Abstract
The discovery that subanesthetic doses of (R,S)-ketamine (ketamine) and (S)-ketamine (esketamine) rapidly induce antidepressant effects and promote sustained actions following drug clearance in depressed patients who are treatment-resistant to other therapies has resulted in a paradigm shift in the conceptualization of how rapidly and effectively depression can be treated. Consequently, the mechanism(s) that next generation antidepressants may engage to improve pathophysiology and resultant symptomology are being reconceptualized. Impaired excitatory glutamatergic synapses in mood-regulating circuits are likely a substantial contributor to the pathophysiology of depression. Metaplasticity is the process of regulating future capacity for plasticity by priming neurons with a stimulation that alters later neuronal plasticity responses. Accordingly, the development of treatment modalities that specifically modulate the duration, direction, or magnitude of glutamatergic synaptic plasticity events such as long-term potentiation (LTP), defined here as metaplastogens, may be an effective approach to reverse the pathophysiology underlying depression and improve depression symptoms. We review evidence that the initiating mechanisms of pharmacologically diverse rapid-acting antidepressants (i.e., ketamine mimetics) converge on consistent downstream molecular mediators that facilitate the expression/maintenance of increased synaptic strength and resultant persisting antidepressant effects. Specifically, while the initiating mechanisms of these therapies may differ (e.g., cell type-specificity, N-methyl-D-aspartate (NMDA) receptor subtype-selective inhibition vs activation, metabotropic glutamate receptor 2/3 antagonism, AMPA receptor potentiation, 5-HT receptor-activating psychedelics, etc.), the sustained therapeutic mechanisms of putative rapid-acting antidepressants will be mediated, in part, by metaplastic effects that converge on consistent molecular mediators to enhance excitatory neurotransmission and altered capacity for synaptic plasticity. We conclude that the convergence of these therapeutic mechanisms provides the opportunity for metaplasticity processes to be harnessed as a druggable plasticity mechanism by next-generation therapeutics. Further, targeting metaplastic mechanisms presents therapeutic advantages including decreased dosing frequency and associated diminished adverse responses by eliminating the requirement for the drug to be continuously present.
Major depressive disorder (MDD) is a leading disability in the world, affecting more than 280 million people globally [1] and costing the United States economy hundreds of billions of USD annually [2]. Antidepressant drug discovery from the middle 20th century until the past decade has mostly centered on the premise of ameliorating MDD-specific impairments in monoaminergic signaling (e.g., serotonin, norepinephrine, dopamine, etc.) in the central nervous system, leading to the development of drugs such as selective monoamine reuptake inhibitors [3, 4]. Major drawbacks of these drugs are their requirement to be administered daily, a delayed onset of therapeutic benefit, and a modest response/remission rate [5-8], resulting in sustained suffering and a higher risk of unwanted outcomes, such as suicide, in depressed individuals. Many patients who do respond to typical monoaminergic therapies also discontinue their use due to side effects or adverse drug responses [9].
The emergence of rapid-acting antidepressants that may act on glutamatergic neurotransmission such as (R,S)-ketamine (ketamine) and (S)-ketamine (esketamine) has yielded a paradigm shift in the approach to depression research and treatment, which increasingly focuses on modulating glutamatergic transmission to ameliorate impaired synaptic plasticity [10-12]. Following administration of a sub-anesthetic dose, ketamine induces rapid clinical antidepressant actions coincident with drug exposure [13-17]. This discovery facilitated the development of a nasal spray containing the stereoisomer esketamine (Spravato ®) for treatment-resistant depression [18, 19]. While the effects of ketamine and esketamine are sustained after clearance of the parent drug or its biologically active metabolites, typically the effects are more sustained following repeated administration [16, 20-22]. These findings have led to many assessments of potential ketamine mimetics acting as NMDAR antagonists [23-34] in anticipation that they will maintain the rapid and sustained antidepressant efficacy of ketamine [35]. However, ketamine and its (S)-ketamine stereoisomer present potential clinical challenges including N-methyl-D-aspartate receptor (NMDAR) inhibition-dependent dissociative/psychomimetic effects that occur even at subanesthetic, antidepressant doses [36, 37] and misuse liability that restricts the administration of these therapeutics to medically supervised settings [38-40].
Furthermore, many clinical studies have revealed that NMDAR antagonists do not induce robust, rapid, and/or sustained antidepressant effects [23-34] compared to what has been observed with ketamine [10, 12, 41, 42]. This leads to the conclusion that NMDAR antagonism is not solely responsible for the antidepressant effects of ketamine [43]. As a consequence, novel rapid-acting antidepressant drug development is increasingly looking beyond drug mechanisms that rely upon NMDAR inhibition [35, 44]. This shift is supported by preclinical studies that have found antidepressant effects of several bioactive, stereoisomer ketamine metabolites, which may contribute to the therapeutic effects of ketamine. This includes the norketamines and the hydroxynorketamines (HNKs), and in particular, the major HNK metabolite found in humans and rodents following administration of a subanesthetic dose of ketamine, (2S,6S;2R,6R)-HNK [45]. HNK’s antidepressant-relevant mechanism is independent of NMDAR inhibition [46, 47].
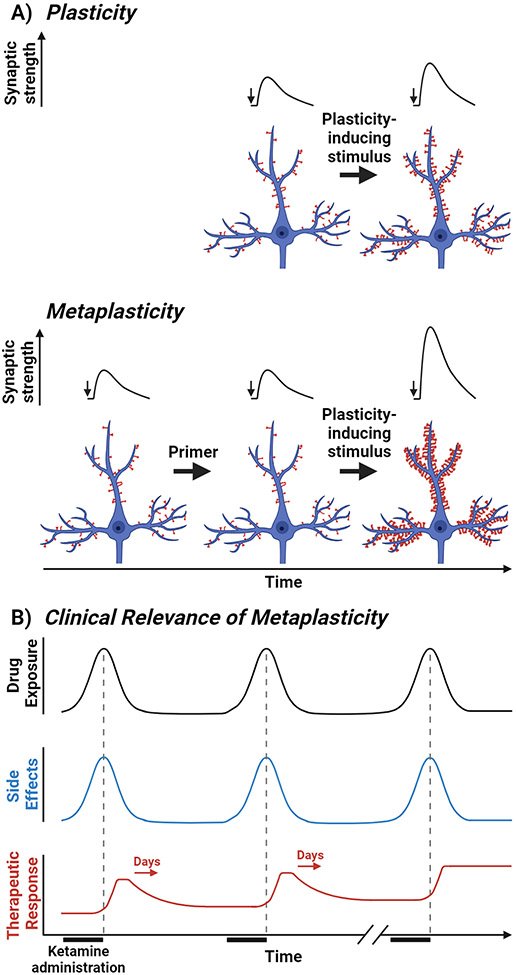
The present moment is an exciting, controversial period in the conceptualization of rapid-acting antidepressant mechanisms. Numerous pharmacologically diverse, putative ketamine mimetics (e.g., NMDAR positive allosteric modulator (PAMs), metabotropic glutamate receptor 2/3 antagonists, α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid receptors (AMPAR) PAMS, serotonergic psychedelics) are being assessed for antidepressant efficacy in clinical trials [35, 48-50]. The distinct pharmacological initiating mechanisms of these proposed therapeutics suggest that each classification engages divergent signaling cascades to facilitate sustained antidepressant effects. However, we argue that the antidepressant-relevant induction mechanism of each class of putative ketamine mimetics leads to sustained antidepressant effects via persistently (after the drug has been eliminated) modifying the threshold for the induction of synaptic plasticity through a process known as metaplasticity. In contrast to directly changing synaptic efficacy via induction of synaptic plasticity, a metaplastic stimulation acts as a primer, shifting the threshold for altering synaptic efficacy by a successive stimulus (Figure 1A). Notably, studies that we will review (vide infra) have found that ketamine, putative ketamine mimetics, and noninvasive neuromodulatory stimulation activate metaplastic mechanisms, which may prepare neural circuitry for correction upon subsequent stimuli including additional pharmacotherapy, psychotherapy, or neuromodulation treatment (Figure 1B). Thus, viewing metaplasticity as a convergent druggable mechanism across pharmacologically diverse, putative ketamine mimetics indicates a consolidatory mechanism. Importantly, such a unified viewpoint may facilitate the discovery of novel therapeutics, i.e., metaplastogens, to engage shared molecular mediators downstream of antidepressant-activated metaplastic mechanism(s) that may be targeted by next-generation therapeutics (Figure 1B).
Figure 1. Translatable metaplasticity concepts.
(A) Distinctions between plasticity and metaplasticity. (Top) Standard synaptic plasticity induction results in a quantitatively greater excitatory postsynaptic potential (EPSP) in response to the same stimulus (small arrow) after plasticity induction. This alteration in synaptic efficacy results in enhanced excitatory synaptic transmission and structural plasticity as illustrated in the pyramidal cell. (Bottom) In contrast, metaplasticity involves a priming stimulus persistently altering the threshold for a change in synaptic efficacy without changing basal synaptic transmission or neuronal morphology. An example is shown where the priming stimulus lowers the threshold for synaptic potentiation, leading to the same plasticity induction event eliciting a quantitatively greater evoked EPSP response and augmented structural plasticity compared to the response elicited without the priming stimulus. (B) Clinical relevance and advantages of targeting metaplastic mechanisms to promote sustained antidepressant effects. Following intravenous administration, ketamine is rapidly eliminated and side effects generally follow these pharmacokinetics. Acute antidepressant effects are typically observed after exposure and can extend for hours or days. Repeated ketamine administration elicits significantly greater antidepressant effects, and these effects typically persist longer than after a single administration [16, 20-22]. A single administration of ketamine leading to an enhanced antidepressant effect in response to the same treatment days later is consistent with the concept of metaplasticity where the first treatment lowers the threshold for persistent alterations in synaptic efficacy and neural morphology. Targeting metaplastic mechanism(s) to yield persistent antidepressant effects presents therapeutic benefits that may enhance patient compliance such as reduced dosing frequency and, thus, adverse responses because the necessity for the drug to be continuously present is eliminated. Created with Biorender.com
SYNAPTIC MECHANISMS OF PLASTICITY
Short-term and long-term synaptic plasticity
The capacity for synapses to detect alterations in activity, integrate/store information, and when appropriate, adapt to novel stimulation via synaptic plasticity shapes behavioral responses and, therefore, is one of the most essential tasks of the nervous system. Hebbian plasticity illustrates this where the repetitive and contextual characteristics of an experience are associated with the pairing of repeated, persistent presynaptic stimuli with postsynaptic events such as membrane potential depolarization, leading to modulation of synaptic efficacy [51] and experience-dependent learning [52, 53]. Many variations of short-term [54] and long-term [55] synaptic plasticity have been reported. Importantly for this review, these plasticity mechanisms have been known to be 1) primed by activation of metaplastic mechanisms [56] and 2) engaged by rapid-acting antidepressants [10]. Thus, we will briefly review some forms of short-term and long-term synaptic plasticity here with a particular emphasis on NMDAR activation-dependent long-term plasticity.
Numerous forms of short-term plasticity such as synaptic facilitation and depression have been characterized [54]. An intense investigation of long-term alterations in synaptic plasticity began after the discovery that synaptic potentiation persisted for hours after the application of brief, high-frequency stimuli to the dentate gyrus of anesthetized rabbits [57, 58]. The NMDAR is a well-established mediator of activity-dependent changes in neuroplasticity and is an ionotropic, ligand- and voltage-gated receptor [59-61], and has been considered a molecular detector of Hebbian plasticity. This is due to two requirements of NMDAR activity: i) availability of glutamate, which binds to the GluN2 subunit, and ii) membrane depolarization resulting in the release of a voltage-dependent Mg2+ block that enables Ca2+ influx [62]. The most well-studied forms of persisting, NMDAR-dependent alterations in synaptic transmission are long-term potentiation (LTP) and long-term depression (LTD), particularly due to findings suggesting these endpoints are synaptic substrates of learning and memory [63].
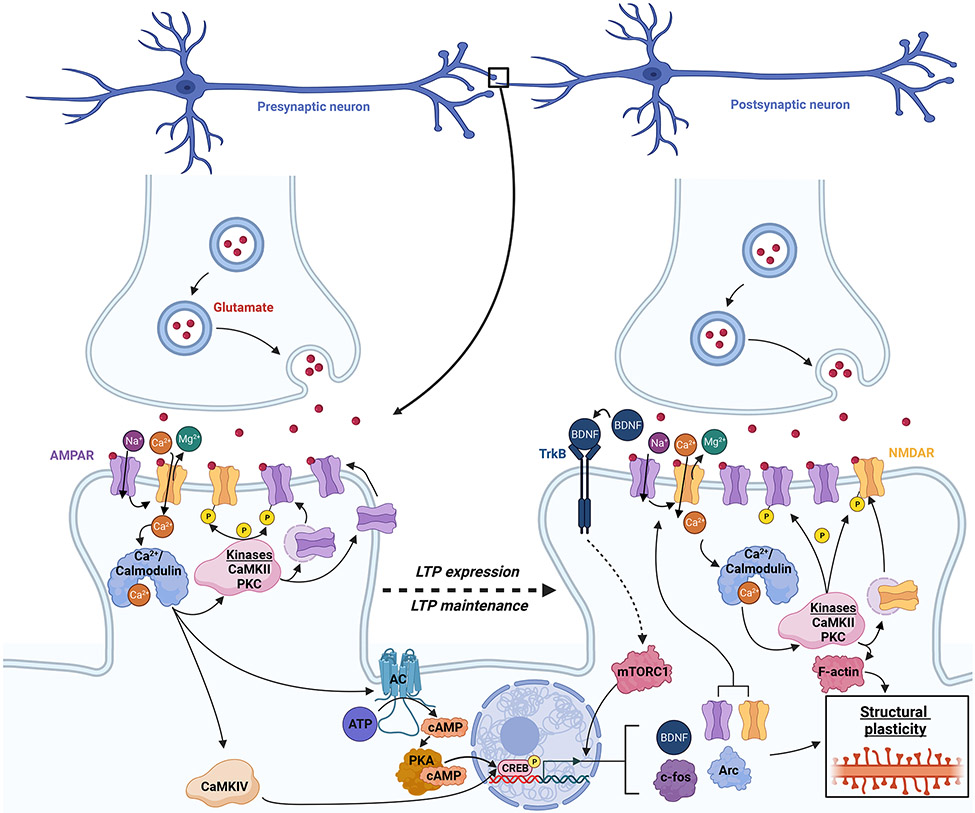
The persistent synaptic alterations inherent to NMDAR-dependent LTP/LTD has been described to involve three critical phases: induction, expression, and maintenance (Figure 2) [55]. Electrophysiology studies generally initiate LTP induction via high-frequency, patterned stimuli (e.g., individual or repeated 1 s train(s) of 100 Hz), leading to exocytosis of vesicular glutamate from presynaptic terminals. Persistent postsynaptic cell depolarization after glutamate binds to AMPARs allows for a sufficiently large NMDAR-mediated influx of Ca2+ to promote an interaction of this divalent cation with calmodulin, producing the Ca2+/calmodulin complex. The Ca2+/calmodulin complex subsequently mobilizes and activates kinases localized to dendritic spines, such as cAMP-dependent protein kinase A (PKA), protein kinase C (PKC), and Ca2+/calmodulin-dependent protein kinase II (CaMKII) [64].
