Abstract
Residential biomass burning is an important source of black carbon (BC) exposure among rural communities in low- and middle-income countries. We collected 7165 personal BC samples and individual/household level information from 3103 pregnant women enrolled in the Household Air Pollution Intervention Network trial. Women in the intervention arm received free liquefied petroleum gas stoves and fuel throughout pregnancy; women in the control arm continued the use of biomass stoves. Median (IQR) postintervention BC exposures were 9.6 μg/m3 (5.2–14.0) for controls and 2.8 μg/m3 (1.6–4.8) for the intervention group. Using mixed models, we characterized predictors of BC exposure and assessed how exposure contrasts differed between arms by select predictors. Primary stove type was the strongest predictor (R2 = 0.42); the models including kerosene use, kitchen location, education, occupation, or stove use hours also provided additional explanatory power from the base model adjusted only for the study site. Our full, trial-wide, model explained 48% of the variation in BC exposures. We found evidence that the BC exposure contrast between arms differed by study site, adherence to the assigned study stove, and whether the participant cooked. Our findings highlight factors that may be addressed before and during studies to implement more impactful cookstove intervention trials.
Keywords: household air pollution, exposure assessment, exposure models, intervention, black carbon (BC), biomass fuel stoves, liquefied petroleum gas, Guatemala, India, Peru, Rwanda
Short abstract
Our study adds to the scientific discourse on understanding and mitigating black carbon exposures in resource-constrained settings.
Introduction
Approximately 2.3 billion people are exposed to household air pollution due to the residential combustion of polluting biomass fuels (e.g., wood, dung, charcoal), coal, and kerosene used for household energy needs.1 Exposure to household air pollution ranks among the top risk factors contributing to the global burden of disease and accounted for 2.3 million deaths and more than 90 million disability-adjusted life years (DALYs) in 2019 with disproportionate adverse health effects in low- and middle-income countries (LMICs).2 Health outcomes associated with household air pollution include adverse respiratory (acute respiratory infection in both adults and children, chronic obstructive pulmonary disease, and lung cancer), cardiovascular (cerebrovascular disease, ischemic heart disease, and cardiovascular mortality), and birth (low birth weight and small for gestational age) outcomes.3−11
Household air pollution is primarily characterized via measurements of particulate matter with an aerodynamic diameter of ≤2.5 μm (PM2.5) and carbon monoxide (CO).12 PM2.5 is a heterogeneous chemical mixture containing elemental carbon (EC), commonly referred to as black carbon (BC), organic carbon (OC), polycyclic aromatic hydrocarbons (PAHs), and various metal species.13 BC, the most light-absorbing portion of PM2.5, is a byproduct of incomplete combustion and is therefore a more specific marker of combustion-related sources than PM2.5 alone. BC has been gaining attention due to its global warming potential14 and its associations with adverse health effects.15,16 Residential biomass burning is the top-ranked source of BC globally (∼35%) with increasing emissions17 due to growing rural populations in LMICs.18 More studies of BC in LMICs are needed to better gauge its contribution to adverse climate impacts and human health.
To date, BC remains largely understudied in settings where polluting fuels are used for daily cooking. The majority of epidemiology studies linking BC to health outcomes have been conducted in Europe and North America.19,20 Many health and exposure studies in LMICs have reported the effectiveness of cookstove interventions in providing meaningful health benefits or reductions in exposure to household air pollution.21−27 Few cookstove intervention trials have assessed personal BC exposures.23,28,29
While several space- and time-dependent factors potentially impact PM2.5 exposures due to household air pollution (e.g., stove type, kitchen location, time spent cooking), little is known about how these factors are associated with personal BC exposures.30 Findings from a global exposure assessment of 2541 households across 8 LMICs from the PURE-AIR cohort suggest that BC concentrations vary according to study site and primary and secondary cooking fuels used.31 A more comprehensive assessment of 870 individuals from the PURE-AIR cohort found that stove and fuel type, hours spent cooking, and having a window in the kitchen were important factors influencing personal BC exposure.32 The study did not collect longitudinal data nor did it address potentially substantial contributions from kerosene used for lighting.32 Other studies of BC exposures among individuals in LMICs identified roof type, number of bedrooms, ventilation, heating and lighting fuel, kitchen type, temperature, and ambient air pollutant concentrations to be significant predictors of personal BC, though these studies are cross-sectional and/or limited in their geographical scope.33−35 There is a need for longitudinal analyses across multiple settings to fully elucidate how space- and time-dependent factors impact BC exposures in resource-limited settings where exposure to household air pollution is substantial.
The Household Air Pollution Intervention Network (HAPIN) randomized controlled trial provided liquefied petroleum gas (LPG) stoves and continuous free fuel distribution in four LMICs.36 Details on personal exposures to PM2.5, BC, and CO among pregnant women in the HAPIN trial, both overall and by intervention arm and study site, have been published previously.37 Here, we explore the association between BC exposure and a variety of household characteristics, participant practices, and other factors assessed at baseline and follow-up visits. To complement this analysis, we also evaluate how select factors potentially modified the effectiveness of the LPG intervention in reducing personal BC exposures in the HAPIN trial.
Methods
Study Setting
The HAPIN study (registration NCT02944682) was a randomized controlled trial evaluating the health effects of an introduced LPG stove and free fuel intervention versus the continued use of traditional cookstoves in Guatemala, India, Peru, and Rwanda.36 In each study site, ∼800 households were enrolled totaling 3195 pregnant women (aged 18–35 years) randomized to either control or intervention arm.36 As part of HAPIN, we analyzed 24 h personal BC exposures from the 3103 (97%) pregnant women with at least one valid measurement (n = 7,165 BC measures) across the four study sites.
HAPIN specifically chose rural communities without other major ambient air pollution sources and a high proportion of homes that typically use traditional biomass cookstoves for cooking and heating purposes to reflect locations where a household air pollution intervention would be expected to provide maximum exposure reductions. Details regarding study site characteristics, inclusion and exclusion criteria, and overall study design are described elsewhere.36,38 Pregnancy-related exposures as well as details on total versus valid samples collected during pregnancy are reported in our previous work.37 We provide a brief description of the HAPIN exposure sampling plan during pregnancy below.
Exposure Measurement
24 h average exposure measurements were conducted three times during pregnancy. Baseline measures were collected at 9–20 weeks of gestation before the LPG stove was introduced. Two follow-up measurements were made at 24–28 (postintervention visit 1) and 32–36 (postintervention visit 2) weeks of gestation. At each visit, participants were asked to wear customized vests or aprons fitted with an air-monitoring instrument near their breathing zone. If participants were to conduct activities that could damage the equipment, they were asked to remove the vest but keep it nearby (within 1–2m). Wearing compliance for our study participants was reported in our previous work.37
PM2.5 was collected using the RTI Enhanced Children’s MicroPEM (ECM, RTI International, Research Triangle Park). The ECM uses a 2.5 μm size-cut impactor at a flow rate of 0.3 L/min to collect gravimetric samples on 15 mm poly(tetrafluoroethylene) (Teflon) filters (Measurement Technology Laboratories). The ECM also logs temperature, relative humidity, and triaxial accelerometry.
BC concentrations from PM2.5 filter samples were estimated using the Sootscan Model OT21 Optical Transmissometers (Magee Scientific) at either the University of Georgia (UGA, Athens, GA), for samples collected in Guatemala, Peru, and Rwanda, or at Sri Ramachandra Institute for Higher Education and Research (SRIHER, Chennai, India), for samples collected in India. We measured the optical transmittance of filters and compared the intensity of light through a postsampled and reference filter. Over 97% of the reference filters, at UGA, were the presampled filters themselves, while at SRIHER, the reference filter was a blank laboratory filter.37
To estimate BC concentrations, we used an equation derived from Presler-Jur et al., 2017 that measures particle light absorption (eq 1):
| 1 |
Here, [BC] is the BC mass concentration, I0 is the intensity of light through a reference filter, I is the intensity of light through a postsampled filter, A is the area of the filter, V is the air sample volume, and σ is the attenuation cross section. This equation relates absorbance and mass content. We used the attenuation cross section value reported in Garland et al., 2017 (σ = 13.7 μg/cm2) for Teflon filters collected from similar source types.
Data Collection on Individual and Household Characteristics
At the baseline visit, trained local field technicians administered questionnaires to assess baseline participant characteristics (e.g., age, family size, and access to electricity) and sources of household exposures (e.g., primary stove and fuel types used for cooking, heating, and lighting). At all exposure visits, including at baseline, technicians also collected information regarding behavioral practices that occurred during the prior 24 h sampling period (e.g., whether the participant cooked or not, stove and fuels used, any use of kerosene, self-reported hours of primary stove use, etc.) as well as additional household characteristics such as food insecurity, kitchen location, roof type, and the self-reported smoke from a source other than the participant’s stove. Primary stove types were categorized as open fires or LPG stoves, chimney stoves, or other improved biomass stoves such as portable biomass stoves, comals (i.e., smooth, flat griddles typically used in Central America), charcoal-burning Imbabura stoves, and wood-burning Rondereza stoves. Our questionnaires were not specific enough for us to discern whether kerosene fuel was used explicitly for lighting or cooking activities during the sampling period. Seasonality was dichotomized into dry and rainy seasons according to the respective climate and weather patterns in Guatemala,40 India,41 Peru,42 and Rwanda.43 More in-depth descriptions of individual and household characteristics are provided in Text S1.
