Abstract
The intrinsic subtype of triple-negative breast cancer (TNBC) is based on genomic evaluation. In this study, we report the survival and pathological complete response (pCR) rates of TNBC patients subtyped by IHC and treated with neoadjuvant chemotherapy (NACT). A retrospective cohort of 187 TNBC patients who received NACT between 2008 and 2017 was used, and IHC subtyping was performed on biopsy specimens before chemotherapy. The subtyping revealed predominantly basal-like tumors (IHC-BL, 61%), followed by basal-like immune-suppressed tumors (IHC-BLIS, 31%), mesenchymal tumors (12.5%), luminal androgen receptor tumors (IHC-LAR, 12%), and basal-like immune-activated tumors (IHC-BLIA, 10.9%). The pCR rate varied among subtypes, with IHC-BLIA showing the highest (30.0%) and IHC-LAR showing the lowest (4.5%). IHC-BLIS led in recurrence sites. Overall and disease-free survival analyses did not show significant differences among subtypes, although IHC-BLIA demonstrated a trend toward better survival, and IHC-mesenchymal, worse. Patients who achieved pCR exhibited significantly better disease-free survival and overall survival than non-responders. This study underscores the potential of IHC-based subtyping in TNBC management, highlighting distinct response patterns to neoadjuvant chemotherapy and potential implications for treatment strategies. Further research is warranted to validate these findings and explore tailored therapeutic approaches for specific TNBC subtypes.
Keywords: triple-negative breast cancer, immunohistochemistry, neoadjuvant chemotherapy
1. Introduction
According to Cancer Research UK, triple-negative breast cancer (TNBC) accounts for approximately 15% of malignancies affecting the breast. Characterized by the absence of estrogen, progesterone, and Her2 receptor positivity, it is usually associated with a poor prognosis, and chemotherapy remains the main basis of systemic treatment [1]. In the last decade, the relevant benefits of chemotherapy combined with immunotherapy and targeted therapy for patients with pathogenic germline BRCA mutations have positively impacted outcomes in both curative and palliative settings [2].
However, TNBC represents a heterogeneous group of several subtypes with distinct drivers, survival outcomes, and responses to systemic therapy [3]. Several classifications have been proposed and validated, largely based on genomic evaluation of the tumors [4]. In 2011, Lehmann et al. characterized seven subtypes by gene expression, including one unstable. Basal-like 1 (BL1) is associated with genomic repair pathway deficiencies; basal-like 2 (BL2) is enriched in growth factor signaling-related genes; immunomodulatory (IM) is enriched in immunological signaling; and mesenchymal (MES) and mesenchymal stem–like (MSL) are enriched in components and pathways related to cell motility and the luminal androgen receptor (LAR), and androgen and metabolism genes are enriched [5]. Later, in 2015, Burstein described four subtypes, namely, LAR, MES, basal-like immune-suppressed (BLIS), and immune-activated (BLIA) subtypes [6]. One year later, the FUSCC classification introduced the immune-modulatory (IM) subtype, along with the known MES, BLIS and LAR subtypes [7].
All the above classifications are based on molecular profiling, which could be valuable at the patient level for precision medicine approaches once some mutations predict the benefit of targeted therapy. However, for most patients, the treatment options will remain limited. Moreover, technical challenges, such as the need for fresh tissue, the length of time needed to perform the analysis, and the significantly high costs, impact its wide use in standard practice [8,9].
Immunohistochemistry (IHC) is an established laboratory method for evaluating the presence of antigens that is widely used in breast cancer and is pivotal for tailoring systemic treatments (e.g., the human epidermal growth factor receptor 2—HER2) [10]. Moreover, IHC is significantly less expensive and laborious than gene expression and has been evaluated in several studies as a surrogate marker of established intrinsic genomic-based subtyping assays, as summarized in Table 1 [11,12,13,14,15,16,17,18]. Although some studies have provided survival data amongst the subtypes, the effect of chemotherapy on the pathological complete response, and if it serves as surrogate biomarker of survival, has not been reported.
Table 1.
Retrospective studies evaluating IHC as a surrogate for TNBC subtyping.
| Choi J et al., 2012 [11] | Kim S et al., 2018 [12] | Kumar S et al., 2020 [13] | Zhao S et al., 2020 [14] | Yoo T-K et al., 2021 [15] | Lian J et al., 2022 [16] | Leeha M et al., 2023 [17] | Hu H. et al. [18] | |||
|---|---|---|---|---|---|---|---|---|---|---|
| Total subjects | 122 | 200 | 245 | 210 | 183 | 214 | 145 | 93 | 195 | 123 |
| Methods used for subtyping | IHC | IHC | IHC | RNA and Gene expression and IHC staining | RNA and Gene expression and IHC staining | IHC | RNA and Gene expression and IHC staining | IHC | ||
| Adjuvant treatment | Chemo or radiation based on staging | NR | NR | ~93% (taxane 75.7% and non-taxane 17.6%) | ~90% (62.8% and 26.8%) | ~91% (84.1% and 7.0%) | NR | NR | ~ 90% (regimen not disclosed) | NR |
