Abstract
Diabetic retinopathy (DR) is a major vision-threatening disease among the working-age population worldwide. Present therapeutic strategies such as intravitreal injection of anti-VEGF and laser photocoagulation mainly target proliferative DR. However, there is a need for early effective management in patients with early stage of DR before its progression into the more severe sight-threatening proliferative stage. Nutraceuticals, natural functional foods with few side effects, have been proposed to be beneficial in patients with DR. Over the decades, many studies, either in vitro or in vivo, have demonstrated the advantages of a number of nutraceuticals in DR with their antioxidative, anti-inflammatory, neuroprotective, or vasoprotective effects. However, only a few clinical trials have been conducted, and their outcomes varied. The low bioavailability and instability of many nutraceuticals have indeed hindered their utilization in clinical use. In this context, nanoparticle carriers have been developed to deliver nutraceuticals and to improve their bioavailability. Despite its preclinical nature, research of interventive nutraceuticals for DR may yield promising information in their clinical applications.
Keywords: blindness, diabetes, dietary supplement, inflammation, nanotechnology, natural product, neovascularization, oxidative stress, retina, vessel
1. Introduction
Diabetic retinopathy (DR) is one of the microvascular complications of diabetes mellitus. It is a major cause of blindness worldwide especially among working-age adults, making it an extensive burden for both families and countries [1,2,3]. It was estimated that DR affects about 35% of diabetic patients globally [4].
DR starts as non-proliferative DR (NPDR) and progresses to proliferative DR (PDR). In NPDR, microaneurysms, small hemorrhages, hard exudates, cotton wool spots, venous beadings, and intraretinal microvascular abnormalities can be observed during ophthalmic examination. Later, new vessels growing toward the vitreous cavity from the retina occur in PDR [5]. Vitreous hemorrhage and tractional retinal detachment often happen in the later stages of PDR. Diabetic macular edema (DME) is another severe manifestation and can arise at any stage of DR. Based on the impact on vision, mild and moderate NPDR are categorized as non-vision-threatening DR, while vision-threatening DR (VTDR) includes severe NPDR, PDR, and DME [2].
2. Pathophysiology of DR
Hyperglycemia in diabetes triggers oxidative stress and inflammation through multiple pathways, which, in turn, lead to the development of DR. Through the tricarboxylic acid (TCA) cycle, a high level of glucose causes overproduction of electron donors (nicotinamide adenine dinucleotide (NADH) and flavin adenine dinucleotide (FADH2)), resulting in increased proton gradient across the inner mitochondrial membrane [6]. The overproduction of reactive oxygen species (ROS) exposes the retina to oxidative stress. Hyperglycemia-induced oxidative stress is heavily involved in the pathology of DR. The increase in the upstream glycolytic metabolites also induces (i) the accumulation of the advanced glycation end products (AGEs) and the activation of the receptor for AGEs (RAGEs); (ii) the activation of protein kinase C (PKC); (iii) the increased hexosamine pathway flux; and (iv) the active polyol pathway, a two-step metabolic pathway where glucose is reduced to sorbitol and then to fructose [7,8,9]. The disturbance of these four metabolic pathways, in turn, aggravates oxidative stress [10].
Oxidative stress not only augments the aforementioned metabolic pathways but also causes mitochondrial damage, cell death, inflammation, and lipid peroxidation in the retina. Notably, lipids make up one-third of the retina’s dry weight, of which approximately 40% are saturated fatty acids (SFA), 21% are monounsaturated fatty acids (MUFA), and 35% are polyunsaturated fatty acids (PUFA) [11,12]. Due to the sensitivity of PUFAs to oxidation, the retina exhibits high vulnerability to oxidative stress, making lipid peroxidation an important contributor to the progression of DR [10]. In the presence of oxygen-derived free radicals, lipid is oxidized and the products, such as hydroxyhexenal and hydroxynonenal, can interact with cellular DNA and proteins in the retina, leading to the damage of retinal cells like photoreceptors and retinal pigment epithelial (RPE) cells [13,14].
Inflammation is also crucial in the development of DR. Persistent inflammation triggers the activation of various immune cells, including microglia and macrophages [15]. Upregulation of pro-inflammatory chemokines such as interleukin (IL)-8, IL-1β, and tumor necrosis factor (TNF)-α have been detected in the aqueous and vitreous fluid as well as the serum of patients with PDR [16,17,18,19]. The pivotal mediators of inflammatory responses, nuclear factor-kappa B (NF-κB) and NOD-like receptor family pyrin domain containing 3 (NLRP3) inflammasomes are also highly related to the progression of DR [20,21,22,23]. Inflammation partly contributes to pericyte depletion and leukostasis, the adhesion of leukocytes to the retinal vasculature [24]. Leukostasis can, in turn, lead to injury and death of endothelial cells, nonperfusion of capillaries, ischemia, and disruption of the blood–retinal barrier (BRB), resulting in retinal vascular leakage [25]. Meanwhile, the subsequent retinal nonperfusion and ischemia not only further exacerbate oxidative stress, and promote the release of pro-inflammatory factors, but also induce proangiogenic factors like vascular endothelial growth factor (VEGF) and angiopoietin-2 (Ang-2) [26,27,28,29]. The process of VEGF-mediated angiogenesis ultimately leads to the progression of NPDR to PDR [30].
Emerging evidence indicates that neurodegeneration in the retina is another major characteristic of DR. Functional studies using multifocal electroretinography reported reduced amplitudes and increased peak implicit times in a proportion of patients with DR, suggesting a role of neuro-retinal dysfunction in the pathogenesis of DR [31,32,33]. Besides functional changes, the peripapillary retinal nerve fiber layer has been detected to be significantly thinner in diabetic patients compared with controls [34]. Research using animal models that mimic DR has consistently demonstrated a significant involvement of functional impairment and cell death of retinal ganglion cells (RGCs), amacrine cells, and photoreceptors [35,36,37].
3. Treatments for DR
Currently, the primary focus of intervention is on the vision-threatening stage of DR: PDR and DME. Panretinal photocoagulation (PRP) is the mainstay treatment and is considered the standard care for PDR [5]. Intravitreal injection of anti-VEGF (e.g., Ranibizumab and Aflibercept) is a developing therapy and could be considered for additional treatment in patients with high-risk PDR [38]. For the central-involved DME, intravitreal anti-VEGF has become the first-line therapy as recommended in 2019′s Preferred Practice Pattern by the American Academy of Ophthalmology (AAO) and 2022′s evidence-based guidelines in China [38,39]. Steroids such as intravitreal triamcinolone acetonide (IVTA) are suitable and can be tailored for patients with PDR or DME [5]. Recently, intravitreal Faricimab, the bispecific antibody that binds to and inhibits both vascular VEGF-A and Ang-2, has been approved to treat DME in numerous countries and regions including America, Europe, China, and Japan [40,41,42]. Despite the advances in treatments of PDR, management for NPDR is still limited; it primarily focuses on glycemic and blood pressure control as well as lipid-lowering strategies [5]. In this context, nutraceuticals have been proposed to be a promising adjunctive treatment that offers potential curative benefits for patients with NPDR, and even PDR.
4. Nutraceuticals
Nutraceuticals are natural functional foods that provide medical or health benefits. Some nutraceuticals, such as carotenoids, are strong antioxidants with the potential to scavenge the ROS. Some exert anti-inflammatory effects and may regulate the expression of NF-κB [43]. Some nutraceuticals have been shown to be advantageous to both neuronal and microvascular functions [44]. As natural foods, nutraceuticals are easily accessible and affordable. Moreover, proper dietary supplementation of nutraceuticals is considered safe and less likely to cause side effects that are commonly associated with many anti-diabetic medications, such as hypoglycemia, liver and kidney damage, and gastric discomfort.
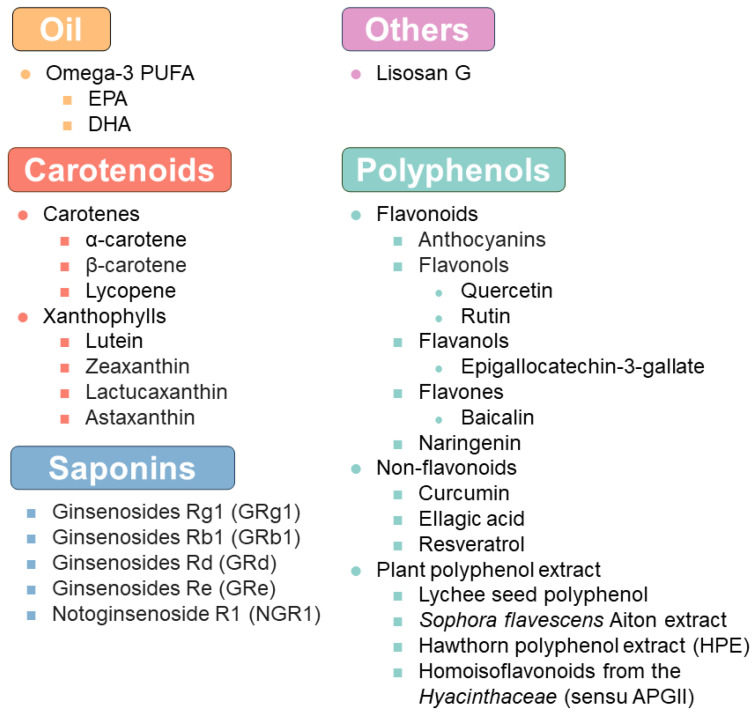
The role of nutraceuticals in DR was reviewed a few years ago [45,46]. Here, we focused on providing an update on the evidence of nutraceutical intervention in DR (Figure 1 and Table 1 and Table 2). Furthermore, we discussed the advances in delivery systems for these nutraceuticals that may help to resolve the bioavailability issues.
Figure 1.
A summary of the nutraceuticals mentioned in the present review.
The search strategy and selection criteria were as follows: we searched Google Scholar and PubMed for original research articles as well as meta-analysis/systematic reviews. The research terms were “diabetic retinopathy”, “nutraceuticals”, or “delivery system” in combination with the term of a specific nutraceutical (e.g., lutein) or delivery system (e.g., liposomes). We chose publications within the last 5 years (2019 to March 2024) to illustrate recent advances. However, common references and important older publications were also included to provide a more comprehensive overview. Review articles, book chapters, and clinical guidelines were cited to provide readers with more detailed information.
4.1. Oil
Diabetic dyslipidemia is very common among patients with type 2 diabetes mellitus (T2DM), with a prevalence of 72–85% [47]. Docosahexaenoic acid (DHA), oleic acid (OA), and arachidonic acid (AA) are the “primary PUFAs” in the photoreceptor outer segments of the human retina [48]. These PUFAs are not only crucial for the structure, homeostasis, and function of the retina but are also effective antioxidants and anti-inflammatory substances [49,50,51]. A combined cohort study analyzed the association between omega-3 PUFAs and DR using data from the Multi-Ethnic Study of Atherosclerosis (MESA) and Genetics of Latino Diabetic Retinopathy (GOLDR). It concluded that DHA was negatively linked to the occurrence and severity of DR [52].
Another potential indicator of the severity of DR is the ratio of omega-6 (ω-6)/omega-3 (ω-3) fatty acids. Some of these fatty acids are metabolized by the same enzymes and are, therefore, competitors in the metabolic pathways [53]. It has been suggested that the ω-6/ω-3 ratio was more important than individual indicators [54]. A low ω-6/ω-3 ratio is generally considered to have a protective effect against certain chronic diseases such as coronary heart disease, autoimmune diseases, and diabetes by reducing the production of pro-inflammatory mediators [55,56,57]. However, in 2021, Zhao et al. reported that the ω-6/ω-3 ratio was positively related to the incidence of DM, but higher serum ω-6/ω-3 ratio was inversely associated with DR in a case–control study [58]. The authors explained that DM is a complex condition of metabolism and changes in ω-6/ω-3 ratio might not be a straightforward process that only increases with disease progression and can be affected by the composition of individual PUFAs [58]. In fact, it has been noted that both ω-3 and the ω-6 lipid products of cytochrome P450 oxidase 2C were shown to aggravate retinal and choroidal neovascularization in mice [59,60]. Therefore, the correlation between ω-6/ω-3 ratio and DR may be intricate.
Nevertheless, the idea of applying lipids as a source of diet supplements to aid DR has been proposed for years. Fish oil, soybean oil, and olive oil have been proposed as nutritional recommendations for the public due to their high proportion of healthy components such as PUFAs. Indeed, many preclinical evaluation experiments conducted in animal models have shown that supplementation of omega-3 PUFAs or DHA alone exerted protective effects in DR. Dietary PUFAs resulted in a beneficial effect on pathological retinal neovascularization in the mouse oxygen-induced retinopathy (OIR), an animal model of DR [61]. Here, DHA, and its enzymatic oxidation products (4-hydroxy-docosahexaenoic acid) as well as some bioactive omega-3 PUFA-derived mediators (neuroprotectinD1, resolvinD1 and resolvinE1) were found to have anti-angiogenic effects [61,62,63]. Several observational clinical studies also suggested a potential beneficial role of omega-3 PUFA-enriched diets such as fish-originated long-chain omega-3 PUFAs in lowering the risk of VTDR [64,65,66]. In a randomized controlled trial (RCT) in patients with DME, intravitreal ranibizumab combined with DHA supplementation was shown to reduce central subfield macular thickness but did not improve the visual acuity as compared with ranibizumab alone after a 2-year follow-up [67]. Despite these findings, a prospective clinical study (PAOXRED study) showed that intake of 1050 mg/day DHA for 2 years did not appear to mitigate NPDR progression [68]. Likewise, a prospective clinical study (ASCEND-Eye) found that daily oral supplementation of 1 g omega-3 fatty acids [containing 460 mg Eicosapentaenoic acid (EPA) and 380 mg DHA] for 6.5 years did not yield better outcomes versus control in DR progression [69]. Overall, the effect of PUFA supplements on DR remains ambiguous. PUFA-rich diets may be beneficial but may have a less significant effect, especially in vision improvement. PUFA may provide more of a supportive beneficial effect than a therapeutic one.
4.2. Carotenoids
Carotenoids are organic pigments mainly produced by plants or algae. They include two groups: carotenes (hydrocarbon carotenoids) and xanthophylls (oxygen-containing carotenoids). Alpha-carotene and beta-carotene are provitamin A carotenoids that can be converted to vitamin A via the beta-carotene monooxygenase type 1 (BCMO1) enzyme in the intestine [70]. Vitamin A is a family of fat-soluble retinoic acids, chiefly retinol and retinyl esters. One active derivative of vitamin A, 11-cis-retinal, is a critical component of rhodopsin that contributes to light perception [71]. Lutein, zeaxanthin, and meso-zeaxanthin are xanthophylls presented as macular pigments in the human eyes and contribute to absorbing damaging visible light and quenching ROS [72]. Lutein and zeaxanthin cannot be synthesized de novo and must be obtained from the diet. Meso-zeaxanthin is a metabolite of lutein but can also be absorbed from the diet. Carotenoids have been utilized as dietary supplementations for decades due to their importance in the eyes [73].
Some studies have revealed a relationship between decreased levels of carotenoids and the risk of DR. It was reported that the mean plasma levels of carotenoids were significantly lower in the DR group compared with the control group and DM patients without DR [74,75,76]. In in vitro or in vivo models, oral supplementation of lutein was demonstrated to have antioxidative, anti-inflammatory, and anti-angiogenic effects; it helps to rescue the retinal morphological changes caused by hyperglycemia [77,78,79]. Lycopene is another carotene that can inhibit oxidative damage to DNA, lipids, and proteins [80]. Oral intake of lycopene has been shown to be effective in preventing elevated inflammation and oxidative stress in the alloxan-induced diabetic eye tissues, the optic nerve in particular [81]. Astaxanthin, a xanthophyll produced by algae and found in many marine organisms, has sparked widespread interest among scientists in managing DR. Astaxanthin, either administered orally, intraperitoneally, or by intravitreal injection, is reported to suppress oxidative stress, downregulate inflammation, alleviate apoptosis, and help to improve visual acuity and control blood glucose via the phosphoinositide 3-kinase (PI3K)/Akt/nuclear factor erythroid 2-related factor 2 (Nrf2) pathway and hypoxia-inducible factor alpha (HIF-1α) pathway [82,83,84,85,86,87,88,89]. Another xanthophyll, lactucaxanthin is a carotenoid from lettuce. Lately, there is evidence to show that lactucaxanthin administered through oral consumption could modulate ROS and downregulate the expression of angiogenesis markers such as VEGF and HIF-1α. It exhibited the greater potential of being a bioactive anti-angiogenic nutrient supplement for DR when compared to lutein [90,91].
Carotenoid-rich natural plants have attracted widespread attention, with the belief that they have fewer side effects. Lutein-rich purple sweet potato leaf extract has been shown to suppress retinal inflammation and increase retina thickness while palm oil mill effluent-derived beta-carotene could alleviate oxidative stress as well as regulate BRB function in diabetic rats [92,93]. However, high doses of carotenoid supplementation may not benefit retinal function. A high-dose carotenoid-enriched carrot powder diet was reported to exacerbate retina function in streptozotocin (STZ)-induced diabetic rats [94]. It was found that the hepatic metabolism of carotenoids into retinoids in diabetic rats was lower compared with the non-diabetic rats, which partially contributed to this phenomenon [94]. Indeed, different delivery methods, dosage levels, administration durations, and metabolic statuses may lead to different results. Likewise, the outcomes after carotenoid supplementation are inconsistent in clinical trials [95,96,97]. However, two recent systematic reviews concluded that carotenoids may delay the onset and impede the development of DR as an adjunctive nutritional strategy, but they also stressed the need for longer, high-quality, placebo-controlled, and large-scale prospective clinical trials [98,99]. In addition, the lipophilic nature of carotenoids, as well as their absorption properties in the gastrointestinal tract, causes relatively low bioavailability with conventional pharmaceutical packaging and delivery methods. Therefore, further studies on the packaging of carotenoids and improvement of administration approaches are in demand.
4.3. Polyphenol
Polyphenols are found in many plant foods like fruits, vegetables, tea, coffee, and wine. Polyphenols can be broadly classified into four subgroups, including phenolic acids, flavonoids, stilbenes, and lignans [100]. Characterized by the presence of multiple phenol units or phenolic rings, polyphenols exhibit strong antioxidant capabilities. Numerous studies have demonstrated that dietary polyphenols hold many potential health attributes like anti-inflammatory, anti-carcinogenic, and anti-diabetic effects, preventing the development of chronic diseases like cardiovascular diseases and neurodegenerative disorders [101,102]. Here, we briefly introduced the roles of several polyphenols in DR.