Figure 2. Molecular mechanisms of NMDAR activation-dependent LTP.
Canonical NMDAR activation-dependent LTP induction is initiated by simultaneous AMPAR-mediated postsynaptic depolarization and glutamate binding to the NMDAR, facilitating NMDAR activation and Ca2+ influx after the release of an NMDAR Mg2+ block. LTP expression is instigated by Ca2+/calmodulin-dependent signaling that enables postsynaptic kinase activity (e.g., CaMKII, PKC) to promote enhanced synaptic transmission via numerous alterations including phosphorylation of glutamatergic receptors, trafficking of AMPARs to the postsynaptic membrane, and lateral diffusion of extrasynaptic AMPARs. Initiation of gene transcription is mediated by numerous signaling cascades (e.g., adenylyl cyclase-cAMP-PKA) and protein kinases (e.g., CaMKIV). LTP maintenance requires de novo protein synthesis either in the soma (e.g., CREB-dependent gene transcription and subsequent translation of proteins such as c-fos, Arc, AMPAR, NMDAR; BDNF-TrkB-mTORC1 also contribute) or translation of transcripts localized to dendrites, yielding long-lasting alterations in synaptic efficacy. Abbreviations: AC, adenylyl cyclase; AMPAR, α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid receptor; ATP, adenosine triphosphate; BDNF, brain-derived neurotrophic factor; CaMKII, Ca2+-calmodulin-dependent protein kinase II; CaMKII, Ca2+-calmodulin-dependent protein kinase IV; cAMP, cyclic adenosine monophosphate; CREB, cAMP response element-binding protein; LTP, long-term potentiation; mTORC1, mechanistic target of rapamycin complex 1; NMDAR, N-methyl-D-aspartate receptor; PKA, protein kinase A; PKC, protein kinase C; TrkB, tropomyosin receptor kinase B. Created with Biorender.com
Kinase activity facilitates LTP expression about one hour after LTP induction [64, 65]. During LTP expression, CaMKII, PKA, and PKC potentiate synaptic efficacy through many mechanisms including phosphorylation-dependent enhancement of AMPAR conduction [66-69], the insertion of AMPARs in the postsynaptic density [70-72], and actin polymerization-mediated dendritic spine enlargement [73, 74].
The kinase activity-dependent phase of LTP expression gives rise to LTP maintenance, which begins several hours after induction, persists over a period of days [58, 75], and is dependent on postsynaptic protein synthesis [76]. Mechanisms of LTP maintenance are numerous and complex [65], but well-studied somatic, nuclear transcription mechanisms involved in LTP maintenance include Ca2+/calmodulin-dependent activation of postsynaptic adenylyl cyclase-cAMP-PKA [77, 78] and CaMKII/IV [79] thereafter enabling extracellular signal-regulated kinase-induced phosphorylation of transcription factor cAMP response element-binding protein (CREB) [80, 81]. Multiple mechanisms of CREB activation enable fine-tuning of cAMP response element-dependent molecular effectors (e.g., brain-derived neurotrophic factor [BDNF], Arc, c-fos, etc.). LTP maintenance also contributes to structural plasticity via the enhancement of dendritic spine density and de novo spine development [73, 81-83]. It is also established that BDNF-tropomyosin receptor kinase B (TrkB)-mammalian target of rapamycin complex 1 (mTORC1)-dependent signaling plays critical roles in LTP maintenance [84].
Rather than high-frequency tetanic stimuli, electrophysiological induction of LTD can be initiated by repeated low-frequency stimulation (e.g., 1 Hz for 15 min). Similar to LTP induction, low-frequency stimulation enables Ca2+ to enter the postsynaptic cell via NMDAR, but due to modest NMDAR channel opening, a relative reduction of Ca2+ influx occurs compared to LTP, resulting in LTD induction that leads to activation of protein phosphatases that promote LTD expression [85]. A phosphatase that features prominently in LTD expression is calcineurin, a Ca2+/calmodulin-sensitive phosphatase that is activated in parallel with CaMKII activation [86]. Low-level Ca2+ influx inherent to LTD induction enables transient activation of CaMKII but sustained activation of calcineurin due to greater affinity of the phosphatase for Ca2+/calmodulin, promoting LTD expression via calcineurin-induced activation of protein phosphatase 1-mediated dephosphorylation of surface level AMPARs [87, 88]. Calcineurin and other phosphatases contribute to LTD expression through endocytosis of surface AMPARs as well [89]. The alterations in synaptic transmission that persist via LTD maintenance are protein synthesis-dependent and yield a reduction in the size of dendritic spines, and in some cases, the removal of spines [90, 91].
While we have framed the mechanisms underlying NMDAR-dependent LTP/LTD expression and maintenance as sequential, many of these molecular events have been shown to occur simultaneously, underscoring the elegant endogenous molecular machinery involved in maintaining shifts in long-term synaptic efficacy that are modulated by activation of metaplastic mechanisms.
Metaplasticity: a druggable mechanism in the context of depression?
Many forms of stimuli can influence subsequent alterations in synaptic plasticity. Specifically, the threshold for the modification of synaptic efficacy can be altered as a result of previous experience [92]. That is, a priming event that induces neural activity (e.g., stimulation, stress, environmental enrichment, pharmacological agents, etc.) may persistently influence subsequent synaptic plasticity induction events (e.g., LTP, LTD) by a phenomenon known as metaplasticity (Figure 1A) [93]. Prominent theories such as the Bienenstock, Cooper, and Munro (BCM) model have been proposed to explain how experience primes synapses for subsequent nonlinear shifts in synaptic efficacy [94]. Within the BCM model, the capacity for activated synapses to exhibit a shift in efficacy is dependent upon a dynamic, bidirectional modification threshold. The modification threshold can be thought of as a sliding scale where the history of synaptic activity may promote or diminish the capacity for synaptic potentiation. For instance, the threshold for the capacity of LTP formation is reduced following periods of low activity, leading to a greater likelihood for the generation of LTP. The BCM model is supported by findings in a preclinical model of amblyopia in which the threshold for thalamocortical synaptic potentiation was reduced via visual deprivation, resulting in a subsequent capacity for restoration of ocular dominance plasticity in adult rats [95].
There are several other key features of metaplasticity beyond the experience-dependent component. For instance, unlike plasticity exerted by direct effects, or concurrent plasticity events that impact one another, metaplastic effects necessitate that the activity induced by the priming event activate a metaplastic mechanism(s) that persists until exposure to successive stimuli [56]. Activated metaplastic mechanisms as commonly studied persist for minutes to hours but may last up to days after exposure to pharmacological agents [96] or behavioral experiences [97] that activate such mechanisms. That is, metaplastic effects occur following the termination of the priming stimulus (e.g., electrical stimulation of neural cells [92], clearance of a drug that activates cellular signaling [98], or behavioral experiences that stimulate physiological actions [99, 100]) that activate metaplastic mechanisms. Repeated exposure to the same metaplasticity induction stimulus can also enhance or prolong the activation of metaplastic mechanisms [101]. Thus, metaplastic effects will be referred to as a sustained, persisting, or prolonged effect(s) of therapeutic interventions herein. Further, in many cases, the efficacy of synaptic transmission is not directly modulated by metaplasticity but rather the metaplastic event alters the capacity of cellular activity for depression/potentiation upon subsequent plasticity events [92, 102, 103]. Thus, metaplasticity can be defined as plasticity that alters the duration, direction, or magnitude of future synaptic plasticity induction events, presenting as quantitative (e.g., a change in the magnitude of potentiation or depression due to modulating the ability of the synapse to respond to a stimulus) or qualitative (e.g., shifting from LTD to LTP) alterations in the capacity for adjustments in synaptic efficacy.
One of the most well-investigated initiators of metaplasticity is the NMDAR [56]. NMDAR-associated metaplasticity may occur homosynaptically (i.e., at synapses activated during the priming stimulation) or heterosynaptically (i.e., at synapses inactivated or weakly activated during the priming stimulation), and has been proposed to act as a regulator of synaptic plasticity through diverse mechanisms that subsequently facilitate adaptations in synaptic efficacy [104]. For instance, prior, repeated, homosynaptic activation of the NMDAR has been shown to impair LTP and facilitate LTD in the CA1 subfield of the hippocampus [92, 105]. NMDAR-dependent heterosynaptic metaplasticity has been observed in numerous synapses including the dentate gyrus where LTP induction in medial perforant pathway synapses persistently prevented LTP induction in the lateral perforant pathway in vivo [96]. These NMDAR-mediated metaplastic shifts have been proposed to fine-tune the saturation of synaptic potentiation, acting homeostatically to protect against aberrant levels of excitation as observed in disease states such as epilepsy [106]. NMDAR-dependent metaplasticity has also been postulated to modulate the stimulus threshold needed for learning including enhancing the capability for consolidation of novel information or impairing the capacity for synaptic plasticity events to integrate superfluous new knowledge [104].
Consistent with the hypothesis that metaplasticity is vital for maintaining nervous system activity, dysfunctional metaplasticity has been implicated in diverse conditions and disease states [104]. Specifically, stress, a major etiological factor in depression [107, 108], has been shown to induce complex network effects in rodents [109] where acute swimming stress or in vitro exogenous application of corticosterone enhanced LTP generation in the ventral hippocampus but impaired LTP formation in the dorsal hippocampus [110]. Excessive activation of GluN2B-containing NMDARs following amyloid-β-mediated impairment in glutamate uptake (priming event) has been linked to hippocampal LTP inhibition in preclinical studies of Alzheimer’s Disease [111, 112]. Many metaplastic effects of cocaine have also been reported, including a persistent enhancement of LTP formation in the ventral (but not dorsal) hippocampus [98, 113], effects that contribute to aberrant plasticity in mesocorticolimbic circuitry that may underlie the durability of drug-associated memories and risk of relapse [114].
As discussed in the next section, therapies used in psychiatry have been found in preclinical studies to alter the threshold for plasticity induction and enhance antidepressant efficacy. Thus, metaplasticity mechanisms themselves may serve as druggable mechanisms for novel treatments. Accordingly, the field of psychiatry is primed for investigations aimed at i) leveraging the metaplastic mechanisms engaged by treatment modalities (e.g., pharmacotherapies, neuromodulation) to enhance antidepressant efficacy and/or reduce adverse drug effects and ii) designing novel therapeutics, i.e.,metaplastogens, which directly harness metaplasticity.
METAPLASTIC EFFECTS OF RAPID-ACTING ANTIDEPRESSANTS
There are clinical reports of deficits in excitatory neurotransmission and activity-dependent synaptic plasticity contributing to the pathophysiology of MDD (Table 1). For clinical and preclinical reviews of synaptic plasticity deficits in the context of depression see: [11, 115-117]. Thus, it follows that the discovery and development of metaplastogens that induce increased ability of circuits and synapses to respond with beneficial changes in synaptic strength may be an effective approach in improving depressive symptoms as well as to underlying pathophysiology. Here, we examine several putative pharmacological mechanisms of rapid-acting antidepressants including a discussion of the convergence of their downstream, antidepressant-relevant molecular effects that may be involved in therapeutic metaplastic mechanisms. We also discuss potential opportunities for leveraging metaplasticity to optimize existing antidepressant therapies, and to influence novel treatment discovery.
Table 1. Examples of synaptic plasticity deficits associated with human depression.