| IHC-Apocrine/LAR definition | AR and/or GGT1 > 10% | AR > 1% | AR ≥ 1% | AR ≥ 10% | AR Allred score 8 (5 + 3) | AR ≥ 10% | AR Allred score 8 (5 + 3) | AR ≥ 10%, regardless of the expression of other markers) | ||
| IHC-BLIS definition | NR | FOXC1 ≥ 4 and IDO-1 ≤ 10% | NR | AR–, CD8-, FOXC1 > 10% | NR | TIL low; AR < 10%; CD8 < 20%; FOXC1 ≥10% | NR | AR < 10%, CD8 TIL < 20%, FOX-C1 < 10%, and regardless of DCLK1 values | ||
| IHC-BLIA or IM definition | NR | IDO-1 > 10% and FOX-C1 < 4 | NR | AR– and CD8 TIL activated ≥20% | LAR-negative and TIL score > 70% | AR <10%; TIL high; CD8 ≥ 20% | LAR-negative and TIL score > 70% | AR < 10%, CD8 TIL ≥ 20%, and regardless of FOX-C1 and DCLK1 values | ||
| IHC-Basal definition | CK5/6 > 10% and/or EGFR moderate or intense | CK5/6 and/or EGFR > 1% | BL1: EGFR < 4, CK5/6 ≥ 4 and/or CK4/14 ≥ 4 | NR | LAR -, IM -, MES -, and with diffuse and strong p16 staining | NR | NR | CK5/6 and or EGFR+ | ||
| BL2: EGFR ≥ 4, irrespective of CK5/6 and/or CK4/14 result | ||||||||||
| IHC-Claudin-low/Mesenchymal definition | Claudin 3, 4, 7 negative and/or e-cadherin negative | Claudin-3 negative and or e-Cadherin negative | E-cadherin, Claudin 3 and 7 ≥ 4, Vimentin ≥ 4 | AR–CD8-FOXC1-DCLK1 ≥ 10% | LAR negative and TIL score < 20% | Metaplastic features; AR < 10%; CD8 < 20%; FOXC1 < 10% | LAR negative and TIL score < 20% | AR < 10%, CD8 TIL < 20%, FOX-C1 < 10% and DCLK1 ≥ 10%, | ||
| IHC-Mixed definition | 2 characteristics of 2 different subtypes | 2 or 3 different tumors | ≥2 of other categories | NR | NR | NR | NR | NR | ||
| IHC-Unclassifiable definition | Not belonging to any subtype | None of the above features | Did not fit in any category | AR–CD8-FOXC1-DCLK1- | All other manifestations | Not reported | All other manifestations | AR < 10%, CD8 TIL < 20%, FOX-C1 < 10% and DCLK1 < 10% | ||
| IHC-LAR rate | 12 (9.8%) | 22 (11%) | 41 (16.7%) | 60 (28.6%) | 42 (23%) | 53 (24.8%) | 26 (17.9%) | 23 (24.7%) | 37 (18.9%) | 28 (28.6%) |
| IHC-BLIS rate | NR | 11 (5.5%) | NR | 80 (38.1%) | 71 (38.8%) | 90 (42.1%) | NR | 39 (41.9%) | 103 (52.8%) | 20 (20.4%) |
| IHC-BLIA or IM rate | NR | 27 (13.5%) | NR | 40 (19.4%) | 34 (18.6%) | 39 (18.2%) | 21 (14.5%) | 24 (25.8%) | 34 (17.4%) | 39 (39.8%) |
| IHC-Basal rate | 27 (22.1%) | 85 (42.5%) | BL 36 (14.6%); BL1 32 (13.1%); BL2 4 (1.6%) | 120 (57.1%) | 105 (57.4%) | 129 (60.3%) | BL1 27 (18.6%) | 63 (67.7%) | 137 (70.2%) | |
| IHC-Mesenchymal rate | 28 (23%) | 23 (11.5%) | 70 (28.6%) | 16 (7.6%) | 18 (9.8%) | 17 (7.9%) | 44 (30.3%) | 7 (7.5%) | 1 (0.5%) | 11 (11.2%) |
| IHC-Mixed rate | 23 (18.9%) | 60 (30%) LAR + MES 8 (4%); LAR + BL 27 (13.5%); MES + BL 19 (9.5%); LAR + MES + BL 6 (3%) |
37 (15.1%) | 0 | 0 | 0 | NR | 0 | NR | NR |
| IHC-Unclassifiable rate | 32 (26.2%) | 10 (5%) | 61 (24.9%) | 14 (6.7%) | 18 (9.8%) | 15 (7%) | 18 (12.4%) | 0 | 20 (10.2%) | 25 (20.3%) |
| Confirmation method | no | no | no | mRNA | mRNA | no | mRNA | no | ||
| follow-up median | 59.5 months | 41 m (0–64) | 40 m (12–58) | 40.95 m (IQR 23.48–89.22) | 62 m (IQR 43–105) | |||||
| Disease-free survival (DFS) | Basal-like and unclassifiable show less favorable prognosis, mesenchymal and mixed intermediate and AR showed a better prognosis Ck 5/6 and Claudin positivity worse DFS |
BLIS—worse prognosis LAR, BLIA, BL and NOS—favorable This was also true for Burstein (4 subtypes). FOXC1–worse prognosis |
NA | IM (HR = 0.07), LAR (HR = 0.18), BLIS (HR = 0.26) better RFS than MES | MES worse RFS | NA | Significantly worse DFS for M subtype according to surrogate subtypes and although not clinically significant IM tends to be better survival | No significant difference Low recurrence 11 cases (11.83%) |
5 y 64.7% and no subtypes difference | IM-inflamed better DFS compared to others and BLIS the worse survival |
| Overall Survival (OS) | Cohesion disruption linked with worse survival | NA | Mesenchymal and unclassified shorted OS (68.2 and 69.2 m) | T + N + IHC was superior to T + N categories in time dependent AUC | NA | NA | NA | NA | 5 y OS = 65.0% IM significantly better OS but other did not differentiate between each other |
IM-inflamed better breast specific survival and BLIS the worse compared to others |
Legend: IHC—immunohistochemistry; LAR—luminal androgen receptor; AR—androgen receptor; RNA—ribonucleic acid; GGT1—gamma-glutamyl transferase 1; FOXC1—Forkhead Box C1; IDO-1—indoleamine 2,3 dioxygenase-1; CD8—cluster of differential 8; TIL—tumor infiltrating lymphocytes; CK—cytokeratin; EGFR—endothelial growth factor receptor; IM—immunomodulatory; M—mesenchymal; DCLK1—doublecortin like kinase 1; MES—mesenchymal; T—tumor; N—lymph node; AUC—area under the curve; IQR—interquartile range; NA—not applicable; NR—not reported.
In this study, we report the survival and pCR rates of patients who underwent IHC subtyping using our panel and who received neoadjuvant chemotherapy.
2. Results
One hundred eighty-seven women were included in this analysis; the mean age was 52.43 (SD = 12.79) years, the mean tumor size was 47.64 (SD = 53.61) millimeters, and the patients’ characteristics are summarized in Table 2.
Table 2.
Clinical and pathological summary.