Statistical Analysis
We conducted a descriptive analysis of the study population at baseline. Summary statistics for BC exposures according to select combustion-related factors expected and postintervention BC exposures among the control and intervention groups are provided in the Supporting Information. For all further analyses via linear models, we natural log-transformed BC exposures to meet regression assumptions. We conducted all analyses in R (versions 3.6 and 4.0, R Foundation for Statistical Computing, Vienna, Austria).
To assess the association between covariates and personal BC, we employed a series of linear mixed-effects models with random intercepts for participants to account for the correlation of repeated measurements made on the same participant. We ran mixed models for all HAPIN measures (adjusting for study site) and for each study site separately to look at univariate associations between covariates and exposure; results are provided in Supporting Information (eq 2). Here, yij is the jth measurement of BC for participant i; β0 is the overall intercept (mean); β1 is the coefficient for the study site adjustment (not included in the site-specific models); β2 is the coefficient for the covariate (X2) of interest in the model; αi is the random intercept for participant i; and εij is the random error. These models assume that αi and εij are independent and normally distributed with variances σ2b (i.e., variance between individuals) and σ2w (i.e., variance within individuals), respectively. HAPIN-wide bivariate models where the marginal R2 values are greater than that from the HAPIN-wide univariate study site model show instances where a covariable provided additional explanatory power. We then ran multivariable mixed-effects regression analyses to assess this relationship after adjusting for other model covariates (eq 3). Covariates were selected to be included in the model using a backward stepwise regression procedure that eliminated nonsignificant (p > 0.05) variables. A brief description of our analysis with imputed missing questionnaire data is provided in Text S2.
| 2 |
| 3 |
All models were constructed, selected, validated, and analyzed using the lme444 and sjPlot45 packages in R. Additionally, for each model, we estimated the root-mean-square error (RMSE) with the rmse46 package in R and obtained the marginal R2 value and intraclass correlation (ICC) using the sjPlot45 package in R. We calculated the RMSE as a metric for the absolute fit of the model to the data by taking the square root of the average of the squared residuals. The marginal R2 value represents the proportion of the variance in personal BC explained only by the fixed effects of the predictors included in the model. We determined the ICC, conditional on the predictors in the model, by estimating the proportion of the total variance in personal BC attributable to the variance between participants (eq 4).
| 4 |
We constructed linear mixed-effects models with an interaction term between the arm and all covariates included in the full models to assess which predictors potentially modified the effectiveness of the intervention (eq 5). Parameters with significant interaction coefficients were deemed to show potential effect modification. Next, we evaluated each predictor with significant interaction coefficients, separately, after controlling for all other covariates found to be associated with personal BC in previous models (eq 6). Although not completely comparable to BC exposure contrasts between arms reported in Johnson et al.,37 which only controlled for study site in the HAPIN-wide model, deviations from Johnson et al.37 results show how select predictors potentially modified the effect of the intervention in reducing exposures to BC. We used the emmeans package in R to compute and compare the marginal means in each sublevel of the treatment arm.47 For this analysis, we categorized self-reported stove use hours and relative humidity by quantile (i.e., ≤25th percentile, middle 50%, ≥75th percentile) and replaced primary stove type with a dichotomous indicator for adherence to the stove assignment in each treatment arm. Participants in the control and intervention arms adhered to the stove assignment if they, respectively, used a biomass or LPG stove as their primary stove.
| 5 |
| 6 |
Results
Summary of Study Population
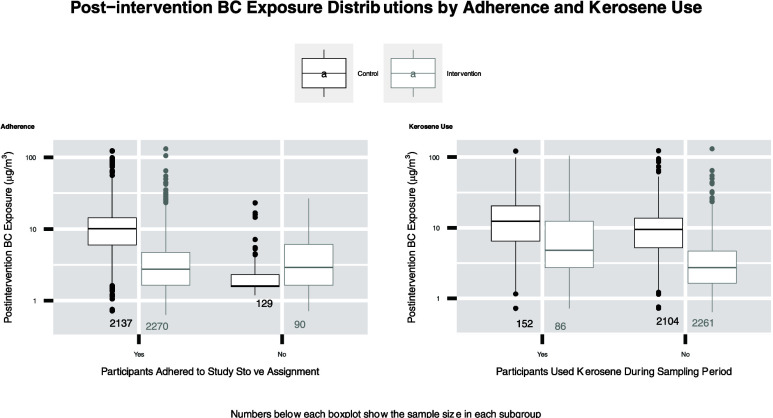
Baseline participant and household characteristics are provided in Table 1. The majority (70%) of our participants ranged in age from 20 to 29 years. Wood was the predominant cooking fuel used at baseline in Guatemala (99%) and India (100%). Cow dung was the most common cooking fuel used in Peru (87%); in Rwanda, participants used both wood (73%) and charcoal (25%). Electricity was the predominant primary lighting source in all study sites except for Rwanda where only 28% of the participants used electricity as their primary lighting source. Summary statistics for personal BC measurements overall and by select combustion-related factors are provided in Table S1. The majority of our 7165 personal BC measures were from participants using either open fires (49%) or LPG stoves (34%) as their primary stove type. Overall, the median (IQR) BC exposure level was 7.1 μg/m3 (2.9–12.6), and exposures ranged from 0.6 to 132.6 μg/m3. After restricting the data to postintervention study visits, median (IQR) BC exposures were 9.6 μg/m3 (5.2–14.0) and 2.8 μg/m3 (1.6–4.8) in the control and intervention arms, respectively (Table S2). Our complete data set, comprising both questionnaire/field observation and exposure data, includes approximately 81% (n = 5791) of our total BC measures. We have missing data for kitchen volume (13%), roof material (12%), wall material (12%), temperature and relative humidity (5%), hours of self-reported stove use during the 24 h sampling period (2%), food security (2%), kitchen location (2%), participant occupation (<1%), other sources of smoke (1%), lighting fuel (<1%), fuel type (<1%), and kerosene use (<1%) (Figure S1).
Table 1. Summary of Baseline Participant and Household Characteristics of the 3103 Women Included in the Study.
| HAPIN | Guatemala | India | Peru | Rwanda | ||
|---|---|---|---|---|---|---|
| characteristic | category | N (%) | N (%) | N (%) | N (%) | N (%) |
| total | 3103 (100%) | 791 (100%) | 787 (100%) | 753 (100%) | 772 (100%) | |
| age | <20 | 388 (13%) | 119 (15%) | 126 (16%) | 94 (12%) | 49 (6%) |
| 20–24 | 1161 (37%) | 320 (40%) | 380 (48%) | 264 (35%) | 197 (26%) | |
| 25–29 | 979 (32%) | 226 (29%) | 223 (28%) | 245 (33%) | 285 (37%) | |
| 30–35 | 568 (18%) | 122 (15%) | 58 (7%) | 149 (20%) | 239 (31%) | |
| primary cooking fuel | charcoal | 190 (6%) | 190 (25%) | |||
| cow dung | 656 (21%) | 656 (87%) | ||||
| other | 30 (1%) | 3 (0%) | 9 (1%) | 18 (2%) | ||
| wood | 2220 (72%) | 784 (99%) | 787 (100%) | 87 (12%) | 562 (73%) | |
| missing | 7 (0%) | 4 (1%) | 1 (0%) | 2 (0%) | ||
| primary lighting source | electricity | 2362 (76%) | 697 (88%) | 757 (96%) | 688 (91%) | 220 (28%) |
| kerosene lamp | 81 (3%) | 6 (1%) | 16 (2%) | 1 (0%) | 58 (8%) | |
| other | 179 (6%) | 72 (9%) | 30 (4%) | 77 (10%) | ||
| solar light | 275 (9%) | 2 (0%) | 3 (0%) | 22 (3%) | 248 (32%) | |
| torch (battery) | 199 (6%) | 10 (1%) | 11 (1%) | 11 (1%) | 167 (22%) | |
| participant’s occupation | agriculture | 1479 (48%) | 6 (1%) | 333 (42%) | 568 (75%) | 572 (74%) |
| commercial | 126 (4%) | 17 (2%) | 4 (1%) | 23 (3%) | 82 (11%) | |
| household | 1335 (43%) | 733 (93%) | 425 (54%) | 121 (16%) | 56 (7%) | |
| other | 154 (5%) | 29 (4%) | 25 (3%) | 40 (5%) | 60 (8%) | |
| missing | 9 (0%) | 6 (1%) | ||||
| family size | small (≤4) | 1994 (64%) | 386 (49%) | 572 (73%) | 386 (49%) | 617 (80%) |
| medium (5–9) | 1022 (33%) | 340 (43%) | 212 (27%) | 340 (43%) | 148 (19%) | |
| large (>10) | 79 (3%) | 61 (8%) | 3 (0%) | 61 (8%) | 5 (1%) | |
| missing | 8 (0%) | 4 (1%) | ||||
| household food insecurity | none | 1743 (56%) | 435 (55%) | 634 (81%) | 388 (52%) | 286 (37%) |
| mild | 835 (27%) | 249 (31%) | 113 (14%) | 259 (34%) | 214 (28%) | |
| moderate/severe | 474 (15%) | 93 (12%) | 36 (5%) | 95 (13%) | 250 (32%) | |
| missing | 51 (2%) | 14 (2%) | 4 (1%) | 11 (1%) | 22 (3%) | |
| participant’s education | no complete formal education | 804 (32%) | 311 (46%) | 235 (34%) | 24 (4%) | 234 (41%) |
| primary school complete | 861 (34%) | 268 (40%) | 195 (28%) | 168 (28%) | 230 (40%) | |
| secondary school or equivalent complete | 873 (34%) | 95 (14%) | 269 (38%) | 404 (68%) | 105 (18%) | |
| missing | 1 (0%) | 1 (0%) | 0 (0%) | 0 (0%) | 0 (0%) |
Major Predictors of Black Carbon Exposures
HAPIN-wide (adjusted for study site) and site-specific associations between personal BC and single household, individual, and environmental characteristics, unadjusted for other covariates, are provided in Table S3. Primary stove type and study site explained the most variation in personal BC among all other covariates in our HAPIN-wide analysis (R2 = 0.42), and stove type remained important in each site-specific model (R2 range 0.36–0.48). The HAPIN-wide models including kerosene use, kitchen location, participant occupation, participant education, and stove use hours provided additional explanatory power compared to the model including only the study site with R2 values ranging from 0.09 to 0.1. Fuel type had considerable explanatory power at baseline in Rwanda (R2 = 0.21) where charcoal users had lower (−48, 95% CI: −52, −41) BC exposures than wood users. However, in Peru, there was no significant difference in BC exposures among wood and cow dung users at baseline.