4.3.1. Flavonoids
Flavonoids are the most abundant and versatile class of polyphenols, featuring a common C6-C3-C6 backbone structure. Flavonoids can be further divided into several subcategories, including anthocyanidins, flavonols, flavanols (catechins and proanthocyanidins), flavones, isoflavones, flavanones, and chalcones [103].
Anthocyanins
Anthocyanins are natural water-soluble pigments found inside the vacuoles in the cytosol and they contribute to the reddish-blue color of many fruits and vegetables. Black raspberry-derived anthocyanins (BRAs) have been extensively studied and demonstrated to regulate Nrf2 gene expression, attenuate ROS levels, reduce caspase-1-induced inflammation, and lower VEGFA levels, resulting in the melioration of blood glucose, lipid dysmetabolism, and retinopathy in diabetic rats [104,105]. Cyanidin-3-glucoside (C3G), also called chrysanthemin, is one of the most widely distributed anthocyanins found in nature. Similar to BRAs, C3G showed protective effects in in vivo and in vitro models of DR but gained more attention for its relative stability and easier absorbance [106,107,108]. Molecular docking analysis revealed that C3G could combine well with 78-kDa glucose-regulated protein (GRP78), a major endoplasmic reticulum (ER) chaperone protein, hence regulating ER stress [105,109]. In a recent open-label clinical trial, oral supplementation of 320 mg/day of anthocyanins for 4 weeks significantly reduced the pro-inflammatory biomarkers (IL-6, IL-18, and TNF-α) in T2DM patients [110]. Such evidence suggests that anthocyanins are a valuable dietary supplement for individuals with diabetes or DR.
Flavonols
Quercetin is a flavonol and a plant pigment. Unlike anthocyanins, quercetin is insoluble in cold water, poorly soluble in hot water, but quite soluble in alcohol and lipids [111]. It is a strong antioxidant with five hydroxyl groups (-OH). Quercetin also exerts potent anti-inflammatory effects in DR through downregulating the level of NLRP3 inflammasomes and NF-κB signaling [112,113]. It was shown to inhibit autophagy and apoptosis and alleviate ER stress, therefore limiting pathological angiogenesis [112,113,114,115]. By upregulating nerve and synapse-associated proteins like postsynaptic density (PSD) 93, PSD95, nerve growth factor (NGF), and brain-derived neurotrophic factor (BDNF), quercetin is considered to be neurotrophic and neuroprotective in DR [113,114]. Interestingly, it was reported that oral consumption of quercetin not only regulated the Nrf2 pathway but also helped to reconstruct microbial community structure and inhibited intestinal dysbiosis, protecting retinal function through the gut–retina axis in DR [116]. Together, these studies indicate that quercetin is a functional nutraceutical that is helpful for DR.
Rutin, also known as quercetin-3-O-rutinoside, has identical antioxidant properties and demonstrates therapeutic potential for DR. Oral administration of rutin in STZ-induced DR rats resulted in a lower level of VEGF and a significantly lower tortuosity index [117].
Flavanols
Flavanols, also called flavan-3-ols, are commonly found in foods like tea, cocoa, grapes, apples, and berries. Flavanols contain several compounds like catechin, epicatechin, epigallocatechin, epicatechin gallate, and epigallocatechin gallate. Epigallocatechin-3-gallate (EGCG) is the most abundant and bioactive catechin in green tea. A cross-sectional clinical study suggested that long-term tea consumption was significantly associated with a lower risk of DR [118]. Concordantly, EGCG was shown to stimulate autophagy and reduce apoptosis in the high glucose (HG)-treated rat primary retinal Müller cells [119]. Peracetate-protected (e)-EGCG (pro-EGCG) is a prodrug of EGCG with enhanced stability and bioavailability. Pro-EGCG was reported to be anti-inflammatory and could mitigate cell proliferation and pro-angiogenic factor production through the ROS/Thioredoxin-interacting protein (TXNIP)/NLRP3 inflammasome axis [120]. Another catechin, catechin 7-O-β-D-apiofuranoside (C7A), the main bioactive component of Ulmus davidiana extract, was demonstrated to prevent pericyte apoptosis and reduce endothelial permeability, suggesting its potential as a protective agent for reducing vascular leakage in DR [121].
Naringenin
Naringenin is a natural flavonoid found primarily in citrus fruits such as tomatoes and oranges. Naringenin is a strong antioxidant and was shown to upregulate the level of endothelial nitric oxide synthase (eNOS), downregulate the level of ROS, and inhibit apoptosis in HG-insulted human retinal endothelial cells (HREC) [122]. In a study using an HG-induced DR zebrafish model, naringenin could regress glucose levels and reduce oxidative stress, normalize VEGF overexpression, and finally inhibit macular degeneration of early DR in zebrafish [123].
4.3.2. Non-Flavonoids
Curcumin
Curcumin is the principal active polyphenolic compound of the turmeric plant (Curcuma longa). The effects of curcumin on DR have been widely explored. Curcumin could promote the Nrf2/Heme Oxygenase-1 (HO-1) signaling process through extracellular signal-regulated kinase 1/2 (ERK1/2) activation, hence inhibiting HG-induced injury in ARPE-19 retinal pigment epithelial cells and improving retina morphology in STZ-treated rats [124,125]. In addition, it was reported that curcumin could inhibit the PI3K/Akt/mammalian target of the rapamycin (mTOR) signaling pathway, suppressing inflammation in HG-treated ARPE-19 retinal pigment epithelial cells [126]. A prospective clinical trial evaluated the effects of a fixed formula with curcumin (200 mg), artemisia (80 mg), bromelain (80 mg), and black pepper (2 mg) on DR patients [127]. The researchers found that the formula could restore central retinal thickness, visual acuity, and vessel density in T2DM patients with or without DME [127]. These findings provided the rationale for curcumin to serve as a functional supplementation for the management of DR in the healthcare setting.
Resveratrol
Chemically, resveratrol is a stilbene derivative containing two isomeric forms: cis-resveratrol and trans-resveratrol, with the latter being the more biologically active and widely studied form. Resveratrol serves as an effective scavenger of free radicals and a modulator of various cellular signaling pathways [128]. In the context of DR, resveratrol is involved in multiple pathways that regulate oxidative stress, apoptosis, and inflammation, such as mitogen-activated protein kinases (MAPK) signaling, protein kinase R (PKR) signaling, and PKC signaling [129,130,131,132]. Resveratrol is a promising food additive for DR patients, as it was also shown to inhibit endothelial-to-mesenchymal transition and decrease retinal vascular permeability [129,131].
4.3.3. Plant Polyphenol Extracts
Lychee seed polyphenol
Litchi seeds, rich in diverse bioactive compounds like flavonoids and saponins, are traditionally used in some Chinese medicine formulas with the efficacy of promoting qi and dispelling stagnation [133,134]. A purified fraction containing polyphenols in Lychee seed (LSP) was recently proven to ameliorate DR by suppressing HG-induced inflammation and apoptosis and hindering angiogenesis [133,135]. These results expanded the therapeutic potential of LSP and helped to extend the usage of these ostensibly obsolete seeds.
Sophora flavescens Aiton extract (SFE)
Sophora flavescens Aiton or “Kushen” is a widely used traditional Chinese medicine. A recent study based on untargeted retinal metabolomics explored the distribution of flavonoids of SFE in rat’s aqueous humor and retina after oral administration of SFE [136]. Notably, SFE was reported to guard against DR by regulating the synthetic metabolic pathways, enhancing the adoption of SFE in clinical practice [136].
Hawthorn polyphenol extract (HPE)
Hawthorn contains various bioactive compounds including flavonoids and triterpenoids with pharmacological benefits for different diseases [137]. It was demonstrated that HPE inhibited oxidative damage, inflammation, and apoptosis via the AMP-activated protein kinase (AMPK)/sirtuin 1(SIRT1)/NF-κB pathway and miR-34a/SIRT1/p53 pathway in ARPE-19 retinal pigment epithelial cells [138]. This study supported the use of HPE as a food supplementation for attenuating hyperglycemia-induced retinal damage [138].
Homoisoflavonoids from the Hyacinthaceae (sensu APGII)
Hyacinthus subfamily members hold an important place in traditional medicine. The potent homoisoflavonoids from the Hyacinthaceae (sensu APGII) displayed anti-proliferative activity and in vitro anti-angiogenic efficacy in HRECs [139].
4.4. Saponins
Saponins are a large group of amphiphilic glycosides of steroids and triterpenes present mainly in land plants. Ginsenosides, a specific class of saponins, are the major pharmacologically active components of ginseng plants like Panax ginseng [140]. There are various specific types of ginsenosides including ginsenosides Rg1 (GRg1), ginsenosides Rb1 (GRb1), ginsenosides Rd (GRd), and ginsenosides Re (GRe). GRg1 has received great interest over the years. GRg1 was reported to inhibit proliferation, migration, and angiogenesis in the HG-insulted HREC via the lncRNA SNHG7/miR-2116-5p/sirtuin-3 (SIRT3) axis [141]. Peroral supplementation of GRg1 alleviated inflammation, inhibited angiogenesis, and decreased cell apoptosis in retinal neurons in the genetically diabetic (db/db) mice and STZ-induced DR rats [142,143]. GRg1 can also be administered as eye drops to mice with DR. After 15 days of eye drop administration, the db/db mice yielded better visual function [144]. Other ginsenosides, GRe, GRd, and GRb1 also showed strong potential to scavenge ROS and inhibit apoptosis and angiogenesis, attenuating HG-induced cell injury [145,146,147,148].
Notoginsenoside R1 (NGR1) is a distinctive bioactive saponin compound found mainly in the roots of Panax notoginseng, another well-known medicinal herb. Oral NGR1 was shown to rescue retinal function by inhibiting mitophagy and apoptosis, alleviating oxidative stress and inflammation through PTEN-induced putative kinase protein 1 (PINK1)-dependent activation of mitophagy in db/db mice [149]. A recent study revealed that Panax notoginseng saponins, which contain NGR1, GRg1, GRe, GRb1, and GRd, could alleviate DR by inhibiting retinal inflammation via the NF-κB signaling pathway with the assumption that GRg1 and GRb1 may be the major pharmacological components [150]. These studies indicate that saponins carry the potency to alleviate DR, but more in vivo studies and clinical trials are still warranted.
Table 1.
Effects of nutraceuticals in DR-related models (basic studies).
| Dietary Source/Compound | In Vivo/In Vitro | Dosage | Duration | Cell Culture/Animal Model | Effects | Year | Refs. |
|---|---|---|---|---|---|---|---|
| Oil | |||||||
| DHA for cells; ω3-PUFAs for mouse | In vitro and in vivo | DHA (50 μM) | 24 h | DMOG treated HRMECs | AMPK-dependent anti-neovascularization effect | 2023 | [63] |
| 50 μL of oil rich in ω3-PUFAs (240 mg/g/day of DHA and 360 mg/g/day of EPA), (p.o.) | P1–P17 for nursing mother | Mouse OIR model | |||||
| Carotenoids | |||||||
| Astaxanthin | In vitro | 10, 20, 40 μM | Pretreated for 6 h | H2O2-induced and UVB-induced oxidative stress in ARPE-19 cells | Antioxidative effect | 2022 | [83] |
| Astaxanthin | In vitro | 10, 20, 50 μM | 24 h | 661 W cell line | PI3K/Akt/Nrf2 pathway mediated antioxidative and anti-apoptotic effects | 2022 | [82] |
| Lutein | In vitro | 0.5, 1.0 μM | 24 h | HG-induced damage in ARPE-19 cells | PI3K/AKT/Nrf2 and Erk1/2 pathways mediated antioxidative effect; protected RPE from diabetes-associated damages | 2020 | [78] |
| Astaxanthin | In vivo | 10 or 100 ng/µL (i.vit.); 0.5 or 5 mg/kg (i.p.) |
Once | OIR (C57BL/6J mice) | Anit-neovascularization and anti-apoptotic effects | 2019 | [84] |
| Astaxanthin | In vivo | 10 or 20 mg/kg/day (p.o.) | 21 days | STZ-induced DR (Swiss albino mice) | Inhibited processes of neuron-specific enolase activity; improved visual acuity function; controlled blood glucose; regulated oxidative stress (catalase) and neuron-specific enolase activity | 2022 | [85] |
| Astaxanthin | In vivo | 20 mg/kg/day (p.o.) | 45 days | STZ-induced DR (rats) | Nrf2/keap1 pathway mediated anti-apoptotic, anti-inflammation, and antioxidative effects | 2023 | [88] |
| Astaxanthin | In vivo | 4.8 mg/kg/day (p.o.) | 7 days | Hyper caloric diet-induced DR (Psammomys obesus) | Inhibited aldose reductase activity | 2019 | [87] |
| Carotenoid-enriched carrot powder diet | In vivo | β-carotene (61.9 mg/kg/day), α-carotene (43.1 mg/kg/day) (p.o.) | 9 weeks | STZ-induced DR (rats) | Exacerbated retina dysfunction | 2020 | [94] |
| Lutein | In vivo | Water dispersible form of lutein (4.2 or 8.4 mg/kg/day) (p.o.) | From 6 weeks to 9 months | Ins2Akita/+ mice | Suppressed retinal inflammation, protected retinal vasculature, and preserved retinal function | 2020 | [77] |
| Lutein or lactucaxanthin | In vivo | Lutein or lactucaxanthin micelles (200 μM, i.e., 0.23 mg/kg/day body weight of rats) (p.o.) | 8 weeks | STZ-induced DR (rats) | Downregulated ER stress (ATF4, ATF6, and XBP1), inflammatory markers (TNF-α, IL-6, NF-κB, and ICAM-1), and VEGFA. Antioxidative, anti-inflammatory effects | 2023 | [90] |
| Lutein-rich purple sweet potato leaf extract | In vivo | 200 or 400 mg/kg/day (p.o.) | 12 weeks | STZ-induced DR (rats) | Suppressed retinal inflammation, increased retina thickness | 2023 | [92] |
| Lutein and trapa bispinosa roxb. extract (TBE) | In vivo | Solidified food mixed with lutein (13.3 mg/kg/day) and TBE (133.3 mg/kg/day) | 8 weeks | C57BL/ksj-db/db mice | Downregulated GFAP and VEGF; improved the impaired regulation of retinal blood flow | 2022 | [151] |
| Lycopene | In vivo | 4 mg/kg/day (p.o.) | 3 months | Alloxan-induced diabetic optic neuropathy | Antioxidative, anti-inflammatory, ameliorated the tissue damage on the optic nerve | 2018 | [81] |
| Palm oil mill effluent-derived beta-carotene | In vivo | 50 or 100 mg/kg/day (p.o.) | 21 days | STZ-induced DR (rats) | Regulated BRB function; antioxidative effect | 2023 | [93] |
| Lutein | In vitro and in vivo | Lutein (10 µM) or oxidized lutein (40 nM) | 48 h | HG-induced damage in ARPE-19 cells | Activated AMPK and quenched ROS to maintain mtDNA integrity and mitochondrial biogenesis; antioxidative, anti-inflammatory effects | 2019 | [79] |
| One dose/day (p.o.) | 8 weeks | STZ-induced DR (rats) | |||||
| Lutein or lactucaxanthin | In vitro and in vivo | Lutein (10 μM) or lactucaxanthin (5 or 10 μM) | 48 h | HG-induced damage in ARPE-19 cells | Downregulated angiogenesis markers through HIF-1α/ER stress/VEGF axis; antioxidative and anti-angiogenic effects, altered the retina structural damages | 2021 | [91] |
| Lutein or lactucaxanthin micelles (200 μM, i.e., 0.23 mg/kg/day) (p.o.) | 8 weeks | STZ-induced DR (rats) | |||||
| Astaxanthin | In vivo and in vitro | 1, 5, 10 μM | 48 h | HG-induced damage in ARPE-19 cells | Antioxidative and anti-inflammatory effects through PI3K/Akt/NF-κB pathway | 2022 | [86] |
| Micellar astaxanthin (3 mg/kg/day) (p.o.) | 8 weeks | STZ-induced DR (rat) | |||||
| Astaxanthin | In vivo and in vitro | 1, 5, 10 μM | 48 h | ARPE-19 cells under hyperglycemic w/o hypoxic (CoCl2) condition | Downregulated VEGF through HIF-1α and XBP1 signaling pathway; restored ZO-1; modulated the diabetes-induced retinal morphological changes | 2021 | [89] |
