myocardial infarction and stroke. In addition, 20% of patients require revision surgery within 3 months (16). By contrast, dislocation has been reported in 3-22% of cases as a complication of tumor arthroplasty (11,17). The risk of periprosthetic failure has also been reported (17-19). In the present study, implant failure occurred in one case of intramedullary nailing, which was subsequently replaced with an oncological prosthesis.
Typically, patients with metastatic bone tumors are in a terminal state (20,21). Regarding overall patient survival, the 1-year survival range is 42-75% (15,22,23). Fractures have been associated with an increased mortality risk in patients with malignant bone disease (24). Although the survival rate of patients with metastases remains low, advancements in medical treatment have led to certain differences in tumor histology. In this context, ‘improving the survival rate of the implant relative to the patient's lifespan’ is essential. Furthermore, appropriate treatment options should be selected with careful consideration of the patient's life expectancy.
Previously, patients with pathological fractures demonstrated similar morbidity and mortality rates to the non-pathological fracture cohort but exhibited higher rates of perioperative blood transfusions and unscheduled readmissions (25). In the present study, pathological fractures were associated with longer operative times and greater blood loss than incisional fractures. However, no significant difference was observed in survival rates. Therefore, treatment should be initiated prior to the occurrence of pathological fractures.
The present study has certain limitations. First, the sample size was small. However, no problems were encountered during the analyses. Second, it was a retrospective study. Finally, the follow-up period was relatively short. Despite these limitations, as many patients as possible were enrolled during the study period.
Mirels' classification, which has been the most commonly used thus far, assumes that a prognosis of at least 6 weeks is a prerequisite for surgery (26,27); however, our algorithm is different in that surgery can be indicated even when the prognosis is <6 weeks, which we consider novel. In fact, the present study included six cases with a prognosis of 1 month. Pathological fractures due to lower extremity malignancies are load-bearing bones, thereby causing severe activity of daily living (ADL) disability. Therefore, we think that our algorithm will prove beneficial in maintaining ADL at an ideal status until the patient's death.
In conclusion, oncologic surgeons must evaluate patients' PS and other systemic conditions, including age, life expectancy and presence of complications before considering the optimal reconstructive approach to the anatomic site to be treated.
Acknowledgements
Not applicable.
Funding Statement
Funding: No funding was received.
Availability of data and materials
The data generated in the present study may be requested from the corresponding author.
Authors' contributions
Conceptualization: KH, SN, TI and KG; methodology: KH, SN, TI, RK and KG; software: KH, RK and SN; validation: SN, NS, TI, RK and KG; formal analysis: SN, NS, TI and KG; investigation: KH, TI, RK and SN; data curation: KH, SN, TI, RK and KG; writing-original draft preparation: KH, SN, TI, RK and KG; writing-review and editing: KH, SN, TI, RK and KG. Checking and confirming the authenticity of the raw data: KH and KG. All authors have read and agreed to the published version of the manuscript.
Ethics approval and consent to participate
Ethical approval for this study was obtained from the Ethics Committee of Kindai University Hospital (Osaka, Japan; approval no. 31-153). Written informed consent was obtained from all participants included in the current study.
Patient consent for publication
Consent for publication was obtained from all participants included in the current study.
Competing interests
The authors declare that they have no competing interests.
References
- 1.Guzik G. Oncological and functional results after surgical treatment of bone metastases at the proximal femur. BMC Surg. 2018;18(5) doi: 10.1186/s12893-018-0336-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fontanella C, Fanotto V, Rihawi K, Aprile G, Puglisi F. Skeletal metastases from breast cancer: Pathogenesis of bone tropism and treatment strategy. Clin Exp Metastasis. 2015;32:819–833. doi: 10.1007/s10585-015-9743-0. [DOI] [PubMed] [Google Scholar]
- 3.Scorianz M, Gherlinzoni F, Campanacci DA. Metastases to the long bones: Algorithm of treatment. In: Management of Bone Metastases. Denaro V, Di Martino A and Piccioli A (eds). Springer, Cham, pp93-102, 2019. [Google Scholar]
- 4.Hage WD, Aboulafia AJ, Aboulafia DM. Incidence, location, and diagnostic evaluation of metastatic bone disease. Orthop Clin North Am. 2000;31:515–528. doi: 10.1016/s0030-5898(05)70171-1. [DOI] [PubMed] [Google Scholar]
- 5.Piccioli A, Spinelli MS, Maccauro G. Impending fracture: A difficult diagnosis. Injury. 2014;45 (Suppl 6):S138–S141. doi: 10.1016/j.injury.2014.10.038. [DOI] [PubMed] [Google Scholar]
- 6.Younis M, Barnhill SW, Maguire J, Pretell-Mazzini J. Management of humeral impending or pathological fractures with intramedullary nailing: Reaming versus non reaming technique-a retrospective comparative study. Musculoskelet Surg. 2022;106:35–41. doi: 10.1007/s12306-020-00668-6. [DOI] [PubMed] [Google Scholar]