Described are studies that compared measures of plasticity responses in individuals with major depressive disorder (MDD) compared to healthy controls (HC). After visual stimuli exposure, visually evoked responses are postsynaptic potentials recorded from the occipital region via electroencephalogram (EEG). Paired associative stimulation protocols involve ulnar nerve stimulation coupled with single-pulse transcranial magnetic stimulation (TMS) to the motor cortex to elicit a motor-evoked response assessed by peripheral motor-evoked potentials (MEPs). Theta burst stimulation (TBS) involves a shorter duration of TMS administration compared to non-TBS TMS due to the delivery of recurrent pulses in the theta range (4-7 Hz) at a high frequency to produce an alternating electromagnetic field that activates cortical neurons resulting in peripheral MEP responses. This table represents a subset of relevant studies and is not a complete listing of all available studies. DLPFC, dorsolateral prefrontal cortex; HC, healthy controls; LTD, long-term depression; LTP, long-term potentiation; TBS, theta burst stimulation.
| Study | Group studied | Method | Outcome |
|---|---|---|---|
| Normann [213] | 40 MDD; 74 HC | Visually-evoked EEG responses | Impaired cortical synaptic transmission and LTP-like responses |
| Kuhn [214] | 27 MDD; 27 HC | Paired associative stimulation evoked MEPs | Impaired cortical LTP-like responses |
| Noda [215] | 29 MDD; 28 HC | Paired associative stimulation evoked MEPs | Impaired DLPFC LTP-like responses |
| Player [216] | 23 MDD; 23 HC | Paired associative stimulation evoked MEPs | Impaired cortical LTP-like responses |
| Yu [217] | 31 MDD; 29 HC (all females) | Continuous TBS-evoked MEPs | Impaired cortical LTD-like activity |
Conceptualization of NMDAR inhibitors as rapid-acting antidepressants
Ketamine, derived from phencyclidine (PCP), became a more widely used dissociative anesthetic than PCP due to its shorter half-life, improved therapeutic window, and reduction in adverse effects [118, 119]. Decades later ketamine was shown to induce rapid and sustained antidepressant effects in adults [13, 14] and antidepressant-like effects in rodents (e.g., [120]). Ketamine is now considered to be the prototypical pharmacological rapid-acting antidepressant [10]. The initiating mechanism of ketamine’s rapid and sustained antidepressant effects has been presumed to be due to its activity-dependent, inhibitory profile at the NMDAR [119, 121]. Specifically, immediate pharmacological actions of ketamine result in the inhibition of NMDAR activity and NMDAR-dependent transmission, with the results of some studies suggesting preferential blockade of NMDAR subtypes [47, 122-124], although the reported selectivity of ketamine is debated and may be due to variations in glutamate concentration, Mg2+ concentration, and subcellular pH level between experimental systems [45]. Multiple NMDAR inhibition-dependent hypotheses have been proposed to explain the rapid and sustained antidepressant actions of ketamine. Some of the most prominent hypotheses converge on a mechanism that activates impaired circuits in MDD pathophysiology to ultimately enhance the strength of excitatory synapses in brain regions involved in reward, cognition, and mood by means of i) disinhibition of glutamatergic transmission via selective inhibition of NMDARs on GABAergic interneurons, ii) inhibition of spontaneous synaptic NMDAR activity, iii) inhibition of NMDAR-dependent lateral habenula bursting activity, and iv) selective inhibition of extrasynaptic, GluN2B-containing NMDARs [121].
Prior environmental [125-127] or pharmacological [128] stimuli that decrease GluN2B-containing NMDAR activity have been shown to subsequently stimulate metaplastic mechanisms in the visual cortex of developing, juvenile mice, increasing neuronal GluN2B while later decreasing GluN2A surface expression to reduce the GluN2A:GluN2B ratio and lowering the threshold for LTP formation [129, 130]. Outside of the context of developmental studies, a subanesthetic dose of ketamine has been shown to increase GluN2B protein levels and reduce the GluN2A:GluN2B ratio in the mPFC of rats 24 h after administration [131], suggesting that blockade of GluN2B-containing NMDARs with ketamine may induce a delayed shift in the threshold for alterations in synaptic efficacy towards one in which potentiation is more readily achieved, potentially through trafficking of NMDARs to synaptic sites. Selective blockade of GluN2B-containing NMDARs has been reported in some studies to be essential for the antidepressant-relevant effects of ketamine [132, 133]. For instance, GluN2B antagonist CP-101,606 induces acute and prolonged antidepressant-like effects [134], and ex vivo hippocampal LTP formation was enhanced up to 24 h after administration in rodents [135].
However, clinical trials with nonselective and GluN2B-selective NMDAR antagonists did not find robust, rapid, and/or persistent antidepressant effects similar to ketamine [23-34], raising questions about the essential role of NMDAR antagonism for the induction/persistence of antidepressant mechanisms. Limitations of ketamine, such as anesthetic and dissociative/psychomimetic effects as well as misuse liability, have been associated with its inhibitory actions at the NMDAR [36, 37, 40, 46, 136]. These concerns are underscored by several other components of ketamine’s pharmacology and metabolism including i) (R)-ketamine exhibiting greater antidepressant-like efficacy in preclinical models than racemic ketamine or (S)-ketamine while being a less potent inhibitor of the NMDAR [46, 137, 138], ii) high doses/concentrations of ketamine not inducing antidepressant-relevant behaviors, enhancing synaptic transmission, or altering the capacity for changes in synaptic efficacy [139-142], iii) evidence of ketamine-induced dissociation, which has been linked to NMDAR-dependent inhibition, not consistently being associated with antidepressant efficacy [143], and iv) ketamine metabolite (2R,6R)-HNK being sufficient for the induction of rapid and sustained antidepressant-like effects via a non-NMDAR-dependent mechanism [46, 47].
Pharmacological direct and indirect NMDAR activators
Emerging evidence suggests that the profile of ketamine’s antidepressant-relevant effects involves a role for NMDAR activation. This includes the finding that ketamine treatment enhances the capacity for canonical NMDAR activation-dependent synaptic potentiation. For instance, preclinical studies have found that ketamine application to hippocampal slices requires NMDAR activation to rapidly enhance synaptic transmission [142] and engages metaplastic mechanisms as evidenced by an enhanced ability to form LTP at the Schaffer collateral-CA1 (SC-CA1) synapse after ketamine wash-out [141]. To our knowledge, Moskal, Burgdorf, and colleagues were the first to report persistently enhanced ex vivo LTP formation, which has been replicated by other research groups [135, 139, 144-146]. Augmented capacity to form LTP when recording in vivo at the hippocampal SC-CA1 synapse [147] and the hippocampus-accumbens pathway [148] in Wistar-Kyoto rats, a rat line that inherently contains many of the neurological impairments presented in MDD [149], after ketamine administration has also been described. A sustained enhancement of ex vivo LTP formation at the SC-CA1 synapse after treatment with a subanesthetic dose of the stereoisomer (S)-ketamine has been found as well [150, 151]. Persisting metaplastic effects of ketamine in rodent subcortical structures are evidenced by reduced capacity for ex vivo LTP recorded from the nucleus accumbens core [152] and promotion of an AMPAR-dependent form of ex vivo LTD in dopaminergic neurons of the ventral tegmental area after treatment [153]. Further, hippocampal metaplasticity measured ex vivo, as evidenced by an enhanced capacity to generate LTP 24 h after ketamine administration, required NMDAR activation [139]. These findings are consistent with the hypothesis that rapid-acting antidepressants promote metaplastic changes [154] that lead to activity-dependent alterations in synaptic efficacy that ameliorate MDD-relevant deficits in synaptic transmission [10].
The hypothesis that ketamine improves depression symptomology by enhancing excitatory transmission of depression-weakened synapses has led to the investigation and development of several classes of therapeutics that produce a ketamine-like enhancement in glutamatergic transmission via NMDAR inhibition-independent mechanism(s). These include direct and indirect NMDAR activators, an approach that is in line with the role of NMDARs in enhancing synaptic efficacy via canonical NMDAR-dependent LTP (Figure 2). For instance, indirect stimulation of the NMDAR glycine site via glycine transporter inhibition with sarcosine (N-methyl-glycine) treatment resulted in a significantly greater antidepressant effect than citalopram in subjects with MDD [155]. Direct NMDAR activation via positive allosteric modulation (PAM) facilitates long-lasting NMDAR-dependent metaplasticity in rodents as revealed by enhancement of ex vivo hippocampal LTP formation one week after administration of the NMDAR PAM NYX-2925 [156] and a persisting elevation in the ability to form in vivo auditory-evoked LTP as measured by EEG one hour after administration [157]. Accordingly, induction and maintenance of antidepressant effects via enhancement of NMDAR activity via PAM has shown potential as an approach to developing novel therapeutics [35]. For instance, administration of NMDAR PAM rapastinel promotes rapid and sustained antidepressant-like effects in rodents, which were associated with increased mature spine density in the primary apical dendrites of the dentate gyrus and layer V pyramidal cells in the mPFC as well as activity-dependent stimulation of dentate gyrus/PFC BDNF-TrkB-mTOR signaling without psychotomimetic/dissociative side effects [158-162]. Antidepressant-like effects of rapastinel also coincided with alterations in synaptic plasticity when administered to rodents including i) rapid enhancement of LTP and reduction of LTD at the SC-CA1 synapse following in vitro application to hippocampal slices [163], ii) an increase in the capacity to generate mPFC LTP recorded from pyramidal cells after bath application [158], and iii) persistent metaplasticity as revealed by enhanced ex vivo LTP at the SC-CA1 synapse up to one week after a single administration [162]. However, after positive phase II results [164], rapastinel treatment failed to induce significantly greater antidepressant effects than placebo in phase III trials (ClinicalTrials.gov Identifiers: NCT02951988, NCT02943577, NCT02943564 [165]).
Another potent, orally bioavailable, NMDAR PAM that shares similar pharmacology to rapastinel, zelquistinel (AGN-751) [166], was well-tolerated in a phase II clinical trial for the treatment of MDD but, while improving depression symptomology, did not separate from placebo (ClinicalTrials.gov Identifier: NCT03586427) and is currently being assessed in a separate phase II trial (ClinicalTrials.gov Identifier: NCT03726658). LTP formation in the rodent mPFC following acute zelquistinel exposure was augmented, while dose-dependent and persistent metaplasticity in the hippocampus and mPFC of rats was observed as evidenced by sustained facilitation of LTP formation seven days after a single drug administration [166]. Interestingly, an inverted U-shaped curve in the capacity to form LTP ex vivo was observed in the hippocampus of mice 24 h after zelquistinel administration, presumably due to impairing NMDAR activity at higher doses. Thus, while canonical metaplasticity theories suggest a nonlinear, sliding scale conception of metaplastic mechanism activation [167], the inverted U profile of pharmacotherapies such as zelquistinel underscores one of many unique features of metaplasticity that should be carefully considered when assessing dose-dependent metaplastic effects [94].
Overall, preclinical studies of NMDAR PAMs that activate metaplastic mechanisms support the thesis that antidepressant treatment modalities that potentiate NMDAR activity promote persisting antidepressant-like effects via a downstream metaplastic mechanism that converges with that of ketamine. However, similar to non-ketamine NMDAR inhibitors, there have been notable challenges in translating promising NMDAR PAM preclinical findings into clinical results. These challenges may be the result of shortcomings in clinical study design such as drug administration protocol, placebo effect, and/or subject heterogeneity. Additionally, it has yet to be revealed which GluN subtype may be the optimal target for antidepressant PAM development as ketamine-like effects with nonselective GluN2 [166] and selective GluN2A PAMs [139] have been reported. Mixed findings with NMDAR PAMs underscore the necessity for additional inquiry into their detailed short-term and long-term antidepressant mechanism, and that investigation of metaplasticity-engaging pharmaceuticals that modify the activity of effectors downstream of the NMDAR may be a viable route for developing novel MDD therapeutics.
Converging druggable metaplasticity mechanisms of ketamine mimetics
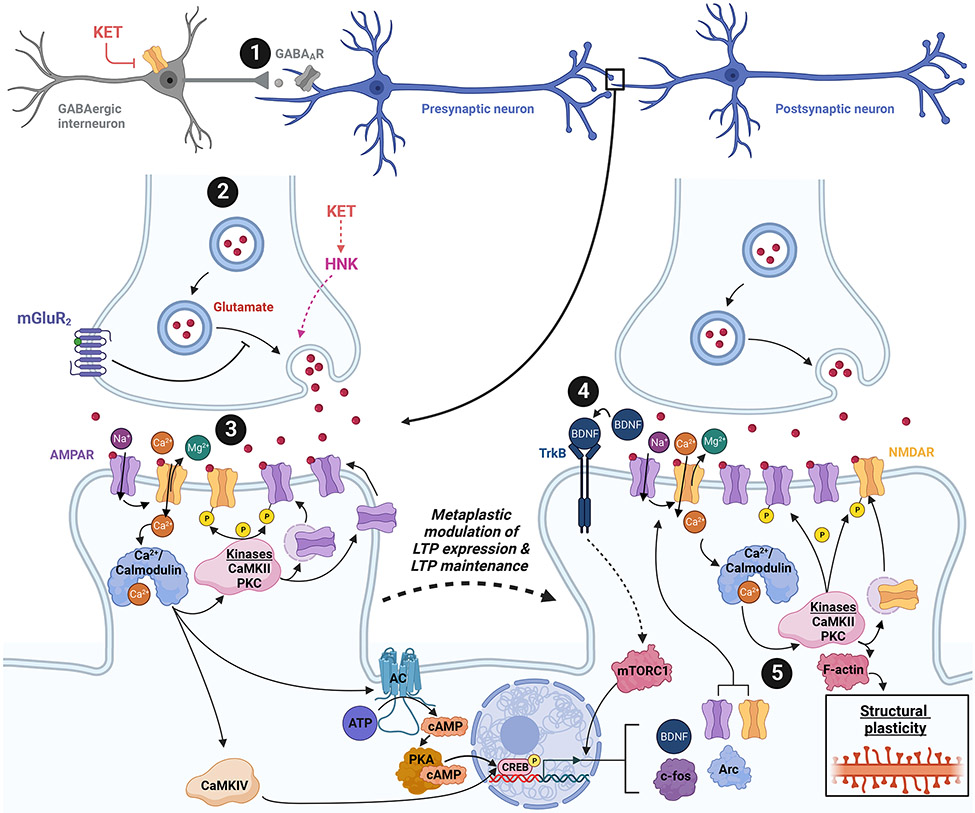
Although acting through distinct induction mechanisms (i.e., PAM or putative antagonism), we have thus far highlighted how the fulcrum of metaplasticity within this review, the NMDAR, may be pharmacologically manipulated to activate metaplastic, antidepressant-relevant mechanisms that converge around consistent molecular signaling cascades to persistently increase the strength of excitatory neurotransmission, presumably by engaging mediators of canonical NMDAR activation-dependent LTP (Figure 3). The activation of metaplastic mechanisms by alternative ketamine mimetics centers around stimulation of induction mechanisms that engage canonical NMDAR activation-dependent long-term synaptic plasticity including i) disinhibiting glutamatergic neuron activity, ii) increasing the probability of glutamate release, iii) augmenting glutamatergic receptor activity, and iv) enhancing neurotrophic signaling. A number of strategies may be used to engage these metaplasticity induction sites, highlighting a substantial opportunity to employ selective pharmacotherapy and/or neuromodulatory approaches in the design of next-generation antidepressant metaplastogens to engage unexplored antidepressant mechanisms.