HAPIN-wide multivariable mixed regression coefficients between personal BC and select factors are provided in Figure 1; site-specific coefficients are provided in Figures S2–S5. We observed variation between study sites as BC exposures were lower in India (−22, 95% CI: −29, −14) and Peru (−52, 95% CI: −57, −46), compared to Guatemala. However, the most variation in BC exposures was observed as an exposure gradient according to the primary stove and fuel types: compared to traditional open fires, BC was lower for LPG (−70, 95% CI: −72, −69), followed by other improved biomass stoves (−29, 95% CI: −35, −24), and chimney stoves (−20, 95% CI: −27, −13), respectively. Additionally, participants with secondary LPG (−12, 95% CI: −21, −3) or biomass (10, 95% CI: 3, 17) stoves had lower and higher BC exposures than those with no secondary stoves, respectively. General use of kerosene was associated with an increase (49, 95% CI: 38, 60) in personal BC across HAPIN and was included in each site-specific model except Peru, which had minimal kerosene users. In these models, any kerosene use, versus no use of kerosene, was associated with an increase in personal BC in Guatemala (22, 95% CI: 1, 48), India (50, 95% CI: 36, 65), and Rwanda (63, 95% CI: 39, 92). Kerosene lamp users had 32% (95% CI: 14, 52) higher BC exposures than those that used electricity for lighting. Another combustion-related variable impacting BC exposures was self-reported smoke from a neighbor’s kitchen, which was associated with elevated BC exposures (14, 95% CI: 6, 23) compared to when no other sources of outside smoke were reported.
Figure 1.
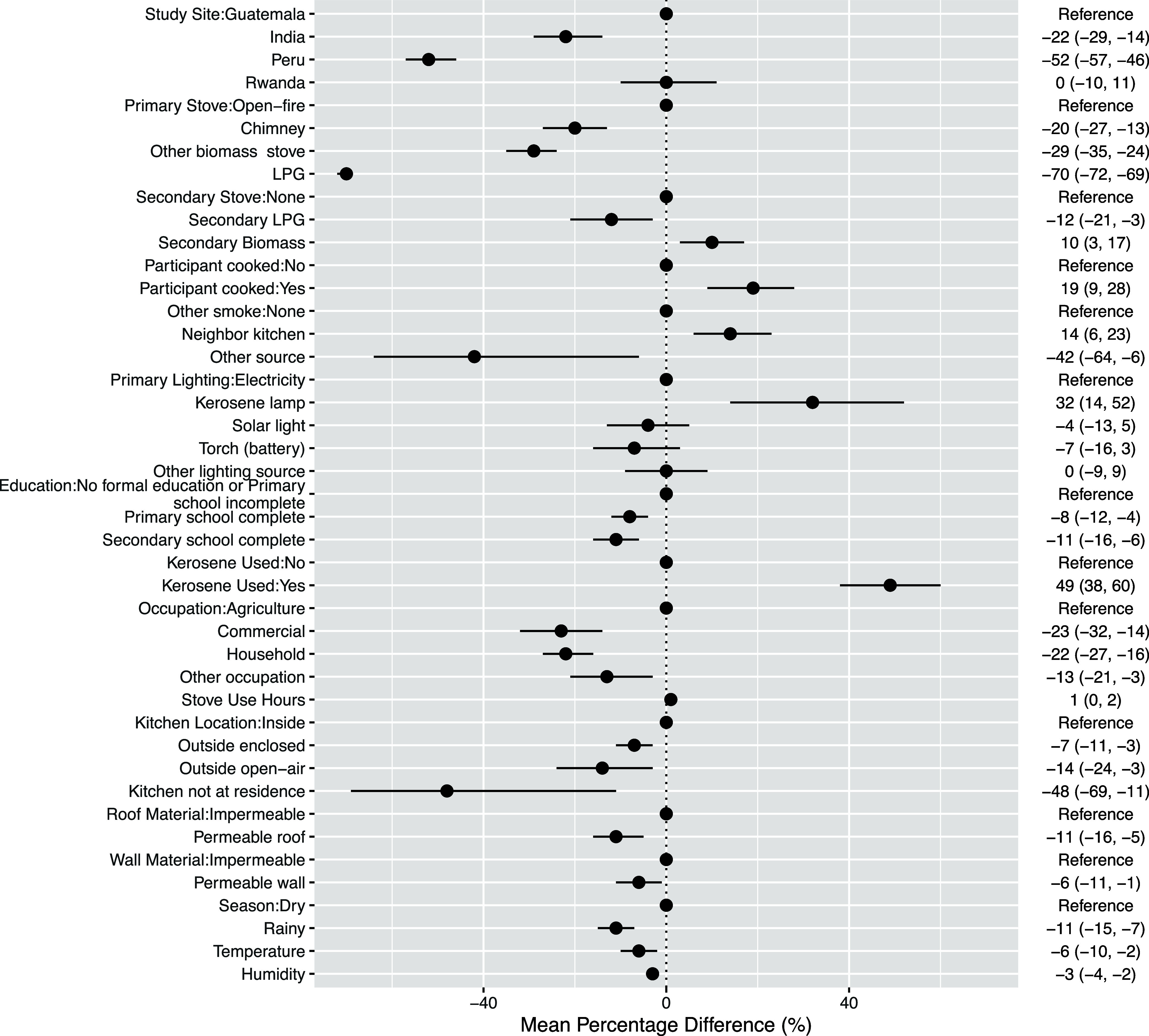
HAPIN-wide multivariable mixed-effects regression coefficients (with 95% confidence intervals). Numeric coefficients represent the mean percentage change of the geometric mean in BC exposure compared to the reference category based on the final multivariable linear regression models. Coefficients for relative humidity and kitchen volume represent a 5 unit increase in percentage and 10 unit increase in volume, respectively.
We also observed associations between personal BC and other individual and household characteristics as well as environmental conditions. We observed an exposure gradient according to kitchen location: compared to participants with kitchens located inside the home, BC exposures were lower for those with outside enclosed kitchens (−7, 95% CI: −11, −3), outside open-air kitchens (−14, 95% CI: −24, −3), and kitchens that were not located at the residence (−48, 95% CI: −69, −11) respectively. Participants who worked either in the household (−22, 95% CI: −27, −16) or as vendors (−23, 95% CI: −32, −14) had lower BC exposures compared to those working in agriculture. Participants with permeable roof (−11%, 95% CI: −16, −5) and wall (−6, 95% CI: −11, −1) materials had lower BC exposures than those with impermeable roof and wall materials. Each additional hour of stove use was positively associated with personal BC (1, 95% CI: 0, 2). BC exposures were found to be lower for participants with primary (−8, 95% CI: −12, −4) or secondary (−11, 95% CI: −16, −6) school education, compared to those with no formal education. Every 5% increase in relative humidity was negatively associated with personal BC (−3, 95% CI: −4, −2). We also observed every 5 °C increase in temperature to be negatively associated with personal BC (−6, 95% CI: −10, −2) and found BC exposures to be lower in the rainy season (−11, 95% CI: −15, −7) compared to the dry season. The rainy season was also associated with lower BC exposures, compared to the dry season, in Guatemala (−6, 95% CI: −10, 0) and Rwanda (−23, 95% CI: −30, −17).
Model Performance and Fit
Model performance and fit statistics are provided in Table 2 and are comparable to those from models with imputed data for missing covariates (Table S4). Our HAPIN-wide model explained 48% of the variation in BC exposures among our study population with similar marginal R2 values for each site-specific model. The within-individual variance in personal BC was much greater than the between-individual variance as our ICC was 0.20 in the full HAPIN model. The RMSE between the natural logged-transformed predicted and measured BC exposures was 7.7 μg/m3.
