The bacterium Helicobacter pylori can infect the stomach during childhood and cause lifelong chronic gastritis, which can lead to peptic ulcer disease. Curing H pylori infection cures ulcer disease.1–5 And since reinfection in adults is extremely rare,6 adequate treatment permanently cures this former chronic recurrent, serious disease. If ulcers do not recur neither do ulcer perforation or bleeding; quality of life increases,7 sick leave decreases, and less money is spent on visiting the doctor and drugs.
Antibiotic resistance needs to be taken into account when designing treatment for H pylori infection.8 Over the past decade many different therapies were promoted and recommendations changed rapidly. Most doctors lost track, and a great variety of treatments is being used.9 In this article we will try to provide a basic framework on which treatment can be based.
Summary points
The therapeutic goal is to cure H pylori infection in all ulcer patients
Several equally effective regimens are available, but even the best fail in 5-20% of patients
Antibiotic resistance is usually induced after failure, and initial regimens should not compromise future therapeutic possibilities
Doctors should choose two complementary regimens, which if used consecutively come close to 100% cure
Treatment should start with a regimen based on clarithromycin with a back up regimen based on metronidazole unless resistance is above 15%, in which case the order should be reversed
Triple regimens which combine clarithromycin and metronidazole should not be used as there is no valid empirical back up regimen after failure
Methods
This article is based largely on our experience in treating H pylori infection. We base our recommendations on basic bacteriological principles and on a regularly updated in-house computer database that contains the results of all published therapeutic studies.
Who should be treated?
Treatment to eradicate H pylori in patients with a proved ulcer is cost effective and benefits the patient and society.10 All patients with a history of ulcers, who often use acid suppressants on demand, therefore need to be identified and treated.3 Whether patients without ulcers benefit from antibiotics is unclear. Empirical antibiotic treatment has been suggested for dyspepsia in order to cure all patients with “hidden” ulcer.11 In populations with a high incidence of ulcer disease it might be cheaper to prescribe antibiotics to all dyspeptic patients positive for H pylori than to investigate all dyspeptic patients to identify those with ulcers.
Selecting a regimen
An evidence based choice of treatment is impossible because we lack large randomised trials comparing the highly effective regimens.4,8,9,11–13 Dual treatment with proton pump inhibitors is now obsolete due to lack of efficacy. Several triple or quadruple therapies have been sufficiently investigated and seem to be able to cure either 80% (intention to treat) or 90% (per protocol) of patients. The table shows currently useful treatments, but none has surfaced as the final treatment of choice. Metronidazole (or tinidazole) and clarithromycin are the two key antibiotics. Antibiotic resistance against these two drugs, either primary or induced after treatment, is clinically important.8
Dual treatments
Dual treatments combining a proton pump inhibitor with either amoxicillin or clarithromycin were popular a few years ago as they were easy to explain and well tolerated. They have now been abandoned because they were not very effective. The newer regimen of 14 days' treatment with ranitidine bismuth citrate plus clarithromycin is effective and has few side effects. In randomised trials it was superior to other dual treatments.14–16 It is easy to take and therefore attractive for general practice.
Triple treatments
Triple treatment with a bismuth compound, tetracycline (or amoxicillin), and metronidazole is cheap and well investigated.2,4,5,7–9,11,13 It may cause side effects, but these are usually not severe and have not led to non-compliance in trials.17,18 It reaches high cure rates in metronidazole sensitive strains after seven days2,8 but requires 14 days to eradicate a substantial percentage of resistant strains.2,8,18 This regimen is widely used in cost sensitive markets, but even in the United States it is still popular.19
Bismuth triple therapy has mainly been surpassed by seven day triple regimens using proton pump inhibitors; these combine omeprazole, lansoprazole, or pantoprazole with two antibiotics. Most studies use the antibiotics twice daily. There is some evidence that the optimal dose is 20 mg twice daily for omeprazole, 30 mg twice daily for lansoprazole,20 and 40 mg twice daily for pantoprazole.21 The appropriate antibiotics are metronidazole (or tinidazole), amoxicillin, and clarithromycin. Several guidelines recommend proton pump inhibitor triple regimens as first line treatment.4–6,11 Proton pump inhibitors are most commonly combined with amoxicillin 1000 mg twice daily and clarithromycin 500 mg twice daily. This regimen has fewer side effects then other triple regimens,22 but it is only moderately effective in clarithromycin resistant strains and secondary resistance is usually induced when treatment fails.