Figure 3. Strategies for targeting metaplastic mechanisms.
Results from preclinical studies suggest that the antidepressant-like effects of ketamine coincide with sustained, beneficial metaplasticity in brain regions implicated in the pathophysiology of depression. Numerous strategies can be used in envisioning ketamine mimetics that may leverage metaplastic mechanisms (metaplastogens) in a manner that coincides with rapid and prolonged antidepressant effects. 1. Disinhibition of glutamatergic neuron activity: Ketamine may work as an antidepressant by disinhibiting glutamatergic neurons via preferential inhibition of NMDARs localized to interneurons [17, 121]. Sustained metaplasticity and long-lasting antidepressant effects are observed after ketamine treatment. Administration of a subanesthetic dose of ketamine is proposed to preferentially block NMDARs localized to interneurons to disinhibit principal cell activity. Reducing the tone of GABAergic activity via negative allosteric modulation (NAM) may also yield similar results (e.g., α5 GABA NAM MRK-016 [11, 211]). 2. Increase probability of glutamate release: Hepatic metabolism of ketamine produces norketamine and, subsequently, hydroxynorketamines. (2R,6R)-HNK has been shown to rapidly enhance glutamatergic transmission via increased probability of glutamate release, followed by sustained metaplasticity and persisting antidepressant-like effects [3]. Inhibition of the glutamate autoreceptor mGluR2 has also been proposed to enhance the probability of glutamate release, augment glutamatergic transmission, facilitate sustained changes in the capacity for synaptic plasticity, and induce prolonged antidepressant-like effects [212]. 3. Augmentation of glutamatergic receptor activity: Direct activation of NMDARs via positive allosteric modulation promotes enhanced glutamatergic transmission, alters the threshold for LTP formation, and results in enduring antidepressant-like effects. Evidence also suggests sustained metaplasticity and antidepressant effects detected after ketamine administration require NMDAR activation [139]. 4. Increase neurotrophic signaling: Ketamine and numerous metaplasticity-engaging putative ketamine mimetics converge around a mechanism that increases neurotrophic signaling (i.e., BDNF-TrkB-mTORC1), suggesting that targeting antidepressant-relevant metaplastic mechanisms to facilitate neurotrophic factor production may be a viable route for designing novel therapeutics. 5. Enhance or prolong mechanisms underlying the expression or maintenance of potentiated synaptic efficacy: The metaplasticity observed after treatment with ketamine and putative ketamine mimetics alters the duration, direction, or magnitude of synaptic plasticity, suggesting that developing therapeutics that engage metaplastic mechanisms along a pathway that converges with canonical NMDAR activation-dependent LTP to modulate mediators of LTP maintenance is a route that may yield exciting, novel treatment modalities for depression. Abbreviations: AC, adenylyl cyclase; AMPAR, α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid receptor; ATP, adenosine triphosphate; BDNF, brain-derived neurotrophic factor; CaMKII, Ca2+-calmodulin-dependent protein kinase II; CaMKII, Ca2+-calmodulin-dependent protein kinase IV; cAMP, cyclic adenosine monophosphate; CREB, cAMP response element-binding protein; GABA, γ-aminobutyric acid; GABAAR, GABAA receptor; HNK, (2R,6R)-hydroxynorketamine; KET, (R,S)-ketamine; LTP, long-term potentiation; mGluR2, metabotropic glutamate receptor subtype 2; mTORC1, mechanistic target of rapamycin complex 1; NMDAR, N-methyl-D-aspartate receptor; PKA, protein kinase A; PKC, protein kinase C; TrkB, tropomyosin receptor kinase B. Created with Biorender.com
Evidence of sustained metaplasticity following administration of ketamine metabolite (2R,6R)-HNK has been reported where enhanced capacity for hippocampal [147] and amygdalar [168] LTP formation was observed 3.5 h and 24 h after (2R,6R)-HNK treatment, respectively. (2R,6R)-HNK has been found to initiate its rapid antidepressant-relevant effects through an NMDAR-independent mechanism and has completed phase I clinical trials (ClinicalTrials.gov Identifier: NCT04711005) [46, 47, 169-172]. In vivo (2R,6R)-HNK administration leads to ketamine-like, antidepressant-relevant synaptic effects in rodents in multiple brain regions including the prefrontal cortex [173], basolateral amygdala [168], hippocampus [46, 147], and ventrolateral periaqueductal gray [174, 175]. Specifically, acute (2R,6R)-HNK exposure rapidly enhances presynaptic-mediated synaptic transmission at the SC-CA1 synapse in hippocampal slices via increased probability of glutamate release as reflected by decreased paired-pulse facilitation in addition to elevated miniature excitatory postsynaptic current frequency, but not amplitude [170, 176]. Similar to parent compound ketamine, the sustained antidepressant-like effects of (2R,6R)-HNK also require AMPAR activity [46, 174] in addition to postsynaptic L-type voltage-gated Ca2+ channel-dependent enhancement of intracellular Ca2+ levels, which contribute to BDNF-TrkB-mTORC1-dependent activity-[177]. However, the role of these proteins in persistently altering the threshold for changes in synaptic efficacy following (2R,6R)-HNK treatment has not been directly investigated.
A substantial number of reports have shown that antagonists of the mGluR2/3 induce rapid and sustained antidepressant-like effects in rodents [48, 178, 179], generating expectations for mGluR2/3 antagonists such as TS-161 in phase II clinical trials for MDD (ClinicalTrials.gov Identifier: NCT04821271). While the individual, sustained, ex vivo metaplastic effects of mGluR2/3 antagonists when administered to rodents at antidepressant-relevant doses have not been reported, Pałucha-Poniewiera [151] found that administration of subthreshold doses of (R)-ketamine and a mGluR2/3 antagonist that, when combined, led to antidepressant-relevant effects including enhanced LTP formation in the PFC 72 h after drug administration. This result is in line with another study that found that combined administration of subthreshold doses of (2R,6R)-HNK and a mGluR2/3 antagonist elicited antidepressant-like behavioral responses [180]. As the mGluR2 acts as an autoreceptor on hippocampal/mPFC principal cells to directly regulate glutamatergic signaling whereas the mGluR3, which is primarily expressed on glial cells, indirectly reduces excitatory neurotransmission [48], the antidepressant effect of group II mGluRs is presumably due to an increase in the excitatory to inhibitory tone of brain regions implicated in the pathophysiology of MDD. The antidepressant-relevant effects of mGluR2/3 antagonists have been found to converge with those of ketamine and (2R,6R)-HNK [180], and mGluR2/3 agonists/PAMs block the antidepressant-relevant effects of ketamine [181-183]. Like ketamine, antidepressant-relevant effects of mGluR2/3 antagonists have been reported to require AMPAR [184-186], NMDAR [139], and BDNF-TrkB-dependent signaling [151, 184, 187, 188] while also stimulating mTORC1-dependent activity [179]. These data suggest that these proteins, and others associated with their activity, may be starting points for assessing the metaplastic, antidepressant-relevant mechanisms activated after mGluR2/3 antagonist treatment.
With abundant evidence highlighting the convergence of molecular mechanisms underlying the persistent therapeutic effects of pharmacologically diverse, rapid-acting antidepressants, there is an opportunity to harness metaplastic mechanisms as druggable targets by combining multiple metaplasticity-inducing treatment modalities (i.e., pharmacotherapy and noninvasive neuromodulation) that converge on shared molecular targets to augment therapeutic efficacy and/or mitigate adverse responses inherent to each individual treatment modality (Figure 3). Similar to ketamine, the antidepressant effects of noninvasive, targeted neuromodulatory therapies such as transcranial magnetic stimulation (TMS) are NMDAR activation-dependent [189]. Non-targeted neuromodulatory approaches like electroconvulsive therapy (ECT) and the preclinical equivalent, electroconvulsive seizures (ECS), appear to also induce therapeutic effects via activity-dependent plasticity that involves NMDAR activation [190-192]. This is consistent with findings of subanesthetic ketamine administration occluding the potentiating effects of ECS in the rat hippocampus [190, 193, 194]. Further, the magnitude and/or duration of the antidepressant effects of pharmacological (i.e., ketamine) interventions have been shown to be augmented by evidence-based psychotherapy [195, 196] or repeated ketamine administration [16], indicating that antidepressant engagement of metaplastic mechanisms may prepare synapses for subsequent increases in activity-dependent synaptic efficacy. The same has also been proposed for noninvasive neuromodulatory interventions combined with psychotherapy [197]. For instance, in subjects with MDD, ketamine infusion 11 hours before ECT administration facilitated a significantly greater antidepressant effect compared to ECT alone, suggesting a metaplastic priming effect of ketamine [198]. A separate small double-blind, placebo-controlled study detected a trend for a significant reduction in early remission of depression symptomology in MDD subjects who received ketamine and ECT on alternating days [199]. Reports have identified an apparent metaplastic, priming effect of adjunctive D-cycloserine at a dose that is proposed to induce partial agonist activity at the NMDAR glycine site on a form of TMS, intermittent theta burst stimulation (iTBS), which delivers recurrent pulses in the theta range (4-7 Hz) at a high frequency to produce an alternating electromagnetic field that activates cortical neurons. Specifically, D-cycloserine pretreatment primed the synaptic alterations induced by iTBS in the motor cortex in healthy controls [200]. Low-dose D-cycloserine has also been found to enhance the capacity for TMS-induced, motor-evoked synaptic plasticity without affecting pre-TMS basal motor excitability in healthy subjects [201]. After D-cycloserine treatment, synaptic plasticity in the motor cortex was normalized [202] and the antidepressant effect of iTBS in subjects with MDD was augmented [203]. Outside of activating NMDAR-mediated signaling, it is currently unclear what metaplastic mechanisms are engaged by approaches that combine pharmacotherapy and neuromodulation treatments. Thus, there is an opportunity for exploring metaplastic mechanisms engaged by both treatment modalities, an endeavor that may lead to the design of novel antidepressant treatment regimens.
FUTURE DIRECTIONS
Evidence presented in this review suggests that ketamine, as well as pharmacologically diverse, rapid-acting antidepressants in development, engage metaplastic mechanisms that may, in part, contribute to the induction and persistence of their therapeutic benefits in the context of depression. Specifically, many such putative antidepressants converge on a signaling cascades that activates i) metaplastic mechanisms that lower the threshold for synaptic potentiation in healthy conditions and ii) ameliorative metaplastic mechanisms to improve impaired capacity for synaptic potentiation in the context of depression (e.g., clinical MDD, preclinical chronic stress animal models, etc.). We suggest that antidepressant-relevant metaplasticity may be a useful, robust tool that can be leveraged to increase the probability of discovering and developing successful antidepressants.
As the field of MDD research has transitioned to a period in which the predictive validity of commonly used behavioral paradigms of antidepressant efficacy is under intense scrutiny [204], robust, quantifiable, and reproducible metrics must fill this void. Assessment of antidepressant-induced metaplasticity may be a relevant endpoint. Further, there are numerous potential therapeutic benefits of metaplasticity as a druggable mechanism. As therapeutic metaplastic mechanisms are persistently active following elimination of the drug substance, patient burden is diminished by less frequent dosing. Sustained activation of therapeutic mechanisms in the absence of a molecule that may elicit adverse responses when present in the body (e.g., ketamine) may improve patient quality of life by reducing drug side-effects (Figure 1B). As such, determining if a particular MDD treatment modality (e.g., pharmacotherapy, neuromodulation, psychotherapy) induces a greater, or longer-lasting, shift in the capacity for a change in synaptic efficacy by subsequent stimuli could provide researchers/clinicians with an opportunity to improve antidepressant response or decrease patient burden.
Distinct pharmacotherapies proposed as novel treatments for depression converge to implicate molecular signaling cascades that result in increased strength of excitatory neurotransmission by engaging mediators of NMDAR activation-dependent LTP, notably AMPAR, NMDAR, BDNF-TrkB, and mTORC1 (Figure 3). While the necessity of such effectors in producing persistent antidepressant-like behavioral effects after ketamine treatment has been evaluated, only the NMDAR has been directly investigated as a necessary contributor to the antidepressant-relevant metaplastic mechanism(s) at the synaptic level [139], underscoring a knowledge gap in the mechanisms of antidepressant-relevant metaplasticity. While the NMDAR appears involved in the activation of metaplastic mechanisms after ketamine treatment, more work is needed to determine if ketamine mimetics similarly activate NMDAR-mediated metaplasticity, and if other well-established initiators of metaplasticity (i.e., group I mGluRs [56]) alone or in combination with one another are involved in metaplastic effects.
There is also a paucity of studies that have characterized the temporal progression of metaplasticity detected following the administration of antidepressants. A major obstacle in these investigations will be disentangling the acute, rapid effects of antidepressants when the drug is still present in vivo compared to the sustained metaplastic effects following elimination. Likewise, there has been insufficient investigation of the mechanisms underlying the expression/maintenance of metaplasticity after the induction of such effects. Further investigation into the mechanism(s) that drive the persistent shift in the capacity for changes in synaptic activity by prior treatment with rapid-acting antidepressants (e.g., ketamine) or other emerging neuropsychiatric therapeutics (e.g., psychedelics) is warranted [205, 206]. Intriguingly a study found that ketamine and psychedelics (e.g., 3,4-methylenedioxy methamphetamine, psilocybin, lysergic acid diethylamide, and ibogaine) converge on shared metaplastic actions to persistently augment the capacity for social reward learning, underscoring the potential of diverse psychedelics for engaging metaplasticity [206], potentially providing an explanation for priming antidepressant and other psychiatric actions that are augmented by psychotherapy [207].
Combining in vivo or ex vivo electrophysiological (e.g., LTP or LTD induction protocols) and behavioral measures of plasticity that rely on those same synapses [208, 209] provides researchers with tools to quantify the activation of metaplasticity mechanisms by prior stimuli [Additional behavioral protocols reviewed in 56]. Such investigations could reveal exciting opportunities for novel targets that could be engaged for ameliorating symptomology presented in psychiatric disorders. Utilizing a fine-tuned, personalized approach [210] that involves simultaneous administration of rapid-acting pharmacotherapies that activate metaplastic mechanisms along with circuit-selective neuromodulation in individuals with depression could be used to design treatment regimens for MDD. Indeed, the study of the metaplastic mechanisms engaged by antidepressants is in a nascent state, providing opportunities for exciting discoveries and clinical advancements.