Table 2. Measured and Modeled Exposure Summaries with Linear Mixed Model Statisticsa.
| measured
exposure |
modeled exposure |
model statistics |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| study site | model parameters | sample size | median (μg/m3) | mean (μg/m3) | SD (μg/m3) | sample size | median (μg/m3) | mean (μg/m3) | SD (μg/m3) | RMSE (μg/m3) | ICC | marginal R2 |
| HAPIN | study site + primary stove type + secondary stove type + participant cooked + other sources of smoke + primary lighting source + education + general kerosene use + occupation + stove use hours + kitchen location + roof material + wall material + season + temperature + humidity | 7165 | 7.1 | 9.3 | 9.5 | 5791 | 7.2 | 6.2 | 2.0 | 7.7 | 0.20 | 0.48 |
| Guatemala | primary stove type + secondary stove type + other sources of smoke + general kerosene use + kitchen volume + humidity + season | 2000 | 9.2 | 10 | 8.4 | 1799 | 9.7 | 7.8 | 1.7 | 6.9 | 0.25 | 0.50 |
| India | primary stove type + primary lighting source + general kerosene use + occupation + wall material + stove use hours + season + temperature + humidity | 1874 | 6.3 | 9.6 | 10.7 | 1784 | 6.6 | 5.8 | 2.1 | 8.7 | 0.18 | 0.45 |
| Peru | primary stove type + secondary stove type + stove use hours + participant cooked + kitchen location + age at baseline + family size | 1553 | 2.4 | 7.5 | 10.3 | 1516 | 4.5 | 4.0 | 2.1 | 8.3 | 0.24 | 0.46 |
| Rwanda | primary stove type + participant cooked + other sources of smoke + general kerosene use + occupation + food insecurity + kitchen volume + season | 1738 | 7.9 | 9.7 | 8.4 | 1142 | 8.1 | 7.4 | 1.6 | 5.8 | 0.06 | 0.49 |
SD = standard deviation; RMSE = root mean square error; ICC = intraclass correlation.
Potential for Effect Modification
HAPIN-wide, postintervention BC exposure contrasts between arms, by select factors, are shown in Figure 2; site-specific exposure contrasts are shown in Figures S6–S8. We found no potential for effect modification in Guatemala. Sample sizes for the control and intervention measures for each comparison are provided in Table S5. As reported by Johnson et al.37 (base model), BC exposures in the intervention group were significantly lower (−62, 95% CI: −65, −60) than those in the control group across all HAPIN sites. This contrast between groups was altered for participants who resided in Peru (−70, 95% CI: – 73, 66) and Rwanda (−53, 95% CI: −58, −47) and for participants who did not adhere to the assigned stove type (54, 95% CI: −19, 99) as confidence intervals for these effect estimates did not overlap that from Johnson et al.37 In India, the exposure contrast between groups was attenuated for kerosene users (−51, 95% CI: −62, −36) and enhanced when the humidity was in the lowest quartile (−77, 95% CI: −81, −72) compared to the BC exposure contrast reported by Johnson et al.37 (−69, 95% CI: −73, −66). In Peru, we estimated that the BC exposure contrast increased (from −62, 95% CI: −66, −57 to −72, 95% CI: −75, −69) after restricting to participants who adhered to the study stove assignment. We also found that the BC exposure contrasts between groups were enhanced for participants who used their stoves longer. In Rwanda, we observed the contrast between groups to be attenuated among participants who were in the “other” occupation category (i.e., participants did not work at home, as a vendor, or in agriculture) (−33, 95% CI: −49, −12).
Figure 2.
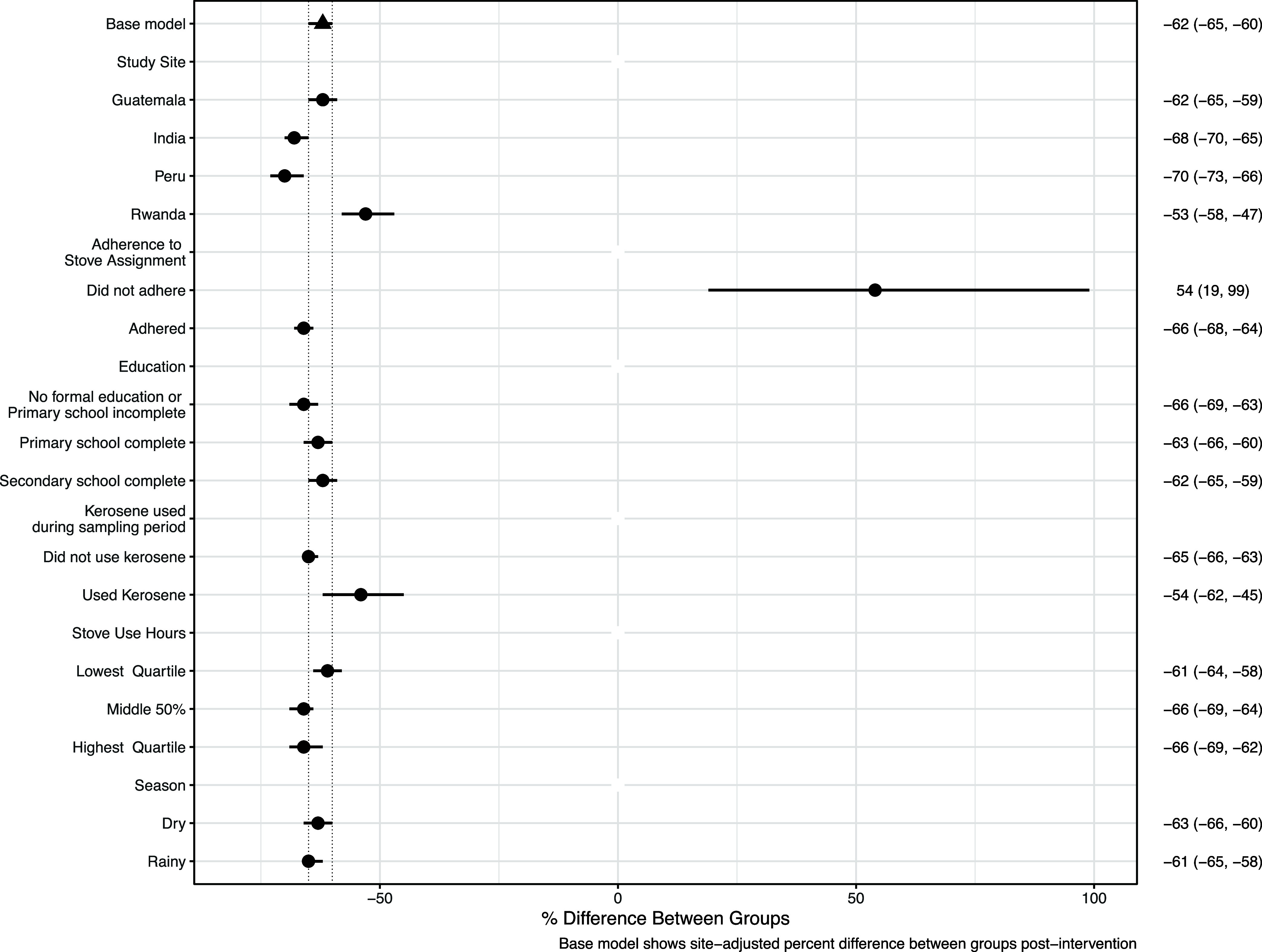
Hapin-wide postrandomization BC exposure contrasts (with 95% confidence intervals) between treatment arms (control vs intervention) by selected factors. Effect estimates outside of the confidence intervals reported in Johnson et al. 2022 (triangle) show how select factors potentially modified the effectiveness of the intervention in reducing personal exposures to BC. The percent differences in personal BC exposure between treatment arms were calculated within each subvariable using the emmeans package in R, which computes and compares marginal means.
Discussion
Study Overview
We conducted one of the largest and most comprehensive BC exposure assessment studies to date, comprising 7165 24 h measures from 3103 pregnant women across four diverse countries. We observed differences in personal exposures to BC according to primary stove type and kerosene use. In HAPIN-wide and site-specific analyses, we consistently observed a strong gradient where exposures were highest among participants using open fires, followed by those using improved biomass, than those using LPG stoves, respectively. Elevated exposures to BC were observed among kerosene users, compared to nonusers, for participants in Guatemala, India, and Rwanda, which highlights the potential importance of kerosene in these settings. These findings also support the notion that adherence to the HAPIN study stove assignment and general kerosene use can potentially impact the BC exposure contrast between treatment arms postrandomization; these effects were most prominent for participants in Peru and India, respectively.
Our study-wide and country-specific models performed moderately well (R2 range: 0.45–0.50) with R2 values similar to that reported for predicting personal PM2.5 exposures using only survey-based data in Kenya (R2 = 0.51)48 and higher than that reported for predicting global personal BC with survey data, ambient PM2.5, and household concentration levels (R2 range: 0.33–0.39),32 which highlights the explanatory power of information from questionnaires. Future studies may improve the predictive power of exposure models by more accurately characterizing the temporal changes in study participants’ activities in real-world conditions. Of particular importance is how certain temporal changes in time activity patterns are associated with combustion-related sources of air pollution like indoor smoking, garbage burning, crop burning, or the use of biomass for heating.
We also observed greater within-participant variance compared to between-participant variance in BC exposures, even after adjusting for key predictors of exposure. The ICC in our covariate-adjusted HAPIN-wide model (0.20) was higher than those observed for personal PM2.5 (0.16) and BC (0.11) exposures among adults in China,35 lower than that observed for carbon monoxide (CO) exposure among children in The Gambia (0.27),49 and overlapped with ICCs observed for exposures among adult women in Guatemala50 (CO: 0.17–0.33) and peri-urban India51 (PM2.5: 0.22; BC: 0.21). The direct comparison of ICCs across studies can be misleading given the differences in the predictors,52 target population, and pollutants assessed. Our ICCs, along with those from other longitudinal studies, suggest that a single 24 h exposure measurement does not sufficiently characterize longer-term exposures to investigate chronic health effects.