| Variables | Mean | SD | |||
| Age | 52.42 | 12.79 | |||
| Tumor size | 47.64 | 53.61 | |||
| Number of positive lymph nodes (Mean (SD)) | 2.14 | 4.01 | |||
| ki67 (Mean (SD)) | 65.47 | 24.49 | |||
| Variables | Number of Subjects | Percentage | |||
| Clinical tumor(T) stage | T1–T2 | 58 | 31.0%) | ||
| T3 | 57 | (30.5%) | |||
| T4 | 72 | (38.5%) | |||
| Clinical lymph node (N) stage | N0 | 79 | (42.2%) | ||
| N1 | 78 | (41.7%) | |||
| N2 | 28 | (15.0%) | |||
| N3 | 2 | (1.1%) | |||
| Histologic subtype | Invasive ductal carcinoma | 176 | (94.2%) | ||
| other | 10 | 5.3% | |||
| NA | 1 | 0.5% | |||
| Tumor grade | 1 | 2 | 1.1% | ||
| 2 | 59 | 31.6% | |||
| 3 | 118 | 63.1% | |||
| NA | 8 | 4.8% | |||
| Angiolymphatic invasion | Yes | 98 | 52.4% | ||
| no | 39 | 20.9% | |||
| Not-assessed | 50 | 26.7% | |||
| Lymphatic infiltrate | Yes | 32 | 17.1% | ||
| No | 100 | 53.5% | |||
| Not-assessed | 55 | 29.4% | |||
| IHC-subtype | Basal-like | Unspecified | 36 | 19.6% | |
| Immunosuppressed | 57 | 31.0% | |||
| Imunoactivated | 20 | 10.9% | |||
| Luminal androgen receptor | 22 | 12.0% | |||
| Mesenchymal | 23 | 12.5% | |||
| Mixed | 21 | 11.4% | |||
| Unclassifiable | 4 | 2.2% | |||
| Not amendable of subtyping | 3 | 1.6% | |||
| Neoadjuvant chemotherapy | ACx4 + TXTx4 | 144 | 77% | ||
| ACx4 + wPacx12 | 19 | 10.2% | |||
| TCx4 | 5 | 2.7% | |||
| Other regimens | 19 | 10.2% | |||
| Surgery modality | Modified radical mastectomy | 120 | 64.2% | ||
| Conventional mastectomy | 17 | 9.1% | |||
| Conservative surgery | 50 | 26.7% | |||
| Pathologic response | Complete | 28 | 15.0% | ||
| Non-complete | 159 | 85.0% | |||
| Pathologic complete response according to IHC-subtype | Basal-like | Unspecified | 7 | 19.4% | |
| Immunosuppressed | 8 | 14.0% | |||
| Imunoactivated | 6 | 30.0% | |||
| Luminal androgen receptor | 1 | 4.5% | |||
| Mesenchymal | 4 | 17.4% | |||
| Mixed | 1 | 4.8% | |||
| Unclassifiable | 1 | 25.0% | |||
Legend: SD—standard deviation; N—number of patients; AC—anthracycline + cyclophosphamide; TXT—docetaxel; wPac—weekly paclitaxel; TC—docetaxel + platinum; x4—4 cycles; x12—12 cycles.
After balancing pros and cons from the antibodies used by studies presented in Table 1, we chose the following four for our analysis: IDO-1—Indoleamine 2,3-dioxygenase (IDO-1), Forkhead Box C1 (FOX-C1), claudin-3 [19], and androgen receptor. Staining for all 4 markers was possible in 98.4% (184s) of the patients and partially in 3 patients due to tissue exhaustion. We successfully identified the characteristics of 4 subtypes in 96.3% (183) of patients. Overall, the frequency of the IHC-basal-like (BL) subtype was 61% (114). The percentages of basal subtypes identified by IHC-BLIS and IHC-BLIA were 31% (57) and 10.9% (20), respectively. The second most common subtype was IHC-MES 12.5% (23), followed by IHC-LAR 12.0% (22) and IHC-mixed 11.4% (21) (Table 2).
Among the 28 (15%) patients who achieved pCR, 75% exhibited an IHC-BL, 14.28% exhibited an IHC-MES feature, and 7.4% exhibited an IHC-LAR feature. The pCR rate in the IHC-BLIA group was the highest (30%), and that in the IHC-LAR group was the lowest (4.5%) (p = 0.24) (Table 3).
Table 3.
Summary of the characteristics of patients who achieved a pathological complete response.
| Subject Number | Age | Clinical Stage (TNM) | Histological Subtype | Grade | Ki67(%) | Neoadjuvant Regimen (x Number of Cycles) | Subtype |
|---|---|---|---|---|---|---|---|
| Patient 1 | 66 | T4N1M0 | IDC | 2 | 90 | cx3 + wPacx3 | IHC-BLIS |
| Patient 2 | 63 | T3N0M0 | IDC | 3 | 5 | ACx4 + TXTx4 | IHC-unclassifiable |
| Patient 3 | 54 | T3N1M0 | IDC | 3 | 70 | ACx4 + TXTx4 | IHC-MES |
| Patient 4 | 67 | TxN2M0 | IDC | NR | 70 | ACx4 + TXTx4 | IHC-LAR |
| Patient 5 | 47 | T3N0M0 | IDC | 3 | 95 | ACx4 + TXTx4 | IHC-BLIS |
| Patient 6 | 60 | T4N2M0 | IDC | 3 | 80 | ACx4 + TXTx4 | IHC-BL-unspecific |
| Patient 7 | 47 | T4N1M0 | IDC | 3 | 80 | ACx4 + TXTx4 | IHC-BL-unspecific |
| Patient 8 | 52 | T4N1M0 | IDC | 3 | 90 | ACx4 + TXTx4 | IHC-LAR/BLIS |
| Patient 9 | 56 | T3N0M0 | IDC | 2 | 50 | ACx4 + TXTx4 | IHC-MES |
| Patient 10 | 44 | T3N1M0 | IDC | 3 | 95 | ACx4 + TXTx4 | IHC-BL-unspecific |
| Patient 11 | 61 | T4N2M0 | IDC | 2 | 70 | ACx4 + TXTx4 | IHC-BLIA |
| Patient 12 | 39 | T3N0M0 | Other | NR | 95 | ACx4 + TXTx4 | IHC-BLIS |
| Patient 13 | 47 | T2N0M0 | IDC | 2 | 95 | ACx4 + TXTx4 | IHC-BLIA |
| Patient 14 | 46 | T4N3M0 | IDC | 2 | 60 | ACx4 + TXTx4 | IHC-BL-unspecific |
| Patient 15 | 44 | T3N0M0 | IDC | 3 | 90 | ACx4 + TXTx4 | IHC-BLIS |
| Patient 16 | 68 | T4N0M0 | IDC | 2 | 75 | ACx4 + TXTx4 | IHC-BLIA |
| Patient 17 | 64 | T4N2M0 | IDC | 3 | 70 | TCx4 + ACx6 | IHC-BL-unspecific |
| Patient 18 | 41 | T3N0M0 | IDC | 3 | 70 | ACx4 + TXTx4 | IHC-BLIA |
| Patient 19 | 63 | T4N0M0 | IDC | 2 | 15 | ACx4 + TXTx4 | IHC-BLIA |
| Patient 20 | 34 | T4N0M0 | IDC | 3 | 100 | ACx4 + TXTx4 | IHC-BLIS |
| Patient 21 | 37 | T3N0M0 | IDC | 3 | 50 | ACx4 + TXTx4 | IHC-BLIS |
| Patient 22 | 71 | T2N1M0 | IDC | 2 | 50 | ACx4 + wPacx4 | IHC-BLIA |
| Patient 23 | 43 | T3N0M0 | IDC | 3 | 70 | ACx4 + TXTx4 | IHC-BLIS |
| Patient 24 | 47 | T2N0M0 | IDC | 2 | 5 | ACx4 + TXTx4 | IHC-MES |
| Patient 25 | 62 | T1N0M0 | IDC | 3 | 80 | ACx4 + TXTx4 | IHC-BL-unspecific |
| Patient 26 | 51 | T2N1M0 | IDC | 3 | 80 | ACx4 + TXTx4 | IHC-MES |
| Patient 27 | 27 | T2N0M0 | IDC | 3 | 95 | ACx4 + TXTx4 | IHC-BLIS |
| Patient 28 | 59 | T4N0M0 | IDC | 3 | 60 | ACx4 + wPacx4 | IHC-BL-unspecific |
Legend: T—tumor; N—lymph nodes; M—metastasis; IDC—invasive ductal carcinoma; NR—not reported; AC—anthracycline + cyclophosphamide; TXT—docetaxel; wPac—weekly paclitaxel; TC—docetaxel + platinum; x4—4 cycles; x3—3 cycles; IHC—Immunohistochemistry; BLIS—basal-like immunosuppressed; BLIA—basal-like immunoactivated; LAR—luminal androgen receptor; MES—Mesenchymal.