ACKNOWLEDGEMENTS
We thank Drs. Gustavo Medeiros, John Donello, John Wagner, Fernando Goes, Carlos Zarate, and all members of the Gould laboratory for critical reviews of the manuscript.
FUNDING AND DISCLOSURE
This work was supported by NIH/NIMH R01MH107615 and U.S. Department of Veterans Affairs Merit Awards 1I01BX004062 and 1I01BX006018 to TDG. The contents of this manuscript do not represent the views of the U.S. Department of Veterans Affairs or the United States Government. TDG is listed as an inventor in patents and patent applications related to the pharmacology and use of a ketamine metabolite, (2R,6R)-hydroxynorketamine, in the treatment of depression, anxiety, anhedonia, suicidal ideation, and post-traumatic stress disorders. TDG has assigned his patent rights to the University of Maryland, Baltimore, but will share a percentage of any royalties that may be received by the University of Maryland, Baltimore. KAB declares no competing interests.
REFERENCES
- 1.WHO. Mental Disorders. World Health Organization: https://www.who.int/news-room/fact-sheets/detail/mental-disorders, 2022, pp 1–2. [Google Scholar]
- 2.Greenberg PE, Fournier A-A, Sisitsky T, Simes M, Berman R, Koenigsberg SH et al. The economic burden of adults with major depressive disorder in the United States (2010 and 2018). Pharmacoeconomics 2021; 39(6): 653–665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Riggs LM, Gould TD. Ketamine and the future of rapid-acting antidepressants. Annu Rev Clin Psychol 2021; 17: 207–231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Duman RS, Heninger GR, Nestler EJ. A molecular and cellular theory of depression. Arch Gen Psychiatry 1997; 54(7): 597–606. [DOI] [PubMed] [Google Scholar]
- 5.Rush AJ, Trivedi MH, Wisniewski SR, Nierenberg AA, Stewart JW, Warden D et al. Acute and longer-term outcomes in depressed outpatients requiring one or several treatment steps: a STAR* D report. Am J Psychiatry 2006; 163(11): 1905–1917. [DOI] [PubMed] [Google Scholar]
- 6.Gaynes BN, Lux L, Gartlehner G, Asher G, Forman-Hoffman V, Green J et al. Defining treatment-resistant depression. Depress Anxiety 2020; 37(2): 134–145. [DOI] [PubMed] [Google Scholar]
- 7.Trevino K, McClintock SM, Fischer NM, Vora A, Husain MM. Defining treatment-resistant depression: a comprehensive review of the literature. Ann Clin Psychiatry 2014; 26(3): 222–232. [PubMed] [Google Scholar]
- 8.Lewis G, Marston L, Duffy L, Freemantle N, Gilbody S, Hunter R et al. Maintenance or discontinuation of antidepressants in primary care. N Engl J Med 2021; 385(14): 1257–1267. [DOI] [PubMed] [Google Scholar]
- 9.Demyttenaere K, Enzlin P, Dewé W, Boulanger B, De Bie J, De Troyer W et al. Compliance with antidepressants in a primary care setting, 1: beyond lack of efficacy and adverse events. J Clin Psychiatry 2001; 62: 30–33. [PubMed] [Google Scholar]
- 10.Gould TD, Zarate CA Jr, Thompson SM. Molecular pharmacology and neurobiology of rapid-acting antidepressants. Annu Rev Pharmacol Toxicol 2019; 59: 213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Thompson SM. Plasticity of synapses and reward circuit function in the genesis and treatment of depression. Neuropsychopharmacology 2022: 1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Niciu MJ, Ionescu DF, Richards EM, Zarate CA. Glutamate and its receptors in the pathophysiology and treatment of major depressive disorder. J Neural Transm 2014; 121(8): 907–924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zarate CA, Singh JB, Carlson PJ, Brutsche NE, Ameli R, Luckenbaugh DA et al. A randomized trial of an N-methyl-D-aspartate antagonist in treatment-resistant major depression. Arch Gen Psychiatry 2006; 63(8): 856–864. [DOI] [PubMed] [Google Scholar]
- 14.Berman RM, Cappiello A, Anand A, Oren DA, Heninger GR, Charney DS et al. Antidepressant effects of ketamine in depressed patients. Biol Psychiatry 2000; 47(4): 351–354. [DOI] [PubMed] [Google Scholar]
- 15.Fava M, Freeman MP, Flynn M, Judge H, Hoeppner BB, Cusin C et al. Double-blind, placebo-controlled, dose-ranging trial of intravenous ketamine as adjunctive therapy in treatment-resistant depression (TRD). Mol Psychiatry 2020; 25(7): 1592–1603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Murrough JW, Perez AM, Pillemer S, Stern J, Parides MK, aan het Rot M et al. Rapid and longer-term antidepressant effects of repeated ketamine infusions in treatment-resistant major depression. Biol Psychiatry 2013; 74(4): 250–256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Abdallah CG, Sanacora G, Duman RS, Krystal JH. The neurobiology of depression, ketamine and rapid-acting antidepressants: Is it glutamate inhibition or activation? Pharmacol Ther 2018; 190: 148–158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Daly EJ, Singh JB, Fedgchin M, Cooper K, Lim P, Shelton RC et al. Efficacy and safety of intranasal esketamine adjunctive to oral antidepressant therapy in treatment-resistant depression: a randomized clinical trial. JAMA Psychiatry 2018; 75(2): 139–148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cristea IA, Naudet F. US Food and Drug Administration approval of esketamine and brexanolone. Lancet Psychiatry 2019; 6(12): 975–977. [DOI] [PubMed] [Google Scholar]
- 20.Shiroma PR, Thuras P, Wels J, Albott CS, Erbes C, Tye S et al. A randomized, double-blind, active placebo-controlled study of efficacy, safety, and durability of repeated vs single subanesthetic ketamine for treatment-resistant depression. Transl Psychiatry 2020; 10(1): 206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kryst J, Kawalec P, Mitoraj AM, Pilc A, Lasoń W, Brzostek T. Efficacy of single and repeated administration of ketamine in unipolar and bipolar depression: a meta-analysis of randomized clinical trials. Pharmacol Rep 2020; 72: 543–562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Aan Het Rot M, Collins KA, Murrough JW, Perez AM, Reich DL, Charney DS et al. Safety and efficacy of repeated-dose intravenous ketamine for treatment-resistant depression. Biol Psychiatry 2010; 67(2): 139–145. [DOI] [PubMed] [Google Scholar]
- 23.Zarate CA Jr, Singh JB, Quiroz JA, De Jesus G, Denicoff KK, Luckenbaugh DA et al. A double-blind, placebo-controlled study of memantine in the treatment of major depression. Am J Psychiatry 2006; 163(1): 153–155. [DOI] [PubMed] [Google Scholar]
- 24.Lee S-Y, Chen S-L, Chang Y-H, Chen PS, Huang S-Y, Tzeng N-S et al. Add-on memantine to valproate treatment increased HDL-C in bipolar II disorder. J Psychiatr Res 2013; 47(10): 1343–1348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Smith EG, Deligiannidis KM, Ulbricht CM, Landolin CS, Patel JK, Rothschild AJ. Antidepressant augmentation using the N-methyl-D-aspartate antagonist memantine: a randomized, double-blind, placebo-controlled trial. J Clin Psychiatry 2013; 74(10): 867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Omranifard V, Shirzadi E, Samandari S, Afshar H, Maracy MR. Memantine add on to citalopram in elderly patients with depression: A double-blind placebo-controlled study. J Res Med Sci 2014; 19(6): 525. [PMC free article] [PubMed] [Google Scholar]
- 27.Ibrahim L, DiazGranados N, Jolkovsky L, Brutsche N, Luckenbaugh DA, Herring WJ et al. A randomized, placebo-controlled, crossover pilot trial of the oral selective NR2B antagonist MK-0657 in patients with treatment-resistant major depressive disorder. J Clin Psychopharmacol 2012; 32(4): 551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Preskorn SH, Baker B, Kolluri S, Menniti FS, Krams M, Landen JW. An innovative design to establish proof of concept of the antidepressant effects of the NR2B subunit selective N-methyl-D-aspartate antagonist, CP-101,606, in patients with treatment-refractory major depressive disorder. J Clin Psychopharmacol 2008; 28(6): 631–637. [DOI] [PubMed] [Google Scholar]
- 29.Paterson B, Fraser H, Wang C, Marcus R. A randomized, double-blind, placebo-controlled, sequential parallel study of CERC-301 in the adjunctive treatment of subjects with severe depression and recent active suicidal ideation despite antidepressant treatment. Age 2015; 18: 70. [Google Scholar]
- 30.Cerecor. Cerecor Reports Top-Line Data from CERC-301 Phase 2 Study for Major Depressive Disorder. Cerecor, Inc.2016. [Google Scholar]
- 31.Park LT, Kadriu B, Gould TD, Zanos P, Greenstein D, Evans JW et al. A randomized trial of the N-methyl-d-aspartate receptor glycine site antagonist prodrug 4-chlorokynurenine in treatment-resistant depression. Int J Neuropsychopharmacol 2020; 23(7): 417–425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zarate CA Jr, Mathews D, Ibrahim L, Chaves JF, Marquardt C, Ukoh I et al. A randomized trial of a low-trapping nonselective N-methyl-D-aspartate channel blocker in major depression. Biol Psychiatry 2013; 74(4): 257–264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sanacora G, Johnson MR, Khan A, Atkinson SD, Riesenberg RR, Schronen JP et al. Adjunctive lanicemine (AZD6765) in patients with major depressive disorder and history of inadequate response to antidepressants: a randomized, placebo-controlled study. Neuropsychopharmacology 2017; 42(4): 844–853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sanacora G, Smith M, Pathak S, Su H, Boeijinga P, McCarthy D et al. Lanicemine: a low-trapping NMDA channel blocker produces sustained antidepressant efficacy with minimal psychotomimetic adverse effects. Mol Psychiatry 2014; 19(9): 978–985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Correll CU, Solmi M, Cortese S, Fava M, Højlund M, Kraemer HC et al. The future of psychopharmacology: a critical appraisal of ongoing phase 2/3 trials, and of some current trends aiming to de-risk trial programmes of novel agents. World Psychiatry 2023; 22(1): 48–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zanos P, Moaddel R, Morris PJ, Riggs LM, Highland JN, Georgiou P et al. Ketamine and ketamine metabolite pharmacology: insights into therapeutic mechanisms. Pharmacol Rev 2018; 70(3): 621–660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Krystal JH, Karper LP, Seibyl JP, Freeman GK, Delaney R, Bremner JD et al. Subanesthetic effects of the noncompetitive NMDA antagonist, ketamine, in humans: psychotomimetic, perceptual, cognitive, and neuroendocrine responses. Arch Gen Psychiatry 1994; 51(3): 199–214. [DOI] [PubMed] [Google Scholar]
- 38.Liu Y, Lin D, Wu B, Zhou W. Ketamine abuse potential and use disorder. Brain Res Bull 2016; 126: 68–73. [DOI] [PubMed] [Google Scholar]
- 39.Turner EH. Esketamine for treatment-resistant depression: seven concerns about efficacy and FDA approval. Lancet Psychiatry 2019; 6(12): 977–979. [DOI] [PubMed] [Google Scholar]
- 40.Bonaventura J, Lam S, Carlton M, Boehm MA, Gomez JL, Solís O et al. Pharmacological and behavioral divergence of ketamine enantiomers: implications for abuse liability. Mol Psychiatry 2021; 26(11): 6704–6722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Serafini G, Pompili M, Innamorati M, Dwivedi Y, Brahmachari G, Girardi P. Pharmacological properties of glutamatergic drugs targeting NMDA receptors and their application in major depression. Curr Pharm Des 2013; 19(10): 1898–1922. [DOI] [PubMed] [Google Scholar]
- 42.Newport DJ, Carpenter LL, McDonald WM, Potash JB, Tohen M, Nemeroff CB et al. Ketamine and other NMDA antagonists: early clinical trials and possible mechanisms in depression. Am J Psychiatry 2015; 172(10): 950–966. [DOI] [PubMed] [Google Scholar]
- 43.Wei Y, Chang L, Hashimoto K. Molecular mechanisms underlying the antidepressant actions of arketamine: beyond the NMDA receptor. Mol Psychiatry 2022; 27(1): 559–573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Chaki S, Watanabe M. Antidepressants in the post-ketamine Era: Pharmacological approaches targeting the glutamatergic system. Neuropharmacology 2022: 109348. [DOI] [PubMed] [Google Scholar]
- 45.Hess EM, Riggs LM, Michaelides M, Gould TD. Mechanisms of ketamine and its metabolites as antidepressants. Biochem Pharmacol 2022; 197: 114892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Zanos P, Moaddel R, Morris PJ, Georgiou P, Fischell J, Elmer GI et al. NMDAR inhibition-independent antidepressant actions of ketamine metabolites. Nature 2016; 533(7604): 481–486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lumsden EW, Troppoli TA, Myers SJ, Zanos P, Aracava Y, Kehr J et al. Antidepressant-relevant concentrations of the ketamine metabolite (2 R, 6 R)-hydroxynorketamine do not block NMDA receptor function. Proc Natl Acad Sci U S A 2019; 116(11): 5160–5169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Onisiforou A, Georgiou P, Zanos P. Role of group II metabotropic glutamate receptors in ketamine's antidepressant actions. Pharmacol Biochem Behav 2023: 173531. [DOI] [PubMed] [Google Scholar]