Stove and Fuel as Predictors for Black Carbon Exposures
We observed substantial variation in personal BC according to stove and fuel types as shown in effect estimates from the overall (Figures 1 and S2) and site-specific (Figure S3) plots of multivariable linear regression coefficients. A previous assessment of household BC in eight LMICs observed a concentration gradient for household BC comparing gas to coal (+53% increase), wood (+142% increase), and other biomass (+190% increase) fuels.32 Although not completely comparable, we observed similar findings according to stove/fuel types where BC exposures increased going from LPG to other biomass stove users. The distinction between these stove types is driven primarily by the fuel type and combustion conditions associated with each stove. For example, in Rwanda, Imbabura stove users predominantly cooked with charcoal and had lower BC exposures than those burning wood with Rondereza or open-fire stoves. This finding is in line with both field-39 and lab-based studies,53 which suggest that charcoal has a lower BC emission factor (reported as quantities of emitted BC per unit of fuel used) than wood. We observed no significant differences in BC exposures among wood and cow dung users in Peru (Table S3), possibly suggesting that these two fuel types have similar burning efficiencies.
Our assessment of the stove type used during sampling allowed us to evaluate how the exposure contrast between arms changed after adjusting for adherence to the study stove assignment. HAPIN-wide, we found that adherence potentially modified the BC exposure contrast between groups; this effect was most pronounced in Peru. The percentage of Peruvian participants in control homes exclusively using an LPG stove in the past 24 h at baseline, postintervention visit 1, and postintervention visit 2 was 6, 22, and 23%, respectively. Although these percentages are much smaller than those for corresponding participants in intervention homes that reported exclusive LPG use at follow-up (96–97%),54 we estimated that the BC exposure contrast between arms would be greater by about 12% had participants adhered to stove assignments in Peru.
Kerosene Use as a Predictor for Personal Black Carbon
Kerosene was an important driver of BC exposures in our data, likely due to the relatively high BC emission factor of this combustion source. Kerosene reportedly emits PM2.5 comprised mostly of BC (88–100%),55 which highlights the importance of studying the impact kerosene has on BC exposures in resource-limited areas of LMICs. The percentage of women with access to electricity for our study population in Rwanda (∼35%) was relatively higher than estimates in rural sub-Saharan Africa (SSA) (12%),56 yet much lower than that among women from the other HAPIN study sites (>90%).48 The lower access to electricity in Rwanda possibly suggests an increased reliance on fuel-based lighting sources like kerosene lamps and may explain why the magnitude of the association between kerosene use and BC exposure was greater than that seen in the other HAPIN IRCs. The elevated BC exposures seen among kerosene users in Rwanda were in line with those seen in Mozambique when comparing women using kerosene (+81%) to women using electricity as a lighting source.34 In Uganda, interventions of solar lighting systems versus fuel-based lighting sources resulted in massive reductions (>90%) in BC exposures,57 which suggests that exposures from fuel-based lighting sources can reduce the impact of a clean burning cookstove intervention on BC exposures. Future intervention programs may benefit from aiming to mitigate both cookstoves and lighting sources in tandem to comprehensively reduce exposures in resource-limited areas of LMICs, particularly in SSA.
The role of kerosene use for pregnant women in India is less clear than it is for those in Rwanda. For example, virtually all of our participants in India either had access to electricity or used electricity as a primary lighting source;37 however, ∼20% of participants used kerosene during sampling at baseline. While this percentage remained relatively constant in the control arm postrandomization, the percentage of those using kerosene nearly halved in the intervention arm postrandomization (Table S6). Additionally, unlike in Rwanda, both kerosene-related variables (e.g., general kerosene use during sampling and primary lighting source) were selected in the multivariable predictive model for India, which possibly alludes to multiple uses of kerosene in this study site. These assertions, along with technicians’ observations of Indian mothers using kerosene as a fire starter in the control group for cooking, imply that the intervention had an unforeseen benefit in reducing the need to use kerosene in the intervention arm postrandomization. Both kerosene-related variables that we assessed have the potential to modify the BC exposure contrast between treatment arms; however, we observed the general kerosene use variable to impact the intervention substantially in India where the exposure contrast was sharply attenuated among kerosene users.
Study Limitations
The HAPIN study design included many strengths, such as robust sample size, global representation among LMICs, clear distinctions of stove and fuel use, repeated measures of personal BC, and comprehensive assessment of individual and group-level factors that can potentially impact exposures; our study also has some weaknesses. First, the current study only has two repeated postrandomization measures for individuals in the LPG stove intervention arm, limiting our ability to assess the within-participant variance among this group. Second, we have missing survey data; however, after conducting the same analysis with imputed data for missing variables, both nonimputed and imputed model results were similar to one another. Third, our questionnaires were not specific enough to discern the different uses of kerosene among our study population. However, we provided empirical evidence supporting our field exposure team’s suspicion that participants in India additionally used kerosene to ignite biomass or as a backup cooking fuel as opposed to using kerosene solely as a lighting source like participants in the other study sites. Future exposure assessments may benefit from administering more specific surveys to parse the potential impacts of exposure to kerosene from cooking and lighting practices. Fourth, combustion-related sources other than the cookstove (i.e., crop and waste burning, use of biomass for heating, indoor smoking, and other relevant sources) were identified in our questionnaire, yet we found no significant associations between these sources and BC likely due to the constraints of our HAPIN study design (e.g., eligibility criteria and selection of study sites with minimal ambient sources). Finally, HAPIN purposefully selected study sites that reduced the contribution of air pollution from traffic sources. Additionally, ambient measures of exposures were not available during the time of our data analysis for this work. Therefore, our results do not account for this source’s contribution to exposures among our study population and may impact the portability of our findings to other settings with significant traffic- or industry-related source profiles.
Implications for Future Cookstove Interventions
The current study provides one of the most comprehensive assessments of personal BC exposures in LMICs. Our exposure modeling may provide important information to future studies aiming to mitigate and quantify the health risks associated with exposure to BC in settings where household air pollution is dominated by cookstove sources. This information can be used in future exposure and health studies to estimate exposures among this demographic on a grander scale than personal monitoring would allow. Furthermore, we identified several factors that can impact exposure to BC and explored how select factors potentially modified the effect of an LPG intervention in reducing exposure to BC. Our findings highlight the importance of both stove adherence as well as the mitigation of kerosene use in cookstove intervention trials to achieve more effective exposure contrasts between treatment groups. In conclusion, the information gleaned from the current study may be leveraged before and during future studies to implement more impactful cookstove intervention trials.
Acknowledgments
The HAPIN trial was funded by the U.S. National Institutes of Health (cooperative agreement 1UM1HL134590) in collaboration with the Bill & Melinda Gates Foundation [OPP1131279]. The investigators would like to thank the members of the advisory committee—Drs. Patrick Breysse, Donna Spiegelman, and Joel Kaufman—for their valuable insight and guidance throughout the implementation of the trial. We also wish to acknowledge all research staff and study participants for their dedication to and participation in this important trial. This publication was also supported by Grant # T42OH008436 from NIOSH. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of NIOSH. A multidisciplinary, independent Data and Safety Monitoring Board (DSMB) appointed by the National Heart, Lung, and Blood Institute (NHLBI) monitored the quality of the data and protected the safety of patients enrolled in the HAPIN trial. The DSMB consisted of Catherine Karr (Chair), Nancy R. Cook, Stephen Hecht, Joseph Millum, Nalini Sathiakumar (deceased), Paul K. Whelton, and Gail Weinmann and Thomas Croxton (Executive Secretaries). Program Coordination: Gail Rodgers, Bill & Melinda Gates Foundation; Claudia L. Thompson, National Institute of Environmental Health Sciences; Mark J. Parascandola, National Cancer Institute; Marion Koso-Thomas, Eunice Kennedy Shriver National Institute of Child Health and Human Development; Joshua P. Rosenthal, Fogarty International Center; Concepcion R. Nierras, NIH Office of Strategic Coordination—The Common Fund; Katherine Kavounis, Dong-Yun Kim, Barry S. Schmetter (deceased), and Antonello Punturieri, NHLBI. This research represents the NIH’s contribution to the Global Alliance for Chronic Diseases (GACD) coordinated call for research on the prevention and management of chronic lung diseases for 2016. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the US National Institutes of Health or the Department of Health and Human Services. The study protocol has been reviewed and approved by institutional review boards (IRBs) or Ethics Committees at Emory University (00089799), Johns Hopkins University (00007403), Sri Ramachandra Institute of Higher Education and Research (IEC-N1/16/JUL/54/49) and the Indian Council of Medical Research—Health Ministry Screening Committee (5/8/4–30/(Env)/Indo-US/2016-NCD-I), Universidad del Valle de Guatemala (146–08–2016) and Guatemalan Ministry of Health National Ethics Committee (11-2016), Asociación Beneficia PRISMA (CE2981.17), the London School of Hygiene and Tropical Medicine (11664–5), the Rwandan National Ethics Committee (No.357/RNEC/2018), and Washington University in St. Louis (201611159). The study has been registered with ClinicalTrials.gov (Identifier NCT02944682). No authors have any competing interests to disclose. HAPIN Investigators: Vigneswari Aravindalochanan, Gloriose Bankundiye, Dana Boyd Barr, Vanessa Burrowes, Alejandra Bussalleu, Eduardo Canuz, Adly Castan ~aza, Howard H. Chang, Yunyun Chen, Marilú Chiang, Rachel Craik, Mary Crocker, Victor G. Davila-Roman, Lisa de las Fuentes, Oscar De León, Lisa Elon, Juan Gabriel Espinoza, Irma Sayury Pineda Fuentes, Sarada S. Garg, Ahana Ghosh, Dina Goodman-Palmer, Laura Grajeda, Savannah Gupton, Sarah Hamid, Stella M. Hartinger, Steven A. Harvey, Mayari Hengstermann, Ian Hennessee, Phabiola Herrera, Shakir Hossen, Marjorie Howard, Penelope P. Howards, Lindsay Jaacks, Shirin Jabbarzadeh, Margaret A. Laws, Pattie Lenzen, Jiawen Liao, Amy E. Lovvorn, Jane Mbabazi, Eric D. McCollum, Julia N. McPeek, Rachel Meyers, J. Jaime Miranda, Libny Monroy, Lawrence Moulton, Alexie Mukeshimana, Krishnendu Mukhopadhyay, Bernard Mutariyani, Abidan Nambajimana, Durairaj Natesan, Azhar Nizam, Jean de Dieu Ntivuguruzwa, Aris T. Papageorghiou, Naveen Puttaswamy, Elisa Puzzolo, Karthikeyan Dharmapuri Rajamani, Sarah Rajkumar, Usha Ramakrishnan, Rengaraj Ramasami, Alexander Ramirez, Ghislaine Rosa, Joshua Rosenthal, P. Barry Ryan, Sudhakar Saidam, Zoe Sakas, Sankar Sambandam, Jeremy A. Sarnat, Suzanne Simkovich, Sheela S. Sinharoy, Kirk R. Smith, Damien Swearing, Gurusamy Thangavel, Ashley Toenjes, Jean Damascene Uwizeyimana, Viviane Valdes, Amit Verma, Jiantong Wang, Megan Warnock, Kendra N. Williams, Wenlu Ye, Bonnie N. Young, and Ashley Younger.