Patients who achieved pCR had a significantly better median disease-free (mDFS) survival NR (not reached) (CI—confidence interval: >50%) vs. no-pCR 30 m (months) (CI: 18-NR) (p = 0.00022). Overall, it was also significantly greater in patients who achieved pCR according to the NR (CI: >50%) than in those who did not achieve pCR according to the 58-m (CI: 40-NR) no-pCR (p = 0.00018). (Supplementary Figures S1 and S2).
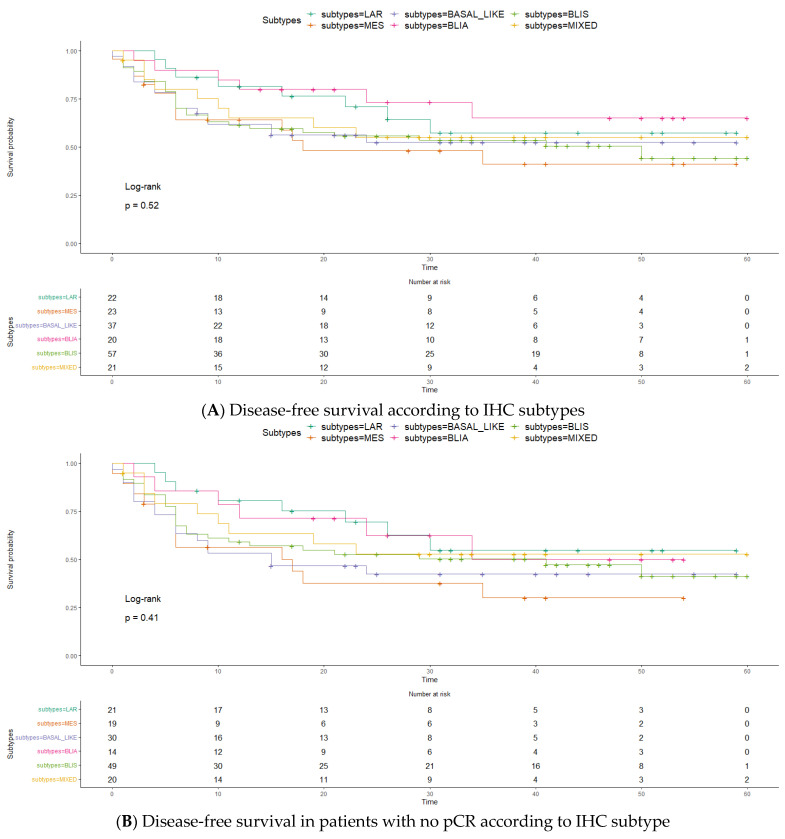
Most of the recurrences occurred in the first 20 months following surgery. mDFS did not significantly differ among subtypes (p = 0.52). (Figure 1A) IHC-BLIA demonstrated a greater mDFS for patients with NR (CI: 34-NR) than for patients with all other subtypes (CI: 23-NR). The mDFS was also NR for the IHC-LAR, IHC-mixed, and IHC-BL groups. IHC-BLIS patients had the second worst mDFS, 50 m (CI: 11-NR), and IHC-MES patients had a markedly short mDFS, 16 m (CI: 6-NR). Interestingly, the mDFS curves for patients who did not achieve pCR were less distinct among subtypes, suggesting that pCR has a crucial role regardless of intrinsic subtype. IHC-MES followed by IHC-BL showed worse survival: respectively, 17 m (CI: 6-NR) and 15 m (CI: 6-NR) (p = 0.41) (Figure 1B).
Figure 1.
Legend: BLIS basal-like immunosuppressed; BLIA—basal-like immunoactivated; LAR—luminal androgen receptor; MES—mesenchymal. The time, expressed in months.
Overall survival analysis also revealed no significant differences among subtypes (p = 0.61) (Figure 1C). IHC-BLIA had a greater mOS, NR (95% CI: NR > 50%) than the other subtypes at 60 m (95% CI: 48-NR) (p = 0.081). IHC-BLIA exhibit the graphically highest mOS, with an NR (95% CI: 39-NR) mOS for patients who did not achieve pCR and IHC-MES was associated with a worse survival with 37 m (95% CI: 27-NR) (p = 0.73) (Figure 1D).
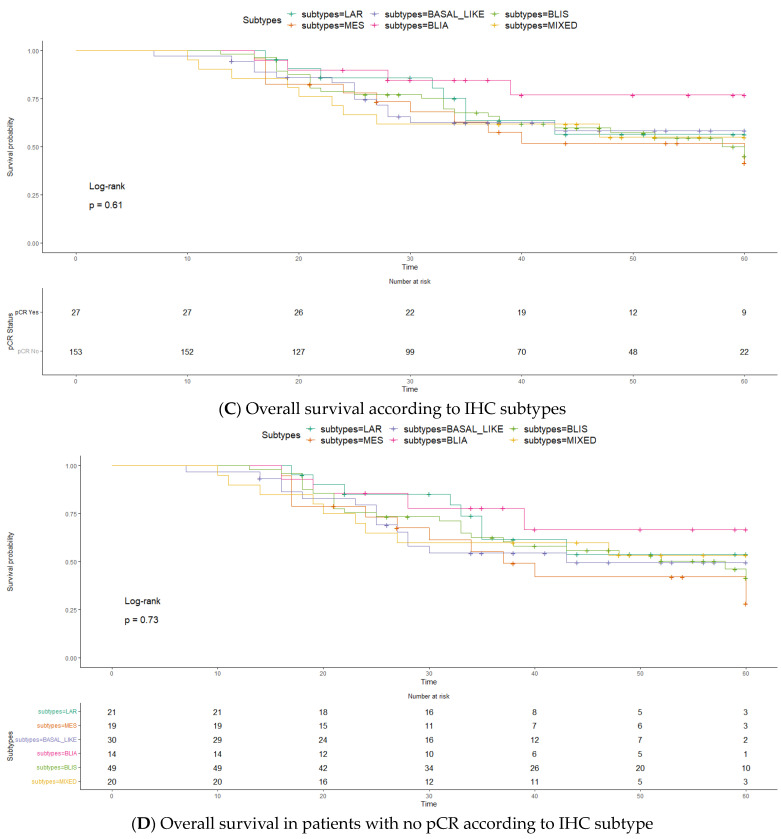
The pattern of recurrence was graphically distinct among subtypes, although not statistically significant. IHC-BLIS led recurrence in each category, and interestingly, no local or cerebral relapse occurred in patients with the IHC-LAR subtype (Figure 2).