Proton pump inhibitors are sometimes combined with amoxicillin and metronidazole twice or thrice daily. This regimen is only moderately effective in metronidazole resistant strains over seven days.8,18,23,24 In areas with a high prevalence of resistance treatment should be increased to 10 or 14 days.18 Regimens combining proton pump inhibitors with metronidazole 400 or 500 mg and clarithromycin 250 mg or 500 mg twice daily are less effective in patients with primary metronidazole or clarithromycin resistance.22,24,25 If treatment fails the regimen may induce resistance against one or both of the antibiotics used in this regimen.
A new group of triple regimens has been developed that replaces proton pump inhibitors with ranitidine bismuth citrate. These produce less acid suppression but provide the additional antimicrobial action of bismuth. In most patients with sensitive strains replacing proton pump inhibitors with ranitidine bismuth citrate will not increase efficacy, but it might prevent induction of resistance when treatment fails. The cure rate may also be improved in patients with resistant strains, although a very large study will be needed to prove this. So far no clinically important differences have been found in randomised trials directly comparing triple regimens with proton pump inhibitors and those with ranitidine bismuth citrate.
Quadruple treatments
Addition of acid suppressants increases the efficacy of bismuth triple regimens.26 Quadruple treatment is more effective with proton pump inhibitors then with histamine-2 receptor antagonists17 and when tetracycline and metronidazole are incorporated. In meta-analyses the quadruple regimen had the highest cure rates,5,6,12 but it is also the most complicated regimen with the greatest number of tablets each day. Nevertheless, studies have found good compliance, with a drop out rate comparable with that of the easier triple therapies.17 A course of seven days seems to cure both metronidazole sensitive and resistant strains; sensitive strains are eradicated in four days.8 The high cure rate at day 4 shows its potency and wide therapeutic window.
Second line treatment
Eradication is more difficult with second line treatment,27 and repeated regimens might need to be prolonged. Some bacteria can be killed easily (steep kill curve) and other bacteria are more difficult to kill. During treatment the substrains with the steepest kill curve will disappear first. The bacteria that are the least susceptible remain if treatment fails. Bacteria of this “difficult to kill” substrain then increase their numbers and repopulate the stomach. Moreover such remaining strains may also have become resistant against one or both key antibiotics.28 For obvious reasons patients who do not comply with treatment are overrepresented among those whose treatment fails. These factors may explain the lower cure rates with retreatment. Some authors have reported that in some patients the infection cannot be eradicated,27 but in our experience this is rare.
Quadruple regimens have been suggested as the optimal second line treatment.11 Although they have been used successfully after failure of regimens containing clarithromycin,29–32 results after regimens containing metronidazole were disappointing.33,34 The large number of “difficult to kill” H pylori which have also become resistant to metronidazole is giving concern. This shows that there is as yet no ideal second line treatment.
Logical framework for treatment
If initial antibiotic treatment fails, another attempt must follow and if necessary a third or fourth until the infection is cured in 100% of cases. Ideally follow up treatment should be guided by susceptibility data, but this information is often unavailable. No ulcer patient should be discharged until there is documented proof by endoscopy, breath test, or six month follow up serology that H pylori is eliminated.35 None of the regimens in the table is inferior or superior to another. Even the best regimens fail in 5-20% of cases. We therefore need to focus on what we have to offer to those who are not cured. Since treatment to eradicate H pylori is increasing, the number of failures will rise and be of increasing clinical importance. Many of these patients will be referred for specialist care.