Supporting Information Available
The Supporting Information is available free of charge at https://pubs.acs.org/doi/10.1021/acs.est.3c09991.
Description of individual and household characteristics (Text S1); description of imputation analysis (Text S2); summary statistics of personal BC (μg/m3) overall and by select factors (Table S1); postintervention personal BC (μg/m3) by treatment arm and IRC (Table S2); HAPIN-wide and IRC-specific association between personal BC and select factors (Table S3); exposure summary and model performance mixed-effects analysis with imputed data (Table S4); sample sizes (N measures) of comparison groups (control vs intervention) postintervention (Table S5); number (%) of baseline and postrandomization measures by treatment arm and kerosene use in India (Table S6); percent of missing data for each factor (Figure S1); Guatemala-specific multivariable linear regression coefficients (Figure S2); India-specific multivariable linear regression coefficients (Figure S3); Peru-specific multivariable linear regression coefficients (Figure S4); Rwanda-specific multivariable linear regression coefficients (Figure S5); postintervention BC exposure contrasts between treatment arms in India (Figure S6); postintervention BC exposure contrasts between treatment arms in Peru (Figure S7); postintervention BC exposure contrasts between treatment arms in Rwanda (Figure S8) (PDF)
The authors declare no competing financial interest.
Supplementary Material
References
- World Bank and WHO, Washington DC, IEA, IRENA, UNSD . Tracking SDG 7: The Energy Progress Report, 2023, License: Creative Commons Attribution—NonCommercial 3.0 IGO (CC BY-NC 3.0 IGO) 2023https://trackingsdg7.esmap.org/data/files/download-documents/sdg7-report2023-full_report.pdf>.
- Bennitt F. B.; Wozniak S. S.; Causey K.; Burkart K.; Brauer M. Estimating disease burden attributable to household air pollution: new methods within the Global Burden of Disease Study. Lancet Glob. Health 2021, 9, S18. 10.1016/S2214-109X(21)00126-1. [DOI] [Google Scholar]
- Balakrishnan K.; Steenland K.; Clasen T.; Chang H.; Johnson M.; Pillarisetti A.; Ye W.; Naeher L. P.; Diaz-Artiga A.; McCracken J. P.; Thompson L. M.; Rosa G.; Kirby M. A.; Thangavel G.; Sambandam S.; Mukhopadhyay K.; Puttaswamy N.; Aravindalochanan V.; Garg S.; Ndagijimana F.; Hartinger S.; UnderHill L.; Kearns K. A.; Campbell D.; Kremer J.; Waller L.; Jabbarzadeh S.; Wang J.; Chen Y.; Rosenthal J.; Quinn A.; Papageorghiou A. T.; Ramakrishnan U.; Howards P. P.; Checkley W.; Peel J. L.; Investigators H.. Exposure–response relationships for personal exposure to fine particulate matter (PM2·5), carbon monoxide, and black carbon and birthweight: Results from the multi-country Household Air Pollution Intervention Network (HAPIN) trial 2022 10.1101/2022.08.06.22278373. [DOI] [PMC free article] [PubMed]
- Bruce N.; Pope D.; Rehfuess E.; Balakrishnan K.; Adair-Rohani H.; Dora C. WHO indoor air quality guidelines on household fuel combustion: Strategy implications of new evidence on interventions and exposure–risk functions. Atmos. Environ. 2015, 106, 451–457. 10.1016/j.atmosenv.2014.08.064. [DOI] [Google Scholar]
- Gordon S. B.; Bruce N. G.; Grigg J.; Hibberd P. L.; Kurmi O. P.; Lam K. B.; Mortimer K.; Asante K. P.; Balakrishnan K.; Balmes J.; Bar-Zeev N.; Bates M. N.; Breysse P. N.; Buist S.; Chen Z.; Havens D.; Jack D.; Jindal S.; Kan H.; Mehta S.; Moschovis P.; Naeher L.; Patel A.; Perez-Padilla R.; Pope D.; Rylance J.; Semple S.; Martin W. J. Respiratory risks from household air pollution in low and middle income countries. Lancet Respir Med. 2014, 2, 823–60. 10.1016/S2213-2600(14)70168-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee K. K.; Bing R.; Kiang J.; Bashir S.; Spath N.; Stelzle D.; Mortimer K.; Bularga A.; Doudesis D.; Joshi S. S.; Strachan F.; Gumy S.; Adair-Rohani H.; Attia E. F.; Chung M. H.; Miller M. R.; Newby D. E.; Mills N. L.; McAllister D. A.; Shah A. S. V. Adverse health effects associated with household air pollution: a systematic review, meta-analysis, and burden estimation study. Lancet Glob. Health 2020, 8, e1427–e1434. 10.1016/S2214-109X(20)30343-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quansah R.; Semple S.; Ochieng C. A.; Juvekar S.; Armah F. A.; Luginaah I.; Emina J. Effectiveness of interventions to reduce household air pollution and/or improve health in homes using solid fuel in low-and-middle income countries: A systematic review and meta-analysis. Environ. Int. 2017, 103, 73–90. 10.1016/j.envint.2017.03.010. [DOI] [PubMed] [Google Scholar]
- Simkovich S. M.; Goodman D.; Roa C.; Crocker M. E.; Gianella G. E.; Kirenga B. J.; Wise R. A.; Checkley W. The health and social implications of household air pollution and respiratory diseases. npj Primary Care Respir. Med. 2019, 29, 12 10.1038/s41533-019-0126-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith K. R.; Bruce N.; Balakrishnan K.; Adair-Rohani H.; Balmes J.; Chafe Z.; Dherani M.; Hosgood H. D.; Mehta S.; Pope D.; Rehfuess E. Millions Dead: How Do We Know and What Does It Mean? Methods Used in the Comparative Risk Assessment of Household Air Pollution. Annu. Rev. Public Health 2014, 35, 185–206. 10.1146/annurev-publhealth-032013-182356. [DOI] [PubMed] [Google Scholar]
- Thakur M.; Nuyts P. A. W.; Boudewijns E. A.; Flores Kim J.; Faber T.; Babu G. R.; van Schayck O. C. P.; Been J. V. Impact of improved cookstoves on women’s and child health in low and middle income countries: a systematic review and meta-analysis. Thorax 2018, 73, 1026–1040. 10.1136/thoraxjnl-2017-210952. [DOI] [PubMed] [Google Scholar]
- Younger A.; Alkon A.; Harknett K.; Jean Louis R.; Thompson L. M. Adverse birth outcomes associated with household air pollution from unclean cooking fuels in low- and middle-income countries: A systematic review. Environ. Res. 2022, 204, 112274 10.1016/j.envres.2021.112274. [DOI] [PubMed] [Google Scholar]
- Naeher L. P.; Brauer M.; Lipsett M.; Zelikoff J. T.; Simpson C. D.; Koenig J. Q.; Smith K. R. Woodsmoke Health Effects: A Review. Inhal. Toxicol. 2007, 19, 67–106. 10.1080/08958370600985875. [DOI] [PubMed] [Google Scholar]
- Secrest M. H.; Schauer J. J.; Carter E. M.; Baumgartner J. Particulate matter chemical component concentrations and sources in settings of household solid fuel use. Indoor Air 2017, 27, 1052–1066. 10.1111/ina.12389. [DOI] [PubMed] [Google Scholar]
- Bond T. C.; Doherty S. J.; Fahey D. W.; Forster P. M.; Berntsen T.; DeAngelo B. J.; Flanner M. G.; Ghan S.; Kärcher B.; Koch D.; Kinne S.; Kondo Y.; Quinn P. K.; Sarofim M. C.; Schultz M. G.; Schulz M.; Venkataraman C.; Zhang H.; Zhang S.; Bellouin N.; Guttikunda S. K.; Hopke P. K.; Jacobson M. Z.; Kaiser J. W.; Klimont Z.; Lohmann U.; Schwarz J. P.; Shindell D.; Storelvmo T.; Warren S. G.; Zender C. S. Bounding the role of black carbon in the climate system: A scientific assessment. J. Geophys. Res.: Atmos. 2013, 118, 5380–5552. 10.1002/jgrd.50171. [DOI] [Google Scholar]
- Grahame T. J.; Klemm R.; Schlesinger R. B. Public health and components of particulate matter: The changing assessment of black carbon. J. Air Waste Manage. Assoc. 2014, 64, 620–660. 10.1080/10962247.2014.912692. [DOI] [PubMed] [Google Scholar]
- Wang Y.; Shupler M.; Birch A.; Chu Y. L.; Jeronimo M.; Rangarajan S.; Mustaha M.; Heenan L.; Seron P.; Saavedra N.; Oliveros M. J.; Lopez-Jaramillo P.; Camacho P. A.; Otero J.; Perez-Mayorga M.; Yeates K.; West N.; Ncube T.; Ncube B.; Chifamba J.; Yusuf R.; Khan A.; Liu Z.; Cheng X.; Wei L.; Tse L. A.; Mohan D.; Kumar P.; Gupta R.; Mohan I.; Jayachitra K. G.; Mony P. K.; Rammohan K.; Nair S.; Lakshmi P. V. M.; Sagar V.; Khawaja R.; Iqbal R.; Kazmi K.; Yusuf S.; Brauer M.; Hystad P. Personal and household PM2.5 and black carbon exposure measures and respiratory symptoms in 8 low- and middle-income countries. Environ. Res. 2022, 212, 113430 10.1016/j.envres.2022.113430. [DOI] [PubMed] [Google Scholar]
- Xu H.; Ren Y.; Zhang W.; Meng W.; Yun X.; Yu X.; Li J.; Zhang Y.; Shen G.; Ma J.; Li B.; Cheng H.; Wang X.; Wan Y.; Tao S. Updated Global Black Carbon Emissions from 1960 to 2017: Improvements, Trends, and Drivers. Environ. Sci. Technol. 2021, 55, 7869–7879. 10.1021/acs.est.1c03117. [DOI] [PubMed] [Google Scholar]
- Ritchie H.; Roser M.; Our World in Data . Urbanization 2018https://ourworldindata.org/urbanization>.