| Micellar astaxanthin (3 mg/kg/day) (p.o.) | 8 weeks | STZ-induced DR (rats) | |||||
| Polyphenol | |||||||
| Anthocyanin | In vitro | Cyanidin-3-O glucoside (10 μM) | Pretreated 1 h and incubated for 24 h | HG-induced damage in ARPE-19 cells | Antioxidative effect | 2022 | [104] |
| Anthocyanin | In vitro | Blueberry anthocyanin extracts (12.5, 25, and 50 mg/L); Cyanidin-3-O glucoside (5, 10, 20 μM) | 12 h, 24 h, or 48 h | HG-induced injury in ARPE-19 cells | Antioxidative effect mediated by REDD1/GSK3β pathway; downregulated VEGFA | 2023 | [106] |
| Anthocyanin; Verbascoside | In vitro | Cyanidin-3-O glucoside (5, 10, or 50 μM), Verbascoside (5, 10 or 50 μM) | 48 h | HG-induced damage in HRECs | Antioxidative effect; protected integrity (ZO-1, VE-cadherin ↑) and function of epithelial cell layers | 2022 | [107] |
| Catechin 7-O-β-D-apiofuranoside (C7A) | In vitro | 4 μg/mL | 72 h | HG-induced injury in HRMECs and pericytes | Inhibited pericyte apoptosis by reducing p38 and JNK activity; reduced endothelial permeability | 2023 | [121] |
| Curcumin | In vitro | 10 µM | 12 h | HG-induced injury in ARPE-19 | Anti-inflammatory effect via ROS/PI3K/AKT/mTOR signaling pathway | 2019 | [126] |
| Curcumin | In vitro | 15 µM | 24 h | HG-induced injury in ARPE-19 | Antioxidative effect via ERK1/2-mediated Nrf2/HO-1 pathway | 2019 | [125] |
| Epigallocatechin-3-gallate (EGCG) | In vitro | 10, 20, or 30 μM | 24 h | HG-induced damage in rat primary retinal Müller cells | Stimulated autophagy and reduced apoptosis | 2019 | [119] |
| Hawthorn polyphenol extract (HPE) | In vitro | 10 μg/mL | 24 h | HG-induced injury in ARPE-19 | Regulated mir-34a/SIRT1/p53 signaling to reduce acetylation; inhibited oxidative damage, inflammation, and apoptosis through AMPK/SIRT1/NF-κB pathway | 2021 | [138] |
| Homoisoflavonoids from the Hyacinthaceae (sensu APGII) | In vitro | 0.001–0.5 µM | 48 h | HRECs | In vitro anti-angiogenic efficacy and anti-proliferative activity | 2019 | [139] |
| Naringenin | In vitro | 1 or 10 µM | 24, 48, and 72 h | HG-induced injury in HRECs | Antioxidative and anti-apoptotic effects | 2022 | [122] |
| Peracetate-protected epigallocatechin-3-gallate (pro-EGCG) | In vitro | 10, 20, 30 μM | 24 h | HG-induced damage in mouse primary retinal Müller cells | Anti-inflammatory effect via inhibition of ROS/TXNIP/NLRP3 inflammasome; mitigated cell proliferation and pro-angiogenic factor production | 2020 | [120] |
| Quercetin | In vitro | 20, 40, or 80 µM | 48 h | HG-induced injury in HRMECs | Inhibited NLRP3 inflammasome-mediated inflammation and autophagy, inhibited angiogenesis | 2021 | [112] |
| Resveratrol | In vitro | 1 µM | 24 h | HG-induced injury in HRECs | Inhibited PKC, antioxidative effects; inhibited NOX-mediated endothelial-to-mesenchymal transition | 2021 | [131] |
| Curcumin | In vivo | 200 mg/kg/day (p.o.) (combined with subcutaneous insulin, 4–6 IU/day) | 4 weeks | STZ-induced DR (rats) | Nrf2/HO-1 pathway mediated antioxidative and anti-apoptosis effects; improved retina morphology | 2021 | [124] |
| Naringenin | In vivo | 25, 50, or 75 µM | 3 h post-fertilization to 5 days post-fertilization | HG-induced DR (zebrafish) | Antioxidative effect; regressed the glucose levels and cellular damage; inhibited of macular degeneration | 2023 | [123] |
| Quercetin | In vivo | 50 mg/kg/day (p.o.) | 12 weeks | HFD and STZ-induced DR (rat) | Downregulated levels of blood glucose and oxidative stress, inhibited inflammation and improved dysbacteriosis and retinal function through gut–retina axis and Nrf2 pathway | 2024 | [116] |
| Quercetin | In vivo | 150 mg/kg/day (p.o.) | 16 weeks | STZ-induced DR (rats) | Anti-inflammatory, anti-angiogenic, and neurotrophic effects by inducing HO-1 | 2021 | [113] |
| Quercetin | In vivo | 35, 70 mg/kg (p.o.) | 12 weeks | db/db mice | Inhibited oxidative stress, apoptosis, and neurodegeneration via SIRT1/ER signaling pathway | 2020 | [114] |
| Resveratrol (trans-resveratrol) | In vivo | 5 mg/kg (i.p.) | Five days a week for one month | STZ-induced DR (rats) | Anti-apoptotic effect through MAPK signaling (CASP3, JNK1, p38αMAPK, ERK1 ↓; Bcl-2 ↑) | 2021 | [132] |
| Resveratrol | In vivo | 5 and 10 mg/kg/d (p.o.) | 30, 32, 34, and 36 weeks | STZ-induced DR (rats) | RAX/P-PKR pathway-mediated anti-apoptotic effects | 2022 | [130] |
| Rutin | In vivo | 50 mg/kg (p.o.) | 24 weeks | STZ-induced DR (rats) | Downregulated the levels of VEGF, TNF-α, and aldose reductase; antioxidative effect; reduced retinal vessel tortuosity index | 2019 | [117] |
| Sophora flavescens Aiton extract | In vivo | 37.5, 75, 150 mg/kg/day (p.o.) | 4 months | HFD and STZ-induced DR (rats) | Antioxidative, anti-inflammatory effects; ameliorated retinal morphological changes | 2022 | [136] |
| Anthocyanin | In vitro and in vivo | 150, 250, or 450 μg/mL | Pretreated 2 h and incubated for 48 h for cells | HG-induced human RPECs injury | Anti-apoptotic and antioxidative effects; alleviated ER stress; improved retina morphology changes | 2023 | [105] |
| 35 or 140 mg/kg/day (p.o.) | 6 weeks | STZ and high fat and high sucrose diet-induced DR rats | |||||
| Anthocyanin (Cyanidin-3-O glucoside) | In vitro and in vivo | 10 µM | 48 h | HG/CoCl2-induced damage in HRECs, BV2 microglia cells | Alleviated the inflammation, microglial activation, and angiogenesis; inhibited vascular leakage | 2021 | [108] |
| 20 mg/kg/day (p.o.) | 1 month | STZ-induced DR (mice) | |||||
| Lychee seed polyphenol | In vitro and in vivo | 8, 16, or 32 μg/mL | / | HG-induced damage in HRECs | Inhibited NLRP3 inflammasome-related inflammation; upregulated tight junction proteins; anti-angiogenesis and anti-apoptotic effects | 2023 | [133] |
| 50, 100, or 200 mg/kg/day (p.o.) | 6 weeks | db/db mice | |||||
| Resveratrol | In vitro and in vivo | 10, 50, or 100 µM | 24 h | HG-induced injury in rat retinal endothelial cells | Decreased retinal vascular permeability, inhibited retinal apoptosis, anti-inflammatory effect | 2019 | [129] |
| 0.1 or 1 μg/mL (i.vit.); 5, 10, or 50 μg/kg/day (tail vein injection) |
12 weeks | STZ-induced DR (rats) | |||||
| Quercetin (Q) and its 8-methyl pentamethyl ether derivative (8MQPM) | In vitro and ex vivo | 25 µM | 24 h | HRECs treated with conditioned medium from Y-79 human retinoblastoma cell line or stimulated by VEGFA | Akt, ERK, and JNK mediated anti-angiogenic effect | 2019 | [115] |
| / | / | Ex vivo rabbit aortic ring assay | |||||
| Saponins | |||||||
| Ginsenoside Rb1 (GRb1) | In vitro | 5, 10, 20 μM | 48 or 72 h | HG-induced injury in rat retinal capillary endothelial cells | Quenched ROS and inhibited DNA damage and apoptosis through NMNAT–NAD–PARP–SIRT axis | 2019 | [146] |
| Ginsenoside Re (Re) | In vitro | 3 μM | 24 h | HG-induced retinal endothelial RF/6A cell injury | Anti-angiogenesis and anti-apoptotic effects through upregulating PI3K/AKT pathway and inhibiting HIF-1α/VEGF signaling | 2020 | [148] |
| Ginsenoside-Rg1 (GRg1) | In vitro | 10 μM | 48 h | HG-induced injury in HRECs | Inhibited HG-induced proliferation, migration, and angiogenesis via lncRNA SNHG7/mir-2116-5p/SIRT3 axis | 2022 | [141] |
| Ginsenoside Rb1 (GRb1) | In vivo | 20, 40 mg/kg/day (i.p.) | 4 weeks | STZ-induced DR (rats) | Antioxidative effects | 2019 | [147] |
| Ginsenoside-Rg1 (GRg1) | In vivo | 25, 50, or 225 mg/kg/day (p.o.) | 8 weeks | db/db mice | Inhibited GCL and INL cell apoptosis | 2020 | [142] |
| Ginsenoside-Rg1 (GRg1) | In vivo | 2.5, 5, or 10 mg/kg (eye drops, twice a day) | 15 days | C57BL/ksj-db/db mice | IRS-1/Akt/GSK3β signaling-mediated neuroprotective effect | 2019 | [144] |
| Ginsenoside Rd (GRd) | In vitro and in vivo | 1, 3, 10, or 30 μΜ | 24 h | HG-induced injury in HUVECs | Downregulated NOX2 and ameliorated oxidative stress, mitochondrial dysfunction, and endothelial apoptosis via AMPK/SIRT1 signaling | 2022 | [145] |
| 10 μL 1% (w/v) GRd as eye drops, daily | 1 month | STZ-induced DR (C57BL/6 mice) | |||||
| Ginsenoside-Rg1 (GRg1) | In vitro and in vivo | 10 μM | 48 h | HG-induced injury in HRMECs | Anti-angiogenesis and anti-inflammatory effects via mir-216a-5p-mediated downregulation of TLR4/NF-κB signaling pathway | 2023 | [143] |
| 0.5 mL (5 g/mL) (p.o.) | 16 weeks | STZ-induced DR (rats) | |||||
| Panax notoginseng saponins | In vitro and in vivo | 25 μM | 24 h | HG-induced injury in MIO-M1 cells | NF-κB signaling pathway-mediated anti-inflammatory effect; attenuated elevated BRB disruption | 2024 | [150] |
| 40, 80, or 160 mg/kg (p.o.) | 1 month | STZ-induced DR (rats) | |||||
| Notoginsenoside R1 (NGR1) | In vitro and in vivo | 5, 10, 20, 40 μΜ | 72 h | HG-induced injury in rMC-1 cells | Enhanced PINK1-dependent activation of mitophagy; downregulated VEGF and upregulated PEDF; inhibited apoptosis; antioxidative and anti-inflammatory effects; restored retinal function | 2019 | [149] |
| 30 mg/kg/day (p.o.) | 12 weeks | db/db mice | |||||
Abbreviations: Administration routes: i.p., intraperitoneal injection; i.vit., intravitreal injection; p.o., per os (by mouth). Others: AMPK, AMP-activated protein kinase; ATF4, activating transcription factor 4; ATF6, activating transcription factor 6; BRB, blood–retinal barrier; CASP3, caspase-3; DHA, docosahexaenoic acid; DMOG, dimethyloxalylglycine; ER, endoplasmic reticulum; Erk1/2, extracellular signal-regulated kinase 1/2; GCL, ganglion cell layer; GFAP, glial fibrillary acidic protein; GSK3β, glycogen synthase kinase 3 beta; HG, high glucose; HFD, high-fat diet; HIF-1α, hypoxia-inducible factor-1 alpha; HRECs, human retinal endothelial cells; HRMECs, human retinal microvascular endothelial cells; HUVECs, human umbilical vein endothelial cells; ICAM-1, intercellular adhesion molecule-1; INL, inner nuclear layer; IRS-1, insulin receptor substrate 1; JNK, c-Jun N-terminal kinase; keap1, Kelch-like ECH-associated protein 1; NAD, nicotinamide adenine dinucleotide; NF-κB, nuclear factor-kappa B; NLRP3, NOD-like receptor family, pyrin domain-containing 3; NMNAT, nicotinamide mononucleotide adenylyltransferase; NOX, NADPH oxidase; Nrf2, nuclear factor erythroid 2-related factor 2; OIR, oxygen-induced retinopathy; PARP, poly(ADP-ribose) polymerase; PEDF, pigment epithelium-derived factor; PI3K, phosphoinositide 3-kinase; PKC, protein kinase C; RAX/P-PKR pathway, retinal apoptosis through RAX/PKR pathway; REDD1, regulated in development and DNA damage response 1; RPEC, retinal pigment epithelial cells; ROS, reactive oxygen species; SIRT1, sirtuin 1; SNHG7, small nucleolar RNA host gene 7; STZ, streptozotocin; TLR4, toll-like receptor 4; TNF-α, tumor necrosis factor-alpha; TXNIP, thioredoxin-interacting protein; UVB, ultraviolet B; VEGF, vascular endothelial growth factor; VEGFA, vascular endothelial growth factor A; VE-cadherin, vascular endothelial cadherin; XBP1, X-box binding protein 1; ZO-1, zonula occludens-1; ↓: down-regulated; ↑: up-regulated.
Table 2.
Effects of nutraceuticals in DR (clinical studies).
| Dietary Compound | Family of Compound | Type | Dosage | Supplementation Period | Candidates | Effects | Year | Refs. |
|---|---|---|---|---|---|---|---|---|
| Omega-3 PUFAs (DHA/EPA) | Oil | Prospective | 1 g omega-3 fatty acids (containing 460 mg EPA and 380 mg DHA) daily | 6.5 years | T1DM/T2DM with or without DR | No benefits for DR. | 2023 | [69] |
| DHA | Oil | Prospective | 1050 mg/day | 2 years | NPDR (any stage) | Did not appear to influence the slowing of the progression of NPDR | 2022 | [68] |
| Brudyretina: high rich DHA (1050 mg/d) nutraceutical formulation, (DHA, EPA, a mixture of B vitamins, vitamins C and E, lutein, zeaxanthin, and minerals) | Oil plus others | Prospective | 3 capsules of Brudyretina 1.5 g once daily | 90 days | T2DM with NPDR (24 patients) | No difference in BCVA and central subfield macular thickness. Total antioxidant capacity levels increased, and plasma IL-6 levels decreased | 2018 | [152] |
| Lutein | Carotenoids | Prospective | 10 mg/day of lutein | 36 weeks | T2DM with NPDR (30 patients) | Improved contrast sensitivity | 2017 | [95] |
| Lutein (L) and zeaxanthin (Z) | Carotenoids | Retrospective | Z (0.5 mg/day) or Z (0.5 mg/day) + L (6 mg/day) | 4 months | NPDR (72 patients) | Lutein supplement showed no benefits | 2019 | [97] |
| Lycopene | Carotenoids | Cross-sectional | Lycopene intake was assessed by using a food frequency questionnaire | / | T2DM patients and healthy controls | Ameliorated oxidative stress | 2021 | [96] |
| Anthocyanin | Polyphenol | Prospective | 320 mg/day | 4 weeks | Healthy controls; T2DM; T2DM-at-risk | Anti-inflammatory (IL-6, IL-18, TNF-α ↓) | 2021 | [110] |
| Curcumin, artemisia, bromelain, and black pepper | Combo | Prospective | Curcumin (200 mg), artemisia (80 mg), bromelain (80 mg), and black pepper (2 mg) | 6 months | T2DM with or without mild to moderate DME | Increased central retinal thickness, visual acuity, and vessel density of the deep capillary plexus | 2022 | [127] |
Abbreviations: BCVA, best-corrected visual acuity; DHA, docosahexaenoic acid; DME, diabetic macular edema; DR, diabetic retinopathy; EPA, eicosapentaenoic acid; IL-6, interleukin-6; IL-18, interleukin-18; NPDR, non-proliferative diabetic retinopathy; PUFA, polyunsaturated fatty acids; T1DM, type 1 diabetes mellitus; T2DM, type 2 diabetes mellitus; TNF-α, tumor necrosis factor-alpha; ↓: down-regulated.
5. Delivery Systems
Despite the powerful health-promoting properties of nutraceuticals such as antioxidant and anti-inflammatory properties, the bioavailability of most nutraceuticals is low. The oral bioavailability of nutraceuticals mainly involves the following processes: liberation from the food structures, solubilization in the digestive fluids, interaction with gastrointestinal components, epithelial cell permeation, chemical disintegration, and metabolic transformation [153,154]. Carotenoids are known to be lipophilic and extremely vulnerable to environmental stresses like heat, oxygen, light exposure, and unfavorable pH in the gastrointestinal tract (GIT). The tendency towards oxidative degradation, incomplete release from the food matrix, and low solubility have resulted in their poor bioavailability [155,156]. As for polyphenols, despite the abundance of studies investigating the effects of polyphenols on human health, only a few studies have considered the bioavailability of polyphenols to further support their bio-effect in vivo. The bioavailability varies among different classes of polyphenols; but, in general, polyphenols have a low oral bioavailability, which is mainly due to extensive biotransformation mediated by phase I and phase II reactions in the enterocytes and liver, as well as in the intestinal microbiota [157,158].
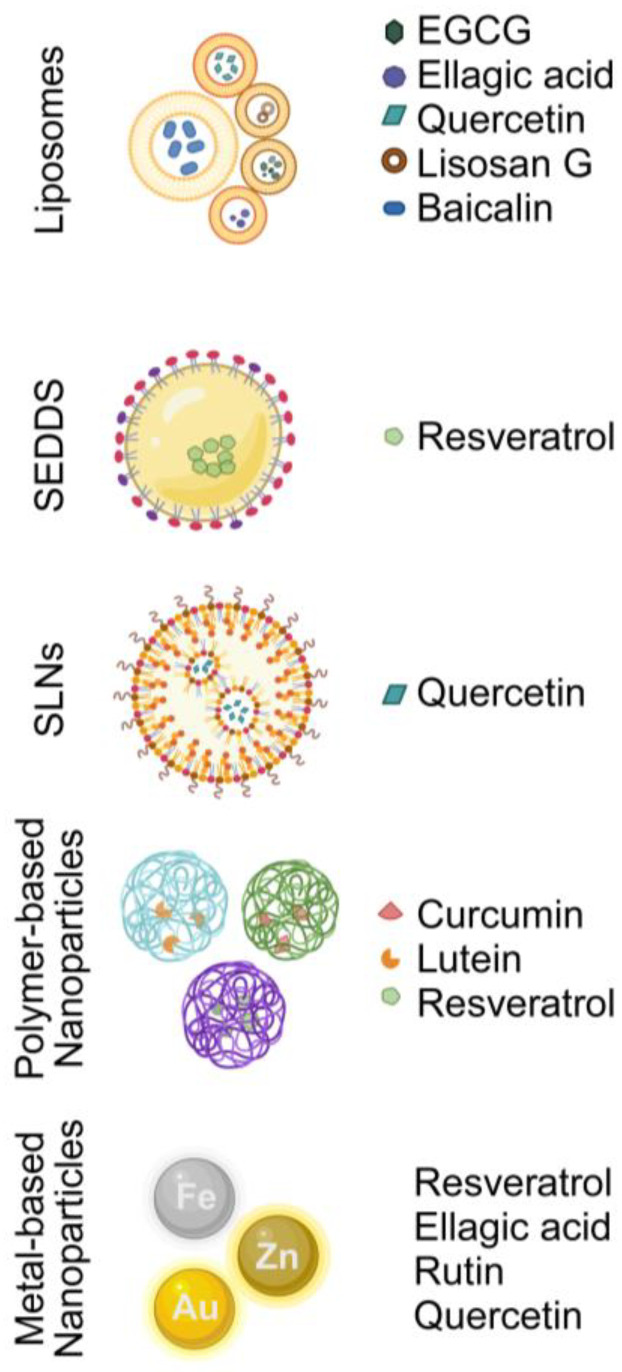
Furthermore, the blood–ocular barrier hinders the entry of peroral bioactive compounds into the posterior segment. Over the decades, scientists have attempted to introduce and refine nutrient carriers and delivery systems to yield higher bioavailability and, thus, better efficacy. Nanoencapsulation technology has been developed to overcome unwanted conditions such as gastrointestinal digestion and cellular metabolism. Here, we discussed a few of the typically used classes of nano-delivery systems and summarized some nutraceutical-loaded nanocarriers that can be potentially applied in DR (Figure 2 and Table 3). The classification of nanocarriers could fall into three groups: (i) lipid and surfactant-based nanocarriers, (ii) biopolymer-based nanocarriers, and (iii) metal-based nanoparticles [154,159].