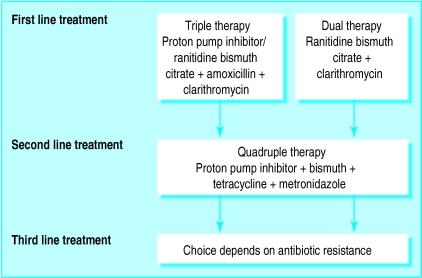
The choice of a second line treatment depends on which treatment was used initially. If a clarithromycin based regimen was used a metronidazole based regimen should be used afterwards, and vice versa (fig 1). It seems unwise to use the same antibiotic twice. Doctors should choose a set of two treatment regimens that complement each other and which if used consecutively come close to the desired 100% cure.
Figure 1.
General principles of treatment to eradicate H pylori
The first choice should not be a regimen that combines clarithromycin and metronidazole. Although this regimen is very effective, patients who are not cured will have at least single, and usually double, resistance,33,34,36,37 and no logical empirical treatment remains afterwards. This is particularly important in areas with a high prevalence of primary metronidazole resistance, where more treatment failures and thus more double resistance will occur.37 Double resistance could become a serious clinical problem. Endoscopy with culture and susceptibility testing is therefore essential after these regimens in all patients, and especially in patients with positive breath test results, to select further options.
If instead the initial treatment uses either metronidazole or clarithromycin combined with another antibiotic the choice of second line treatment is clear from the beginning and does not depend on culture results. An easier and cheaper follow up schedule can therefore be used with these regimens.35 Culture and susceptibility testing are required only after a failed second attempt to select a third line treatment (fig 1).
Future trials are needed to study consecutive combinations of treatments. Authors must focus on reporting antimicrobial susceptibility before and after treatment8,28 and on finding the optimal complementary “back up” regimen to their initial treatment.
Recommendations for treatment
Local (geographical) prevalence of antimicrobial resistance will determine whether it is better to start with a regimen based on clarithromycin or one based on metronidazole.8,28 Presently clarithromycin resistance is below 10% in most populations. Treatment can therefore usually start with a regimen based on clarithromycin with a seven day quadruple regimen (proton pump inhibitor, bismuth, tetracycline, and metronidazole) as second line treatment (fig 2). Different antibiotics are used in subsequent attempts, and two prospective studies show over 98% overall cure with this approach.31,32 Ranitidine bismuth citrate plus clarithromycin is used for patients with penicillin allergy. Regimens based on metronidazole should be used first if clarithromycin resistance is over 15%. Triple regimens using metronidazole are less effective in primary metronidazole resistant strains,8,18,23,24 but the quadruple regimen seem to perform well.8,26 It can therefore be used in almost all populations, and we recommend the quadruple regimen as first line treatment when clarithromycin resistance is a problem. Metronidazole based triple regimens can, however, safely be used in areas with a low prevalence of metronidazole resistance.
Figure 2.
Recommended treatment strategy in areas with low primary prevalence of clarithromycin resistance
Regimens containing both clarithromycin and metronidazole are no more effective than regimens with only one of these antibiotics. Because of problems with resistance we suggest that both key antibiotics should not be used together until a valid empirical back up regimen is available.
In general the likelihood of cure can be increased by increasing the length of treatment. Although seven day treatment is standard for proton pump inhibitor and ranitidine bismuth citrate triple regimens, the success rate can be improved by prescribing a 10-14 day course in patients who have had previous failure or in whom the consequence of failure could be life threatening—for example, patients presenting with complications of ulcer such as bleeding.
Table 1.