- US EPA . Integrated Science Assessment (ISA) for Particulate Matter 2019https://www.epa.gov/isa/integrated-science-assessment-isa-particulate-matter>.
- World Health Organization (WHO) . WHO global air quality guidelines: particulate matter (PM2.5 and PM10), ozone, nitrogen dioxide, sulfur dioxide and carbon monoxide 2021https://apps.who.int/iris/handle/10665/345329>. [PubMed]
- Alexander D. A.; Northcross A.; Karrison T.; Morhasson-Bello O.; Wilson N.; Atalabi O. M.; Dutta A.; Adu D.; Ibigbami T.; Olamijulo J.; Adepoju D.; Ojengbede O.; Olopade C. O. Pregnancy outcomes and ethanol cook stove intervention: A randomized-controlled trial in Ibadan, Nigeria. Environ. Int. 2018, 111, 152–163. 10.1016/j.envint.2017.11.021. [DOI] [PubMed] [Google Scholar]
- Aung T. W.; Baumgartner J.; Jain G.; Sethuraman K.; Reynolds C.; Marshall J. D.; Brauer M. Effect on blood pressure and eye health symptoms in a climate-financed randomized cookstove intervention study in rural India. Environ. Res. 2018, 166, 658–667. 10.1016/j.envres.2018.06.044. [DOI] [PubMed] [Google Scholar]
- Checkley W.; Williams K. N.; Kephart J. L.; Fandiño-Del-Rio M.; Steenland N. K.; Gonzales G. F.; Naeher L. P.; Harvey S. A.; Moulton L. H.; Davila-Roman V. G. Effects of a household air pollution intervention with liquefied petroleum gas on cardiopulmonary outcomes in Peru. A randomized controlled trial. Am. J. Respir. Crit. Care Med. 2021, 203, 1386–1397. 10.1164/rccm.202006-2319OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chillrud S. N.; Ae-Ngibise K. A.; Gould C. F.; Owusu-Agyei S.; Mujtaba M.; Manu G.; Burkart K.; Kinney P. L.; Quinn A.; Jack D. W.; Asante K. P. The effect of clean cooking interventions on mother and child personal exposure to air pollution: results from the Ghana Randomized Air Pollution and Health Study (GRAPHS). J. Expo. Sci. Environ. Epidemiol. 2021, 31, 683–698. 10.1038/s41370-021-00309-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katz J.; Tielsch J. M.; Khatry S. K.; Shrestha L.; Breysse P.; Zeger S. L.; Kozuki N.; Checkley W.; LeClerq S. C.; Mullany L. C. Impact of Improved Biomass and Liquid Petroleum Gas Stoves on Birth Outcomes in Rural Nepal: Results of 2 Randomized Trials. Global Health: Sci. Pract. 2020, 8, 372–382. 10.9745/GHSP-D-20-00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pope D.; Bruce N.; Dherani M.; Jagoe K.; Rehfuess E. Real-life effectiveness of ‘improved’ stoves and clean fuels in reducing PM 2.5 and CO: Systematic review and meta-analysis. Environ. Int. 2017, 101, 7–18. 10.1016/j.envint.2017.01.012. [DOI] [PubMed] [Google Scholar]
- Pope D.; Johnson M.; Fleeman N.; Jagoe K.; Duarte R.; Maden M.; Ludolph R.; Bruce N.; Shupler M.; Adair-Rohani H.; Lewis J. Are cleaner cooking solutions clean enough? A systematic review and meta-analysis of particulate and carbon monoxide concentrations and exposures. Environ. Res. Lett. 2021, 16, 083002 10.1088/1748-9326/ac13ec. [DOI] [Google Scholar]
- Fandiño-Del-Rio M.; Kephart J. L.; Williams K. N.; Shade T.; Adekunle T.; Steenland K.; Naeher L. P.; Moulton L. H.; Gonzales G. F.; Chiang M.; Hossen S.; Chartier R. T.; Koehler K.; Checkley W.; Household Air Pollution Concentrations after Liquefied Petroleum Gas Interventions in Rural Peru: Findings from a One-Year Randomized Controlled Trial Followed by a One-Year Pragmatic Crossover Trial. Environ. Health Perspect. 2022, 130, 057007 10.1289/EHP10054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young B. N.; Good N.; Peel J. L.; Benka-Coker M. L.; Keller J. P.; Rajkumar S.; Walker E. S.; Volckens J.; L’Orange C.; Quinn C.; Africano S.; Osorto Pinel A. B.; Clark M. L. Reduced Black Carbon Concentrations following a Three-Year Stepped-Wedge Randomized Trial of the Wood-Burning Justa Cookstove in Rural Honduras. Environ. Sci. Technol. Lett. 2022, 14, 538–542. 10.1021/acs.estlett.2c00098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark M. L.; Peel J. L.; Balakrishnan K.; Breysse P. N.; Chillrud S. N.; Naeher L. P.; Rodes C. E.; Vette A. F.; Balbus J. M. Health and Household Air Pollution from Solid Fuel Use: The Need for Improved Exposure Assessment. Environ. Health Perspect. 2013, 121, 1120–1128. 10.1289/ehp.1206429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shupler M.; Hystad P.; Birch A.; Miller-Lionberg D.; Jeronimo M.; Arku R. E.; Chu Y. L.; Mushtaha M.; Heenan L.; Rangarajan S.; Seron P.; Lanas F.; Cazor F.; Lopez-Jaramillo P.; Camacho P. A.; Perez M.; Yeates K.; West N.; Ncube T.; Ncube B.; Chifamba J.; Yusuf R.; Khan A.; Hu B.; Liu X.; Wei L.; Tse L. A.; Mohan D.; Kumar P.; Gupta R.; Mohan I.; Jayachitra K. G.; Mony P. K.; Rammohan K.; Nair S.; Lakshmi P. V. M.; Sagar V.; Khawaja R.; Iqbal R.; Kazmi K.; Yusuf S.; Brauer M. Household and personal air pollution exposure measurements from 120 communities in eight countries: results from the PURE-AIR study. Lancet Planet. Health 2020, 4, e451–e462. 10.1016/S2542-5196(20)30197-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y.; Shupler M.; Birch A.; Chu Y. L.; Jeronimo M.; Rangarajan S.; Mustaha M.; Heenan L.; Seron P.; Lanas F.; Salazar L.; Saavedra N.; Oliveros M. J.; Lopez-Jaramillo P.; Camacho P. A.; Otero J.; Perez-Mayorga M.; Yeates K.; West N.; Ncube T.; Ncube B.; Chifamba J.; Yusuf R.; Khan A.; Liu Z.; Bo H.; Wei L.; Tse L. A.; Mohan D.; Kumar P.; Gupta R.; Mohan I.; Jayachitra K. G.; Mony P. K.; Rammohan K.; Nair S.; Lakshmi P. V. M.; Sagar V.; Khawaja R.; Iqbal R.; Kazmi K.; Yusuf S.; Brauer M.; Hystad P. Measuring and predicting personal and household Black Carbon levels from 88 communities in eight countries. Sci. Total Environ. 2022, 818, 151849 10.1016/j.scitotenv.2021.151849. [DOI] [PubMed] [Google Scholar]
- Fandiño-Del-Rio M.; Kephart J. L.; Williams K. N.; Moulton L. H.; Steenland K.; Checkley W.; Koehler K. Household air pollution exposure and associations with household characteristics among biomass cookstove users in Puno, Peru. Environ. Res. 2020, 191, 110028 10.1016/j.envres.2020.110028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curto A.; Donaire-Gonzalez D.; Manaca M. N.; González R.; Sacoor C.; Rivas I.; Gascon M.; Wellenius G. A.; Querol X.; Sunyer J.; Macete E.; Menéndez C.; Tonne C. Predictors of personal exposure to black carbon among women in southern semi-rural Mozambique. Environ. Int. 2019, 131, 104962 10.1016/j.envint.2019.104962. [DOI] [PubMed] [Google Scholar]