Figure 2.
An illustration of the delivery systems mentioned in the present review. (Abbreviations: EGCG, epigallocatechin gallate; SEDDS, self-emulsifying drug delivery system; SLNS, solid lipid nanoparticles).
5.1. Lipid and Surfactant-Based Nanocarriers
5.1.1. Nanoemulsions
Nanoemulsions (NEs) are emulsion systems carrying droplets with diameters ranging between 50 and 1000 nm. They exist in multiple forms including oil-in-water (O/W) NEs and water-in-oil (W/O) NEs [160]. It is well-demonstrated that carotenoids can be absorbed more easily when administered together with fat [161]. Olive oil, rich in oleic acids, was reported to boost the intestinal absorption of lutein in mice [162]. Using NE technology, lutein-encapsulated oleic–linoleic acid O/W NEs could improve the oral bioavailability of lutein (5.83 folds bioaccessibility of free lutein) in rats [163]. Furthermore, smaller O/W NEs containing lutein (~10 nm) are promising candidates for topical ocular application to eye diseases related to oxidative stress [164]. It was demonstrated that with penetratin modification, lutein NEs could not only be better taken up by ARPE-19 retinal pigment epithelial cells but also show higher bioactivity in inhibiting HUVEC migration [165]. In addition, with the assistance of an in situ gel, the residence time of the pre-corneal drug containing lutein in the eye was prolonged when instilled in the lower conjunctival sac in the rats; this further increased the amount of drug reaching the fundus, alleviating the sodium iodate-induced retina damage [165]. Despite the better stability and bioavailability, these lutein NEs have not been tested in in vitro or in vivo models of DR, and extended investigation is needed to promote the applications of NEs in DR. Apart from lutein, it is also worthwhile to develop and explore NE technology for other carotenoids in the context of DR.
5.1.2. Liposomes and Nanoliposomes
Liposomes are spherical or oval vesicles with phospholipid bilayers and an aqueous core with diameters ranging from tens of nanometers to hundreds of micrometers. Nanoliposomes are nano-sized liposomes with diameters below 200 nm [166]. Liposomes have been wildly applied in the drug industry for their ability to carry and enhance the stability of hydrophilic (in the aqueous core) and lipophilic (between the lipid bilayers) substances [166,167]. In addition, the phospholipid bilayers in liposomes allow for high biocompatibility; when modified with targeting ligand-like antibodies, targeted delivery can be achieved [168].
The application of liposomes in encapsulating certain nutraceuticals has been investigated over recent years. Baicalin is a flavonoid with anti-inflammatory, antioxidant, and anti-angiogenic effects in the eye [169,170]. However, baicalin is poorly soluble and unstable in basic pH. In order to improve its bioavailability, Ashraf et al. fabricated and compared different baicalin vesicular systems (liposomes, penetration enhancer vesicles, and transfersomes) and found that baicalin liposomes displayed the highest absorption rate [171]. Another example is anthocyanins, which are unstable and sensitive to many influences, such as oxygen, temperature, and UV radiation. Anthocyanins-loaded nanoliposomes manufactured with ultrasonication showed higher stability, cellular uptake by Caco-2 cells, and antioxidative properties in vitro [172]. It was reported that N-trimethyl chitosan (TMC)-coated liposomes of C3G (a specific type of anthocyanins) could alleviate the oxidative stress caused by selenite sodium in rats as a precorneal drug [173]. Likewise, TMC-coated flexible liposomes with resveratrol were shown to pass through the biological barrier and reach the ocular fundus as eye drops to mitigate the blue-light-induced retinal damage in ICR mice [174].
For diabetic complications, the application of liposomes has also been explored. Oral administration of pegylated quercetin liposomes elevated quercetin concentrations in plasma compared with non-encapsulated quercetin, resulting in significant attenuation of the oxidative stress indicators in serum and kidneys and amelioration STZ-induced diabetic nephropathy in rats [175]. Similarly, intraperitoneal injection of liposomal EGCG was demonstrated to suppress oxidative stress and enhance the total antioxidant capacity of plasma (TAC), thiols, and catalase in STZ-induced DR rats [176]. In addition, EGCG-loaded nanoliposomes could lower the level of matrix-metalloproteinase-2 (MMP-2) and -9 (MMP-9), which are important in the progression of DR [176]. Lisosan G (LG) is a fermented powder acquired from whole grains that is protective of DR due to its abundance of bioactive substances, like polyphenols, alpha-lipoic acid, PUFAs, and vitamins [177]. Recently, a 6-week gavage of LG-encapsulated liposomes was shown to significantly rescue the retinal function of STZ-induced DR [178].
Besides encapsulating nutraceuticals in liposomes, specific ligands can be added to modify the liposomes, such as the isoDGR, a tripeptide motif that can combine with αvβ3 integrin [179]. Li and his colleagues invented one kind of liposome co-loaded with ellagic acid and hemoglobin and adjusted with TAT peptide to promote cellular uptake as well as isoDGR to achieve targeted delivery (EA-Hb/TAT&isoDGR-Lipo) [180]. EA-Hb/TAT&isoDGR-Lipo displayed great efficacy when administered intravenously or as an eye drop in ameliorating DR in db/db mice by scavenging ROS, downregulating the expression of GFAP, HIF-1α, VEGF, and p-VEGFR2 [180].
5.1.3. Self-Emulsifying Drug Delivery Systems (SEDDSs)
Different ratios of oils and surfactants, together with lipophilic substances, form isotropic solutions called SEDDSs. SEDDSs are named after their spontaneous formation of emulsions or microemulsions after being added to water and lightly agitated [154]. With droplet sizes smaller than 200 nm, self-nanoemulsifying drug delivery systems (SNEDDSs) are superior for their good absorption rate and dispersion in the tissue [181]. Zingale et al. developed an SNEDDS loaded with resveratrol (RSV-SNEDDS) and tested its biocompatibility in a rabbit corneal epithelial cell line (SIRC) [182]. The RSV-SNEDDS displayed improved solubility, stability, and bioavailability, suggesting that SNEDDSs can be used as promising nanocarriers for drugs to deliver toward the posterior ocular segment [182].
5.1.4. Solid Lipid Nanoparticles
Solid lipid nanoparticles (SLNs), consisting of solid lipids with melting points higher than 40 °C, are a nontoxic nanocarrier system that provide outstanding solubilization of lipophilic compounds and excellent protection of the contents in the complex environment of the gastrointestinal tract [154]. SLNs of quercetin, a nanoformulation of quercetin (NQ), were generated and demonstrated competence in treating STZ-induced DR in a zebrafish model [183]. Intraperitoneal injection of NQ restored the retinal function in the STZ-induced DR zebrafish by lowering the blood glucose level, regulating the homocysteine pathway, and scavenging ROS [183,184].
5.2. Polymer-Based Nanocarriers
Apart from the lipid-based and surfactant-based nanocarriers, biopolymeric nanoparticles using biopolymer-like polysaccharides, proteins, polyethylene glycol (PEG), and polylactic acid are another important category of nano-delivery system [154]. Toragall and Baskaran developed a lutein-loaded chitosan–sodium alginate-based nanocarrier system (LNCs) and found that LNCs led to higher retinal lutein levels in STZ-induced DR rats when administered orally, with 2.80-fold of area under the curve (AUC) compared to the micellar lutein-treated group [185]. Later, they found that LNCs could slow and control the release of lutein from LNCs, and showed better cellular antioxidant and anti-angiogenic efficacy in ARPE-19 retinal pigment epithelial cells by activating Nrf2 translocation and downregulating the level of VEGF through HIF-1α and activating transcription factor-4 (ATF4)/X-box binding protein 1 (XBP-1) signaling [186].
Resveratrol has also been reported to be modified and loaded in a polyelectrolyte microcapsule and covered by rhodamine 6G (PMs-Rv-Rh6G) [187]. PMs-Rv-Rh6G exhibited a high ratio (60%) of internalization by D407 cells with anti-VEGF and anti-inflammatory effects, suggesting its potential application as an intravitreal injection to treat DR [187]. Besides being used in management alone, nanoparticles of nutraceuticals used in combination with the standard treatments can achieve better outcomes. It was demonstrated that the STZ-induced DR rats treated with insulin jointly with oral delivery of the curcumin-laden double-headed nanoparticles displayed ameliorated diabetic cataracts and retinopathy compared to those treated with insulin alone [188].
5.3. Metal-Based Nanoparticles
Comprised of metals or metal oxides, metal-based nanoparticles enjoy a promising future in drug or gene delivery and magnetic diagnostics as they can be conjugated with antibodies, ligands, and contents of interest [189]. Marella et al. used ZnO nanoparticles to encapsulate ellagic acid (NEA) [190]. The NEA showed improved solubility and biological inhibitory actions on aldose reductase and α-glucosidase but at the same time displayed minimal toxicity and a low degradation rate of ellagic acid [190]. Gui et al. produced an ultrasmall (5–10 nm) coordination polymer nanodots nanozyme by coupling quercetin with low-toxic iron ions (Fe-Quer NZs) [191]. It was reported that Fe-Quer NZs mimicked the activity of three antioxidant enzymes, superoxide dismutase, peroxidase, and catalase, and, in turn, showed an excellent ability to protect against inflammation, oxidative stress, microvascular leakage, and angiogenesis in STZ-induced diabetic rats [191]. Moreover, data from the optical coherence tomography angiography (OCTA) imaging reveal that oral intake of Fe-Quer NZs restored the retinal blood flow and fundus blood density in STZ-damaged retinae, suggesting their utilization in early NPDR [191].
Gold nanoparticles (AuNPs) are highly flavored as drug delivery systems for their chemical stability, low toxicity, easy functionalization (strong affinity for functional groups like thiols), and photo-responsive activity [192]. When rutin was conjugated with AuNPs, these nanoparticles (AuNPsR) showed higher oral bioavailability with increased antioxidant capacity and the function to improve the fundus appearance of retinal arterioles [193]. Stoia et al. utilized the strengths of the active anisotropic gold bipyramidal nanoparticles (AuBPs) as efficient photothermal agents and fabricated a resveratrol-encapsulated nanocarrier with a calcium carbonate core (CaCO3 MC-AuBPs) [194]. CaCO3 MC-AuBPs are of great interest in treating retinal diseases like DR as they process the power of the controlled release of therapeutic resveratrol based on the laser-induced thermoplasmonic effect at the retinal level [194].
Interestingly, bioactive nutraceuticals can not only be the core compounds loaded in the nanoparticles, but they can also serve as green adjunctive reagents in the process of synthesis of drug delivery systems [195]. For example, resveratrol was used as a stabilizing and reducing agent when fabricating a type of AuNPs [196]. These resveratrol-coated AuNPs demonstrated a remedial effect on STZ-induced DR in rats [196]. Such manifestations all highlight the great potential of nutraceuticals in DR.
Table 3.
A summary on the studies in delivery systems for nutraceuticals in DR-related models.
| Compound | In Vivo or In Vitro | Dosage and Administration Way | Name of the Product | Particle Size (nm) | Cell Culture/Animal Model | Effects | Improvements | Year | Refs. |
|---|---|---|---|---|---|---|---|---|---|
| Nanoemulsions | |||||||||
| Lutein | In vivo | 600 μM of lutein (p.o.) | Lutein-NEL | 110 ± 8 | Rats | / | Improve the bioaccessibility of lutein | 2021 | [163] |
| Liposomes | |||||||||
| Baicalin | In vivo | As eye drops, instilled (100 μL) in the conjunctival sac | Baicalin vesicles | 667–1341 | Rabbits | Antioxidative | Improve stabilization, sterilization endurance, and safety with pharmacokinetic superiority | 2018 | [171] |
| Epigallocatechin-5-gallate (EGCG); liposomal EGCG | In vivo | 2.5 mg/100 g b.w./day (i.p., once a day for two consecutive days before STZ administration) | Liposomal nanoformulation of EGCG | 170 | STZ-induced DR (rats) | Antioxidative | Superior antioxidant activity of L-EGCG; enhanced availability of EGCG | 2020 | [176] |
| Ellagic acid (EA) | In vitro and in vivo | 10 µg/mL | Liposomes (EA-Hb/TAT and isoDGR-Lipo) | 170.77–212.90 | Hyperglycemia/hypoxia-induced injury in ARPE-19 cells/HUVECs | Ameliorated retinal structure, antioxidative, downregulated the expression of GFAP, HIF-1α, VEGF, and p-VEGFR2 | Better cellular uptake; potential as eye drops; co-loaded with Hb | 2023 | [180] |
| 5 mg/kg (i.v., once every 3 days for 6 weeks); as eye drops | db/db mice | ||||||||
| Lisosan G | In vivo | 1 g kg/day (p.o.) | Lisosan G in liposomes (LipoLG) | ~130 | STZ-induced DR (mice) | Restored retinal function, downregulated typical molecular hallmarks of DR (oxidative stress, inflammation, glial reaction, apoptosis, VEGF expression, and BRB breakdown) | Good entrapment efficiency of Lisosan G, good storage stability | 2023 | [178] |
| Quercetin | In vivo | 50, 200 mg/kg (p.o.) | Pegylated quercetin liposomes (Q-PEGL) | 128.8 ± 18.05 | STZ-induced diabetic nephropathy (rats) | FBG level ↓, antioxidative | Maintaining higher quercetin concentrations in plasma | 2020 | [175] |
| SNEDDS | |||||||||
| Resveratrol | In vitro | As eye drops | RSV-SNEDDS | <100 | Rabbit corneal epithelial cell line (SIRC) | / | Improved solubility, stability, and bioavailability; reduced drug loss during storage | 2024 | [182] |
| Solid lipid nanoparticles | |||||||||
| Quercetin | In vivo | 5 and 10 mg/kg (i.p. for 21 days) | Nano-formulation of quercetin (NQ) | 157.1–528.2 | STZ-induced DR (zebrafish) | Neuroprotective, ameliorated DR | Good bioavailability | 2020 | [183] |
| Polymeric nanocarriers | |||||||||
| Curcumin | In vivo | nCUR (20 mg CUR equivalent/kg/day, p.o.) with or without subcutaneous insulin (2 IU/rat/day) | PLGA-GA2-CUR nanoparticles (nCUR) | 261 | STZ-induced DR (rats) | Anti-inflammatory and anti-hyperglycemic; prevented diabetic cataracts and retinopathy | Well-tolerated, lower nanoparticle toxicity | 2023 | [188] |
| Lutein | In vitro | Micellar lutein (10 μM) or LNCs (10 μM lutein) (0, 3, 6, 12, 18, 24 h) | Double-layered chitosan–sodium alginate-based lutein nanocarrier (LNCs) | 95 ± 5 | H2O2/CoCl2-treated ARPE-19 cells | Anti-angiogenic, antioxidative | Increased cellular uptake, slowed and controlled lutein release; LNCs improved the cellular efficacy of lutein by curtailing oxidative stress. | 2023 | [186] |
| Lutein | In vitro and in vivo | 0, 1, 5, 10, 15, 15, 20, or 50 μM for 24 h | Lutein-loaded chitosan–sodium alginate-based nanocarrier systems (LNCs) | 98 ± 5 | H2O2-treated ARPE-19 cells | Antioxidative | Longer half-life of lutein, higher bioavailability | 2021 | [185] |
| 600 μM (p.o.) | STZ-induced DR (rat) | ||||||||
| Resveratrol | In vitro | Intravitreal injection | PMs-Rv-Rh6G | 3579 ± 0.19 | HRPE cells (D407) | Anti-VEGF, anti-inflammatory | High-efficiency encapsulation of resveratrol | 2019 | [187] |
| Metal-based and biopolymeric nanoparticles | |||||||||
| Resveratrol | In vitro | / | NIR light-responsive thermoplasmonic-triggered release of therapeutic resveratrol-carrying polymeric microcapsules (MC) | <100 | HRPE cells (D407) | Anti-VEGF | Light-triggered delivery and release; high stability; great biocompatibility | 2022 | [194] |
| Metal-based nanoparticles | |||||||||
| Ellagic acid (EA) | In silico docking study | / | Nano-encapsulated ellagic acid (NEA) | 161–297 | / | Inhibitory actions on aldose reductase and α-glucosidase | Improved the solubility and biological responses besides minimizing toxicity and degradation | 2020 | [190] |
| Rutin | In vivo | Rutin (10 mg/kg/day) or AuNPsR (0.6 mL/day); (p.o. for 7 days) | AuNPsR | 8–22 (mean = 15) | STZ-induced DR (rats) | Antioxidative, improved fundus appearance of retinal arterioles, decreased MDA, and increased antioxidant capacity | Improved bioavailability, green synthesis | 2023 | [193] |
| Quercetin | In vitro and in vivo | Fe-Quer NZs (25, 50, 100, or 200 µg/mL) for 48 h | Ultrasmall Fe-Quer nanozymes (NZs) | 5–10 | HG-induced injury in HUVECs and monkey choroid–retinal endothelial cells (RF) | Protected against inflammation, oxidative stress damage, microvascular leakage, and angiogenesis | Exhibiting excellent water dispersibility and efficient ROS scavenging ability | 2023 | [191] |
| 60 mg/kg (p.o.) | STZ-induced DR (rats) | ||||||||
Abbreviations: Administration routes: i.p., intraperitoneal injection; i.v., intravenous injection; p.o., per os (by mouth). Others: BRB, blood–retinal barrier; FBG, fasting blood glucose; GFAP, glial fibrillary acidic protein; Hb, hemoglobin; HIF-1α, hypoxia-inducible factor-1 alpha; p-VEGFR2, phosphorylated vascular endothelial growth factor receptor 2; STZ, streptozotocin; VEGF, vascular endothelial growth factor; ↓: down-regulated.
6. Conclusions and Further Remarks
Overall, ample evidence has demonstrated the promising potential of nutraceuticals in managing DR, either through oral administration, injections, or even through topical application. Meanwhile, scientists are also motivated to explore the underlying mechanisms of nutraceuticals in DR-related models. Indeed, most nutraceuticals display strong antioxidant and anti-inflammatory properties. Furthermore, some of them could protect neurons, neuroglia, and epithelial cells and improve retinal function and retinal vascular function. Such effects may involve different pathways like NF-κB and HIF-1α signaling, which can provide clues on the roles of nutraceuticals in DR.