Treatment regimens which have been repeatedly shown to be effective in eradicating H pylori
| Length of treatment (days) | Component drugs | |||
|---|---|---|---|---|
| Regimens based on clarithromycin | ||||
| 14 | Ranitidine bismuth citrate 400 mg twice daily | Clarithromycin 500 mg twice daily | ||
| 7-10 | Ranitidine bismuth citrate 400 mg twice daily | Amoxicillin 1000 mg twice daily | Clarithromycin 500 mg twice daily | |
| 7-10 | Proton pump inhibitor twice daily | Amoxicillin 1000 mg twice daily | Clarithromycin 500 mg twice daily | |
| Regimens based on metronidazole (or tinidazole) | ||||
| 14 | Bismuth compound 4 times/day | Tetracycline 500 mg 4 times/day | Metronidazole 400-500 mg 3-4 times/day | |
| 7-10 | Proton pump inhibitor twice daily | Amoxicillin 500 mg 2-3 times/day | Metronidazole 400-500 mg 2-3 times/day | |
| 4-7 | Proton pump inhibitor twice daily | Colloidal bismuth subcitrate 4 times/day | Tetracycline 500 mg 4 times/day | Metronidazole 400-500 mg 3-4 times/day |
| Regimens based on clarithromycin plus metronidazole (or tinidazole) | ||||
| 7 | Ranitidine bismuth citrate 400 mg twice daily | Clarithromycin 500 mg twice daily | Metronidazole 400-500 mg twice daily | |
| 7 | Proton pump inhibitor twice daily | Clarithromycin 500 mg twice daily | Metronidazole 400-500 mg twice daily | |
Acknowledgments
Competing interests: Both authors have received funding for speaking or research projects from many different pharmaceutical companies producing some of the drugs mentioned in this paper.
References
- 1.Hopkins RJ, Girardi LS, Turney EA. Relationship between H pylori eradication and reduced duodenal and gastric ulcer recurrence: a review. Gastroenterology. 1996;110:1244–1252. doi: 10.1053/gast.1996.v110.pm8613015. [DOI] [PubMed] [Google Scholar]
- 2.De Boer WA, Tytgat GNJ. The best therapy for Helicobacter pylori infection. Should efficacy or side effect profile determine our choice? Scand J Gastroenterol. 1995;30:401–407. doi: 10.3109/00365529509093298. [DOI] [PubMed] [Google Scholar]
- 3.Neil GA. Do ulcers burn out or burn on? Managing duodenal ulcer diathesis in the Helicobacter pylori era. Am J Gastroenterol. 1997;92:387–392. [PubMed] [Google Scholar]
- 4.Penston JG. Review article: clinical aspects of Helicobacter pylori eradication therapy in peptic ulcer disease. Aliment Pharmacol Ther. 1996;10:469–486. doi: 10.1046/j.1365-2036.1996.40182000.x. [DOI] [PubMed] [Google Scholar]
- 5.Soll AH. Consensus statement. Medical treatment of peptic ulcer disease. Practice guidelines. JAMA. 1996;275:622–629. doi: 10.1001/jama.275.8.622. [DOI] [PubMed] [Google Scholar]
- 6.Van der Hulst RWM, Rauws EAJ, Koycu B, Keller JJ, Ten Kate FJW, Dankert J, et al. Helicobacter pylori reinfection is virtually absent after successful eradication. J Infect Dis. 1997;176:196–200. doi: 10.1086/514023. [DOI] [PubMed] [Google Scholar]
- 7.Wilhelmsen I. Quality of life and Helicobacter pylori eradication. Scand J Gastroenterol. 1996;31(suppl 221):18–20. [PubMed] [Google Scholar]
- 8.De Boer WA, Tytgat GNJ. How to treat H pylori infection. Should treatment strategies be based on testing bacterial susceptibility? A personal viewpoint. Eur J Gastroenterol Hepatol. 1996;8:709–716. [PubMed] [Google Scholar]
- 9.Penston JG, Mistry KR. Eradication of Helicobacter pylori in general practice. Aliment Pharmacol Ther. 1996;10:139–145. doi: 10.1046/j.1365-2036.1996.745128000.x. [DOI] [PubMed] [Google Scholar]