- 7.Blagden SP, Charman SC, Sharples LD, Magee LR, Gilligan D. Performance status score: Do patients and their oncologists agree? Br J Cancer. 2003;89:1022–1027. doi: 10.1038/sj.bjc.6601231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Enneking WF, Dunham W, Gebhardt MC, Malawar M, Pritchard DJ. A system for the functional evaluation of reconstructive procedures after surgical treatment of tumors of the musculoskeletal system. Clin Orthop Relat Res. 1993;286:241–246. [PubMed] [Google Scholar]
- 9.Harrington KD. Orthopedic surgical management of skeletal complications of malignancy. Cancer. 1997;80 (Suppl 8):S1614–S1627. doi: 10.1002/(sici)1097-0142(19971015)80:8+<1614::aid-cncr12>3.3.co;2-0. [DOI] [PubMed] [Google Scholar]
- 10.Hu YC, Lun DX, Wang H. Clinical features of neoplastic pathological fracture in long bones. Chin Med J (Engl) 2012;125:3127–3132. [PubMed] [Google Scholar]
- 11.Angelini A, Trovarelli G, Berizzi A, Pala E, Breda A, Maraldi M, Ruggieri P. Treatment of pathologic fractures of the proximal femur. Injury. 2018;49 (Suppl 3):S77–S83. doi: 10.1016/j.injury.2018.09.044. [DOI] [PubMed] [Google Scholar]
- 12.Willeumier JJ, van der Linden YM, van de Sande MAJ, Dijkstra PDS. Treatment of pathological fractures of the long bones. EFORT Open Rev. 2016;1:136–145. doi: 10.1302/2058-5241.1.000008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Goryń T, Pieńkowski A, Szostakowski B, Zdzienicki M, Ługowska I, Rutkowski P. Functional outcome of surgical treatment of adults with extremity osteosarcoma after megaprosthetic reconstruction-single-center experience. J Orthop Surg Res. 2019;14(346) doi: 10.1186/s13018-019-1379-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wedin R, Bauer HC, Wersäll P. Failures after operation for skeletal metastatic lesions of long bones. Clin Orthop Relat Res. 1999;358:128–139. [PubMed] [Google Scholar]
- 15.Wedin R, Bauer HC. Surgical treatment of skeletal metastatic lesions of the proximal femur: Endoprosthesis or reconstruction nail? J Bone Joint Surg Br. 2005;87:1653–1657. doi: 10.1302/0301-620X.87B12.16629. [DOI] [PubMed] [Google Scholar]
- 16.Jacofsky DJ, Haidukewych GJ, Zhang H, Sim FH. Complications and results of arthroplasty for salvage of failed treatment of malignant pathologic fractures of the hip. Clin Orthop Relat Res. 2004;427:52–56. doi: 10.1097/01.blo.0000143572.96021.93. [DOI] [PubMed] [Google Scholar]
- 17.Moore J, Isler M, Barry J, Mottard S. Major wound complication risk factors following soft tissue sarcoma resection. Eur J Surg Oncol. 2014;40:1671–1676. doi: 10.1016/j.ejso.2014.10.045. [DOI] [PubMed] [Google Scholar]
- 18.Piccioli A, Rossi B, Scaramuzzo L, Spinelli MS, Yang Z, Maccauro G. Intramedullary nailing for treatment of pathologic femoral fractures due to metastases. Injury. 2014;45:412–417. doi: 10.1016/j.injury.2013.09.025. [DOI] [PubMed] [Google Scholar]
- 19.Dunn J, Kusnezov N, Bader J, Waterman BR, Orr J, Belmont PJ. Long versus short cephalomedullary nail for trochanteric femur fractures (OTA 31-A1, A2 and A3): A systematic review. J Orthop Traumatol. 2016;17:361–367. doi: 10.1007/s10195-016-0405-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Roudier MP, True LD, Higano CS, Vesselle H, Ellis W, Lange P, Vessella RL. Phenotypic heterogeneity of end-stage prostate carcinoma metastatic to bone. Hum Pathol. 2003;34:646–653. doi: 10.1016/s0046-8177(03)00190-4. [DOI] [PubMed] [Google Scholar]
- 21.Ganesh K, Massagué J. Targeting metastatic cancer. Nat Med. 2021;27:34–44. doi: 10.1038/s41591-020-01195-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mavrogenis AF, Pala E, Romagnoli C, Romantini M, Calabro T, Ruggieri P. Survival analysis of patients with femoral metastases. J Surg Oncol. 2012;105:135–141. doi: 10.1002/jso.22061. [DOI] [PubMed] [Google Scholar]
- 23.Chandrasekar CR, Grimer RJ, Carter SR, Tillman RM, Abudu A, Buckley L. Modular endoprosthetic replacement for tumours of the proximal femur. J Bone Joint Surg Br. 2009;91:108–112. doi: 10.1302/0301-620X.91B1.20448. [DOI] [PubMed] [Google Scholar]
- 24.Saad F, Lipton A, Cook R, Chen YM, Smith M, Coleman R. Pathologic fractures correlate with reduced survival in patients with malignant bone disease. Cancer. 2007;110:1860–1867. doi: 10.1002/cncr.22991. [DOI] [PubMed] [Google Scholar]
- 25.Boddapati V, Held MB, Levitsky M, Charette RS, Neuwirth AL, Geller JA. Risks and complications after arthroplasty for pathological or impending pathological fracture of the hip. J Arthroplasty. 2021;36:2049–2054.e5. doi: 10.1016/j.arth.2021.02.004. [DOI] [PubMed] [Google Scholar]
- 26.Errani C, Mavrogenis AF, Cevolani L, Spinelli S, Piccioli A, Maccauro G, Baldini N, Donati D. Treatment for long bone metastases based on a systematic literature review. Eur J Orthop Surg Traumatol. 2017;27:205–211. doi: 10.1007/s00590-016-1857-9. [DOI] [PubMed] [Google Scholar]
- 27.Mirels H. Metastatic disease in long bones. A proposed scoring system for diagnosing impending pathologic fractures. Clin Orthop Relat Res. 1989;249:256–264. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data generated in the present study may be requested from the corresponding author.