However, when it comes to practical clinical utilization, some prominent candidates lost their magic, as indicated in some clinical trial studies, such as omega-3 PUFAs. Additionally, the relatively low bioavailability (low bioaccessibility, absorption rate, or transformation) of most nutraceutical-like carotenoids and polyphenols impedes their practical application. Moreover, some DM patients may have impaired liver and renal function, which prevents them from taking relatively large doses of nutraceuticals that are tested to be effective. However, the technique of nanoparticle delivery systems offers the benefits of greater carrying capacity and better bioavailability for nutraceuticals. Notably, the targeted and controlled-release modifications of nanoparticles have enabled tailored delivery of nutraceuticals to the retina. This is of great importance as many active nutraceuticals cannot reach high concentrations in the retina due to the blood–ocular barrier. However, the newly emerging products are mainly in their initial stages of research and development, with most studies being in vitro and few being in vivo; further research is crucial to provide important information for supporting and promoting their clinical application in NPDR and DR.
Advancements in nutraceutical delivery designs and industrialized production not only aid in disease prevention and patient recovery, but also meet market demands. According to Mordor Intelligence research company, the global nutraceutical market in 2024 is estimated to be USD 488.41 billion, with a compound annual growth rate of 5.09% from 2024 to 2029 [https://www.mordorintelligence.com/industry-reports/global-nutraceuticals-market-industry (accessed on 22 May 2024)]. The growing interest in functional foods among consumers stems mainly from increased health awareness and potential health benefits of nutraceuticals, as well as economic growth and customer spending. Thus, research on nutraceuticals is essential in view of their scientific and socio-economic impact.
In conclusion, despite their relatively low bioavailability and low efficiency compared to many drugs, nutraceuticals, especially when administrated orally, possess the advantages of being nontoxic and easily accessible with few complications. Nutraceuticals offer strong antioxidant and anti-inflammatory effects, making them potential retino-protective prophylactic daily supplementations for patients affected by NPDR and possibly PDR, improving their quality of life. With the power of nano-delivery technology, nutraceuticals can better benefit DR patients as a more effective, precise, and harmless adjunctive treatment strategy.
Abbreviations
| AGEs | Advanced glycation end products |
| AMPK | AMP-activated protein kinase |
| Ang-2 | Angiopoietin 2 |
| AuNPs | Gold nanoparticles |
| BRAs | Black raspberry-derived anthocyanins |
| BRB | Blood–retinal barrier |
| C3G | Cyanidin-3-glucoside |
| DHA | Docosahexaenoic acid |
| DME | Diabetic macular edema |
| DR | Diabetic retinopathy |
| EGCG | Epigallocatechin-3-gallate |
| eNOS | Endothelial nitric oxide synthase |
| EPA | Eicosapentaenoic acid |
| ER | Endoplasmic reticulum |
| ERK1/2 | Extracellular signal-regulated kinase 1/2 |
| FADH2 | Flavin adenine dinucleotide |
| GIT | Gastrointestinal tract |
| GRP78 | 78-kDa glucose-regulated protein |
| HG | High glucose |
| HIF-1α | Hypoxia-inducible factor alpha |
| HO-1 | Heme Oxygenase-1 |
| HREC | Human retinal endothelial cells |
| IL | Interleukin |
| MAPK | Mitogen-activated protein kinases |
| mTOR | Mammalian target of rapamycin |
| MUFA | Monounsaturated fatty acids |
| NEs | Nanoemulsions |
| NF-κb | Nuclear factor-kappa B |
| NGF | Nerve growth factor |
| NLRP3 | NOD-like receptor family pyrin domain containing 3 |
| NPDR | Nonproliferative diabetic retinopathy |
| Nrf2 | Nuclear factor erythroid 2-related factor 2 |
| O/W | Oil-in-water |
| OA | Oleic acid |
| OIR | Oxygen-induced retinopathy |
| PDR | Proliferative diabetic retinopathy |
| PI3K | Phosphoinositide 3 kinase |
| PKC | Protein kinase C |
| PKR | Protein kinase R |
| PRP | Panretinal photocoagulation |
| PSD | Postsynaptic density |
| PUFA | Polyunsaturated fatty acids |
| RAGEs | Receptor for AGEs |
| RCT | Randomized controlled trial |
| ROS | Reactive oxygen species |
| RPE | Retinal pigment epithelial cells |
| SEDDS | Self-emulsifying drug delivery systems |
| SFA | Saturated fatty acids |
| SIRT1 | Sirtuin 1 |
| SIRT3 | Sirtuin 3 |
| SNEDDS | Self-nanoemulsifying drug delivery systems |
| STZ | Streptozotocin |
| T1DM | Type 1 diabetes mellitus |
| T2DM | Type 2 diabetes mellitus |
| TCA | Tricarboxylic acid |
| TNF-α | Tumor necrosis factor-α |
| TXNIP | Thioredoxin-interacting protein |
| VEGF | Vascular endothelial growth factor |
| VTDR | Vision-threatening diabetic retinopathy |
| W/O | Water-in-oil |
Author Contributions
Conceptualization, X.Y. and A.C.Y.L.; writing—original draft preparation, X.Y.; writing—review and editing, A.C.Y.L., N.S.K.F. and W.C.L.; funding acquisition, A.C.Y.L. All authors have read and agreed to the published version of the manuscript.
Conflicts of Interest
The authors declare no conflicts of interest.
Funding Statement
This research was funded by The Health and Medical Research Fund, the Food and Health Bureau, The Government of the Hong Kong Special Administration Region of China (No. 09201116) to A.C.Y.L. and General Research Fund, Research Grants Council, The Government of the Hong Kong Special Administrative Region (17112919) to A.C.Y.L.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Yamada M., Hiratsuka Y., Roberts C.B., Pezzullo M.L., Yates K., Takano S., Miyake K., Taylor H.R. Prevalence of Visual Impairment in the Adult Japanese Population by Cause and Severity and Future Projections. Ophthalmic Epidemiol. 2010;17:50–57. doi: 10.3109/09286580903450346. [DOI] [PubMed] [Google Scholar]
- 2.Lundeen E.A., Burke-Conte Z., Rein D.B., Wittenborn J.S., Saaddine J., Lee A.Y., Flaxman A.D. Prevalence of Diabetic Retinopathy in the US in 2021. JAMA Ophthalmol. 2023;141:747–754. doi: 10.1001/jamaophthalmol.2023.2289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Liu L., Wu X., Liu L., Geng J., Yuan Z., Shan Z., Chen L. Prevalence of Diabetic Retinopathy in Mainland China: A Meta-Analysis. PLoS ONE. 2012;7:e45264. doi: 10.1371/journal.pone.0045264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yau J.W.Y., Rogers S.L., Kawasaki R., Lamoureux E.L., Kowalski J.W., Bek T., Chen S.-J., Dekker J.M., Fletcher A., Grauslund J., et al. Global Prevalence and Major Risk Factors of Diabetic Retinopathy. Diabetes Care. 2012;35:556–564. doi: 10.2337/dc11-1909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bandello F., Zarbin M.A., Lattanzio R., Zucchiatti I. Clinical Strategies in the Management of Diabetic Retinopathy: A Step-by-Step Guide for Ophthalmologists. 2nd ed. Springer; Cham, Switzerland: 2019. [Google Scholar]
- 6.Nyengaard J.R., Ido Y., Kilo C., Williamson J.R. Interactions between Hyperglycemia and Hypoxia: Implications for Diabetic Retinopathy. Diabetes. 2004;53:2931–2938. doi: 10.2337/diabetes.53.11.2931. [DOI] [PubMed] [Google Scholar]
- 7.Lorenzi M. The Polyol Pathway as a Mechanism for Diabetic Retinopathy: Attractive, Elusive, and Resilient. Exp. Diabetes Res. 2007;2007:61038. doi: 10.1155/2007/61038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chiu C.-J., Taylor A. Dietary Hyperglycemia, Glycemic Index and Metabolic Retinal Diseases. Prog. Retin. Eye Res. 2011;30:18–53. doi: 10.1016/j.preteyeres.2010.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Browning D.J. Diabetic Retinopathy Evidence-Based Management. Springer; New York, NY, USA: 2010. [Google Scholar]
- 10.Kang Q., Yang C. Oxidative Stress and Diabetic Retinopathy: Molecular Mechanisms, Pathogenetic Role and Therapeutic Implications. Redox Biol. 2020;37:101799. doi: 10.1016/j.redox.2020.101799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Agbaga M.-P., Brush R.S., Mandal M.N.A., Henry K., Elliott M.H., Anderson R.E. Role of Stargardt-3 Macular Dystrophy Protein (ELOVL4) in the Biosynthesis of Very Long Chain Fatty Acids. Proc. Natl. Acad. Sci. USA. 2008;105:12843–12848. doi: 10.1073/pnas.0802607105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fliesler S.J., Anderson R.E. Chemistry and Metabolism of Lipids in the Vertebrate Retina. Prog. Lipid Res. 1983;22:79–131. doi: 10.1016/0163-7827(83)90004-8. [DOI] [PubMed] [Google Scholar]
- 13.Tanito M., Elliott M.H., Kotake Y., Anderson R.E. Protein Modifications by 4-Hydroxynonenal and 4-Hydroxyhexenal in Light-Exposed Rat Retina. Investig. Ophthalmol. Vis. Sci. 2005;46:3859–3868. doi: 10.1167/iovs.05-0672. [DOI] [PubMed] [Google Scholar]
- 14.Choudhary S., Xiao T., Srivastava S., Zhang W., Chan L.L., Vergara L.A., Van Kuijk F.J.G.M., Ansari N.H. Toxicity and Detoxification of Lipid-Derived Aldehydes in Cultured Retinal Pigmented Epithelial Cells. Toxicol. Appl. Pharmacol. 2005;204:122–134. doi: 10.1016/j.taap.2004.08.023. [DOI] [PubMed] [Google Scholar]
- 15.Zeng H., Green W.R., Tso M.O.M. Microglial Activation in Human Diabetic Retinopathy. Arch. Ophthalmol. 2008;126:227–232. doi: 10.1001/archophthalmol.2007.65. [DOI] [PubMed] [Google Scholar]
- 16.Vujosevic S., Simó R. Local and Systemic Inflammatory Biomarkers of Diabetic Retinopathy: An Integrative Approach. Investig. Ophthalmol. Vis. Sci. 2017;58:BIO68–BIO75. doi: 10.1167/iovs.17-21769. [DOI] [PubMed] [Google Scholar]
- 17.Zhou J., Wang S., Xia X. Role of Intravitreal Inflammatory Cytokines and Angiogenic Factors in Proliferative Diabetic Retinopathy. Curr. Eye Res. 2012;37:416–420. doi: 10.3109/02713683.2012.661114. [DOI] [PubMed] [Google Scholar]
- 18.Dai Y., Wu Z., Wang F., Zhang Z., Yu M. Identification of Chemokines and Growth Factors in Proliferative Diabetic Retinopathy Vitreous. BioMed Res. Int. 2014;2014:486386. doi: 10.1155/2014/486386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mason R.H., Minaker S.A., Lahaie Luna G., Bapat P., Farahvash A., Garg A., Bhambra N., Muni R.H. Changes in Aqueous and Vitreous Inflammatory Cytokine Levels in Proliferative Diabetic Retinopathy: A Systematic Review and Meta-Analysis. Eye. 2022:1–51. doi: 10.1038/s41433-022-02127-x. [DOI] [PubMed] [Google Scholar]
- 20.Loukovaara S., Piippo N., Kinnunen K., Hytti M., Kaarniranta K., Kauppinen A. NLRP3 Inflammasome Activation Is Associated with Proliferative Diabetic Retinopathy. Acta Ophthalmol. 2017;95:803–808. doi: 10.1111/aos.13427. [DOI] [PubMed] [Google Scholar]
- 21.Ding X., Sun Z., Guo Y., Tang W., Shu Q., Xu G. Inhibition of NF-κB Ameliorates Aberrant Retinal Glia Activation and Inflammatory Responses in Streptozotocin-Induced Diabetic Rats. Ann. Transl. Med. 2023;11:197. doi: 10.21037/atm-22-2204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mitamura Y., Harada T., Harada C., Ohtsuka K., Kotake S., Ohno S., Tanaka K., Takeuchi S., Wada K. NF-kappaB in Epiretinal Membranes after Human Diabetic Retinopathy. Diabetologia. 2003;46:699–703. doi: 10.1007/s00125-003-1084-x. [DOI] [PubMed] [Google Scholar]
- 23.Chen H., Zhang X., Liao N., Mi L., Peng Y., Liu B., Zhang S., Wen F. Enhanced Expression of NLRP3 Inflammasome-Related Inflammation in Diabetic Retinopathy. Investig. Ophthalmol. Vis. Sci. 2018;59:978–985. doi: 10.1167/iovs.17-22816. [DOI] [PubMed] [Google Scholar]
- 24.Spencer B.G., Estevez J.J., Liu E., Craig J.E., Finnie J.W. Pericytes, Inflammation, and Diabetic Retinopathy. Inflammopharmacology. 2020;28:697–709. doi: 10.1007/s10787-019-00647-9. [DOI] [PubMed] [Google Scholar]
- 25.van der Wijk A.-E., Hughes J.M., Klaassen I., Van Noorden C.J.F., Schlingemann R.O. Is Leukostasis a Crucial Step or Epiphenomenon in the Pathogenesis of Diabetic Retinopathy? J. Leukoc. Biol. 2017;102:993–1001. doi: 10.1189/jlb.3RU0417-139. [DOI] [PubMed] [Google Scholar]
- 26.Khalaf N., Helmy H., Labib H., Fahmy I., El Hamid M.A., Moemen L. Role of Angiopoietins and Tie-2 in Diabetic Retinopathy. Electron. Physician. 2017;9:5031–5035. doi: 10.19082/5031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Aiello L.P., Avery R.L., Arrigg P.G., Keyt B.A., Jampel H.D., Shah S.T., Pasquale L.R., Thieme H., Iwamoto M.A., Park J.E. Vascular Endothelial Growth Factor in Ocular Fluid of Patients with Diabetic Retinopathy and Other Retinal Disorders. N. Engl. J. Med. 1994;331:1480–1487. doi: 10.1056/NEJM199412013312203. [DOI] [PubMed] [Google Scholar]
- 28.Li S.-Y., Fu Z.J., Lo A.C.Y. Hypoxia-Induced Oxidative Stress in Ischemic Retinopathy. Oxid. Med. Cell. Longev. 2012;2012:426769. doi: 10.1155/2012/426769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pe’er J., Shweiki D., Itin A., Hemo I., Gnessin H., Keshet E. Hypoxia-Induced Expression of Vascular Endothelial Growth Factor by Retinal Cells Is a Common Factor in Neovascularizing Ocular Diseases. Lab. Investig. J. Tech. Methods Pathol. 1995;72:638–645. [PubMed] [Google Scholar]
- 30.Pe’er J., Folberg R., Itin A., Gnessin H., Hemo I., Keshet E. Upregulated Expression of Vascular Endothelial Growth Factor in Proliferative Diabetic Retinopathy. Br. J. Ophthalmol. 1996;80:241–245. doi: 10.1136/bjo.80.3.241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Reis A., Mateus C., Melo P., Figueira J., Cunha-Vaz J., Castelo-Branco M. Neuroretinal Dysfunction with Intact Blood-Retinal Barrier and Absent Vasculopathy in Type 1 Diabetes. Diabetes. 2014;63:3926–3937. doi: 10.2337/db13-1673. [DOI] [PubMed] [Google Scholar]
- 32.Santos A.R., Ribeiro L., Bandello F., Lattanzio R., Egan C., Frydkjaer-Olsen U., García-Arumí J., Gibson J., Grauslund J., Harding S.P., et al. Functional and Structural Findings of Neurodegeneration in Early Stages of Diabetic Retinopathy: Cross-Sectional Analyses of Baseline Data of the EUROCONDOR Project. Diabetes. 2017;66:2503–2510. doi: 10.2337/db16-1453. [DOI] [PubMed] [Google Scholar]
- 33.Palmowski A.M., Sutter E.E., Bearse M.A., Fung W. Mapping of Retinal Function in Diabetic Retinopathy Using the Multifocal Electroretinogram. Investig. Ophthalmol. Vis. Sci. 1997;38:2586–2596. [PubMed] [Google Scholar]
- 34.Gundogan F.C., Akay F., Uzun S., Yolcu U., Çağıltay E., Toyran S. Early Neurodegeneration of the Inner Retinal Layers in Type 1 Diabetes Mellitus. Ophthalmol. J. Int. Ophtalmol. Int. J. Ophthalmol. Z. Augenheilkd. 2016;235:125–132. doi: 10.1159/000442826. [DOI] [PubMed] [Google Scholar]
- 35.Zhu H., Zhang W., Zhao Y., Shu X., Wang W., Wang D., Yang Y., He Z., Wang X., Ying Y. GSK3β-Mediated Tau Hyperphosphorylation Triggers Diabetic Retinal Neurodegeneration by Disrupting Synaptic and Mitochondrial Functions. Mol. Neurodegener. 2018;13:62. doi: 10.1186/s13024-018-0295-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bui B.V., Loeliger M., Thomas M., Vingrys A.J., Rees S.M., Nguyen C.T.O., He Z., Tolcos M. Investigating Structural and Biochemical Correlates of Ganglion Cell Dysfunction in Streptozotocin-Induced Diabetic Rats. Exp. Eye Res. 2009;88:1076–1083. doi: 10.1016/j.exer.2009.01.009. [DOI] [PubMed] [Google Scholar]
- 37.Simó R., Stitt A.W., Gardner T.W. Neurodegeneration in Diabetic Retinopathy: Does It Really Matter? Diabetologia. 2018;61:1902–1912. doi: 10.1007/s00125-018-4692-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Flaxel C.J., Adelman R.A., Bailey S.T., Fawzi A., Lim J.I., Vemulakonda G.A., Ying G. Diabetic Retinopathy Preferred Practice Pattern®. Ophthalmology. 2020;127:P66–P145. doi: 10.1016/j.ophtha.2019.09.025. [DOI] [PubMed] [Google Scholar]