- 10.Bodger K, Daly MJ, Heatley RV. Clinical economics review: Helicobacter pylori associated peptic ulcer disease. Aliment Pharmacol Ther. 1997;11:273–282. doi: 10.1046/j.1365-2036.1997.145321000.x. [DOI] [PubMed] [Google Scholar]
- 11.Current European concepts in the management of Helicobacter pylori infection. the Maastricht consensus report. Gut. 1997;41:8–13. doi: 10.1136/gut.41.1.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Van der Hulst RWM, Keller JJ, Rauws EAJ, Tytgat GNJ. Treatment of Helicobacter pylori infection in humans: a review of the world literature. Helicobacter. 1996;1:6–19. doi: 10.1111/j.1523-5378.1996.tb00003.x. [DOI] [PubMed] [Google Scholar]
- 13.Treiber G. The influence of drug dosage on Helicobacter pylori eradication: a cost-effectiveness analysis. Am J Gastroenterol. 1996;91:246–257. [PubMed] [Google Scholar]
- 14.Kolkman JJ, Tan TG, Oudkerk Pool M, van Kleef WA, Geraedts AAM, Timmerman RJ, et al. Ranitidine bismuth citrate with clarithromycin versus omeprazole with amoxycillin in the cure of Helicobacter pylori infection. Aliment Pharmacol Ther. 1997;11:1123–1129. doi: 10.1046/j.1365-2036.1997.00254.x. [DOI] [PubMed] [Google Scholar]
- 15.Pare P, Romaozinho J, Bardhan KD, French PC, Roberts PM. Ranitidine bismuth citrate is more effective than omeprazole in the eradication of H pylori when co-prescribed with clarithromycin. Gastroenterology. 1997;112:A251. [Google Scholar]
- 16.Megraud F, Pichavant R, Palegry D, French PC, Roberts PM. Ranitidine bismuth citrate co-prescribed with clarithromycin is more effective in the eradication of Helicobacter pylori than omeprazole with clarithromycin. Gut. 1997;41(suppl 1):A92. [Google Scholar]
- 17.Chiba N, Hunt RH. Bismuth, metronidazole and tetracycline and acid suppression in H pylori eradication: a meta-analysis. Gut. 1996;39(suppl 2):A36–A37. [Google Scholar]
- 18.Lerang F, Moum B, Ragnhildstveit E, Haug JB, Hauge T, Tolas P, et al. A comparison between omeprazole-based triple therapy and bismuth based triple therapy for the treatment of Helicobacter pylori infection: a prospective randomized 1-year follow-up study. Am J Gastroenterol. 1997;92:653–658. [PubMed] [Google Scholar]
- 19.Breuer T, Goodman KJ, Malaty HM, Sudhop T, Graham DY. How do clinicians practising in the US manage Helicobacter pylori related gastrointestinal diseases? Am J Gastroenterol. 1998;93:553–556. doi: 10.1111/j.1572-0241.1998.164_b.x. [DOI] [PubMed] [Google Scholar]
- 20.Buda A, Dal BO N, Kusstatscher S, Grassi SA, Crestani B, Battaglia G, et al. Different lansoprazole dosages in H pylori eradication therapy: a prospective multicenter randomized study comparing 30 mg bid versus 15 mg bid. Gut. 1997;41(suppl1):A92. [Google Scholar]
- 21.Lamouliatte H, de Mascarel A, Megraud F, Samoyeau R. Double blind study comparing once daily versus twice daily dosage of PPI with amoxicillin-clarithromycin for H pylori cure. Gut. 1997;41(suppl 1):A93. [Google Scholar]
- 22.Huang JQ, Wilkinson JM, Chiba RH, Hunt RH. One week clarithromycin 500 mg bid is better than 250 mg bid for eradicating H pylori infection when combined with proton pump inhibitor and metronidazole or amoxicillin: a meta-analysis. Gut. 1997;41(suppl 1):A90–A91. [Google Scholar]
