Acute and chronic management strategies in heart failure are aimed at improving both symptoms and prognosis, although management in individual patients will depend on the underlying aetiology and the severity of the condition. It is imperative that the diagnosis of heart failure is accompanied by an urgent attempt to establish its cause, as timely intervention may greatly improve the prognosis in selected cases—for example, in patients with severe aortic stenosis.
Survival rates (%) compared with chronic heart failure
| At 1 year | At 2 years | At 3 years | |
|---|---|---|---|
| Breast cancer | 88 | 80 | 72 |
| Prostate cancer | 75 | 64 | 55 |
| Colon cancer | 56 | 48 | 42 |
| Heart failure | 67 | 41 | 24 |
Management of acute heart failure
Assessment
Common presenting features include anxiety, tachycardia, and dyspnoea. Pallor and hypotension are present in more severe cases: the triad of hypotension (systolic blood pressure <90 mm Hg), oliguria, and low cardiac output constitutes a diagnosis of cardiogenic shock. Severe acute heart failure and cardiogenic shock may be related to an extensive myocardial infarction, sustained cardiac arrhythmias (for example, atrial fibrillation or ventricular tachycardia), or mechanical problems (for example, acute papillary muscle rupture or postinfarction ventricular septal defect).
Killip classification
| Class | Clinical features | Hospital mortality (%) |
|---|---|---|
| Class I | No signs of left ventricular dysfunction | 6 |
| Class II | S3 gallop with or without mild to moderate pulmonary congestion | 30 |
| Class III | Acute severe pulmonary oedema | 40 |
| Class IV | Shock syndrome | 80-90 |
Severe acute heart failure is a medical emergency, and effective management requires an assessment of the underlying cause, improvement of the haemodynamic status, relief of pulmonary congestion, and improved tissue oxygenation. Clinical and radiographic assessment of these patients provides a guide to severity and prognosis: the Killip classification has been developed to grade the severity of acute and chronic heart failure.
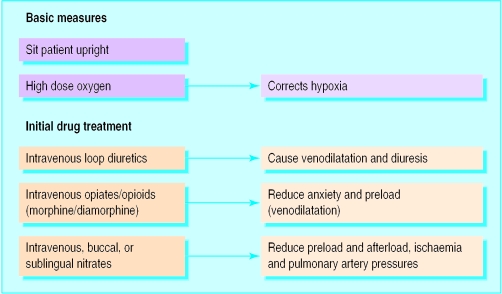
Treatment
Basic measures should include sitting the patient in an upright position with high concentration oxygen delivered via a face mask. Close observation and frequent reassessment are required in the early hours of treatment, and patients with acute severe heart failure, or refractory symptoms, should be monitored in a high dependency unit. Urinary catheterisation facilitates accurate assessment of fluid balance, while arterial blood gases provide valuable information about oxygenation and acid-base balance. The “base excess” is a guide to actual tissue perfusion in patients with acute heart failure: a worsening (more negative) base excess generally indicates lactic acidosis, which is related to anaerobic metabolism, and is a poor prognostic feature. Correction of hypoperfusion will correct the metabolic acidosis; bicarbonate infusions should be reserved for only the most refractory cases.
Intravenous loop diuretics, such as frusemide (furosemide), induce transient venodilatation, when administered to patients with pulmonary oedema, and this may lead to symptomatic improvement even before the onset of diuresis. Loop diuretics also increase the renal production of vasodilator prostaglandins. This additional benefit is antagonised by the administration of prostaglandin inhibitors, such as non-steroidal anti-inflammatory drugs, and these agents should be avoided where possible. Parenteral opiates or opioids (morphine or diamorphine) are an important adjunct in the management of severe acute heart failure, by relieving anxiety, pain, and distress and reducing myocardial oxygen demand. Intravenous opiates and opioids also produce transient venodilatation, thus reducing preload, cardiac filling pressures, and pulmonary congestion.
Nitrates (sublingual, buccal, and intravenous) may also reduce preload and cardiac filling pressures and are particularly valuable in patients with both angina and heart failure. Sodium nitroprusside is a potent, directly acting vasodilator, which is normally reserved for refractory cases of acute heart failure.