- 39.Fundus Disease Group of Ophthalmological Society of Chinese Medical Association. Fundus Disease Group of Ophthalmologist Branch of Chinese Medical Doctor Association Evidence-Based Guidelines for Diagnosis and Treatment of Diabetic Retinopathy in China. Chin. J. Ocul. Fundus Dis. 2022;39:99–124. doi: 10.3760/cma.j.cn511434-20230110-00018. [DOI] [Google Scholar]
- 40.Zhi X., Li Q., Shao L. Approvals by the China NMPA in 2023. Nat. Rev. Drug Discov. 2024;23:164–165. doi: 10.1038/d41573-024-00034-2. [DOI] [PubMed] [Google Scholar]
- 41.Shirley M. Faricimab: First Approval. Drugs. 2022;82:825–830. doi: 10.1007/s40265-022-01713-3. [DOI] [PubMed] [Google Scholar]
- 42.Ferro Desideri L., Traverso C.E., Nicolò M., Munk M.R. Faricimab for the Treatment of Diabetic Macular Edema and Neovascular Age-Related Macular Degeneration. Pharmaceutics. 2023;15:1413. doi: 10.3390/pharmaceutics15051413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ba W., Xu W., Deng Z., Zhang B., Zheng L., Li H. The Antioxidant and Anti-Inflammatory Effects of the Main Carotenoids from Tomatoes via Nrf2 and NF-κB Signaling Pathways. Nutrients. 2023;15:4652. doi: 10.3390/nu15214652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Abu-Amero K.K., Kondkar A.A., Chalam K.V. Resveratrol and Ophthalmic Diseases. Nutrients. 2016;8:200. doi: 10.3390/nu8040200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Dow C., Mancini F., Rajaobelina K., Boutron-Ruault M.-C., Balkau B., Bonnet F., Fagherazzi G. Diet and Risk of Diabetic Retinopathy: A Systematic Review. Eur. J. Epidemiol. 2018;33:141–156. doi: 10.1007/s10654-017-0338-8. [DOI] [PubMed] [Google Scholar]
- 46.Rossino M.G., Casini G. Nutraceuticals for the Treatment of Diabetic Retinopathy. Nutrients. 2019;11:771. doi: 10.3390/nu11040771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Athyros V.G., Doumas M., Imprialos K.P., Stavropoulos K., Georgianou E., Katsimardou A., Karagiannis A. Diabetes and Lipid Metabolism. Hormones. 2018;17:61–67. doi: 10.1007/s42000-018-0014-8. [DOI] [PubMed] [Google Scholar]
- 48.Liu Y., Zhang D., Hu J., Liu G., Chen J., Sun L., Jiang Z., Zhang X., Chen Q., Ji B. Visible Light-Induced Lipid Peroxidation of Unsaturated Fatty Acids in the Retina and the Inhibitory Effects of Blueberry Polyphenols. J. Agric. Food Chem. 2015;63:9295–9305. doi: 10.1021/acs.jafc.5b04341. [DOI] [PubMed] [Google Scholar]
- 49.Georgiou M., Prokopiou E. Diabetic Retinopathy and the Role of Omega-3 PUFAs: A Narrative Review. Exp. Eye Res. 2023;231:109494. doi: 10.1016/j.exer.2023.109494. [DOI] [PubMed] [Google Scholar]
- 50.Eynard A.R., Repossi G. Role of Ω3 Polyunsaturated Fatty Acids in Diabetic Retinopathy: A Morphological and Metabolically Cross Talk among Blood Retina Barriers Damage, Autoimmunity and Chronic Inflammation. Lipids Health Dis. 2019;18:114. doi: 10.1186/s12944-019-1049-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Behl T., Kotwani A. Omega-3 Fatty Acids in Prevention of Diabetic Retinopathy. J. Pharm. Pharmacol. 2017;69:946–954. doi: 10.1111/jphp.12744. [DOI] [PubMed] [Google Scholar]
- 52.Weir N.L., Guan W., Karger A.B., Klein B.E., Meuer S.M., Cotch M.F., Guo X., Li X., Tan J., Genter P. Omega-3 Fatty Acids Are Associated with Decreased Presence and Severity of Diabetic Retinopathy: A Combined Analysis of MESA and GOLDR Cohorts. Retina. 2023;43:984–991. doi: 10.1097/IAE.0000000000003745. [DOI] [PubMed] [Google Scholar]
- 53.Saini R.K., Keum Y.-S. Omega-3 and Omega-6 Polyunsaturated Fatty Acids: Dietary Sources, Metabolism, and Significance—A Review. Life Sci. 2018;203:255–267. doi: 10.1016/j.lfs.2018.04.049. [DOI] [PubMed] [Google Scholar]
- 54.Brown T.J., Brainard J., Song F., Wang X., Abdelhamid A., Hooper L. Omega-3, Omega-6, and Total Dietary Polyunsaturated Fat for Prevention and Treatment of Type 2 Diabetes Mellitus: Systematic Review and Meta-Analysis of Randomised Controlled Trials. BMJ. 2019;366:l4697. doi: 10.1136/bmj.l4697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Simopoulos A.P. The Importance of the Omega-6/Omega-3 Fatty Acid Ratio in Cardiovascular Disease and Other Chronic Diseases. Exp. Biol. Med. 2008;233:674–688. doi: 10.3181/0711-MR-311. [DOI] [PubMed] [Google Scholar]
- 56.Wendell S.G., Baffi C., Holguin F. Fatty Acids, Inflammation, and Asthma. J. Allergy Clin. Immunol. 2014;133:1255–1264. doi: 10.1016/j.jaci.2013.12.1087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Simopoulos A.P. The Importance of the Ratio of Omega-6/Omega-3 Essential Fatty Acids. Biomed. Pharmacother. 2002;56:365–379. doi: 10.1016/s0753-3322(02)00253-6. [DOI] [PubMed] [Google Scholar]
- 58.Zhao S., Jin D., Wang S., Xu Y., Li H., Chang Y., Ma Y., Xu Y., Guo C., Peng F., et al. Serum ω-6/ω-3 Polyunsaturated Fatty Acids Ratio and Diabetic Retinopathy: A Propensity Score Matching Based Case-Control Study in China. EClinicalMedicine. 2021;39:101089. doi: 10.1016/j.eclinm.2021.101089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Gong Y., Fu Z., Liegl R., Chen J., Hellström A., Smith L.E. ω-3 and ω-6 Long-Chain PUFAs and Their Enzymatic Metabolites in Neovascular Eye Diseases. Am. J. Clin. Nutr. 2017;106:16–26. doi: 10.3945/ajcn.117.153825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Gong Y., Fu Z., Edin M.L., Liu C.-H., Wang Z., Shao Z., Fredrick T.W., Saba N.J., Morss P.C., Burnim S.B., et al. Cytochrome P450 Oxidase 2C Inhibition Adds to ω-3 Long-Chain Polyunsaturated Fatty Acids Protection against Retinal and Choroidal Neovascularization. Arterioscler. Thromb. Vasc. Biol. 2016;36:1919–1927. doi: 10.1161/ATVBAHA.116.307558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Connor K.M., SanGiovanni J.P., Lofqvist C., Aderman C.M., Chen J., Higuchi A., Hong S., Pravda E.A., Majchrzak S., Carper D., et al. Increased Dietary Intake of Omega-3-Polyunsaturated Fatty Acids Reduces Pathological Retinal Angiogenesis. Nat. Med. 2007;13:868–873. doi: 10.1038/nm1591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Sapieha P., Stahl A., Chen J., Seaward M.R., Willett K.L., Krah N.M., Dennison R.J., Connor K.M., Aderman C.M., Liclican E., et al. 5-Lipoxygenase Metabolite 4-HDHA Is a Mediator of the Antiangiogenic Effect of Omega-3 Polyunsaturated Fatty Acids. Sci. Transl. Med. 2011;3:69ra12. doi: 10.1126/scitranslmed.3001571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Dátilo M.N., Formigari G.P., de Faria J.B.L., de Faria J.M.L. AMP Kinase Activation by Omega-3 Polyunsaturated Fatty Acid Protects the Retina against Ischemic Insult: An in Vitro and in Vivo Study. Exp. Eye Res. 2023;226:109345. doi: 10.1016/j.exer.2022.109345. [DOI] [PubMed] [Google Scholar]
- 64.Alsbirk K.E., Seland J.H., Assmus J. Diabetic Retinopathy and Visual Impairment in a Norwegian Diabetic Coast Population with a High Dietary Intake of Fish Oils. An Observational Study. Acta Ophthalmol. 2022;100:e532–e538. doi: 10.1111/aos.14977. [DOI] [PubMed] [Google Scholar]
- 65.Chew E.Y. Dietary Intake of Omega-3 Fatty Acids from Fish and Risk of Diabetic Retinopathy. JAMA. 2017;317:2226–2227. doi: 10.1001/jama.2017.1926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Sala-Vila A., Díaz-López A., Valls-Pedret C., Cofán M., García-Layana A., Lamuela-Raventós R.-M., Castañer O., Zanon-Moreno V., Martinez-Gonzalez M.A., Toledo E., et al. Dietary Marine ω-3 Fatty Acids and Incident Sight-Threatening Retinopathy in Middle-Aged and Older Individuals with Type 2 Diabetes: Prospective Investigation From the PREDIMED Trial. JAMA Ophthalmol. 2016;134:1142–1149. doi: 10.1001/jamaophthalmol.2016.2906. [DOI] [PubMed] [Google Scholar]
- 67.Lafuente M., Ortín L., Argente M., Guindo J.L., López-Bernal M.D., López-Román F.J., García M.J., Domingo J.C., Lajara J. Combined Intravitreal Ranibizumab and Oral Supplementation with Docosahexaenoic Acid and Antioxidants for Diabetic Macular Edema: Two-Year Randomized Single-Blind Controlled Trial Results. Retina. 2017;37:1277–1286. doi: 10.1097/IAE.0000000000001363. [DOI] [PubMed] [Google Scholar]
- 68.Piñas García P., Hernández Martínez F.J., Aznárez López N., Castillón Torre L., Tena Sempere M.E. Supplementation with a Highly Concentrated Docosahexaenoic Acid (DHA) in Non-Proliferative Diabetic Retinopathy: A 2-Year Randomized Double-Blind Placebo-Controlled Study. Antioxidants. 2022;11:116. doi: 10.3390/antiox11010116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Sammons E.L., Buck G., Bowman L.J., Stevens W.M., Hammami I., Parish S., Armitage J. ASCEND-Eye: Effects of Omega-3 Fatty Acids on Diabetic Retinopathy. Ophthalmology. 2023;131:526–533. doi: 10.1016/j.ophtha.2023.11.030. [DOI] [PubMed] [Google Scholar]
- 70.Kedishvili N.Y. Enzymology of Retinoic Acid Biosynthesis and Degradation. J. Lipid Res. 2013;54:1744–1760. doi: 10.1194/jlr.R037028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Carazo A., Macáková K., Matoušová K., Krčmová L.K., Protti M., Mladěnka P. Vitamin A Update: Forms, Sources, Kinetics, Detection, Function, Deficiency, Therapeutic Use and Toxicity. Nutrients. 2021;13:1703. doi: 10.3390/nu13051703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Bernstein P.S., Li B., Vachali P.P., Gorusupudi A., Shyam R., Henriksen B.S., Nolan J.M. Lutein, Zeaxanthin, and Meso-Zeaxanthin: The Basic and Clinical Science Underlying Carotenoid-Based Nutritional Interventions against Ocular Disease. Prog. Retin. Eye Res. 2016;50:34–66. doi: 10.1016/j.preteyeres.2015.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Mares J. Lutein and Zeaxanthin Isomers in Eye Health and Disease. Annu. Rev. Nutr. 2016;36:571–602. doi: 10.1146/annurev-nutr-071715-051110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.She C., Shang F., Zhou K., Liu N. Serum Carotenoids and Risks of Diabetes and Diabetic Retinopathy in a Chinese Population Sample. Curr. Mol. Med. 2017;17:287–297. doi: 10.2174/1566524017666171106112131. [DOI] [PubMed] [Google Scholar]
- 75.Shalini T., Jose S.S., Prasanthi P.S., Balakrishna N., Viswanath K., Reddy G.B. Carotenoid Status in Type 2 Diabetes Patients with and without Retinopathy. Food Funct. 2021;12:4402–4410. doi: 10.1039/D0FO03321A. [DOI] [PubMed] [Google Scholar]
- 76.Brazionis L., Rowley K., Itsiopoulos C., O’Dea K. Plasma Carotenoids and Diabetic Retinopathy. Br. J. Nutr. 2008;101:270–277. doi: 10.1017/S0007114508006545. [DOI] [PubMed] [Google Scholar]
- 77.Wang W., Tam K.C., Ng T.C., Goit R.K., Chan K.L.S., Lo A.C.Y. Long-Term Lutein Administration Attenuates Retinal Inflammation and Functional Deficits in Early Diabetic Retinopathy Using the Ins2 Akita/+ Mice. BMJ Open Diabetes Res. Care. 2020;8:e001519. doi: 10.1136/bmjdrc-2020-001519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Shivarudrappa A.H., Ponesakki G. Lutein Reverses Hyperglycemia-Mediated Blockage of Nrf2 Translocation by Modulating the Activation of Intracellular Protein Kinases in Retinal Pigment Epithelial (ARPE-19) Cells. J. Cell Commun. Signal. 2020;14:207–221. doi: 10.1007/s12079-019-00539-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Nanjaiah H., Vallikannan B. Lutein Upregulates the PGC-1α, NRF1, and TFAM Expression by AMPK Activation and Downregulates ROS to Maintain mtDNA Integrity and Mitochondrial Biogenesis in Hyperglycemic ARPE-19 Cells and Rat Retina. Biotechnol. Appl. Biochem. 2019;66:999–1009. doi: 10.1002/bab.1821. [DOI] [PubMed] [Google Scholar]
- 80.BACANLI M., BAŞARAN N., BAŞARAN A.A. Lycopene: Is It Beneficial to Human Health as an Antioxidant? Turk. J. Pharm. Sci. 2017;14:311–318. doi: 10.4274/tjps.43043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Icel E., Icel A., Uçak T., Karakurt Y., Elpeze B., Çimen F.K., Süleyman H. The Effects of Lycopene on Alloxan Induced Diabetic Optic Neuropathy. Cutan. Ocul. Toxicol. 2019;38:88–92. doi: 10.1080/15569527.2018.1530258. [DOI] [PubMed] [Google Scholar]
- 82.Lai T.-T., Yang C.-M., Yang C.-H. Astaxanthin Protects Retinal Photoreceptor Cells against High Glucose-Induced Oxidative Stress by Induction of Antioxidant Enzymes via the PI3K/Akt/Nrf2 Pathway. Antioxidants. 2020;9:729. doi: 10.3390/antiox9080729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Oh S., Kim Y.J., Lee E.K., Park S.W., Yu H.G. Antioxidative Effects of Ascorbic Acid and Astaxanthin on ARPE-19 Cells in an Oxidative Stress Model. Antioxidants. 2020;9:833. doi: 10.3390/antiox9090833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Küçüködük A., Helvacioglu F., Haberal N., Dagdeviren A., Bacanli D., Yilmaz G., Akkoyun I. Antiproliferative and Anti-Apoptotic Effect of Astaxanthin in an Oxygen-Induced Retinopathy Mouse Model. Can. J. Ophthalmol. 2019;54:65–74. doi: 10.1016/j.jcjo.2018.02.017. [DOI] [PubMed] [Google Scholar]
- 85.Subramanian A., Thirunavukkarasu J., Muthuraman A. Astaxanthin Ameliorates Diabetic Retinopathy in Swiss Albino Mice via Inhibitory Processes of Neuron-Specific Enolase Activity. Processes. 2022;10:1318. doi: 10.3390/pr10071318. [DOI] [Google Scholar]
- 86.Janani R., Anitha R.E., Divya P., Chonche M., Baskaran V. Astaxanthin Ameliorates Hyperglycemia Induced Inflammation via PI3K/Akt–NF–κB Signaling in ARPE-19 Cells and Diabetic Rat Retina. Eur. J. Pharmacol. 2022;926:174979. doi: 10.1016/j.ejphar.2022.174979. [DOI] [PubMed] [Google Scholar]
- 87.Benlarbi-Ben Khedher M., Hajri K., Dellaa A., Baccouche B., Hammoum I., Boudhrioua-Mihoubi N., Dhifi W., Ben Chaouacha-Chekir R. Astaxanthin Inhibits Aldose Reductase Activity in Psammomys Obesus, a Model of Type 2 Diabetes and Diabetic Retinopathy. Food Sci. Nutr. 2019;7:3979–3985. doi: 10.1002/fsn3.1259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Fang J., Bai W., Yang L. Astaxanthin Inhibits Oxidative Stress and Apoptosis in Diabetic Retinopathy. Acta Histochem. 2023;125:152069. doi: 10.1016/j.acthis.2023.152069. [DOI] [PubMed] [Google Scholar]
- 89.Janani R., Anitha R.E., Perumal M.K., Divya P., Baskaran V. Astaxanthin Mediated Regulation of VEGF through HIF1α and XBP1 Signaling Pathway: An Insight from ARPE-19 Cell and Streptozotocin Mediated Diabetic Rat Model. Exp. Eye Res. 2021;206:108555. doi: 10.1016/j.exer.2021.108555. [DOI] [PubMed] [Google Scholar]
- 90.Rani E.A., Janani R., Chonche M.J., Vallikannan B. Lactucaxanthin Regulates the Cascade of Retinal Oxidative Stress, Endoplasmic Reticulum Stress and Inflammatory Signaling in Diabetic Rats. Ocul. Immunol. Inflamm. 2023;31:320–328. doi: 10.1080/09273948.2022.2027464. [DOI] [PubMed] [Google Scholar]
- 91.Anitha R.E., Janani R., Peethambaran D., Baskaran V. Lactucaxanthin Protects Retinal Pigment Epithelium from Hyperglycemia-Regulated Hypoxia/ER Stress/VEGF Pathway Mediated Angiogenesis in ARPE-19 Cell and Rat Model. Eur. J. Pharmacol. 2021;899:174014. doi: 10.1016/j.ejphar.2021.174014. [DOI] [PubMed] [Google Scholar]