- Lee M.; Carter E.; Yan L.; Chan Q.; Elliott P.; Ezzati M.; Kelly F.; Schauer J. J.; Wu Y.; Yang X.; Zhao L.; Baumgartner J. Determinants of personal exposure to PM2.5 and black carbon in Chinese adults: A repeated-measures study in villages using solid fuel energy. Environ. Int. 2021, 146, 106297 10.1016/j.envint.2020.106297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clasen T.; Checkley W.; Peel J. L.; Balakrishnan K.; McCracken J. P.; Rosa G.; Thompson L. M.; Barr D. B.; Clark M. L.; Johnson M. A. Design and rationale of the HAPIN study: a multicountry randomized controlled trial to assess the effect of liquefied petroleum gas stove and continuous fuel distribution. Environ. Health Perspect. 2020, 128, 047008 10.1289/EHP6407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson M.; Pillarisetti A.; Piedrahita R.; Balakrishnan K.; Peel J. L.; Steenland K.; Underhill L. J.; Rosa G.; Kirby M. A.; Díaz-Artiga A.; McCracken J.; Clark M. L.; Waller L.; Chang H. H.; Wang J.; Dusabimana E.; Ndagijimana F.; Sambandam S.; Mukhopadhyay K.; Kearns K. A.; Campbell D.; Kremer J.; Rosenthal J. P.; Checkley W.; Clasen T.; Naeher L.; Exposure Contrasts of Pregnant Women during the Household Air Pollution Intervention Network Randomized Controlled Trial. Environ. Health Perspect. 2022, 130, 097005 10.1289/EHP10295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson M. A.; Steenland K.; Piedrahita R.; Clark M. L.; Pillarisetti A.; Balakrishnan K.; Peel J. L.; Naeher L. P.; Liao J.; Wilson D.; Sarnat J.; Underhill L. J.; Burrowes V.; McCracken J. P.; Rosa G.; Rosenthal J.; Sambandam S.; de Leon O.; Kirby M. A.; Kearns K.; Checkley W.; Clasen T.; Air Pollutant Exposure and Stove Use Assessment Methods for the Household Air Pollution Intervention Network (HAPIN) Trial. Environ. Health Perspect. 2020, 128, 047009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garland C.; Delapena S.; Prasad R.; L’Orange C.; Alexander D.; Johnson M. Black carbon cookstove emissions: A field assessment of 19 stove/fuel combinations. Atmos. Environ. 2017, 169, 140–149. 10.1016/j.atmosenv.2017.08.040. [DOI] [Google Scholar]
- Atlas W.; Weather Atlas . Yearly & Monthly weather - Guatemala City, Guatemala. https://www.weather-atlas.com/en/guatemala/guatemala-city-climate.
- Wikipedia . Climate of Tamil Nadu 2023https://en.wikipedia.org/w/index.php?title=Climate_of_Tamil_Nadu&oldid=1189733990.
- Atlas W.; Weather Atlas . Yearly & Monthly weather - Puno, Peru. https://www.weather-atlas.com/en/peru/puno-climate.
- Atlas W.; Weather Atlas . Yearly & Monthly weather - Kayonza, Rwanda. https://www.weather-atlas.com/en/rwanda/kayonza-climate.
- Bates D.; Maechler M.; Bolker B.; Walker S.; Christensen R. H. B.; Singmann H.; Dai B.; Scheipl F.; Grothendieck G.; Green P.; Fox J.; Bauer A.. Linear Mixed-Effects Models using ‘Eigen’ and S4, simulate formula, 2023https://cran.r-project.org/web/packages/lme4/index.html, P. N. K. (shared copyright on & Tanaka, E. lme4.
- Lüdecke D.; Bartel A.; Schwemmer C.; Powell C.; Djalovski A.; Titz J.. sjPlot: Data Visualization for Statistics in Social Science 2023https://cran.r-project.org/web/packages/sjPlot/index.html.
- RMSE: Root Mean Square Error Loss in MLmetrics: Machine Learning Evaluation Metrics. https://rdrr.io/cran/MLmetrics/man/RMSE.html.
- Lenth R. V.; Bolker B.; Buerkner P.; Giné-Vázquez I.; Herve M.; Jung M.; Love J.; Miguez F.; Riebl H.; Singmann H.. emmeans: Estimated Marginal Means, aka Least-Squares Means 2024https://cran.r-project.org/web/packages/emmeans/index.html.
- Johnson M.; Piedrahita R.; Pillarisetti A.; Shupler M.; Menya D.; Rossanese M.; Delapeña S.; Penumetcha N.; Chartier R.; Puzzolo E. Modeling approaches and performance for estimating personal exposure to household air pollution: A case study in Kenya. Indoor Air 2021, 31, 1441–1457. 10.1111/ina.12790. [DOI] [PubMed] [Google Scholar]
- Dionisio K. L.; Howie S. R. C.; Dominici F.; Fornace K. M.; Spengler J. D.; Donkor S.; Chimah O.; Oluwalana C.; Ideh R. C.; Ebruke B.; Adegbola R. A.; Ezzati M. The exposure of infants and children to carbon monoxide from biomass fuels in The Gambia: a measurement and modeling study. J. Expo. Sci. Environ. Epidemiol. 2012, 22, 173–181. 10.1038/jes.2011.47. [DOI] [PubMed] [Google Scholar]
- McCracken J. P.; Schwartz J.; Bruce N.; Mittleman M.; Ryan L. M.; Smith K. R. Combining individual-and group-level exposure information: child carbon monoxide in the Guatemala woodstove randomized control trial. Epidemiology 2009, 20, 127–136. 10.1097/EDE.0b013e31818ef327. [DOI] [PubMed] [Google Scholar]
- Sanchez M.; Milà C.; Sreekanth V.; Balakrishnan K.; Sambandam S.; Nieuwenhuijsen M.; Kinra S.; Marshall J. D.; Tonne C. Personal exposure to particulate matter in peri-urban India: predictors and association with ambient concentration at residence. J. Expo. Sci. Environ. Epidemiol. 2020, 30, 596–605. 10.1038/s41370-019-0150-5. [DOI] [PubMed] [Google Scholar]
- Keller J. P.; Clark M. L. Estimating long-term average household air pollution concentrations from repeated short-term measurements in the presence of seasonal trends and crossover. Environ. Epidemiol. 2022, 6, e188 10.1097/EE9.0000000000000188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacCarty N.; Bentson S.; Cushman K.; Au J.; Li C.; Murugan G.; Still D. Stratification of particulate matter in a kitchen: A comparison of empirical to predicted concentrations and implications for cookstove emissions targets. Energy Sustainable Dev. 2020, 54, 14–24. 10.1016/j.esd.2019.09.006. [DOI] [Google Scholar]
- Quinn A. K.; Williams K. N.; Thompson L. M.; Harvey S. A.; Piedrahita R.; Wang J.; Quinn C.; Pillarisetti A.; McCracken J. P.; Rosenthal J. P.; Kirby M. A.; Artiga A. D.; Thangavel G.; Rosa G.; Miranda J. J.; Checkley W.; Peel J. L.; Clasen T. F. Fidelity and Adherence to a Liquefied Petroleum Gas Stove and Fuel Intervention during Gestation: The Multi-Country Household Air Pollution Intervention Network (HAPIN) Randomized Controlled Trial. Int. J. Environ. Res. Public. Health 2021, 18, 12592. 10.3390/ijerph182312592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lam N. L.; Chen Y.; Weyant C.; Venkataraman C.; Sadavarte P.; Johnson M. A.; Smith K. R.; Brem B. T.; Arineitwe J.; Ellis J. E.; Bond T. C. Household Light Makes Global Heat: High Black Carbon Emissions From Kerosene Wick Lamps. Environ. Sci. Technol. 2012, 46, 13531–13538. 10.1021/es302697h. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crousillat E.; Hamilton R.; Antmann P.. Addressing the electricity access gap. 2010.
- Wallach E. S.; Lam N. L.; Nuwagira E.; Muyanja D.; Tayebwa M.; Valeri L.; Tsai A. C.; Vallarino J.; Allen J. G.; Lai P. S. Effect of a solar lighting intervention on fuel-based lighting use and exposure to household air pollution in rural Uganda: A randomized controlled trial. Indoor Air 2022, 32, e12986 10.1111/ina.12986. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.