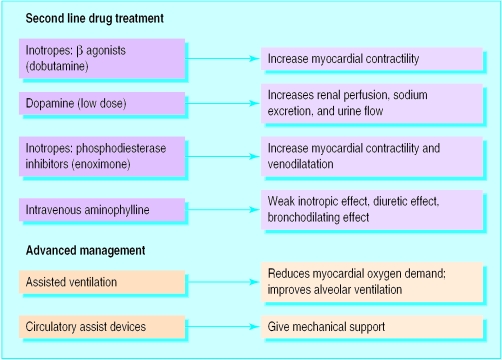
Short term inotropic support
In cases of severe refractory heart failure in which the cardiac output remains critically low, the circulation can be supported for a critical period of time with inotropic agents. For example, dobutamine and dopamine have positive inotropic actions, acting on the β1 receptors in cardiac muscle. Phosphodiesterase inhibitors (for example, enoximone) are less commonly used, and long term use of these agents is associated with increased mortality. Intravenous aminophylline is now rarely used for treating acute heart failure. Inotropic agents in general increase the potential for cardiac arrhythmias.
Intravenous inotropes and circulatory assist devices
Short term support with intravenous inotropes or circulatory assist devices, or with both, may temporarily improve haemodynamic status and peripheral perfusion
Such support can act as a bridge to corrective valve surgery or cardiac transplantation in acute and chronic heart failure
Chronic heart failure
Chronic heart failure can be “compensated” or “decompensated.” In compensated heart failure, symptoms are stable, and many overt features of fluid retention and pulmonary oedema are absent. Decompensated heart failure refers to a deterioration, which may present either as an acute episode of pulmonary oedema or as lethargy and malaise, a reduction in exercise tolerance, and increasing breathlessness on exertion. The cause or causes of decompensation should be considered and identified; they may include recurrent ischaemia, arrhythmias, infections, and electrolyte disturbance. Atrial fibrillation is common, and poor control of ventricular rate during exercise despite adequate control at rest should be addressed.
Management of chronic heart failure
General advice
Counselling—about symptoms and compliance
Social activity and employment
Vaccination (influenza, pneumococcal)
Contraception
General measures
Diet (for example, reduce salt and fluid intake)
Stop smoking
Reduce alcohol intake
Take exercise
Treatment options—pharmacological
Diuretics (loop and thiazide)
Angiotensin converting enzyme inhibitors
β Blockers
Digoxin
Spironolactone
Vasodilators (hydralazine/nitrates)
Anticoagulation
Antiarrhythmic agents
Positive inotropic agents
Treatment options—devices and surgery
Revascularisation (percutaneous transluminal coronary angioplasty and coronary artery bypass graft)
Valve replacement (or repair)
Pacemaker or implantable cardiodefibrillator
Ventricular assist devices
Heart transplantation
Common features of chronic heart failure include breathlessness and reduced exercise tolerance, and management is directed at relieving these symptoms and improving quality of life. Secondary but important objectives are to improve prognosis and reduce hospital admissions.
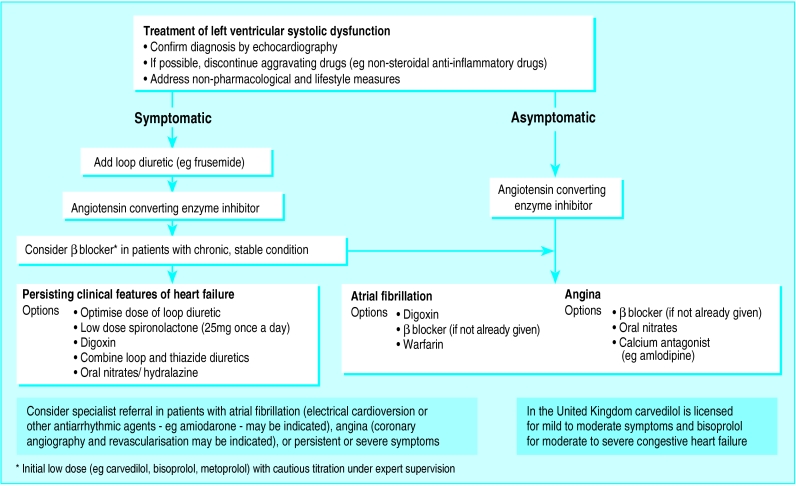
Initial management
Non-pharmacological and lifestyle measures should be addressed. Loop diuretics are valuable if there is evidence of fluid overload, although these may be reduced once salt and water retention has been treated. Angiotensin converting enzyme inhibitors should be introduced at an early stage, in the absence of clear contraindications. Angiotensin II receptor antagonists are an appropriate alternative in patients who are intolerant to angiotensin converting enzyme inhibitors. β Blockers (carvedilol, bisoprolol, metoprolol) are increasingly used in stable patients, although these agents require low dose initiation and cautious titration under specialist supervision. Oral digoxin has a role in patients with left ventricular systolic impairment, in sinus rhythm, who remain symptomatic despite optimal doses of diuretics and angiotensin converting enzyme inhibitors. Warfarin should be considered in patients with atrial fibrillation.