- 92.Hisamuddin A.S.-D.B., Naomi R., Manan K.A.B., Bahari H., Othman F., Embong H., Ismail A., Ahmed Q.U., Jumidil S.H., Hussain M.K., et al. The Role of Lutein-Rich Purple Sweet Potato Leaf Extract on the Amelioration of Diabetic Retinopathy in Streptozotocin-Induced Sprague-Dawley Rats. Front. Pharmacol. 2023;14:1175907. doi: 10.3389/fphar.2023.1175907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Paramaswaran Y., Subramanian A., Paramakrishnan N., Ramesh M., Muthuraman A. Therapeutic Investigation of Palm Oil Mill Effluent-Derived Beta-Carotene in Streptozotocin-Induced Diabetic Retinopathy via the Regulation of Blood–Retina Barrier Functions. Pharmaceuticals. 2023;16:647. doi: 10.3390/ph16050647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.McClinton K.J., Aliani M., Kuny S., Sauvé Y., Suh M. Differential Effect of a Carotenoid-Rich Diet on Retina Function in Non-Diabetic and Diabetic Rats. Nutr. Neurosci. 2020;23:838–848. doi: 10.1080/1028415X.2018.1563664. [DOI] [PubMed] [Google Scholar]
- 95.Zhang P.-C., Wu C.-R., Wang Z.-L., Wang L.-Y., Han Y., Sun S.-L., Li Q.-S., Ma L. Effect of Lutein Supplementation on Visual Function in Nonproliferative Diabetic Retinopathy. Asia Pac. J. Clin. Nutr. 2017;26:406–411. doi: 10.6133/apjcn.032016.13. [DOI] [PubMed] [Google Scholar]
- 96.Leh H.E., Mohd Sopian M., Abu Bakar M.H., Lee L.K. The Role of Lycopene for the Amelioration of Glycaemic Status and Peripheral Antioxidant Capacity among the Type II Diabetes Mellitus Patients: A Case–Control Study. Ann. Med. 2021;53:1060–1066. doi: 10.1080/07853890.2021.1943515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Ren Y., Qi Y., Su X., Luan H., Sun Q. Therapeutic Effect of Lutein Supplement on Non-Proliferative Diabetic Retinopathy. Medicine. 2019;98:e15404. doi: 10.1097/MD.0000000000015404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Fathalipour M., Fathalipour H., Safa O., Nowrouzi-Sohrabi P., Mirkhani H., Hassanipour S. The Therapeutic Role of Carotenoids in Diabetic Retinopathy: A Systematic Review. Diabetes Metab. Syndr. Obes. 2020;13:2347–2358. doi: 10.2147/DMSO.S255783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Lem D.W., Gierhart D.L., Davey P.G. A Systematic Review of Carotenoids in the Management of Diabetic Retinopathy. Nutrients. 2021;13:2441. doi: 10.3390/nu13072441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Pandey K.B., Rizvi S.I. Plant Polyphenols as Dietary Antioxidants in Human Health and Disease. Oxid. Med. Cell. Longev. 2009;2:270–278. doi: 10.4161/oxim.2.5.9498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.de Araújo F.F., de Paulo Farias D., Neri-Numa I.A., Pastore G.M. Polyphenols and Their Applications: An Approach in Food Chemistry and Innovation Potential. Food Chem. 2021;338:127535. doi: 10.1016/j.foodchem.2020.127535. [DOI] [PubMed] [Google Scholar]
- 102.Sharma A., Kaur M., Katnoria J.K., Nagpal A.K. Polyphenols in Food: Cancer Prevention and Apoptosis Induction. Curr. Med. Chem. 2018;25:4740–4757. doi: 10.2174/0929867324666171006144208. [DOI] [PubMed] [Google Scholar]
- 103.Patil V.M., Masand N. Chapter 12—Anticancer Potential of Flavonoids: Chemistry, Biological Activities, and Future Perspectives. In: Atta-ur-Rahman, editor. Studies in Natural Products Chemistry. Volume 59. Elsevier; Amsterdam, The Netherlands: 2018. pp. 401–430. [Google Scholar]
- 104.Li R., Ye Z., Yang W., Xu Y.-J., Tan C.-P., Liu Y. Blueberry Anthocyanins from Commercial Products: Structure Identification and Potential for Diabetic Retinopathy Amelioration. Molecules. 2022;27:7475. doi: 10.3390/molecules27217475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Xiao T., Zhi Y., Tian F., Huang F., Cheng X., Wu A., Tao L., Guo Z., Shen X. Ameliorative Effect of Black Raspberry Anthocyanins on Diabetes Retinopathy by Inhibiting Axis Protein Tyrosine Phosphatase 1B-Endoplasmic Reticulum Stress. J. Funct. Foods. 2023;107:105696. doi: 10.1016/j.jff.2023.105696. [DOI] [Google Scholar]
- 106.Li R., Ye Z., Xu Y., Liu Y. Cyanidin-3-O-Glucoside from Blueberry Anthocyanin Extracts Protects ARPE-19 Cells against High Glucose Damage via REDD1/GSK3β Pathway. Food Biosci. 2023;56:103322. doi: 10.1016/j.fbio.2023.103322. [DOI] [Google Scholar]
- 107.Anfuso C.D., Giurdanella G., Longo A., Cosentino A., Agafonova A., Rusciano D., Lupo G. Antioxidant Activity of Cyanidin-3-O-Glucoside and Verbascoside in an in Vitro Model of Diabetic Retinopathy. Front. Biosci.-Landmark. 2022;27:308. doi: 10.31083/j.fbl2711308. [DOI] [PubMed] [Google Scholar]
- 108.Zhao F., Gao X., Ge X., Cui J., Liu X. Cyanidin-3-o-Glucoside (C3G) Inhibits Vascular Leakage Regulated by Microglial Activation in Early Diabetic Retinopathy and Neovascularization in Advanced Diabetic Retinopathy. Bioengineered. 2021;12:9266–9278. doi: 10.1080/21655979.2021.1996512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Wang M., Wey S., Zhang Y., Ye R., Lee A.S. Role of the Unfolded Protein Response Regulator GRP78/BiP in Development, Cancer, and Neurological Disorders. Antioxid. Redox Signal. 2009;11:2307–2316. doi: 10.1089/ars.2009.2485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Nikbakht E., Singh I., Vider J., Williams L.T., Vugic L., Gaiz A., Kundur A.R., Colson N. Potential of Anthocyanin as an Anti-Inflammatory Agent: A Human Clinical Trial on Type 2 Diabetic, Diabetic at-Risk and Healthy Adults. Inflamm. Res. 2021;70:275–284. doi: 10.1007/s00011-021-01438-1. [DOI] [PubMed] [Google Scholar]
- 111.Anand David A.V., Arulmoli R., Parasuraman S. Overviews of Biological Importance of Quercetin: A Bioactive Flavonoid. Pharmacogn. Rev. 2016;10:84–89. doi: 10.4103/0973-7847.194044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Li R., Chen L., Yao G.-M., Yan H.-L., Wang L. Effects of Quercetin on Diabetic Retinopathy and Its Association with NLRP3 Inflammasome and Autophagy. Int. J. Ophthalmol. 2021;14:42–49. doi: 10.18240/ijo.2021.01.06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Chai G.-R., Liu S., Yang H.-W., Chen X.-L. Quercetin Protects against Diabetic Retinopathy in Rats by Inducing Heme Oxygenase-1 Expression. Neural Regen. Res. 2021;16:1344–1350. doi: 10.4103/1673-5374.301027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Hu T., Shi J.-J., Fang J., Wang Q., Chen Y.-B., Zhang S.-J. Quercetin Ameliorates Diabetic Encephalopathy through SIRT1/ER Stress Pathway in Db/Db Mice. Aging. 2020;12:7015. doi: 10.18632/aging.103059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Lupo G., Cambria M.T., Olivieri M., Rocco C., Caporarello N., Longo A., Zanghì G., Salmeri M., Foti M.C., Anfuso C.D. Anti-Angiogenic Effect of Quercetin and Its 8-Methyl Pentamethyl Ether Derivative in Human Microvascular Endothelial Cells. J. Cell. Mol. Med. 2019;23:6565–6577. doi: 10.1111/jcmm.14455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Liu Y., Gong Y., Li M., Li J. Quercetin Protects against Hyperglycemia-Induced Retinopathy in Sprague Dawley Rats by Regulating the Gut-Retina Axis and Nuclear Factor Erythroid-2–Related Factor 2 Pathway. Nutr. Res. 2024;122:55–67. doi: 10.1016/j.nutres.2023.12.003. [DOI] [PubMed] [Google Scholar]
- 117.Gupta S.K., Sharma H.P., Das U., Velpandian T., Saklani R. Effect of Rutin on Retinal VEGF, TNF-α, Aldose Reductase, and Total Antioxidant Capacity in Diabetic Rats: Molecular Mechanism and Ocular Pharmacokinetics. Int. Ophthalmol. 2020;40:159–168. doi: 10.1007/s10792-019-01165-x. [DOI] [PubMed] [Google Scholar]
- 118.Xu C., Bi M., Jin X., Zhu M., Wang G., Zhao P., Qin X., Xu X., Sun X., Ji N., et al. Long-Term Tea Consumption Is Associated with Reduced Risk of Diabetic Retinopathy: A Cross-Sectional Survey among Elderly Chinese from Rural Communities. J. Diabetes Res. 2020;2020:e1860452. doi: 10.1155/2020/1860452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Wang L., Sun X., Zhu M., Du J., Xu J., Qin X., Xu X., Song E. Epigallocatechin-3-Gallate Stimulates Autophagy and Reduces Apoptosis Levels in Retinal Müller Cells under High-Glucose Conditions. Exp. Cell Res. 2019;380:149–158. doi: 10.1016/j.yexcr.2019.04.014. [DOI] [PubMed] [Google Scholar]
- 120.Du J., Wang Y., Tu Y., Guo Y., Sun X., Xu X., Liu X., Wang L., Qin X., Zhu M., et al. A Prodrug of Epigallocatechin-3-Gallate Alleviates High Glucose-Induced pro-Angiogenic Factor Production by Inhibiting the ROS/TXNIP/NLRP3 Inflammasome Axis in Retinal Müller Cells. Exp. Eye Res. 2020;196:108065. doi: 10.1016/j.exer.2020.108065. [DOI] [PubMed] [Google Scholar]
- 121.Kim I., Seo J., Lee D.H., Kim Y.-H., Kim J.-H., Wie M.-B., Byun J.-K., Yun J.-H. Ulmus Davidiana 60% Edible Ethanolic Extract for Prevention of Pericyte Apoptosis in Diabetic Retinopathy. Front. Endocrinol. 2023;14:1138676. doi: 10.3389/fendo.2023.1138676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Xue B., Wang Y. Naringenin Upregulates GTPCH1/eNOS to Ameliorate High Glucose-Induced Retinal Endothelial Cell Injury. Exp. Ther. Med. 2022;23:428. doi: 10.3892/etm.2022.11355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Sudhakaran G., Chandran A., Sreekutty A.R., Madesh S., Pachaiappan R., Almutairi B.O., Arokiyaraj S., Kari Z.A., Tellez-Isaias G., Guru A., et al. Ophthalmic Intervention of Naringenin Decreases Vascular Endothelial Growth Factor by Counteracting Oxidative Stress and Cellular Damage in In Vivo Zebrafish. Molecules. 2023;28:5350. doi: 10.3390/molecules28145350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Xie T., Chen X., Chen W., Huang S., Peng X., Tian L., Wu X., Huang Y. Curcumin Is a Potential Adjuvant to Alleviates Diabetic Retinal Injury via Reducing Oxidative Stress and Maintaining Nrf2 Pathway Homeostasis. Front. Pharmacol. 2021;12:796565. doi: 10.3389/fphar.2021.796565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Bucolo C., Drago F., Maisto R., Romano G.L., D’Agata V., Maugeri G., Giunta S. Curcumin Prevents High Glucose Damage in Retinal Pigment Epithelial Cells through ERK1/2-Mediated Activation of the Nrf2/HO-1 Pathway. J. Cell. Physiol. 2019;234:17295–17304. doi: 10.1002/jcp.28347. [DOI] [PubMed] [Google Scholar]
- 126.Ran Z., Zhang Y., Wen X., Ma J. Curcumin Inhibits High Glucose-induced Inflammatory Injury in Human Retinal Pigment Epithelial Cells through the ROS-PI3K/AKT/mTOR Signaling Pathway. Mol. Med. Rep. 2019;19:1024–1031. doi: 10.3892/mmr.2018.9749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Chiosi F., Rinaldi M., Campagna G., Manzi G., De Angelis V., Calabrò F., D’Andrea L., Tranfa F., Costagliola C. Effect of a Fixed Combination of Curcumin, Artemisia, Bromelain, and Black Pepper Oral Administration on Optical Coherence Tomography Angiography Indices in Patients with Diabetic Macular Edema. Nutrients. 2022;14:1520. doi: 10.3390/nu14071520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Meng X., Zhou J., Zhao C.-N., Gan R.-Y., Li H.-B. Health Benefits and Molecular Mechanisms of Resveratrol: A Narrative Review. Foods. 2020;9:340. doi: 10.3390/foods9030340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Chen Y., Meng J., Li H., Wei H., Bi F., Liu S., Tang K., Guo H., Liu W. Resveratrol Exhibits an Effect on Attenuating Retina Inflammatory Condition and Damage of Diabetic Retinopathy via PON1. Exp. Eye Res. 2019;181:356–366. doi: 10.1016/j.exer.2018.11.023. [DOI] [PubMed] [Google Scholar]
- 130.Zeng K., Wang Y., Huang L., Song Y., Yu X., Deng B., Zhou X. Resveratrol Inhibits Neural Apoptosis and Regulates RAX/P-PKR Expression in Retina of Diabetic Rats. Nutr. Neurosci. 2022;25:2560–2569. doi: 10.1080/1028415X.2021.1990462. [DOI] [PubMed] [Google Scholar]
- 131.Giordo R., Nasrallah G.K., Posadino A.M., Galimi F., Capobianco G., Eid A.H., Pintus G. Resveratrol-Elicited PKC Inhibition Counteracts NOX-Mediated Endothelial to Mesenchymal Transition in Human Retinal Endothelial Cells Exposed to High Glucose. Antioxidants. 2021;10:224. doi: 10.3390/antiox10020224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Al-Hussaini H., Kittaneh R.S., Kilarkaje N. Effects of Trans-Resveratrol on Type 1 Diabetes-Induced up-Regulation of Apoptosis and Mitogen-Activated Protein Kinase Signaling in Retinal Pigment Epithelium of Dark Agouti Rats. Eur. J. Pharmacol. 2021;904:174167. doi: 10.1016/j.ejphar.2021.174167. [DOI] [PubMed] [Google Scholar]
- 133.Xiang X.-H., Wei J., Wang X.-F., Xu Q., Yu C.-L., He C.-L., Long T., Guo M.-S., Chen X., Zhou X.-G., et al. Lychee Seed Polyphenol Ameliorates DR via Inhibiting Inflammasome/Apoptosis and Angiogenesis in hRECs and Db/Db Mice. Biomed. Pharmacother. 2023;167:115478. doi: 10.1016/j.biopha.2023.115478. [DOI] [PubMed] [Google Scholar]
- 134.Liu Y., Nie X., Wang J., Zhao Z., Wang Z., Ju F. Visualizing the Distribution of Flavonoids in Litchi (Litchi chinenis) Seeds through Matrix-Assisted Laser Desorption/Ionization Mass Spectrometry Imaging. Front. Plant Sci. 2023;14:1144449. doi: 10.3389/fpls.2023.1144449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Tang Y., Xiong R., Wu A.-G., Yu C.-L., Zhao Y., Qiu W.-Q., Wang X.-L., Teng J.-F., Liu J., Chen H.-X., et al. Polyphenols Derived from Lychee Seed Suppress Aβ (1-42)-Induced Neuroinflammation. Int. J. Mol. Sci. 2018;19:2109. doi: 10.3390/ijms19072109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Luo Y., Zhao K., Li Z., Gao Y., Lin M., Li Y., Wang S., Liu Y., Chen L. Effect of the Ethyl Acetate Extract of Sophora Flavescens Aiton on Diabetic Retinopathy Based on Untargeted Retinal Metabolomics. J. Chromatogr. B Anal. Technol. Biomed. Life Sci. 2022;1198:123233. doi: 10.1016/j.jchromb.2022.123233. [DOI] [PubMed] [Google Scholar]
- 137.Kim E., Jang E., Lee J.-H. Potential Roles and Key Mechanisms of Hawthorn Extract against Various Liver Diseases. Nutrients. 2022;14:867. doi: 10.3390/nu14040867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Liu S., Fang Y., Yu J., Chang X. Hawthorn Polyphenols Reduce High Glucose-Induced Inflammation and Apoptosis in ARPE-19 Cells by Regulating miR-34a/SIRT1 to Reduce Acetylation. J. Food Biochem. 2021;45:e13623. doi: 10.1111/jfbc.13623. [DOI] [PubMed] [Google Scholar]
- 139.Schwikkard S., Whitmore H., Sishtla K., Sulaiman R.S., Shetty T., Basavarajappa H.D., Waller C., Alqahtani A., Frankemoelle L., Chapman A., et al. The Antiangiogenic Activity of Naturally Occurring and Synthetic Homoisoflavonoids from the Hyacinthaceae (Sensu APGII) J. Nat. Prod. 2019;82:1227–1239. doi: 10.1021/acs.jnatprod.8b00989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Khan S., Tosun A., Kim Y.S. Chapter 31—Ginsenosides as Food Supplements and Their Potential Role in Immunological and Neurodegenerative Disorders. In: Watson R.R., Preedy V.R., editors. Bioactive Nutraceuticals and Dietary Supplements in Neurological and Brain Disease. Academic Press; San Diego, CA, USA: 2015. pp. 303–309. [Google Scholar]
- 141.Xue L., Hu M., Li J., Li Y., Zhu Q., Zhou G., Zhang X., Zhou Y., Zhang J., Ding P. Ginsenoside Rg1 Inhibits High Glucose-Induced Proliferation, Migration, and Angiogenesis in Retinal Endothelial Cells by Regulating the lncRNA SNHG7/miR-2116-5p/SIRT3 Axis. J. Oncol. 2022;2022:6184631. doi: 10.1155/2022/6184631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Gao Y., Ji Y., Luo Y., Sun J., Sun G., Sun X. Ginsenoside Rg1 Prevents Early Diabetic Retinopathy via Reducing Retinal Ganglion Cell Layer and Inner Nuclear Layer Cell Apoptosis in Db/Db Mice. Ann. Transl. Med. 2020;8:232. doi: 10.21037/atm.2019.12.155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Xue L., Hu M., Zhu Q., Li Y., Zhou G., Zhang X., Zhou Y., Zhang J., Ding P. GRg1 Inhibits the TLR4/NF-kB Signaling Pathway by Upregulating miR-216a-5p to Reduce Growth Factors and Inflammatory Cytokines in DR. Mol. Biol. Rep. 2023;50:9379–9394. doi: 10.1007/s11033-023-08895-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Ying Y., Zhang Y.-L., Ma C.-J., Li M.-Q., Tang C.-Y., Yang Y.-F., Zeng J.-H., Huang X.-Y., Yi J., Wang X.-M., et al. Neuroprotective Effects of Ginsenoside Rg1 against Hyperphosphorylated Tau-Induced Diabetic Retinal Neurodegeneration via Activation of IRS-1/Akt/GSK3β Signaling. J. Agric. Food Chem. 2019;67:8348–8360. doi: 10.1021/acs.jafc.9b02954. [DOI] [PubMed] [Google Scholar]