- 49.Witkin JM, Lippa A. Potentiation of AMPA receptors for rapid therapeutic gain in psychiatry has reached a new level of excitement. Neuropsychopharmacology: Official Publication of the American College of Neuropsychopharmacology 2023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Raison CL, Sanacora G, Woolley J, Heinzerling K, Dunlop BW, Brown RT et al. Single-Dose Psilocybin Treatment for Major Depressive Disorder: A Randomized Clinical Trial. JAMA 2023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Hebb DO. The organization of behavior: a neuropsychological theory. John Wiley & Sons: New York, NY, 1949. [Google Scholar]
- 52.Caporale N, Dan Y. Spike timing-dependent plasticity: a Hebbian learning rule. Annu Rev Neurosci 2008; 31(1): 25–46. [DOI] [PubMed] [Google Scholar]
- 53.Whitlock JR, Heynen AJ, Shuler MG, Bear MF. Learning induces long-term potentiation in the hippocampus. Science 2006; 313(5790): 1093–1097. [DOI] [PubMed] [Google Scholar]
- 54.Regehr WG. Short-term presynaptic plasticity. Cold Spring Harb Perspect Biol 2012; 4(7): a005702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Lüscher C, Malenka RC. NMDA receptor-dependent long-term potentiation and long-term depression (LTP/LTD). Cold Spring Harb Perspect Biol 2012; 4(6): a005710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Abraham WC. Metaplasticity: tuning synapses and networks for plasticity. Nat Rev Neurosci 2008; 9(5): 387–387. [DOI] [PubMed] [Google Scholar]
- 57.Nicoll RA. A brief history of long-term potentiation. Neuron 2017; 93(2): 281–290. [DOI] [PubMed] [Google Scholar]
- 58.Bliss TV, Lømo T. Long-lasting potentiation of synaptic transmission in the dentate area of the anaesthetized rabbit following stimulation of the perforant path. J Physiol 1973; 232(2): 331–356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Collingridge GL, Kehl S, McLennan Ht. Excitatory amino acids in synaptic transmission in the Schaffer collateral-commissural pathway of the rat hippocampus. J Physiol 1983; 334(1): 33–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Hollmann M, Heinemann S. Cloned glutamate receptors. Annu Rev Neurosci 1994; 17(1): 31–108. [DOI] [PubMed] [Google Scholar]
- 61.Paoletti P, Bellone C, Zhou Q. NMDA receptor subunit diversity: impact on receptor properties, synaptic plasticity and disease. Nat Rev Neurosci 2013; 14(6): 383–400. [DOI] [PubMed] [Google Scholar]
- 62.Mayer ML, Westbrook GL, Guthrie PB. Voltage-dependent block by Mg2+ of NMDA responses in spinal cord neurones. Nature 1984; 309(5965): 261–263. [DOI] [PubMed] [Google Scholar]
- 63.Nabavi S, Fox R, Proulx CD, Lin JY, Tsien RY, Malinow R. Engineering a memory with LTD and LTP. Nature 2014; 511(7509): 348–352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Lisman J, Schulman H, Cline H. The molecular basis of CaMKII function in synaptic and behavioural memory. Nat Rev Neurosci 2002; 3(3): 175–190. [DOI] [PubMed] [Google Scholar]
- 65.Herring BE, Nicoll RA. Long-term potentiation: from CaMKII to AMPA receptor trafficking. Annu Rev Physiol 2016; 78: 351–365. [DOI] [PubMed] [Google Scholar]
- 66.Derkach V, Barria A, Soderling TR. Ca2+/calmodulin-kinase II enhances channel conductance of α-amino-3-hydroxy-5-methyl-4-isoxazolepropionate type glutamate receptors. Proc Natl Acad Sci U S A 1999; 96(6): 3269–3274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Barria A, Muller D, Derkach V, Griffith LC, Soderling TR. Regulatory phosphorylation of AMPA-type glutamate receptors by CaM-KII during long-term potentiation. Science 1997; 276(5321): 2042–2045. [DOI] [PubMed] [Google Scholar]
- 68.Mammen AL, Kameyama K, Roche KW, Huganir RL. Phosphorylation of the α-amino-3-hydroxy-5-methylisoxazole4-propionic acid receptor GluR1 subunit by calcium/calmodulin-dependent kinase II. J Biol Chem 1997; 272(51): 32528–32533. [DOI] [PubMed] [Google Scholar]
- 69.Benke TA, Lüthi A, Isaac JT, Collingridge GL. Modulation of AMPA receptor unitary conductance by synaptic activity. Nature 1998; 393(6687): 793–797. [DOI] [PubMed] [Google Scholar]
- 70.Ehlers MD. Reinsertion or degradation of AMPA receptors determined by activity-dependent endocytic sorting. Neuron 2000; 28(2): 511–525. [DOI] [PubMed] [Google Scholar]
- 71.Boehm J, Kang M-G, Johnson RC, Esteban J, Huganir RL, Malinow R. Synaptic incorporation of AMPA receptors during LTP is controlled by a PKC phosphorylation site on GluR1. Neuron 2006; 51(2): 213–225. [DOI] [PubMed] [Google Scholar]
- 72.Esteban JA, Shi S-H, Wilson C, Nuriya M, Huganir RL, Malinow R. PKA phosphorylation of AMPA receptor subunits controls synaptic trafficking underlying plasticity. Nat Neurosci 2003; 6(2): 136–143. [DOI] [PubMed] [Google Scholar]
- 73.Matsuzaki M, Honkura N, Ellis-Davies GC, Kasai H. Structural basis of long-term potentiation in single dendritic spines. Nature 2004; 429(6993): 761–766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Harvey CD, Yasuda R, Zhong H, Svoboda K. The spread of Ras activity triggered by activation of a single dendritic spine. Science 2008; 321(5885): 136–140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Abraham WC, Williams JM. LTP maintenance and its protein synthesis-dependence. Neurobiol Learn Mem 2008; 89(3): 260–268. [DOI] [PubMed] [Google Scholar]
- 76.Vickers CA, Dickson KS, Wyllie DJA. Induction and maintenance of late-phase long-term potentiation in isolated dendrites of rat hippocampal CA1 pyramidal neurones. J Physiol 2005; 568(3): 803–813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Chetkovich DM, Sweatt JD. NMDA receptor activation increases cyclic AMP in area CA1 of the hippocampus via calcium/calmodulin stimulation of adenylyl cyclase. J Neurochem 1993; 61(5): 1933–1942. [DOI] [PubMed] [Google Scholar]
- 78.Nguyen PV, Kandel ER. Brief theta-burst stimulation induces a transcription-dependent late phase of LTP requiring cAMP in area CA1 of the mouse hippocampus. Learn Mem 1997; 4(2): 230–243. [DOI] [PubMed] [Google Scholar]
- 79.Sun P, Enslen H, Myung PS, Maurer RA. Differential activation of CREB by Ca2+/calmodulin-dependent protein kinases type II and type IV involves phosphorylation of a site that negatively regulates activity. Genes Dev 1994; 8(21): 2527–2539. [DOI] [PubMed] [Google Scholar]
- 80.Ofir R, Dwarki V, Rashid D, Verma IM. CREB represses transcription of fos promoter: role of phosphorylation. Gene Expr 1991; 1(1): 55–60. [PMC free article] [PubMed] [Google Scholar]
- 81.Lee Y-S, Silva AJ. The molecular and cellular biology of enhanced cognition. Nat Rev Neurosci 2009; 10(2): 126–140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Toni N, Buchs P-A, Nikonenko I, Bron C, Muller D. LTP promotes formation of multiple spine synapses between a single axon terminal and a dendrite. Nature 1999; 402(6760): 421–425. [DOI] [PubMed] [Google Scholar]
- 83.Kasai H, Fukuda M, Watanabe S, Hayashi-Takagi A, Noguchi J. Structural dynamics of dendritic spines in memory and cognition. Trends Neurosci 2010; 33(3): 121–129. [DOI] [PubMed] [Google Scholar]
- 84.Panja D, Bramham CR. BDNF mechanisms in late LTP formation: a synthesis and breakdown. Neuropharmacology 2014; 76: 664–676. [DOI] [PubMed] [Google Scholar]
- 85.Collingridge GL, Peineau S, Howland JG, Wang YT. Long-term depression in the CNS. Nat Rev Neurosci 2010; 11(7): 459–473. [DOI] [PubMed] [Google Scholar]
- 86.Lisman J. A mechanism for the Hebb and the anti-Hebb processes underlying learning and memory. Proc Natl Acad Sci U S A 1989; 86(23): 9574–9578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Carroll RC, Beattie EC, Von Zastrow M, Malenka RC. Role of AMPA receptor endocytosis in synaptic plasticity. Nat Rev Neurosci 2001; 2(5): 315–324. [DOI] [PubMed] [Google Scholar]
- 88.Mulkey RM, Endo S, Shenolikar S, Malenka RC. Involvement of a calcineurin/inhibitor-1 phosphatase cascade in hippocampal long-term depression. Nature 1994; 369(6480): 486–488. [DOI] [PubMed] [Google Scholar]
- 89.Lüscher C, Xia H, Beattie EC, Carroll RC, von Zastrow M, Malenka RC et al. Role of AMPA receptor cycling in synaptic transmission and plasticity. Neuron 1999; 24(3): 649–658. [DOI] [PubMed] [Google Scholar]
- 90.Nägerl UV, Eberhorn N, Cambridge SB, Bonhoeffer T. Bidirectional activity-dependent morphological plasticity in hippocampal neurons. Neuron 2004; 44(5): 759–767. [DOI] [PubMed] [Google Scholar]
- 91.Zhou Q, Homma KJ, Poo M-m. Shrinkage of dendritic spines associated with long-term depression of hippocampal synapses. Neuron 2004; 44(5): 749–757. [DOI] [PubMed] [Google Scholar]
- 92.Huang Y-Y, Colino A, Selig DK, Malenka RC. The influence of prior synaptic activity on the induction of long-term potentiation. Science 1992; 255(5045): 730–733. [DOI] [PubMed] [Google Scholar]
- 93.Abraham WC, Bear MF. Metaplasticity: the plasticity of synaptic plasticity. Trends Neurosci 1996; 19(4): 126–130. [DOI] [PubMed] [Google Scholar]
- 94.Cooper LN, Bear MF. The BCM theory of synapse modification at 30: interaction of theory with experiment. Nat Rev Neurosci 2012; 13(11): 798–810. [DOI] [PubMed] [Google Scholar]
- 95.He H-Y, Ray B, Dennis K, Quinlan EM. Experience-dependent recovery of vision following chronic deprivation amblyopia. Nat Neurosci 2007; 10(9): 1134–1136. [DOI] [PubMed] [Google Scholar]
- 96.Abraham WC, Mason-Parker SE, Bear MF, Webb S, Tate WP. Heterosynaptic metaplasticity in the hippocampus in vivo: a BCM-like modifiable threshold for LTP. Proc Natl Acad Sci U S A 2001; 98(19): 10924–10929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Buschler A, Manahan-Vaughan D. Brief environmental enrichment elicits metaplasticity of hippocampal synaptic potentiation in vivo. Front Behav Neurosci 2012; 6: 85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Keralapurath MM, Clark JK, Hammond S, Wagner JJ. Cocaine-or stress-induced metaplasticity of LTP in the dorsal and ventral hippocampus. Hippocampus 2014; 24(5): 577–590. [DOI] [PubMed] [Google Scholar]
- 99.Zelcer I, Cohen H, Richter-Levin G, Lebiosn T, Grossberger T, Barkai E. A cellular correlate of learning-induced metaplasticity in the hippocampus. Cereb Cortex 2006; 16(4): 460–468. [DOI] [PubMed] [Google Scholar]
- 100.Shen H, Moussawi K, Zhou W, Toda S, Kalivas PW. Heroin relapse requires long-term potentiation-like plasticity mediated by NMDA2b-containing receptors. Proc Natl Acad Sci U S A 2011; 108(48): 19407–19412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Maggio N, Segal M. Persistent changes in ability to express long-term potentiation/depression in the rat hippocampus after juvenile/adult stress. Biol Psychiatry 2011; 69(8): 748–753. [DOI] [PubMed] [Google Scholar]
- 102.Satoshi F, Yoichiro K, Masami M, Hidekazu F, Hiroshi S, Kenya K et al. The long-term suppressive effect of prior activation of synaptic inputs by low-frequency stimulation on induction of long-term potentiation in CA1 neurons of guinea pig hippocampal slices. Exp Brain Res 1996; 111: 305–312. [PubMed] [Google Scholar]
- 103.Abraham WC, Huggett A. Induction and reversal of long-term potentiation by repeated high-frequency stimulation in rat hippocampal slices. Hippocampus 1997; 7(2): 137–145. [DOI] [PubMed] [Google Scholar]
- 104.Hulme SR, Jones OD, Abraham WC. Emerging roles of metaplasticity in behaviour and disease. Trends Neurosci 2013; 36(6): 353–362. [DOI] [PubMed] [Google Scholar]
- 105.Holland LL, Wagner JJ. Primed facilitation of homosynaptic long-term depression and depotentiation in rat hippocampus. J Neurosci 1998; 18(3): 887–894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Nasarudeen R, Singh A, Rana ZS, Punnakkal P. Epileptiform activity induced metaplasticity impairs bidirectional plasticity in the hippocampal CA1 synapses via GluN2B NMDA receptors. Exp Brain Res 2022: 1–11. [DOI] [PubMed] [Google Scholar]
- 107.Fava M, Kendler KS. Major depressive disorder. Neuron 2000; 28(2): 335–341. [DOI] [PubMed] [Google Scholar]
- 108.Krishnan V, Nestler EJ. Animal models of depression: molecular perspectives. Curr Top Behav Neurosci 2011: 121–147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Segal M, Richter-Levin G, Maggio N. Stress-induced dynamic routing of hippocampal connectivity: A hypothesis. Hippocampus 2010; 20(12): 1332–1338. [DOI] [PubMed] [Google Scholar]
- 110.Maggio N, Segal M. Striking variations in corticosteroid modulation of long-term potentiation along the septotemporal axis of the hippocampus. J Neurosci 2007; 27(21): 5757–5765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Li S, Jin M, Koeglsperger T, Shepardson NE, Shankar GM, Selkoe DJ. Soluble Aβ oligomers inhibit long-term potentiation through a mechanism involving excessive activation of extrasynaptic NR2B-containing NMDA receptors. J Neurosci 2011; 31(18): 6627–6638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Rönicke R, Mikhaylova M, Rönicke S, Meinhardt J, Schröder UH, Fändrich M et al. Early neuronal dysfunction by amyloid β oligomers depends on activation of NR2B-containing NMDA receptors. Neurobiol Aging 2011; 32(12): 2219–2228. [DOI] [PubMed] [Google Scholar]