Supervised exercise programmes are of proved benefit, and regular exercise should be encouraged in patients with chronic stable heart failure
Severe congestive heart failure
Despite conventional treatment with diuretics and angiotensin converting enzyme inhibitors, hospital admission may be necessary in severe congestive heart failure. Fluid restriction is important—fluid intake should be reduced to 1-1.5 litres/24 h, and dietary salt restriction may be helpful.
Weighing the patient daily is valuable in monitoring the response to treatment
Education, counselling, and support
A role is emerging for heart failure liaison nurses in educating and supporting patients and their families, promoting long term compliance, and supervising treatment changes in the community
Depression is common, underdiagnosed, and often undertreated; counselling is therefore important for patients and families, and the newer antidepressants (particularly the selective serotonin reuptake inhibitors) seem to be well tolerated and are useful in selected patients
Short term bed rest is valuable until signs and symptoms improve: rest reduces the metabolic demand and increases renal perfusion, thus improving diuresis. Although bed rest potentiates the action of diuretics, it increases the risk of venous thromboembolism, and prophylactic subcutaneous heparin should be considered in immobile inpatients. Full anticoagulation is not advocated routinely unless concurrent atrial fibrillation is present, although it may be considered in patients with very severe impairment of left ventricular systolic function, associated with significant ventricular dilatation. Intravenous loop diuretics may be administered to overcome the short term problem of gut oedema and reduced absorption of tablets, and these may be used in conjunction with an oral thiazide or thiazide-like diuretic (metolazone). Low dose spironolactone (25 mg) improves morbidity and mortality in severe (New York Heart Association class IV) heart failure, when combined with conventional treatment (loop diuretics and angiotensin converting enzyme inhibitors). Potassium concentrations should be closely monitored after the addition of spironolactone.
Special procedures
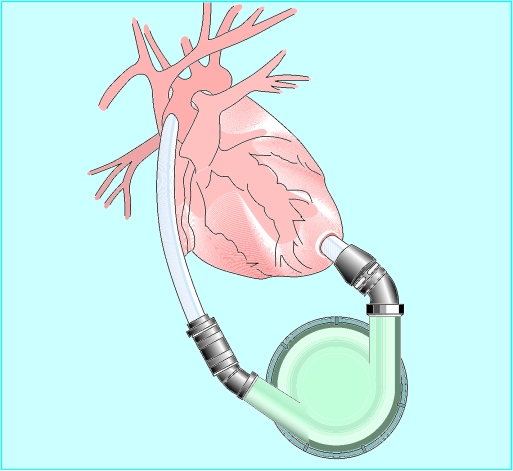
Intra-aortic balloon pumping and mechanical devices
Intra-aortic balloon counterpulsation and left ventricular assist devices are used as bridges to corrective valve surgery, cardiac transplantation, or coronary artery bypass surgery in the presence of poor cardiac function. Mechanical devices are indicated if (a) there is a possibility of spontaneous recovery (for example, peripartum cardiomyopathy, myocarditis) or (b) as a bridge to cardiac surgery (for example, ruptured mitral papillary muscle, postinfarction ventricular septal defect) or transplantation. Intra-aortic balloon counterpulsation is the most commonly used form of mechanical support.
Revascularisation and other operative strategies
Impaired ventricular function in itself is not an absolute contraindication to cardiac surgery, although the operative risks are increased. Ischaemic heart disease is the most common precursor of chronic heart failure in Britain: coronary ischaemia should be identified and revascularisation considered with coronary artery bypass surgery or occasionally percutaneous coronary angioplasty. The concept of “hibernating” myocardium is increasingly recognised, although the most optimal and practical methods of identifying hibernation remain open to debate. Revascularisation of hibernating myocardium may lead to an improvement in the overall left ventricular function.