- 23.Thys JC, van Zwet AA, Thys WJ, van der Wouden EJ, Kooy A. One-week triple therapy with omeprazole, amoxycillin and tinidazole for Helicobacter pylori infection: the significance of imidazole resistance. Aliment Pharmacol Ther. 1997;11:305–309. doi: 10.1046/j.1365-2036.1997.155329000.x. [DOI] [PubMed] [Google Scholar]
- 24.Misiewicz JJ, Harris AW, Bardhan KD, Levi S, O'Morain C, Cooper BT, et al. One week triple therapy for Helicobacter pylori: a multicentre comparative study. Gut. 1997;41:735–739. doi: 10.1136/gut.41.6.735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lind T, Megraud F, Unge P, Bayerdorffer E, O'Morain C, Spiller R, et al. The MACH2 study: role of omeprazole in eradication of Helicobacter pylori with 1-week triple therapies. Gastroenterology. 1999;116:248–253. doi: 10.1016/s0016-5085(99)70119-8. [DOI] [PubMed] [Google Scholar]
- 26.De Boer WA, Driessen WMM, Jansz AR, Tytgat GNJ. Effect of acid suppression on efficacy of treatment for Helicobacter pylori. Lancet. 1995;345:817–820. doi: 10.1016/s0140-6736(95)92962-2. [DOI] [PubMed] [Google Scholar]
- 27.Borody TJ, Shortis NP. Treatment of patients with failed eradication—a personal view. In: Hunt RH, Tytgat GNJ, editors. Helicobacter pylori: basic mechanisms to clinical cure. Dordrecht: Kluwer Academic; 1996. pp. 357–365. [Google Scholar]
- 28.Graham DY, de Boer WA, Tytgat GNJ. Choosing the best anti-Helicobacter therapy: effect of antimicrobial resistance. Am J Gastroenterol. 1996;91:1072–1076. [PubMed] [Google Scholar]
- 29.De Koster E, De Reuck, Jonas C, Denis P, Otero J, Buset M, et al. French triple works fine in Brussels. Gastroenterology. 1997;112:A99. [Google Scholar]
- 30.Lee JM, Fallon C, Breslin NP, Hyde DK. H pylori eradication: quadruple therapy is effective in triple therapy failures. Gastroenterology. 1997;112:A195. [Google Scholar]
- 31.Huelin Benitez J, Jimenez Perez M, Duran Campos A, Espana P, Contreras J, De la Cruz Lombardo JM, et al. Quadruple therapy with omeprazole, tetracycline, metronidazole and bismuth as a second option after failure of a first eradication therapy. Gut. 1998;43(suppl 2):A86. [Google Scholar]
- 32.Borda F, Martinez A, Echarri A, Jimenez J, Rodriguez C, Jara C, et al. Clinical practice results of quadruple treatment in Helicobacter pylori eradication failure with OCA-7. Gut. 1998;43(suppl 2):A81. [Google Scholar]
- 33.Goddard AF, Logan RPH, Atherton JC, Hawkey CJ, Spiller RC. Maastricht consensus report regimen for second-line treatment of H pylori infection: how does it perform in practice? Gut. 1997;41(suppl 1):A96. [Google Scholar]
- 34.Peitz U, Nusch A, Sulliga M, Becker T, Stolte M, Borsch G. Second-line treatment of Helicobacter pylori infection. Gut. 1997;41(suppl 1):A104. [Google Scholar]
- 35.Katelaris PH, Jones DB. Testing for Helicobacter pylori infection after antibiotic treatment. Am J Gastroenterol. 1997;92:1245–1247. [PubMed] [Google Scholar]
- 36.Kist M, Strobel S, Folsch UR, Kirchner T, Hahn EG, von Kleist DH, et al. Prospective assessment of the impact of primary antimicrobial resistance on cure rates of Helicobacter pylori infections. Gut. 1997;41(suppl 1):A90. [Google Scholar]
- 37.Buckley MJM, Xia HX, Hyde DM, Keane CT, O'Morain CA. Metronidazole resistance reduces efficacy of triple therapy and leads to secondary clarithromycin resistance. Dig Dis Sci. 1997;42:2111–2115. doi: 10.1023/a:1018882804607. [DOI] [PubMed] [Google Scholar]