- 145.Tang K., Qin W., Wei R., Jiang Y., Fan L., Wang Z., Tan N. Ginsenoside Rd Ameliorates High Glucose-Induced Retinal Endothelial Injury through AMPK-STRT1 Interdependence. Pharmacol. Res. 2022;179:106123. doi: 10.1016/j.phrs.2022.106123. [DOI] [PubMed] [Google Scholar]
- 146.Fan C., Ma Q., Xu M., Qiao Y., Zhang Y., Li P., Bi Y., Tang M. Ginsenoside Rb1 Attenuates High Glucose-Induced Oxidative Injury via the NAD-PARP-SIRT Axis in Rat Retinal Capillary Endothelial Cells. Int. J. Mol. Sci. 2019;20:4936. doi: 10.3390/ijms20194936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Dong C., Liu P., Wang H., Dong M., Li G., Li Y. Ginsenoside Rb1 Attenuates Diabetic Retinopathy in Streptozotocin-Induced Diabetic Rats1. Acta Cir. Bras. 2019;34:e201900201. doi: 10.1590/s0102-8650201900201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Xie W., Zhou P., Qu M., Dai Z., Zhang X., Zhang C., Dong X., Sun G., Sun X. Ginsenoside Re Attenuates High Glucose-Induced RF/6A Injury via Regulating PI3K/AKT Inhibited HIF-1α/VEGF Signaling Pathway. Front. Pharmacol. 2020;11:695. doi: 10.3389/fphar.2020.00695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Zhou P., Xie W., Meng X., Zhai Y., Dong X., Zhang X., Sun G., Sun X. Notoginsenoside R1 Ameliorates Diabetic Retinopathy through PINK1-Dependent Activation of Mitophagy. Cells. 2019;8:213. doi: 10.3390/cells8030213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Wang Y., Sun X., Xie Y., Du A., Chen M., Lai S., Wei X., Ji L., Wang C. Panax Notoginseng Saponins Alleviate Diabetic Retinopathy by Inhibiting Retinal Inflammation: Association with the NF-κB Signaling Pathway. J. Ethnopharmacol. 2024;319:117135. doi: 10.1016/j.jep.2023.117135. [DOI] [PubMed] [Google Scholar]
- 151.Hanaguri J., Yokota H., Kushiyama A., Kushiyama S., Watanabe M., Yamagami S., Nagaoka T. Beneficial Effect of Long-Term Administration of Supplement with Trapa Bispinosa Roxb. and Lutein on Retinal Neurovascular Coupling in Type 2 Diabetic Mice. Front. Physiol. 2022;13:788034. doi: 10.3389/fphys.2022.788034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.González-Herrero M.E.R., Ruiz M., Román F.J.L., Sánchez J.M.M., Domingo J.C. Supplementation with a Highly Concentrated Docosahexaenoic Acid plus Xanthophyll Carotenoid Multivitamin in Nonproliferative Diabetic Retinopathy: Prospective Controlled Study of Macular Function by Fundus Microperimetry. Clin. Ophthalmol. 2018;12:1011–1020. doi: 10.2147/OPTH.S157635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.McClements D.J., Li F., Xiao H. The Nutraceutical Bioavailability Classification Scheme: Classifying Nutraceuticals According to Factors Limiting Their Oral Bioavailability. Annu. Rev. Food Sci. Technol. 2015;6:299–327. doi: 10.1146/annurev-food-032814-014043. [DOI] [PubMed] [Google Scholar]
- 154.Dima C., Assadpour E., Dima S., Jafari S.M. Bioavailability of Nutraceuticals: Role of the Food Matrix, Processing Conditions, the Gastrointestinal Tract, and Nanodelivery Systems. Compr. Rev. Food Sci. Food Saf. 2020;19:954–994. doi: 10.1111/1541-4337.12547. [DOI] [PubMed] [Google Scholar]
- 155.Boonlao N., Ruktanonchai U.R., Anal A.K. Enhancing Bioaccessibility and Bioavailability of Carotenoids Using Emulsion-Based Delivery Systems. Colloids Surf. B Biointerfaces. 2022;209:112211. doi: 10.1016/j.colsurfb.2021.112211. [DOI] [PubMed] [Google Scholar]
- 156.Soukoulis C., Bohn T. A Comprehensive Overview on the Micro- and Nano-Technological Encapsulation Advances for Enhancing the Chemical Stability and Bioavailability of Carotenoids. Crit. Rev. Food Sci. Nutr. 2018;58:1–36. doi: 10.1080/10408398.2014.971353. [DOI] [PubMed] [Google Scholar]
- 157.Manach C., Williamson G., Morand C., Scalbert A., Rémésy C. Bioavailability and Bioefficacy of Polyphenols in Humans. I. Review of 97 Bioavailability Studies. Am. J. Clin. Nutr. 2005;81:230S–242S. doi: 10.1093/ajcn/81.1.230S. [DOI] [PubMed] [Google Scholar]
- 158.Di Lorenzo C., Colombo F., Biella S., Stockley C., Restani P. Polyphenols and Human Health: The Role of Bioavailability. Nutrients. 2021;13:273. doi: 10.3390/nu13010273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Sharma A.R., Lee Y.-H., Bat-Ulzii A., Bhattacharya M., Chakraborty C., Lee S.-S. Recent Advances of Metal-Based Nanoparticles in Nucleic Acid Delivery for Therapeutic Applications. J. Nanobiotechnol. 2022;20:501. doi: 10.1186/s12951-022-01650-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Ashaolu T.J. Nanoemulsions for Health, Food, and Cosmetics: A Review. Environ. Chem. Lett. 2021;19:3381. doi: 10.1007/s10311-021-01216-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Yonekura L., Nagao A. Intestinal Absorption of Dietary Carotenoids. Mol. Nutr. Food Res. 2007;51:107–115. doi: 10.1002/mnfr.200600145. [DOI] [PubMed] [Google Scholar]
- 162.Nidhi B., Ramaprasad T.R., Baskaran V. Dietary Fatty Acid Determines the Intestinal Absorption of Lutein in Lutein Deficient Mice. Food Res. Int. 2014;64:256–263. doi: 10.1016/j.foodres.2014.06.034. [DOI] [PubMed] [Google Scholar]
- 163.Toragall V., Srirangam P., Jayapala N., Baskaran V. Lutein Encapsulated Oleic—Linoleic Acid Nanoemulsion Boosts Oral Bioavailability of the Eye Protective Carotenoid Lutein in Rat Model. Mater. Today Commun. 2021;28:102522. doi: 10.1016/j.mtcomm.2021.102522. [DOI] [Google Scholar]
- 164.Lim C., Kim D., Sim T., Hoang N.H., Lee J.W., Lee E.S., Youn Y.S., Oh K.T. Preparation and Characterization of a Lutein Loading Nanoemulsion System for Ophthalmic Eye Drops. J. Drug Deliv. Sci. Technol. 2016;36:168–174. doi: 10.1016/j.jddst.2016.10.009. [DOI] [Google Scholar]
- 165.Ge Y., Zhang A., Sun R., Xu J., Yin T., He H., Gou J., Kong J., Zhang Y., Tang X. Penetratin-Modified Lutein Nanoemulsion in-Situ Gel for the Treatment of Age-Related Macular Degeneration. Expert Opin. Drug Deliv. 2020;17:603–619. doi: 10.1080/17425247.2020.1735348. [DOI] [PubMed] [Google Scholar]
- 166.Alavi M., Mozafari M.R., Hamblin M.R., Hamidi M., Hajimolaali M., Katouzian I. Industrial-Scale Methods for the Manufacture of Liposomes and Nanoliposomes: Pharmaceutical, Cosmetic, and Nutraceutical Aspects. Micro Nano Bio Asp. 2022;1:26–35. doi: 10.22034/MNBA.2022.159371. [DOI] [Google Scholar]
- 167.Khorasani S., Danaei M., Mozafari M.R. Nanoliposome Technology for the Food and Nutraceutical Industries. Trends Food Sci. Technol. 2018;79:106–115. doi: 10.1016/j.tifs.2018.07.009. [DOI] [Google Scholar]
- 168.Zarrabi A., Alipoor Amro Abadi M., Khorasani S., Mohammadabadi M.-R., Jamshidi A., Torkaman S., Taghavi E., Mozafari M.R., Rasti B. Nanoliposomes and Tocosomes as Multifunctional Nanocarriers for the Encapsulation of Nutraceutical and Dietary Molecules. Molecules. 2020;25:638. doi: 10.3390/molecules25030638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Lin M., Li L., Li L., Pokhrel G., Qi G., Rong R., Zhu T. The Protective Effect of Baicalin against Renal Ischemia-Reperfusion Injury through Inhibition of Inflammation and Apoptosis. BMC Complement. Altern. Med. 2014;14:19. doi: 10.1186/1472-6882-14-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Jo H., Jung S.H., Bin Yim H., Lee S.J., Kang K.D. The Effect of Baicalin in a Mouse Model of Retinopathy of Prematurity. BMB Rep. 2015;48:271–276. doi: 10.5483/BMBRep.2015.48.5.131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Ashraf O., Nasr M., Nebsen M., Said A.M.A., Sammour O. In Vitro Stabilization and in Vivo Improvement of Ocular Pharmacokinetics of the Multi-Therapeutic Agent Baicalin: Delineating the Most Suitable Vesicular Systems. Int. J. Pharm. 2018;539:83–94. doi: 10.1016/j.ijpharm.2018.01.041. [DOI] [PubMed] [Google Scholar]
- 172.Sun Y., Chi J., Ye X., Wang S., Liang J., Yue P., Xiao H., Gao X. Nanoliposomes as Delivery System for Anthocyanins: Physicochemical Characterization, Cellular Uptake, and Antioxidant Properties. LWT. 2021;139:110554. doi: 10.1016/j.lwt.2020.110554. [DOI] [Google Scholar]
- 173.Zhang J., Liang X., Li X., Guan Z., Liao Z., Luo Y., Luo Y. Ocular Delivery of Cyanidin-3-Glycoside in Liposomes and Its Prevention of Selenite-Induced Oxidative Stress. Drug Dev. Ind. Pharm. 2016;42:546–553. doi: 10.3109/03639045.2015.1088867. [DOI] [PubMed] [Google Scholar]
- 174.Gu H., Chen P., Liu X., Lian Y., Xi J., Li J., Song J., Li X. Trimethylated Chitosan-Coated Flexible Liposomes with Resveratrol for Topical Drug Delivery to Reduce Blue-Light-Induced Retinal Damage. Int. J. Biol. Macromol. 2023;252:126480. doi: 10.1016/j.ijbiomac.2023.126480. [DOI] [PubMed] [Google Scholar]
- 175.Tang L., Li K., Zhang Y., Li H., Li A., Xu Y., Wei B. Quercetin Liposomes Ameliorate Streptozotocin-Induced Diabetic Nephropathy in Diabetic Rats. Sci. Rep. 2020;10:2440. doi: 10.1038/s41598-020-59411-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Bulboaca A.E., Boarescu P.-M., Porfire A.S., Dogaru G., Barbalata C., Valeanu M., Munteanu C., Râjnoveanu R.M., Nicula C.A., Stanescu I.C. The Effect of Nano-Epigallocatechin-Gallate on Oxidative Stress and Matrix Metalloproteinases in Experimental Diabetes Mellitus. Antioxidants. 2020;9:172. doi: 10.3390/antiox9020172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Amato R., Rossino M.G., Cammalleri M., Locri F., Pucci L., Dal Monte M., Casini G. Lisosan G Protects the Retina from Neurovascular Damage in Experimental Diabetic Retinopathy. Nutrients. 2018;10:1932. doi: 10.3390/nu10121932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Amato R., Melecchi A., Pucci L., Canovai A., Marracci S., Cammalleri M., Dal Monte M., Caddeo C., Casini G. Liposome-Mediated Delivery Improves the Efficacy of Lisosan G against Retinopathy in Diabetic Mice. Cells. 2023;12:2448. doi: 10.3390/cells12202448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Höltke C. isoDGR-Peptides for Integrin Targeting: Is the Time Up for RGD? J. Med. Chem. 2018;61:7471–7473. doi: 10.1021/acs.jmedchem.8b01123. [DOI] [PubMed] [Google Scholar]
- 180.Li Z., Yu H., Liu C., Wang C., Zeng X., Yan J., Sun Y. Efficiency Co-Delivery of Ellagic Acid and Oxygen by a Non-Invasive Liposome for Ameliorating Diabetic Retinopathy. Int. J. Pharm. 2023;641:122987. doi: 10.1016/j.ijpharm.2023.122987. [DOI] [PubMed] [Google Scholar]
- 181.Date A.A., Desai N., Dixit R., Nagarsenker M. Self-Nanoemulsifying Drug Delivery Systems: Formulation Insights, Applications and Advances. Nanomed. 2010;5:1595–1616. doi: 10.2217/nnm.10.126. [DOI] [PubMed] [Google Scholar]
- 182.Zingale E., Bonaccorso A., D’Amico A.G., Lombardo R., D’Agata V., Rautio J., Pignatello R. Formulating Resveratrol and Melatonin Self-Nanoemulsifying Drug Delivery Systems (SNEDDS) for Ocular Administration Using Design of Experiments. Pharmaceutics. 2024;16:125. doi: 10.3390/pharmaceutics16010125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Wang S., Du S., Wang W., Zhang F. Therapeutic Investigation of Quercetin Nanomedicine in a Zebrafish Model of Diabetic Retinopathy. Biomed. Pharmacother. 2020;130:110573. doi: 10.1016/j.biopha.2020.110573. [DOI] [PubMed] [Google Scholar]
- 184.Rishitha N., Muthuraman A. Therapeutic Evaluation of Solid Lipid Nanoparticle of Quercetin in Pentylenetetrazole Induced Cognitive Impairment of Zebrafish. Life Sci. 2018;199:80–87. doi: 10.1016/j.lfs.2018.03.010. [DOI] [PubMed] [Google Scholar]
- 185.Toragall V., Baskaran V. Chitosan-Sodium Alginate-Fatty Acid Nanocarrier System: Lutein Bioavailability, Absorption Pharmacokinetics in Diabetic Rat and Protection of Retinal Cells against H2O2 Induced Oxidative Stress In Vitro. Carbohydr. Polym. 2021;254:117409. doi: 10.1016/j.carbpol.2020.117409. [DOI] [PubMed] [Google Scholar]
- 186.Toragall V., Muzaffar J.C., Baskaran V. Lutein Loaded Double-Layered Polymer Nanocarrier Modulate H2O2 and CoCl2 Induced Oxidative and Hypoxia Damage and Angiogenic Markers in ARPE-19 Cells. Int. J. Biol. Macromol. 2023;240:124378. doi: 10.1016/j.ijbiomac.2023.124378. [DOI] [PubMed] [Google Scholar]
- 187.Ruginǎ D., Ghiman R., Focșan M., Tăbăran F., Copaciu F., Suciu M., Pintea A., Aștilean S. Resveratrol-Delivery Vehicle with Anti-VEGF Activity Carried to Human Retinal Pigmented Epithelial Cells Exposed to High-Glucose Induced Conditions. Colloids Surf. B Biointerfaces. 2019;181:66–75. doi: 10.1016/j.colsurfb.2019.04.022. [DOI] [PubMed] [Google Scholar]
- 188.Ganugula R., Arora M., Dwivedi S., Chandrashekar D.S., Varambally S., Scott E.M., Kumar M.N.V.R. Systemic Anti-Inflammatory Therapy Aided by Curcumin-Laden Double-Headed Nanoparticles Combined with Injectable Long-Acting Insulin in a Rodent Model of Diabetes Eye Disease. ACS Nano. 2023;17:6857–6874. doi: 10.1021/acsnano.3c00535. [DOI] [PubMed] [Google Scholar]
- 189.Mody V.V., Siwale R., Singh A., Mody H.R. Introduction to Metallic Nanoparticles. J. Pharm. Bioallied Sci. 2010;2:282. doi: 10.4103/0975-7406.72127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Marella S., Hema K., Shameer S., Prasad T.N.V.K.V. Nano-Ellagic Acid: Inhibitory Actions on Aldose Reductase and α-Glucosidase in Secondary Complications of Diabetes, Strengthened by in Silico Docking Studies. 3 Biotech. 2020;10:439. doi: 10.1007/s13205-020-02411-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Gui S., Tang W., Huang Z., Wang X., Gui S., Gao X., Xiao D., Tao L., Jiang Z., Wang X. Ultrasmall Coordination Polymer Nanodots Fe-Quer Nanozymes for Preventing and Delaying the Development and Progression of Diabetic Retinopathy. Adv. Funct. Mater. 2023;33:2300261. doi: 10.1002/adfm.202300261. [DOI] [Google Scholar]
- 192.Giljohann D.A., Seferos D.S., Daniel W.L., Massich M.D., Patel P.C., Mirkin C.A. Gold Nanoparticles for Biology and Medicine. Angew. Chem. Int. Ed. 2010;49:3280–3294. doi: 10.1002/anie.200904359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Moldovan M., Păpurică A.-M., Muntean M., Bungărdean R.M., Gheban D., Moldovan B., Katona G., David L., Filip G.A. Effects of Gold Nanoparticles Phytoreduced with Rutin in an Early Rat Model of Diabetic Retinopathy and Cataracts. Metabolites. 2023;13:955. doi: 10.3390/metabo13080955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Stoia D., Pop R., Campu A., Nistor M., Astilean S., Pintea A., Suciu M., Rugina D., Focsan M. Hybrid Polymeric Therapeutic Microcarriers for Thermoplasmonic-Triggered Release of Resveratrol. Colloids Surf. B Biointerfaces. 2022;220:112915. doi: 10.1016/j.colsurfb.2022.112915. [DOI] [PubMed] [Google Scholar]
- 195.Küünal S., Rauwel P., Rauwel E. Chapter 14—Plant Extract Mediated Synthesis of Nanoparticles. In: Barhoum A., Makhlouf A.S.H., editors. Emerging Applications of Nanoparticles and Architecture Nanostructures. Elsevier; Amsterdam, The Netherlands: 2018. pp. 411–446. Micro and Nano Technologies. [Google Scholar]
- 196.Dong Y., Wan G., Yan P., Qian C., Li F., Peng G. Fabrication of Resveratrol Coated Gold Nanoparticles and Investigation of Their Effect on Diabetic Retinopathy in Streptozotocin Induced Diabetic Rats. J. Photochem. Photobiol. B. 2019;195:51–57. doi: 10.1016/j.jphotobiol.2019.04.012. [DOI] [PubMed] [Google Scholar]