Figure 2.
Pattern of recurrence among IHC subtypes. Legend: (A) Visceral recurrence; (B) Non-visceral/non-local/non-cerebral recurrence; (C) Local recurrence; (D) Cerebral recurrence. BLIS—basal-like immunosuppressed; BLIA—basal-like immunoactivated; LAR—luminal androgen receptor; MES—mesenchymal.
3. Discussion
This study is groundbreaking in terms of demonstrating pCR rates among TBNC subtypes using IHC. We found numerically higher pCR rates in the IHC-BLIA (30%) subgroup and a trend toward longer DFS and OS, while in the IHC-MES subgroup, survival was worse despite the pCR rate (17.4%) being closer to that of the whole population analyzed (15.0%). Achieving pCR was associated with longer disease-free and overall survival.
The basal-like subtype was predominant in our sample, with 61.5% of the tumors harboring a basal component. In 2010, Oakman, C. et al. reported higher rates of the BL phenotype in TNBC patients (71–91%) [20]. Interestingly, Lehmann et al. in 2011 reported that 49% of BL cases were characterized by intrinsic subtyping, but IHC seems to indicate a higher percentage (88%), and very likely, only half of these cases would correlate with the intrinsic BL subtype [5]. We observed rates somewhat closer to those reported by Zhao et al. and Jing Liang et al. [14,16] Identifying basal-like TNBC is clinically relevant, as data showed a benefit from adjuvant chemotherapy for patients with non-basal-like tumors and residual disease following surgery, despite the use of neoadjuvant chemotherapy [21,22].
We identified a predominance of IHC-BLIS (31.0%) over IHC-BLIA (10.9%) in our population, which likely contributed to the overall modest pathological response rate of 15.0%. Although our IHC-BLIS rates are somewhat comparable to the values found by the authors performing IHC subtyping, the overall percentage of patients with the IHC-BLIA subtype is markedly lower (Table 1). On the other hand, we found a numerically higher pCR rate in IHC-BLIA (30.0%) than the pCR rate in IHC-BLIS (14.0%), although not statistically significant. Based on recent publications, the new standard of care for early and high-risk TNBC patients includes immunotherapy alongside a taxane-platinum-based dose-dense chemotherapy, regardless of the presence of immune receptors/markers [23]. However, data are still needed to understand the efficacy of these regimens in TNBC patient subpopulations.
Immuno-inflammation occurred solely at the IHC-IM subtype according to Jing Lian et al. (2022), but a significant proportion of the other subtypes are immune-excluded, which raises the question of whether those subjects would benefit from immunotherapy in clinic [16].
IHC-MES was the second most common subtype, and numerically, it was associated with worse mDFS and mOS, which is consistent with the findings in the literature [13,14,15]. Unfortunately, the benefit of conventional adjuvant systemic treatment for this subtype is often poor, if any, given its specific molecular characteristics, which has motivated researchers to consider regimens mimicking sarcomatous disease [24]. Moreover, given the preclinical and clinical activity of mTOR, PI3K, SRC/ABL, and angiogenesis inhibitors, we believe that tailored treatment for this subtype could be warranted [2].
The IHC-LAR subtype had the lowest pCR rate (4.5%) and was the third most common subtype in our sample. A long-standing effort has been made to offer anti-androgen targeting for this subtype, with no translation in registrational approvals. The main challenges might include the unreliable behavior of AR as a driver in TNBC, compared to that of ER in HR+ disease, as well as the cutoff of AR intensity to trigger intervention and the high-bar endpoints chosen in clinical trials to evaluate the AR-targeting effect [25]. As mentioned above, the current best adjuvant treatment for patients with residual disease is capecitabine; however, for specific subtypes, such as LAR, the benefit is unclear. Therefore, to answer this question and by leveraging our knowledge of prostate cancer, where androgen deprivation therapy plus androgen receptor pathway inhibitors can be combined with docetaxel, we believe that a cohort of patients with IHC-LAR in a potential umbrella trial for intrinsic subtypes of TNBC should be considered to receive adjuvant capecitabine plus ARPI [26].
The pattern of recurrence we observed in our IHC-based subtyping cohort aligned with that expected in the literature (Table 1). Notably, brain relapse, a known independent factor of poor prognosis, occurred in 8% of the patients with IHC-MES, 14% in IHC-BLIS, and approximately 10% of those with the other IHC subtypes, but interestingly, no patients with IHC-LAR experienced brain relapse. There is a longstanding discussion on how to optimize relapse monitoring in high-risk breast tumors, but no clear consensus has been reached. Our data could assist in identifying patients with a greater risk of recurrence, which could deserve more individualized monitoring given specific patterns of disease relapse and therefore might benefit from brain and visceral imaging, as well as promising emerging techniques, such as circulating tumor DNA, in addition to the current recommended approaches [27].
Our study demonstrated a low percentage of unclassifiable (2.2%) and IHC-mixed (11.4%) compared to the other studies mentioned in Table 1. In a study conducted by Yoo in 2022, the majority of patients with IHC-unclassifiable had presented with mesenchymal subtype on genomic classification [15]. Interestingly, Zhao et al., Leeha et al., and Hu et al. did not report mixed subtypes by using their IHC panels [14,17,18]. We believe IHC-unclassifiable and IHC-mixed should be expected given the IHC assay limitations, and support the heterogeneous features of a significant proportion of TNBCs [28]. Although this population is smaller, we are conducting further research to elucidate how they should be handled, and, more specifically, the role of additional testing to better define this population.
Although the results of this study are promising, they should be interpreted in light of these limitations. Our retrospective design imposes challenges in survival analysis including selection and recall bias. The eventual changes in TNBC treatment protocols over the study period could introduce a confounding variable to the outcomes evaluated, as well as other variables not analyzed, such as comorbidities and genomic background. In the case of implementation, our proposed IHC panel will eventually increase in cost compared to the current standard of practice recommendation and could eventually cause delays in standard of practice results delivery. Moreover, there are several technical hurdles linked to standardizing IHC protocols for diagnostic protocols, including their validation and approval by regulatory bodies, which would be required before the panel we proposed is considered outside of a research environment. There is no consensus about the use of an IHC subtyping panel, and IHC staining was performed utilizing archival tumor tissue from 2008 onward, which could have impacted the performance of the assay and requires validation using an established method for intrinsic genomic subtyping.
4. Materials and Methods
4.1. Sample Selection and Outcome Definitions
Patients with localized or locally advanced TNBC who were treated with neoadjuvant chemotherapy followed by curative surgery at the same institution between January 2008 and December 2017 and who had available biopsy and surgical specimens met the inclusion criteria for this retrospective cohort.