- 113.Preston CJ, Brown KA, Wagner JJ. Cocaine conditioning induces persisting changes in ventral hippocampus synaptic transmission, long-term potentiation, and radial arm maze performance in the mouse. Neuropharmacology 2019; 150: 27–37. [DOI] [PubMed] [Google Scholar]
- 114.Chiamulera C, Piva A, Abraham WC. Glutamate receptors and metaplasticity in addiction. Curr Opin Pharmacol 2021; 56: 39–45. [DOI] [PubMed] [Google Scholar]
- 115.Castrén E. Neuronal network plasticity and recovery from depression. JAMA Psychiatry 2013; 70(9): 983–989. [DOI] [PubMed] [Google Scholar]
- 116.Sanacora G, Treccani G, Popoli M. Towards a glutamate hypothesis of depression: an emerging frontier of neuropsychopharmacology for mood disorders. Neuropharmacology 2012; 62(1): 63–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Thompson SM, Kallarackal AJ, Kvarta MD, Van Dyke AM, LeGates TA, Cai X. An excitatory synapse hypothesis of depression. Trends Neurosci 2015; 38(5): 279–294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Domino EF, Chodoff P, Corssen G. Pharmacologic effects of CI-581, a new dissociative anesthetic, in man. Clin Pharmacol Ther 1965; 6(3): 279–291. [DOI] [PubMed] [Google Scholar]
- 119.Domino EF, Warner DS. Taming the ketamine tiger. Anesthesiology 2010; 113(3): 678–684. [DOI] [PubMed] [Google Scholar]
- 120.Maeng S, Zarate CA Jr, Du J, Schloesser RJ, McCammon J, Chen G et al. Cellular mechanisms underlying the antidepressant effects of ketamine: role of α-amino-3-hydroxy-5-methylisoxazole-4-propionic acid receptors. Biol Psychiatry 2008; 63(4): 349–352. [DOI] [PubMed] [Google Scholar]
- 121.Zanos P, Gould T. Mechanisms of ketamine action as an antidepressant. Mol Psychiatry 2018; 23(4): 801–811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Dravid SM, Erreger K, Yuan H, Nicholson K, Le P, Lyuboslavsky P et al. Subunit-specific mechanisms and proton sensitivity of NMDA receptor channel block. J Physiol 2007; 581(1): 107–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Kotermanski SE, Johnson JW. Mg2+ imparts NMDA receptor subtype selectivity to the Alzheimer's drug memantine. J Neurosci 2009; 29(9): 2774–2779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Yamakura T, Mori H, Masaki H, Shimoji K, Mishina M. Different sensitivities of NMDA receptor channel subtypes to non-competitive antagonists. Neuroreport 1993; 4(6): 687–690. [DOI] [PubMed] [Google Scholar]
- 125.Quinlan EM, Olstein DH, Bear MF. Bidirectional, experience-dependent regulation of N-methyl-D-aspartate receptor subunit composition in the rat visual cortex during postnatal development. Proc Natl Acad Sci U S A 1999; 96(22): 12876–12880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Quinlan EM, Philpot BD, Huganir RL, Bear MF. Rapid, experience-dependent expression of synaptic NMDA receptors in visual cortex in vivo. Nat Neurosci 1999; 2(4): 352–357. [DOI] [PubMed] [Google Scholar]
- 127.Frenkel MY, Bear MF. How monocular deprivation shifts ocular dominance in visual cortex of young mice. Neuron 2004; 44(6): 917–923. [DOI] [PubMed] [Google Scholar]
- 128.Chen WS, Bear MF. Activity-dependent regulation of NR2B translation contributes to metaplasticity in mouse visual cortex. Neuropharmacology 2007; 52(1): 200–214. [DOI] [PubMed] [Google Scholar]
- 129.Cho KK, Bear MF. Promoting neurological recovery of function via metaplasticity. Future Neurol 2010; 5(1): 21–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Philpot BD, Cho KK, Bear MF. Obligatory role of NR2A for metaplasticity in visual cortex. Neuron 2007; 53(4): 495–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Piva A, Caffino L, Mottarlini F, Pintori N, Castillo Díaz F, Fumagalli F et al. Metaplastic effects of ketamine and MK-801 on glutamate receptors expression in rat medial prefrontal cortex and hippocampus. Mol Neurobiol 2021; 58: 3443–3456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Gerhard DM, Pothula S, Liu R-J, Wu M, Li X-Y, Girgenti MJ et al. GABA interneurons are the cellular trigger for ketamine’s rapid antidepressant actions. J Clin Invest 2020; 130(3): 1336–1349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Pothula S, Kato T, Liu R-J, Wu M, Gerhard D, Shinohara R et al. Cell-type specific modulation of NMDA receptors triggers antidepressant actions. Mol Psychiatry 2021; 26(9): 5097–5111. [DOI] [PubMed] [Google Scholar]
- 134.Qin Y, Guo X, Song W, Liang Z, Wang Y, Feng D et al. Antidepressant-like effect of CP-101,606: Evidence of mTOR pathway activation. Mol Cell Neurosci 2023; 124: 103821. [DOI] [PubMed] [Google Scholar]
- 135.Graef JD, Newberry K, Newton A, Pieschl R, Shields E, Luan F-n et al. Effect of acute NR2B antagonist treatment on long-term potentiation in the rat hippocampus. Brain Res 2015; 1609: 31–39. [DOI] [PubMed] [Google Scholar]
- 136.Rocha B, Ward A, Egilmez Y, Lytle D, Emmett-Oglesby M. Tolerance to the discriminative stimulus and reinforcing effects of ketamine. Behav Pharmacol 1996; 7(2): 160–168. [PubMed] [Google Scholar]
- 137.Yang C, Shirayama Y, Zhang J, Ren Q, Yao W, Ma M et al. R-ketamine: a rapid-onset and sustained antidepressant without psychotomimetic side effects. Transl Psychiatry 2015; 5(9): e632–e632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Zhang J-C, Li S-X, Hashimoto K. R (−)-ketamine shows greater potency and longer lasting antidepressant effects than S (+)-ketamine. Pharmacol Biochem Behav 2014; 116: 137–141. [DOI] [PubMed] [Google Scholar]
- 139.Zanos P, Brown KA, Georgiou P, Yuan P, Zarate CA, Thompson SM et al. NMDA Receptor Activation-Dependent Antidepressant-Relevant Behavioral and Synaptic Actions of Ketamine. J Neurosci 2023; 43(6): 1038–1050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Kim J-W, Monteggia LM. Increasing doses of ketamine curtail antidepressant responses and suppress associated synaptic signaling pathways. Behav Brain Res 2020; 380: 112378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Izumi Y, Zorumski CF. Metaplastic effects of subanesthetic ketamine on CA1 hippocampal function. Neuropharmacology 2014; 86: 273–281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Izumi Y, Hsu FF, Conway CR, Nagele P, Mennerick SJ, Zorumski CF. Nitrous Oxide, a Rapid Antidepressant, Has Ketamine-like Effects on Excitatory Transmission in the Adult Hippocampus. Biol Psychiatry 2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Ballard ED, Zarate CA Jr. The role of dissociation in ketamine’s antidepressant effects. Nat Commun 2020; 11(1): 6431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Burgdorf J, Zhang X-l, Nicholson KL, Balster RL, David Leander J, Stanton PK et al. GLYX-13, a NMDA receptor glycine-site functional partial agonist, induces antidepressant-like effects without ketamine-like side effects. Neuropsychopharmacology 2013; 38(5): 729–742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Widman AJ, Stewart AE, Erb EM, Gardner E, McMahon LL. Intravascular ketamine increases theta-burst but not high frequency tetanus induced LTP at CA3-CA1 synapses within three hours and devoid of an increase in spine density. Front Synaptic Neurosci 2018; 10: 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Yang Y, Ju W, Zhang H, Sun L. Effect of ketamine on LTP and NMDAR EPSC in hippocampus of the chronic social defeat stress mice model of depression. Front Behav Neurosci 2018; 12: 229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Aleksandrova LR, Wang YT, Phillips AG. Ketamine and its metabolite,(2R, 6R)-HNK, restore hippocampal LTP and long-term spatial memory in the Wistar-Kyoto rat model of depression. Mol Brain 2020; 13(1): 1–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Belujon P, Grace AA. Restoring mood balance in depression: ketamine reverses deficit in dopamine-dependent synaptic plasticity. Biol Psychiatry 2014; 76(12): 927–936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Aleksandrova LR, Wang YT, Phillips AG. Evaluation of the Wistar-Kyoto rat model of depression and the role of synaptic plasticity in depression and antidepressant response. Neurosci Biobehav Rev 2019; 105: 1–23. [DOI] [PubMed] [Google Scholar]
- 150.Zhu X, Zhang F, You Y, Wang H, Yuan S, Wu B et al. S-ketamine exerts antidepressant effects by regulating Rac1 GTPase mediated synaptic plasticity in the hippocampus of stressed rats. Cell Mol Neurobiol 2023; 43(1): 299–314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Pałucha-Poniewiera A, Bobula B, Rafało-Ulińska A. The Antidepressant-like Activity and Cognitive Enhancing Effects of the Combined Administration of (R)-Ketamine and LY341495 in the CUMS Model of Depression in Mice Are Related to the Modulation of Excitatory Synaptic Transmission and LTP in the PFC. Pharmaceuticals 2023; 16(2): 288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Yao N, Skiteva O, Zhang X, Svenningsson P, Chergui K. Ketamine and its metabolite (2R, 6R)-hydroxynorketamine induce lasting alterations in glutamatergic synaptic plasticity in the mesolimbic circuit. Mol Psychiatry 2018; 23(10): 2066–2077. [DOI] [PubMed] [Google Scholar]
- 153.Skiteva O, Yao N, Chergui K. Ketamine induces opposite changes in AMPA receptor calcium permeability in the ventral tegmental area and nucleus accumbens. Transl Psychiatry 2021; 11(1): 530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Zorumski CF, Izumi Y. NMDA receptors and metaplasticity: mechanisms and possible roles in neuropsychiatric disorders. Neurosci Biobehav Rev 2012; 36(3): 989–1000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Huang C-C, Wei I-H, Huang C-L, Chen K-T, Tsai M-H, Tsai P et al. Inhibition of glycine transporter-I as a novel mechanism for the treatment of depression. Biol Psychiatry 2013; 74(10): 734–741. [DOI] [PubMed] [Google Scholar]
- 156.Khan MA, Houck DR, Gross AL, Zhang X-l, Cearley C, Madsen TM et al. NYX-2925 is a novel NMDA receptor-specific spirocyclic-β-lactam that modulates synaptic plasticity processes associated with learning and memory. Int J Neuropsychopharmacol 2018; 21(3): 242–254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Burgdorf JS, Christian E, Sørensen L, Stanton PK, Leaderbrand K, Madsen T et al. A translational EEG-based approach to assess modulation of long-lasting NMDAR-dependent synaptic plasticity. Psychopharmacology (Berl) 2019; 236: 3687–3693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Donello JE, Banerjee P, Li Y-X, Guo Y-X, Yoshitake T, Zhang X-L et al. Positive N-methyl-D-aspartate receptor modulation by rapastinel promotes rapid and sustained antidepressant-like effects. Int J Neuropsychopharmacol 2019; 22(3): 247–259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Moskal JR, Burch R, Burgdorf JS, Kroes RA, Stanton PK, Disterhoft JF et al. GLYX-13, an NMDA receptor glycine site functional partial agonist enhances cognition and produces antidepressant effects without the psychotomimetic side effects of NMDA receptor antagonists. Expert Opin Investig Drugs 2014; 23(2): 243–254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Pothula S, Liu R-J, Wu M, Sliby A-N, Picciotto MR, Banerjee P et al. Positive modulation of NMDA receptors by AGN-241751 exerts rapid antidepressant-like effects via excitatory neurons. Neuropsychopharmacology 2021; 46(4): 799–808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Shen M, Lv D, Liu X, Wang C. ERK/mTOR signaling may underlying the antidepressant actions of rapastinel in mice. Transl Psychiatry 2022; 12(1): 522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Burgdorf J, Zhang X-L, Weiss C, Gross A, Boikess SR, Kroes RA et al. The long-lasting antidepressant effects of rapastinel (GLYX-13) are associated with a metaplasticity process in the medial prefrontal cortex and hippocampus. Neuroscience 2015; 308: 202–211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Zhang X-l Sullivan JA, Moskal JR Stanton PK. A NMDA receptor glycine site partial agonist, GLYX-13, simultaneously enhances LTP and reduces LTD at Schaffer collateral–CA1 synapses in hippocampus. Neuropharmacology 2008; 55(7): 1238–1250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Preskorn S, Macaluso M, ZAMMIT G, MOSKAL JR, BURCH RM, Group G-CS. Randomized proof of concept trial of GLYX-13, an N-methyl-D-aspartate receptor glycine site partial agonist, in major depressive disorder nonresponsive to a previous antidepressant agent. J Psychiatr Pract 2015; 21(2): 140–149. [DOI] [PubMed] [Google Scholar]
- 165.Kato T, Duman RS. Rapastinel, a novel glutamatergic agent with ketamine-like antidepressant actions: convergent mechanisms. Pharmacol Biochem Behav 2020; 188: 172827. [DOI] [PubMed] [Google Scholar]