Indications and contraindications to cardiac transplantation in adults
Indications
End stage heart failure—for example, ischaemic heart disease and dilated cardiomyopathy
Rarely, restrictive cardiomyopathy and peripartum cardiomyopathy
Congenital heart disease (often combined heart-lung transplantation required)
Absolute contraindications
Recent malignancy (other than basal cell and squamous cell carcinoma of the skin)
Active infection (including HIV, Hepatitis B, Hepatitis C with liver disease)
Systemic disease which is likely to affect life expectancy
Significant pulmonary vascular resistance
Relative contraindications
Recent pulmonary embolism
Symptomatic peripheral vascular disease
Obesity
Severe renal impairment
Psychosocial problems—for example, lack of social support, poor compliance, psychiatric illness
Age (over 60-65 years)
Correction of valve disease, most commonly in severe aortic stenosis or mitral incompetence (not secondary to left ventricular dilatation), relieves a mechanical cause of heart failure; closure of an acute ventricular septal defect or mitral valve surgery for acute mitral regurgitation, complicating a myocardial infarction, may be lifesaving. Surgical excision of a left ventricular aneurysm (aneurysectomy) is appropriate in selected cases. Novel surgical procedures such as extensive ventricular reduction (Batista operation) and cardiomyoplasty have been associated with successful outcome in a small number of patients, although the high mortality, and the limited evidence of substantial benefit, has restricted the widespread use of these procedures.
Cardiac transplantation
The outcome in cardiac transplantation is now good, with long term improvements in survival and quality of life in patients with severe heart failure. However, although the demand for cardiac transplantation has increased over recent years, the number of transplant operations has remained stable, owing primarily to limited availability of donor organs.
Key references
Dargie HJ, McMurray JJ. Diagnosis and management of heart failure. BMJ 1994;308:321-8.
ACC/AHA Task Force Report. Guidelines for the evaluation and management of heart failure. J Am Coll Cardiol 1995;26:1376-98.
Hunt SA. Current status of cardiac transplantation. JAMA 1998;280:1692-8.
Remme WJ. The treatment of heart failure. The Task Force of the Working Group on Heart Failure of the European Society of Cardiology. Eur Heart J 1997;18:736-53.
The procedure now carries a perioperative mortality of less than 10%, with approximate one, five, and 10 year survival rates of 92%, 75%, and 60% respectively (much better outcomes than with optimal drug treatment, which is associated with a one year mortality of 30-50% in advanced heart failure). Cardiac transplantation should be considered in patients with an estimated one year survival of <50%. Well selected patients over 55-60 years have a survival rate comparable to those of younger patients. Patients need strong social and psychological support; transplant liaison nurses are valuable in this role.
The long term survival of the transplanted human heart is compromised by accelerated graft atherosclerosis which results in small vessel coronary artery disease and an associated deterioration in left ventricular performance. This can occur as early as three months and is the major cause of graft loss after the first year. The anti-rejection regimens currently used may result in an acceleration of pre-existing atherosclerotic vascular disease—hence the exclusion of patients who already have significant peripheral vascular disease. Rejection is now a less serious problem, with the use of cyclosporin and other immunosuppressant agents.
Nevertheless, the supply of donors limits the procedure. The Eurotransplant database (1990-5) indicates that 25% of patients listed for transplantation die on the waiting list, with 60% receiving transplants at two years (most within 12 months). Although ventricular assist devices may be valuable during the wait for transplantation, the routine use of xenotransplants is unlikely in the short or medium term.
Figure.
Chest x ray film in patient with acute pulmonary oedema
Figure.
Acute heart failure: basic measures and initial drug treatment
Figure.
Acute heart failure: second line drug treatment and advanced management
Figure.
Example of management algorithm for left ventricular dysfunction
Figure.
Left ventricular assist device
Figure.
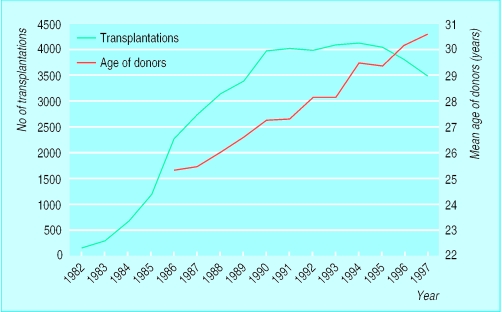
Number of heart transplantations worldwide and mean age of donors
Acknowledgments
The graph showing cardiac transplantations worldwide is adapted with permission from Hosenpud et al (J Heart Lung Transplant 1998;17:656-8). The table showing survival rates is adapted from Hobbs (Heart 1999;82(suppl IV):IV8-10).
Footnotes
T Millane is consultant cardiologist in the department of cardiology, City Hospital, Birmingham; G Jackson is consultant cardiologist in the department of cardiology at Guy's and St Thomas's Hospital, London.
The ABC of heart failure is edited by C R Gibbs, M K Davies, and G Y H Lip. CRG is research fellow and GYHL is consultant cardiologist and reader in medicine in the university department of medicine and the department of cardiology, City Hospital, Birmingham; MKD is consultant cardiologist in the department of cardiology, Selly Oak Hospital, Birmingham. The series will be published as a book in the spring.