From medical files, clinical and pathological data were collected to construct a database using an electronic case report form (Supplementary file S1.).
For this study, TNBC was defined as estrogen and progesterone receptor < 1% and HER2-negative +1 or +2 without fish amplification. Pathological complete response (pCR) was defined as the absence of invasive cancer on surgical specimens from the breast and axilla (ypT0/Tis pN0). Disease-free survival (DFS) was defined as the time between the day of the cycle of one day of chemotherapy regimen administration until cancer recurrence or cancer-related death. Overall survival (OS) was defined as the time between the day of the cycle one day after chemotherapy regimen administration until death related to any cause. In the case of loss of follow-up, the appointment date at the NCI, which contains information about disease and survival, was used to censor the patient for the analysis.
4.2. IHC Analysis and Interpretation
Tissue samples were converted into histological sections on previously salinized slides. Evaluation of the cellular atypia pattern was performed by hematoxylin-eosin (HE) staining. The evaluated tumor area was selected by a pathologist, and the in situ regions within the invasive tumors were also delineated to allow a better evaluation of the stains. Tissue sections were immunoassayed with a Polymer Detection System (RE7150-K, Leica Biosystems Newcastle Ltd., Balliol Business Park West, Benton Lane, Newcastle Upon Tyne NE12 8EW, UK) according to the protocol established by the manufacturer. Primary antibodies were incubated with the tissues for 18 h at 4 °C at different dilutions determined by titration, as shown in Table 4.
Table 4.
Antibodies used in the analysis.
| Antibody | Definition of Positivity Expression | Brand | Dilution | Control |
|---|---|---|---|---|
| IDO-1 | >10% of tumor cells | Abcam *, Cambridge, UK | 1:1000 | Breast |
| Claudin-3 | Allred score ≥ 4 | Abcam *, Cambridge, UK | 1:200 | Breast |
| Androgen Receptor | ≥20% of tumor cells | Cell Marque™, California, US | 1:400 | Gallbladder |
| FOX-C1 | Moderate (M) or intense (I) | Abcam *, Cambridge, UK | 1:300 | Breast |
| Ki-67 | ≥1% of tumor cells | Ventana®-Roche, Rotkreuz, Switzerland | Ready to use | Breast |
Legend: IDO-1—Indoleamine 2,3-dioxygenase, FOX-C1—Forkhead Box C1. * abcam is a registered trademark of Abcam Plc.
The antibody panel was adapted from studies reported in Table 1 and interpretation of the singleplex IHC staining results was performed by the author F.R., as shown in Table 5.
Table 5.
Immunohistochemistry analysis and interpretation.
| IHC-Subtype | Antibody Results | |||||
|---|---|---|---|---|---|---|
| IDO-1 | FOX-C1 | AR | Claudin-3 | |||
| Basal-like unspecific | IDO-1 ≤ 10% and FOX-C1 < 4 or IDO > 10% and FOX-C1 ≥ 4 |
<10% | W, M or I | |||
| Basal-like immune-suppressed | ≤10% | ≥4 | <10% | |||
| Basal-like immune-activated | >10% | <4 | <10% | |||
| Luminal androgen receptor | ≤10% | <4 | ≥10% | |||
| Mesenchymal | any | any | any | 0 | ||
| Mixed (criteria for ≥ 2 subtypes) | BLIS | LAR | ≤10% | ≥4 | ≥10% | W, M or I |
| BLIA | LAR | >10% | <4 | ≥10% | ||
| BL | LAR | IDO-1 ≤ 10% and FOX-C1 < 4 or IDO > 10% and FOX-C1 ≥ 4 |
≥10% | |||
| MES | LAR | any | any | ≥10% | 0 | |
| Unclassifiable | ≤10% | ≤2 | <5% | W, M or I | ||
Legend: IHC—immunohistochemistry; BL—basal-like; BLIS—basal-like immunosuppressed; BLIA—basal-like immunoactivated; LAR—luminal androgen receptor; MES—mesenchymal; W—weak; M—moderate; I—intense; IDO-1—indoleamine 2,3-dioxygenase (IDO-1), FOX-C1—Forkhead Box C1; AR—androgen receptor.
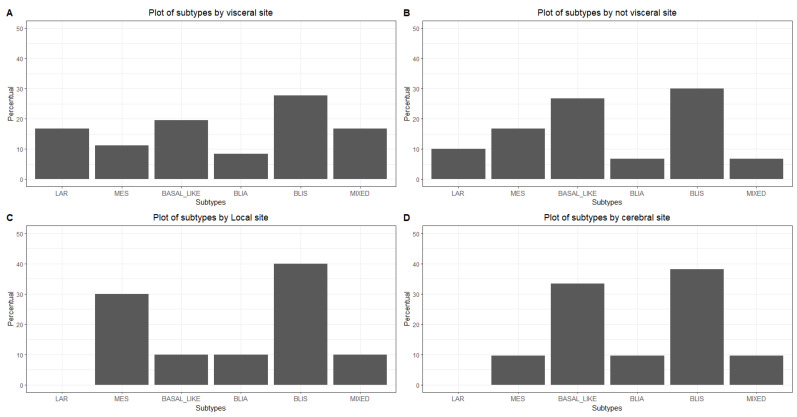
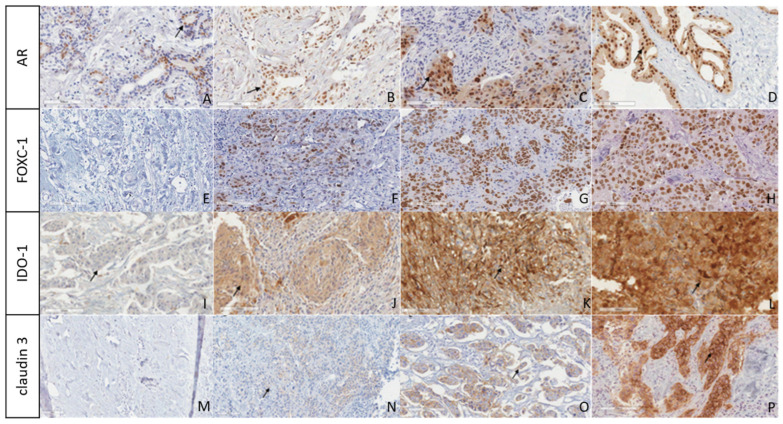
The scoring was reviewed by the senior authors E.A., and the final scores agreed between F.R. and E.A. The digitalization was performed using the Aperio Scanner and a representative illustration of the staining is shown in Figure 3.
Figure 3.
Immunostaining panel of tumor samples. Legend: Anti-AR immunostaining nuclear expression was observed in 10–30% (A), 31–50% (B), 51–75% (C), and 76–100% (D). Anti-FOXC1 immunostains were stratified according to nuclear staining intensity: negative (E), 4+ (F), 6+ (G), and 8+ (H). Anti-IDO1 immunostains were stratified according to the intensity of cytoplasmic staining in the tumor region as: ≤10% (I), 50% (J), 80% (K), and 100% (L). Anti-claudin immunostains were stratified according to the intensity of membrane staining in the tumor region as negative (M), weak (N), moderate (O), and intense (P). Magnification: 20×. Scale bar: 100 µm.