- 166.Burgdorf JS, Zhang X-L, Stanton PK, Moskal JR, Donello JE. Zelquistinel is an orally bioavailable novel NMDA receptor allosteric modulator that exhibits rapid and sustained antidepressant-like effects. Int J Neuropsychopharmacol 2022; 25(12): 979–991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Bienenstock EL, Cooper LN, Munro PW. Theory for the development of neuron selectivity: orientation specificity and binocular interaction in visual cortex. J Neurosci 1982; 2(1): 32–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Xu Y, Yu Z, Chen S, Li Z, Long X, Chen M et al. (2R, 6R)-hydroxynorketamine targeting the basolateral amygdala regulates fear memory. Neuropharmacology 2023: 109402. [DOI] [PubMed] [Google Scholar]
- 169.Morris PJ, Moaddel R, Zanos P, Moore CE, Gould T, Zarate CA Jr et al. Synthesis and N-methyl-d-aspartate (NMDA) receptor activity of ketamine metabolites. Org Lett 2017; 19(17): 4572–4575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Riggs LM, Aracava Y, Zanos P, Fischell J, Albuquerque EX, Pereira EF et al. (2R, 6R)-hydroxynorketamine rapidly potentiates hippocampal glutamatergic transmission through a synapse-specific presynaptic mechanism. Neuropsychopharmacology 2020; 45(2): 426–436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Moaddel R, Abdrakhmanova G, Kozak J, Jozwiak K, Toll L, Jimenez L et al. Sub-anesthetic concentrations of (R, S)-ketamine metabolites inhibit acetylcholine-evoked currents in α7 nicotinic acetylcholine receptors. Eur J Pharmacol 2013; 698(1-3): 228–234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Suzuki K, Nosyreva E, Hunt KW, Kavalali ET, Monteggia LM. Effects of a ketamine metabolite on synaptic NMDAR function. Nature 2017; 546(7659): E1–E3. [DOI] [PubMed] [Google Scholar]
- 173.Pham TH, Defaix C, Xu X, Deng S-X, Fabresse N, Alvarez J-C et al. Common neurotransmission recruited in (R, S)-ketamine and (2R, 6R)-hydroxynorketamine–induced sustained antidepressant-like effects. Biol Psychiatry 2018; 84(1): e3–e6. [DOI] [PubMed] [Google Scholar]
- 174.Chou D, Peng H-Y, Lin T-B, Lai C-Y, Hsieh M-C, Wen Y-C et al. (2R, 6R)-hydroxynorketamine rescues chronic stress-induced depression-like behavior through its actions in the midbrain periaqueductal gray. Neuropharmacology 2018; 139: 1–12. [DOI] [PubMed] [Google Scholar]
- 175.Ye L, Ko C-Y, Huang Y, Zheng C, Zheng Y, Chou D. Ketamine metabolite (2R, 6R)-hydroxynorketamine enhances aggression via periaqueductal gray glutamatergic transmission. Neuropharmacology 2019; 157: 107667. [DOI] [PubMed] [Google Scholar]
- 176.Riggs LM, Thompson SM, Gould TD. (2R, 6R)-hydroxynorketamine rapidly potentiates optically-evoked Schaffer collateral synaptic activity. Neuropharmacology 2022: 109153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Fukumoto K, Fogaça MV, Liu R-J, Duman C, Kato T, Li X-Y et al. Activity-dependent brain-derived neurotrophic factor signaling is required for the antidepressant actions. Proc Natl Acad Sci U S A 2019; 116(1): 297–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Chaki S, Yoshikawa R, Hirota S, Shimazaki T, Maeda M, Kawashima N et al. MGS0039: a potent and selective group II metabotropic glutamate receptor antagonist with antidepressant-like activity. Neuropharmacology 2004; 46(4): 457–467. [DOI] [PubMed] [Google Scholar]
- 179.Dwyer JM, Lepack AE, Duman RS. mTOR activation is required for the antidepressant effects of mGluR2/3 blockade. Int J Neuropsychopharmacol 2012; 15(4): 429–434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Zanos P, Highland JN, Stewart BW, Georgiou P, Jenne CE, Lovett J et al. (2R, 6R)-hydroxynorketamine exerts mGlu2 receptor-dependent antidepressant actions. Proc Natl Acad Sci U S A 2019; 116(13): 6441–6450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Witkin J, Mitchell S, Wafford K, Carter G, Gilmour G, Li J et al. Comparative effects of LY3020371, a potent and selective metabotropic glutamate (mGlu) 2/3 receptor antagonist, and ketamine, a noncompetitive N-Methyl-d-Aspartate receptor antagonist in rodents: evidence supporting the use of mGlu2/3 antagonists, for the treatment of depression. J Pharmacol Exp Ther 2017; 361(1): 68–86. [DOI] [PubMed] [Google Scholar]
- 182.Chin C-L, Upadhyay J, Marek GJ, Baker SJ, Zhang M, Mezler M et al. Awake rat pharmacological magnetic resonance imaging as a translational pharmacodynamic biomarker: metabotropic glutamate 2/3 agonist modulation of ketamine-induced blood oxygenation level dependence signals. J Pharmacol Exp Ther 2011; 336(3): 709–715. [DOI] [PubMed] [Google Scholar]
- 183.Wyckhuys T, Langlois X, Schmidt M, Stroobants S, Staelens S. The [18F] FDG μPET readout of a brain activation model to evaluate the metabotropic glutamate receptor 2 positive allosteric modulator JNJ-42153605. J Pharmacol Exp Ther 2014; 350(2): 375–386. [DOI] [PubMed] [Google Scholar]
- 184.Lepack AE, Bang E, Lee B, Dwyer JM, Duman RS. Fast-acting antidepressants rapidly stimulate ERK signaling and BDNF release in primary neuronal cultures. Neuropharmacology 2016; 111: 242–252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Karasawa J-i, Shimazaki T, Kawashima N, Chaki S. AMPA receptor stimulation mediates the antidepressant-like effect of a group II metabotropic glutamate receptor antagonist. Brain Res 2005; 1042(1): 92–98. [DOI] [PubMed] [Google Scholar]
- 186.Koike H, Chaki S. Requirement of AMPA receptor stimulation for the sustained antidepressant activity of ketamine and LY341495 during the forced swim test in rats. Behav Brain Res 2014; 271: 111–115. [DOI] [PubMed] [Google Scholar]
- 187.Dong C, Zhang J-c, Yao W, Ren Q, Ma M, Yang C et al. Rapid and sustained antidepressant action of the mGlu2/3 receptor antagonist MGS0039 in the social defeat stress model: comparison with ketamine. Int J Neuropsychopharmacol 2017; 20(3): 228–236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Koike H, Fukumoto K, Iijima M, Chaki S. Role of BDNF/TrkB signaling in antidepressant-like effects of a group II metabotropic glutamate receptor antagonist in animal models of depression. Behav Brain Res 2013; 238: 48–52. [DOI] [PubMed] [Google Scholar]
- 189.Huang Y-Z, Chen R-S, Rothwell JC, Wen H-Y. The after-effect of human theta burst stimulation is NMDA receptor dependent. Clin Neurophysiol 2007; 118(5): 1028–1032. [DOI] [PubMed] [Google Scholar]
- 190.Ren L, Hao X, Min S, Deng J, Chen Q, Chen H et al. Anesthetics alleviate learning and memory impairment induced by electroconvulsive shock by regulation of NMDA receptor-mediated metaplasticity in depressive rats. Neurobiol Learn Mem 2018; 155: 65–77. [DOI] [PubMed] [Google Scholar]
- 191.Reid IC, Stewart CA. Seizures, memory and synaptic plasticity. Seizure 1997; 6(5): 351–359. [DOI] [PubMed] [Google Scholar]
- 192.Li M, Yao X, Sun L, Zhao L, Xu W, Zhao H et al. Effects of electroconvulsive therapy on depression and its potential mechanism. Front Psychol 2020; 11: 80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Stewart CA, Reid IC. Ketamine prevents ECS-induced synaptic enhancement in rat hippocampus. Neurosci Lett 1994; 178(1): 11–14. [DOI] [PubMed] [Google Scholar]
- 194.Chen AC-H, Shin K-H, Duman RS, Sanacora G. ECS-induced mossy fiber sprouting and BDNF expression are attenuated by ketamine pretreatment. J ECT 2001; 17(1): 27–32. [DOI] [PubMed] [Google Scholar]
- 195.Wilkinson ST, Rhee TG, Joormann J, Webler R, Ortiz Lopez M, Kitay B et al. Cognitive behavioral therapy to sustain the antidepressant effects of ketamine in treatment-resistant depression: a randomized clinical trial. Psychother Psychosom 2021; 90(5): 318–327. [DOI] [PubMed] [Google Scholar]
- 196.Drozdz SJ, Goel A, McGarr MW, Katz J, Ritvo P, Mattina GF et al. Ketamine assisted psychotherapy: a systematic narrative review of the literature. J Pain Res 2022: 1691–1706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Tatti E, Phillips AL, Paciorek R, Romanella SM, Dettore D, Di Lorenzo G et al. Boosting psychological change: combining non-invasive brain stimulation with psychotherapy. Neurosci Biobehav Rev 2022: 104867. [DOI] [PubMed] [Google Scholar]
- 198.Zhang J, Tian H, Li J, Ji S, Chen S, Zhu J et al. Ketamine plus propofol-electroconvulsive therapy (ECT) transiently improves the antidepressant effects and the associated brain functional alterations in patients with propofol-ECT-resistant depression. Psychiatry Res 2020; 287: 112907. [DOI] [PubMed] [Google Scholar]
- 199.Altinay M, Karne H, Anand A. Administration of sub-anesthetic dose of ketamine and electroconvulsive treatment on alternate week days in patients with treatment resistant depression: a double blind placebo controlled trial. Psychopharmacol Bull 2019; 49(1): 8. [PMC free article] [PubMed] [Google Scholar]
- 200.Wrightson JG, Cole J, Sohn MN, McGirr A. The effects of D-Cycloserine on corticospinal excitability after repeated spaced intermittent theta-burst transcranial magnetic stimulation: A randomized controlled trial in healthy individuals. Neuropsychopharmacology 2023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Brown JC, DeVries WH, Korte JE, Sahlem GL, Bonilha L, Short EB et al. NMDA receptor partial agonist, d-cycloserine, enhances 10 Hz rTMS-induced motor plasticity, suggesting long-term potentiation (LTP) as underlying mechanism. Brain Stimul 2020; 13(3): 530–532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Cole J, Selby B, Ismail Z, McGirr A. D-cycloserine normalizes long-term motor plasticity after transcranial magnetic intermittent theta-burst stimulation in major depressive disorder. Clin Neurophysiol 2021; 132(8): 1770–1776. [DOI] [PubMed] [Google Scholar]
- 203.Cole J, Sohn MN, Harris AD, Bray SL, Patten SB, McGirr A. Efficacy of adjunctive D-cycloserine to intermittent theta-burst stimulation for major depressive disorder: A randomized clinical trial. JAMA Psychiatry 2022; 79(12): 1153–1161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Reardon S. Depression researchers rethink mouse swim test. Nature 2019; 571(7766): 456–457. [DOI] [PubMed] [Google Scholar]
- 205.Kim J-W, Autry AE, Na ES, Adachi M, Björkholm C, Kavalali ET et al. Sustained effects of rapidly acting antidepressants require BDNF-dependent MeCP2 phosphorylation. Nat Neurosci 2021; 24(8): 1100–1109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Nardou R, Sawyer E, Song YJ, Wilkinson M, Padovan-Hernandez Y, de Deus JL et al. Psychedelics reopen the social reward learning critical period. Nature 2023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Nayak S, Johnson MW. Psychedelics and psychotherapy. Pharmacopsychiatry 2021; 54(04): 167–175. [DOI] [PubMed] [Google Scholar]
- 208.Oh MM, Kuo AG, Wu WW, Sametsky EA, Disterhoft JF. Watermaze learning enhances excitability of CA1 pyramidal neurons. J Neurophysiol 2003; 90(4): 2171–2179. [DOI] [PubMed] [Google Scholar]
- 209.Moyer JR Jr, Thompson LT, Disterhoft JF. Trace eyeblink conditioning increases CA1 excitability in a transient and learning-specific manner. J Neurosci 1996; 16(17): 5536–5546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Scangos KW, State MW, Miller AH, Baker JT, Williams LM. New and emerging approaches to treat psychiatric disorders. Nat Med 2023: 1–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Zanos P, Nelson ME, Highland JN, Krimmel SR, Georgiou P, Gould TD et al. A negative allosteric modulator for alpha5 subunit-containing GABA receptors exerts a rapid and persistent antidepressant-like action without the side effects of the NMDA receptor antagonist ketamine in mice. eNeuro 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Chaki S, Watanabe M. mGlu2/3 receptor antagonists for depression: overview of underlying mechanisms and clinical development. Eur Arch Psychiatry Clin Neurosci 2023: 1–12. [DOI] [PubMed] [Google Scholar]
- 213.Normann C, Schmitz D, Fürmaier A, Döing C, Bach M. Long-term plasticity of visually evoked potentials in humans is altered in major depression. Biol Psychiatry 2007; 62(5): 373–380. [DOI] [PubMed] [Google Scholar]
- 214.Kuhn M, Mainberger F, Feige B, Maier JG, Mall V, Jung NH et al. State-dependent partial occlusion of cortical LTP-like plasticity in major depression. Neuropsychopharmacology 2016; 41(6): 1521–1529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Noda Y, Zomorrodi R, Vila-Rodriguez F, Downar J, Farzan F, Cash RF et al. Impaired neuroplasticity in the prefrontal cortex in depression indexed through paired associative stimulation. Depress Anxiety 2018; 35(5): 448–456. [DOI] [PubMed] [Google Scholar]
- 216.Player MJ, Taylor JL, Weickert CS, Alonzo A, Sachdev P, Martin D et al. Neuroplasticity in depressed individuals compared with healthy controls. Neuropsychopharmacology 2013; 38(11): 2101–2108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Yu C, Li A, Li X, Chen Z, Wang P, Dong Z et al. Impaired LTD-like motor cortical plasticity in female patients with major depression disorder. Neuropharmacology 2020; 179: 108268. [DOI] [PubMed] [Google Scholar]