For positive controls, tissues suggested by the antibody manufacturer’s datasheets were used. The reaction was visualized using diaminobenzidine (DAB), followed by hematoxylin counterstaining. Negative controls were prepared without the primary antibody. The positivity of the staining was analyzed in ten random fields and determined by manual counting using ImageJ version 1.54 [29] software according to the preestablished equation below.
Sc represents the number of stained cells in each field, where s = [1, 2, ∙∙∙, 10]; Tc represents the total number of cells in each field, where t = [1, 2, ∙∙∙, 10]; and p represents the mean percentage of positivity.
4.3. Statistical Analysis
Continuous variables are shown as the mean and standard deviation, and categorical variables are shown as the total value and percentage of the total value.
The time to overall survival was computed as the time of diagnosis until death or the last patient contact, and the disease-free survival time was computed as the time of surgery until recurrence or last patient contact.
The Kaplan–Meier method was sed to estimate survival curves, and the log rank test was performed to evaluate whether there were differences in covariate levels via univariate analysis. The significance level adopted to reject the null hypothesis was alpha equal to 0.05. A bar plot was used to demonstrate the frequency of subtypes at each site.
5. Conclusions
We successfully demonstrated that an affordable and widely reproducible panel of IHC assays can be used to subtype TNBC. Moreover, we were the first to demonstrate the pCR rate among IHC subtypes.
Acknowledgments
We acknowledge the support of patients treated at NCI Brazil, which contributed to this research, as well as the site personnel’s dedication to research.
Supplementary Materials
The supporting information can be downloaded at https://www.mdpi.com/article/10.3390/ijms25115825/s1.
Author Contributions
Conceptualization, B.d.P., S.C. and E.A.; methodology, B.d.P., S.C., P.V., F.R., C.A.M.d.S. and E.A.; software, B.d.P., C.A.M.d.S. and E.A.; validation, P.V. and E.A.; formal analysis, B.d.P., S.C., C.A.M.d.S. and E.A.; investigation, B.d.P., S.C., P.V., F.R., C.A.M.d.S. and E.A.; resources, B.d.P., S.C., P.V., F.R., C.A.M.d.S. and E.A.; data curation, B.d.P., S.C., C.A.M.d.S. and E.A.; writing—original draft preparation, B.d.P., S.C., C.A.M.d.S. and E.A.; writing—review and editing, B.d.P., S.C., P.V., F.R., C.A.M.d.S. and E.A.; visualization, B.d.P., S.C., C.A.M.d.S. and E.A.; supervision, S.C. and E.A.; project administration, B.d.P., S.C., C.A.M.d.S. and E.A.; funding acquisition, E.A. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Review Board (or Ethics Committee) of the National Cancer Institute (NCI) in Rio de Janeiro Brazil Ethics Committee, under the number CAAE: 22893219.1.0000.5274.
Informed Consent Statement
Patient consent was waived due to the retrospective nature of this research and lack of impact on the clinical decision, which was already taken before the study.
Data Availability Statement
Authors are open to discuss data sharing on the terms of the National Cancer Institute.
Conflicts of Interest
The authors declare no conflicts of interest.
Funding Statement
This research was funded by the Conselho Nacional de Desenvolvimento Cientifico e Tecnologico (CNPq) grant no. 210.462/2021.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Cancer Research UK . Triple Negative Breast Cancer. Cancer Research UK; London, UK: 2023. [(accessed on 1 March 2023)]. Available online: https://www.cancerresearchuk.org/about-cancer/breast-cancer/types/triple-negative-breast-cancer. [Google Scholar]
- 2.de Paula B., Kieran R., Koh S.S., Crocamo S., Abdelhay E., Muñoz-Espín D. Targeting Senescence as a Therapeutic Opportunity for Triple-Negative Breast Cancer. Mol. Cancer Ther. 2023;22:583–598. doi: 10.1158/1535-7163.MCT-22-0643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rala de Paula B.H., Kumar S., Morosini F.M., Cardoso D.E.C., de Sousa C.A., Crocamo S. Real-world assessment of the effect of impact of tumor size on pathological complete response rates in triple negative breast cancer after neoadjuvant chemotherapy. Chin. Clin. Oncol. 2020;9:78. doi: 10.21037/cco-20-111. [DOI] [PubMed] [Google Scholar]
- 4.Marra A., Trapani D., Viale G., Criscitiello C., Curigliano G. Practical classification of triple-negative breast cancer: Intratumoral heterogeneity, mechanisms of drug resistance, and novel therapies. NPJ Breast Cancer. 2020;6:54. doi: 10.1038/s41523-020-00197-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lehmann B.D., Bauer J.A., Chen X., Sanders M.E., Chakravarthy A.B., Shyr Y., Pietenpol J.A. Identification of human triple-negative breast cancer subtypes and preclinical models for selection of targeted therapies. J. Clin. Investig. 2011;121:2750–2767. doi: 10.1172/JCI45014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Burstein M.D., Tsimelzon A., Poage G.M., Covington K.R., Contreras A., Fuqua S.A., Savage M.I., Osborne C.K., Hilsenbeck S.G., Chang J.C., et al. Comprehensive Genomic Analysis Identifies Novel Subtypes and Targets of Triple-Negative Breast Cancer. Clin. Cancer Res. 2015;21:1688–1698. doi: 10.1158/1078-0432.CCR-14-0432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Liu Y.-R., Jiang Y.-Z., Xu X.-E., Yu K.-D., Jin X., Hu X., Zuo W.-J., Hao S., Wu J., Liu G.-Y., et al. Comprehensive transcriptome analysis identifies novel molecular subtypes and subtype-specific RNAs of triple-negative breast cancer. Breast Cancer Res. 2016;18:33. doi: 10.1186/s13058-016-0690-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bianchini G., De Angelis C., Licata L., Gianni L. Treatment landscape of triple-negative breast cancer—Expanded options, evolving needs. Nat. Rev. Clin. Oncol. 2022;19:91–113. doi: 10.1038/s41571-021-00565-2. [DOI] [PubMed] [Google Scholar]
- 9.Yang R., Li Y., Wang H., Qin T., Yin X., Ma X. Therapeutic progress and challenges for triple negative breast cancer: Targeted therapy and immunotherapy. Mol. Biomed. 2022;3:8. doi: 10.1186/s43556-022-00071-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rossi C., Fraticelli S., Fanizza M., Ferrari A., Ferraris E., Messina A., Della Valle A., Anghelone C.A.P., Lasagna A., Rizzo G., et al. Concordance of immunohistochemistry for predictive and prognostic factors in breast cancer between biopsy and surgical excision: A single-centre experience and review of the literature. Breast Cancer Res. Treat. 2023;198:573–582. doi: 10.1007/s10549-023-06872-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Choi J., Jung W.-H., Koo J.S. Clinicopathologic features of molecular subtypes of triple negative breast cancer based on immunohistochemical markers. Histol. Histopathol. 2012;27:1481–1493. doi: 10.14670/HH-27.1481. [DOI] [PubMed] [Google Scholar]
- 12.Kim S., Moon B.-I., Lim W., Park S., Cho M.S., Sung S.H. Feasibility of Classification of Triple Negative Breast Cancer by Immunohistochemical Surrogate Markers. Clin. Breast Cancer. 2018;18:e1123–e1132. doi: 10.1016/j.clbc.2018.03.012. [DOI] [PubMed] [Google Scholar]
- 13.Kumar S.M., Bal A.M., Das A.M., Bhattacharyya S., Laroiya I., Khare S., Singh G. Molecular Subtyping of Triple Negative Breast Cancer by Surrogate Immunohistochemistry Markers. Appl. Immunohistochem. Mol. Morphol. 2020;29:251–257. doi: 10.1097/PAI.0000000000000897. [DOI] [PubMed] [Google Scholar]
- 14.Zhao S., Ma D., Xiao Y., Li X.-M., Ma J.-L., Zhang H., Xu X.-L., Lv H., Jiang W.-H., Yang W.-T., et al. Molecular Subtyping of Triple-Negative Breast Cancers by Immunohistochemistry: Molecular Basis and Clinical Relevance. Oncologist. 2020;25:e1481–e1491. doi: 10.1634/theoncologist.2019-0982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yoo T.-K., Kang J., Lee A., Chae B.J. A triple-negative breast cancer surrogate subtype classification that correlates with gene expression subtypes. Breast Cancer Res. Treat. 2022;191:599–610. doi: 10.1007/s10549-021-06437-8. [DOI] [PubMed] [Google Scholar]
- 16.Lian J., Ma H.-X., Xu E.-W., Bu P., Yun K.-M., Xi Y.-F. Subclassifying triple-negative breast cancers and its potential clinical utility. Virchows Arch. 2022;481:13–21. doi: 10.1007/s00428-022-03329-0. [DOI] [PubMed] [Google Scholar]
- 17.Leeha M., Kanokwiroon K., Laohawiriyakamol S., Thongsuksai P. Immunohistochemistry-based molecular subtyping of triple-negative breast cancer and its prognostic significance. Pathol. Oncol. Res. 2023;29:1611162. doi: 10.3389/pore.2023.1611162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hu H., Tong K., Tsang J., Ko C., Tam F., Loong T., Tse G. Subtyping of triple-negative breast cancers: Its prognostication and implications in diagnosis of breast origin. ESMO Open. 2024;9:102993. doi: 10.1016/j.esmoop.2024.102993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jääskeläinen A., Soini Y., Jukkola-Vuorinen A., Auvinen P., Haapasaari K.-M., Karihtala P. High-level cytoplasmic claudin 3 expression is an independent predictor of poor survival in triple-negative breast cancer. BMC Cancer. 2018;18:223. doi: 10.1186/s12885-018-4141-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Oakman C., Viale G., Di Leo A. Management of triple negative breast cancer. Breast. 2010;19:312–321. doi: 10.1016/j.breast.2010.03.026. [DOI] [PubMed] [Google Scholar]
- 21.Lluch A., Barrios C.H., Torrecillas L., Ruiz-Borrego M., Bines J., Segalla J., Guerrero-Zotano Á., García-Sáenz J.A., Torres R., de la Haba J., et al. Phase III Trial of Adjuvant Capecitabine After Standard Neo-/Adjuvant Chemotherapy in Patients with Early Triple-Negative Breast Cancer (GEICAM/2003-11\_CIBOMA/2004-01) J. Clin. Oncol. 2020;38:203–213. doi: 10.1200/JCO.19.00904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mayer I.A., Zhao F., Arteaga C.L., Symmans W.F., Park B.H., Burnette B.L., Tevaarwerk A.J., Garcia S.F., Smith K.L., Makower D.F., et al. Randomized Phase III Postoperative Trial of Platinum-Based Chemotherapy Versus Capecitabine in Patients with Residual Triple-Negative Breast Cancer Following Neoadjuvant Chemotherapy: ECOG-ACRIN EA1131. J. Clin. Oncol. 2021;39:2539–2551. doi: 10.1200/JCO.21.00976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Han H.S., Vikas P., Costa R.L., Jahan N., Taye A., Stringer-Reasor E.M. Early-Stage Triple-Negative Breast Cancer Journey: Beginning, End, and Everything in Between. Am. Soc. Clin. Oncol. Educ. B. 2023;43:e390464. doi: 10.1200/EDBK_390464. [DOI] [PubMed] [Google Scholar]
- 24.Yin L., Duan J.-J., Bian X.-W., Yu S. Triple-negative breast cancer molecular subtyping and treatment progress. Breast Cancer Res. 2020;22:61. doi: 10.1186/s13058-020-01296-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Xu M., Yuan Y., Yan P., Jiang J., Ma P., Niu X., Ma S., Cai H., Yang K. Prognostic Significance of Androgen Receptor Expression in Triple Negative Breast Cancer: A Systematic Review and Meta-Analysis. Clin. Breast Cancer. 2020;20:e385–e396. doi: 10.1016/j.clbc.2020.01.002. [DOI] [PubMed] [Google Scholar]
- 26.Fizazi K., Foulon S., Carles J., Roubaud G., McDermott R., Fléchon A., Tombal B., Supiot S., Berthold D., Ronchin P., et al. Abiraterone plus prednisone added to androgen deprivation therapy and docetaxel in de novo metastatic castration-sensitive prostate cancer (PEACE-1): A multicentre, open-label, randomised, phase 3 study with a 2 × 2 factorial design. Lancet. 2022;399:1695–1707. doi: 10.1016/S0140-6736(22)00367-1. [DOI] [PubMed] [Google Scholar]
- 27.Aldrich J., Canning M., Bhave M. Monitoring of Triple Negative Breast Cancer After Neoadjuvant Chemotherapy. Clin. Breast Cancer. 2023;23:832–834. doi: 10.1016/j.clbc.2023.08.001. [DOI] [PubMed] [Google Scholar]
- 28.Asleh K., Riaz N., Nielsen T.O. Heterogeneity of triple negative breast cancer: Current advances in subtyping and treatment implications. J. Exp. Clin. Cancer Res. 2022;41:265. doi: 10.1186/s13046-022-02476-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Schneider C.A., Rasband W.S., Eliceiri K.W. NIH Image to ImageJ: 25 years of image analysis. Nat. Methods. 2012;9:671–675. doi: 10.1038/nmeth.2089. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Authors are open to discuss data sharing on the terms of the National Cancer Institute.